Method Presentation of a New Integrated Orthodontic-Conservative Approach for Minimally Invasive Full Mouth Rehabilitation: Speed Up Therapy
Abstract
1. Introduction
2. Case Report
2.1. Therapeutic Plan
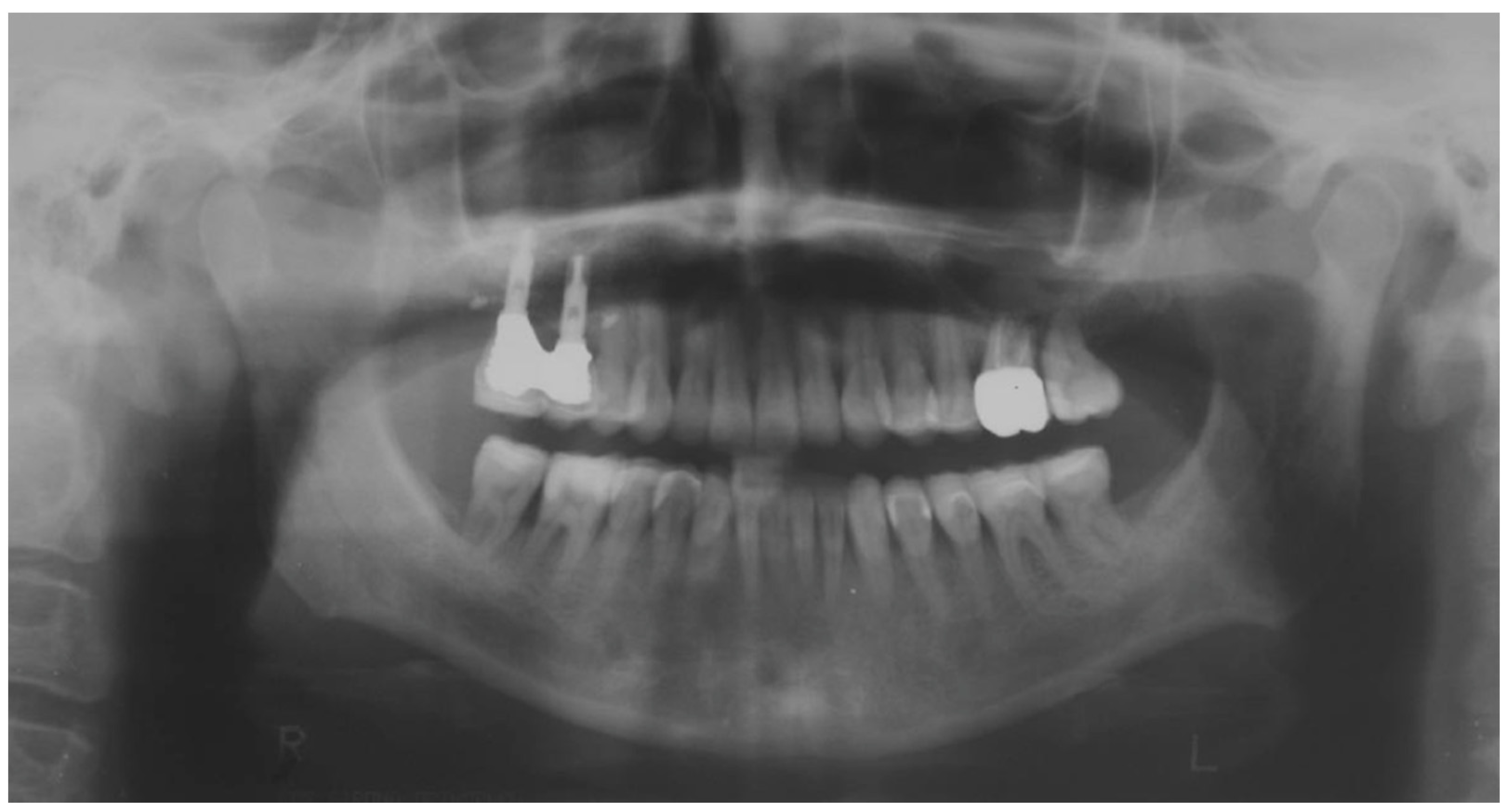
2.2. Clinical Example
2.3. Outcome Achieved
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Redi, F.; Marchio, V.; Derchi, G.; Lardani, L.; Redi, L.; Lanteri, V. Aesthetic parameters of the human profile through the 20th century as an aid for orthodontic treatment. Int. J. Clin. Dent. 2021, 14, 253–261. [Google Scholar]
- Schlueter, N.; Tveit, A.B. Prevalence of erosive tooth wear in risk groups. Monogr. Oral Sci. 2014, 25, 74–98. [Google Scholar] [CrossRef] [PubMed]
- Bartlett, D. Intrinsic causes of erosion. Monogr. Oral Sci. 2006, 20, 119–139. [Google Scholar] [CrossRef]
- Jaeggi, T.; Lussi, A. Prevalence, incidence and distribution of erosion. Monogr. Oral Sci. 2014, 25, 55–73. [Google Scholar] [CrossRef]
- Abate, A.; Gaffuri, F.; Lanteri, V.; Fama, A.; Ugolini, A.; Mannina, L.; Maspero, C. A CBCT based analysis of the correlation between volumetric morphology of the frontal sinuses and the facial growth pattern in caucasian subjects. A cross-sectional study. Head Face Med. 2022, 18, 4. [Google Scholar] [CrossRef] [PubMed]
- Larsen, I.B.; Westergaard, J.; Stoltze, K.; Larsen, A.I.; Gyntelberg, F.; Holmstrup, P. A clinical index for evaluating and monitoring dental erosion. Community Dent. Oral Epidemiol. 2000, 28, 211–217. [Google Scholar] [CrossRef] [PubMed]
- Smith, B.G.; Knight, J.K. An index for measuring the wear of teeth. Br. Dent. J. 1984, 156, 435–438. [Google Scholar] [CrossRef]
- Freitas, A.C.J.; Silva, A.M.; Lima Verde, M.A.R.; Jorge de Aguiar, J.R.P. Oral rehabilitation of severely worn dentition using an overlay for immediate re-establishment of occlusal vertical dimension. Gerodontology 2012, 29, 75–80. [Google Scholar] [CrossRef]
- Derchi, G.; Marchio, V.; Borgia, V.; Özcan, M.; Giuca, M.R.; Barone, A. Twelve-year longitudinal clinical evaluation of bonded indirect composite resin inlays. Quintessence Int. 2019, 50, 448–454. [Google Scholar] [CrossRef]
- Didier, H.; Assandri, F.; Gaffuri, F.; Cavagnetto, D.; Abate, A.; Villanova, M.; Maiorana, C. The Role of Dental Occlusion and Neuromuscular Behavior in Professional Ballet Dancers’ Performance: A Pilot Study. Healthcare 2021, 9, 251. [Google Scholar] [CrossRef]
- Sim, H.-Y.; Kim, H.-S.; Jung, D.-U.; Lee, H.; Lee, J.-W.; Han, K.; Yun, K.-I. Association between orthodontic treatment and periodontal diseases: Results from a national survey. Angle Orthod. 2017, 87, 651–657. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.-I.; Park, S.-B. A multidisciplinary approach for the management of pathologic tooth migration in a patient with moderately advanced periodontal disease. Int. J. Periodontics Restor. Dent. 2012, 32, 225–231. [Google Scholar]
- Gupta, S.; Jain, S.; Gupta, P.; Deoskar, A. Determining skeletal maturation using insulin-like growth factor I (IGF-I) test. Prog. Orthod. 2012, 13, 288–295. [Google Scholar] [CrossRef] [PubMed]
- Baccetti, T.; Franchi, L.; McNamara, J.A.J. An improved version of the cervical vertebral maturation (CVM) method for the assessment of mandibular growth. Angle Orthod. 2002, 72, 316–323. [Google Scholar] [CrossRef]
- Downs, W.B. Variations in facial relationships: Their significance in treatment and prognosis. Am. J. Orthod. 1948, 34, 812–840. [Google Scholar] [CrossRef]
- Cossellu, G.; Lanteri, V.; Lione, R.; Ugolini, A.; Gaffuri, F.; Cozza, P.; Farronato, M. Efficacy of ketoprofen lysine salt and paracetamol/acetaminophen to reduce pain during rapid maxillary expansion: A randomized controlled clinical trial. Int. J. Paediatr. Dent. 2019, 29, 58–65. [Google Scholar] [CrossRef] [PubMed]
- Matarese, G.; Isola, G.; Ramaglia, L.; Dalessandri, D.; Lucchese, A.; Alibrandi, A.; Fabiano, F.; Cordasco, G. Periodontal biotype: Characteristic, prevalence and dimensions related to dental malocclusion. Minerva Stomatol. 2016, 65, 231–238. [Google Scholar]
- Lanteri, V.; Farronato, G.; Lanteri, C.; Caravita, R.; Cossellu, G. The efficacy of orthodontic treatments for anterior crowding with Invisalign compared with fixed appliances using the Peer Assessment Rating Index. Quintessence Int. 2018, 49, 581–587. [Google Scholar] [CrossRef]
- Lanteri, V.; Poggi, S.; Blasi, S.; De Angelis, D.; Gangale, S.; Farronato, M.; Maiorani, C.; Butera, A. Periodontal aspects of orthodontic treatment with invisalign® versus fixed appliances in the same patients—A pilot study. Int. J. Clin. Dent. 2020, 13, 419–447. [Google Scholar]
- Rossini, G.; Parrini, S.; Castroflorio, T.; Deregibus, A.; Debernardi, C.L. Efficacy of clear aligners in controlling orthodontic tooth movement: A systematic review. Angle Orthod. 2015, 85, 881–889. [Google Scholar] [CrossRef]
- Lanteri, V.; Cavagnetto, D.; Abate, A.; Mainardi, E.; Gaffuri, F.; Ugolini, A.; Maspero, C. Buccal Bone Changes Around First Permanent Molars and Second Primary Molars after Maxillary Expansion with a Low Compliance Ni-Ti Leaf Spring Expander. Int. J. Environ. Res. Public Health 2020, 17, 9104. [Google Scholar] [CrossRef] [PubMed]
- Lanteri, V.; Abate, A.; Cavagnetto, D.; Ugolini, A.; Gaffuri, F.; Gianolio, A.; Maspero, C. Cephalometric Changes Following Maxillary Expansion with Ni-Ti Leaf Springs Palatal Expander and Rapid Maxillary Expander: A Retrospective Study. Appl. Sci. 2021, 11, 5748. [Google Scholar] [CrossRef]
- Acharya, V.; Victor, D. Orthodontic management of patients undergoing prosthetic rehabilitation. J. Calif. Dent. Assoc. 2015, 43, 185–191. [Google Scholar] [PubMed]
- Small, B.W. Pre-prosthetic orthodontics for esthetics and function in restorative dentistry. Gen. Dent. 2011, 59, 91–94. [Google Scholar] [PubMed]
- Maspero, C.; Abate, A.; Inchingolo, F.; Dolci, C.; Cagetti, M.G.; Tartaglia, G.M. Incidental Finding in Pre-Orthodontic Treatment Radiographs of an Aural Foreign Body: A Case Report. Children 2022, 9, 421. [Google Scholar] [CrossRef] [PubMed]
- Vailati, F.; Carciofo, S. Treatment planning of adhesive additive rehabilitations: The progressive wax-up of the three-step technique. Int. J. Esthet. Dent. 2016, 11, 356–377. [Google Scholar] [PubMed]
- Vailati, F.; Belser, U.C. Full-mouth adhesive rehabilitation of a severely eroded dentition: The three-step technique. Part 1. Eur. J. Esthet. Dent. Off. J. Eur. Acad. Esthet. Dent. 2008, 3, 30–44. [Google Scholar]
- Vailati, F.; Belser, U.C. Classification and treatment of the anterior maxillary dentition affected by dental erosion: The ACE classification. Int. J. Periodontics Restorative Dent. 2010, 30, 559–571. [Google Scholar] [PubMed]
- Lo Giudice, A.; Ortensi, L.; Farronato, M.; Lucchese, A.; Lo Castro, E.; Isola, G. The step further smile virtual planning: Milled versus prototyped mock-ups for the evaluation of the designed smile characteristics. BMC Oral Health 2020, 20, 165. [Google Scholar] [CrossRef] [PubMed]
- Vailati, F.; Belser, U.C. Full-mouth adhesive rehabilitation of a severely eroded dentition: The three-step technique. Part 3. Eur. J. Esthet. Dent. Off. J. Eur. Acad. Esthet. Dent. 2008, 3, 236–257. [Google Scholar]
- Belser, U.C.; Magne, P.; Magne, M. Ceramic laminate veneers: Continuous evolution of indications. J. Esthet. Dent. 1997, 9, 197–207. [Google Scholar] [CrossRef]
- Vailati, F.; Belser, U.C. Full-mouth adhesive rehabilitation of a severely eroded dentition: The three-step technique. Part 2. Eur. J. Esthet. Dent. Off. J. Eur. Acad. Esthet. Dent. 2008, 3, 128–146. [Google Scholar]
- Grippo, J.O.; Simring, M.; Schreiner, S. Attrition, abrasion, corrosion and abfraction revisited: A new perspective on tooth surface lesions. J. Am. Dent. Assoc. 2004, 135, 1105–1109. [Google Scholar] [CrossRef] [PubMed]
- Lussi, A.; Carvalho, T.S. Erosive tooth wear: A multifactorial condition of growing concern and increasing knowledge. Monogr. Oral Sci. 2014, 25, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Sfondrini, M.F.; Butera, A.; Di Michele, P.; Luccisano, C.; Ottini, B.; Sangalli, E.; Gallo, S.; Pascadopoli, M.; Gandini, P.; Scribante, A. Microbiological Changes during Orthodontic Aligner Therapy: A Prospective Clinical Trial. Appl. Sci. 2021, 11, 6758. [Google Scholar] [CrossRef]
- Butera, A.; Maiorani, C.; Morandini, A.; Simonini, M.; Morittu, S.; Barbieri, S.; Bruni, A.; Sinesi, A.; Ricci, M.; Trombini, J.; et al. Assessment of Genetical, Pre, Peri and Post Natal Risk Factors of Deciduous Molar Hypomineralization (DMH), Hypomineralized Second Primary Molar (HSPM) and Molar Incisor Hypomineralization (MIH): A Narrative Review. Children 2021, 8, 432. [Google Scholar] [CrossRef]
- Zharmagambetova, A.; Tuleutayeva, S.; Akhmetova, S.; Zharmagambetov, A. MICROBIOLOGICAL ASPECTS OF THE ORTHODONTIC TREATMENT. Georgian Med. News 2017, 264, 39–43. [Google Scholar]
- Bartlett, D.; Ganss, C.; Lussi, A. Basic Erosive Wear Examination (BEWE): A new scoring system for scientific and clinical needs. Clin. Oral Investig. 2008, 12 (Suppl. 1), S65–S68. [Google Scholar] [CrossRef]















| Before | After | |
|---|---|---|
| Disharmonious smile | Yes | No |
| Dyschromia, dysmorphia, abrasions, and erosions of teeth | Yes | No |
| Anterior crowding in the upper arch | Yes | No |
| Anterior crowding in the lower arch | Yes | No |
| Upper transverse discrepancy | Yes | No |
| Presence of buccal corridors or black tunnels | Yes | No |
| Curve of Spee alteration | Yes | No |
| Curve of Wilson alteration | Yes | No |
| Functional movements with altered guides | Yes | No |
| Pain and/or noise ATM | Yes | No |
| Parameter Examined | Clinical Significance | Result Obtained |
|---|---|---|
| Smile symmetry | Smile symmetry refers to the mirror agreement between the two sides of the mouth but can also consider the bi-pupillary line, the incisal line, and the labial commissure. | YES |
| Horizontal symmetry | It originates from the presence of similar elements placed in a regular sequence, as verified in a dentition with teeth well aligned in the horizontal plane. | YES |
| Vertical symmetry | Recall the same principle as above, referring to the vertical direction. | YES |
| Repeated report | It indicates the division of space into portions that may not be identical in shape and size but arranged to generate a harmonious connection between them. This is what is verified between opposing hemiarches with well-arranged teeth, inspiring a sense of order and balance. | YES |
| Prospective effect | The contour of the buccal surface and the alignment of the inclined planes of the teeth is decisive in generating a correct perspective effect. The different length or strong color difference of even one element can impair the perspective effect and compromise the sense of harmony of the whole. | YES |
| Lip height | Useful distinction in static and dynamic harmony. The average height of the upper vermilion is 7.1 mm in the male and 7.7 mm in the female. The lower vermilion is normally more extensive, about 10 mm on average; these are statistical values, with wide individual variations. | YES |
| Lip line | The height of the upper lip, relative to the upper central incisors, can be classified as low, medium, or high, on the basis of the amount of crown exposure. | YES |
| Smile line | Smile line is a curved line passing through the incisal margin of the upper incisors, parallel to the inner margin of the lower lip. | YES |
| Curvature of the upper lip | With superior convexity, it extends from the center toward the lateral triangular spaces. When rectilinear or worse with inverted convexity, it gives the subject a sad and unattractive expression. | YES |
| Frontal axial alignment | The smooth slope of the long axis of the front elements helps generate a sense of regularity. | YES |
| Tooth alignment in the arch | Recalls the anatomical harmony represented by the correct positioning of teeth in the center of the alveolar ridge. | YES |
| Contact point alignment | In the anterior sectors, the contact points are located near the incisal third and their sequence defines a curvilinear pattern. | YES |
| Color | Color is one of the cardinal elements of dental aesthetic recovery. It must always be evaluated in a much broader context, involving many other periodontal, labial, and skin parameters of the patient. | YES |
| Gingival scalloping | Gingival parabolas are decisive for the aesthetic effect of the frontal group. Orthodontic treatment can contribute to their harmonization. | YES |
| Negative space | A restrained smile enhances the characteristics of the teeth, while an excessive smile imparts an unattractive sense of emptiness. | YES |
| Arch geometry | There are several types of arch form related to individual craniofacial conformation that must be recreated or respected by orthodontic treatment. | YES |
| Buccal corridors o black tunnels | A restrained smile enhances the characteristics of the teeth, while an excessive smile imparts an unattractive sense of emptiness. | YES |
| Fibonacci golden proportion | It evaluates proportions by relating harmony to numerical values. In the dental field, it can find application in the evaluation of various dental and facial morphological parameters. | YES |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Foschi, D.; Abate, A.; Maspero, C.; Solimei, L.; Lanteri, C.; Lanteri, V. Method Presentation of a New Integrated Orthodontic-Conservative Approach for Minimally Invasive Full Mouth Rehabilitation: Speed Up Therapy. Biomedicines 2022, 10, 2536. https://doi.org/10.3390/biomedicines10102536
Foschi D, Abate A, Maspero C, Solimei L, Lanteri C, Lanteri V. Method Presentation of a New Integrated Orthodontic-Conservative Approach for Minimally Invasive Full Mouth Rehabilitation: Speed Up Therapy. Biomedicines. 2022; 10(10):2536. https://doi.org/10.3390/biomedicines10102536
Chicago/Turabian StyleFoschi, Davide, Andrea Abate, Cinzia Maspero, Luca Solimei, Claudio Lanteri, and Valentina Lanteri. 2022. "Method Presentation of a New Integrated Orthodontic-Conservative Approach for Minimally Invasive Full Mouth Rehabilitation: Speed Up Therapy" Biomedicines 10, no. 10: 2536. https://doi.org/10.3390/biomedicines10102536
APA StyleFoschi, D., Abate, A., Maspero, C., Solimei, L., Lanteri, C., & Lanteri, V. (2022). Method Presentation of a New Integrated Orthodontic-Conservative Approach for Minimally Invasive Full Mouth Rehabilitation: Speed Up Therapy. Biomedicines, 10(10), 2536. https://doi.org/10.3390/biomedicines10102536









