High Levels of Progesterone Receptor B in MCF-7 Cells Enable Radical Anti-Tumoral and Anti-Estrogenic Effect of Progestin
Abstract
:1. Introduction
2. Materials and Methods
2.1. Cell Culture
2.2. Establishment of Stable Overexpression of PRB in MCF-7 Cells
2.3. Adenoviral Transduction
2.4. Treatment with Promegestone (R5020) and 17β-Estradiol (E2)
2.5. Cell Growth and Cell Cycle Analysis
2.6. BrdU Incorporation
2.7. Tumorsphere Formation in Matrigel
2.8. Cell Recovery from Matrigel for Quantification
2.9. Effect of R5020 on Cell Growth and DNA Fragmentation in 2% Matrigel
2.10. Protein Lysate Collection and Western Blotting Analysis
2.11. RNA Extraction and Gene Expression Analysis
2.12. Flow Cytometry Analysis of CD44+ and CD24+ Population
2.13. Detection of Chromatin-Bound ERα and FOXA1 by Cell Fractionation
2.14. Statistical Analysis
3. Results
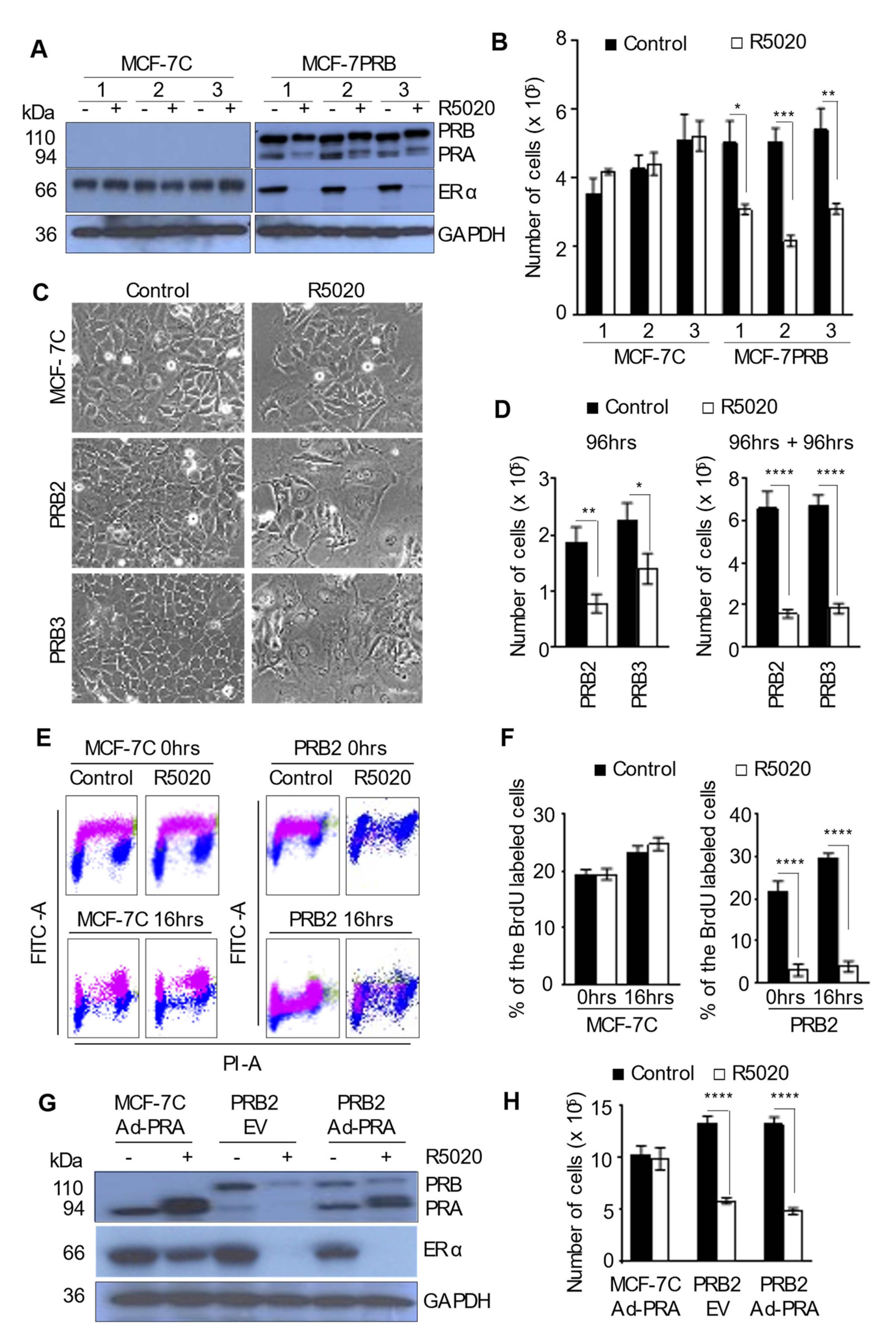
3.1. R5020 Induces Replicative Senescence in MCF-7 Cells Expressing High Levels of PRB
3.2. PRA Exerts No Effect on Cell Growth in Response to R5020
3.3. Progestin Exerts Biphasic Effect on Cell Cycle Regulators
3.4. R5020-Induced Replicative Senescence in MCF-7PRB Cells Is Associated with Senescence-Associated Secretory Phenotype (SASP)
3.5. R5020 Enhanced CD24+CD44+ Population in MCF-7PRB Cells
3.6. R5020 Inhibits Tumorsphere Formation and Induces Massive Apoptosis of MCF-7PRB Cells in Matrigel Culture
3.7. R5020 Exerts Robust Anti-Estrogenic Effect in MCF-7PRB Cells
3.8. R5020 Suppress the Genomic Effect of Estrogen through Inhibiting the Expression of ERα and Its Pioneer Factor FOXA1
4. Discussion
4.1. Progestin Exerts Strong Anti-Tumoral Effects in MCF-7 Cells with High Levels of Stably Transfected PRB
4.2. The Mechanisms for High Levels of PRB-Mediated Growth Arrest Are Multifaceted
4.3. R5020 Also Induces Molecular Changes That Promote Survival
4.4. High Levels of PRB Mediates the Radical Anti-Estrogenic Effect by Down-Regulating ERα and FOXA1
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| American Type Culture Collection | (ATCC); |
| Cyclin A2 gene | (CCNA2); |
| Cyclin B1 gene | (CCNB1); |
| Cyclin D1 gene | (CCND1); |
| Cyclin E1 gene | (CCNE1); |
| Cyclin dependent kinases | (CDKs); |
| Cycle Threshold | (CT); |
| Cycloheximide | (CHX); |
| Dextran-Coated Charcoal Treated | (DCC-FCS); |
| Dulbecco’s Modified Eagle’s Medium | (DMEM); |
| Estradiol 17β, | (E2); |
| Estrogen Receptor | (ER); |
| Estrogen receptor gene | (ESR-1); |
| Fetal Calf Serum | (FCS); |
| Human Glyceraldehyde-3-Phosphate Dehydrogenase | (GAPDH); |
| Horseradish Peroxidase, | (HRP); |
| Hormone Replacement Therapy | (HRT); |
| Nuclear Factor Kappa B | (NF-κB); |
| Microtubule-associated Protein 1 Light Chain 3 | (LC3B); |
| Mitogen-activated Protein Kinases | (MAPK); |
| Multiplication of Infection | (MOI); |
| Vector Control | (cDNA); |
| Polyvinylidene Difluoride | (PDVF); |
| Progesterone Receptor | (PR); |
| Progesterone Receptor isoform A | (PRA); |
| Progesterone Receptor isoform B | (PRB); |
| Propidium Iodide (PI): Phosphatase and Tensin homolog on chromosome 10 | (PTEN); |
| Synthetic Progestin promegestone | (R5020); |
| Retinoblastoma protein | (RB); |
| Retinoblastoma gene | (Rb); |
| Sodium Dodecyl Sulfate | (SDS); |
| Standard Error of the Mean | (SEM). |
References
- Osborne, C.K.; Schiff, R. Mechanisms of endocrine resistance in breast cancer. Annu. Rev. Med. 2011, 62, 233–247. [Google Scholar] [CrossRef] [PubMed]
- Sathyamoorthy, N.; Lange, C.A. Progesterone and Breast Cancer: An NCI Workshop Report. Horm. Cancer 2020, 11, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Hagan, C.R.; Lange, C.A. Molecular determinants of context-dependent progesterone receptor action in breast cancer. BMC Med. 2014, 12, 32. [Google Scholar] [CrossRef] [PubMed]
- Rossouw, J.E.; Anderson, G.L.; Prentice, R.L.; LaCroix, A.Z.; Kooperberg, C.; Stefanick, M.L.; Jackson, R.D.; Beresford, S.A.; Howard, B.V.; Johnson, K.C.; et al. Risks and benefits of estrogen plus progestin in healthy postmenopausal women: Principal results From the Women’s Health Initiative randomized controlled trial. JAMA 2002, 288, 321–333. [Google Scholar] [CrossRef]
- Beral, V. Breast cancer and hormone-replacement therapy in the Million Women Study. Lancet 2003, 362, 419–427. [Google Scholar] [CrossRef]
- Collaborative Group on Hormonal Factors in Breast, C. Type and timing of menopausal hormone therapy and breast cancer risk: Individual participant meta-analysis of the worldwide epidemiological evidence. Lancet 2019, 394, 1159–1168. [Google Scholar] [CrossRef]
- Manson, J.E.; Chlebowski, R.T.; Stefanick, M.L.; Aragaki, A.K.; Rossouw, J.E.; Prentice, R.L.; Anderson, G.; Howard, B.V.; Thomson, C.A.; LaCroix, A.Z.; et al. Menopausal hormone therapy and health outcomes during the intervention and extended poststopping phases of the Women’s Health Initiative randomized trials. JAMA 2013, 310, 1353–1368. [Google Scholar] [CrossRef]
- Buzdar, A.; Douma, J.; Davidson, N.; Elledge, R.; Morgan, M.; Smith, R.; Porter, L.; Nabholtz, J.; Xiang, X.; Brady, C. Phase III, multicenter, double-blind, randomized study of letrozole, an aromatase inhibitor, for advanced breast cancer versus megestrol acetate. J. Clin. Oncol. 2001, 19, 3357–3366. [Google Scholar] [CrossRef]
- Abrams, J.; Aisner, J.; Cirrincione, C.; Berry, D.A.; Muss, H.B.; Cooper, M.R.; Henderson, I.C.; Panasci, L.; Kirshner, J.; Ellerton, J.; et al. Dose-response trial of megestrol acetate in advanced breast cancer: Cancer and leukemia group B phase III study 8741. J. Clin. Oncol. 1999, 17, 64–73. [Google Scholar] [CrossRef]
- Lundgren, S. Progestins in breast cancer treatment. A review. Acta Oncol. 1992, 31, 709–722. [Google Scholar] [CrossRef]
- Chlebowski, R.T.; Anderson, G.L.; Aragaki, A.K.; Manson, J.E.; Stefanick, M.L.; Pan, K.; Barrington, W.; Kuller, L.H.; Simon, M.S.; Lane, D.; et al. Association of Menopausal Hormone Therapy With Breast Cancer Incidence and Mortality During Long-term Follow-up of the Women’s Health Initiative Randomized Clinical Trials. JAMA 2020, 324, 369–380. [Google Scholar] [CrossRef] [PubMed]
- Carroll, J.S.; Hickey, T.E.; Tarulli, G.A.; Williams, M.; Tilley, W.D. Deciphering the divergent roles of progestogens in breast cancer. Nat. Rev. Cancer 2017, 17, 54–64. [Google Scholar] [CrossRef] [PubMed]
- Horwitz, K.B.; Sartorius, C.A. 90 Years of Progesterone: Progesterone and progesterone receptors in breast cancer: Past, present, future. J. Mol. Endocrinol. 2020, 65, T49–T63. [Google Scholar] [CrossRef] [PubMed]
- An, W.; Lin, H.; Ma, L.; Zhang, C.; Zheng, Y.; Cheng, Q.; Ma, C.; Wu, X.; Zhang, Z.; Zhong, Y.; et al. Progesterone activates GPR126 to promote breast cancer development via the Gi pathway. Proc. Natl. Acad. Sci. USA 2022, 119, e2117004119. [Google Scholar] [CrossRef]
- Groshong, S.D.; Owen, G.I.; Grimison, B.; Schauer, I.E.; Todd, M.C.; Langan, T.A.; Sclafani, R.A.; Lange, C.A.; Horwitz, K.B. Biphasic regulation of breast cancer cell growth by progesterone: Role of the cyclin-dependent kinase inhibitors, p21 and p27(Kip1). Mol. Endocrinol. 1997, 11, 1593–1607. [Google Scholar] [CrossRef]
- Musgrove, E.A.; Lee, C.S.L.; Sutherland, R.L. Progestins Both Stimulate and Inhibit Breast-Cancer Cell-Cycle Progression While Increasing Expression of Transforming Growth Factor-Alpha, Epidermal Growth-Factor Receptor, C-Fos, and C-Myc Genes. Mol. Cell Biol. 1991, 11, 5032–5043. [Google Scholar] [CrossRef]
- Lin, V.C.; Ng, E.H.; Aw, S.E.; Tan, M.G.; Chan, V.S.; Ho, G.H. Progestins inhibit the growth of MDA-MB-231 cells transfected with progesterone receptor complementary DNA. Clin. Cancer. Res. 1999, 5, 395–403. [Google Scholar]
- Lin, V.C.; Eng, A.S.; Hen, N.E.; Ng, E.H.; Chowdhury, S.H. Effect of progesterone on the invasive properties and tumor growth of progesterone receptor-transfected breast cancer cells MDA-MB-231. Clin. Cancer. Res. 2001, 7, 2880–2886. [Google Scholar]
- Boonyaratanakornkit, V.; Scott, M.P.; Ribon, V.; Sherman, L.; Anderson, S.M.; Maller, J.L.; Miller, W.T.; Edwards, D.P. Progesterone receptor contains a proline-rich motif that directly interacts with SH3 domains and activates c-Src family tyrosine kinases. Mol. Cell 2001, 8, 269–280. [Google Scholar] [CrossRef]
- Migliaccio, A.; Piccolo, D.; Castoria, G.; Di Domenico, M.; Bilancio, A.; Lombardi, M.; Gong, W.; Beato, M.; Auricchio, F. Activation of the Src/p21ras/Erk pathway by progesterone receptor via cross-talk with estrogen receptor. EMBO J. 1998, 17, 2008–2018. [Google Scholar] [CrossRef]
- Lin, V.C.; Aw, S.E.; Ng, E.H.; Tan, M.G. Demonstration of mixed properties of RU486 in progesterone receptor (PR)-transfected MDA-MB-231 cells: A model for studying the functions of progesterone analogues. Br. J Cancer 2001, 85, 1978–1986. [Google Scholar] [CrossRef] [PubMed]
- Zheng, Z.Y.; Zheng, S.M.; Bay, B.H.; Aw, S.E.; V, C.L.L. Anti-estrogenic mechanism of unliganded progesterone receptor isoform B in breast cancer cells. Breast Cancer Res. Treat. 2007, 110, 111–125. [Google Scholar] [CrossRef] [PubMed]
- Vignon, F.; Bardon, S.; Chalbos, D.; Rochefort, H. Antiestrogenic effect of R5020, a synthetic progestin in human breast cancer cells in culture. J. Clin. Endocrinol. Metab. 1983, 56, 1124–1130. [Google Scholar] [CrossRef] [PubMed]
- Mohammed, H.; Russell, I.A.; Stark, R.; Rueda, O.M.; Hickey, T.E.; Tarulli, G.A.; Serandour, A.A.; Birrell, S.N.; Bruna, A.; Saadi, A.; et al. Progesterone receptor modulates ERalpha action in breast cancer. Nature 2015, 523, 313–317. [Google Scholar] [CrossRef] [PubMed]
- Singhal, H.; Greene, M.E.; Tarulli, G.; Zarnke, A.L.; Bourgo, R.J.; Laine, M.; Chang, Y.F.; Ma, S.; Dembo, A.G.; Raj, G.V.; et al. Genomic agonism and phenotypic antagonism between estrogen and progesterone receptors in breast cancer. Sci. Adv. 2016, 2, e1501924. [Google Scholar] [CrossRef] [PubMed]
- Daniel, A.R.; Gaviglio, A.L.; Knutson, T.P.; Ostrander, J.H.; D’Assoro, A.B.; Ravindranathan, P.; Peng, Y.; Raj, G.V.; Yee, D.; Lange, C.A. Progesterone receptor-B enhances estrogen responsiveness of breast cancer cells via scaffolding PELP1- and estrogen receptor-containing transcription complexes. Oncogene 2015, 34, 506–515. [Google Scholar] [CrossRef]
- Zheng, Z.Y.; Bay, B.H.; Aw, S.E.; Lin, V.C. A novel antiestrogenic mechanism in progesterone receptor-transfected breast cancer cells. J. Biol. Chem. 2005, 280, 17480–17487. [Google Scholar] [CrossRef]
- De Amicis, F.; Zupo, S.; Panno, M.L.; Malivindi, R.; Giordano, F.; Barone, I.; Mauro, L.; Fuqua, S.A.W.; Ando, S. Progesterone Receptor B Recruits a Repressor Complex to a Half-PRE Site of the Estrogen Receptor alpha Gene Promoter. Mol. Endocrinol. 2009, 23, 454–465. [Google Scholar] [CrossRef]
- Alexander, I.E.; Shine, J.; Sutherland, R.L. Progestin regulation of estrogen receptor messenger RNA in human breast cancer cells. Mol. Endocrinol. 1990, 4, 821–828. [Google Scholar] [CrossRef]
- Wiley, C.D.; Campisi, J. From ancient pathways to aging cells - Connecting metabolism and cellular senescence. Cell Metab. 2016, 23, 1013–1021. [Google Scholar] [CrossRef] [PubMed]
- Jacobsen, B.M.; Horwitz, K.B. Progesterone receptors, their isoforms and progesterone regulated transcription. Mol. Cell Endocrinol. 2012, 357, 18–29. [Google Scholar] [CrossRef]
- Leo, J.C.; Wang, S.M.; Guo, C.H.; Aw, S.E.; Zhao, Y.; Li, J.M.; Hui, K.M.; Lin, V.C. Gene regulation profile reveals consistent anticancer properties of progesterone in hormone-independent breast cancer cells transfected with progesterone receptor. Int. J. Cancer 2005, 117, 561–568. [Google Scholar] [CrossRef] [PubMed]
- McGowan, E.M.; Clarke, C.L. Effect of overexpression of progesterone receptor A on endogenous progestin-sensitive endpoints in breast cancer cells. Mol. Endocrinol. 1999, 13, 1657–1671. [Google Scholar] [CrossRef]
- Chellappan, S.P.; Hiebert, S.; Mudryj, M.; Horowitz, J.M.; Nevins, J.R. The E2f Transcription Factor Is a Cellular Target for the Rb Protein. Cell 1991, 65, 1053–1061. [Google Scholar] [CrossRef]
- Coppe, J.P.; Desprez, P.Y.; Krtolica, A.; Campisi, J. The Senescence-Associated Secretory Phenotype: The Dark Side of Tumor Suppression. Annu. Rev. Pathol.-Mech. 2010, 5, 99–118. [Google Scholar] [CrossRef] [PubMed]
- Ortiz-Montero, P.; Londono-Vallejo, A.; Vernot, J.P. Senescence-associated IL-6 and IL-8 cytokines induce a self- and cross-reinforced senescence/inflammatory milieu strengthening tumorigenic capabilities in the MCF-7 breast cancer cell line. Cell Commun. Signal. 2017, 15, 17. [Google Scholar] [CrossRef]
- Paciotti, G.F.; Tamarkin, L. Interleukin-1 Directly Regulates Hormone-Dependent Human Breast Cancer Cell Proliferation in Vitro. Mol. Endocrinol. 1988, 2, 459–464. [Google Scholar] [CrossRef] [PubMed]
- Chiu, J.W.; Binte Hanafi, Z.; Chew, L.C.Y.; Mei, Y.; Liu, H. IL-1alpha Processing, Signaling and Its Role in Cancer Progression. Cells 2021, 10, 92. [Google Scholar] [CrossRef]
- Orjalo, A.V.; Bhaumik, D.; Gengler, B.K.; Scott, G.K.; Campisi, J. Cell surface-bound IL-1alpha is an upstream regulator of the senescence-associated IL-6/IL-8 cytokine network. Proc. Natl. Acad. Sci. USA 2009, 106, 17031–17036. [Google Scholar] [CrossRef]
- Chien, Y.; Scuoppo, C.; Wang, X.; Fang, X.; Balgley, B.; Bolden, J.E.; Premsrirut, P.; Luo, W.; Chicas, A.; Lee, C.S.; et al. Control of the senescence-associated secretory phenotype by NF-kappaB promotes senescence and enhances chemosensitivity. Genes Dev. 2011, 25, 2125–2136. [Google Scholar] [CrossRef] [PubMed]
- Mercurio, F.; Zhu, H.; Murray, B.W.; Shevchenko, A.; Bennett, B.L.; Li, J.; Young, D.B.; Barbosa, M.; Mann, M.; Manning, A.; et al. IKK-1 and IKK-2: Cytokine-activated IkappaB kinases essential for NF-kappaB activation. Science 1997, 278, 860–866. [Google Scholar] [CrossRef] [PubMed]
- Sasaki, C.Y.; Barberi, T.J.; Ghosh, P.; Longo, D.L. Phosphorylation of RelA/p65 on serine 536 defines an I{kappa}B{alpha}-independent NF-{kappa}B pathway. J. Biol. Chem. 2005, 280, 34538–34547. [Google Scholar] [CrossRef] [PubMed]
- Axlund, S.D.; Yoo, B.H.; Rosen, R.B.; Schaack, J.; Kabos, P.; Labarbera, D.V.; Sartorius, C.A. Progesterone-inducible cytokeratin 5-positive cells in luminal breast cancer exhibit progenitor properties. Horm. Cancer 2013, 4, 36–49. [Google Scholar] [CrossRef] [PubMed]
- Li, W.; Ma, H.; Zhang, J.; Zhu, L.; Wang, C.; Yang, Y. Unraveling the roles of CD44/CD24 and ALDH1 as cancer stem cell markers in tumorigenesis and metastasis. Sci. Rep. 2017, 7, 13856. [Google Scholar] [CrossRef]
- Tan, S.; Bajalovic, N.; Wong, E.S.P.; Lin, V.C.L. Ligand-activated progesterone receptor B activates transcription factor EB to promote autophagy in human breast cancer cells. Exp. Cell Res. 2019, 382, 111433. [Google Scholar] [CrossRef]
- Carroll, J.S.; Liu, X.S.; Brodsky, A.S.; Li, W.; Meyer, C.A.; Szary, A.J.; Eeckhoute, J.; Shao, W.; Hestermann, E.V.; Geistlinger, T.R.; et al. Chromosome-wide mapping of estrogen receptor binding reveals long-range regulation requiring the forkhead protein FoxA1. Cell 2005, 122, 33–43. [Google Scholar] [CrossRef]
- Hurtado, A.; Holmes, K.A.; Ross-Innes, C.S.; Schmidt, D.; Carroll, J.S. FOXA1 is a key determinant of estrogen receptor function and endocrine response. Nat. Genet. 2011, 43, 27–33. [Google Scholar] [CrossRef] [PubMed]
- Meyer, M.E.; Gronemeyer, H.; Turcotte, B.; Bocquel, M.T.; Tasset, D.; Chambon, P. Steroid hormone receptors compete for factors that mediate their enhancer function. Cell 1989, 57, 433–442. [Google Scholar] [CrossRef]
- Cittelly, D.M.; Finlay-Schultz, J.; Howe, E.N.; Spoelstra, N.S.; Axlund, S.D.; Hendricks, P.; Jacobsen, B.M.; Sartorius, C.A.; Richer, J.K. Progestin suppression of miR-29 potentiates dedifferentiation of breast cancer cells via KLF4. Oncogene 2012, 32, 2555–2564. [Google Scholar] [CrossRef]
- Finlay-Schultz, J.; Cittelly, D.M.; Hendricks, P.; Patel, P.; Kabos, P.; Jacobsen, B.M.; Richer, J.K.; Sartorius, C.A. Progesterone downregulation of miR-141 contributes to expansion of stem-like breast cancer cells through maintenance of progesterone receptor and Stat5a. Oncogene 2015, 34, 3676–3687. [Google Scholar] [CrossRef]
- Al-Hajj, M.; Wicha, M.S.; Benito-Hernandez, A.; Morrison, S.J.; Clarke, M.F. Prospective identification of tumorigenic breast cancer cells. Proc. Natl. Acad. Sci. USA 2003, 100, 3983–3988. [Google Scholar] [CrossRef] [PubMed]
- Sheridan, C.; Kishimoto, H.; Fuchs, R.K.; Mehrotra, S.; Bhat-Nakshatri, P.; Turner, C.H.; Goulet, R., Jr.; Badve, S.; Nakshatri, H. CD44+/CD24- breast cancer cells exhibit enhanced invasive properties: An early step necessary for metastasis. Breast Cancer Res. 2006, 8, R59. [Google Scholar] [CrossRef] [PubMed]
- Salminen, A.; Kauppinen, A.; Kaarniranta, K. Emerging role of NF-kappaB signaling in the induction of senescence-associated secretory phenotype (SASP). Cell Signal. 2012, 24, 835–845. [Google Scholar] [CrossRef]
- Rovillain, E.; Mansfield, L.; Caetano, C.; Alvarez-Fernandez, M.; Caballero, O.L.; Medema, R.H.; Hummerich, H.; Jat, P.S. Activation of nuclear factor-kappa B signalling promotes cellular senescence. Oncogene 2011, 30, 2356–2366. [Google Scholar] [CrossRef] [PubMed]
- Sgagias, M.K.; Kasid, A.; Danforth, D.N. Interleukin-1-Alpha and Tumor-Necrosis-Factor-Alpha (Tnf Alpha) Inhibit Growth and Induce Tnf Messenger-Rna in Mcf-7 Human Breast-Cancer Cells. Mol. Endocrinol. 1991, 5, 1740–1747. [Google Scholar] [CrossRef]
- Danforth, D.N., Jr.; Sgagias, M.K. Interleukin-1 alpha and interleukin-6 act additively to inhibit growth of MCF-7 breast cancer cells in vitro. Cancer Res. 1993, 53, 1538–1545. [Google Scholar] [PubMed]
- Kang, T.W.; Yevsa, T.; Woller, N.; Hoenicke, L.; Wuestefeld, T.; Dauch, D.; Hohmeyer, A.; Gereke, M.; Rudalska, R.; Potapova, A.; et al. Senescence surveillance of pre-malignant hepatocytes limits liver cancer development. Nature 2011, 479, 547–551. [Google Scholar] [CrossRef] [PubMed]
- Acosta, J.C.; Banito, A.; Wuestefeld, T.; Georgilis, A.; Janich, P.; Morton, J.P.; Athineos, D.; Kang, T.W.; Lasitschka, F.; Andrulis, M.; et al. A complex secretory program orchestrated by the inflammasome controls paracrine senescence. Nat. Cell Biol. 2013, 15, 978–990. [Google Scholar] [CrossRef]
- Kale, J.; Osterlund, E.J.; Andrews, D.W. BCL-2 family proteins: Changing partners in the dance towards death. Cell Death Differ. 2018, 25, 65–80. [Google Scholar] [CrossRef] [PubMed]
- Pattingre, S.; Tassa, A.; Qu, X.; Garuti, R.; Liang, X.H.; Mizushima, N.; Packer, M.; Schneider, M.D.; Levine, B. Bcl-2 antiapoptotic proteins inhibit Beclin 1-dependent autophagy. Cell 2005, 122, 927–939. [Google Scholar] [CrossRef]
- Lima, R.T.; Martins, L.M.; Guimaraes, J.E.; Sambade, C.; Vasconcelos, M.H. Specific downregulation of bcl-2 and xIAP by RNAi enhances the effects of chemotherapeutic agents in MCF-7 human breast cancer cells. Cancer Gene Ther. 2004, 11, 309–316. [Google Scholar] [CrossRef]
- Akar, U.; Chaves-Reyez, A.; Barria, M.; Tari, A.; Sanguino, A.; Kondo, Y.; Kondo, S.; Arun, B.; Lopez-Berestein, G.; Ozpolat, B. Silencing of Bcl-2 expression by small interfering RNA induces autophagic cell death in MCF-7 breast cancer cells. Autophagy 2008, 4, 669–679. [Google Scholar] [CrossRef] [PubMed]
- Tan, S.K.; Lin, Z.H.; Chang, C.W.; Varang, V.; Chng, K.R.; Pan, Y.F.; Yong, E.L.; Sung, W.K.; Cheung, E. AP-2gamma regulates oestrogen receptor-mediated long-range chromatin interaction and gene transcription. EMBO J. 2011, 30, 2569–2581. [Google Scholar] [CrossRef] [PubMed]
- Nezis, I.P.; Shravage, B.V.; Sagona, A.P.; Johansen, T.; Baehrecke, E.H.; Stenmark, H. Autophagy as a trigger for cell death: Autophagic degradation of inhibitor of apoptosis dBruce controls DNA fragmentation during late oogenesis in Drosophila. Autophagy 2010, 6, 1214–1215. [Google Scholar] [CrossRef] [PubMed]
- Aupperlee, M.D.; Leipprandt, J.R.; Bennett, J.M.; Schwartz, R.C.; Haslam, S.Z. Amphiregulin mediates progesterone-induced mammary ductal development during puberty. Breast Cancer Res. 2013, 15, R44. [Google Scholar] [CrossRef]
- Peterson, E.A.; Jenkins, E.C.; Lofgren, K.A.; Chandiramani, N.; Liu, H.; Aranda, E.; Barnett, M.; Kenny, P.A. Amphiregulin Is a Critical Downstream Effector of Estrogen Signaling in ERalpha-Positive Breast Cancer. Cancer Res. 2015, 75, 4830–4838. [Google Scholar] [CrossRef] [PubMed]
- Singhal, H.; Greene, M.E.; Zarnke, A.L.; Laine, M.; Al Abosy, R.; Chang, Y.F.; Dembo, A.G.; Schoenfelt, K.; Vadhi, R.; Qiu, X.; et al. Progesterone receptor isoforms, agonists and antagonists differentially reprogram estrogen signaling. Oncotarget 2018, 9, 4282–4300. [Google Scholar] [CrossRef] [PubMed]
- Le Dily, F.; Vidal, E.; Cuartero, Y.; Quilez, J.; Nacht, A.S.; Vicent, G.P.; Carbonell-Caballero, J.; Sharma, P.; Villanueva-Canas, J.L.; Ferrari, R.; et al. Hormone-control regions mediate steroid receptor-dependent genome organization. Genome Res. 2019, 29, 29–39. [Google Scholar] [CrossRef] [PubMed]
- Mieczkowski, K.; Kitowska, K.; Braun, M.; Galikowska-Bogut, B.; Gorska-Arcisz, M.; Piasecka, D.; Stawiski, K.; Zaczek, A.J.; Nejc, D.; Kordek, R.; et al. FGF7/FGFR2-JunB signalling counteracts the effect of progesterone in luminal breast cancer. Mol. Oncol. 2022. [Google Scholar] [CrossRef] [PubMed]
- Swinstead, E.E.; Miranda, T.B.; Paakinaho, V.; Baek, S.; Goldstein, I.; Hawkins, M.; Karpova, T.S.; Ball, D.; Mazza, D.; Lavis, L.D.; et al. Steroid Receptors Reprogram FoxA1 Occupancy through Dynamic Chromatin Transitions. Cell 2016, 165, 593–605. [Google Scholar] [CrossRef]
- Wen, W.; Chen, Z.; Bao, J.; Long, Q.; Shu, X.O.; Zheng, W.; Guo, X. Genetic variations of DNA bindings of FOXA1 and co-factors in breast cancer susceptibility. Nat. Commun. 2021, 12, 5318. [Google Scholar] [CrossRef] [PubMed]
- Kurozumi, S.; Matsumoto, H.; Hayashi, Y.; Tozuka, K.; Inoue, K.; Horiguchi, J.; Takeyoshi, I.; Oyama, T.; Kurosumi, M. Power of PgR expression as a prognostic factor for ER-positive/HER2-negative breast cancer patients at intermediate risk classified by the Ki67 labeling index. BMC Cancer 2017, 17, 354. [Google Scholar] [CrossRef] [PubMed]





| Primer Name | Primer Sequence–5’ to 3’ | |
|---|---|---|
| AREG | Forward | GTGGTGCTGTCGCTCTTGATA |
| Reverse | CCCCAGAAAATGGTTCACGCT | |
| ERα | Forward | GAGGGCAGGGGTGAA |
| Reverse | GGCCAGGCTGTTCTTCTTAG | |
| FOXA1 | Forward | GCAATACTCGCCTTACGGCT |
| Reverse | TACACACCTTGGTAGTACGCC | |
| IL-1α | Forward | AGATGCCTGAGATACCCAAAACC |
| Reverse | CCAAGCACACCCAGTAGTCT | |
| IL1β | Forward | TTCGACACATGGGATAACGAGG |
| Reverse | TTTTTGCTGTGAGTCCCGGAG | |
| IL-8 | Forward | GGGCCAAGAGAATATCCGAAC |
| Reverse | TGGATCCTGGCTAGCAGACTA | |
| NFKBIA | Forward | CTCCGAGACTTTCGAGGAAATAC |
| Reverse | GCCATTGTAGTTGGTAGCCTTCA | |
| pS2 | Forward | GCCATCGAGAACACTCAAGAAGAAG |
| Reverse | ACTGTGTCACCAGCCAGATGGA | |
| 36B4 | Forward | GATTGGCTACCCAACTGTTGCA |
| Reverse | CAGGGGCAGCAGCCACAAAGGC | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bajalovic, N.; Or, Y.Z.; Woo, A.R.E.; Lee, S.H.; Lin, V.C.L. High Levels of Progesterone Receptor B in MCF-7 Cells Enable Radical Anti-Tumoral and Anti-Estrogenic Effect of Progestin. Biomedicines 2022, 10, 1860. https://doi.org/10.3390/biomedicines10081860
Bajalovic N, Or YZ, Woo ARE, Lee SH, Lin VCL. High Levels of Progesterone Receptor B in MCF-7 Cells Enable Radical Anti-Tumoral and Anti-Estrogenic Effect of Progestin. Biomedicines. 2022; 10(8):1860. https://doi.org/10.3390/biomedicines10081860
Chicago/Turabian StyleBajalovic, Natasa, Yu Zuan Or, Amanda R. E. Woo, Shi Hao Lee, and Valerie C. L. Lin. 2022. "High Levels of Progesterone Receptor B in MCF-7 Cells Enable Radical Anti-Tumoral and Anti-Estrogenic Effect of Progestin" Biomedicines 10, no. 8: 1860. https://doi.org/10.3390/biomedicines10081860
APA StyleBajalovic, N., Or, Y. Z., Woo, A. R. E., Lee, S. H., & Lin, V. C. L. (2022). High Levels of Progesterone Receptor B in MCF-7 Cells Enable Radical Anti-Tumoral and Anti-Estrogenic Effect of Progestin. Biomedicines, 10(8), 1860. https://doi.org/10.3390/biomedicines10081860





