Unmet Need for Oral Corticosteroids Use and Exacerbations of Asthma in Primary Care in Taiwan
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Questionnaire
2.3. Date Analysis
3. Results
3.1. Background of Asthma Treating Physicians
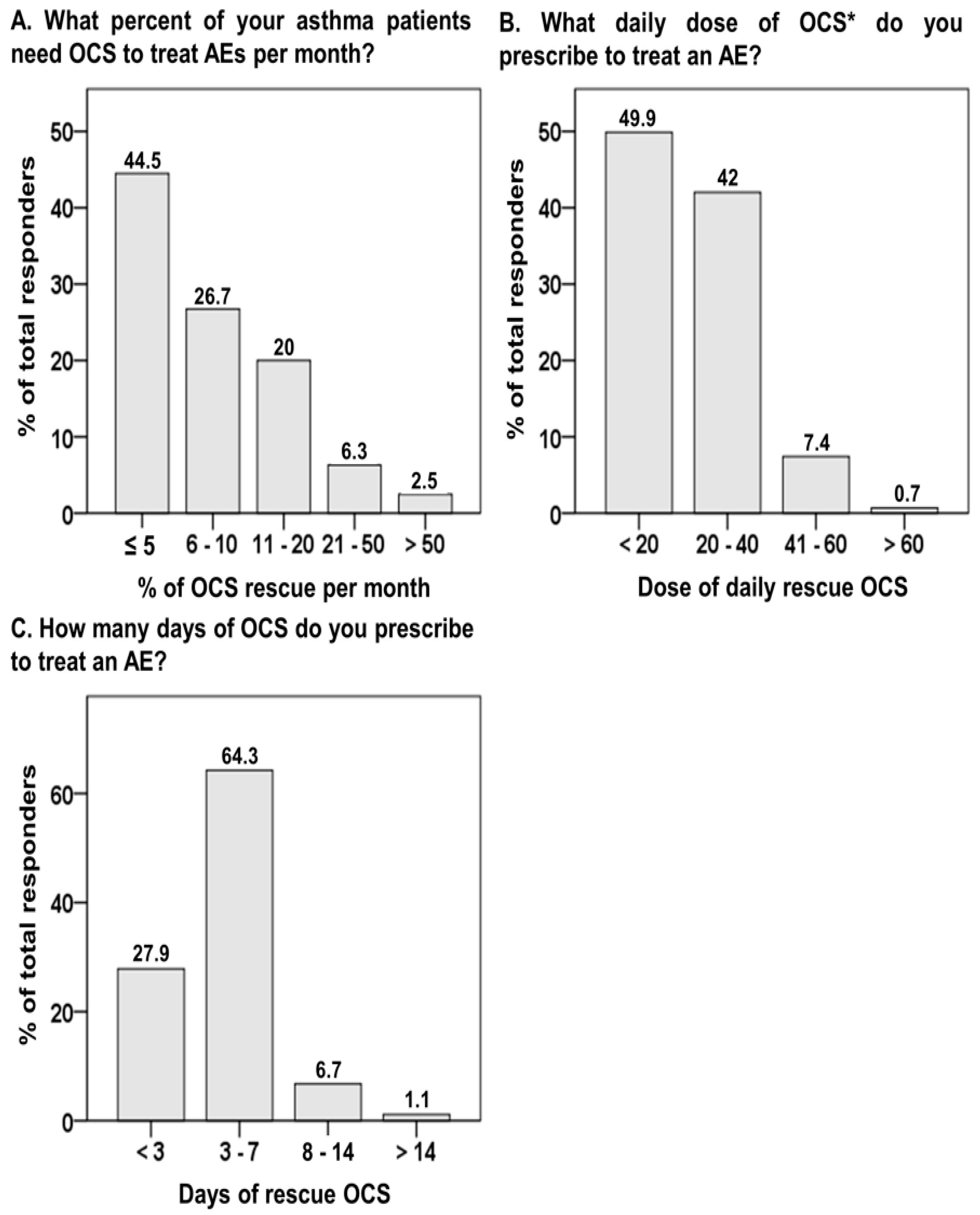
3.2. Oral Corticosteroid for Acute Exacerbation
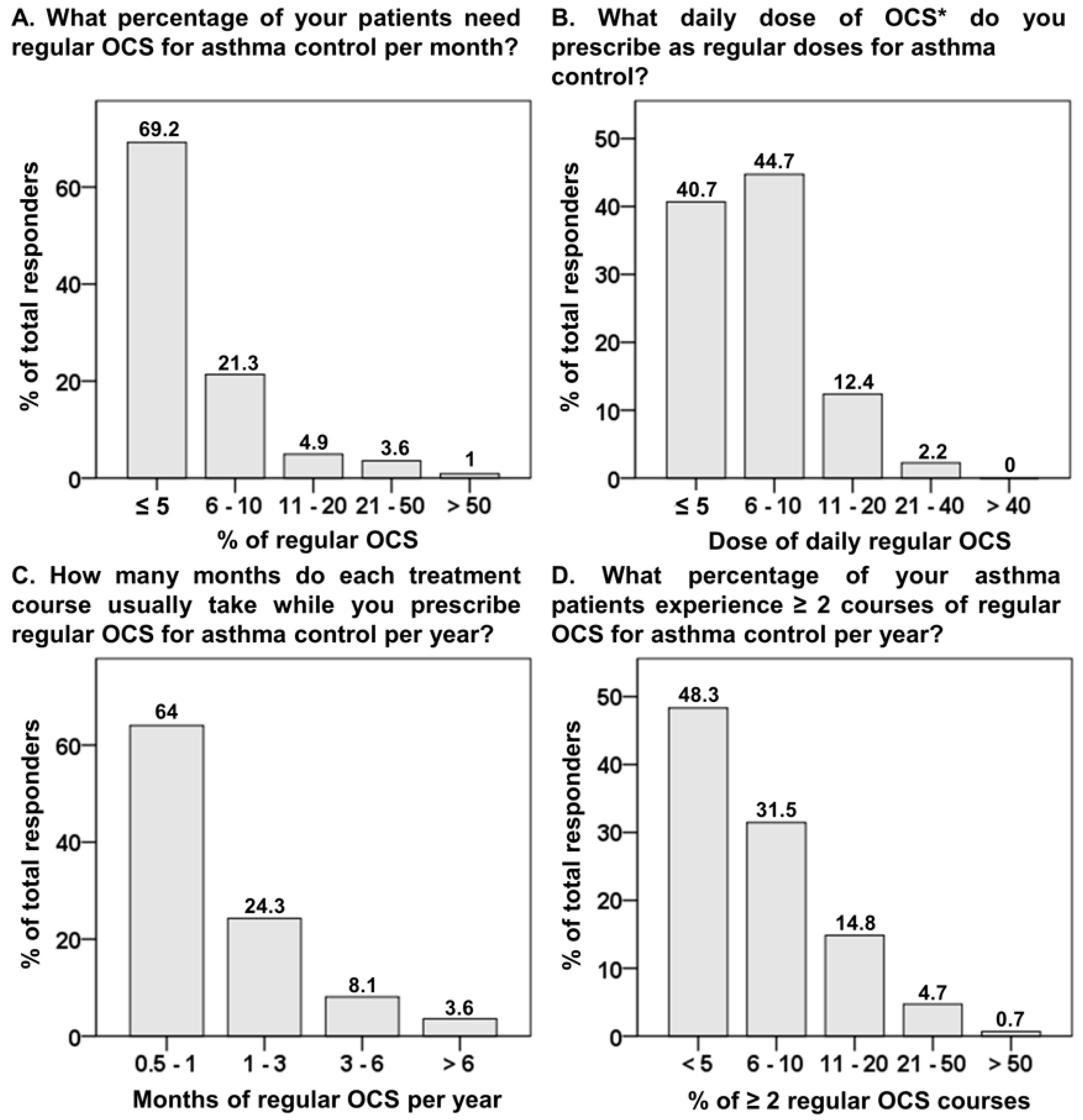
3.3. Regular Oral Corticosteroid for Asthma Control
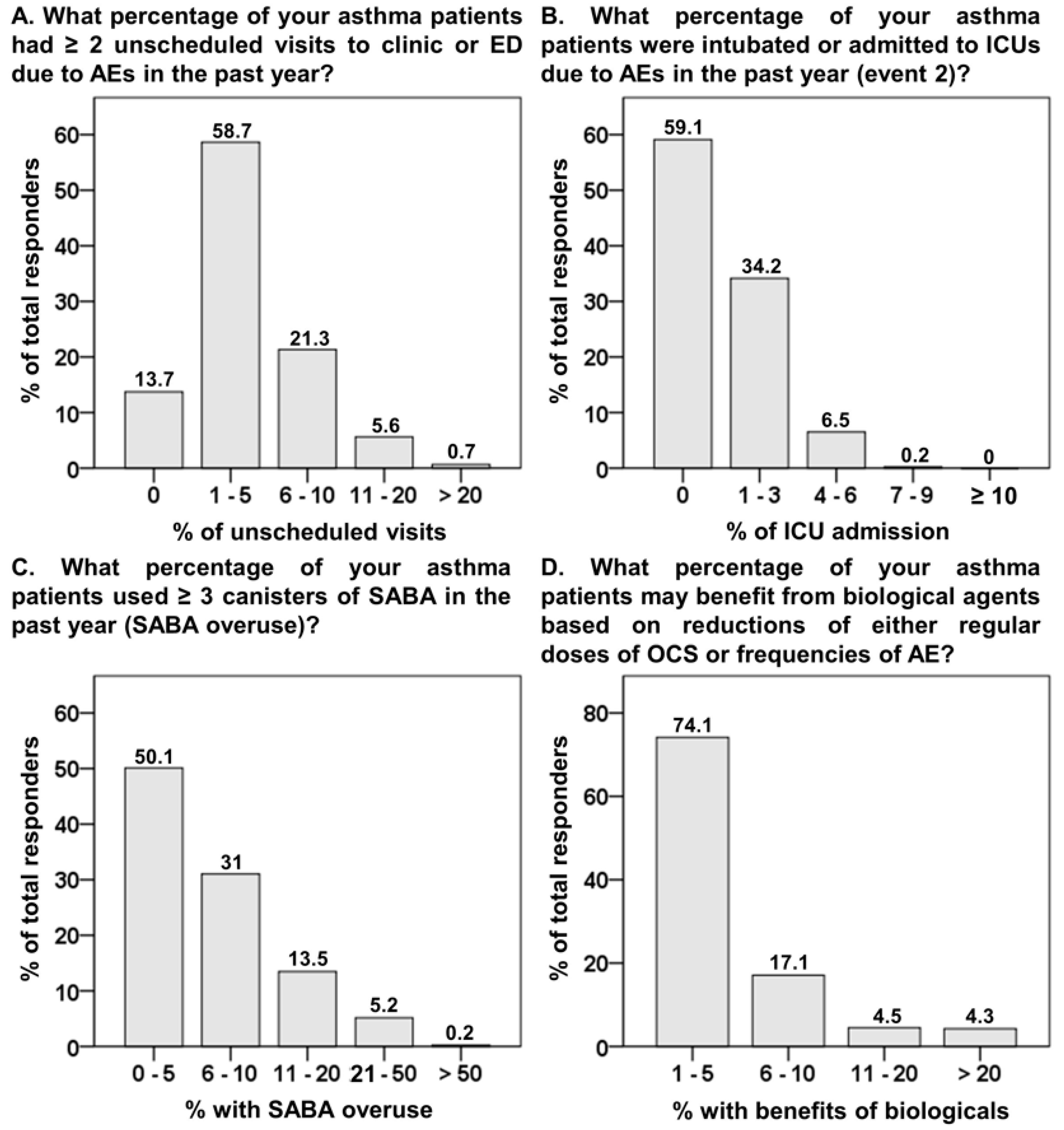
3.4. Asthma Control Status
3.5. Differential Concepts between Pulmonologists and Non-Pulmonologists
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Diseases, G.B.D.; Injuries, C. Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1204–1222. [Google Scholar]
- Ivanova, J.I.; Bergman, R.; Birnbaum, H.G.; Colice, G.L.; Silverman, R.A.; McLaurin, K. Effect of asthma exacerbations on health care costs among asthmatic patients with moderate and severe persistent asthma. J. Allergy Clin. Immunol. 2012, 129, 1229–1235. [Google Scholar] [CrossRef] [PubMed]
- Global Initiative for Asthma (GINA). Global Strategy for Asthma Management and Prevention. Updated 2019. Available online: https://ginasthma.org/wp-content/uploads/2019/06/GINA-2019-main-report-June-2019-wms.pdf (accessed on 1 June 2019).
- Sweeney, J.; Patterson, C.C.; Menzies-Gow, A.; Niven, R.M.; Mansur, A.H.; Bucknall, C.; Chaudhuri, R.; Price, D.; Brightling, C.E.; Heaney, L.G.; et al. Comorbidity in severe asthma requiring systemic corticosteroid therapy: Cross-sectional data from the Optimum Patient Care Research Database and the British Thoracic Difficult Asthma Registry. Thorax 2016, 71, 339–346. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chou, C.L.; Perng, D.W.; Lin, T.L.; Lin, A.M.; Chen, T.J.; Wu, M.S.; Chou, Y.C. Analysis of prescription pattern and guideline adherence in the management of asthma among medical institutions and physician specialties in Taiwan between 2000 and 2010. Clin. Ther. 2015, 37, 2275–2285. [Google Scholar] [CrossRef]
- Dalal, A.A.; Duh, M.S.; Gozalo, L.; Robitaille, M.N.; Albers, F.; Yancey, S.; Ortega, H.; Forshag, M.; Lin, X.; Lefebvre, P. Dose-Response Relationship Between Long-Term Systemic Corticosteroid Use and Related Complications in Patients with Severe Asthma. J. Manag. Care Spec. Pharm. 2016, 22, 833–847. [Google Scholar] [CrossRef] [PubMed]
- Volmer, T.; Effenberger, T.; Trautner, C.; Buhl, R. Consequences of long-term oral corticosteroid therapy and its side-effects in severe asthma in adults: A focused review of the impact data in the literature. Eur. Respir. J. 2018, 52, 1800703. [Google Scholar] [CrossRef] [PubMed]
- Chang, Y.L.; Ko, H.K.; Lu, M.S.; Chou, C.L.; Su, K.C.; Hsu, C.C.; Chou, K.T.; Chen, T.J.; Perng, D.W.; Chou, Y.C. Independent risk factors for death in patients admitted for asthma exacerbation in Taiwan. NPJ Prim. Care Respir. Med. 2020, 30, 7. [Google Scholar] [CrossRef] [Green Version]
- Yang, J.F.; Chaudhuri, R.; Thomson, N.C.; Ramparsad, N.; O’Pray, H.; Barclay, S.; MacBride-Stewart, S.; McCallum, C.; Sharma, V.; McSharry, C.; et al. Insights into frequent asthma exacerbations from a primary care perspective and the implications of UK National Review of Asthma Deaths recommendations. NPJ Prim. Care Respir. Med. 2018, 28, 35. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McGregor, M.C.; Krings, J.G.; Nair, P.; Castro, M. Role of Biologics in Asthma. Am. J. Respir. Crit. Care Med. 2019, 199, 433–445. [Google Scholar] [CrossRef] [PubMed]
- Chung, L.P.; Upham, J.W.; Bardin, P.G.; Hew, M. Rational oral corticosteroid use in adult severe asthma: A narrative review. Respirology 2020, 25, 161–172. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Menzies-Gow, A.; Canonica, G.W.; Winders, T.A.; Correia de Sousa, J.; Upham, J.W.; Fink-Wagner, A.H. A Charter to Improve Patient Care in Severe Asthma. Adv. Ther. 2018, 35, 1485–1496. [Google Scholar] [CrossRef] [PubMed]
- Nwaru, B.I.; Ekstrom, M.; Hasvold, P.; Wiklund, F.; Telg, G.; Janson, C. Overuse of short-acting beta2-agonists in asthma is associated with increased risk of exacerbation and mortality: A nationwide cohort study of the global SABINA programme. Eur. Respir. J. 2020, 55, 1901872. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mazurek, J.M.; Syamlal, G. Prevalence of Asthma, Asthma Attacks, and Emergency Department Visits for Asthma Among Working Adults—National Health Interview Survey, 2011–2016. Morb. Mortal. Wkly. Rep. 2018, 67, 377–386. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pendergraft, T.B.; Stanford, R.H.; Beasley, R.; Stempel, D.A.; Roberts, C.; McLaughlin, T. Rates and characteristics of intensive care unit admissions and intubations among asthma-related hospitalizations. Ann. Allergy Asthma Immunol. 2004, 93, 29–35. [Google Scholar] [CrossRef] [PubMed]
- Choi, K.; Han, S.; Suh, H.S. Emergency department visits and hospitalisations for emergent asthmatic symptoms from 2014 to 2016: Cross-sectional study in Korea. BMJ Open 2020, 10, e036237. [Google Scholar] [CrossRef] [PubMed]
- Nanchal, R.; Kumar, G.; Majumdar, T.; Taneja, A.; Patel, J.; Dagar, G.; Jacobs, E.R.; Whittle, J. Utilization of mechanical ventilation for asthma exacerbations: Analysis of a national database. Respir. Care 2014, 59, 644–653. [Google Scholar] [CrossRef] [Green Version]
- Pauwels, R.A.; Löfdahl, C.G.; Postma, D.S.; Tattersfield, A.E.; O’Byrne, P.; Barnes, P.J.; Ullman, A. Effect of inhaled formoterol and budesonide on exacerbations of asthma. Formoterol and Corticosteroids Establishing Therapy (FACET) International Study Group. N. Engl. J. Med. 1997, 337, 1405–1411. [Google Scholar] [CrossRef]
- Tattersfield, A.E.; Postma, D.S.; Barnes, P.J.; Svensson, K.; Bauer, C.A.; O’Byrne, P.M.; Löfdahl, C.G.; Pauwels, R.A.; Ullman, A. Exacerbations of asthma: A descriptive study of 425 severe exacerbations. The FACET International Study Group. Am. J. Respir. Crit. Care Med. 1999, 160, 594–599. [Google Scholar] [CrossRef]
- de Roos, E.W.; Lahousse, L.; Verhamme, K.M.C.; Braunstahl, G.J.; In’t Veen, J.; Stricker, B.H.; Brusselle, G.G.O. Incidence and predictors of asthma exacerbations in middle-aged and older adults: The Rotterdam Study. ERJ Open Res. 2021, 7, 00126. [Google Scholar] [CrossRef] [PubMed]
- Suehs, C.M.; Menzies-Gow, A.; Price, D.; Bleecker, E.R.; Canonica, G.W.; Gurnell, M.; Bourdin, A. Expert Consensus on the Tapering of Oral Corticosteroids for the Treatment of Asthma. A Delphi Study. Am. J. Respir. Crit. Care Med. 2021, 203, 871–881. [Google Scholar] [CrossRef] [PubMed]
- McDonald, V.M.; Hiles, S.A.; Godbout, K.; Harvey, E.S.; Marks, G.B.; Hew, M.; Peters, M.; Bardin, P.G.; Reynolds, P.N.; Upham, J.W.; et al. Treatable traits can be identified in a severe asthma registry and predict future exacerbations. Respirology 2019, 24, 37–47. [Google Scholar] [CrossRef] [PubMed]
- Chung, K.F.; Wenzel, S.E.; Brozek, J.L.; Bush, A.; Castro, M.; Sterk, P.J.; Adcock, I.M.; Bateman, E.D.; Bel, E.H.; Bleecker, E.R.; et al. International ERS/ATS guidelines on definition, evaluation and treatment of severe asthma. Eur. Respir. J. 2014, 43, 343–373. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hyland, M.E.; Whalley, B.; Jones, R.C.; Masoli, M. A qualitative study of the impact of severe asthma and its treatment showing that treatment burden is neglected in existing asthma assessment scales. Qual. Life Res. 2015, 24, 631–639. [Google Scholar] [CrossRef] [PubMed]
- Blaiss, M.S. The Management of Severe Asthma: Economic Analysis of the Cost of Treatments for Severe Asthma. Available online: https://www.worldallergy.org/educational_programs/world_allergy_forum/anaheim2005/blaiss.php (accessed on 1 June 2019).
- Chen, H.; Johnson, C.A.; Haselkorn, T.; Lee, J.H.; Israel, E. Subspecialty differences in asthma characteristics and management. Mayo Clin. Proc. 2008, 83, 786–793. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Eisner, M.D.; Katz, P.P.; Yelin, E.H.; Henke, J.; Smith, S.; Blanc, P.D. Assessment of asthma severity in adults with asthma treated by family practitioners, allergists, and pulmonologists. Med. Care 1998, 36, 1567–1577. [Google Scholar] [CrossRef]
- Nyenhuis, S.M.; Akkoyun, E.; Liu, L.; Schatz, M.; Casale, T.B. Real-World Assessment of Asthma Control and Severity in Children, Adolescents, and Adults with Asthma: Relationships to Care Settings and Comorbidities. J. Allergy Clin. Immunol. Pract. 2020, 8, 989–996.e1. [Google Scholar] [CrossRef]
- Wu, T.Y.; Majeed, A.; Kuo, K.N. An overview of the healthcare system in Taiwan. Lond. J. Prim. Care 2010, 3, 115–119. [Google Scholar] [CrossRef]
| Healthcare Facility | Medical Specialty | ||||
|---|---|---|---|---|---|
| Pediatrics (n = 79) | ENT (n = 60) | FM (n = 80) | IM (n = 52) | Pulmonology (n = 174) | |
| Doctor’s office (n = 286) | 78 | 59 | 73 | 48 | 28 |
| Community hospital (n = 159) | 1 | 1 | 7 | 4 | 146 |
| Do you Think Which Factors Contribute to Regular Use of OCS for Asthma Control? (Multiple Choices Allowed) | Total (n = 445) | Non-Pulmonologist (n = 271) | Pulmonologist (n = 174) |
|---|---|---|---|
| Disease entity of asthma | 183 (41.1) | 87 (32.1) | 96 (55.2) * |
| Non-adherence or misuse of inhaler | 152 (34.2) | 117 (43.2) | 35 (20.1) * |
| Exposure of allergens/air pollution | 77 (17.3) | 42 (15.5) | 35 (20.1) |
| Comorbidity | 57 (12.8) | 33 (12.2) | 24 (13.8) |
| Questions | Cut-Off Value | Non-Pulmonologist (n = 271) | Pulmonologist (n = 174) | p * |
|---|---|---|---|---|
| Section 1. Oral corticosteroid (OCS) for acute exacerbation (AE) | ||||
| How many percent of your asthma patients need OCS to treat AEs per month? | ≥6 % | 153 (56.5) | 94 (54) | 0.342 |
| What daily dose of OCS (prednisolone or equivalent in mg) do you prescribe to treat an AE? | ≥20 mg | 121 (44.6) | 102 (58.6) | 0.005 |
| How many days of OCS do you prescribe to treat an AE? | ≥3 days | 162 (59.8) | 159 (91.4) | <0.001 |
| Section 2. Regular corticosteroid (OCS) for asthma control | ||||
| How many percent of your patients need regular OCS for asthma control per month? | ≥6 % | 79 (29.2) | 58 (33.3) | 0.4 |
| What daily dose of OCS (prednisolone or equivalent in mg) do you prescribe as regular doses for asthma control? | ≥6 mg | 147 (54.2) | 117 (67.2) | 0.008 |
| How many months do each treatment course usually take while you prescribe regular OCS for asthma control per year? | ≥1 month | 80 (29.5) | 80 (46) | 0.001 |
| How many percent of your asthma patients experience ≥2 courses of regular OCS for asthma control per year? | ≥6 % | 133 (49.1) | 97 (55.7) | 0.175 |
| Section 3: Asthma control status | ||||
| How many percent of your asthma patients had ≥2 unscheduled visits to clinic or emergent department due to AEs in the past year? | ≥1 % | 221 (81.5) | 163 (93.7) | <0.001 |
| How many percent of your asthma patients were intubated or admitted to intensive care units due to AEs in the past year? | ≥1 % | 76 (28) | 106 (61) | <0.001 |
| How many percent of your asthma patients used ≥3 canisters of short-acting β2 agonists (SABA) in the past year? | ≥6 % | 113 (41.7) | 109 (62.6) | <0.001 |
| How many percent of your asthma patients may benefit from biological agents based on reductions of either regular doses of OCS or frequencies of AE? | ≥6 % | 55 (20.3) | 60 (34.5) | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, Y.-W.; Hsiao, Y.-H.; Ko, H.-K.; Jeng, T.-H.; Su, K.-C.; Perng, D.-W. Unmet Need for Oral Corticosteroids Use and Exacerbations of Asthma in Primary Care in Taiwan. Biomedicines 2022, 10, 3253. https://doi.org/10.3390/biomedicines10123253
Chen Y-W, Hsiao Y-H, Ko H-K, Jeng T-H, Su K-C, Perng D-W. Unmet Need for Oral Corticosteroids Use and Exacerbations of Asthma in Primary Care in Taiwan. Biomedicines. 2022; 10(12):3253. https://doi.org/10.3390/biomedicines10123253
Chicago/Turabian StyleChen, Yen-Wen, Yi-Han Hsiao, Hsin-Kuo Ko, Tien-Hsin Jeng, Kang-Cheng Su, and Diahn-Warng Perng. 2022. "Unmet Need for Oral Corticosteroids Use and Exacerbations of Asthma in Primary Care in Taiwan" Biomedicines 10, no. 12: 3253. https://doi.org/10.3390/biomedicines10123253
APA StyleChen, Y. -W., Hsiao, Y. -H., Ko, H. -K., Jeng, T. -H., Su, K. -C., & Perng, D. -W. (2022). Unmet Need for Oral Corticosteroids Use and Exacerbations of Asthma in Primary Care in Taiwan. Biomedicines, 10(12), 3253. https://doi.org/10.3390/biomedicines10123253






