Inflammation and Barrier Function Deficits in the Bladder Urothelium of Patients with Chronic Spinal Cord Injury and Recurrent Urinary Tract Infections
Abstract
:1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sekhon, L.H.; Fehlings, M.G. Epidemiology, demographics, and pathophysiology of acute spinal cord injury. Spine 2001, 26, S2–S12. [Google Scholar] [CrossRef] [PubMed]
- Consortium for Spinal Cord Medicine. Bladder management for adults with spinal cord injury: A clinical practice guideline for health-care providers. J. Spinal Cord Med. 2006, 29, 527–573. [Google Scholar]
- Eckert, M.J.; Martin, M.J. Trauma: Spinal Cord Injury. Surg. Clin. N. Am. 2017, 97, 1031–1045. [Google Scholar] [CrossRef] [PubMed]
- Ku, J.H. The management of neurogenic bladder and quality of life in spinal cord injury. BJU Int. 2006, 98, 739–745. [Google Scholar] [CrossRef]
- Manack, A.; Motsko, S.P.; Haag-Molkenteller, C.; Dmochowski, R.R.; Goehring Jr, E.L.; Nguyen-Khoa, B.A.; Jones, J.K. Epidemiology and healthcare utilization of neurogenic bladder patients in a US claims database. Neurourol. Urodyn. 2011, 30, 395–401. [Google Scholar] [CrossRef]
- Vizzard, M.A. Neurochemical plasticity and the role of neurotrophic factors in bladder reflex pathways after spinal cord injury. Prog. Brain Res. 2006, 152, 97–115. [Google Scholar]
- Cameron, A.P.; Rodriguez, G.M.; Schomer, K.G. Systematic review of urological followup after spinal cord injury. J. Urol. 2012, 187, 391–397. [Google Scholar] [CrossRef]
- Gormley, E.A. Urologic complications of the neurogenic bladder. Urol. Clin. N. Am. 2010, 37, 601–607. [Google Scholar] [CrossRef] [PubMed]
- Togan, T.; Azap, O.K.; Durukan, E.; Arslan, H. The prevalence, etiologic agents and risk factors for urinary tract infection among spinal cord injury patients. Jundishapur J. Microbiol. 2014, 7, e8905. [Google Scholar] [CrossRef] [Green Version]
- De Ruz, A.E.; Leoni, E.G.; Cabrera, R.H. Epidemiology and risk factors for urinary tract infection in patients with spinal cord injury. J. Urol. 2000, 164, 1285–1289. [Google Scholar] [CrossRef]
- Bonkat, G.; Bartoletti, R.; Bruyère, F.; Cai, T.; Geerlings, S.E.; Köves, B.; Schubert, S.; Wagenlehner, F. Guidelines Associates: Devlies, W.; Horváth, J.; Mantica, G.; Mezei, T.; Pilatz, A.; Pradere, B.; Veeratterapillay, R. Urological Infections. EAU Guidelines. In Proceedings of the EAU Annual Congress, Milan, Italy, 2021; ISBN 978-94-92671-13-4. Available online: https://uroweb.org/guideline/urological-infections/ (accessed on 15 December 2021).
- Chaudhry, R.; Madden-Fuentes, R.J.; Ortiz, T.K.; Balsara, Z.; Tang, Y.; Nseyo, U.; Wiener, J.S.; Ross, S.S.; Seed, P.C. Inflammatory response to Escherichia coli urinary tract infection in the neurogenic bladder of the spinal cord injured host. J. Urol. 2014, 191, 1454–1461. [Google Scholar] [CrossRef] [PubMed]
- Birder, L.A. Role of the urothelium in urinary bladder dysfunction following spinal cord injury. Prog. Brain Res. 2006, 152, 135–146. [Google Scholar] [PubMed]
- Birder, L.A.; Groat, W.C. Mechanisms of disease: Involvement of the urothelium in bladder dysfunction. Nat. Clin. Pract. Urol. 2007, 4, 46–54. [Google Scholar] [CrossRef] [Green Version]
- Birder, L.A.; Andersson, K.E. Urothelial signaling. Physiol. Rev. 2013, 93, 653–680. [Google Scholar] [CrossRef] [Green Version]
- Birder, L.A. Role of the urothelium in bladder function. Scand. J. Urol. Nephrol. Suppl. 2004, 215, 48–53. [Google Scholar] [CrossRef] [PubMed]
- Shie, J.H.; Kuo, H.C. Higher levels of cell apoptosis and abnormal E-cadherin expression in the urothelium are associated with inflammation in patients with interstitial cystitis/painful bladder syndrome. BJU Int. 2011, 108, E136–E141. [Google Scholar] [CrossRef]
- Chuang, F.C.; Kuo, H.C. Increased urothelial cell apoptosis and chronic inflammation are associated with recurrent urinary tract infection in women. PLoS ONE 2013, 8, e63760. [Google Scholar] [CrossRef] [Green Version]
- Krebs, J.; Wöllner, J.; Pannek, J. Risk factors for symptomatic urinary tract infections in individuals with chronic neurogenic lower urinary tract dysfunction. Spinal Cord 2016, 54, 682–686. [Google Scholar] [CrossRef]
- Linsenmeyer, T.A. Catheter-associated urinary tract infections in persons with neurogenic bladders. J. Spinal Cord Med. 2018, 41, 132–141. [Google Scholar] [CrossRef]
- Mysorekar, I.U.; Hultgren, S.J. Mechanisms of uropathogenic Escherichia coli persistence and eradication from the urinary tract. Proc. Natl. Acad. Sci. USA 2006, 103, 14170–14175. [Google Scholar] [CrossRef] [Green Version]
- Shin, K.; Lee, J.; Guo, N.; Kim, J.; Lim, A.; Qu, L.; Mysorekar, I.U.; Beachy, P.A. Hedgehog/Wnt feedback supports regenerative proliferation of epithelial stem cells in bladder. Nature 2011, 472, 110–114. [Google Scholar] [CrossRef] [Green Version]
- Acharya, P.; Beckel, J.; Ruiz, W.G.; Wang, E.; Rojas, R.; Birder, L.A.; Apodaca, G. Distribution of the tight junction proteins ZO-1, occludin, and claudin-4, -8, and -12 in bladder epithelium. Am. J. Physiol. Ren. Physiol. 2004, 287, F305–F318. [Google Scholar] [CrossRef]
- Hu, P.; Meyers, S.; Liang, F.X.; Deng, F.M.; Kachar, B.; Zeidel, M.L.; Sun, T.T. Role of membrane proteins in permeability barrier function: Uroplakin ablation elevates urothelial permeability. Am. J. Physiol. Ren. Physiol. 2002, 283, F1200–F1207. [Google Scholar] [CrossRef] [Green Version]
- Wu, X.R.; Kong, X.P.; Pellicer, A.; Kreibich, G.; Sun, T.T. Uroplakins in urothelial biology, function, and disease. Kidney Int. 2009, 75, 1153–1165. [Google Scholar] [CrossRef] [Green Version]
- Zwaans, B.M.M.; Carabulea, A.L.; Bartolone, S.N.; Ward, E.P.; Chancellor, M.B.; Lamb, L.E. Voiding defects in acute radiation cystitis driven by urothelial barrier defect through loss of E-cadherin, ZO-1 and Uroplakin III. Sci. Rep. 2021, 11, 19277. [Google Scholar] [CrossRef] [PubMed]
- Apodaca, G.; Kiss, S.; Ruiz, W.; Meyers, S.; Zeidel, M.; Birder, L.A. Disruption of bladder epithelium barrier function after spinal cord injury. Am. J. Physiol. Ren. Physiol. 2003, 284, F966–F976. [Google Scholar] [CrossRef]
- Homma, Y.; Ueda, T.; Tomoe, H.; Lin, A.T.L.; Kuo, H.C.; Lee, M.H.; Lee, J.G.; Kim, D.Y.; Lee, K.S. Interstitial cystitis guideline committee. Clinical guidelines for interstitial cystitis and hypersensitive bladder syndrome. Int. J. Urol. 2009, 16, 597–615. [Google Scholar] [CrossRef] [PubMed]
- Kullmann, A.F.; Truschel, S.T.; Wolf-Johnston, A.S.; McDonnell, B.M.; Lynn, A.M.; Kanai, A.J.; Kessler, T.M.; Apodaca, G.; Birder, L.A. Acute spinal cord injury is associated with mitochondrial dysfunction in mouse urothelium. Neurourol. Urodyn. 2019, 38, 1551–1559. [Google Scholar] [CrossRef]
- Norbury, C.J.; Hickson, I.D. Cellular responses to DNA damage. Annu. Rev. Pharmacol. Toxicol. 2001, 41, 367–401. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jiang, Y.H.; Liu, H.T.; Kuo, H.C. Urothelial dysfunction and chronic inflammation in patients with spinal cord injuries at different levels and correlation with urodynamic findings. Neurourol. Urodyn. 2015, 34, 757–762. [Google Scholar] [CrossRef]
- Chen, M.C.; Blunt, L.W.; Pins, M.R.; Klumpp, D.J. Tumor necrosis factor promotes differential trafficking of bladder mast cells in neurogenic cystitis. J. Urol. 2006, 175, 754–759. [Google Scholar] [CrossRef]
- Chen, M.C.; Mudge, C.S.; Klumpp, D.J. Urothelial lesion formation is mediated by TNFR1 during neurogenic cystitis. Am. J. Physiol. Ren. Physiol. 2006, 291, F741–F749. [Google Scholar] [CrossRef]
- Wang, W.; Wang, X.; Chun, J.; Vilaysane, A.; Clark, S.; French, G.; Bracey, N.A.; Trpkov, K.; Bonni, S.; Duff, H.J.; et al. Inflammasome-independent NLRP3 augments TGF-β signaling in kidney epithelium. J. Immunol. 2013, 190, 1239–1249. [Google Scholar] [CrossRef] [Green Version]
- Hughes, J.F.M.; Sexton, S.J.; Jin, H.; Govada, V.; Purves, J.T. Bladder fibrosis during outlet obstruction is triggered through the NLRP3 inflammasome and the production of IL-1β. Am. J. Physiol. Ren. Physiol. 2017, 313, F603–F610. [Google Scholar] [CrossRef] [Green Version]
- Wu, Z.; Li, Y.; Liu, Q.; Liu, Y.; Chen, L.; Zhao, H.; Guo, H.; Zhu, K.; Zhou, N.; Chai, T.C.; et al. Pyroptosis engagement and bladder urothelial cell-derived exosomes recruit mast cells and induce barrier dysfunction of bladder urothelium after uropathogenic E. coli infection. Am. J. Physiol. Cell Physiol. 2019, 317, C544–C555. [Google Scholar] [CrossRef] [PubMed]
- Akiyama, Y.; Maeda, D.; Morikawa, T.; Niimi, A.; Nomiya, A.; Yamada, Y.; Igawa, Y.; Goto, A.; Fukayama, M.; Homma, Y. Digital quantitative analysis of mast cell infiltration in interstitial cystitis. Neurourol. Urodyn. 2018, 37, 650–657. [Google Scholar] [CrossRef] [Green Version]
- Jhang, J.F.; Lin, T.Y.; Ho, H.C.; Jiang, Y.H.; Hsu, Y.H.; Birder, L.A.; Kuo, H.C. Deficits of urothelial cell proliferation, cytoskeleton, and barrier function protein expressions in patients with recurrent and persistent urinary tract infections. Low. Urin. Tract Symptoms. 2021, 13, 203–209. [Google Scholar] [CrossRef]
- Kullmann, F.A.; Clayton, D.R.; Ruiz, W.G.; Wolf-Johnston, A.; Gauthier, C.; Kanai, A.; Birder, L.A.; Apodaca, G. Urothelial proliferation and regeneration after spinal cord injury. Am. J. Physiol. Ren. Physiol. 2017, 313, F85–F102. [Google Scholar] [CrossRef]
- Wojdasiewicz, P.; Poniatowski, Ł.A.; Turczyn, P.; Frasuńska, J.; Paradowska-Gorycka, A.; Tarnacka, B. Significance of Omega-3 Fatty Acids in the Prophylaxis and Treatment after Spinal Cord Injury in Rodent Models. Mediators Inflamm. 2020, 29, 3164260. [Google Scholar] [CrossRef]
- Jia, C.; Liao, L.M.; Chen, G.; Sui, Y. Detrusor botulinum toxin A injection significantly decreased urinary tract infection in patients with traumatic spinal cord injury. Spinal Cord 2013, 51, 487–490. [Google Scholar] [CrossRef] [PubMed] [Green Version]



| Antibodies | Company | Catalog Number | Dilution | KDa |
|---|---|---|---|---|
| E-cadherin | BD Biosciences | BD610181 | 1:5000 | 120 |
| ZO-1 | Genetex | GTX108627 | 1:500 | 190 |
| UPK3 | Abcam | ab157801 | 1:500 | 32 |
| CK20 | Abcam | ab76126 | 1:2500 | 48 |
| CK14 | Abcam | ab9220 | 1:1000 | 58 |
| CK5 | Abcam | ab52635 | 1:1000 | 62 |
| TP63 | Abcam | ab53039 | 1:1000 | 77 |
| CD34 | Abcam | ab81289 | 1:10,000 | 120 |
| SHH | Abcam | ab53281 | 1:1000 | 51 |
| Ki-67 | Abcam | ab16667 | 1:1000 | 358 |
| BAX | Cell Signaling Technology | CST2772S | 1:500 | 20.5 |
| BCL-2 | Cell Signaling Technology | CST15071 | 1:1000 | 26 |
| P53 | Abcam | ab131442 | 1:1000 | 53 |
| Tryptase | Merck | mab1222 | 1:1000 | 31 |
| TNF-α | Cell Signaling Technology | CST3707S | 1:500 | 17/25 |
| TGF-β | Cell Signaling Technology | CST56E4 | 1:500 | 55 |
| GAPDH | Genetex | GTX100118 | 1:10,000 | 37 |
| VUDS | SCI | Total (N = 23) | Control (N = 6) | p-Value # | p-Value * | p-Value ** | |
|---|---|---|---|---|---|---|---|
| rUTI (N = 8) | Non-rUTI (N = 15) | ||||||
| Pdet | 44.63 ± 35.60 | 27.93 ± 10.18 | 33.74 ± 23.14 | 15.00 ± 2.83 | 0.232 | 0.131 | 0.273 |
| Qmax | 4.75 ± 5.39 | 5.40 ± 6.19 | 5.17 ± 5.8 | 19.67 ± 14.84 | 0.805 | 0.245 | 0.231 |
| Volume | 98.25 ± 127.25 | 69.93 ± 95.39 | 79.78 ± 105.51 | 317.00 ± 124.47 | 0.552 | 0.006 | 0.001 |
| PVR | 197.50 ± 165.34 | 185.33 ± 118.98 | 189.57 ± 133.19 | 35.00 ± 60.62 | 0.840 | 0.178 | 0.062 |
| FSF | 123.88 ± 91.83 | 127.73 ± 87.12 | 126.39 ± 86.7 | 144.33 ± 75.08 | 0.922 | 0.941 | 0.736 |
| FS | 170.00 ± 147.44 | 173.27 ± 106.21 | 172.13 ± 118.73 | 201.67 ± 87.15 | 0.952 | 0.920 | 0.683 |
| Compliance | 29.71 ± 31.44 | 34.65 ± 39.47 | 32.93 ± 36.21 | 89.40 ± 50.74 | 0.763 | 0.074 | 0.022 |
| BCI | 68.38 ± 52.85 | 54.93 ± 36.23 | 59.61 ± 42.03 | 145.00 ± 73.54 | 0.478 | 0.043 | 0.015 |
| CBC | 295.75 ± 232.76 | 255.27 ± 123.00 | 269.35 ± 165.09 | 352.00 ± 71.39 | 0.587 | 0.607 | 0.407 |
| VE | 0.31 ± 0.30 | 0.26 ± 0.26 | 0.28 ± 0.27 | 0.88 ± 0.21 | 0.681 | 0.005 | 0.001 |
| SCI Total (N = 23) | SCI, rUTI (N = 8) | SCI, Non-rUTI (N = 15) | Control (N = 6) | p-Value * | p-Value # | |
|---|---|---|---|---|---|---|
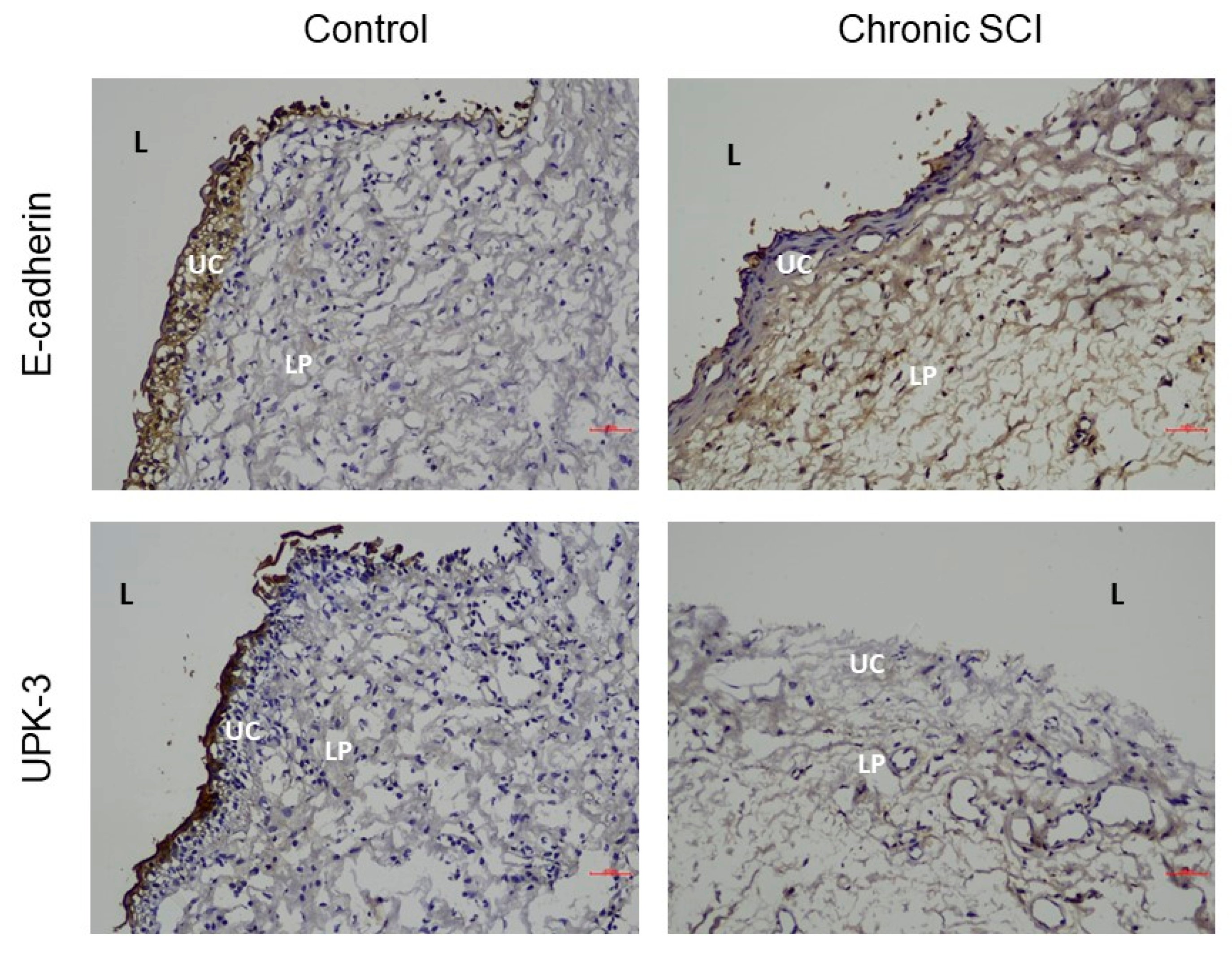
| E-cadherin | 0.45 ± 0.40 | 0.33 ± 0.39 | 0.32 ± 0.28 | 0.96 ± 0.31 | 0.000 | 0.001 |
| ZO-1 | 0.42 ± 0.39 | 0.36 ± 0.40 | 0.32 ± 0.36 | 0.73 ± 0.38 | 0.027 | 0.089 |
| UPK3 | 0.42 ± 0.39 | 0.28 ± 0.22 | 0.27 ± 0.23 | 0.97 ± 0.41 | 0.000 | 0.000 |
| CK20 | 0.34 ± 0.22 | 0.38 ± 0.30 | 0.34 ± 0.19 | 0.28 ± 0.21 | 0.448 | 0.697 |
| CK14 | 0.67 ± 0.32 | 0.77 ± 0.37 | 0.60 ± 0.34 | 0.74 ± 0.13 | 0.408 | 0.420 |
| CK5 | 0.27 ± 0.25 | 0.36 ± 0.35 | 0.22 ± 0.14 | 0.26 ± 0.35 | 0.934 | 0.614 |
| TP63 | 0.79 ± 0.50 | 0.86 ± 0.47 | 0.89 ± 0.56 | 0.43 ± 0.19 | 0.049 | 0.148 |
| CD34 | 0.48 ± 0.35 | 0.40 ± 0.36 | 0.54 ± 0.39 | 0.44 ± 0.24 | 0.791 | 0.663 |
| Shh | 0.57 ± 0.22 | 0.58 ± 0.27 | 0.54 ± 0.21 | 0.63 ± 0.23 | 0.485 | 0.721 |
| Ki-67 | 0.10 ± 0.10 | 0.11 ± 0.11 | 0.12 ± 0.11 | 0.04 ± 0.04 | 0.011 | 0.254 |
| BAX | 0.34 ± 0.27 | 0.35 ± 0.25 | 0.45 ± 0.27 | 0.06 ± 0.03 | 0.000 | 0.004 |
| BCL-2 | 0.56 ± 0.46 | 0.48 ± 0.39 | 0.64 ± 0.56 | 0.45 ± 0.21 | 0.537 | 0.628 |
| P53 | 0.41 ± 0.27 | 0.43 ± 0.23 | 0.48 ± 0.30 | 0.23 ± 0.18 | 0.062 | 0.166 |
| Tryptase | 0.78 ± 0.69 | 1.15 ± 0.80 | 0.72 ± 0.69 | 0.44 ± 0.24 | 0.026 | 0.115 |
| TNF-α | 0.34 ± 0.22 | 0.40 ± 0.19 | 0.39 ± 0.19 | 0.14 ± 0.25 | 0.009 | 0.034 |
| TGF-β | 0.85 ± 0.44 | 0.97 ± 0.39 | 0.94 ± 0.32 | 0.43 ± 0.54 | 0.006 | 0.026 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wu, S.-Y.; Jiang, Y.-H.; Jhang, J.-F.; Hsu, Y.-H.; Ho, H.-C.; Kuo, H.-C. Inflammation and Barrier Function Deficits in the Bladder Urothelium of Patients with Chronic Spinal Cord Injury and Recurrent Urinary Tract Infections. Biomedicines 2022, 10, 220. https://doi.org/10.3390/biomedicines10020220
Wu S-Y, Jiang Y-H, Jhang J-F, Hsu Y-H, Ho H-C, Kuo H-C. Inflammation and Barrier Function Deficits in the Bladder Urothelium of Patients with Chronic Spinal Cord Injury and Recurrent Urinary Tract Infections. Biomedicines. 2022; 10(2):220. https://doi.org/10.3390/biomedicines10020220
Chicago/Turabian StyleWu, Shu-Yu, Yuan-Hong Jiang, Jia-Fong Jhang, Yung-Hsiang Hsu, Han-Chen Ho, and Hann-Chorng Kuo. 2022. "Inflammation and Barrier Function Deficits in the Bladder Urothelium of Patients with Chronic Spinal Cord Injury and Recurrent Urinary Tract Infections" Biomedicines 10, no. 2: 220. https://doi.org/10.3390/biomedicines10020220
APA StyleWu, S.-Y., Jiang, Y.-H., Jhang, J.-F., Hsu, Y.-H., Ho, H.-C., & Kuo, H.-C. (2022). Inflammation and Barrier Function Deficits in the Bladder Urothelium of Patients with Chronic Spinal Cord Injury and Recurrent Urinary Tract Infections. Biomedicines, 10(2), 220. https://doi.org/10.3390/biomedicines10020220







