Natural History of Isolated Below-Knee Vein Thrombosis in Patients with Spinal Cord Injury
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Participants
2.2. Statistical Analyses
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Prevention of venous thromboembolism in individuals with spinal cord injury: Clinical practice guidelines for health care providers. Top Spinal Cord. Inj. Rehabil. 2016, 22, 209–240. [CrossRef] [PubMed]
- Miranda, A.R.; Hassouna, H.I. Mechanisms of thrombosis in spinal cord injury. Hematol. Oncol. Clin. N. Am. 2000, 14, 401–416. [Google Scholar] [CrossRef]
- Authors/Task Force Members; Konstantinides, S.V.; Torbicki, A.; Agnelli, G.; Danchin, N.; Fitzmaurice, D.; Galiè, N.; Gibbs, J.S.R.; Huisman, M.V.; Humbert, M.; et al. 2014 ESC Guidelines on the diagnosis and management of acute pulmonary embolism: The Task Force for the Diagnosis and Management of Acute Pulmonary Embolism of the European Society of Cardiology (ESC) Endorsed by the European Respiratory Society (ERS). Eur. Heart J. 2014, 35, 3033–3080. [Google Scholar]
- Lee, L.H.; Gallus, A.; Jindal, R.; Wang, C.; Wu, C.-C. Incidence of venous thromboembolism in Asian populations: A systematic review. Thromb. Haemost. 2017, 117, 2243–2260. [Google Scholar] [CrossRef]
- Koh, I.J.; Kim, J.H.; Kim, M.S.; Jang, S.W.; Kim, C.; In, Y. Is routine thromboprophylaxis needed in Korean patients undergoing unicompartmental knee arthroplasty? J. Korean Med. Sci. 2016, 31, 443. [Google Scholar] [CrossRef] [Green Version]
- Do, J.G.; Kim, D.H.; Sung, D.H. Incidence of deep vein thrombosis after spinal cord injury in Korean patients at acute rehabilitation unit. J. Korean Med. Sci. 2013, 28, 1382. [Google Scholar] [CrossRef] [Green Version]
- Anwar, F.; Al-Khayer, A.; El-Mahrouki, H.; Purcell, M. Gastrointestinal bleeding in spinal injuries patient: Is prophylaxis essential. Alcohol 2013, 6, a607. [Google Scholar]
- Liew, N.C.; Alemany, G.V.; Angchaisuksiri, P.; Bang, S.M.; Choi, G.; De Silva, D.A.; Hong, J.M.; Lee, L.; Li, Y.J.; Rajamoney, G.N.; et al. Asian venous thromboembolism guidelines: Updated recommendations for the prevention of venous thromboembolism. J. Int. Union Angiol. 2016, 36, 1–20. [Google Scholar]
- Kearon, C.; Akl, E.A.; Ornelas, J.; Blaivas, A.; Jimenez, D.; Bounameaux, H.; Huisman, M.; King, C.S.; Morris, T.A.; Sood, N.; et al. Antithrombotic therapy for VTE disease: CHEST guideline and expert panel report. Chest 2016, 149, 315–352. [Google Scholar] [CrossRef]
- Fehlings, M.G.; Tetreault, L.A.; Aarabi, B.; Anderson, P.; Arnold, P.M.; Brodke, D.S.; Burns, A.S.; Chiba, K.; Dettori, J.R.; Furlan, J.C.; et al. A Clinical Practice Guideline for the Management of Patients with Acute Spinal Cord Injury: Recommendations on the Type and Timing of Anticoagulant Thromboprophylaxis. Glob. Spine J. 2017, 7, 212S–220S. [Google Scholar] [CrossRef]
- Guyatt, G.H.; Akl, E.A.; Crowther, M.; Schünemann, H.J.; Gutterman, D.D.; Lewis, S.Z. Introduction to the ninth edition: Antithrombotic therapy and prevention of thrombosis: American College of Chest Physicians evidence-based clinical practice guidelines. Chest 2012, 141, 48S–52S. [Google Scholar] [CrossRef] [Green Version]
- Fleck, D.; Albadawi, H.; Wallace, A.; Knuttinen, G.; Naidu, S.; Oklu, R. Below-knee deep vein thrombosis (DVT): Diagnostic and treatment patterns. Cardiovasc. Diagn. Ther. 2017, 7 (Suppl. 3), S134. [Google Scholar] [CrossRef]
- Marino, R.J.; Graves, D.E. Metric properties of the ASIA motor score: Subscales improve correlation with functional activities11No commercial party having a direct financial interest in the results of the research supporting this article has or will confer a benefit upon the author(s) or upon any organization with which the author(s) is/are associated. Arch. Phys. Med. Rehabil. 2004, 85, 1804–1810. [Google Scholar]
- Cifu, D.X. Braddom’s Physical Medicine and Rehabilitation; Elsevier Health Sciences: Philadelphia, PA, USA, 2020. [Google Scholar]
- Geerts, W.H.; Code, K.I.; Jay, R.M.; Chen, E.; Szalai, J.P. A prospective study of venous thromboembolism after major trauma. N. Engl. J. Med. 1994, 331, 1601–1606. [Google Scholar] [CrossRef]
- Spinal Cord Injury Thromboprophylaxis Investigators. Prevention of venous thromboembolism in the rehabilitation phase after spinal cord injury: Prophylaxis with low-dose heparin or enoxaparin. J. Trauma Acute Care Surg. 2003, 54, 1111–1115. [Google Scholar] [CrossRef]
- Klatsky, A.L.; Armstrong, M.A.; Poggi, J. Risk of pulmonary embolism and/or deep venous thrombosis in Asian-Americans. Am. J. Cardiol. 2000, 85, 1334–1337. [Google Scholar] [CrossRef]
- Masuda, E.M.; Kistner, R.L. The case for managing calf vein thrombi with duplex surveillance and selective anticoagulation. Disease-A-Month 2010, 10, 601–613. [Google Scholar] [CrossRef]
- Monreal, M.; Ruiz, J.; Olazabal, A.; Arias, A.; Roca, J. Deep venous thrombosis and the risk of pulmonary embolism: A systematic study. Chest 1992, 102, 677–681. [Google Scholar]
- Shin, J.C.; Kim, D.H.; Yu, S.J.; Yang, H.E.; Yoon, S.Y. Epidemiologic change of patients with spinal cord injury. Ann. Rehabil. Med. 2013, 37, 50. [Google Scholar] [CrossRef] [Green Version]
- El Masri, W.; Cochrane, P.; Silver, J. Gastrointestinal bleeding in patients with acute spinal injuries. Injury 1982, 14, 162–167. [Google Scholar] [CrossRef]
- Leramo, O.B.; Tator, C.H.; Hudson, A.R. Massive gastroduodenal hemorrhage and perforation in acute spinal cord injury. Surg. Neurol. 1982, 17, 186–190. [Google Scholar] [CrossRef]
- Chikuda, H.; Yasunaga, H.; Takeshita, K.; Horiguchi, H.; Kawaguchi, H.; Ohe, K.; Fushimi, K.; Tanaka, S. Mortality and morbidity after high-dose methylprednisolone treatment in patients with acute cervical spinal cord injury: A propensity-matched analysis using a nationwide administrative database. Emerg. Med. J. 2014, 31, 201–206. [Google Scholar] [CrossRef]
- Hammond, F.M.; Horn, S.D.; Smout, R.J.; Chen, D.; DeJong, G.; Scelza, W.; Jha, A.; Ballard, P.H.; Bloomgarden, J. Acute Rehospitalizations During Inpatient Rehabilitation for Spinal Cord Injury. Arch. Phys. Med. Rehabil. 2013, 94, S98–S105. [Google Scholar] [CrossRef] [PubMed]
- Mowrey, K. The challenge of assessing and diagnosing acute abdomen in tetraplegics: A case study. J. Neurosci. Nurs. 2007, 39, 5–8. [Google Scholar] [CrossRef]
- Johnsen, S.P.; Sørensen, H.T.; Mellemkjœr, L.; Blot, W.J.; Nielsen, G.L.; McLaughlin, J.K.; Olsen, J.H. Hospitalisation for upper gastrointestinal bleeding associated with use of oral anticoagulants. Thromb. Haemost. 2001, 86, 563–568. [Google Scholar]
- Schwartz, T.; Hingorani, A.; Ascher, E.; Marks, N.; Shiferson, A.; Jung, D.; Jimenez, R.; Jacob, T. Pulmonary Embolism Without Deep Venous Thrombosis. Ann. Vasc. Surg. 2012, 26, 973–976. [Google Scholar] [CrossRef]
| Variable | Data |
|---|---|
| Age (Median, interquartile range) | 66.0, 54.0–74.5 |
| lower-extremity motor score (Median, interquartile range) | 28.0, 11.0–32.0 |
| Sex (Male: Female) | 19:8 |
| Ambulation (No. of patients) Sitter: Walker | 22:5 |
| Cause of injury (No. of patients) | |
| Traumatic | 12 |
| Non-traumatic | |
| Spondylotic myelopathy | 12 |
| Cord infarct | 1 |
| Metastasis | 2 |
| Initial Duplex ultrasound (No. of patients, %) | |
| Unilateral: Bilateral | 14(51.9%): 13(48.1%) |
| Follow-up duplex ultrasound (No. of patients) Non-DVT: DVT | 11:16 |
| Interval (day) between duplex ultrasound (median, interquartile range) | 17.0, 10.0–23.5 |
| The American Spinal Injury Association Impairment Scale (No. of patients, %) | |
| A | 1 (3.7%) |
| B | 6 (22.3%) |
| C | 10 (37.0%) |
| D | 10 (37.0%) |
| Non–NOAC Group | NOAC Group | p-Value | |
|---|---|---|---|
| Number | 16 | 11 | |
| The American Spinal Injury Association Impairment Scale | |||
| (No. of patients, %) | |||
| A | 0 | 1 | |
| B | 6 | 0 | |
| C | 4 | 6 | |
| D | 6 | 4 | |
| Age (median, interquartile range) | 68, 60–68 | 63, 50.5–67.5 | 0.25 |
| Male and Female (No. of patients) | 12:4 | 7:4 | 0.675 |
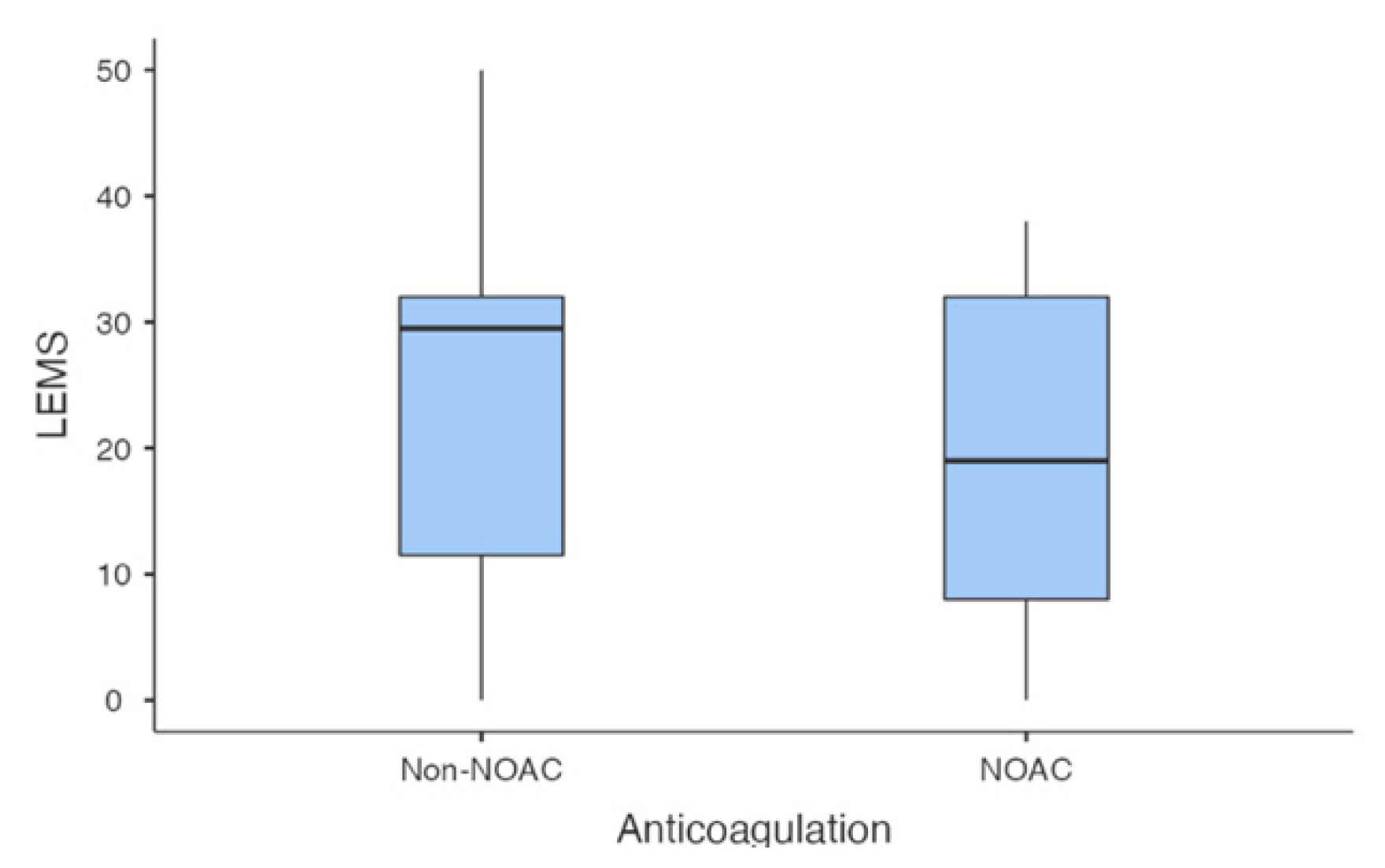
| lower-extremity motor score (median, interquartile range) | 29.5, 11.5–32.0 | 19, 8.0–32.0 | 0.40 |
| Ambulation (No. of patients) | |||
| Sitter vs. walker | 13:3 | 9:2 | 0.97 |
| Initial duplex ultrasound (No. of patients) | |||
| Unilateral:Bilateral | 10:6 | 4:7 | 0.18 |
| Trauma vs. Non-trauma (No. of patients) | 8:8 | 4:7 | 0.69 |
| Operation vs. Non-operation (No. of patients) | 12:4 | 10:1 | 0.61 |
| Follow-up Duplex ultrasound | |||
| (No. of patients) | |||
| No DVT vs. DVT | 5:11 | 6:5 | |
| Proximal propagation | 0 | 0 | 0.23 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cho, J.-H.; Lee, D.-G. Natural History of Isolated Below-Knee Vein Thrombosis in Patients with Spinal Cord Injury. Healthcare 2021, 9, 861. https://doi.org/10.3390/healthcare9070861
Cho J-H, Lee D-G. Natural History of Isolated Below-Knee Vein Thrombosis in Patients with Spinal Cord Injury. Healthcare. 2021; 9(7):861. https://doi.org/10.3390/healthcare9070861
Chicago/Turabian StyleCho, Jang-Hyuk, and Dong-Gyu Lee. 2021. "Natural History of Isolated Below-Knee Vein Thrombosis in Patients with Spinal Cord Injury" Healthcare 9, no. 7: 861. https://doi.org/10.3390/healthcare9070861
APA StyleCho, J.-H., & Lee, D.-G. (2021). Natural History of Isolated Below-Knee Vein Thrombosis in Patients with Spinal Cord Injury. Healthcare, 9(7), 861. https://doi.org/10.3390/healthcare9070861






