Neutrophils Play an Important Role in the Recurrence of Chronic Rhinosinusitis with Nasal Polyps
Abstract
:1. Introduction
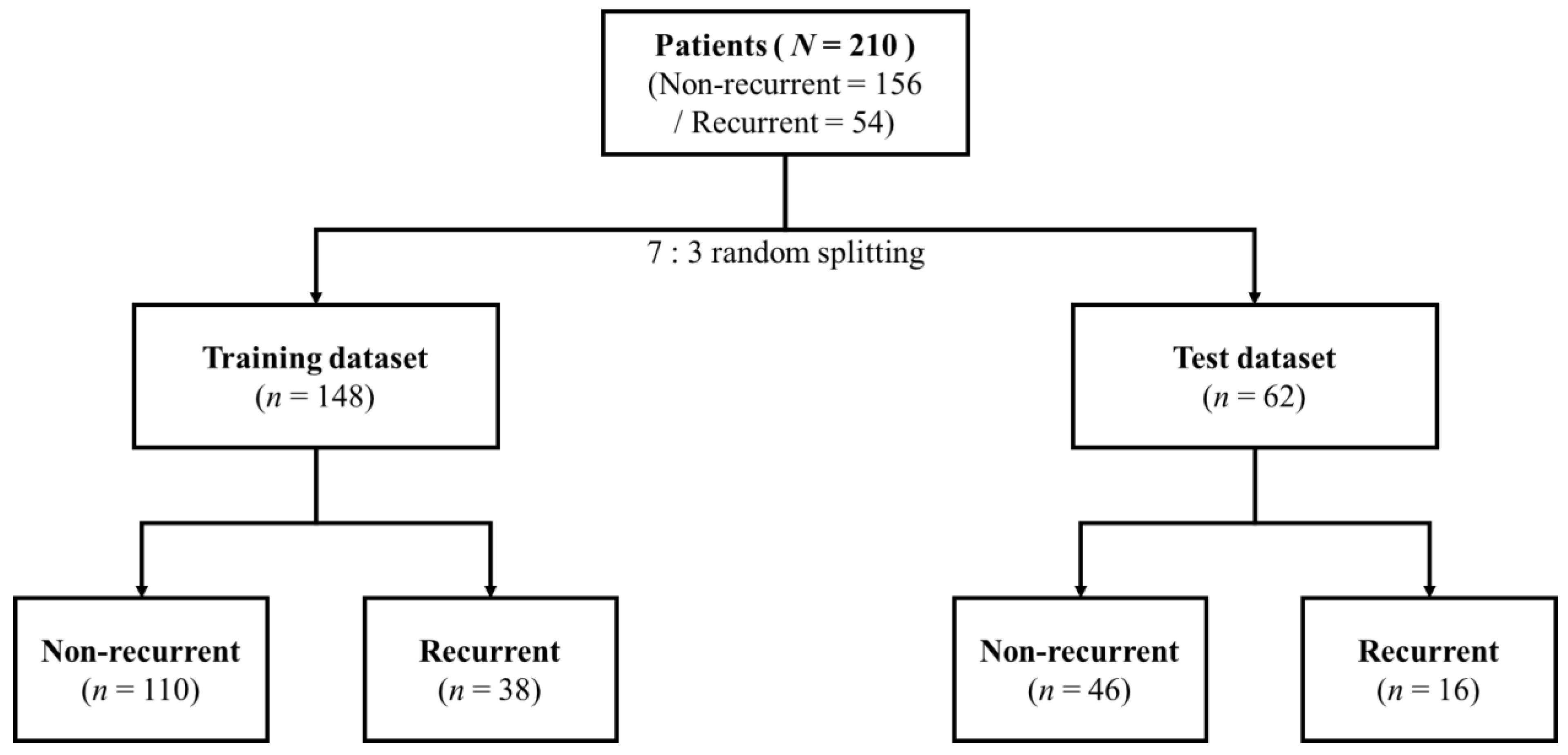
2. Materials and Methods
2.1. Patients and Tissue Samples
2.2. Cytokine Measurement
2.3. Statistical Analysis
3. Results
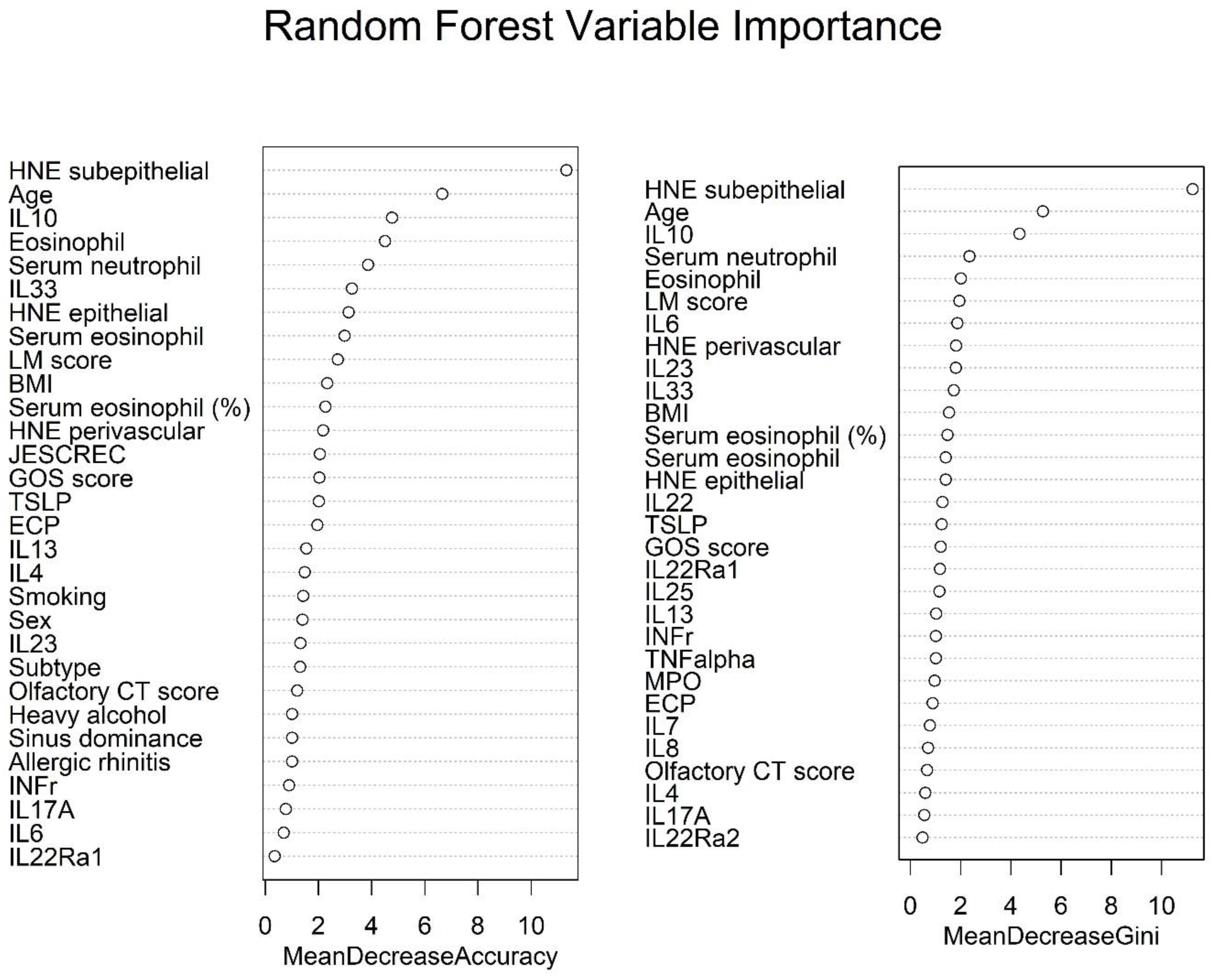
Prediction of Surgical Outcomes for CRSwNP
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Fokkens, W.J.; Lund, V.J.; Hopkins, C.; Hellings, P.W.; Kern, R.; Reitsma, S. EPOS2020: A Major Step Forward. Rhinology 2020, 58, 1–464. [Google Scholar] [CrossRef] [PubMed]
- Bassiouni, A.; Wormald, P.-J. Role of frontal sinus surgery in nasal polyp recurrence. Laryngoscope 2013, 123, 36–41. [Google Scholar] [CrossRef] [PubMed]
- DeConde, A.S.; Mace, J.C.; Levy, J.M.; Rudmik, L.; Alt, J.A.; Smith, T.L. Prevalence of polyp recurrence after endoscopic sinus surgery for chronic rhinosinusitis with nasal polyposis. Laryngoscope 2017, 127, 550–555. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stein, N.R.; Jafari, A.; DeConde, A.S. Revision rates and time to revision following endoscopic sinus surgery: A large database analysis. Laryngoscope 2018, 128, 31–36. [Google Scholar] [CrossRef] [PubMed]
- Kato, A.; Schleimer, R.P.; Bleier, B.S. Mechanisms and pathogenesis of chronic rhinosinusitis. J. Allergy Clin. Immunol. 2022, 149, 1491–1503. [Google Scholar] [CrossRef]
- Delemarre, T.; Bochner, B.S.; Simon, H.-U.; Bachert, C. Rethinking neutrophils and eosinophils in chronic rhinosinusitis. J. Allergy Clin. Immunol. 2021, 148, 327–335. [Google Scholar] [CrossRef]
- Kim, D.-K.; Lee, B.C.; Park, K.J.; Son, G.M. Effect of Obstructive Sleep Apnea on Immunity in Cases of Chronic Rhinosinusitis With Nasal Polyps. Clin. Exp. Otorhinolaryngol. 2021, 14, 390–398. [Google Scholar] [CrossRef]
- Persson, E.K.; Verstraete, K.; Heyndrickx, I.; Gevaert, E.; Aegerter, H.; Percier, J.-M.; Deswarte, K.; Verschueren, K.H.G.; Dansercoer, A.; Gras, D.; et al. Protein crystallization promotes type 2 immunity and is reversible by antibody treatment. Science 2019, 364, eaaw4295. [Google Scholar] [CrossRef]
- Delemarre, T.; Holtappels, G.; De Ruyck, N.; Zhang, N.; Nauwynck, H.; Bachert, C.; Gevaert, E. A substantial neutrophilic inflammation as regular part of severe type 2 chronic rhinosinusitis with nasal polyps. J. Allergy Clin. Immunol. 2020, 147, 179–188.e2. [Google Scholar] [CrossRef]
- Ryu, G.; Kim, D.-K.; Dhong, H.-J.; Eun, K.M.; Lee, K.E.; Kong, I.G.; Kim, H.; Chung, S.-K.; Kim, D.-Y.; Rhee, C.-S.; et al. Immunological Characteristics in Refractory Chronic Rhinosinusitis with Nasal Polyps Undergoing Revision Surgeries. Allergy, Asthma Immunol. Res. 2019, 11, 664–676. [Google Scholar] [CrossRef]
- Kim, D.-K.; Kim, J.Y.; Han, Y.E.; Kim, J.K.; Lim, H.-S.; Eun, K.M.; Yang, S.K.; Kim, D.W. Elastase-Positive Neutrophils Are Associated With Refractoriness of Chronic Rhinosinusitis With Nasal Polyps in an Asian Population. Allergy Asthma Immunol. Res. 2020, 12, 42–55. [Google Scholar] [CrossRef]
- Kim, D.K.; Lim, H.S.; Eun, K.M.; Seo, Y.; Kim, J.K.; Kim, Y.S.; Kim, D.W. Subepithelial neutrophil infiltration as a predictor of the surgical outcome of chronic rhinosinusitis with nasal polyps. Rhinology 2021, 59, 173–180. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.W. Can Neutrophils Be a Cellular Biomarker in Asian Chronic Rhinosinusitis? Clin. Exp. Otorhinolaryngol. 2019, 12, 325–326. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.-K.; Jin, H.R.; Eun, K.M.; Mutusamy, S.; Cho, S.H.; Oh, S.; Kim, D.W. Non-Eosinophilic Nasal Polyps Shows Increased Epithelial Proliferation and Localized Disease Pattern in the Early Stage. PLoS ONE 2015, 10, e0139945. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, D.-K.; Kang, S.I.; Kong, I.G.; Cho, Y.H.; Song, S.K.; Hyun, S.J.; Cho, S.D.; Han, S.-Y.; Cho, S.-H.; Kim, D.W. Two-Track Medical Treatment Strategy According to the Clinical Scoring System for Chronic Rhinosinusitis. Allergy Asthma Immunol. Res. 2018, 10, 490–502. [Google Scholar] [CrossRef]
- Mantovani, A.; Cassatella, M.A.; Costantini, C.; Jaillon, S. Neutrophils in the activation and regulation of innate and adaptive immunity. Nat. Rev. Immunol. 2011, 11, 519–531. [Google Scholar] [CrossRef]
- Wang, H.; Pan, L.; Liu, Z. Neutrophils as a Protagonist and Target in Chronic Rhinosinusitis. Clin. Exp. Otorhinolaryngol. 2019, 12, 337–347. [Google Scholar] [CrossRef] [Green Version]
- Tomassen, P.; Vandeplas, G.; Van Zele, T.; Cardell, L.-O.; Arebro, J.; Olze, H.; Förster-Ruhrmann, U.; Kowalski, M.L.; Olszewska-Ziąber, A.; Holtappels, G.; et al. Inflammatory endotypes of chronic rhinosinusitis based on cluster analysis of biomarkers. J. Allergy Clin. Immunol. 2016, 137, 1449–1456.e4. [Google Scholar] [CrossRef] [Green Version]
- Gevaert, E.; Delemarre, T.; De Volder, J.; Zhang, N.; Holtappels, G.; De Ruyck, N.; Persson, E.; Heyndrickx, I.; Verstraete, K.; Aegerter, H.; et al. Charcot-Leyden crystals promote neutrophilic inflammation in patients with nasal polyposis. J. Allergy Clin. Immunol. 2019, 145, 427–430.e4. [Google Scholar] [CrossRef] [Green Version]
- Hwang, C.S.; Park, S.C.; Cho, H.-J.; Park, D.-J.; Yoon, J.-H.; Kim, C.-H. Eosinophil extracellular trap formation is closely associated with disease severity in chronic rhinosinusitis regardless of nasal polyp status. Sci. Rep. 2019, 9, 8061. [Google Scholar] [CrossRef]
- Ueki, S.; Tokunaga, T.; Melo, R.C.N.; Saito, H.; Honda, K.; Fukuchi, M.; Konno, Y.; Takeda, M.; Yamamoto, Y.; Hirokawa, M.; et al. Charcot-Leyden crystal formation is closely associated with eosinophil extracellular trap cell death. Blood 2018, 132, 2183–2187. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Watelet, J.B.; Demetter, P.; Claeys, C.; Van Cauwenberge, P.; Cuvelier, C.; Bachert, C. Neutrophil-Derived Metalloproteinase-9 Predicts Healing Quality after Sinus Surgery. Laryngoscope 2005, 115, 56–61. [Google Scholar] [CrossRef] [PubMed]
- Watelet, J.-B.; Claeys, C.; Van Cauwenberge, P.; Bachert, C. Predictive and monitoring value of matrix metalloproteinase-9 for healing quality after sinus surgery. Wound Repair Regen. 2004, 12, 412–418. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Meng, Y.; Lou, H.; Wang, K.; Wang, C.; Zhang, L. Blood eosinophil count combined with asthma history could predict chronic rhinosinusitis with nasal polyp recurrence. Acta Oto-Laryngol. 2021, 141, 279–285. [Google Scholar] [CrossRef] [PubMed]
- Thorwarth, R.M.; Scott, D.W.; Lal, D.; Marino, M.J. Machine learning of biomarkers and clinical observation to predict eosinophilic chronic rhinosinusitis: A pilot study. Int. Forum Allergy Rhinol. 2021, 11, 8–15. [Google Scholar] [CrossRef] [PubMed]
- Wu, Q.; Chen, J.; Deng, H.; Ren, Y.; Sun, Y.; Wang, W.; Yuan, L.; Hong, H.; Zheng, R.; Kong, W.; et al. Expert-level diagnosis of nasal polyps using deep learning on whole-slide imaging. J. Allergy Clin. Immunol. 2019, 145, 698–701.e6. [Google Scholar] [CrossRef]


| Chronic Rhinosinusitis with Nasal Polyp | Non-Recurrence (n = 156) | Recurrence (n = 54) | p Value |
|---|---|---|---|
| Endotype | 0.036 | ||
| Non-eosinophil | 125 (80.1%) | 35 (64.8%) | |
| Eosinophil | 31 (19.9%) | 19 (35.2%) | |
| Sex | 0.033 | ||
| Male | 130 (83.3%) | 37 (68.5%) | |
| Female | 26 (16.7%) | 17 (31.5%) | |
| Age | 52.8 ± 13.7 | 41.1 ± 13.7 | <0.001 |
| Smoking | 0.834 | ||
| Non-smoker | 99 (63.5%) | 34 (63.0%) | |
| Ex-smoker | 1 (0.6%) | 0 (0.0%) | |
| Current | 56 (35.9%) | 20 (37.0%) | |
| Heavy alcohol | 0.636 | ||
| 0 | 139 (89.1%) | 50 (92.6%) | |
| 1 | 17 (10.9%) | 4 (7.4%) | |
| BMI | 24.5 ± 3.4 | 23.9 ± 2.8 | 0.255 |
| Asthma | 0.029 | ||
| 0 | 147 (94.2%) | 45 (83.3%) | |
| 1 | 9 (5.8%) | 9 (16.7%) | |
| Allergic rhinitis | 0.140 | ||
| 0 | 95 (60.9%) | 26 (48.1%) | |
| 1 | 61 (39.1%) | 28 (51.9%) | |
| LM score | 14.1 ± 4.4 | 17.7 ± 5.1 | <0.001 |
| GOS score | 11.3 ± 8.4 | 16.8 ± 9.2 | <0.001 |
| Sinus dominance | 0.028 | ||
| Ethmoid | 81 (51.9%) | 38 (70.4%) | |
| Maxillary | 75 (48.1%) | 16 (29.6%) | |
| Olfactory CT score | 4.5 ± 2.5 | 5.5 ± 2.4 | 0.010 |
| Eosinophil (tissue) | 27.4 ± 47.1 | 49.7 ± 51.3 | 0.004 |
| HNE epithelial | 12.0 ± 17.5 | 15.2 ± 18.0 | 0.247 |
| HNE subepithelial | 19.9 ± 20.5 | 49.5 ± 31.9 | <0.001 |
| HNE perivascular | 3.3 ± 5.4 | 6.4 ± 6.6 | 0.001 |
| Serum eosinophil (%) | 3.6 ± 2.5 | 4.6 ± 3.5 | 0.051 |
| Serum eosinophil | 232.4 ± 173.0 | 360.4 ± 265.3 | 0.001 |
| Serum neutrophil | 3908.9 ± 1400.8 | 3738.3 ± 1553.0 | 0.454 |
| ECP | 47.2 ± 124.5 | 4.9 ± 9.2 | <0.001 |
| MPO | 6.4 ± 22.0 | 8.5 ± 15.4 | 0.446 |
| IL4 | 22.0 ± 116.1 | 7.5 ± 13.7 | 0.130 |
| IL5 | 69.1 ± 274.4 | 8.6 ± 15.5 | 0.007 |
| IL6 | 97.4 ± 304.7 | 4.9 ± 8.9 | <0.001 |
| IL7 | 12.1 ± 74.2 | 6.0 ± 12.6 | 0.331 |
| IL8 | 22.7 ± 105.6 | 14.6 ± 40.7 | 0.422 |
| IL18A | 29.1 ± 119.3 | 13.3 ± 46.7 | 0.170 |
| INFγ | 50.4 ± 222.7 | 5.0 ± 16.5 | 0.013 |
| TNFɑ | 64.5 ± 264.5 | 2.5 ± 4.6 | 0.004 |
| IL10 | 4.8 ± 8.6 | 63.2 ± 167.2 | 0.013 |
| Chronic Rhinosinusitis with Nasal Polyp | Non-Recurrence (n = 110) | Recurrence (n = 38) | p |
|---|---|---|---|
| Endotype | 0.171 | ||
| Non-eosinophil | 89 (80.9%) | 26 (68.4%) | |
| Eosinophil | 21 (19.1%) | 12 (31.6%) | |
| Sex | 0.017 | ||
| Male | 94 (85.5%) | 25 (65.8%) | |
| Female | 16 (14.5%) | 13 (34.2%) | |
| Age | 53.0 ± 14.3 | 40.3 ± 12.6 | <0.001 |
| Smoking | 0.696 | ||
| Non-smoker | 72 (65.5%) | 23 (60.5%) | |
| ex-smoker | 1 (0.9%) | 0 (0.0%) | |
| Current | 37 (33.6%) | 15 (39.5%) | |
| Heavy alcohol | 0.827 | ||
| 0 | 98 (89.1%) | 35 (92.1%) | |
| 1 | 12 (10.9%) | 3 (7.9%) | |
| BMI | 24.7 ± 3.3 | 24.1 ± 2.9 | 0.301 |
| Asthma | 0.018 | ||
| 0 | 105 (95.5%) | 31 (81.6%) | |
| 1 | 5 (4.5%) | 7 (18.4%) | |
| Allergic rhinitis | 0.244 | ||
| 0 | 66 (60.0%) | 18 (47.4%) | |
| 1 | 44 (40.0%) | 20 (52.6%) | |
| LM score | 13.7 ± 4.2 | 17.7 ± 5.4 | <0.001 |
| GOS score | 10.8 ± 7.8 | 16.9 ± 8.9 | <0.001 |
| Sinus dominance | 0.161 | ||
| Ethmoid | 62 (56.4%) | 27 (71.1%) | |
| Maxillary | 48 (43.6%) | 11 (28.9%) | |
| Olfactory CT score | 4.6 ± 2.5 | 5.7 ± 2.3 | 0.018 |
| Eosinophil (tissue) | 28.7 ± 49.8 | 50.2 ± 55.8 | 0.027 |
| HNE epithelial | 10.6 ± 15.6 | 14.5 ± 18.2 | 0.202 |
| HNE subepithelial | 18.9 ± 15.4 | 49.8 ± 31.5 | <0.001 |
| HNE perivascular | 3.4 ± 5.5 | 7.7 ± 7.3 | 0.002 |
| Serum eosinophil (%) | 3.8 ± 2.6 | 4.8 ± 3.8 | 0.151 |
| Serum eosinophil | 253.4 ± 186.7 | 376.4 ± 282.4 | 0.016 |
| Serum neutrophil | 3858.8 ± 1339.4 | 3814.3 ± 1714.2 | 0.870 |
| ECP | 56.2 ± 137.6 | 4.2 ± 6.3 | <0.001 |
| MPO | 7.4 ± 25.6 | 9.2 ± 16.0 | 0.611 |
| IL4 | 21.3 ± 110.6 | 8.6 ± 15.9 | 0.244 |
| IL5 | 88.1 ± 314.5 | 9.3 ± 16.8 | 0.010 |
| IL6 | 103.1 ± 303.7 | 5.3 ± 10.0 | 0.001 |
| IL7 | 14.7 ± 87.5 | 7.6 ± 14.6 | 0.418 |
| IL8 | 22.3 ± 94.4 | 8.7 ± 21.9 | 0.164 |
| IL18A | 26.5 ± 108.9 | 16.9 ± 55.3 | 0.489 |
| INFγ | 54.5 ± 245.7 | 5.8 ± 19.3 | 0.042 |
| TNFɑ | 69.1 ± 298.2 | 2.5 ± 4.2 | 0.021 |
| IL10 | 4.6 ± 8.5 | 55.7 ± 145.6 | 0.037 |
| Chronic Rhinosinusitis with Nasal Polyp | Non-Recurrence (n = 46) | Recurrence (n = 16) | p |
|---|---|---|---|
| Endotype | 0.169 | ||
| Non-eosinophil | 36 (78.3%) | 9 (56.2%) | |
| Eosinophil | 10 (21.7%) | 7 (43.8%) | |
| Sex | 1.000 | ||
| Male | 36 (78.3%) | 12 (75.0%) | |
| Female | 10 (21.7%) | 4 (25.0%) | |
| Age | 52.4 ± 12.2 | 42.8 ± 16.4 | 0.016 |
| Smoking | <0.001 | ||
| Non-smoker | 27 (58.7%) | 11 (68.8%) | |
| ex-smoker | 0 (0.0%) | 0 (0.0%) | |
| Current | 19 (41.3%) | 5 (31.2%) | |
| Heavy alcohol | 0.962 | ||
| 0 | 41 (89.1%) | 15 (93.8%) | |
| 1 | 5 (10.9%) | 1 (6.2%) | |
| BMI | 24.1 ± 3.6 | 23.6 ± 2.7 | 0.619 |
| Asthma | 1.000 | ||
| 0 | 42 (91.3%) | 14 (87.5%) | |
| 1 | 4 (8.7%) | 2 (12.5%) | |
| Allergic rhinitis | 0.535 | ||
| 0 | 29 (63.0%) | 8 (50.0%) | |
| 1 | 17 (37.0%) | 8 (50.0%) | |
| LM score | 15.0 ± 4.8 | 17.8 ± 4.5 | 0.041 |
| GOS score | 12.5 ± 9.6 | 16.6 ± 10.3 | 0.154 |
| Sinus dominance | 0.109 | ||
| Ethmoid | 19 (41.3%) | 11 (68.8%) | |
| Maxillary | 27 (58.7%) | 5 (31.2%) | |
| Olfactory CT score | 4.3 ± 2.5 | 5.1 ± 2.7 | 0.277 |
| Eosinophil (tissue) | 24.3 ± 40.3 | 48.4 ± 40.1 | 0.043 |
| HNE epithelial | 15.2 ± 21.1 | 16.8 ± 17.9 | 0.796 |
| HNE subepithelial | 22.3 ± 29.5 | 48.9 ± 34.0 | 0.004 |
| HNE perivascular | 3.1 ± 5.0 | 3.1 ± 2.8 | 0.954 |
| Serum eosinophil (%) | 3.1 ± 2.1 | 4.2 ± 2.7 | 0.086 |
| Serum eosinophil | 182.3 ± 122.7 | 322.2 ± 223.0 | 0.028 |
| Serum neutrophil | 4028.8 ± 1546.9 | 3557.8 ± 1106.2 | 0.267 |
| ECP | 25.7 ± 82.7 | 6.6 ± 14.0 | 0.139 |
| MPO | 4.0 ± 9.1 | 6.7 ± 14.0 | 0.469 |
| IL4 | 23.6 ± 129.6 | 5.0 ± 6.0 | 0.338 |
| IL5 | 23.6 ± 129.1 | 6.8 ± 12.3 | 0.387 |
| IL6 | 83.8 ± 310.0 | 3.8 ± 5.3 | 0.087 |
| IL7 | 5.9 ± 19.0 | 2.3 ± 3.4 | 0.234 |
| IL8 | 23.9 ± 129.6 | 28.6 ± 66.1 | 0.853 |
| IL18A | 35.4 ± 142.1 | 4.7 ± 7.8 | 0.151 |
| INFγ | 40.7 ± 156.6 | 3.3 ± 5.8 | 0.112 |
| TNFɑ | 53.6 ± 159.5 | 2.7 ± 5.5 | 0.036 |
| IL10 | 5.3 ± 9.0 | 81.3 ± 214.3 | 0.177 |
| Model | Accuracy | Sensitivity | Specificity | PPV | NPV | F1 Score | AUC | Optimal Cutoff Value |
|---|---|---|---|---|---|---|---|---|
| DT | 0.903 | 0.875 | 0.913 | 0.778 | 0.955 | 0.824 | 0.946 | 0.545 |
| RF | 0.968 | 0.938 | 0.978 | 0.938 | 0.978 | 0.938 | 0.987 | 0.445 |
| SVM | 0.903 | 1.000 | 0.870 | 0.727 | 1.000 | 0.842 | 0.974 | 0.385 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yu, H.; Kim, D.-K. Neutrophils Play an Important Role in the Recurrence of Chronic Rhinosinusitis with Nasal Polyps. Biomedicines 2022, 10, 2911. https://doi.org/10.3390/biomedicines10112911
Yu H, Kim D-K. Neutrophils Play an Important Role in the Recurrence of Chronic Rhinosinusitis with Nasal Polyps. Biomedicines. 2022; 10(11):2911. https://doi.org/10.3390/biomedicines10112911
Chicago/Turabian StyleYu, Hyunjae, and Dong-Kyu Kim. 2022. "Neutrophils Play an Important Role in the Recurrence of Chronic Rhinosinusitis with Nasal Polyps" Biomedicines 10, no. 11: 2911. https://doi.org/10.3390/biomedicines10112911





