Sex Differences in Oxycodone/Naloxone vs. Tapentadol in Chronic Non-Cancer Pain: An Observational Real-World Study
Abstract
1. Introduction
2. Materials and Methods
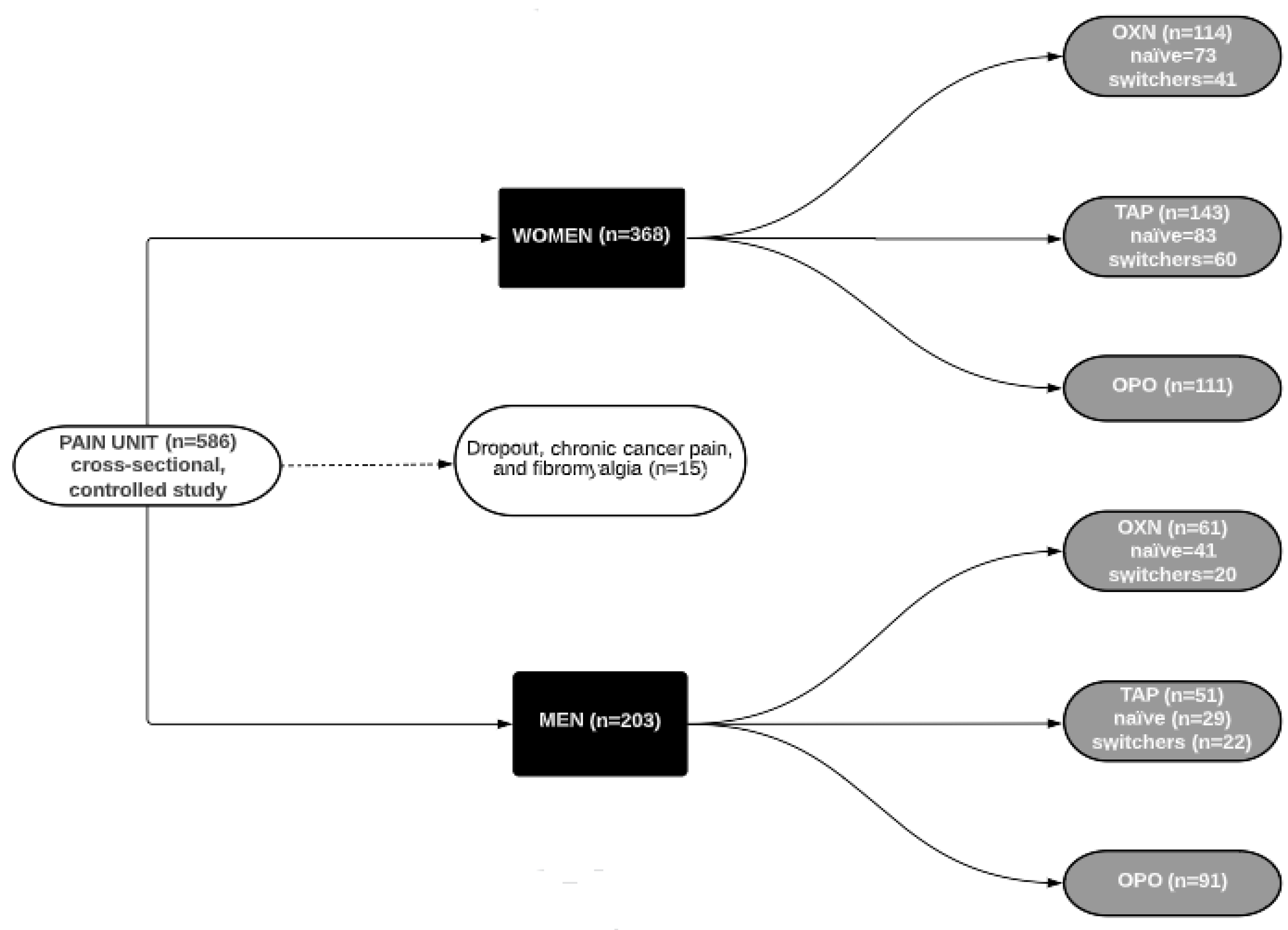
2.1. Study Design
2.2. Participants
2.3. Procedure
2.4. Data Collection
2.5. Drug Prescription and Adverse Events
2.6. Statistical Analysis
3. Results
3.1. Demographic and Clinical Outcomes
Sex-Differences between Opioid Groups
3.2. Pharmacology Variables
Sex-Differences between Opioid Groups
3.3. Safety Profile
Sex-Differences between Opioid Groups
3.4. Multiple Linear and Logistic Regressions
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Pisanu, C.; Franconi, F.; Gessa, G.L.; Mameli, S.; Pinasu, G.M.; Campesi, I.; Leggio, L.; Agabio, R. Sex Differences in the Response to Opioids for Pain Relief: A Systematic Review and Meta-Analysis. Pharmacol. Res. 2019, 148, 104447. [Google Scholar] [CrossRef] [PubMed]
- Kiely, K.M.; Brady, B.; Byles, J. Gender, Mental Health and Ageing. Maturitas 2019, 129, 76–84. [Google Scholar] [CrossRef] [PubMed]
- Margarit, C.; Roca, R.; Inda, M.D.M.; Muriel, J.; Ballester, P.; Flor, A.; Morales, D.; Peiró, A.M. Gender Bias and Genotype Influence on Opioid Safety Profile in Chronic Low Back Pain. Clin. J. Pain 2020, 36, 420–429. [Google Scholar] [CrossRef]
- Beery, T.A. Gender Bias in the Diagnosis and Treatment of Coronary Artery Disease. Heart Lung 1995, 24, 427–435. [Google Scholar] [CrossRef]
- Lopes, G.S.; Bielinski, S.J.; Moyer, A.M.; Black Lii, J.L.; Jacobson, D.J.; Jiang, R.; Larson, N.B.; St Sauver, J.L. Sex Differences in Associations Between CYP2D6 Phenotypes and Response to Opioid Analgesics. Pharmgenomics Pers. Med. 2020, 13, 71–79. [Google Scholar] [CrossRef]
- Samulowitz, A.; Gremyr, I.; Eriksson, E.; Hensing, G. “Brave Men” and “Emotional Women”: A Theory-Guided Literature Review on Gender Bias in Health Care and Gendered Norms towards Patients with Chronic Pain. Pain Res. Manag. 2018, 2018, 6358624. [Google Scholar] [CrossRef] [PubMed]
- Linares, O.A.; Daly, D.; Linares, A.D.; Stefanovski, D.; Boston, R.C. Personalized Oxycodone Dosing: Using Pharmacogenetic Testing and Clinical Pharmacokinetics to Reduce Toxicity Risk and Increase Effectiveness. Pain Med. 2014, 15, 791–806. [Google Scholar] [CrossRef]
- Graziani, M.; Nisticò, R. Gender Difference in Prescription Opioid Abuse: A Focus on Oxycodone and Hydrocodone. Pharmacol. Res. 2016, 108, 31–38. [Google Scholar] [CrossRef]
- Mogil, J.S.; Bailey, A.L. Sex and Gender Differences in Pain and Analgesia. Prog. Brain Res. 2010, 186, 140–157. [Google Scholar] [CrossRef]
- Wiesenfeld-Hallin, Z. Sex Differences in Pain Perception. Gend. Med. 2005, 2, 137–145. [Google Scholar] [CrossRef]
- Pieretti, S.; Di Giannuario, A.; Di Giovannandrea, R.; Marzoli, F.; Piccaro, G.; Minosi, P.; Aloisi, A.M. Gender Differences in Pain and Its Relief. Ann. Ist. Super. Sanita 2016, 52, 184–189. [Google Scholar] [CrossRef] [PubMed]
- Dao, T.T.T.; LeResche, L. Gender Differences in Pain. J. Orofac. Pain 2000, 14, 169–184. [Google Scholar] [CrossRef] [PubMed]
- Canadian Institutes of Health Research. Science Is Better with Sex and Gender. Strategic Plan 2018–2023; Canadian Institutes of Health Research: Ottawa, ON, USA, 2018. [Google Scholar]
- Smith, K.; Hopp, M.; Mundin, G.; Bond, S.; Bailey, P.; Woodward, J.; Palaniappan, K.; Church, A.; Limb, M.; Connor, A. Naloxone as Part of a Prolonged Release Oxycodone/Naloxone Combination Reduces Oxycodone-Induced Slowing of Gastrointestinal Transit in Healthy Volunteers. Expert Opin. Investig. Drugs 2011, 20, 427–439. [Google Scholar] [CrossRef] [PubMed]
- Langford, R.M.; Knaggs, R.; Farquhar-Smith, P.; Dickenson, A.H. Is Tapentadol Different from Classical Opioids? A Review of the Evidence. Br. J. Pain 2016, 10, 217–221. [Google Scholar] [CrossRef] [PubMed]
- Abeyaratne, C.; Lalic, S.; Bell, J.S.; Ilomäki, J. Spontaneously Reported Adverse Drug Events Related to Tapentadol and Oxycodone/Naloxone in Australia. Ther. Adv. Drug Saf. 2018, 9, 197–205. [Google Scholar] [CrossRef]
- Amato, D.; Kruyer, A.; Samaha, A.-N.; Heinz, A. Hypofunctional Dopamine Uptake and Antipsychotic Treatment-Resistant Schizophrenia. Front. Psychiatry 2019, 10, 314. [Google Scholar] [CrossRef]
- Polati, E.; Canonico, P.L.; Schweiger, V.; Collino, M. Tapentadol: An Overview of the Safety Profile. J. Pain Res. 2019, 12, 1569. [Google Scholar] [CrossRef]
- Vondrackova, D.; Leyendecker, P.; Meissner, W.; Hopp, M.; Szombati, I.; Hermanns, K.; Ruckes, C.; Weber, S.; Grothe, B.; Fleischer, W.; et al. Analgesic Efficacy and Safety of Oxycodone in Combination with Naloxone as Prolonged Release Tablets in Patients with Moderate to Severe Chronic Pain. J. Pain 2008, 9, 1144–1154. [Google Scholar] [CrossRef]
- Lopes, G.S.; Bielinski, S.; Moyer, A.M.; Jacobson, D.J.; Wang, L.; Jiang, R.; Larson, N.B.; Miller, V.M.; Zhu, Y.; Cavanaugh, D.C.; et al. Sex Differences in Type and Occurrence of Adverse Reactions to Opioid Analgesics: A Retrospective Cohort Study. BMJ Open 2021, 11, e044157. [Google Scholar] [CrossRef]
- Barrachina, J.; Margarit, C.; Muriel, J.; López-Gil, S.; López-Gil, V.; Vara-González, A.; Planelles, B.; Inda, M.-M.; Morales, D.; Peiró, A.M. Oxycodone/Naloxone vs. Tapentadol in Real-World Chronic Non-Cancer Pain Management: An Observational and Pharmacogenetic Study. Sci. Rep. 2022, 12, 10126. [Google Scholar] [CrossRef]
- European Monitoring Centre for Drugs and Drug Addiction Pregnancy and Opioid Use: Strategies for Treatment. Available online: https://www.emcdda.europa.eu/publications/emcdda-papers/pregnacy-opioid-use_en (accessed on 9 September 2022).
- Baron, R.; Binder, A.; Wasner, G. Neuropathic Pain: Diagnosis, Pathophysiological Mechanisms, and Treatment. Lancet. Neurol. 2010, 9, 807–819. [Google Scholar] [CrossRef]
- Costigan, M.; Scholz, J.; Woolf, C.J. Neuropathic Pain: A Maladaptive Response of the Nervous System to Damage. Annu. Rev. Neurosci. 2009, 32, 1–32. [Google Scholar] [CrossRef] [PubMed]
- Colloca, L.; Ludman, T.; Bouhassira, D.; Baron, R.; Dickenson, A.H.; Yarnitsky, D.; Freeman, R.; Truini, A.; Attal, N.; Finnerup, N.B.; et al. Neuropathic Pain. Nat. Rev. Dis. Prim. 2017, 3, 17002. [Google Scholar] [CrossRef]
- Barrachina, J.; Muriel, J.; Margarit, C.; Planelles, B.; Ballester, P.; Richart-Martínez, M.; Cutillas, E.; Zandonai, T.; Morales, D.; Peiró, A.M. Global Pain State Questionnaire: Reliability, Validity, and Gender Gap. Arch. Intern. Med. Res. 2021, 4, 84–106. [Google Scholar] [CrossRef]
- Bird, S.B.; Dickson, E.W. Clinically Significant Changes in Pain along the Visual Analog Scale. Ann. Emerg. Med. 2001, 38, 639–643. [Google Scholar] [CrossRef] [PubMed]
- Kelly, A.M. The Minimum Clinically Significant Difference in Visual Analogue Scale Pain Score Does Not Differ with Severity of Pain. Emerg. Med. J. 2001, 18, 205. [Google Scholar] [CrossRef]
- Sino, C.G.; Stuffken, R.; Heerdink, E.R.; Schuurmans, M.J.; Souverein, P.C.; Egberts, T.C. The Association between Prescription Change Frequency, Chronic Disease Score and Hospital Admissions: A Case Control Study. BMC Pharmacol. Toxicol. 2013, 14, 39. [Google Scholar] [CrossRef]
- Mercadante, S.; Caraceni, A. Conversion Ratios for Opioid Switching in the Treatment of Cancer Pain: A Systematic Review. Palliat. Med. 2011, 25, 504–515. [Google Scholar] [CrossRef]
- Mercadante, S.; Porzio, G.; Aielli, F.; Adile, C.; Verna, L.; Ficorella, C.; Giarratano, A.; Casuccio, A. Opioid Switching from and to Tapentadol Extended Release in Cancer Patients: Conversion Ratio with Other Opioids. Curr. Med. Res. Opin. 2013, 29, 661–666. [Google Scholar] [CrossRef]
- Faculty of Pain Medicine of the Royal College of Anaesthetists Dose Equivalents and Changing Opioids. Available online: https://fpm.ac.uk/opioids-aware-structured-approach-opioid-prescribing/dose-equivalents-and-changing-opioids (accessed on 26 July 2022).
- Richards, B.L.; Whittle, S.L.; Buchbinder, R. Neuromodulators for Pain Management in Rheumatoid Arthritis. Cochrane Database Syst. Rev. 2012, 1, 2–3. [Google Scholar] [CrossRef]
- Boiarkina, A.; Potapov, A. Impact of Genetic Factors on Severity of Side Effects of Opioids in Patients after Major Surgical Interventions. Klin. Khirurhiia 2014, 5, 52–55. [Google Scholar]
- Spanish Agency of Medicines and Health Products (AEMPS-CIMA) Online Information Center of Medicines of Spanish Agency of Medicines and Health Products (AEMPS-CIMA). Available online: https://cima.aemps.es/cima/publico/home.html (accessed on 17 March 2021).
- Mathieson, K. Making Sense of Biostatistics: Types of Nonprobability Sampling. J. Clin. Res. Best Pract. 2014, 10, 330–333. [Google Scholar] [CrossRef]
- Planelles, B.; Margarit, C.; Inda, M.-D.-M.; Ballester, P.; Muriel, J.; Barrachina, J.; Ajo, R.; Esteban, M.D.; Peiró, A.M. Gender Based Differences, Pharmacogenetics and Adverse Events in Chronic Pain Management. Pharmacogenomics J. 2020, 20, 320–328. [Google Scholar] [CrossRef]
- Jovey, R.D.; Ennis, J.; Gardner-Nix, J.; Goldman, B.; Hays, H.; Lynch, M.; Moulin, D.; Canadian Pain Society. Use of Opioid Analgesics for the Treatment of Chronic Noncancer Pain—A Consensus Statement and Guidelines from the Canadian Pain Society, 2002. Pain Pract. 2019, 5, 3–28. [Google Scholar] [CrossRef] [PubMed]
- Hawkins, E.J.; Malte, C.A.; Grossbard, J.R.; Saxon, A.J. Prevalence and Trends of Concurrent Opioid Analgesic and Benzodiazepine Use Among Veterans Affairs Patients with Post-Traumatic Stress Disorder, 2003-2011. Pain Med. 2015, 16, 1943–1954. [Google Scholar] [CrossRef] [PubMed]
- United Nations. Informe de La Junta Internacional de Fiscalización de Estupefacientes Correspondientes a 2019; United Nations: Viena, Austria, 2020. [Google Scholar]
- Sistema Nacional de Salud; Ministerio de Sanidad. Prestación Farmacéutica En El Sistema Nacional de Salud. Informe Anual Del Sistema Nacional de Salud 2018; Ministerio de Sanidad: Madrid, Spain, 2018. [Google Scholar]
- Huerta, C.; Abbing-Karahagopian, V.; Requena, G.; Oliva, B.; Alvarez, Y.; Gardarsdottir, H.; Miret, M.; Schneider, C.; Gil, M.; Souverein, P.C.; et al. Exposure to Benzodiazepines (Anxiolytics, Hypnotics and Related Drugs) in Seven European Electronic Healthcare Databases: A Cross-National Descriptive Study from the PROTECT-EU Project. Pharmacoepidemiol. Drug Saf. 2016, 25 (Suppl. 1), 56–65. [Google Scholar] [CrossRef]
- Karanti, A.; Bobeck, C.; Osterman, M.; Kardell, M.; Tidemalm, D.; Runeson, B.; Lichtenstein, P.; Landén, M. Gender Differences in the Treatment of Patients with Bipolar Disorder: A Study of 7354 Patients. J. Affect. Disord. 2015, 174, 303–309. [Google Scholar] [CrossRef]
- Boyd, A.; Van de Velde, S.; Pivette, M.; ten Have, M.; Florescu, S.; O’Neill, S.; Caldas-de-Almeida, J.M.; Vilagut, G.; Haro, J.M.; Alonso, J.; et al. Gender Differences in Psychotropic Use across Europe: Results from a Large Cross-Sectional, Population-Based Study. Eur. Psychiatry 2015, 30, 778–788. [Google Scholar] [CrossRef]
- United Nations—Office on Drugs and Crime. Substance Abuse Treatment and Care for Women: Case Studies and Lessons Learned; United Nations: Viena, Austria, 2004. [Google Scholar]
- Chung, J.W.Y.; Zeng, Y.; Wong, T.K.S. Drug Therapy for the Treatment of Chronic Nonspecific Low Back Pain: Systematic Review and Meta-Analysis. Pain Physician 2013, 16, E685–E704. [Google Scholar] [CrossRef]
- Craft, R.M. Sex Differences in Opioid Analgesia: “From Mouse to Man”. Clin. J. Pain 2003, 19, 175–186. [Google Scholar] [CrossRef]
- Muriel, J.; Margarit, C.; Barrachina, J.; Ballester, P.; Flor, A.; Morales, D.; Horga, J.F.; Fernández, E.; Peiró, A.M. Pharmacogenetics and Prediction of Adverse Events in Prescription Opioid Use Disorder Patients. Basic Clin. Pharmacol. Toxicol. 2019, 124, 439–448. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention Understanding the Epidemic|CDC’s Response to the Opioid Overdose Epidemic|CDC. Available online: https://www.cdc.gov/opioids/basics/epidemic.html (accessed on 21 October 2021).
- U.S. Department of Health and Human Services. Final Report: Opioid Use, Misuse, and Overdose in Women; U.S. Department of Health and Human Services: Washington, DC, USA, 2017.
- Nikolov, V.; Petkova, M. Pain Sensitivity among Women with Low Estrogen Levels. Procedia Soc. Behav. Sci. 2010, 5, 289–293. [Google Scholar] [CrossRef]
- Claréus, B.; Renström, E.A. Physicians’ Gender Bias in the Diagnostic Assessment of Medically Unexplained Symptoms and Its Effect on Patient-Physician Relations. Scand. J. Psychol. 2019, 60, 338–347. [Google Scholar] [CrossRef] [PubMed]
- Campesi, I.; Montella, A.; Seghieri, G.; Franconi, F. The Person’s Care Requires a Sex and Gender Approach. J. Clin. Med. 2021, 10, 4770. [Google Scholar] [CrossRef] [PubMed]
- Ruiz-Cantero, M.-T.; Blasco-Blasco, M.; Chilet-Rosell, E.; Peiró, A.M.; Ruiz-Cantero, M.-T.; Blasco-Blasco, M.; Chilet-Rosell, E.; Peiró, A.M. Sesgos de Género En El Esfuerzo Terapéutico: De La Investigación a La Atención Sanitaria. Farm. Hosp. 2020, 44, 109–113. [Google Scholar] [CrossRef] [PubMed]
- Gombert, M.; Ballester, P.; Segura, A.; Peiró, A.M. Introducing Sexual Dysfunction in Mental Care. Expert Opin. Drug Saf. 2021, 20, 69–79. [Google Scholar] [CrossRef]
- Loikas, D.; Wettermark, B.; Von Euler, M.; Bergman, U.; Schenck-Gustafsson, K. Differences in Drug Utilisation between Men and Women: A Cross-Sectional Analysis of All Dispensed Drugs in Sweden. BMJ Open 2013, 3, e002378. [Google Scholar] [CrossRef]
- Orlando, V.; Mucherino, S.; Guarino, I.; Guerriero, F.; Trama, U.; Menditto, E. Gender Differences in Medication Use: A Drug Utilization Study Based on Real World Data. Int. J. Environ. Res. Public Health 2020, 17, 3926. [Google Scholar] [CrossRef]
- Hendriksen, L.C.; van der Linden, P.D.; Lagro-Janssen, A.L.M.; van den Bemt, P.M.L.A.; Siiskonen, S.J.; Teichert, M.; Kuiper, J.G.; Herings, R.M.C.; Stricker, B.H.; Visser, L.E. Sex Differences Associated with Adverse Drug Reactions Resulting in Hospital Admissions. Biol. Sex Differ. 2021, 12, 34. [Google Scholar] [CrossRef]
- López-Ramal, A. Comunicación Telefónica de Eventos Adversos En La Terapéutica Del Dolor: Diferencias Por Sexo y Genética; Miguel Hernández University: Elche, Spain, 2022. [Google Scholar]
- Duvernoy, C.S.; Smith, D.E.; Manohar, P.; Schaefer, A.; Kline-Rogers, E.; Share, D.; McNamara, R.; Gurm, H.S.; Moscucci, M. Gender Differences in Adverse Outcomes after Contemporary Percutaneous Coronary Intervention: An Analysis from the Blue Cross Blue Shield of Michigan Cardiovascular Consortium (BMC2) Percutaneous Coronary Intervention Registry. Am. Heart J. 2010, 159, 677–683.e1. [Google Scholar] [CrossRef]
- Ruiz-Cantero, M.T.; Verdú-Delgado, M. Sesgo de Género En El Esfuerzo Terapéutico. Gac. Sanit. 2004, 18, 118–125. [Google Scholar] [CrossRef] [PubMed]
- Husby, G.K.; Haugen, R.S.; Moen, M.H. Diagnostic Delay in Women with Pain and Endometriosis. Acta Obstet. Gynecol. Scand. 2003, 82, 649–653. [Google Scholar] [CrossRef]
- Schäfer, G.; Prkachin, K.M.; Kaseweter, K.A.; de Williams, A.C. Health Care Providers’ Judgments in Chronic Pain: The Influence of Gender and Trustworthiness. Pain 2016, 157, 1618–1625. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, R.H.N.; Turner, R.M.; Rydell, S.A.; Maclehose, R.F.; Harlow, B.L. Perceived Stereotyping and Seeking Care for Chronic Vulvar Pain. Pain Med. 2013, 14, 1461–1467. [Google Scholar] [CrossRef]
- Tabach Apraiz, A.; Lorena Oyanadel, M.; Gutiérrez Espinoza, H.; Bueno Buker, D.; Tabach Apraiz, A.; Lorena Oyanadel, M.; Gutiérrez Espinoza, H.; Bueno Buker, D. Correlation study between diagnostic opportunity and pain severity in patients with fibromyalgia who enter the Nononcological Chronic Pain Unit at the San Borja Arriarán Clinical Hospital. Rev. La Soc. Española Del Dolor 2019, 26, 331–336. [Google Scholar] [CrossRef]
- Planelles, B.; Margarit, C.; Ajo, R.; Sastre, Y.; Muriel, J.; Inda, M.-D.-M.; Esteban, M.D.; Peiró, A.M. Health Benefits of an Adverse Events Reporting System for Chronic Pain Patients Using Long-Term Opioids. Acta Anaesthesiol. Scand. 2019, 63, 248–258. [Google Scholar] [CrossRef] [PubMed]
- Rao, S.S.C.; Meduri, K. What Is Necessary to Diagnose Constipation? Best Pract. Res. Clin. Gastroenterol. 2011, 25, 127–140. [Google Scholar] [CrossRef]
| Women (n = 368) | Men (n = 203) | OXN | TAP | OPO | ||||
|---|---|---|---|---|---|---|---|---|
| Women (n = 114) | Men (n = 61) | Women (n = 143) | Men (n = 51) | Women (n = 111) | Men (n = 91) | |||
| Age | 66 [55–76] + | 63 [52–73] | 67 [55–76] 65 ± 13 | 62 [53–72] 62 ± 14 | 66 [54–76] 65 ± 14 | 67 [54–77] 66 ± 14 | 67 [52–77] 64 ± 15 | 60 [50–72] 61 ± 14 |
| Pain intensity | 69 [40–80] | 70 [40–80] | 70 [50–80] | 70 [50–80] * | 60 [50–80] | 67.5 [40–80] * | 60 [30–80] | 70 [40–90] * |
| Pain relief | 38 [10–60] | 30 [0–52] | 40 [10–60] * | 50 [10–60] *# | 40 [20–60] * | 30 [0–60] | 27 [0–55] | 20 [0–50] |
| Likert pain intensity | ||||||||
| None | 5 | 6 | 4 | 2 | 4 | 11 | 8 | 7 |
| Mild | 11 | 7 | 15 | 9 | 16 | 15 | 2 | 4 |
| Moderate | 28 | 28 | 27 | 34 | 27 | 26 | 33 | 26 |
| Severe | 42 | 37 | 47 * | 49 * | 43 | 41 * | 33 | 26 |
| Extremely severe | 14 | 22 | 7 * | 6 * | 10 * | 7 * | 24 | 35 |
| Likert pain relief | ||||||||
| None | 21 | 24 | 20 | 24 | 22 | 27 | 21 | 19 |
| Mild | 26 | 31 | 32 | 33 | 21 | 35 | 21 | 20 |
| Moderate | 38 | 33 | 35 | 35 | 41 | 23 | 36 | 38 |
| Severe | 11 | 10 | 10 | 6 | 11 | 12 | 17 | 15 |
| Extremely | 4 | 4 | 3 | 2 | 4 | 4 | 5 | 8 |
| EuroQol (0–100 mm) | 50 [30–60] | 50 [30–60] | 50 [27.5–60] | 50 [30–60] | 50 [30–60] | 50 [30–67.5] | 50 [27–65] | 50 [22–66] |
| Due to pain | ||||||||
| Emergency department visit | 21 | 19 | 35 + | 16 | 17 | 13 * | 29 | 34 |
| Hospital admission | 6 | 7 | 6 | 10 | 5 | 0 | 8 | 9 |
| Prescription change | 30 | 34 | 38 | 49 *# | 28 | 30 | 25 | 27 |
| Due to other causes | ||||||||
| Emergency department visit | 27 + | 19 | 30 | 17 | 30 | 18 | 26 | 21 |
| Hospital admission | 14 | 12 | 23 *# | 20 | 10 | 8 | 10 | 10 |
| Prescription change | 22 + | 15 | 30 +* | 18 | 22 + | 8 | 13 | 18 |
| Pain Medication (%) | Women (n = 368) | Men (n = 203) | OXN | TAP | OPO | |||
|---|---|---|---|---|---|---|---|---|
| Women (n = 114) | Men (n = 61) | Women (n = 143) | Men (n = 51) | Women (n = 111) | Men (n = 91) | |||
| Analgesic | 34 | 38 | 32 | 27 | 38 | 30 | 31 | 49 *++ |
| Tramadol | 12 | 13 | 8 | 6 | 20 +# | 9 | 45 ** | 55 ** |
| NSAIDs | 24 | 28 | 13 | 11 | 12 | 13 | 11 | 13 |
| Opioids (%) | ||||||||
| MEDD (mg/day) | 102 ± 96 | 96 ± 100 | 127 ± 103 +** | 117 ± 122 * | 88 ± 88 | 90 ± 88 | 92 ± 92 | 85 ± 86 |
| Fentanyl transdermal | 19 | 22 | 16 | 16 | 8 | 6 | 37 ** | 36 ** |
| Oxycodone | 3 | 5 | 2 | 2 | 2 | 4 | 11 * | 8 |
| Morphine | 6 | 9 | 2 | 3 | 4 | 11 | 7 ** | 11 |
| Buprenorphine | 5 | 2 | 3 | 2 | 1 | 0 | 14 +** | 4 |
| Hydromorphone | 3 | 1 | 2 | 0 | 1 | 0 | 5 * | 2 |
| Neuromodulators (%) | ||||||||
| Pregabalin | 29 | 33 | 34 | 49 +**# | 23 | 28 | 32 | 25 |
| Gabapentin | 13 | 12 | 13 | 13 | 10 | 11 | 16 | 11 |
| Duloxetine | 18 | 20 | 25 # | 24 * | 14 | 20 | 15 | 18 |
| Benzodiazepines | 39 + | 29 | 46 ++*# | 22 | 32 # | 30 | 40 | 42 * |
| Women (n = 368) | Men (n = 203) | OXN | TAP | OPO | ||||
|---|---|---|---|---|---|---|---|---|
| Women (n = 114) | Men (n = 61) | Women (n = 143) | Men (n = 51) | Women (n = 111) | Men (n = 91) | |||
| Total (%) | 6 [3–8] + | 5 [2–8] | 6 [4–10] **## | 6 [3–8] *# | 5 [3–8] +** | 4 [1–6] | 5 [2–7] | 4 [2–8] |
| Somnolence | 43 | 41 | 48 | 48 * | 39 | 45 | 43 | 33 |
| Dizziness | 37 | 30 | 40 | 31 | 37 | 26 | 34 | 32 |
| Nausea | 24 | 22 | 31 | 25 # | 22 | 13 | 20 | 26 * |
| Vomits | 10 | 7 | 13 | 7 | 8 | 4 | 9 | 9 |
| Constipation | 57 + | 49 | 71 **## | 63 *# | 50 | 43 | 49 | 43 |
| Redness skin | 17 | 13 | 26 *# | 21 *# | 12 | 9 | 14 + | 7 |
| Sexual impotence | 9 | 16 + | 3 | 23 +* | 10 | 19 * | 13 * | 10 |
| Loss of libido | 18 | 31 ++ | 19 | 34 + | 22 | 32 | 12 | 27 + |
| Weight change | 40 ++ | 28 | 48 +* | 23 | 42 | 30# | 33 | 23 |
| Headache | 36 + | 28 | 38 | 39 * | 36 + | 21# | 34 | 21 |
| Itching | 18 | 12 | 30 | 18 | 28 | 15 | 24 | 20 |
| Dry skin | 43 ++ | 26 | 51 +* | 31 | 43 + | 23 | 34 | 31 |
| Xerostomia (dry mouth) | 65 | 61 | 72 | 62 | 64 | 62 | 59 | 60 |
| Edema | 17 | 13 | 23 * | 18 | 19 * | 13 | 9 | 9 |
| Depression | 36 | 34 | 38 | 38 | 37 | 23 | 33 | 37 |
| Insomnia | 33 | 32 | 23 | 18 * | 35 *# | 38 *# | 23 | 31 |
| Nervousness | 45 | 44 | 54 * | 52 | 44 | 34# | 37 | 43 |
| Lack of appetite | 31 | 25 | 33 | 25 | 33 | 21 | 25 | 28 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Barrachina, J.; Margarit, C.; Muriel, J.; López-Gil, V.; López-Gil, S.; Ballester, P.; Mira-Lorente, L.; Agulló, L.; Peiró, A.M. Sex Differences in Oxycodone/Naloxone vs. Tapentadol in Chronic Non-Cancer Pain: An Observational Real-World Study. Biomedicines 2022, 10, 2468. https://doi.org/10.3390/biomedicines10102468
Barrachina J, Margarit C, Muriel J, López-Gil V, López-Gil S, Ballester P, Mira-Lorente L, Agulló L, Peiró AM. Sex Differences in Oxycodone/Naloxone vs. Tapentadol in Chronic Non-Cancer Pain: An Observational Real-World Study. Biomedicines. 2022; 10(10):2468. https://doi.org/10.3390/biomedicines10102468
Chicago/Turabian StyleBarrachina, Jordi, Cesar Margarit, Javier Muriel, Vicente López-Gil, Santiago López-Gil, Pura Ballester, Laura Mira-Lorente, Laura Agulló, and Ana M. Peiró. 2022. "Sex Differences in Oxycodone/Naloxone vs. Tapentadol in Chronic Non-Cancer Pain: An Observational Real-World Study" Biomedicines 10, no. 10: 2468. https://doi.org/10.3390/biomedicines10102468
APA StyleBarrachina, J., Margarit, C., Muriel, J., López-Gil, V., López-Gil, S., Ballester, P., Mira-Lorente, L., Agulló, L., & Peiró, A. M. (2022). Sex Differences in Oxycodone/Naloxone vs. Tapentadol in Chronic Non-Cancer Pain: An Observational Real-World Study. Biomedicines, 10(10), 2468. https://doi.org/10.3390/biomedicines10102468









