Traumatic Events and Eagle Syndrome: Is There Any Correlation? A Systematic Review
Abstract
:1. Introduction
- -
- “Stylo-hyoid classic syndrome”, which is characterized by pharyngeal pain aggravated by swallowing and frequently referred to the ear [2]. Other typical symptoms are headache and the sensation of a foreign body in the throat. Symptoms were thought to be due to impingement of cranial nerves (trigeminal, facial, glossopharyngeal or vagus) by the tip of the styloid process [5].
- -
- “Stylo-carotid artery syndrome” in which its vascular form is attributed to impingement of the internal carotid artery, extracranially, by the styloid process. This can cause a compression when turning the head or in “dissection” of the carotid artery resulting in a transient ischemic accident or stroke.
1.1. Etiopathogenesis
- -
- Theory of Reactive Hyperplasia.
- -
- Theory of Reactive Metaplasia.
- -
- Theory of Anatomic Variance [2].
1.2. Diagnosis
- Clinical manifestations.
- Digital palpation of the process in the tonsillar fossa.
- Radiological findings.
- Lidocaine infiltration test.
- -
- Lateral teleradiography of the head: a disadvantage is that the styloid processes of the two sides may overlap.
- -
- Anterolateral modified Towne’s radiograph: this procedure calculates both the medial and lateral deviation of the process.
- -
- Panoramic radiograph: using this procedure clinicians can typically consider the styloid process to be elongated if its length is more than 1/3 of the length of the ramus of the mandible. An advantage of the orthopantomograph is that the entire length of the styloid process is visible and its deviation can be measured quite accurately.
- -
- Computed tomography: is an effective method for evaluating styloid process length, angulation and other morphological characteristics.
- -
- Sagittal computed tomography angiography: in cases of vascular compression, it can also be effective in assessing blood flow disturbance [2].
1.3. Objectives
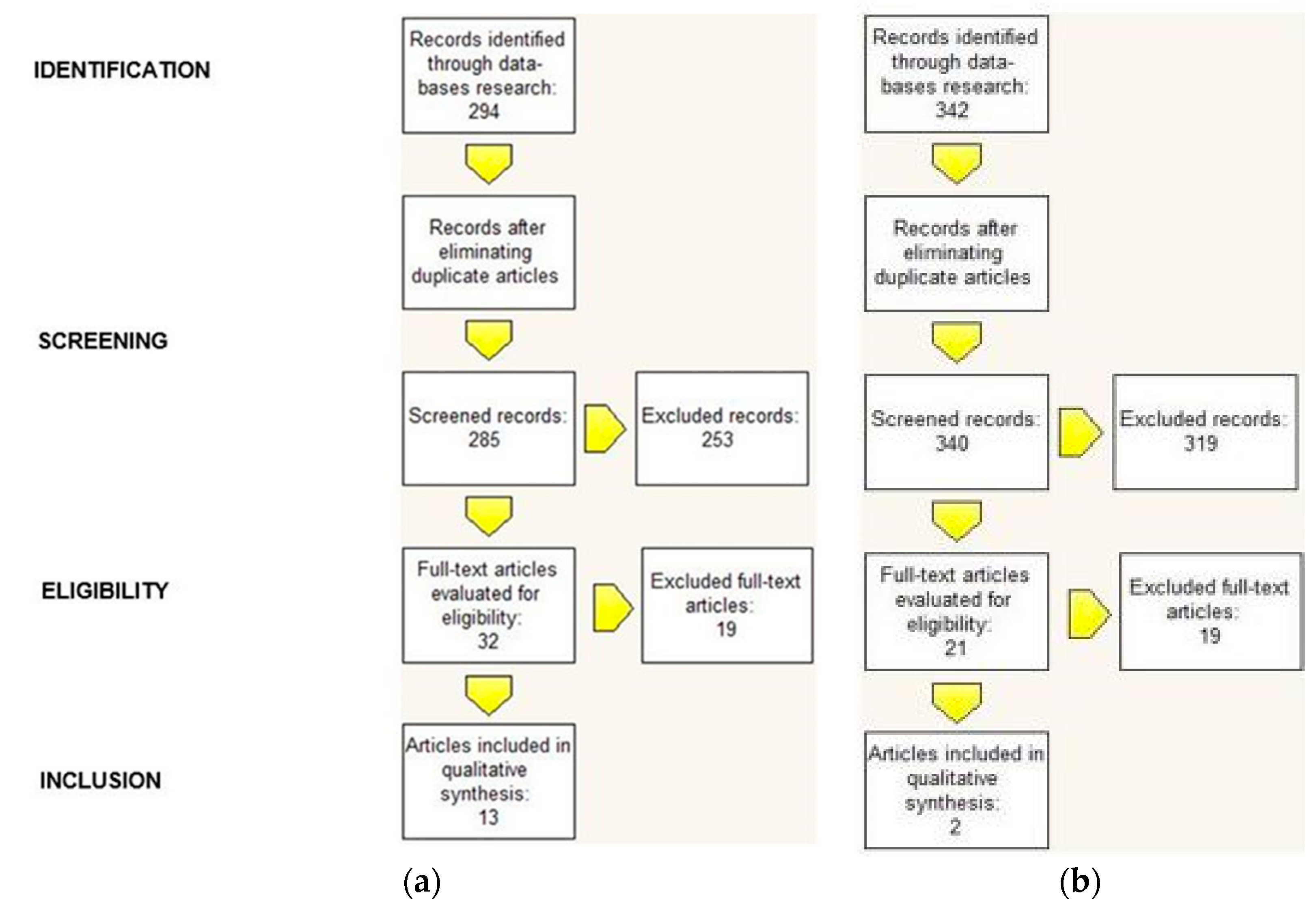
2. Systematic Review
2.1. Protocol and Registration
2.2. Eligibility Criteria
2.3. Information Sources, Search Strategy, and Study Selection
2.4. Data Items
2.5. Summary Measures and Approach to Synthesis
2.6. Risk of Bias
3. Results
3.1. Correlation between Eagle Syndrome and Traumatic Events
3.2. Correlation between Eagle Syndrome and Extractive Dental Events
- -
- Objective examination: extraoral palpation of a bony mass at the level of the tonsillar fossa area.
- -
- Instrumental examinations: panoramic radiograph and computed tomography scans of the neck.
4. Discussion
- (1)
- The traumatic fracture of the styloid process causes the proliferation of granulation tissue, which can compress adjacent structures and give rise to typical signs and symptoms.
- (2)
- The fractured portion can directly irritate or compress the adjacent noble structures and pharyngeal mucosa.
- (1)
- In cases in which the styloid process is initially normoconforming, the traumatic event may trigger two mechanisms that determine the lengthening of the styloid process and the ossification of the stylohyoid ligament:
- Theory of reactive hyperplasia: If the styloid process is properly stimulated by the pharyngeal trauma, ossification can continue from its end towards the stylohyoid ligament. This can occur in the post-trauma healing period and it mainly gives rise to symptoms related to carotid artery impingement.
- Theory of reactive metaplasia: the traumatic event in this case triggers several metaplastic variations at the level of the stylohyoid ligament that lead to its partial ossification. The eventuality of metaplasia can be attributed to the presence of bone centers, such as bone cells, osteoblasts and osteocytes, between the fibrous formations. In this case the symptoms would originate from the region of the stylohyoid ligament and would affect the soft tissues of the neck giving rise, for example, to dysphagia.
- (2)
- In other cases we can, instead, talk about a Theory of anatomical variability: bone and ligament are qualitatively normal and what varies is the lengthening of the styloid process. This theory explains why it is possible to find early radiographic evidence of this type of ossification in children and young adults who have not suffered any prior cervical-pharyngeal trauma. The fact that these anatomical structures are not normal is a risk factor, as traumatic events may trigger the typical symptoms of Eagle syndrome.
- -
- majority of case reports compared to systematic reviews or meta-analyses.
- -
- few works in which the syndrome was correlated with traumatic events.
- -
- articles correlating Eagle’s syndrome with tonsillectomy [19].
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Massey, E.W. Facial pain from an elongated styloid process (Eagle’s syndrome). South Med. J. 1978, 71, 1156–1159. [Google Scholar] [CrossRef] [PubMed]
- Piagkou, M.; Anagnostopoulou, S.; Kouladouros, K.; Piagkos, G. Eagle’s syndrome: A review of the literature. Clin. Anat. 2009, 22, 545–558. [Google Scholar] [CrossRef] [PubMed]
- Jewett, J.; Moriarity, R. Eagle syndrome: An incidental finding in a trauma patient: A case report. J. Emerg. Med. 2014, 46, e9–e12. [Google Scholar] [CrossRef] [PubMed]
- Sowmya, G.V.; Singh, M.P.; Manjunatha, B.S.; Nahar, P.; Astekar, M. A case of unilateral atypical orofacial pain with Eagle’s syndrome. J. Cancer Res. Ther. 2016, 12, 1323. [Google Scholar] [PubMed]
- Mann, A.; Kujath, S.; Friedell, M.L.; Hardouin, S.; Wood, C.; Carter, R.; Stark, K. Eagle Syndrome Presenting after Blunt Trauma. Ann. Vasc. Surg. 2017, 40, 295.e5–295.e8. [Google Scholar] [CrossRef] [PubMed]
- Klécha, A.; Hafian, H.; Devauchelle, B.; Lefèvre, B. A report of post-traumatic Eagle’s Syndrome. Int. J. Oral Maxillofac. Surg. 2008, 37, 970–972. [Google Scholar] [CrossRef] [PubMed]
- Shaifulizan, A.R.; Jaswinder, S.; Rubinderan, M.; Mohammad, K.A. The Development of Eagle’s Syndrome after Neck Trauma. Contemp. Clin. Dent. 2018, 9, 319–322. [Google Scholar]
- Bruno, G.; De Stefani, A.; Barone, M.; Costa, G.; Saccomanno, S.; Gracco, A. The validity of panoramic radiograph as a diagnostic method for elongated styloid process: A systematic review. CRANIO 2019, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Saccomanno, S.; Greco, F.; De Corso, E.; Lucidi, D.; Deli, R.; D’Addona, A.; Paludetti, G. Eagle’s Syndrome, from clinical presentation to diagnosis and surgical treatment: A case report. Acta Otorhinolaryngol. Ital. 2018, 38, 166–169. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.; Green, S. Cochrane Handbook for Systematic Reviews of Interventions, Version 5.1.0. Available online: http://handbook.cochrane.org/ (accessed on 1 December 2016).
- Péus, D.; Kollias, S.S.; Huber, A.M.; Huber, G.F. Recurrent unilateral peripheral facial palsy in a patient with an enlarged styloid process. Head Neck 2018, 41, E34–E37. [Google Scholar] [CrossRef] [PubMed]
- Todo, T.; Alexander, M.; Stokol, C.; Lyden, P.; Braunstein, G.; Gewertz, B. Eagle syndrome revisited: Cerebrovascular complications. Ann. Vasc. Surg. 2012, 26, 729.e1–729.e5. [Google Scholar] [CrossRef] [PubMed]
- Zammit, M.; Chircop, C.; Attard, V.; D’Anastasi, M. Eagle’s syndrome: A piercing matter. BMJ Case Rep. 2018, 11, e226611. [Google Scholar] [CrossRef] [PubMed]
- Schroeder, W. Traumatic Eagle’s syndrome. Otolaryngol. Head Neck Surg. 1991, 104, 371–374. [Google Scholar] [CrossRef] [PubMed]
- Blythe, J.N.; Matthews, N.S.; Connor, S. Eagle’s syndrome after fracture of the elongated styloid process. Br. J. Oral Maxillofac. Surg. 2009, 47, 233–235. [Google Scholar] [CrossRef] [PubMed]
- Koivumäki, A.; Marinescu-Gava, M.; Järnstedt, J.; Sándor, G.K.; Wolff, J. Trauma induced Eagle syndrome. Int. J. Oral Maxillofac. Surg. 2012, 41, 350–353. [Google Scholar] [CrossRef] [PubMed]
- Smith, G.R.; Cherry, J.E. Traumatic Eagle’s syndrome: Report of a case and review of the literature. J. Oral. Maxillofac. Surg. 1988, 46, 606–609. [Google Scholar] [CrossRef]
- Li, S.; Blatt, N.; Jacob, J.; Gupta, N.; Kumar, Y.; Smith, S. Provoked Eagle syndrome after dental procedure: A review of the literature. Neuroradiol. J. 2018, 31, 426–429. [Google Scholar] [CrossRef] [PubMed]
- Leong, S.C.; Karkos, P.D.; Papouliakos, S.M.; Apostolidou, M.T. Unusual complications of tonsillectomy: A systematic review. Am. J. Otolaryngol. 2007, 28, 419–422. [Google Scholar] [CrossRef] [PubMed]
| Correlation between Eagle Syndrome and Traumatic Events | Correlation between Eagle Syndrome and Extractive Dental Events |
|---|---|
| (EAGLE SYNDROME) OR EAGLE’S SYNDROME) OR ELONGATED STYLOID PROCESS) AND (TRAUMA) | (EAGLE SYNDROME) OR EAGLE’S SYNDROME) OR ELONGATED STYLOID PROCESS) AND (DENTAL PROCEDURE) OR TOOTH REMOVAL) OR EXTRACTION) OR DENTISTRY) |
| Title, Authors [Reference] | Article Type | Year | Sex | Age | Traumatic Event Referred | Symptoms | Diagnostic Tools | Diagnosis | Treatment |
|---|---|---|---|---|---|---|---|---|---|
| Facial pain from an elongated styloid process (Eagle’s syndrome) Massey E.W. [1] | Case Report | 1978 | F | 30 | Blunt trauma of left side occipital area | Headache on temporal and occipital area | Lateral Teleradiography of the head: bilaterally elongated styloid processes; left one fractured. | Classic Form | Conservative (no surgical or pharmacological therapy) |
| Eagle syndrome: an incidental finding in a trauma patient: A case report. Jewett et al. [3] | Case Report | 2014 | M | ~50 | Aggression | Neck and back pain; foreign body sensation of right side neck. | CT: elongated right styloid process and ossified right stylohyoid ligament. | Classic Form | Conservative (no surgical or pharmacological therapy) |
| Eagle Syndrome Presenting after Blunt Trauma, Mann A. et al. [5] | 3 Case Reports | 2016 | (5.1) F (5.2) F (5.3) M | (5.1) 73 (5.2) 39 (5.3) 38 | ((5.1) Accidental fall (5.2) Motorbike accident (5.3) Aggression | (5.1) dizziness when rotating head to the left (5.2) left hemiparesis (5.3) left side cervical pain; aphasia; foreign body sensation in pharynx. | (5.1) CT: bilaterally ossified stylohyoid ligament; (5.2) CT: fractured right styloid process; ossified stylohyoid ligament; internal carotid dissecation; (5.3) CT: styloid process contacts internal carotid. | Stylo-Carotid Form | (5.1) Unavailable follow-up; (5.2) Pharmacological and conservative therapy; (5.3) Vascular surgery: stent. |
| A report of post-traumatic Eagle’s Syndrome. Klècha A. et al. [6] | Case Report | 2008 | F | 39 | Car accident with whiplash | Right side TMJ pain; pharyngeal pain; right side ear pain; insomnia; cracking sensation | Panoramic Radiograph: bilaterally ossified stylohyoid ligaments. | Classic Form | Surgical intervention to remove styloid process and part of the stylohyoid ligament with transcervical approach. |
| The Development of Eagle’s Syndrome after Neck Trauma, Shaifulizan AR. et al. [7] | Case Report | 2018 | F | 43 | Trauma while chewing | Persistent pain on the right side of the neck irradiated to the face, temporal and occipital area; pain in the right mandibular angle. | Panoramic Radiograph: elongated right styloid process. Cone Beam CT: right styloid process = 48 mm, left styloid processs = 37 mm | Classic Form | Surgical intervention to remove styloid process with transcervical approach. |
| Recurrent unilateral peripheral facial palsy in a patient with an enlarged styloid process. Peùs D. et al. [11] | Case Report | 2018 | M | 39 | Blunt trauma | Episodes of left hemifacial paresis. | Electroneurography: marked comparative amplitude reduction on the left side -> axonal damage of the left facial nerve MRI + CT: elongated and fractured from its basis left styloid process. | Classic Form with Stylo-Carotid Form Symptoms | Surgical intervention to remove styloid process with transcervical approach. |
| Title | Article Type | Yezar | Sex | Age | Traumatic Event Referred | Symptoms | Diagnostic Tools | Diagnosis | Treatment |
|---|---|---|---|---|---|---|---|---|---|
| Eagle syndrome revisited: cerebrovascular complications. Todo, T. et al. [12] | Case Report | 2012 | M | 57 | Neck manipulation | Transient aphasia; left side neck pain; unstable gait. | Angio CT: bilaterally elongated styloid processes; Angio RMN: bilateral carotid dissecation; MRI: bilateral cortical and subcortical frontoparietal ischemia | Stylo-Carotid Form | Vascular surgery: left carotid trombectomy; angioplasty; stent. |
| Eagle’s syndrome: a piercing matter. Zammit et al. [13] | Case Report | 2018 | M | 45 | Motorbike accident | Right side headache; facial numbness; heavy tongue feeling; right side movements reduction. | CT: bilateral internal carotid dissecation; Angio CT: bilaterally elongated styloid processes. | Stylo-Carotid Form | Pharmacological. |
| Traumatic Eagle’s syndrome. Schroeder W. [14] | Case Report | 1991 | M | 20 | Motorbike accident with right side trauma of the neck and the face | Tenderness on right side neck and mandible; temporomandibular pain in mouth opening and closing | Panoramic Radiograph and Lateral Teleradiography: elongated and fractured right styloid process. | Classic Form | Surgical intervention to remove right styloid process through transpharyngeal approach. |
| Eagle’s syndrome after fracture of the elongated styloid process. Blythe J.L. et al. [15] | Case Report | 2009 | F | 43 | Trauma while chewing | Sharp pain in left submandibular area; left ear crackling | Observation: 20 × 20 mm mass in left submandibular area; tonsillar fossa palpation: pain; CT: elongated and fractured left styloid process. | Classic Form | Conservative and pharmacological therapy with analgesics |
| Trauma induced Eagle syndrome. Koivumäki A. et al. [16] | Case Report | 2012 | F | 52 | Aggression | Left mandible and dysphagia discomfort | Ear area and tonsillar fossa palpation: pain; Panoramic Radiograph: ossified left stylohyoid ligament; CT: left stylohyoid ligament ossified from cranial base to hyoid bone. | Classic Form | Surgical intervention to remove calcified portion through transpharyngeal approach. |
| Traumatic Eagle’s syndrome: report of a case and review of the literature. Smith et al. [17] | Report and review | 1988 | M | 20 | Blunt trauma of righ side mandible | Dysphagia; chewing pain; pain on the right side of the neck; pain when rotating head | Panoramic Radiograph: bilaterally elongated styloid processes; right one fractured; ossified stylohyoid ligaments. | Classic Form | Surgical intervention to remove right styloid process through transpharyngeal approach. |
| Title, Authors [Reference] | Article Type | Year | Sex | Age | Traumatic Event Referred | Symptoms | Diagnostic Tools | Diagnosis | Treatment |
|---|---|---|---|---|---|---|---|---|---|
| A case of unilateral atypical orofacial pain with Eagle’s syndrome. Sowmya GV [4] | Case Report | 2016 | M | 38 | Extraction of the lower right back tooth, three months prior. | Pain in the right side of his face since two months; moderate and intermittent pain radiated to the right temporal and neck region; restricted neck movements on the right side. | Objective examination: extraoral palpation of a bone mass at the level of the tonsillar fossa area; Panoramic Radiograph: bilaterally elongated and ossified styloid processes; CT scan of the neck: right styloid process = 48 mm, left styloid process = 40 mm. | Classic Form | Pharmacological therapy with Diazepam for 5 days, NSAIDs and TENS |
| Provoked Eagle syndrome after dental procedure: A review of the literature. Li S. [18] | Case Report | 2018 | M | 36 | Tooth extraction. | Odynophagia for five days; pain was described as 10/10 in intensity, continuous, sharp, non-radiating, associated with globus sensation, cyclical vomiting and dysphagia; worsening of the pain on swallowing, yawning and chewing. | CT scan of the neck: bilaterally elongated styloid processes: right styloid process = 46 mm left styloid process = 47 mm. | Classic Form | Pharmacological therapy with analgesics. Unavailable follow-up. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Saccomanno, S.; Quinzi, V.; D’Andrea, N.; Albani, A.; Coceani Paskay, L.; Marzo, G. Traumatic Events and Eagle Syndrome: Is There Any Correlation? A Systematic Review. Healthcare 2021, 9, 825. https://doi.org/10.3390/healthcare9070825
Saccomanno S, Quinzi V, D’Andrea N, Albani A, Coceani Paskay L, Marzo G. Traumatic Events and Eagle Syndrome: Is There Any Correlation? A Systematic Review. Healthcare. 2021; 9(7):825. https://doi.org/10.3390/healthcare9070825
Chicago/Turabian StyleSaccomanno, Sabina, Vincenzo Quinzi, Nicola D’Andrea, Arianna Albani, Licia Coceani Paskay, and Giuseppe Marzo. 2021. "Traumatic Events and Eagle Syndrome: Is There Any Correlation? A Systematic Review" Healthcare 9, no. 7: 825. https://doi.org/10.3390/healthcare9070825
APA StyleSaccomanno, S., Quinzi, V., D’Andrea, N., Albani, A., Coceani Paskay, L., & Marzo, G. (2021). Traumatic Events and Eagle Syndrome: Is There Any Correlation? A Systematic Review. Healthcare, 9(7), 825. https://doi.org/10.3390/healthcare9070825









