Six-Month Outcomes in COVID-19 ICU Patients and Their Family Members: A Prospective Cohort Study
Abstract
:1. Introduction
2. Materials & Methods
2.1. Study Participants
2.2. Procedure
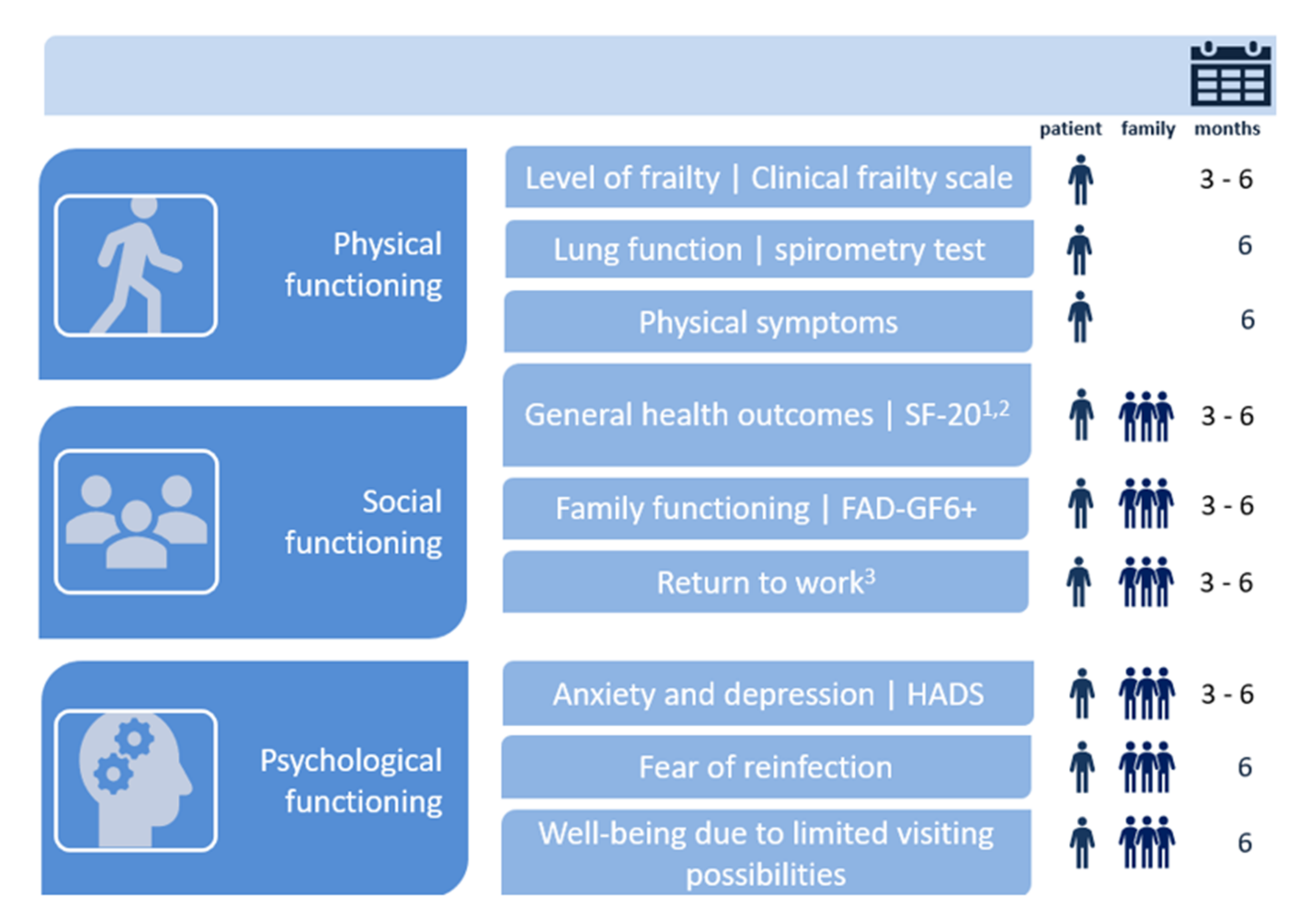
2.3. Outcomes
2.4. Statistical Analysis
3. Results
3.1. Baseline Characteristics
3.2. Results on Health Domains
3.2.1. Physical Functioning
3.2.2. Social Functioning
3.2.3. Psychological Functioning
3.3. Health Care Consumption
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ACCI | Age-adjusted Charlson Comorbidity Index |
| ARDS | Acute respiratory distress syndrome |
| CFS | Clinical Frailty Scale |
| COVID-19 | Coronavirus disease 2019 |
| DLCO | Diffusing lung capacity for carbon monoxide |
| FAD-GF6 | Family Assessment Device |
| FEV1 | Forced expiratory volume in 1 s |
| FEV1/FVC | Forced expiratory ratio |
| COFICS | COVID-19 Follow-up Intensive Care Studies |
| FVC | Forced vital capacity |
| HADS | Hospital Anxiety and Depression Scale |
| ICU | Intensive Care Unit |
| MERS | Middle East Respiratory Syndrome |
| QoL | Quality of Life domains |
| SARS | Severe acute respiratory syndrome |
| SF-20 | Short-Form General Health Survey |
| TLC | Total lung capacity |
Appendix A

References
- World Health Organization: Coronavirus Disease (COVID-2019) Weekly Epidemiological Update 1 June 2021; World Health Organization: Geneva, Switzerland, 2021; Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports (accessed on 3 June 2021).
- Ahmed, H.; Patel, K.; Greenwood, D.C.; Halpin, S.; Lewthwaite, P.; Salawu, A.; Eyre, L.; Breen, A.; O’Connor, R.; Jones, A.; et al. Long-term clinical outcomes in survivors of severe acute respiratory syndrome and Middle East respiratory syndrome coronavirus outbreaks after hospitalisation or ICU admission: A systematic review and meta-analysis. J. Rehabil. Med. 2020, 52, jrm00063. [Google Scholar] [CrossRef]
- Stam, H.J.; Stucki, G.; Bickenbach, J. Covid-19 and Post Intensive Care Syndrome: A Call for Action. J. Rehabil. Med. 2020, 52, jrm00044. [Google Scholar] [CrossRef]
- Federatie Medisch Specialisten. Standpunt Nazorg Voor IC-Patienten Met COVID-19. Available online: http://www.fms.nl (accessed on 23 October 2020).
- Grasselli, G.; Greco, M.; Zanella, A.; Albano, G.; Antonelli, M.; Bellani, G.; Bonanomi, E.; Cabrini, L.; Carlesso, E.; Castelli, G.; et al. Risk Factors Associated with Mortality among Patients with COVID-19 in Intensive Care Units in Lombardy, Italy. JAMA Intern. Med. 2020, 180, 1345–1355. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez-Morales, A.J.; Cardona-Ospina, J.A.; Gutiérrez-Ocampo, E.; Villamizar-Peña, R.; Holguin-Rivera, Y.; Escalera-Antezana, J.P.; Alvarado-Arnez, L.E.; Bonilla-Aldana, D.K.; Franco-Paredes, C.; Henao-Martinez, A.F.; et al. Clinical, laboratory and imaging features of COVID-19: A systematic review and meta-analysis. Travel Med. Infect. Dis. 2020, 34, 101623. [Google Scholar] [CrossRef]
- Zhou, F.; Yu, T.; Du, R.; Fan, G.; Liu, Y.; Liu, Z.; Xiang, J.; Wang, Y.; Song, B.; Gu, X.; et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet 2020, 395, 1054–1062. [Google Scholar] [CrossRef]
- Docherty, A.B.; Harrison, E.M.; Green, C.A.; Hardwick, H.E.; Pius, R.; Norman, L.; Holden, K.A.; Read, J.M.; Dondelinger, F.; Carson, G.; et al. Features of 20,133 UK patients in hospital with COVID-19 using the ISARIC WHO Clinical Characterisation. Protocol: Prospective observational cohort study. BMJ 2020, 369, m1985. [Google Scholar] [CrossRef] [PubMed]
- Needham, D.M.; Davidson, J.; Cohen, H.; Hopkins, R.O.; Weinert, C.; Wunsch, H.; Zawistowski, C.; Bemis-Dougherty, A.; Berney, S.C.; Bienvenu, O.J.; et al. Improving long-term outcomes after discharge from intensive care unit: Report from a stakeholders’ conference. Crit. Care Med. 2012, 40, 502–509. [Google Scholar] [CrossRef] [PubMed]
- Rawal, G.; Yadav, S.; Kumar, R. Post-intensive Care Syndrome: An Overview. J. Transl. Int. Med. 2017, 5, 90–92. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Harvey, M.A.; Davidson, J.E. Postintensive Care Syndrome: Right Care, Right Now… and Later. Crit. Care Med. 2016, 44, 381–385. [Google Scholar] [CrossRef]
- Lemmers, A.L.; Van der Voort, P.H.J. Trust in Intensive Care Patients, Family, and Healthcare Professionals: The Development of a Conceptual Framework Followed by a Case Study. Healthcare 2021, 9, 208. [Google Scholar] [CrossRef] [PubMed]
- Chen, K.Y.; Li, T.; Gong, F.H.; Zhang, J.S.; Li, X.K. Predictors of Health-Related Quality of Life and Influencing Factors for COVID-19 Patients, a Follow-Up at One Month. Front. Psychiatry 2020, 11, 668. [Google Scholar] [CrossRef]
- Carfi, A.; Bernabei, R.; Landi, F.; Gemelli against COVID-19 Post-Acute Care Study Group. Persistent Symptoms in Patients After Acute COVID-19. JAMA 2020, 324, 603–605. [Google Scholar] [CrossRef] [PubMed]
- Wong, A.W.; Shah, A.S.; Johnston, J.C.; Carlsten, C.; Ryerson, C.J. Patient-reported outcome measures after COVID-19: A prospective cohort study. Eur. Respir. J. 2020, 56, 2003276. [Google Scholar] [CrossRef] [PubMed]
- Garrigues, E.; Janvier, P.; Kherabi, Y.; Le Bot, A.; Hamon, A.; Gouze, H.; Doucet, L.; Berkani, S.; Oliosi, E.; Mallart, E.; et al. Post-discharge persistent symptoms and health-related quality of life after hospitalization for COVID-19. J. Infect. 2020, 81, e4–e6. [Google Scholar] [CrossRef] [PubMed]
- Halpin, S.J.; McIvor, C.; Whyatt, G.; Adams, A.; Harvey, O.; McLean, L.; Walshaw, C.; Kemp, S.; Corrado, J.; Singh, R.; et al. Postdischarge symptoms and rehabilitation needs in survivors of COVID-19 infection: A cross-sectional evaluation. J. Med. Virol. 2021, 93, 1013–1022. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.; Huang, L.; Wang, Y.; Li, X.; Ren, L.; Gu, X.; Kang, L.; Guo, L.; Liu, M.; Zhou, X.; et al. 6-month consequences of COVID-19 in patients discharged from hospital: A cohort study. Lancet 2021, 16, 397. [Google Scholar]
- Van der Sar-van der Brugge, S.; Talman, S.; Boonman-de Winter, L.; de Mol, M.; Hoefman, E.; van Etten, R.W.; De Backer, I.C. Pulmonary function and health-related quality of life after COVID-19 pneumonia. Respir. Med. 2021, 176, 106272. [Google Scholar] [CrossRef] [PubMed]
- Holler, J.G.; Eriksson, R.; Jensen, T.Ø.; van Wijhe, M.; Fischer, T.K.; Søgaard, O.S. First wave of COVID-19 hospital admissions in Denmark: A Nationwide population-based cohort study. BMC Infect. Dis. 2021, 21, 39. [Google Scholar] [CrossRef]
- Cardoso, F.S.; Papoila, A.L.; Machado, R.S.; Fidalgo, P. Age, sex, and comorbidities predict ICU admission or mortality in cases with SARS-CoV2 infection: A population-based cohort study. Crit. Care 2020, 24, 465. [Google Scholar] [CrossRef] [PubMed]
- Rockwood, K.; Song, X.; MacKnight, C.; Fidalgo, P. A global clinical measure of fitness and frailty in elderly people. CMAJ 2005, 173, 489–495. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kempen, G.I. The MOS Short-Form General Health Survey: Single item vs multiple measures of health-related quality of life: Some nuances. Psychol. Rep. 1992, 70, 608–610. [Google Scholar] [CrossRef] [PubMed]
- Van Kempen, G.I.; Brilman, E.I.; Heyink, J.W.; Ormel, J. Het meten van de algemene gezondheidstoestand met de MOS Short-Form General Health Survey (SF-20), een handleiding. In Tweede Herziene Druk; Research Institute SHARE, Rijksuniversiteit Groningen, UMCG: Groningen, The Netherlands, 2012. [Google Scholar]
- Hamilton, E.; Carr, A. Systematic Review of Self-Report Family Assessment Measures. Fam. Process. 2016, 55, 16–30. [Google Scholar] [CrossRef] [PubMed]
- Boterhoven de Haan, K.L.; Hafekost, J.; Lawrence, D.; Sawyer, M.G.; Zubrick, S.R. Reliability and validity of a short version of the general functioning subscale of the McMaster Family Assessment Device. Fam. Process. 2015, 54, 116–123. [Google Scholar] [CrossRef]
- Miller, I.W.; Ryan, C.E.; Keitner, G.I.; Bishop, D.S.; Epstein, N.B. The McMaster approach to families: Theory, assessment, treatment and research. J. Fam. Ther. 2000, 22, 168–189. [Google Scholar] [CrossRef]
- Kamdar, B.B.; Suri, R.; Suchyta, M.R.; Digrande, K.F.; Sherwood, K.D.; Colantuoni, E.; Dinglas, V.D.; Needham, D.M.; Hopkins, R.O. Return to work after critical illness: A systematic review and meta-analysis. Thorax 2020, 75, 17–27. [Google Scholar] [CrossRef]
- Zigmond, A.S.; Snaith, R.P. The Hospital Anxiety and Depression Scale. Acta Psychiatr. Scand. 1983, 67, 361–370. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Charlson, M.; Szatrowski, T.P.; Peterson, J.; Gold, J. Validation of a combined comorbidity index. J. Clin. Epidemiol. 1994, 47, 1245–1251. [Google Scholar] [CrossRef]
- Herridge, M.S.; Cheung, A.M.; Tansey, C.M.; Matte-Martyn, A.; Diaz-Granados, N.; Al-Saidi, F.; Cooper, A.B.; Guest, C.B.; Mazer, C.D.; Mehta, S.; et al. One-year outcomes in survivors of the acute respiratory distress syndrome. N. Engl. J. Med. 2003, 348, 683–693. [Google Scholar] [CrossRef] [Green Version]
- Dowdy, D.W.; Eid, M.P.; Dennison, C.R.; Mendez-Tellez, P.A.; Herridge, M.S.; Guallar, E.; Pronovost, P.J.; Needham, D.M. Quality of life after acute respiratory distress syndrome: A meta-analysis. Intensive Care Med. 2006, 32, 1115–1124. [Google Scholar] [CrossRef] [PubMed]
- Parker, A.M.; Sricharoenchai, T.; Raparla, S.; Schneck, K.W.; Bienvenu, O.J.; Needham, D.M. Posttraumatic stress disorder in critical illness survivors: A metaanalysis. Crit. Care Med. 2015, 43, 1121–1129. [Google Scholar] [CrossRef] [PubMed]
- Sasannejad, C.; Ely, E.W.; Lahiri, S. Long-term cognitive impairment after acute respiratory distress syndrome: A review of clinical impact and pathophysiological mechanisms. Crit. Care 2019, 23, 352. [Google Scholar] [CrossRef] [Green Version]
- De Biasio, J.C.; Mittel, A.M.; Mueller, A.L.; Ferrante, L.E.; Kim, D.H.; Shaefi, S. Frailty in Critical Care Medicine: A Review. Anesth. Analg. 2020, 130, 1462–1473. [Google Scholar] [CrossRef]
- Mo, X.; Jian, W.; Su, Z.; Chen, M.; Peng, H.; Lei, C.; Chen, R.; Zhong, N.; Li, S. Abnormal pulmonary function in COVID-19 patients at time of hospital discharge. Eur. Respir. J. 2020, 55, 2001217. [Google Scholar] [CrossRef] [PubMed]
- Liu, K.; Zhang, W.; Yang, Y.; Zhang, J.; Li, Y.; Chen, Y. Respiratory rehabilitation in elderly patients with COVID-19: A randomized controlled study. Complement. Ther. Clin. Pract. 2020, 39, 101166. [Google Scholar] [CrossRef] [PubMed]
- Agård, A.S.; Lomborg, K.; Tønnesen, E.; Egerod, I. Rehabilitation activities, out-patient visits and work in patients and partners the first year after ICU: A descriptive study. Intensive Crit. Care Nurs. 2014, 30, 101–110. [Google Scholar] [CrossRef] [PubMed]
- Van Beusekom, I.; Bakhshi-Raiez, F.; De Keizer, N.F.; Dongelmans, D.A.; Van der Schaaf, M. Reported burden on informal caregivers of ICU survivors: A literature review. Crit. Care 2016, 20, 16. [Google Scholar] [CrossRef] [Green Version]
- Huang, M.; Parker, A.M.; Bienvenu, O.J.; Dinglas, V.D.; Colantuoni, E.; Hopkins, R.O.; Needham, D.M.; National Institutes of Health, National Heart, Lung, and Blood Institute; Acute Respiratory Distress Syndrome Network. Psychiatric Symptoms in Acute Respiratory Distress Syndrome Survivors: A 1-Year National Multicenter Study. Crit. Care Med. 2016, 44, 954–965. [Google Scholar] [CrossRef] [PubMed]
- Chelluri, L.; Im, K.A.; Belle, S.H.; Schulz, R.; Rotondi, A.J.; Donahoe, M.P.; Sirio, C.A.; Mendelsohn, A.B.; Pinsky, M.R. Long-term mortality and quality of life after prolonged mechanical ventilation. Crit. Care Med. 2004, 32, 61–69. [Google Scholar] [CrossRef] [PubMed]
- Montgomery, C.L.; Rolfson, D.B.; Bagshaw, S.M. Frailty and the Association Between Long-Term Recovery After Intensive Care Unit Admission. Crit. Care Clin. 2018, 34, 527–547. [Google Scholar] [CrossRef] [PubMed]
- Cox, C.E.; Docherty, S.L.; Brandon, D.H.; Whaley, C.; Attix, D.K.; Clay, A.S.; Dore, D.V.; Hough, C.L.; White, D.B.; Tulsky, J.A. Surviving critical illness: Acute respiratory distress syndrome as experienced by patients and their caregivers. Crit. Care Med. 2009, 37, 2702–2708. [Google Scholar] [CrossRef] [PubMed]
- Klok, F.A.; Boon, G.J.A.M.; Barco, S.; Endres, M.; Geelhoed, J.J.M.; Knauss, S.; Rezek, S.A.; Spruit, M.A.; Vehreschild, J.; Siegerink, B. The Post-COVID-19 Functional Status scale: A tool to measure functional status over time after COVID-19. Eur. Respir. J. 2020, 56, 2001494. [Google Scholar] [CrossRef] [PubMed]
- Mikkelsen, M.E.; Still, M.; Anderson, B.J.; Bienvenu, O.J.; Brodsky, M.B.; Brummel, N.; Butcher, B.; Clay, A.S.; Felt, H.; Ferrante, L.E.; et al. Society of Critical Care Medicine’s International Consensus Conference on Prediction and Identification of Long-Term Impairments After Critical Illness. Crit. Care Med. 2020, 48, 1670–1679. [Google Scholar] [CrossRef] [PubMed]
- Geense, W.W.; van den Boogaard, M.; Peters, M.A.A.; Simons, K.S.; Ewalds, E.; Vermeulen, H.; van der Hoeven, J.G.; Zegers, M. Physical, Mental, and Cognitive Health Status of ICU-survivors Before ICU Admission: A Cohort Study. Crit. Care Med. 2020, 48, 1271–1279. [Google Scholar] [CrossRef] [PubMed]
- Lee, M.; Kang, J.; Jeong, Y.J. Risk factors for post-intensive care syndrome: A systematic review and meta-analysis. Aust. Crit. Care 2020, 33, 287–294. [Google Scholar] [CrossRef]

| (A) | |
| Variable | ICU Survivors (n = 60) |
| Age, years, median (IQR) | 62.5 (55.3–68.0) |
| Sex, n (%) | |
| Male | 41 (68) |
| Female | 19 (32) |
| Marital status, n (%) | |
| Married/living together | 51 (85) |
| Single | 9 (15) |
| Educational level 1,2, n (%) | |
| Low | 19 (32) |
| Middle | 23 (38) |
| High | 17 (28) |
| Employment status 3, n (%) | |
| Employed | 30 (50) |
| Unemployed | 20 (33) |
| Work rate, pre-admission (100% = full-time), mean (SD) | 79.0 (28.7) |
| Weight, kg, median (IQR) | 92.0 (83.0–104.3) |
| BMI, kg/m2, at ICU admission, median (IQR) | 29.4 (26.6–32.4) |
| BMI, at ICU admission, n (%) | |
| Normal (18.5–25) | 4 (7) |
| Overweight (25–30) | 30 (50) |
| Obese (30–35) | 19 (32) |
| Extremely obese (>35) | 7 (12) |
| APACHE IV2, total score, median (IQR) | 55.0 (45.0–65.3) |
| Comorbidities, n (%) | |
| Hypertension | 20 (33) |
| Diabetes mellitus | 15 (25) |
| Cardiovascular disease | 12 (20) |
| Cerebrovascular disease | 1 (2) |
| COPD/asthma | 6 (10) |
| Chronic kidney disease | 3 (5) |
| Malignancy | 3 (5) |
| ACCI, n (%) | |
| 0–1 | 5 (8) |
| 2–3 | 28 (47) |
| ≥4 | 27 (45) |
| ECMO, n (%) | |
| Yes | 3 (5) |
| No | 57 (95) |
| Length of ECMO, days, median (IQR) | 21.7 (2.5) |
| Mechanical ventilation, days, median (IQR) | 16.3 (10.6–26.5) |
| Delirium during ICU-stay, n (%) | |
| Yes | 29 (48) |
| No | 31 (52) |
| Length of ICU stay, days, median (IQR) | 19.4 (12.3–31.7) |
| Length of hospital stay, days, median (IQR) | 30.6 (21.9–44.7) |
| Discharge location2, n (%) | |
| Home | 25 (42) |
| Other hospital | 10 (17) |
| Nursing home | 4 (7) |
| Rehabilitation center | 20 (33) |
| (B) | |
| Variable | Family (n = 78) |
| Relation to patient, n (%) | |
| Partner | 49 (63) |
| Son/daughter | 22 (28) |
| Parent | 5 (6) |
| Sibling | 2 (3) |
| Age2, years, median (IQR) | 56.0 (41.0–63.0) |
| Sex 2, n (%) | |
| Male | 20 (26) |
| Female | 57 (73) |
| Marital status, n (%) | |
| Married/living together | 66 (85) |
| Single | 12 (15) |
| Educational level 1, n (%) | |
| Low | 16 (21) |
| Middle | 38 (49) |
| High | 24 (31) |
| Employment status, n (%) | |
| Employed | 40 (51) |
| Unemployed | 38 (49) |
| Employment rate, pre-admission (100% = full-time), mean (SD) | 79.9 (26.5) |
| (A) | |||
| Domain | Variable | 3 Months (n = 60) | 6 Months (n = 50) |
| Physical functioning | Physical functioning 1 (range 0–100) | 33.3 (16.7–66.7) | 50.0 (16.7–83.3) |
| Experienced health 1 (range 0–100) | 35.0 (25.0–50.0) | 50.0 (35.0–71.3) | |
| Pain 2 (range 0–100) | 50.0 (25.0–75.0) | 50.0 (0.0–75.0) | |
| Frailty, n (%) | |||
| Not frail (1–3) | 40(67) | 35 (70) | |
| Mildly frail (4–5) | 17 (28) | 14 (28) | |
| Frail (6–8) | 3 (5) | 0 | |
| Lung function 3 | - | ||
| FEV1 < 80%, % of predicted | 7/39 (18) | ||
| FVC L < 80%, % of predicted | 7/35 (20) | ||
| FEV1/FCV < 70% | 1/36 (3) | ||
| TLC < 80%, % of predicted | 0 | ||
| DLCO < 80%, % of predicted | 22/32 (69) | ||
| Weight, kg | 85.5 (80.3–93.5) | 86.8 (80.5–95.0) | |
| Self-reported symptoms 4, n (%) | - | ||
| Any one of the following symptoms | 44 (90) | ||
| Fatigue | 16 (33) | ||
| Weakened condition | 12 (25) | ||
| Cognitive problems | 9 (18) | ||
| Polyneuropathy | 7 (14) | ||
| Impaired hand function | 7 (14) | ||
| Reduced lung function | 5 (10) | ||
| Dyspnea | 5 (10) | ||
| Difficulty walking | 5 (10) | ||
| Muscle weakness/stiffness | 4 (8) | ||
| Difficulty sleeping | 3 (6) | ||
| Shoulder pain | 3 (6) | ||
| Restriction of extremities | 3 (6) | ||
| Social functioning | Role activities 1 (range 0–100) | 0.0 (0.0–0.0) | 0.0 (0.0–0.0) |
| Social functioning 1 (range 0–100) | 60.0 (40.0–80.0) | 80.0 (60.0–100) | |
| Family functioning 1 (range 1–4) | 4.0 (3.3–4.0) | 3.8 (3.2–4.0) | |
| Return to work, n (%) | - | ||
| No change | 3 (10) | ||
| Reduced work rate | 4 (13) | ||
| Occupation change | 3 (10) | ||
| Re-integration | 4 (13) | ||
| Too ill to work | 13 (43) | ||
| Other | 3 (10) | ||
| Work rate (100% = full-time), mean (SD) | - | 22.9 (32.2) | |
| Psychological functioning | Anxiety (range 0–21) | 3.5 (1.0–7.8) | 4.5 (0.3–7.0) |
| Depression (range 0–21) | 4.0 (1.0–6.0) | 2.0 (1.0–6.0) | |
| Fear of reinfection (range 1–10) | - | 5.0 (2.0–7.5) | |
| Miscellaneous | Health care consumption 5, n (%) | ||
| Yes | 60 (100) | 46 (92) | |
| No | 0 | 4 (8) | |
| Readmission | 5 (8) | 5 (10) | |
| General practitioner | 43 (72) | 28 (56) | |
| Home care | 12 (20) | 3 (6) | |
| Physiotherapist | 51 (85) | 43 (86) | |
| Pulmonologist | 42 (70) | 32 (64) | |
| Psychologist | 16 (27) | 10 (20) | |
| Rehabilitation | 25 (42) | 0 | |
| Dietician | 8 (13) | 1 (2) | |
| (B) | |||
| Domain | Variable | 3 Months (n = 78) | 6 Months (n = 67) |
| Physical functioning | Physical functioning 1 (range 0–100) | 100 (83.3–100) | - |
| Experienced health 1 (range 0–100) | 70.0 (55.0–90.0) | - | |
| Pain 2 (range 0–100) | 25.0 (0.0–50.0) | - | |
| Social functioning | Role activities1 (range 0–100) | 100 (50.0–100) | - |
| Social functioning 1 (range 0–100) | 100 (70.0–100) | - | |
| Family functioning 1 (range 1–4) | 3.8 (3.1–4.0) | 3.8 (3.2–4.0) | |
| Return to work 6, n (%) | |||
| No change | 26 (65) | 23 (64) | |
| Reduced work rate | 1 (3) | 5 (14) | |
| Occupation change | 2 (5) | 1 (3) | |
| Re-integration | 5 (13) | 4 (11) | |
| Not returned to work | 4 (10) | 0 | |
| Job loss | 1 (5) | 0 | |
| Unknown | 1 (3) | 3 (8) | |
| Work rate (100% = full-time), mean (sd) | 61.6 (38.7) | 72.5 (27.8) | |
| Psychological functioning | Anxiety (range 0–21) | 3.0 (2.0–7.0) | 4.0 (1.0–8.0) |
| Depression (range 0–21) | 2.0 (1.0–6.0) | 2.0 (1.0–6.0) | |
| Fear of reinfection (range 1–10) | - | 6.0 (4.0–8.0) | |
| Influence no-contact on well-being, n (%) | - | ||
| Yes | 42 (63) | ||
| No | 21 (31) | ||
| Miscellaneous | Health care consumption 7, n (%) | ||
| Yes | 40 (51) | 28 (42) | |
| No | 38 (49) | 39 (58) | |
| General practitioner | 31 (40) | 19 (28) | |
| Psychologist | 9 (12) | 8 (12) | |
| Social work | 19 (24) | 7 (10) | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
van Veenendaal, N.; van der Meulen, I.C.; Onrust, M.; Paans, W.; Dieperink, W.; van der Voort, P.H.J. Six-Month Outcomes in COVID-19 ICU Patients and Their Family Members: A Prospective Cohort Study. Healthcare 2021, 9, 865. https://doi.org/10.3390/healthcare9070865
van Veenendaal N, van der Meulen IC, Onrust M, Paans W, Dieperink W, van der Voort PHJ. Six-Month Outcomes in COVID-19 ICU Patients and Their Family Members: A Prospective Cohort Study. Healthcare. 2021; 9(7):865. https://doi.org/10.3390/healthcare9070865
Chicago/Turabian Stylevan Veenendaal, Nadine, Ingeborg C. van der Meulen, Marisa Onrust, Wolter Paans, Willem Dieperink, and Peter H. J. van der Voort. 2021. "Six-Month Outcomes in COVID-19 ICU Patients and Their Family Members: A Prospective Cohort Study" Healthcare 9, no. 7: 865. https://doi.org/10.3390/healthcare9070865
APA Stylevan Veenendaal, N., van der Meulen, I. C., Onrust, M., Paans, W., Dieperink, W., & van der Voort, P. H. J. (2021). Six-Month Outcomes in COVID-19 ICU Patients and Their Family Members: A Prospective Cohort Study. Healthcare, 9(7), 865. https://doi.org/10.3390/healthcare9070865






