Impact of Physicians’ Competence and Warmth on Chronic Patients’ Intention to Use Online Health Communities
Abstract
:1. Introduction
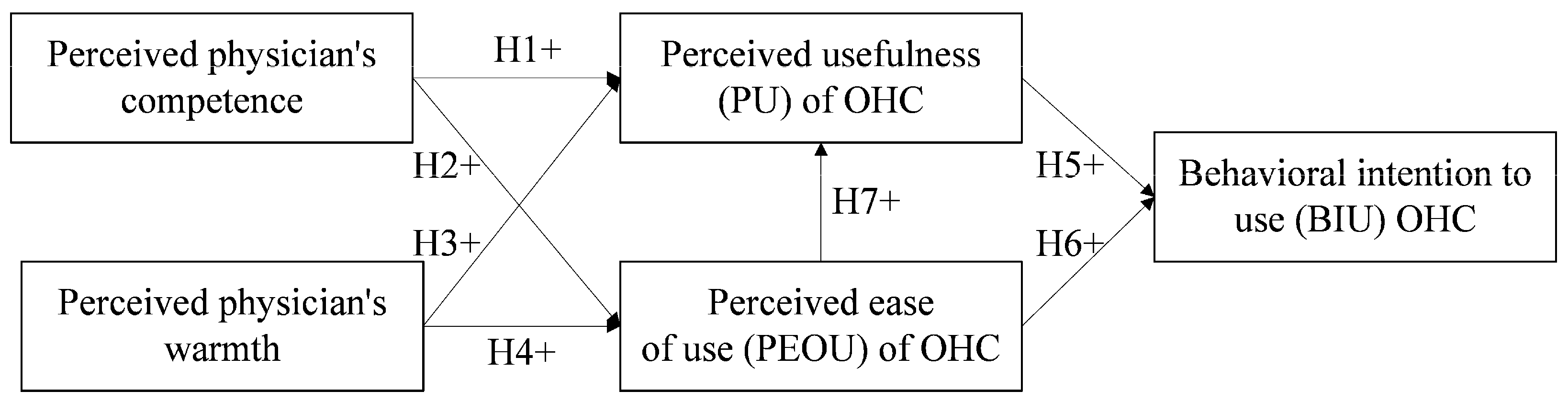
2. Research Model and Hypotheses
2.1. TAM
2.2. Research Model
2.3. Competence
2.4. Warmth
2.5. PU, PEOU, and BIU
3. Materials and Methods
3.1. Instrument Development
3.2. Analysis Tool Selection
3.3. Data Collection and Respondent Profile
4. Results
4.1. Descriptive Statistics
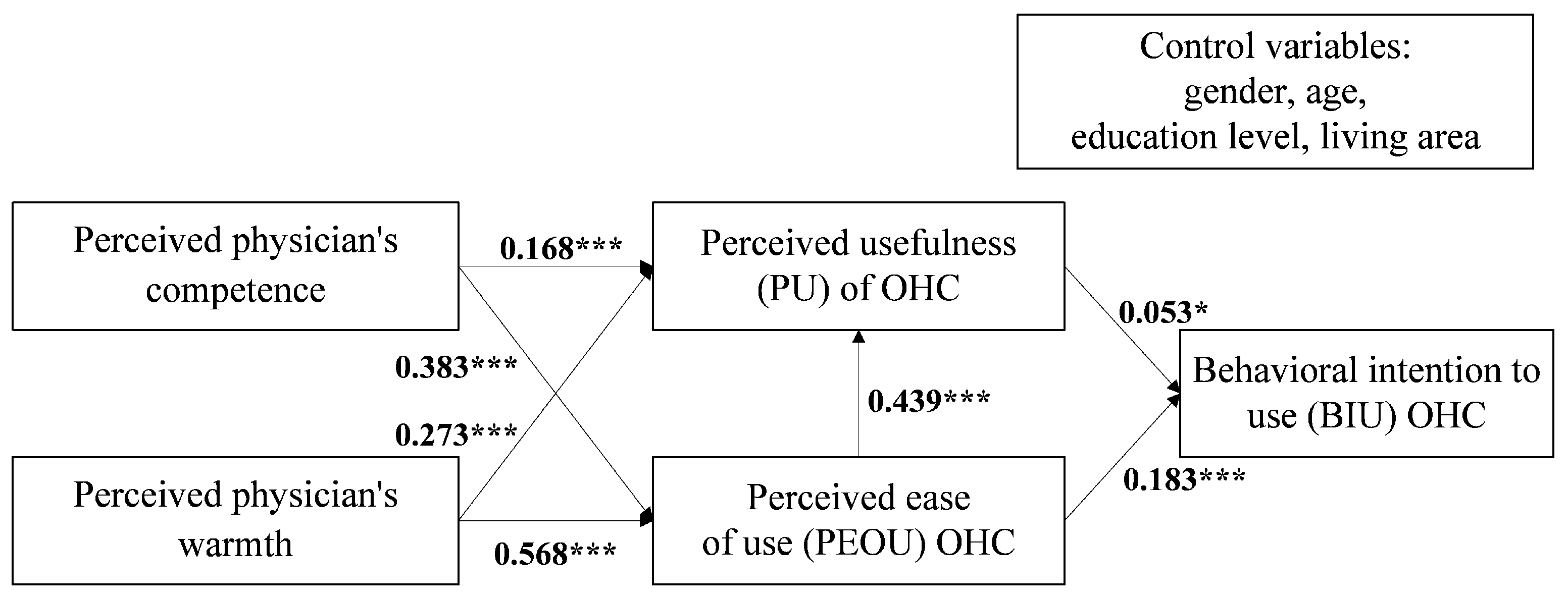
4.2. Hypothesis Testing
5. Discussion
5.1. Principal Findings
5.2. Implications for Practice
5.3. Limitations and Prospects
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
Abbreviations
Appendix A
| Construct | Scale/Scoring | Items |
|---|---|---|
| Behavioral intention to use |
| BIU1: Assuming that I am given the chance to access telemedicine, I intend to use physician-centered OHC services. |
| BIU2: Whenever I need remote medical care from professionals, I would gladly use physician-centered OHCs. | ||
| BIU3: I intend to inform my relatives and friends about physician-centered OHCs. | ||
| Perceived usefulness |
| PU1: Using physician-centered OHCs would improve the quality of my healthcare. |
| PU2: Using physician-centered OHCs would improve my access to healthcare services. | ||
| PU3: Using physician-centered OHCs would be useful in my daily routine. | ||
| Perceived ease of use |
| PEOU1: I find learning to use physician-centered OHCs to be easy. |
| PEOU2: I find it easy to interact with doctors using physician-centered OHCs. | ||
| PEOU3: Interacting with physician-centered OHCs is clear and understandable for me. | ||
| Competence |
| According to your online treatment experience with physician(s) in physician-centered OHCs: |
| C1: How competent are physician(s)? | ||
| C2: How confident are physician(s)? | ||
| C3: How independent are physician(s)? | ||
| C4: How competitive are physician(s)? | ||
| C5: How intelligent are physician(s)? | ||
| Warmth |
| According to your online treatment experience with physician(s) in physician-centered OHCs: |
| C1: How tolerant are physician(s)? | ||
| C2: How warm are physician(s)? | ||
| C3: How good natured are physician(s)? | ||
| C4: How sincere are physician(s)? |
References
- Lu, X.; Zhang, R. Impact of physician-patient communication in online health communities on patient compliance: Cross-sectional questionnaire study. J. Med. Internet Res. 2019, 21, e12891. [Google Scholar] [CrossRef]
- Tahri Sqalli, M.; Al-Thani, D. On how chronic conditions affect the patient-AI interaction: A literature review. Healthcare 2020, 8, 313. [Google Scholar] [CrossRef] [PubMed]
- Devaraj, S.; Kohli, R. Information technology payoff in the health-care industry: A longitudinal study. J. Manag. Inf. Syst. 2000, 16, 41–66. [Google Scholar] [CrossRef]
- Lu, Y.; Wu, Y.; Liu, J.; Li, J.; Zhang, P. Understanding health care social media use from different stakeholder perspectives: A content analysis of an online health community. J. Med. Internet Res. 2017, 19, e109. [Google Scholar] [CrossRef] [PubMed]
- Yang, H.; Guo, X.; Wu, T. Exploring the influence of the online physician service delivery process on patient satisfaction. Dec. Support Syst. 2015, 78, 113–121. [Google Scholar] [CrossRef]
- Dickerson, S.S.; Boehmke, M.; Ogle, C.; Brown, J.K. Seeking and managing hope: Patients’ experiences using the Internet for cancer care. Oncol. Nurs. Forum 2006, 3, e8–e17. [Google Scholar] [CrossRef] [PubMed]
- Bansil, P.; Keenan, N.L.; Zlot, A.I.; Gilliland, J.C. Peer reviewed: Health-related information on the Web: Results from the Health Styles Survey, 2002–2003. Prev. Chronic Dis. 2006, 3, A36. [Google Scholar]
- Liu, Q.B.; Liu, X.; Guo, X. The effects of participating in a physician-driven online health community in managing chronic disease: Evidence from two natural experiments. MIS Q. 2020, 44, 391–419. [Google Scholar] [CrossRef]
- Wu, D.; Gu, H.; Gu, S.; You, H. Individual motivation and social influence: A study of telemedicine adoption in China based on social cognitive theory. Health Policy Technol. 2021, 10, 100525. [Google Scholar] [CrossRef]
- Deng, Z.; Hong, Z.; Zhang, W.; Evans, R.; Chen, Y. The effect of online effort and reputation of physicians on patients’ choice: 3-wave data analysis of China’s good physician website. J. Med. Internet Res. 2019, 21, e10170. [Google Scholar] [CrossRef]
- Lu, N.; Wu, H. Exploring the impact of word-of-mouth about physicians’ service quality on patient choice based on online health communities. BMC Med. Inf. Decis. Mak. 2016, 16, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Cuddy, A.J.; Fiske, S.T.; Glick, P. Warmth and competence as universal dimensions of social perception: The stereotype content model and the BIAS map. Adv. Exp. Soc. Psychol. 2008, 40, 61–149. [Google Scholar] [CrossRef]
- Fiske, S.T.; Cuddy, A.J.; Glick, P. Universal dimensions of social cognition: Warmth and competence. Trends Cogn. Sci. 2007, 11, 77–83. [Google Scholar] [CrossRef] [PubMed]
- Fiske, S.T.; Cuddy, A.J.; Glick, P.; Xu, J. A model of (often mixed) stereotype content: Competence and warmth respectively follow from perceived status and competition. J. Pers. Soc. Psychol. 2002, 82, 878. [Google Scholar] [CrossRef]
- Aaker, J.L.; Garbinsky, E.N.; Vohs, K.D. Cultivating admiration in brands: Warmth, competence, and landing in the “golden quadrant”. J Consum. Psychol. 2012, 22, 191–194. [Google Scholar] [CrossRef]
- Keith, M.J.; Thompson, S.C.; Hale, J.; Lowry, P.B.; Greer, C. Information disclosure on mobile devices: Re-examining privacy calculus with actual user behavior. Int. J. Hum. Comput. Stud. 2013, 71, 1163–1173. [Google Scholar] [CrossRef]
- Ye, T.; Xue, J.; He, M.; Gu, J.; Lin, H.; Xu, B.; Cheng, Y. Psychosocial factors affecting artificial intelligence adoption in health care in China: Cross-sectional study. J. Med. Internet Res. 2019, 21, e14316. [Google Scholar] [CrossRef] [Green Version]
- Davis, F.D. Perceived usefulness, perceived ease of use, and user acceptance of information technology. MIS Q. 1989, 13, 319–340. [Google Scholar] [CrossRef] [Green Version]
- Ducey, A.J.; Coovert, M.D. Predicting tablet computer use: An extended Technology Acceptance Model for physicians. Health Policy Technol. 2016, 5, 268–284. [Google Scholar] [CrossRef]
- Wu, B.; Chen, X. Continuance intention to use MOOCs: Integrating the technology acceptance model (TAM) and task technology fit (TTF) model. Comput. Hum. Behav. 2017, 67, 221–232. [Google Scholar] [CrossRef]
- Dixit, R.V.; Prakash, G. Intentions to use social networking sites (SNS) using technology acceptance model (TAM) an empirical study. Paradigm 2018, 22, 65–79. [Google Scholar] [CrossRef] [Green Version]
- Samar, S.; Ghani, M.; Alnaser, F. Predicting customer’s intentions to use internet banking: The role of technology acceptance model (TAM) in e-banking. Manag. Sci. Lett. 2017, 7, 513–524. [Google Scholar] [CrossRef]
- Tung, F.C.; Chang, S.C.; Chou, C.M. An extension of trust and TAM model with IDT in the adoption of the electronic logistics information system in HIS in the medical industry. Int. J. Med. Inform. 2008, 77, 324–335. [Google Scholar] [CrossRef] [PubMed]
- McClelland, D.C. Testing for competence rather than for “intelligence”. Am. Psychol. 1973, 28, 1. [Google Scholar] [CrossRef] [Green Version]
- Burgess, J.F.; Menachemi, N.; Maciejewski, M.L. Update on the health services research physicianal core competencies. Health Serv. Res. 2018, 53, 3985–4003. [Google Scholar] [CrossRef] [Green Version]
- Hudson Smith, M.; Smith, D. Directing improvements in primary care patient experience through analysis of service quality. Health Serv. Res. 2018, 53, 4647–4666. [Google Scholar] [CrossRef]
- Okazaki, S.; Castañeda, J.A.; Sanz, S.; Henseler, J. Factors affecting mobile diabetes monitoring adoption among physicians: Questionnaire study and path model. J. Med. Internet Res. 2014, 14, e183. [Google Scholar] [CrossRef]
- Peng, Y.; Yin, P.; Deng, Z.; Wang, R. Patient–Physician Interaction and Trust in Online Health Community: The role of perceived usefulness of health information and services. Int. J. Environ. Res. Public Health 2020, 17, 139. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Norman, C.D.; Skinner, H.A. eHealth Literacy: Essential Skills for Consumer Health in a Networked World. J. Med. Internet Res. 2006, 8, e9. [Google Scholar] [CrossRef]
- Mackert, M.; Whitten, P. The relationship between health-care organizations and technology vendors: An overlooked factor in telemedicine success. J. Telemed. Telecare 2007, 13, 50–53. [Google Scholar] [CrossRef]
- Lages, M.; Marques, C.S.; Ferreira, J.J.; Ferreira, F.A. Intrapreneurship and firm entrepreneurial orientation: Insights from the health care service industry. Int. Entrep. Manag. J. 2017, 13, 837–854. [Google Scholar] [CrossRef]
- Parasuraman, A.; Zeithaml, V.A.; Berry, L.L. A conceptual model of service quality and its implications for future research. J. Mark. 1985, 49, 41–50. [Google Scholar] [CrossRef]
- Jenkin, T.A.; Chan, Y.E.; Sabherwal, R. Mutual understanding in information systems development: Changes within and across projects. MIS Q. 2019, 43, 649–672. [Google Scholar] [CrossRef] [Green Version]
- Bolton, R.N.; Drew, J.H. A multistage model of customers’ assessments of service quality and value. J. Consum. Res. 1991, 17, 375–384. [Google Scholar] [CrossRef]
- Karahanna, E.; Straub, D.W. The psychological origins of perceived usefulness and ease-of-use. Inf. Manag. 1999, 35, 237–250. [Google Scholar] [CrossRef]
- Holden, R.J.; Karsh, B.T. The technology acceptance model: Its past and its future in health care. J. Biomed. Inform. 2010, 43, 159–172. [Google Scholar] [CrossRef] [Green Version]
- Antheunis, M.L.; Tates, K.; Nieboer, T.E. Patients’ and health professionals’ use of social media in health care: Motives, barriers and expectations. Patient Educ. Couns. 2013, 92, 426–431. [Google Scholar] [CrossRef] [PubMed]
- Delone, W.H.; McLean, E.R. The DeLone and McLean model of information systems success: A ten-year update. J. Manag. Inf. Syst. 2003, 19, 9–30. [Google Scholar] [CrossRef]
- Awad, N.F.; Krishnan, M.S. The personalization privacy paradox: An empirical evaluation of information transparency and the willingness to be profiled online for personalization. MIS Q. 2006, 30, 13–28. [Google Scholar] [CrossRef] [Green Version]
- Wu, J.H.; Chen, Y.C.; Lin, L.M. Empirical evaluation of the revised end user computing acceptance model. Comput. Hum. Behav. 2007, 23, 162–174. [Google Scholar] [CrossRef]
- Silvestre, A.L.; Sue, V.M.; Allen, J.Y. If you build it, will they come? The Kaiser Permanente model of online health care. Health Aff. 2009, 28, 334–344. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Davis, F.D.; Bagozzi, R.P.; Warshaw, P.R. User acceptance of computer technology: A comparison of two theoretical models. Manag. Sci. 1989, 35, 982–1003. [Google Scholar] [CrossRef] [Green Version]
- Chang, L. A psychometric evaluation of 4-point and 6-point Likert-type scale in relation to reliability and validity. Appl. Psychol. Meas. 1994, 18, 205–215. [Google Scholar] [CrossRef]
- Egea, J.M.O.; González, M.V.R. Explaining physicians’ acceptance of EHCR systems: An extension of TAM with trust and risk factors. Comput. Hum. Behav. 2011, 27, 319–332. [Google Scholar] [CrossRef]
- Wu, B.; Zhang, C. Empirical study on continuance intentions towards E-Learning 2.0 systems. Behav. Inform. Technol. 2014, 33, 1027–1038. [Google Scholar] [CrossRef]
- Kim, T.; Suh, Y.K.; Lee, G.; Choi, B.G. Modelling roles of task-technology fit and self-efficacy in hotel employees’ usage behaviors of hotel information systems. Int. J. Tour. Res. 2010, 12, 709–725. [Google Scholar] [CrossRef]
- Chang, H.H. Task-technology fit and user acceptance of online auction. Int. J. Hum. Comput. Stud. 2010, 68, 69–89. [Google Scholar] [CrossRef]
- Yan, Z.; Wang, T.; Chen, Y.; Zhang, H. Knowledge sharing in online health communities: A social exchange theory perspective. Inf. Manag. 2016, 53, 643–653. [Google Scholar] [CrossRef]
- Fornell, C.; Larcker, D.F. Evaluating structural equation models with unobservable variables and measurement error. J. Mark. Res. 1981, 18, 39–50. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences; Academic Press: New York, NY, USA, 2013. [Google Scholar]
- Li, D.; Hu, Y.; Pfaff, H.; Wang, L.; Deng, L.; Lu, C.; Xia, S.; Cheng, S.; Zhu, X.; Wu, X. Determinants of patients’ intention to use the online inquiry services provided by internet hospitals: Empirical evidence from China. J. Med. Internet Res. 2020, 22, e22716. [Google Scholar] [CrossRef]
- Delanoë, A.; Lépine, J.; Portocarrero, M.E.L.; Robitaille, H.; Turcotte, S.; Lévesque, I.; Wilson, B.J.; Giguere, A.M.C.; Légaré, F. Health literacy in pregnant women facing prenatal screening may explain their intention to use a patient decision aid: A short report. BMC Res. Notes 2016, 9, 1–7. [Google Scholar] [CrossRef] [Green Version]
- Mackey, L.M.; Doody, C.; Werner, E.L.; Fullen, B. Self-management skills in chronic disease management: What role does health literacy have? Med. Decis. Mak. 2016, 36, 741–759. [Google Scholar] [CrossRef] [PubMed]
- Lehning, A.J.; Scharlach, A.E.; Dal Santo, T.S. A web-based approach for helping communities become more “Aging Friendly”. J. Appl. Gerontol. 2010, 29, 415–433. [Google Scholar] [CrossRef]
- Fan, M.Y. Frequency of use, perceived usefulness, and actual usefulness of second language vocabulary strategies: A study of Hong Kong learners. Mod. Lang. J. 2003, 87, 222–241. [Google Scholar] [CrossRef]
- Venkatesh, V.; Thong, J.Y.L.; Xu, X. Consumer acceptance and use of information technology: Extending the unified theory of acceptance and use of technology. MIS Q. 2012, 36, 157–178. [Google Scholar] [CrossRef] [Green Version]
| Demographic Characteristics | Participants, n (%) |
|---|---|
| Age (years) | |
| <20 | 26 (3.7) |
| 20–29 | 342 (48.2) |
| 30–39 | 223 (31.4) |
| 40–49 | 57 (8.0) |
| 50–59 | 47 (6.6) |
| 60 and above | 15 (2.1) |
| Gender | |
| Male | 246 (34.6) |
| Female | 464 (65.4) |
| Resident status | |
| Urban | 509 (71.7) |
| Rural | 201 (28.3) |
| Education | |
| Junior middle school | 15 (2.1) |
| High school | 33 (4.6) |
| Junior college | 78 (11.0 |
| Bachelor’s degree | 368 (51.8) |
| Master’s degree | 198 (27.9) |
| Physician’s degree | 18 (2.5) |
| Construct | Cronbach’s Alpha | CR | AVE | Square Root of AVE |
|---|---|---|---|---|
| Competence | 0.905 | 0.929 | 0.775 | 0.880 |
| Warmth | 0.966 | 0.973 | 0.880 | 0.938 |
| PU | 0.722 | 0.840 | 0.728 | 0.853 |
| PEOU | 0.912 | 0.945 | 0.851 | 0.922 |
| BIU | 0.932 | 0.956 | 0.880 | 0.938 |
| Construct | Competence | Warmth | PU | PEOU | BIU |
|---|---|---|---|---|---|
| Competence | 0.880 | 0.853 | 0.781 | 0.867 | 0.877 |
| Warmth | 0.938 | 0.809 | 0.894 | 0.911 | |
| PU | 0.853 | 0.829 | 0.825 | ||
| PEOU | 0.922 | 0.916 | |||
| BIU | 0.938 |
| Variables | R Square | Control Variables Effects | |||
|---|---|---|---|---|---|
| With Control Variables | Without Control Variables | ΔR2 a | f2b | Effect | |
| BIU | 0.918 | 0.917 | 0.001 | 0.001 | Insignificant |
| PEOU | 0.840 | 0.840 | <0.001 | <0.001 | Insignificant |
| PU | 0.716 | 0.716 | <0.001 | <0.001 | Insignificant |
| Hypothesis | Path Coefficient | t Test | p Value |
|---|---|---|---|
| H1: Competence → PU | 0.168 | 4.218 | <0.001 |
| H2: Competence → PEOU | 0.383 | 9.590 | <0.001 |
| H3: Warmth → PU | 0.273 | 5.630 | <0.001 |
| H4: Warmth → PEOU | 0.568 | 14.482 | <0.001 |
| H5: PU → BIU | 0.053 | 1.999 | 0.046 |
| H6: PEOU → BIU | 0.183 | 5.003 | <0.001 |
| H7: PEOU → PU | 0.439 | 8.277 | <0.001 |
| Effect | Path Coefficients | p Value | CI |
|---|---|---|---|
| Direct effect | |||
| Competence → PU | 0.168 | <0.001 | 0.092–0.251 |
| Competence → PEOU | 0.383 | <0.001 | 0.305–0.461 |
| Warmth → PU | 0.273 | <0.001 | 0.177–0.367 |
| Warmth → PEOU | 0.568 | <0.001 | 0.490–0.643 |
| PU → BIU | 0.053 | 0.046 | 0.003–0.106 |
| PEOU → BIU | 0.183 | <0.001 | 0.110–0.254 |
| PEOU → PU | 0.439 | <0.001 | 0.332–0.539 |
| Indirect effect | |||
| Competence → BIU | 0.088 | <0.001 | 0.053–0.128 |
| Warmth → BIU | 0.131 | <0.001 | 0.082–0.183 |
| Total effect | |||
| Competence → BIU | 0.088 | <0.001 | 0.053–0.128 |
| Warmth → BIU | 0.131 | <0.001 | 0.082–0.183 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, X.; Zhang, R. Impact of Physicians’ Competence and Warmth on Chronic Patients’ Intention to Use Online Health Communities. Healthcare 2021, 9, 957. https://doi.org/10.3390/healthcare9080957
Zhang X, Zhang R. Impact of Physicians’ Competence and Warmth on Chronic Patients’ Intention to Use Online Health Communities. Healthcare. 2021; 9(8):957. https://doi.org/10.3390/healthcare9080957
Chicago/Turabian StyleZhang, Xijing, and Runtong Zhang. 2021. "Impact of Physicians’ Competence and Warmth on Chronic Patients’ Intention to Use Online Health Communities" Healthcare 9, no. 8: 957. https://doi.org/10.3390/healthcare9080957
APA StyleZhang, X., & Zhang, R. (2021). Impact of Physicians’ Competence and Warmth on Chronic Patients’ Intention to Use Online Health Communities. Healthcare, 9(8), 957. https://doi.org/10.3390/healthcare9080957






