Female Reproductive Factors and the Risk of Bronchiectasis: A Nationwide Population-Based Longitudinal Study
Abstract
:1. Introduction
2. Materials and Methods
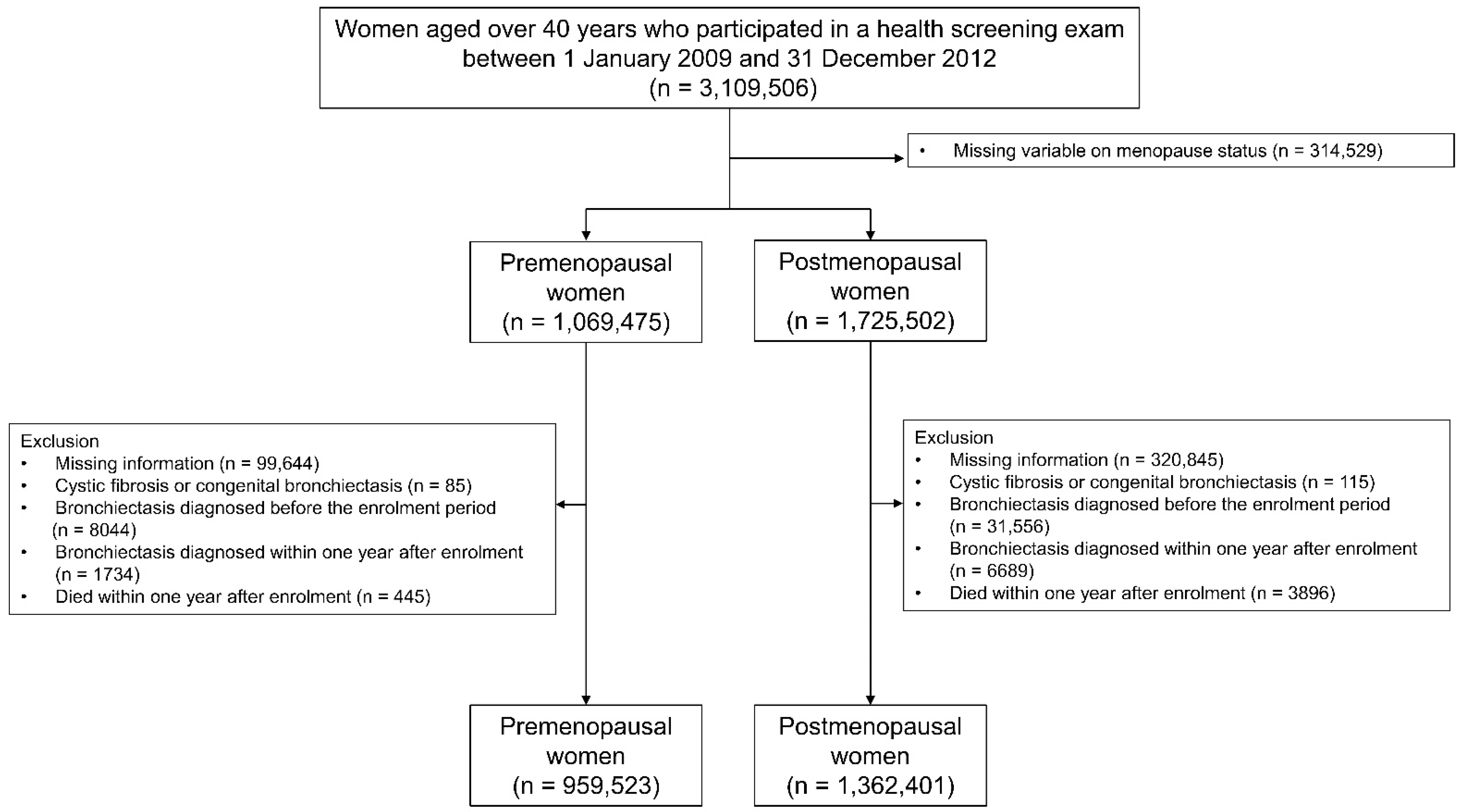
2.1. Study Population and Design
2.2. Exposure
2.3. Outcome
2.4. Covariates
2.5. Statistical Analysis
3. Results
3.1. Baseline Characteristics
3.2. Reproductive Factors and the Risk of Bronchiectasis in Premenopausal Women
3.3. Reproductive Factors and the Risk of Bronchiectasis in Postmenopausal Women
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Leynaert, B.; Sunyer, J.; Garcia-Esteban, R.; Svanes, C.; Jarvis, D.; Cerveri, I.; Dratva, J.; Gislason, T.; Heinrich, J.; Janson, C.; et al. Gender differences in prevalence, diagnosis and incidence of allergic and non-allergic asthma: A population-based cohort. Thorax 2012, 67, 625–631. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Raghavan, D.; Jain, R. Increasing awareness of sex differences in airway diseases. Respirology 2016, 21, 449–459. [Google Scholar] [CrossRef] [PubMed]
- Sørheim, I.-C.; Johannessen, A.; Gulsvik, A.; Bakke, P.S.; Silverman, E.K.; DeMeo, D.L. Gender differences in COPD: Are women more susceptible to smoking effects than men? Thorax 2010, 65, 480–485. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vidaillac, C.; Yong, V.F.L.; Jaggi, T.K.; Soh, M.-M.; Chotirmall, S.H. Gender differences in bronchiectasis: A real issue? Breathe 2018, 14, 108–121. [Google Scholar] [CrossRef]
- Gan, W.Q.; Man, S.F.; Postma, D.S.; Camp, P.; Sin, D.D. Female smokers beyond the perimenopausal period are at increased risk of chronic obstructive pulmonary disease: A systematic review and meta-analysis. Respir. Res. 2006, 7, 52. [Google Scholar] [CrossRef] [Green Version]
- Clougherty, J.E. A growing role for gender analysis in air pollution epidemiology. Environ. Health Perspect. 2010, 118, 167–176. [Google Scholar] [CrossRef] [Green Version]
- Scioscia, G.; Carpagnano, G.E.; Lacedonia, D.; Soccio, P.; Quarato, C.M.I.; Trabace, L.; Fuso, P.; Barbaro, M.P.F. The Role of Airways 17beta-Estradiol as a Biomarker of Severity in Postmenopausal Asthma: A Pilot Study. J. Clin. Med. 2020, 9, 2037. [Google Scholar] [CrossRef]
- Barr, R.G.; Wentowski, C.C.; Grodstein, F.; Somers, S.C.; Stampfer, M.J.; Schwartz, J.; Speizer, F.E.; Camargo, C.A., Jr. Prospective Study of Postmenopausal Hormone Use and Newly Diagnosed Asthma and Chronic Obstructive Pulmonary Disease. Arch. Intern. Med. 2004, 164, 379–386. [Google Scholar] [CrossRef] [Green Version]
- Troisi, R.J.; Speizer, F.E.; Willett, W.C.; Trichopoulos, D.; Rosner, B. Menopause, postmenopausal estrogen preparations, and the risk of adult-onset asthma. A prospective cohort study. Am. J. Respir. Crit. Care Med. 1995, 152, 1183–1188. [Google Scholar] [CrossRef]
- Romieu, I.; Fabre, A.; Fournier, A.; Kauffmann, F.; Varraso, R.; Mesrine, S.; Leynaert, B.; Clavel-Chapelon, F. Postmenopausal hormone therapy and asthma onset in the E3N cohort. Thorax 2010, 65, 292–297. [Google Scholar] [CrossRef] [Green Version]
- Triebner, K.; Johannessen, A.; Puggini, L.; Benediktsdóttir, B.; Bertelsen, R.J.; Bifulco, E.; Dharmage, S.C.; Dratva, J.; Franklin, K.A.; Gíslason, T.; et al. Menopause as a predictor of new-onset asthma: A longitudinal Northern European population study. J. Allergy Clin. Immunol. 2016, 137, 50–57.e6. [Google Scholar] [CrossRef] [PubMed]
- Shah, S.A.; Tibble, H.; Pillinger, R.; McLean, S.; Ryan, D.; Critchley, H.; Price, D.; Hawrylowicz, C.M.; Simpson, C.R.; Soyiri, I.N.; et al. Hormone replacement therapy and asthma onset in menopausal women: National cohort study. J. Allergy Clin. Immunol. 2021, 147, 1662–1670. [Google Scholar] [CrossRef] [PubMed]
- Tang, R.; Fraser, A.; Magnus, M.C. Female reproductive history in relation to chronic obstructive pulmonary disease and lung function in UK biobank: A prospective population-based cohort study. BMJ Open 2019, 9, e030318. [Google Scholar] [CrossRef] [PubMed]
- van der Plaat, D.A.; Pereira, M.; Pesce, G.; Potts, J.F.; Amaral, A.F.S.; Dharmage, S.C.; Garcia-Aymerich, J.M.; Thompson, J.R.; Gómez-Real, F.; Jarvis, D.L.; et al. Age at menopause and lung function: A Mendelian randomisation study. Eur. Respir. J. 2019, 54, 1802421. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.; Choi, H.; Chalmers, J.D.; Dhar, R.; Nguyen, T.Q.; Visser, S.K.; Morgan, L.C.; Oh, Y.-M. Characteristics of bronchiectasis in Korea: First data from the Korean Multicentre Bronchiectasis Audit and Research Collaboration registry and comparison with other international registries. Respirology 2021, 26, 619–621. [Google Scholar] [CrossRef] [PubMed]
- Martinez-García, M.A.; Villa, C.; Dobarganes, Y.; Girón, R.; Maíz, L.; García-Clemente, M.; Sibila, O.; Golpe, R.; Rodríguez, J.; Barreiro, E.; et al. RIBRON: The Spanish online bronchiectasis registry. Characterization of the first 1912 patients. Arch. Bronconeumol. Engl. Ed. 2021, 57, 28–35. [Google Scholar] [CrossRef]
- Snell, N.; Gibson, J.; Jarrold, I.; Quint, J.K. Epidemiology of bronchiectasis in the UK: Findings from the British lung foundation’s ‘Respiratory health of the nation’ project. Respir. Med. 2019, 158, 21–23. [Google Scholar] [CrossRef]
- Huang, H.-Y.; Chung, F.-T.; Lo, C.-Y.; Lin, H.-C.; Huang, Y.-T.; Yeh, C.-H.; Lin, C.-W.; Huang, Y.-C.; Wang, C.-H. Etiology and characteristics of patients with bronchiectasis in Taiwan: A cohort study from 2002 to 2016. BMC Pulm. Med. 2020, 20, 45. [Google Scholar] [CrossRef] [Green Version]
- Aliberti, S.; Sotgiu, G.; Lapi, F.; Gramegna, A.; Cricelli, C.; Blasi, F. Prevalence and incidence of bronchiectasis in Italy. BMC Pulm. Med. 2020, 20, 15. [Google Scholar] [CrossRef]
- Visser, S.K.; Bye, P.T.P.; Fox, G.J.; Burr, L.D.; Chang, A.B.; Holmes-Liew, C.-L.; King, P.; Middleton, P.G.; Maguire, G.P.; Smith, D.; et al. Australian adults with bronchiectasis: The first report from the Australian Bronchiectasis Registry. Respir. Med. 2019, 155, 97–103. [Google Scholar] [CrossRef]
- Ringshausen, F.C.; Rademacher, J.; Pink, I.; de Roux, A.; Hickstein, L.; Ploner, T.; Welte, T.; Diel, R. Increasing bronchiectasis prevalence in Germany, 2009–2017: A population-based cohort study. Eur. Respir. J. 2019, 54, 1900499. [Google Scholar] [CrossRef] [PubMed]
- Aksamit, T.R.; O’Donnell, A.E.; Barker, A.; Olivier, K.N.; Winthrop, K.L.; Daniels, M.L.A.; Johnson, M.; Eden, E.; Griffith, D.; Knowles, M.; et al. Adult Patients With Bronchiectasis: A First Look at the US Bronchiectasis Research Registry. Chest 2017, 151, 982–992. [Google Scholar] [CrossRef]
- Weycker, D.; Hansen, G.L.; Seifer, F.D. Prevalence and incidence of noncystic fibrosis bronchiectasis among US adults in 2013. Chronic Respir. Dis. 2017, 14, 377–384. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Song, S.O.; Jung, C.H.; Song, Y.D.; Park, C.-Y.; Kwon, H.-S.; Cha, B.-S.; Park, J.-Y.; Lee, K.-U.; Ko, K.S.; Lee, B.-W. Background and data configuration process of a nationwide population-based study using the korean national health insurance system. Diabetes Metab. J. 2014, 38, 395–403. [Google Scholar] [CrossRef] [PubMed]
- National Health Insurence Service. National Health Examination Statistical Yearbook 2014; NHIS: Seoul, Korea, 2014. [Google Scholar]
- Lee, Y.-H.; Han, K.; Ko, S.-H.; Ko, K.S.; Lee, K.-U.; Taskforce Team of Diabetes Fact Sheet of the Korean Diabetes Association. Data Analytic Process of a Nationwide Population-Based Study Using National Health Information Database Established by National Health Insurance Service. Diabetes Metab. J. 2016, 40, 79–82. [Google Scholar] [CrossRef]
- Yoo, K.-Y. Cancer Control Activities in the Republic of Korea. Jpn. J. Clin. Oncol. 2008, 38, 327–333. [Google Scholar] [CrossRef]
- Yoo, J.E.; Shin, D.W.; Han, K.; Kim, D.; Yoon, J.W.; Lee, D.-Y. Association of Female Reproductive Factors With Incidence of Fracture Among Postmenopausal Women in Korea. JAMA Netw. Open 2021, 4, e2030405. [Google Scholar] [CrossRef]
- Choi, H.; Yang, B.; Nam, H.; Kyoung, D.S.; Sim, Y.S.; Park, H.Y.; Lee, J.S.; Lee, S.W.; Oh, Y.M.; Ra, S.W.; et al. Population-based prevalence of bronchiectasis and associated comorbidities in South Korea. Eur. Respir. J. 2019, 54, 1900194. [Google Scholar] [CrossRef]
- Yang, B.; Ryu, J.; Kim, T.; Jo, Y.S.; Kim, Y.; Park, H.Y.; Kang, Y.A.; Lee, S.J.; Lee, O.-J.; Moon, J.-Y.; et al. Impact of Bronchiectasis on Incident Nontuberculous Mycobacterial Pulmonary Disease: A 10-Year National Cohort Study. Chest 2021, 159, 1807–1811. [Google Scholar] [CrossRef]
- Choi, H.; Lee, H.; Ryu, J.; Chung, S.J.; Park, D.W.; Sohn, J.W.; Yoon, H.J.; Kim, S.-H. Bronchiectasis and increased mortality in patients with corticosteroid-dependent severe asthma: A nationwide population study. Ther. Adv. Respir. Dis. 2020, 14, 1753466620963030. [Google Scholar] [CrossRef]
- Yang, B.; Han, K.; Kim, S.H.; Lee, D.-H.; Park, S.H.; Yoo, J.E.; Shin, D.W.; Choi, H.; Lee, H. Being Underweight Increases the Risk of Non-Cystic Fibrosis Bronchiectasis in the Young Population: A Nationwide Population-Based Study. Nutrients 2021, 13, 3206. [Google Scholar] [CrossRef] [PubMed]
- Choi, H.; Yang, B.; Kim, Y.J.; Sin, S.; Jo, Y.S.; Kim, Y.; Park, H.Y.; Ra, S.W.; Oh, Y.-M.; Chung, S.J.; et al. Increased mortality in patients with non cystic fibrosis bronchiectasis with respiratory comorbidities. Sci. Rep. 2021, 11, 7126. [Google Scholar] [CrossRef] [PubMed]
- Yoo, J.E.; Kim, D.; Han, K.; Rhee, S.Y.; Shin, D.W.; Lee, H. Diabetes Status and Association with Risk of Tuberculosis among Korean Adults. JAMA Netw. Open 2021, 4, e2126099. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.; Ryu, J.; Nam, E.; Chung, S.J.; Yeo, Y.; Park, D.W.; Park, T.S.; Moon, J.-Y.; Kim, T.-H.; Sohn, J.W.; et al. Increased mortality in patients with corticosteroid-dependent asthma: A nationwide population-based study. Eur. Respir. J. 2019, 54, 1900804. [Google Scholar] [CrossRef] [PubMed]
- Crimi, C.; Ferri, S.; Campisi, R.; Crimi, N. The Link between Asthma and Bronchiectasis: State of the Art. Respir. Int. Rev. Thorac. Dis. 2020, 99, 463–476. [Google Scholar] [CrossRef] [PubMed]
- Crimi, C.; Campisi, R.; Nolasco, S.; Ferri, S.; Cacopardo, G.; Impellizzeri, P.; Pistorio, M.P.; Fagone, E.; Pelaia, C.; Heffler, E.; et al. Type 2-High Severe Asthma with and without Bronchiectasis: A Prospective Observational Multicentre Study. J. Asthma Allergy 2021, 14, 1441–1452. [Google Scholar] [CrossRef]
- Martínez-García, M.; de la Rosa-Carrillo, D.; Soler-Cataluña, J.J.; Catalan-Serra, P.; Ballester, M.; Roca Vanaclocha, Y.; Agramunt, M.; Ballestin, J.; Garcia-Ortega, A.; Oscullo, G.; et al. Bronchial Infection and Temporal Evolution of Bronchiectasis in Patients With Chronic Obstructive Pulmonary Disease. Clin. Infect. Dis. 2021, 72, 403–410. [Google Scholar] [CrossRef]
- Chandrasekaran, R.; Mac Aogáin, M.; Chalmers, J.D.; Elborn, S.J.; Chotirmall, S.H. Geographic variation in the aetiology, epidemiology and microbiology of bronchiectasis. BMC Pulm. Med. 2018, 18, 83. [Google Scholar] [CrossRef]
- Zhu, D.; Chung, H.F.; Pandeya, N.; Dobson, A.J.; Kuh, D.; Crawford, S.L.; Gold, E.B.; Avis, N.E.; Giles, G.G.; Bruinsma, F.; et al. Body mass index and age at natural menopause: An international pooled analysis of 11 prospective studies. Eur. J. Epidemiol. 2018, 33, 699–710. [Google Scholar] [CrossRef]
- Casha, A.R.; Scarci, M. The link between tuberculosis and body mass index. J. Thorac. Dis. 2017, 9, E301–E303. [Google Scholar] [CrossRef] [Green Version]
- McDonald, M.N.; Wouters, E.F.M.; Rutten, E.; Casaburi, R.; Rennard, S.I.; Lomas, D.A.; Bamman, M.; Celli, B.; Agusti, A.; Tal-Singer, R.; et al. It’s more than low BMI: Prevalence of cachexia and associated mortality in COPD. Respir. Res. 2019, 20, 100. [Google Scholar] [CrossRef] [Green Version]
- Sio, Y.Y.; Chew, F.T. Risk factors of asthma in the Asian population: A systematic review and meta-analysis. J. Physiol. Anthropol. 2021, 40, 22. [Google Scholar] [CrossRef] [PubMed]
- Cheng, C.; Wu, H.; Wang, M.; Wang, L.; Zou, H.; Li, S.; Liu, R. Estrogen ameliorates allergic airway inflammation by regulating activation of NLRP3 in mice. Biosci. Rep. 2019, 39, BSR20181117. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dimitropoulou, C.; Drakopanagiotakis, F.; Chatterjee, A.; Snead, C.; Catravas, J.D. Estrogen replacement therapy prevents airway dysfunction in a murine model of allergen-induced asthma. Lung 2009, 187, 116–127. [Google Scholar] [CrossRef] [PubMed]
- Riffo-Vasquez, Y.; Ligeiro de Oliveira, A.P.; Page, C.P.; Spina, D.; Tavares-de-Lima, W. Role of sex hormones in allergic inflammation in mice. Clin. Exp. Allergy 2007, 37, 459–470. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.; Choi, H.; Sim, Y.S.; Park, S.; Kim, W.J.; Yoo, K.H.; Lee, S.J.; Kim, T.-H.; Yang, B.; Jeong, I.; et al. KMBARC registry: Protocol for a multicentre observational cohort study on non-cystic fibrosis bronchiectasis in Korea. BMJ Open 2020, 10, e034090. [Google Scholar] [CrossRef] [Green Version]
- Eun, Y.; Yoo, J.E.; Han, K.D.; Kim, D.H.; Lee, J.; Lee, D.Y.; Lee, D.H.; Kim, H.; Shin, D.W. OP0113 female reproductive factors and risk of joint replacement arthroplasty of knee and hip due to osteoarthritis in postmenopausal women: A nationwide cohort study of 1.36 million women. Ann. Rheum. Dis. 2021, 80, 62–63. [Google Scholar] [CrossRef]
- Bassuk, S.S.; Manson, J.E. The timing hypothesis: Do coronary risks of menopausal hormone therapy vary by age or time since menopause onset? Metabolism 2016, 65, 794–803. [Google Scholar] [CrossRef] [Green Version]
- Jain, R.; Ray, J.M.; Pan, J.-H.; Brody, S.L. Sex hormone-dependent regulation of cilia beat frequency in airway epithelium. Am. J. Respir. Cell Mol. Biol. 2012, 46, 446–453. [Google Scholar] [CrossRef] [Green Version]
- Modelska, K.; Cummings, S. Tibolone for postmenopausal women: Systematic review of randomized trials. J. Clin. Endocrinol. Metab. 2002, 87, 16–23. [Google Scholar] [CrossRef]
- Cho, M.K.; Park, H.M. The National Use of Hormonal Therapy in Postmenopausal Women in 2010. J. Korean Soc. Menopause 2011, 17, 150–154. [Google Scholar] [CrossRef] [Green Version]
- Ferri, S.; Crimi, C.; Heffler, E.; Campisi, R.; Noto, A.; Crimi, N. Vitamin D and disease severity in bronchiectasis. Respir. Med. 2019, 148, 1–5. [Google Scholar] [CrossRef] [PubMed]

| Premenopausal Women | Postmenopausal Women | |||||
|---|---|---|---|---|---|---|
| Subjects Who Did Not Develop Bronchiectasis (n = 944,454) | Subjects Who Did Develop Bronchiectasis (n = 15,069) | p-Value | Subjects Who Did Not Develop Bronchiectasis (n = 1,310,732) | Subjects Who Did Develop Bronchiectasis (n = 51,669) | p-Value | |
| Age (years) | 45.1 ± 4.3 | 46.9 ± 4.9 | <0.01 | 61.6 ± 8.3 | 63.1 ± 8.2 | <0.01 |
| BMI (kg/m2) | 23.2 ± 3.1 | 22.9 ± 3.1 | <0.01 | 24.2 ± 3.2 | 23.8 ± 3.3 | <0.01 |
| Smoking history | <0.01 | <0.01 | ||||
| Non-smoker | 897,230 (95.0) | 14,294 (94.8) | 1,262,129 (96.3) | 49,536 (95.9) | ||
| Ex-smoker | 15,132 (1.6) | 213 (1.5) | 13,705 (1.1) | 600 (1.2) | ||
| Current smoker | 32,092 (3.4) | 562 (3.7) | 34,898 (2.6) | 1533 (2.9) | ||
| Regular physical activity | 0.10 | <0.01 | ||||
| No | 780,458 (82.6) | 12,529 (83.2) | 1,069,822 (81.6) | 42,643 (82.6) | ||
| Yes | 163,996 (17.4) | 2540 (16.8) | 240,910 (18.4) | 9026 (17.4) | ||
| Income (quartile) | <0.01 | <0.01 | ||||
| Q1 (lowest) | 243,033 (25.7) | 3913 (25.9) | 297,366 (22.7) | 11,324 (21.9) | ||
| Q2 | 191,698 (20.3) | 3177 (21.1) | 243,680 (18.6) | 9305 (18.0) | ||
| Q3 | 209,064 (22.1) | 3405 (22.6) | 324,561 (24.8) | 12,718 (24.6) | ||
| Q4 (highest) | 300,659 (31.9) | 4574 (30.4) | 445,125 (33.9) | 18,322 (35.5) | ||
| Age at menarche (years) | 15.1 ± 1.7 | 15.4 ± 1.7 | <0.01 | 16.5 ± 1.8 | 16.6 ± 1.9 | <0.01 |
| Age at menopause (years) | 50.0 ± 4.1 | 49.9 ± 4.1 | <0.01 | |||
| Reproductive period (years) | 33.5 ± 4.4 | 33.3 ± 4.5 | <0.01 | |||
| Parity | <0.01 | <0.01 | ||||
| Nulliparous | 125,964 (13.3) | 2110 (14.0) | 30,511 (2.3) | 1217 (2.4) | ||
| One child | 780,039 (82.0) | 12,401 (82.3) | 77,231 (5.9) | 2738 (5.3) | ||
| Multiparous | 38,451 (4.7) | 558 (3.7) | 1,202,990 (91.8) | 47,714 (92.3) | ||
| Duration of breastfeeding (years) | <0.01 | <0.01 | ||||
| None | 230,001 (24.3) | 3350 (22.2) | 83,450 (6.4) | 3175 (6.1) | ||
| <0.5 | 248,072 (26.2) | 3880 (25.8) | 81,805 (6.3) | 2829 (5.5) | ||
| 0.5–1 | 295,720 (31.3) | 5393 (35.8) | 220,694 (16.8) | 7910 (15.3) | ||
| ≥1 | 170,661 (18.0) | 2446 (16.2) | 924,783 (70.5) | 37,755 (73.1) | ||
| Duration of OC use (years) | 0.18 | <0.01 | ||||
| None | 819,633 (86.7) | 13,011 (86.3) | 1,103,598 (84.2) | 43,783 (84.7) | ||
| <1 | 91,645 (9.7) | 1492 (9.9) | 123,987 (9.5) | 4652 (9.0) | ||
| ≥1 | 33,176 (3.5) | 566 (3.8) | 83,147 (6.3) | 3234 (6.3) | ||
| Duration of HRT (years) | <0.01 | |||||
| None | 1,104,212 (84.2) | 42,837 (82.9) | ||||
| <2 | 120,365 (9.3) | 4985 (9.7) | ||||
| 2–5 | 49,025 (3.7) | 2095 (4.1) | ||||
| ≥5 | 37,130 (2.8) | 1752 (3.3) | ||||
| Comorbidities | ||||||
| Diabetes mellitus | 34,637 (3.6) | 560 (3.7) | 0.75 | 176,001 (13.4) | 6544 (12.6) | <0.01 |
| Dyslipidaemia | 108,512 (11.4) | 1917 (12.7) | <0.01 | 452,441 (34.5) | 17,336 (33.5) | <0.01 |
| Cardiovascular disease | 4669 (0.9) | 145 (1.8) | <0.01 | 50,617 (5.6) | 2597 (7.2) | <0.01 |
| Asthma or COPD | 78,514 (8.3) | 2176 (14.4) | <0.01 | 171,479 (13.0) | 11,949 (23.1) | <0.01 |
| Tuberculosis | 38,681 (4.1) | 1644 (10.9) | <0.01 | 82,289 (6.2) | 6250 (12.1) | <0.01 |
| Total (n) | Bronchiectasis (n) | Follow-Up Duration (PY) | IR (/1000 PY) | HR (95% CI) | ||
|---|---|---|---|---|---|---|
| Univariable | Multivariable | |||||
| Age (years) | 1.07 (1.07, 1.08) | 1.07 (1.07, 1.08) | ||||
| BMI (kg/m2) | 0.97 (0.96, 0.97) | 0.95 (0.95, 0.96) | ||||
| Smoking history | ||||||
| Non-smoker | 911,524 | 14,294 | 7,528,360.8 | 1.89 | Reference | Reference |
| Ex-smoker | 15,345 | 213 | 126,443.2 | 1.68 | 0.88 (0.77, 1.01) | 0.98 (0.85, 1.12) |
| Current smoker | 32,654 | 562 | 268,561.0 | 2.09 | 1.10 (1.01, 1.19) | 1.14 (1.04, 1.24) |
| Regular physical activity | ||||||
| No | 792,987 | 12,529 | 6,545,086.2 | 1.91 | Reference | Reference |
| Yes | 166,536 | 2540 | 1,378,278.9 | 1.84 | 0.96 (0.92, 1.01) | 0.95 (0.91, 1.00) |
| Age at menarche (years) | ||||||
| <12 | 42,696 | 505 | 352,080.1 | 1.43 | 0.56 (0.51, 0.61) | 0.74 (0.67, 0.81) |
| 12–14 | 301,146 | 3792 | 2,486,061.3 | 1.52 | 0.60 (0.57, 0.62) | 0.78 (0.75, 0.82) |
| 14–16 | 439,342 | 7059 | 3,627,513.6 | 1.94 | 0.76 (0.73, 0.79) | 0.89 (0.86, 0.93) |
| ≥16 | 176,339 | 3713 | 1,457,709.0 | 2.54 | Reference | Reference |
| Parity | ||||||
| Nulliparous | 39,009 | 558 | 320,903.4 | 1.73 | Reference | Reference |
| One child | 128,074 | 2110 | 1,056,351.2 | 1.99 | 1.14 (1.04, 1.26) | 1.03 (0.93, 1.14) |
| Multiparous | 792,440 | 12,401 | 6,546,110.7 | 1.89 | 1.08 (1.00, 1.18) | 1.01 (0.92, 1.11) |
| Duration of breastfeeding (years) | ||||||
| None | 173,107 | 2446 | 1,427,337.2 | 1.71 | Reference | Reference |
| <0.5 | 233,351 | 3350 | 1,924,498.6 | 1.74 | 1.01 (0.96, 1.07) | 0.97 (0.92, 1.03) |
| 0.5–1 | 251,952 | 3880 | 2,081,080.5 | 1.86 | 1.08 (1.03, 1.14) | 0.99 (0.93, 1.04) |
| ≥1 | 301,113 | 5393 | 2,490,448.7 | 2.16 | 1.26 (1.20, 1.32) | 1.05 (0.99, 1.11) |
| Duration of OC use (years) | ||||||
| None | 832,644 | 13,011 | 6,875,528.4 | 1.89 | Reference | Reference |
| <1 | 93,137 | 1492 | 769,027.2 | 1.94 | 1.02 (0.97, 1.08) | 1.04 (0.98, 1.09) |
| ≥1 | 33,742 | 566 | 278,809.5 | 2.03 | 1.07 (0.98, 1.16) | 1.02 (0.93, 1.11) |
| Total (n) | Bronchiectasis (n) | Follow-Up Duration (PY) | IR (/1000 PY) | HR (95% CI) | ||
|---|---|---|---|---|---|---|
| Univariable | Multivariable | |||||
| Age (years) | 1.02 (1.02, 1.03) | 1.02 (1.02, 1.03) | ||||
| BMI (kg/m2) | 0.96 (0.95, 0.96) | 0.96 (0.96, 0.97) | ||||
| Smoking history | ||||||
| Non-smoker | 1,311,665 | 49,536 | 10,623,789.8 | 4.66 | Reference | Reference |
| Ex-smoker | 14,305 | 600 | 113,888.1 | 5.26 | 1.13 (1.04, 1.22) | 1.13 (1.04, 1.23) |
| Current smoker | 36,431 | 1533 | 287,390.0 | 5.33 | 1.14 (1.08, 1.20) | 1.10 (1.05, 1.16) |
| Regular physical activity | ||||||
| No | 1,112,465 | 42,643 | 8,985,784.4 | 4.74 | Reference | Reference |
| Yes | 249,936 | 9026 | 2,039,283.6 | 4.42 | 0.93 (0.91, 0.95) | 0.96 (0.94, 0.98) |
| Age at menarche (years) | ||||||
| <12 | 12,954 | 418 | 105,648.2 | 3.96 | 0.79 (0.72–0.87) | |
| 12–14 | 164,560 | 5586 | 1,339,752.9 | 4.17 | 0.83 (0.81–0.86) | |
| 14–16 | 524,836 | 18,996 | 4,255,170.5 | 4.46 | 0.89 (0.88–0.91) | |
| ≥16 | 660,051 | 26,669 | 5,324,496.4 | 5.01 | Reference | |
| Age at menopause (years) | ||||||
| <40 | 24,290 | 1003 | 194,175.6 | 5.17 | Reference | |
| 40–45 | 80,042 | 3225 | 641,612.4 | 5.03 | 0.97 (0.91, 1.05) | |
| 45–50 | 371,284 | 14,078 | 3,004,544.3 | 4.69 | 0.91 (0.85, 0.97) | |
| 50–55 | 740,042 | 27,841 | 5,994,369.0 | 4.64 | 0.90 (0.85, 0.96) | |
| ≥55 | 146,743 | 5522 | 1,190,366.4 | 4.64 | 0.90 (0.84, 0.96) | |
| Reproductive period (years) | ||||||
| <30 | 192,647 | 8018 | 1,543,989.8 | 5.19 | Reference | Reference |
| 30–35 | 568,223 | 22,028 | 4,590,126.7 | 4.80 | 0.95 (0.90, 0.95) | 0.97 (0.95, 0.99) |
| 35–40 | 513,918 | 18,479 | 4,179,829.6 | 4.42 | 0.85 (0.83, 0.87) | 0.94 (0.91, 0.96) |
| ≥40 | 87,613 | 3144 | 711,121.8 | 4.42 | 0.85 (0.82, 0.89) | 0.90 (0.86, 0.94) |
| Parity | ||||||
| Nulliparous | 31,728 | 1217 | 257,028.2 | 4.73 | Reference | Reference |
| One child | 79,969 | 2738 | 650,986.6 | 4.21 | 0.89 (0.83, 0.95) | 0.95 (0.88, 1.02) |
| Multiparous | 1,250,704 | 47,714 | 10,117,053.2 | 4.72 | 0.99 (0.94, 1.05) | 0.98 (0.92, 1.04) |
| Duration of breastfeeding (years) | ||||||
| None | 86,625 | 3175 | 703,992.0 | 4.51 | Reference | Reference |
| <0.5 | 84,634 | 2829 | 690,832.9 | 4.10 | 0.91 (0.86, 0.96) | 0.92 (0.87, 0.97) |
| 0.5–1 | 228,604 | 7910 | 1,860,046.3 | 4.25 | 0.94 (0.91, 0.98) | 0.93 (0.88, 0.97) |
| ≥1 | 962,538 | 37,755 | 7,770,196.7 | 4.86 | 1.08 (1.04, 1.12) | 0.98 (0.94, 1.02) |
| Duration of OC use (years) | ||||||
| None | 1,147,381 | 43,783 | 9,274,646.3 | 4.72 | Reference | Reference |
| <1 | 128,639 | 4652 | 1,048,247.7 | 4.44 | 0.94 (0.91, 0.97) | 0.97 (0.94, 0.99) |
| ≥1 | 86,381 | 3234 | 702,174.0 | 4.61 | 0.98 (0.94, 1.01) | 0.98 (0.94, 1.01) |
| Duration of HRT (years) | ||||||
| None | 1,147,049 | 42,837 | 9,265,189.4 | 4.62 | Reference | Reference |
| <2 | 125,350 | 4985 | 1,025,341.5 | 4.86 | 1.05 (1.02, 1.08) | 1.16 (1.12, 1.19) |
| 2–5 | 51,120 | 2095 | 417,429.4 | 5.02 | 1.09 (1.04, 1.13) | 1.17 (1.12, 1.23) |
| ≥5 | 38,882 | 1752 | 317,107.6 | 5.52 | 1.20 (1.14, 1.25) | 1.24 (1.18, 1.30) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yang, B.; Lee, D.-H.; Han, K.; Choi, H.; Kang, H.K.; Shin, D.W.; Lee, H. Female Reproductive Factors and the Risk of Bronchiectasis: A Nationwide Population-Based Longitudinal Study. Biomedicines 2022, 10, 303. https://doi.org/10.3390/biomedicines10020303
Yang B, Lee D-H, Han K, Choi H, Kang HK, Shin DW, Lee H. Female Reproductive Factors and the Risk of Bronchiectasis: A Nationwide Population-Based Longitudinal Study. Biomedicines. 2022; 10(2):303. https://doi.org/10.3390/biomedicines10020303
Chicago/Turabian StyleYang, Bumhee, Dong-Hwa Lee, Kyungdo Han, Hayoung Choi, Hyung Koo Kang, Dong Wook Shin, and Hyun Lee. 2022. "Female Reproductive Factors and the Risk of Bronchiectasis: A Nationwide Population-Based Longitudinal Study" Biomedicines 10, no. 2: 303. https://doi.org/10.3390/biomedicines10020303
APA StyleYang, B., Lee, D.-H., Han, K., Choi, H., Kang, H. K., Shin, D. W., & Lee, H. (2022). Female Reproductive Factors and the Risk of Bronchiectasis: A Nationwide Population-Based Longitudinal Study. Biomedicines, 10(2), 303. https://doi.org/10.3390/biomedicines10020303







