Integrative Approaches in Acute Ischemic Stroke: From Symptom Recognition to Future Innovations
Abstract
:1. Introduction
2. Onset and Recognition
- The populace of southern Poland displays a level of stroke awareness that can be deemed inadequate, especially when considering the urgency and timeliness needed for effective stroke management.
- Personal experiences, particularly having a friend or relative who has suffered a stroke, stand out as the most influential factor in having adequate stroke knowledge [105].
3. Neuroimaging and Neuroradiology: A Deep Dive
3.1. The Evolution of Neuroimaging in Stroke Diagnosis and Its Historical Context
- A clinical lacunar syndrome does not always correlate with the size of the infarct—it can sometimes be linked to a larger infarct.
- Identifying a lacunar infarct through a CT scan does not negate the need for further angiographic studies, especially if there is a likelihood of detecting an embolic source [109].
3.2. An In-Depth Look into Neuroimaging Modalities and Their Role in Post-Stroke Recovery Prediction
3.3. Post-Stroke Angiogenesis and the Expanding Horizons of Advanced Neuroimaging
3.4. Advancements in Stroke Treatment and the Role of Neuroimaging
3.5. Understanding Cerebral Artery Occlusions and the Evolution of Stroke Treatments
3.6. Harnessing Neuroradiology for Therapy Planning: Delving into Techniques and Implications
3.7. Pioneering Neuroimaging Optimization: Charting the Path to Precision Diagnostics
3.8. Radiologists and Neurologists: Crafting a Symbiotic Diagnostic Journey
3.9. Leveraging Deep Learning in Neuroimaging: A Paradigm Shift
3.10. Comprehensive Cerebral Imaging: Collaborative Diagnostics in Emergency Care
4. Treatment Paradigms
4.1. Pharmacological Approach
4.1.1. Exploring Intravenous Thrombolytic Agents: An In-depth Analysis of Mechanisms, Advantages, and Potential Hazards
- Alteplase and Potential Alternatives in Stroke Treatment. Alteplase currently stands as the sole drug greenlighted by the FDA for the thrombolysis of acute ischemic stroke (AIS). However, the research horizon is dotted with other thrombolytic agents that might potentially rival or replace alteplase in the future. This comprehensive study dives deep into the potency and safety of an array of such agents—urokinase, ateplase, tenecteplase, and reteplase. Through sophisticated computational simulations entwining both pharmacokinetics and pharmacodynamics, paired with a meticulous local fibrinolysis model, we benchmarked the drugs against multiple metrics: clot dissolution timeframe, resistance to plasminogen activator inhibitor (PAI), potential risk of intracranial hemorrhage (ICH), and the latency from drug introduction to clot dissolution [177].
- 2.
- Intracerebral Hemorrhage’s Impact on Mortality Rates. Taking a retrospective stance, this study sifted through data from South Korea’s national health insurance service database, spanning 2005–2018. The focal cohort consisted of hyperacute ischemic stroke patients who had undergone intravenous thrombolysis. A stark comparison was drawn between ICH-afflicted patients and those who avoided ICH. An alarming revelation was that within the 12-month window post-treatment, the mortality rate in the ICH cohort was more than double that of their counterparts (42.8% vs. 17.5%). This suggests that ICH post-thrombolysis can drastically heighten the risk of mortality in hyperacute ischemic stroke patients, amplifying it nearly threefold [182,183].
- 3.
- The Promise of Plasmin Nanoformulations in Ischemic Stroke Treatment. While thrombolytic therapy remains the gold standard for treating ischemic strokes, its current mainstream agent, the tissue plasminogen activator (tPA), often encounters obstacles due to an associated hemorrhage risk. Plasmin, a direct fibrinolytic agent, offers a safer hemostatic profile. However, its therapeutic potential diminishes when introduced intravenously due to rapid inactivation by anti-plasmin. To navigate this, nanoformulations have emerged as viable tools to enhance drug stability. This study unveils a groundbreaking nanoformulation for plasmin, demonstrating increased stability and heightened therapeutic efficacy, potentially redefining ischemic stroke treatment [184].
- 4.
- Decoding Blood–Brain Barrier Deficits Post-Stroke. Utilizing advanced two-photon microscopy, Knowland et al. have painted a vivid picture of changes in tight junctions (TJs) post-stroke in transgenic mouse models. Observations indicated that the blood–brain barrier (BBB) started leaking as early as 6 h post-ischemia, even though profound structural defects in TJs only became evident after 48 h. The increase in endothelial caveolae and transcytosis rate post-ischemia suggests a sequential deterioration of barrier mechanisms, highlighting the multifaceted impacts on the BBB following a stroke [185].
4.1.2. Fibrinolytic Therapy in Acute Ischemic Stroke: A Comprehensive Analysis
Understanding the Fibrinolytic Approach and its Clinical Applications
Complementary Medications Enhancing Mainline Therapy
| Methods | Major Characteristics | Advantages | Limitations | References |
|---|---|---|---|---|
| rTMS (repetitive transcranial magnetic stimulation) |
| Balances excitability across hemispheres and realigns the linguistic network. | Requires the formulation of an optimal treatment protocol; must consider individual variability. | [205,206,207] |
| tDCS (transcranial direct current stimulation) |
| Aids in normalizing brain activity, fostering self-recovery. | Further extensive clinical trials needed for a broader PSA group. | [208] |
- Diving Deeper into Successful Pharmacological Interventions:
4.2. Endovascular Thrombectomy
4.2.1. Evolution of Endovascular Strategies over Time
4.2.2. Mechanisms of Mechanical Thrombectomy
4.2.3. Spotlight on Equipment: Delving into Stent Retrievers, Aspiration Catheters, and Their Innovations
4.2.4. The Benefits and Implications of Surgical Revascularization
4.2.5. Procedure Walkthrough: A Comprehensive Overview from Patient Selection to Post-Operative Care
4.2.6. Early Post-Operative Strokes: An Analysis of Incidence, Risk Factors, and Outcomes
- An American Society of Anesthesiologists (ASA) physical status of ≥3 was associated with a higher risk (adjusted OR: 3.12) [242].
- Surgeries lasting more than 120 min also elevated the risk (adjusted OR: 10.69) [242].
- Experiencing intra-operative hypotension and the usage of inotropes/vasopressors during surgery also increased the risk (adjusted OR: 2.80) [242].
4.2.7. The Transformative Effects of Timely Endovascular Intervention: Key Insights from Case Studies
5. Combined Treatment Modalities
5.1. Global Prevalence and Management of Stroke
5.2. The Promise of Combined Therapies
5.3. Advancements in Stroke Management
5.4. Complications, Implications, and Potential Interventions
5.5. Immune Dynamics Post-Stroke
6. Envisioning Comprehensive Patient Care
- Merging Physical Rehabilitation with Acute Stroke Care:
- 2.
- Pharmacological Enhancements Post-Stroke:
6.1. Objective Evaluation of Non-Pharmacological Therapeutic Interventions in Acute Ischemic Stroke
- Clinical-functional evaluation tools: These instruments, like the Glasgow coma scale (GCS), Glasgow outcome score scale (GOS), modified Rankin scale, and the national institutes of health stroke scale (NIHSS), provide key insights into a patient’s neuro-functional state [283].
- Neuroimaging and Neurophysiological Examinations: Technologies such as structural and functional magnetic resonance imaging, positron emission tomography (PET), single-photon emission computed tomography (SPECT), and repetitive/transcranial magnetic stimulation (r/TMS) give in-depth visuals and data about the brain’s condition. Additionally, considering a patient’s general health and neuro-functional state, tools like functional near-infrared spectroscopy (f/NIR) and diverse immuno-(cyto)/histochemical assays could also be invaluable. Similarly, pairing transcranial magnetic stimulation (TMS) with high-density EEG offers a non-invasive method to perturb and measure, providing insights into both local neuronal conditions and signal dispersion within functional networks. Notably, even in patients who appeared clinically identical (e.g., lacking residual arm functionality or lacking peripheral motor-evoked potential from standard TMS), TMS-EEG unveiled varied response patterns that correlated with subsequent recovery. This underscores the profound potential of TMS-EEG as a novel indicator of the motor network’s functional reserve [284].
6.2. Cardiac Connections to Stroke
6.3. Rehabilitation after Stroke: An Ongoing Journey
6.4. Psychological and Cognitive Repercussions of Stroke
6.5. Education and Intervention: Addressing the Rising Incidence of Stroke
6.6. Community Engagement and Support: Building Resilience among Stroke Survivors
7. Future Horizons in Stroke Management
7.1. On the Brink of Discovery: The Future of Diagnostic Techniques and Treatments
7.2. Advancements in Stroke Prediction: The Role of Machine Learning and Biomarkers
7.3. The Revolutionary Impact of AI and Machine Learning in Stroke Management
7.4. The Technological Revolution in Stroke Diagnostics and Rehabilitation
7.5. Deep Dive into EEG Data for Stroke Prediction
7.6. The Evolution and Potential Future of Cerebrovascular Disease Management
7.7. Bridging Research and Clinical Practices in Stroke Rehabilitation: A Comprehensive Exploration
8. Conclusions
8.1. Interconnected Aspects of Stroke Management: A Comprehensive Overview
8.2. Unveiling the Path Forward: Stroke Research, Cellular Mechanisms, and Clinical Advances
- Immediate Response:
- Upon the onset of stroke symptoms, the emergency medical services (EMS) dispatch is contacted (t = 0).
- Initial Assessment by EMS:
- The EMS team initiates a ‘case entry protocol’ to assess the patient’s medical condition based on specific parameters.
- Patient Transportation:
- The patient is transported to the nearest hospital via ambulance, a process that ideally takes 15 min or less (t ≤ 15 min).
- Traditional Stroke Identification Protocol:
- Best Case: If the EMS has already diagnosed the patient with a stroke, they are directly sent to a specialized stroke unit.
- Alternate Case: If not pre-diagnosed by EMS, the patient is directed to the Emergency Department (ED), where they await assessment alongside patients with various medical emergencies (t ≤ 30 min).
- A neurologist then evaluates the suspected stroke patient (t ≤ 60 min). The most prevalent neurological assessment tool is the NIHSS, followed by a CT/MRI scan for an initial diagnosis (t ≤ 90 min).
- The classification of the stroke subtype is then determined, with the process taking up to 120 min (t ≤ 120 min). Classification methods include the Trial of Org 10172 in Acute Stroke Treatment (TOAST), National Institute of Neurological Disorders and Stroke (NINDS), or Oxford Community Stroke Project (OCSP) schemes.
- The administration of the tissue plasminogen activator (tPA) typically occurs within 3 h from the onset of stroke symptoms (t ≤ 180 min).
- POCT-Enhanced Stroke Identification Protocol:
- The utilization of pre-hospital POCT devices can expedite the timeline from the onset of stroke symptoms to the examination by a neurologist, reducing the wait time to 20 min or less (t ≤ 20 min).
- Leveraging in-hospital POCT tools can decrease the time required for a CT/MRI scan (t ≤ 45 min).
- Most critically, the window for administering tPA can be significantly shortened to between 60 and 90 min post-symptom onset (60 min ≤ t ≤ 90 min).
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Heidenreich, P.A.; Trogdon, J.G.; Khavjou, O.A.; Butler, J.; Dracup, K.; Ezekowitz, M.D.; Finkelstein, E.A.; Hong, Y.; Johnston, S.C.; Khera, A.; et al. Forecasting the Future of Cardiovascular Disease in the United States. Circulation 2011, 123, 933–944. [Google Scholar] [CrossRef] [PubMed]
- O’Donnell, M.J.; Chin, S.L.; Rangarajan, S.; Xavier, D.; Liu, L.; Zhang, H.; Rao-Melacini, P.; Zhang, X.; Pais, P.; Agapay, S.; et al. Global and regional effects of potentially modifiable risk factors associated with acute stroke in 32 countries (INTERSTROKE): A case-control study. Lancet 2016, 388, 761–775. [Google Scholar] [CrossRef] [PubMed]
- Feigin, V.L.; Stark, B.A.; Johnson, C.O.; Roth, G.A.; Bisignano, C.; Abady, G.G.; Abbasifard, M.; Abbasi-Kangevari, M.; Abd-Allah, F.; Abedi, V.; et al. Global, regional, and national burden of stroke and its risk factors, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet Neurol. 2021, 20, 795–820. [Google Scholar] [CrossRef] [PubMed]
- Yan, F.; Yan, S.; Wang, J.; Cui, Y.; Chen, F.; Fang, F.; Cui, W. Association between triglyceride glucose index and risk of cerebrovascular disease: Systematic review and meta-analysis. Cardiovasc. Diabetol. 2022, 21, 226. [Google Scholar] [CrossRef] [PubMed]
- Goldstein, L.B. Introduction for Focused Updates in Cerebrovascular Disease. Stroke 2020, 51, 708–710. [Google Scholar] [CrossRef]
- Haberman, S.; Capildeo, R.; Rose, F.C. The Changing Mortality of Cerebrovascular Disease. QJM 1978, 47, 71–88. [Google Scholar] [CrossRef]
- Portegies, M.; Koudstaal, P.; Ikram, M. Cerebrovascular disease. In Handbook of Clinical Neurology; Elsevier: Amsterdam, The Netherlands, 2016; Volume 138, pp. 239–261. [Google Scholar] [CrossRef]
- de Havenon, A.; Meyer, C.; McNally, J.S.; Alexander, M.; Chung, L. Subclinical Cerebrovascular Disease: Epidemiology and Treatment. Curr. Atheroscler. Rep. 2019, 21, 39. [Google Scholar] [CrossRef]
- Saini, V.; Guada, L.; Yavagal, D.R. Global Epidemiology of Stroke and Access to Acute Ischemic Stroke Interventions. Neurology 2021, 97, S6–S16. [Google Scholar] [CrossRef]
- Ovbiagele, B.; Nguyen-Huynh, M.N. Stroke Epidemiology: Advancing Our Understanding of Disease Mechanism and Therapy. Neurotherapeutics 2011, 8, 319–329. [Google Scholar] [CrossRef]
- Ohene-Frempong, K.; Weiner, S.J.; Sleeper, L.A.; Miller, S.T.; Embury, S.; Moohr, J.W.; Wethers, D.L.; Pegelow, C.H.; Gill, F.M. Cerebrovascular accidents in sickle cell disease: Rates and risk factors. Blood 1998, 91, 288–294. [Google Scholar]
- Xu, J.; Zhang, X.; Jin, A.; Pan, Y.; Li, Z.; Meng, X.; Wang, Y. Trends and Risk Factors Associated With Stroke Recurrence in China, 2007–2018. JAMA Netw. Open 2022, 5, e2216341. [Google Scholar] [CrossRef] [PubMed]
- Putaala, J. Ischemic Stroke in Young Adults. Contin. Lifelong Learn. Neurol. 2020, 26, 386–414. [Google Scholar] [CrossRef] [PubMed]
- Salvadori, E.; Papi, G.; Insalata, G.; Rinnoci, V.; Donnini, I.; Martini, M.; Falsini, C.; Hakiki, B.; Romoli, A.; Barbato, C.; et al. Comparison between Ischemic and Hemorrhagic Strokes in Functional Outcome at Discharge from an Intensive Rehabilitation Hospital. Diagnostics 2020, 11, 38. [Google Scholar] [CrossRef] [PubMed]
- Chugh, C. Acute Ischemic Stroke: Management Approach. Indian J. Crit. Care Med. 2019, 23, 140–146. [Google Scholar] [CrossRef]
- Cao, R.; Qi, P.; Jiang, Y.; Hu, S.; Ye, G.; Zhu, Y.; Li, L.; You, Z.; Chen, J. Preliminary Application of a Quantitative Collateral Assessment Method in Acute Ischemic Stroke Patients With Endovascular Treatments: A Single-Center Study. Front. Neurol. 2021, 12, 714313. [Google Scholar] [CrossRef]
- Oh, M.; Lee, M. Clinical Implications of Prominent Cortical Vessels on Susceptibility-Weighted Imaging in Acute Ischemic Stroke Patients Treated with Recanalization Therapy. Brain Sci. 2022, 12, 184. [Google Scholar] [CrossRef]
- Mirończuk, A.; Kapica-Topczewska, K.; Socha, K.; Soroczyńska, J.; Jamiołkowski, J.; Chorąży, M.; Czarnowska, A.; Mitrosz, A.; Kułakowska, A.; Kochanowicz, J. Disturbed Ratios between Essential and Toxic Trace Elements as Potential Biomarkers of Acute Ischemic Stroke. Nutrients 2023, 15, 1434. [Google Scholar] [CrossRef]
- Chen, C.; Xun, P.; Tsinovoi, C.; McClure, L.A.; Brockman, J.; MacDonald, L.; Cushman, M.; Cai, J.; Kamendulis, L.; Mackey, J.; et al. Urinary cadmium concentration and the risk of ischemic stroke. Neurology 2018, 91, e382–e391. [Google Scholar] [CrossRef]
- Dias, F.A.; Castro-Afonso, L.H.; Zotin, M.C.Z.; Alessio-Alves, F.F.; Filho, R.K.D.V.M.; Camilo, M.R.; Nakiri, G.S.; Abud, D.G.; Pontes-Neto, O.M. Collateral Scores and Outcomes after Endovascular Treatment for Basilar Artery Occlusion. Cerebrovasc. Dis. 2019, 47, 285–290. [Google Scholar] [CrossRef]
- Etherton, M.R.; Barreto, A.D.; Schwamm, L.H.; Wu, O. Neuroimaging Paradigms to Identify Patients for Reperfusion Therapy in Stroke of Unknown Onset. Front. Neurol. 2018, 9, 327. [Google Scholar] [CrossRef]
- Ravindran, A.V.; Killingsworth, M.C.; Bhaskar, S. Cerebral collaterals in acute ischaemia: Implications for acute ischaemic stroke patients receiving reperfusion therapy. Eur. J. Neurosci. 2020, 53, 1238–1261. [Google Scholar] [CrossRef]
- Macleod, M.R.; Lewis, S.C.; Dennis, M.S. Effect of deprivation on time to hospital in acute stroke. J. Neurol. Neurosurg. Psychiatry 2003, 74, 545–546. [Google Scholar] [CrossRef]
- Cox, A.M.; McKevitt, C.; Rudd, A.G.; Da Wolfe, C. Socioeconomic status and stroke. Lancet Neurol. 2006, 5, 181–188. [Google Scholar] [CrossRef]
- Abilleira, S.; Lucente, G.; Ribera, A.; Permanyer-Miralda, G.; Gallofré, M. Patient-related features associated with a delay in seeking care after stroke. Eur. J. Neurol. 2010, 18, 850–856. [Google Scholar] [CrossRef]
- Eriksson, M.; Glader, E.-L.; Norrving, B.; Stegmayr, B.; Asplund, K. Acute stroke alert activation, emergency service use, and reperfusion therapy in Sweden. Brain Behav. 2017, 7, e00654. [Google Scholar] [CrossRef] [PubMed]
- Iosif, C.; Papathanasiou, M.; Staboulis, E.; Gouliamos, A. Social factors influencing hospital arrival time in acute ischemic stroke patients. Neuroradiology 2011, 54, 361–367. [Google Scholar] [CrossRef] [PubMed]
- Niklasson, A.; Herlitz, J.; Jood, K. Socioeconomic disparities in prehospital stroke care. Scand. J. Trauma Resusc. Emerg. Med. 2019, 27, 53. [Google Scholar] [CrossRef]
- Kleindorfer, D.O.; Lindsell, C.J.; Broderick, J.P.; Flaherty, M.L.; Woo, D.; Ewing, I.; Schmit, P.; Moomaw, C.; Alwell, K.; Pancioli, A.; et al. Community socioeconomic status and prehospital times in acute stroke and transient ischemic attack: Do poorer patients have longer delays from 911 call to the emergency department? Stroke 2006, 37, 1508–1513. [Google Scholar] [CrossRef] [PubMed]
- Park, H.A.; Lee, H.A.; Park, J.O. Association between Area-Level Socioeconomic Deprivation and Prehospital Delay in Acute Ischemic Stroke Patients: An Ecological Study. Int. J. Environ. Res. Public Health 2020, 17, 7392. [Google Scholar] [CrossRef] [PubMed]
- Bhaskar, S.; Bivard, A.; Stanwell, P.; Parsons, M.; Attia, J.R.; Nilsson, M.; Levi, C. Baseline collateral status and infarct topography in post-ischaemic perilesional hyperperfusion: An arterial spin labelling study. J. Cereb. Blood Flow Metab. 2016, 37, 1148–1162. [Google Scholar] [CrossRef]
- Leng, X.; Fang, H.; Leung, T.W.; Mao, C.; Xu, Y.; Miao, Z.; Liu, L.; Wong, K.L.; Liebeskind, D.S. Impact of Collateral Status on Successful Revascularization in Endovascular Treatment: A Systematic Review and Meta-Analysis. Cerebrovasc. Dis. 2015, 41, 27–34. [Google Scholar] [CrossRef] [PubMed]
- Qian, J.; Fan, L.; Zhang, W.; Wang, J.; Qiu, J.; Wang, Y. A meta-analysis of collateral status and outcomes of mechanical thrombectomy. Acta Neurol. Scand. 2020, 142, 191–199. [Google Scholar] [CrossRef] [PubMed]
- Helisch, A.; Schaper, W. Arteriogenesis The Development and Growth of Collateral Arteries. Microcirculation 2003, 10, 83–97. [Google Scholar] [CrossRef]
- Rebello, L.C.; Bouslama, M.; Haussen, D.C.; Grossberg, J.A.; Dehkharghani, S.; Anderson, A.; Belagaje, S.R.; Bianchi, N.A.; Grigoryan, M.; Frankel, M.R.; et al. Stroke etiology and collaterals: Atheroembolic strokes have greater collateral recruitment than cardioembolic strokes. Eur. J. Neurol. 2017, 24, 762–767. [Google Scholar] [CrossRef] [PubMed]
- Hassler, E.; Kneihsl, M.; Deutschmann, H.; Hinteregger, N.; Magyar, M.; Wießpeiner, U.; Haidegger, M.; Fandler-Höfler, S.; Eppinger, S.; Niederkorn, K.; et al. Relationship between stroke etiology and collateral status in anterior circulation large vessel occlusion. J. Neurol. 2020, 267, 3362–3370. [Google Scholar] [CrossRef]
- Sinha, A.; Stanwell, P.; Beran, R.G.; Calic, Z.; Killingsworth, M.C.; Bhaskar, S.M.M. Stroke Aetiology and Collateral Status in Acute Ischemic Stroke Patients Receiving Reperfusion Therapy—A Meta-Analysis. Neurol. Int. 2021, 13, 608–621. [Google Scholar] [CrossRef]
- Söderqvist, K.; Kaijser, M.; Söderman, M.; Holmin, S.; Wahlgren, N.; Andersson, T. Mechanical thrombectomy in acute ischemic stroke—Experience from 6 years of practice. Neuroradiology 2014, 56, 477–486. [Google Scholar] [CrossRef]
- Świtońska, M.; Słomka, A.; Korbal, P.; Piekuś-Słomka, N.; Sinkiewicz, W.; Sokal, P.; Żekanowska, E. Association of Neutrophil-to-Lymphocyte Ratio and Lymphocyte-to-Monocyte Ratio with Treatment Modalities of Acute Ischaemic Stroke: A Pilot Study. Medicina 2019, 55, 342. [Google Scholar] [CrossRef]
- Musuka, T.D.; Wilton, S.B.; Traboulsi, M.; Hill, M.D. Diagnosis and management of acute ischemic stroke: Speed is critical. Can. Med. Assoc. J. 2015, 187, 887–893. [Google Scholar] [CrossRef]
- Martínez-Sánchez, P.; Gutiérrez-Fernández, M.; Fuentes, B.; Masjuán, J.; Cases, M.A.d.L.; Novillo-López, M.E.; Díez-Tejedor, E. Biochemical and inflammatory biomarkers in ischemic stroke: Translational study between humans and two experimental rat models. J. Transl. Med. 2014, 12, 220. [Google Scholar] [CrossRef]
- Hill, M.D.; Jackowski, G.; Bayer, N.; Lawrence, M.; Jaeschke, R. Biochemical markers in acute ischemic stroke. Can. Med. Assoc. J. 2000, 162, 1139–1140. [Google Scholar]
- Teppo, K.; Jaakkola, J.; Biancari, F.; Halminen, O.; Putaala, J.; Mustonen, P.; Haukka, J.; Linna, M.; Kinnunen, J.; Tiili, P.; et al. Mental health conditions and risk of first-ever ischaemic stroke and death in patients with incident atrial fibrillation: A nationwide cohort study. Eur. J. Clin. Investig. 2022, 52, e13801. [Google Scholar] [CrossRef] [PubMed]
- Li, W.; Xiao, W.-M.; Chen, Y.-K.; Qu, J.-F.; Liu, Y.-L.; Fang, X.-W.; Weng, H.-Y.; Luo, G.-P. Anxiety in Patients With Acute Ischemic Stroke: Risk Factors and Effects on Functional Status. Front. Psychiatry 2019, 10, 257. [Google Scholar] [CrossRef] [PubMed]
- Hoyer, C.; Schmidt, H.L.; Kranaster, L.; Alonso, A. Impact of psychiatric comorbidity on the severity, short-term functional outcome, and psychiatric complications after acute stroke. Neuropsychiatr. Dis. Treat. 2019, 15, 1823–1831. [Google Scholar] [CrossRef] [PubMed]
- Hwang, J.-H.; Lim, S.-B. Antioxidant and Anti-inflammatory Activities of Broccoli Florets in LPS-stimulated RAW 264.7 Cells. Prev. Nutr. Food Sci. 2014, 19, 89–97. [Google Scholar] [CrossRef]
- Kamal, F.Z.; Lefter, R.; Jaber, H.; Balmus, I.-M.; Ciobica, A.; Iordache, A.-C. The Role of Potential Oxidative Biomarkers in the Prognosis of Acute Ischemic Stroke and the Exploration of Antioxidants as Possible Preventive and Treatment Options. Int. J. Mol. Sci. 2023, 24, 6389. [Google Scholar] [CrossRef]
- Pedersen, P.M.; Jørgensen, H.S.; Nakayama, H.; Raaschou, H.O.; Olsen, T.S. Aphasia in acute stroke: Incidence, determinants, and recovery. Ann. Neurol. 1995, 38, 659–666. [Google Scholar] [CrossRef]
- Ellis, C.; Urban, S. Age and aphasia: A review of presence, type, recovery and clinical outcomes. Top. Stroke Rehabil. 2016, 23, 430–439. [Google Scholar] [CrossRef]
- Butler, R.A.; Ralph, M.A.L.; Woollams, A.M. Capturing multidimensionality in stroke aphasia: Mapping principal behavioural components to neural structures. Brain 2014, 137, 3248–3266. [Google Scholar] [CrossRef]
- Katsari, M.; Angelopoulou, G.; Laskaris, N.; Potagas, C.; Kasselimis, D. Common Neuroanatomical Substrate of Cholinergic Pathways and Language-Related Brain Regions as an Explanatory Framework for Evaluating the Efficacy of Cholinergic Pharmacotherapy in Post-Stroke Aphasia: A Review. Brain Sci. 2022, 12, 1273. [Google Scholar] [CrossRef]
- Mozaffarian, D.; Benjamin, E.J.; Go, A.S.; Arnett, D.K.; Blaha, M.J.; Cushman, M.; de Ferranti, S.; Després, J.-P.; Fullerton, H.J.; Howard, V.J.; et al. Heart disease and stroke statistics—2015 update: A report from the American Heart Association. Circulation 2015, 131, e29–e322. [Google Scholar] [CrossRef] [PubMed]
- Yang, Q.; Tong, X.; Schieb, L.; Vaughan, A.; Gillespie, C.; Wiltz, J.L.; King, S.C.; Odom, E.; Merritt, R.; Hong, Y.; et al. Vital Signs: Recent Trends in Stroke Death Rates—United States, 2000–2015. MMWR Morb. Mortal. Wkly. Rep. 2017, 66, 933–939. [Google Scholar] [CrossRef] [PubMed]
- Knight-Greenfield, A.; Nario, J.J.Q.; Gupta, A. Causes of Acute Stroke. Radiol. Clin. N. Am. 2019, 57, 1093–1108. [Google Scholar] [CrossRef] [PubMed]
- Thrift, A.G.; Thayabaranathan, T.; Howard, G.; Howard, V.J.; Rothwell, P.M.; Feigin, V.L.; Norrving, B.; Donnan, G.A.; Cadilhac, D.A. Global stroke statistics. Int. J. Stroke 2016, 12, 13–32. [Google Scholar] [CrossRef] [PubMed]
- Montaner, J.; Alvarez-Sabín, J. NIH stroke scale and its adaptation to Spanish. Neurologia 2006, 21, 192–202. [Google Scholar]
- Soto-Cámara, R.; González-Santos, J.; González-Bernal, J.; Martín-Santidrian, A.; Cubo, E.; Trejo-Gabriel-Galán, J.M. Factors Associated with Shortening of Prehospital Delay among Patients with Acute Ischemic Stroke. J. Clin. Med. 2019, 8, 1712. [Google Scholar] [CrossRef]
- Tao, W.-D.; Liu, M.; Fisher, M.; Wang, D.-R.; Li, J.; Furie, K.L.; Hao, Z.-L.; Lin, S.; Zhang, C.-F.; Zeng, Q.-T.; et al. Posterior Versus Anterior Circulation Infarction. Stroke 2012, 43, 2060–2065. [Google Scholar] [CrossRef]
- Keselman, B.; Gdovinová, Z.; Jatuzis, D.; Melo, T.P.E.; Vilionskis, A.; Cavallo, R.; Frol, S.; Jurak, L.; Koyuncu, B.; Nunes, A.P.; et al. Safety and Outcomes of Intravenous Thrombolysis in Posterior Versus Anterior Circulation Stroke. Stroke 2020, 51, 876–882. [Google Scholar] [CrossRef]
- Lindsberg, P.J.; Pekkola, J.; Strbian, D.; Sairanen, T.; Mattle, H.P.; Schroth, G. Time window for recanalization in basilar artery occlusion: Speculative synthesis. Neurology 2015, 85, 1806–1815. [Google Scholar] [CrossRef]
- Berndt, M.; Poppert, H.; Steiger, K.; Pelisek, J.; Oberdieck, P.; Maegerlein, C.; Zimmer, C.; Wunderlich, S.; Friedrich, B.; Boeckh-Behrens, T.; et al. Thrombus Histology of Basilar Artery Occlusions. Clin. Neuroradiol. 2020, 31, 753–761. [Google Scholar] [CrossRef]
- Aroor, S.; Singh, R.; Goldstein, L.B. BE-FAST (Balance, Eyes, Face, Arm, Speech, Time). Stroke 2017, 48, 479–481. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Zhao, X.; Xu, F.; Guo, M.; Yang, Y.; Zhong, L.; Weng, X.; Liu, X. A Systematic Review and Meta-Analysis Comparing FAST and BEFAST in Acute Stroke Patients. Front. Neurol. 2022, 12, 765069. [Google Scholar] [CrossRef] [PubMed]
- Puustjärvi, V.; Strbian, D.; Tiainen, M.; Curtze, S.; Tatlisumak, T.; Sairanen, T. Recognition of posterior circulation stroke. Acta Neurol. Scand. 2014, 131, 389–393. [Google Scholar] [CrossRef] [PubMed]
- Halúsková, S.; Herzig, R.; Krajíčková, D.; Hamza, A.; Krajina, A.; Chovanec, V.; Lojík, M.; Raupach, J.; Renc, O.; Šimůnek, L.; et al. Acute Management Should Be Optimized in Patients with Less Specific Stroke Symptoms: Findings from a Retrospective Observational Study. J. Clin. Med. 2021, 10, 1143. [Google Scholar] [CrossRef] [PubMed]
- Sommer, P.; Seyfang, L.; Posekany, A.; Ferrari, J.; Lang, W.; Fertl, E.; Serles, W.; Töll, T.; Kiechl, S.; Greisenegger, S. Prehospital and intra-hospital time delays in posterior circulation stroke: Results from the Austrian Stroke Unit Registry. J. Neurol. 2016, 264, 131–138. [Google Scholar] [CrossRef] [PubMed]
- Tong, X.; Liao, X.; Pan, Y.; Cao, Y.; Wang, C.; Liu, L.; Zheng, H.; Zhao, X.; Wang, C.; Wang, Y.; et al. Intravenous thrombolysis is more safe and effective for posterior circulation stroke. Medicine 2016, 95, e3848. [Google Scholar] [CrossRef]
- Ekkert, A.; Milmantienė, D.; Jokimaitytė, U.; Jatužis, D. Posterior Circulation Stroke Patients Receive Less Reperfusion Therapy Because of Late Arrival and Relative Contraindications: A Retrospective Study. J. Clin. Med. 2023, 12, 5181. [Google Scholar] [CrossRef]
- Tsirlin, I.; Dupierrix, E.; Chokron, S.; Coquillart, S.; Ohlmann, T.; Kim, K.; Kim, J.; Ku, J.; Kim, D.Y.; Chang, W.H.; et al. Uses of Virtual Reality for Diagnosis, Rehabilitation and Study of Unilateral Spatial Neglect: Review and Analysis. CyberPsychology Behav. 2009, 12, 175–181. [Google Scholar] [CrossRef]
- Cinnera, A.M.; Bisirri, A.; Chioccia, I.; Leone, E.; Ciancarelli, I.; Iosa, M.; Morone, G.; Verna, V. Exploring the Potential of Immersive Virtual Reality in the Treatment of Unilateral Spatial Neglect Due to Stroke: A Comprehensive Systematic Review. Brain Sci. 2022, 12, 1589. [Google Scholar] [CrossRef]
- Munn, Z.; Moola, S.; Riitano, D.; Lisy, K. The development of a critical appraisal tool for use in systematic reviews addressing questions of prevalence. Int. J. Health Policy Manag. 2014, 3, 123–128. [Google Scholar] [CrossRef]
- Porritt, K.; Gomersall, J.; Lockwood, C. JBI’s Systematic Reviews: Study selection. AJN Am. J. Nurs. 2014, 114, 47–52. [Google Scholar] [CrossRef] [PubMed]
- Munn, Z.; Tufanaru, C.; Aromataris, E. JBI’s Systematic Reviews: Data extraction. AJN Am. J. Nurs. 2014, 114, 49–54. [Google Scholar] [CrossRef] [PubMed]
- Filep, E.M.; Murata, Y.; Endres, B.D.; Kim, G.; Stearns, R.L.; Casa, D.J. Exertional Heat Stroke, Modality Cooling Rate, and Survival Outcomes: A Systematic Review. Medicina 2020, 56, 589. [Google Scholar] [CrossRef]
- Rhee, J.Y.; Colman, M.A.; Mendu, M.; Shah, S.J.; Fox, M.D.; Rost, N.S.; Kimchi, E.Y. Associations Between Stroke Localization and Delirium: A Systematic Review and Meta-Analysis. J. Stroke Cerebrovasc. Dis. 2022, 31, 106270. [Google Scholar] [CrossRef]
- Abawi, M.; Nijhoff, F.; Agostoni, P.; de Vries, R.; Slooter, A.J.; Emmelot-Vonk, M.H.; Voskuil, M.; Leiner, T.; Doevendans, P.A.; Stella, P.R. Effect of New Cerebral Ischemic Lesions on the Delirium Occurrence After Transcatheter Aortic Valve Replacement. J. Am. Coll. Cardiol. 2016, 68, 1489–1490. [Google Scholar] [CrossRef] [PubMed]
- Strand, T.; Asplund, K.; Eriksson, S.; Hägg, E.; Lithner, F.; Wester, P.O. A non-intensive stroke unit reduces functional disability and the need for long-term hospitalization. Stroke 1985, 16, 29–34. [Google Scholar] [CrossRef] [PubMed]
- Collaboration Stroke Unit Trialists; Langhorne, P. Organised inpatient (stroke unit) care for stroke. Cochrane Database Syst. Rev. 2001, 3, CD000197. [Google Scholar] [CrossRef]
- Clarke, D.; Forster, A. Improving post-stroke recovery: The role of the multidisciplinary health care team. J. Multidiscip. Health 2015, 8, 433–442. [Google Scholar] [CrossRef]
- Clarke, D.J. The role of multidisciplinary team care in stroke rehabilitation. Prog. Neurol. Psychiatry 2013, 17, 5–8. [Google Scholar] [CrossRef]
- Rudd, A.G.; Wade, D.T.; Irwin, P. The National Clinical Guidelines for Stroke. J. R Coll. Physicians Lond. 2000, 34, 131–133. [Google Scholar]
- Askim, T.; Rohweder, G.; Lydersen, S.; Indredavik, B. Evaluation of an extended stroke unit service with early supported discharge for patients living in a rural community. A randomized controlled trial. Clin. Rehabil. 2004, 18, 238–248. [Google Scholar] [CrossRef] [PubMed]
- Fjærtoft, H.; Rohweder, G.; Indredavik, B. Stroke Unit Care Combined With Early Supported Discharge Improves 5-Year Outcome: A randomized controlled trial. Stroke 2011, 42, 1707–1711. [Google Scholar] [CrossRef]
- Sit, J.W.; Chair, S.Y.; Choi, K.C.; Chan, C.W.; Lee, D.T.; Chan, A.W.; Cheung, J.L.; Tang, S.W.; Chan, P.S.; Taylor-Piliae, R.E. Do empowered stroke patients perform better at self-management and functional recovery after a stroke? A randomized controlled trial. Clin. Interv. Aging 2016, 11, 1441–1450. [Google Scholar] [CrossRef] [PubMed]
- Wong, F.K.Y.; Yeung, S.M. Effects of a 4-week transitional care programme for discharged stroke survivors in Hong Kong: A randomised controlled trial. Health Soc. Care Community 2014, 23, 619–631. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Yang, F.; Shi, H.; Yang, C.; Hu, H. What Type of Transitional Care Effectively Reduced Mortality and Improved ADL of Stroke Patients? A Meta-Analysis. Int. J. Environ. Res. Public Health 2017, 14, 510. [Google Scholar] [CrossRef]
- Tseng, M.-C.; Lin, H.-J. Readmission after hospitalization for stroke in Taiwan: Results from a national sample. J. Neurol. Sci. 2009, 284, 52–55. [Google Scholar] [CrossRef]
- Miyai, I.; Sonoda, S.; Nagai, S.; Takayama, Y.; Inoue, Y.; Kakehi, A.; Kurihara, M.; Ishikawa, M. Results of New Policies for Inpatient Rehabilitation Coverage in Japan. Neurorehabilit. Neural Repair 2011, 25, 540–547. [Google Scholar] [CrossRef]
- Chiu, C.-C.; Wang, J.-J.; Hung, C.-M.; Lin, H.-F.; Hsien, H.-H.; Hung, K.-W.; Chiu, H.-C.; Yeh, S.-C.; Shi, H.-Y. Impact of Multidisciplinary Stroke Post-Acute Care on Cost and Functional Status: A Prospective Study Based on Propensity Score Matching. Brain Sci. 2021, 11, 161. [Google Scholar] [CrossRef]
- Bettger, J.A.P.; Kaltenbach, L.; Reeves, M.J.; Smith, E.E.; Fonarow, G.C.; Schwamm, L.H.; Peterson, E.D. Assessing Stroke Patients for Rehabilitation During the Acute Hospitalization: Findings From the Get With The Guidelines–Stroke Program. Arch. Phys. Med. Rehabil. 2013, 94, 38–45. [Google Scholar] [CrossRef]
- McKevitt, C.; Coshall, C.; Tilling, K.; Wolfe, C. Are There Inequalities in the Provision of Stroke Care? Stroke 2005, 36, 315–320. [Google Scholar] [CrossRef]
- Evenson, K.R.; Foraker, R.E.; Morris, D.L.; Rosamond, W.D. A Comprehensive Review of Prehospital and In-Hospital Delay Times in Acute Stroke Care. Int. J. Stroke 2009, 4, 187–199. [Google Scholar] [CrossRef] [PubMed]
- Mosley, I.; Nicol, M.; Donnan, G.; Thrift, A.G.; Dewey, H.M. What is Stroke Symptom Knowledge? Int. J. Stroke 2013, 9, 48–52. [Google Scholar] [CrossRef] [PubMed]
- Jiang, B.; Ru, X.; Sun, H.; Liu, H.; Sun, D.; Liu, Y.; Huang, J.; He, L.; Wang, W. Pre-hospital delay and its associated factors in first-ever stroke registered in communities from three cities in China. Sci. Rep. 2016, 6, 29795. [Google Scholar] [CrossRef] [PubMed]
- Ellis, C.; Barley, J.; Grubaugh, A. Poststroke Knowledge and Symptom Awareness: A Global Issue for Secondary Stroke Prevention. Cerebrovasc. Dis. 2013, 35, 572–581. [Google Scholar] [CrossRef]
- Phipps, M.S.; Cronin, C.A. Management of acute ischemic stroke. BMJ 2020, 368, l6983. [Google Scholar] [CrossRef]
- Saver, J.L.; Smith, E.E.; Fonarow, G.C.; Reeves, M.J.; Zhao, X.; Olson, D.M.; Schwamm, L.H.; Committee, G.W.-S.S.; Investigators. The “golden hour” and acute brain ischemia: Presenting features and lytic therapy in >30,000 patients arriving within 60 minutes of stroke onset. Stroke 2010, 41, 1431–1439. [Google Scholar] [CrossRef]
- Harbison, J.; Hossain, O.; Jenkinson, D.; Davis, J.; Louw, S.J.; Ford, G.A. Diagnostic Accuracy of Stroke Referrals From Primary Care, Emergency Room Physicians, and Ambulance Staff Using the Face Arm Speech Test. Stroke 2003, 34, 71–76. [Google Scholar] [CrossRef]
- Stroebele, N.; Müller-Riemenschneider, F.; Nolte, C.H.; Müller-Nordhorn, J.; Bockelbrink, A.; Willich, S.N. Knowledge of Risk Factors, and Warning Signs of Stroke: A Systematic Review from a Gender Perspective. Int. J. Stroke 2011, 6, 60–66. [Google Scholar] [CrossRef]
- Soto-Cámara, R.; González-Bernal, J.J.; González-Santos, J.; Aguilar-Parra, J.M.; Trigueros, R.; López-Liria, R. Knowledge on Signs and Risk Factors in Stroke Patients. J. Clin. Med. 2020, 9, 2557. [Google Scholar] [CrossRef]
- Dearborn, J.L.; McCullough, L.D. Perception of Risk and Knowledge of Risk Factors in Women at High Risk for Stroke. Stroke 2009, 40, 1181–1186. [Google Scholar] [CrossRef]
- Lundelin, K.; Graciani, A.; García-Puig, J.; Guallar-Castillón, P.; Taboada, J.M.; Rodríguez-Artalejo, F.; Banegas, J.R. Knowledge of Stroke Warning Symptoms and Intended Action in Response to Stroke in Spain: A Nationwide Population-Based Study. Cerebrovasc. Dis. 2012, 34, 161–168. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, A.; Czlonkowska, A.; Ford, G.A.; Fonseca, A.C.; Luijckx, G.J.; Korv, J.; de la Ossa, N.P.; Price, C.; Russell, D.; Tsiskaridze, A.; et al. European Academy of Neurology and European Stroke Organization consensus statement and practical guidance for pre-hospital management of stroke. Eur. J. Neurol. 2017, 25, 425–433. [Google Scholar] [CrossRef] [PubMed]
- Neau, J.-P.; Ingrand, P.; Godeneche, G. Awareness within the French population concerning stroke signs, symptoms, and risk factors. Clin. Neurol. Neurosurg. 2009, 111, 659–664. [Google Scholar] [CrossRef] [PubMed]
- Krzystanek, E.; Krzak-Kubica, A.; Świat, M.; Galus, W.; Gawryluk, J. Adequate Knowledge of Stroke Symptoms, Risk Factors, and Necessary Actions in the General Population of Southern Poland. Brain Sci. 2020, 10, 1009. [Google Scholar] [CrossRef]
- Paul, C.L.; Ryan, A.; Rose, S.; Attia, J.R.; Kerr, E.; Koller, C.; Levi, C.R. How can we improve stroke thrombolysis rates? A review of health system factors and approaches associated with thrombolysis administration rates in acute stroke care. Implement. Sci. 2015, 11, 1–12. [Google Scholar] [CrossRef]
- Fassbender, K.; Walter, S.; Grunwald, I.Q.; Merzou, F.; Mathur, S.; Lesmeister, M.; Liu, Y.; Bertsch, T.; Grotta, J.C. Prehospital stroke management in the thrombectomy era. Lancet Neurol. 2020, 19, 601–610. [Google Scholar] [CrossRef]
- Terecoasă, E.O.; Radu, R.A.; Negrilă, A.; Enache, I.; Cășaru, B.; Tiu, C. Pre-Hospital Delay in Acute Ischemic Stroke Care: Current Findings and Future Perspectives in a Tertiary Stroke Center from Romania—A Cross-Sectional Study. Medicina 2022, 58, 1003. [Google Scholar] [CrossRef]
- Nelson, R.F.; Pullicino, P.; Kendall, B.E.; Marshall, J. Computed tomography in patients presenting with lacunar syndromes. Stroke 1980, 11, 256–261. [Google Scholar] [CrossRef]
- Rothrock, J.F.; Lyden, P.D.; Hesselink, J.R.; Brown, J.J.; Healy, M.E. Brain magnetic resonance imaging in the evaluation of lacunar stroke. Stroke 1987, 18, 781–786. [Google Scholar] [CrossRef]
- Noguchi, K.; Nagayoshi, T.; Watanabe, N.; Kanazawa, T.; Toyoshima, S.; Morijiri, M.; Shojaku, H.; Shimizu, M.; Seto, H. Diffusion-weighted echo-planar MRI of lacunar infarcts. Neuroradiology 1998, 40, 448–451. [Google Scholar] [CrossRef]
- Schonewille, W.J.; Tuhrim, S.; Singer, M.B.; Atlas, S.W. Diffusion-Weighted MRI in Acute Lacunar Syndromes. A clinical-radiological correlation study. Stroke 1999, 30, 2066–2069. [Google Scholar] [CrossRef] [PubMed]
- Ay, H.; Oliveira-Filho, J.; Buonanno, F.S.; Ezzeddine, M.; Schaefer, P.W.; Rordorf, G.; Schwamm, L.H.; Gonzalez, R.G.; Koroshetz, W.J. Diffusion-weighted imaging identifies a subset of lacunar infarction associated with embolic source. Stroke 1999, 30, 2644–2650. [Google Scholar] [CrossRef] [PubMed]
- Tan, M.Y.Q.; Singhal, S.; Ma, H.; Chandra, R.V.; Cheong, J.; Clissold, B.B.; Ly, J.; Srikanth, V.; Phan, T.G. Examining Subcortical Infarcts in the Era of Acute Multimodality CT Imaging. Front. Neurol. 2016, 7, 220. [Google Scholar] [CrossRef] [PubMed]
- Rudilosso, S.; Rodríguez-Vázquez, A.; Urra, X.; Arboix, A. The Potential Impact of Neuroimaging and Translational Research on the Clinical Management of Lacunar Stroke. Int. J. Mol. Sci. 2022, 23, 1497. [Google Scholar] [CrossRef] [PubMed]
- Arboix, A.; Massons, J.; García-Eroles, L.; Targa, C.; Comes, E.; Parra, O. Clinical predictors of lacunar syndrome not due to lacunar infarction. BMC Neurol. 2010, 10, 31. [Google Scholar] [CrossRef]
- Bang, O.Y. Advances in biomarker for stroke patients: From marker to regulator. Precis. Futur. Med. 2017, 1, 32–42. [Google Scholar] [CrossRef]
- Boyd, L.A.; Hayward, K.S.; Ward, N.S.; Stinear, C.M.; Rosso, C.; Fisher, R.J.; Carter, A.R.; Leff, A.P.; Copland, D.A.; Carey, L.M.; et al. Biomarkers of stroke recovery: Consensus-based core recommendations from the Stroke Recovery and Rehabilitation Roundtable. Int. J. Stroke 2017, 12, 480–493. [Google Scholar] [CrossRef]
- Jones, T.A.; Kleim, J.A.; Greenough, W.T. Synaptogenesis and dendritic growth in the cortex opposite unilateral sensorimotor cortex damage in adult rats: A quantitative electron microscopic examination. Brain Res. 1996, 733, 142–148. [Google Scholar] [CrossRef]
- Włodarczyk, L.; Cichon, N.; Saluk-Bijak, J.; Bijak, M.; Majos, A.; Miller, E. Neuroimaging Techniques as Potential Tools for Assessment of Angiogenesis and Neuroplasticity Processes after Stroke and Their Clinical Implications for Rehabilitation and Stroke Recovery Prognosis. J. Clin. Med. 2022, 11, 2473. [Google Scholar] [CrossRef]
- Puig, J.; Pedraza, S.; Blasco, G.; Daunis-I-Estadella, J.; Prats, A.; Prados, F.; Boada, I.; Castellanos, M.; Sánchez-González, J.; Remollo, S.; et al. Wallerian Degeneration in the Corticospinal Tract Evaluated by Diffusion Tensor Imaging Correlates with Motor Deficit 30 Days after Middle Cerebral Artery Ischemic Stroke. Am. J. Neuroradiol. 2010, 31, 1324–1330. [Google Scholar] [CrossRef]
- Lin, D.J.; Cloutier, A.M.; Erler, K.S.; Cassidy, J.M.; Snider, S.B.; Ranford, J.; Parlman, K.; Giatsidis, F.; Burke, J.F.; Schwamm, L.H.; et al. Corticospinal Tract Injury Estimated From Acute Stroke Imaging Predicts Upper Extremity Motor Recovery After Stroke. Stroke 2019, 50, 3569–3577. [Google Scholar] [CrossRef] [PubMed]
- Kang, M.; Jin, S.; Lee, D.; Cho, H. MRI Visualization of Whole Brain Macro- and Microvascular Remodeling in a Rat Model of Ischemic Stroke: A Pilot Study. Sci. Rep. 2020, 10, 4989. [Google Scholar] [CrossRef] [PubMed]
- Yanev, P.; Seevinck, P.R.; Rudrapatna, U.S.; Bouts, M.J.; van der Toorn, A.; Gertz, K.; Kronenberg, G.; Endres, M.; van Tilborg, G.A.; Dijkhuizen, R.M. Magnetic resonance imaging of local and remote vascular remodelling after experimental stroke. J. Cereb. Blood Flow Metab. 2016, 37, 2768–2779. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Torbey, M.T. Angiogenesis and Blood-Brain Barrier Permeability in Vascular Remodeling after Stroke. Curr. Neuropharmacol. 2020, 18, 1250–1265. [Google Scholar] [CrossRef] [PubMed]
- Almeida, S.R.M.; Vicentini, J.; Bonilha, L.; De Campos, B.M.; Casseb, R.F.; Min, L.L. Brain Connectivity and Functional Recovery in Patients With Ischemic Stroke. J. Neuroimaging 2016, 27, 65–70. [Google Scholar] [CrossRef]
- Puig, J.; Blasco, G.; Alberich-Bayarri, A.; Schlaug, G.; Deco, G.; Biarnes, C.; Navas-Martí, M.; Rivero, M.; Gich, J.; Figueras, J.; et al. Resting-State Functional Connectivity Magnetic Resonance Imaging and Outcome After Acute Stroke. Stroke 2018, 49, 2353–2360. [Google Scholar] [CrossRef]
- Blicher, J.U.; Near, J.; Næss-Schmidt, E.; Stagg, C.J.; Johansen-Berg, H.; Nielsen, J.F.; Østergaard, L.; Ho, Y.-C.L. GABA Levels Are Decreased After Stroke and GABA Changes During Rehabilitation Correlate With Motor Improvement. Neurorehabilit. Neural Repair 2014, 29, 278–286. [Google Scholar] [CrossRef]
- Mazibuko, N.; Tuura, R.O.; Sztriha, L.; O’daly, O.; Barker, G.J.; Williams, S.C.R.; O’Sullivan, M.; Kalra, L. Subacute Changes in N-Acetylaspartate (NAA) Following Ischemic Stroke: A Serial MR Spectroscopy Pilot Study. Diagnostics 2020, 10, 482. [Google Scholar] [CrossRef]
- Laaksonen, K.; Helle, L.; Parkkonen, L.; Kirveskari, E.; Mäkelä, J.P.; Mustanoja, S.; Tatlisumak, T.; Kaste, M.; Forss, N. Alterations in Spontaneous Brain Oscillations during Stroke Recovery. PLoS ONE 2013, 8, e61146. [Google Scholar] [CrossRef]
- Zappasodi, F.; Pasqualetti, P.; Rossini, P.M.; Tecchio, F. Acute Phase Neuronal Activity for the Prognosis of Stroke Recovery. Neural Plast. 2019, 2019, e1971875. [Google Scholar] [CrossRef]
- Stinear, C.M.; Byblow, W.D.; Ackerley, S.J.; Barber, P.A.; Smith, M.-C. Predicting Recovery Potential for Individual Stroke Patients Increases Rehabilitation Efficiency. Stroke 2017, 48, 1011–1019. [Google Scholar] [CrossRef]
- Jo, J.Y.; Lee, A.; Kim, M.S.; Park, E.; Chang, W.H.; Shin, Y.-I.; Kim, Y.-H. Prediction of Motor Recovery Using Quantitative Parameters of Motor Evoked Potential in Patients With Stroke. Ann. Rehabil. Med. 2016, 40, 806–815. [Google Scholar] [CrossRef] [PubMed]
- Pellicciari, M.C.; Bonnì, S.; Ponzo, V.; Cinnera, A.M.; Mancini, M.; Casula, E.P.; Sallustio, F.; Paolucci, S.; Caltagirone, C.; Koch, G. Dynamic reorganization of TMS-evoked activity in subcortical stroke patients. NeuroImage 2018, 175, 365–378. [Google Scholar] [CrossRef]
- Zhu, H.; Zhang, Y.; Zhong, Y.; Ye, Y.; Hu, X.; Gu, L.; Xiong, X. Inflammation-Mediated Angiogenesis in Ischemic Stroke. Front. Cell Neurosci. 2021, 15, 652647. [Google Scholar] [CrossRef] [PubMed]
- Callewaert, B.; Jones, E.A.V.; Himmelreich, U.; Gsell, W. Non-Invasive Evaluation of Cerebral Microvasculature Using Pre-Clinical MRI: Principles, Advantages and Limitations. Diagnostics 2021, 11, 926. [Google Scholar] [CrossRef]
- Berge, E.; Whiteley, W.; Audebert, H.; De Marchis, G.M.; Fonseca, A.C.; Padiglioni, C.; de la Ossa, N.P.; Strbian, D.; Tsivgoulis, G.; Turc, G. European Stroke Organisation (ESO) guidelines on intravenous thrombolysis for acute ischaemic stroke. Eur. Stroke J. 2021, 6, I-LXII. [Google Scholar] [CrossRef] [PubMed]
- Eissa, A.; Krass, I.; Levi, C.; Sturm, J.; Ibrahim, R.; Bajorek, B. Understanding the reasons behind the low utilisation of thrombolysis in stroke. Australas. Med. J. 2013, 6, 152–167. [Google Scholar] [CrossRef] [PubMed]
- Psychogios, K.; Safouris, A.; Kargiotis, O.; Magoufis, G.; Andrikopoulou, A.; Papageorgiou, E.; Chondrogianni, M.; Papadimitropoulos, G.; Polyzogopoulou, E.; Spiliopoulos, S.; et al. Advanced Neuroimaging Preceding Intravenous Thrombolysis in Acute Ischemic Stroke Patients Is Safe and Effective. J. Clin. Med. 2021, 10, 2819. [Google Scholar] [CrossRef]
- Tsivgoulis, G.; Katsanos, A.H.; Schellinger, P.D.; Köhrmann, M.; Caso, V.; Palaiodimou, L.; Magoufis, G.; Arthur, A.; Fischer, U.; Alexandrov, A.V. Advanced Neuroimaging in Stroke Patient Selection for Mechanical Thrombectomy. Stroke 2018, 49, 3067–3070. [Google Scholar] [CrossRef]
- Nogueira, R.G.; Jadhav, A.P.; Haussen, D.C.; Bonafe, A.; Budzik, R.F.; Bhuva, P.; Yavagal, D.R.; Ribo, M.; Cognard, C.; Hanel, R.A.; et al. Thrombectomy 6 to 24 Hours after Stroke with a Mismatch between Deficit and Infarct. N. Engl. J. Med. 2018, 378, 11–21. [Google Scholar] [CrossRef]
- Albers, G.W.; Marks, M.P.; Kemp, S.; Christensen, S.; Tsai, J.P.; Ortega-Gutierrez, S.; McTaggart, R.A.; Torbey, M.T.; Kim-Tenser, M.; Leslie-Mazwi, T.; et al. Thrombectomy for Stroke at 6 to 16 Hours with Selection by Perfusion Imaging. N. Engl. J. Med. 2018, 378, 708–718. [Google Scholar] [CrossRef]
- Imran, R.; Mohamed, G.A.; Nahab, F. Acute Reperfusion Therapies for Acute Ischemic Stroke. J. Clin. Med. 2021, 10, 3677. [Google Scholar] [CrossRef] [PubMed]
- Dukelow, S.P.; Herter, T.M.; Bagg, S.D.; Scott, S.H. The independence of deficits in position sense and visually guided reaching following stroke. J. Neuroeng. Rehabil. 2012, 9, 72. [Google Scholar] [CrossRef] [PubMed]
- Otaka, E.; Otaka, Y.; Kasuga, S.; Nishimoto, A.; Yamazaki, K.; Kawakami, M.; Ushiba, J.; Liu, M. Reliability of the thumb localizing test and its validity against quantitative measures with a robotic device in patients with hemiparetic stroke. PLoS ONE 2020, 15, e0236437. [Google Scholar] [CrossRef] [PubMed]
- Fisher, G.; de Oliveira, C.Q.; Verhagen, A.; Gandevia, S.; Kennedy, D. Proprioceptive impairment in unilateral neglect after stroke: A systematic review. SAGE Open Med. 2020, 8, 2050312120951073. [Google Scholar] [CrossRef]
- Chilvers, M.J.; Hawe, R.L.; Scott, S.H.; Dukelow, S.P. Investigating the neuroanatomy underlying proprioception using a stroke model. J. Neurol. Sci. 2021, 430, 120029. [Google Scholar] [CrossRef] [PubMed]
- Hawe, R.L.; Findlater, S.E.; Kenzie, J.M.; Hill, M.D.; Scott, S.H.; Dukelow, S.P. Differential Impact of Acute Lesions Versus White Matter Hyperintensities on Stroke Recovery. J. Am. Heart Assoc. 2018, 7, e009360. [Google Scholar] [CrossRef]
- Kenzie, J.M.; Semrau, J.A.; Findlater, S.E.; Yu, A.Y.; Desai, J.A.; Herter, T.M.; Hill, M.D.; Scott, S.H.; Dukelow, S.P. Localization of Impaired Kinesthetic Processing Post-stroke. Front. Hum. Neurosci. 2016, 10, 505. [Google Scholar] [CrossRef]
- Findlater, S.E.; Desai, J.A.; Semrau, J.A.; Kenzie, J.M.; Rorden, C.; Herter, T.M.; Scott, S.H.; Dukelow, S.P. Central perception of position sense involves a distributed neural network—Evidence from lesion-behavior analyses. Cortex 2016, 79, 42–56. [Google Scholar] [CrossRef]
- Meyer, S.; Kessner, S.S.; Cheng, B.; Bönstrup, M.; Schulz, R.; Hummel, F.C.; De Bruyn, N.; Peeters, A.; Van Pesch, V.; Duprez, T.; et al. Voxel-based lesion-symptom mapping of stroke lesions underlying somatosensory deficits. NeuroImage Clin. 2016, 10, 257–266. [Google Scholar] [CrossRef]
- Feys, H.; De Weerdt, W.; Nuyens, G.; Van De Winckel, A.; Selz, B.; Kiekens, C. Predicting motor recovery of the upper limb after stroke rehabilitation: Value of a clinical examination. Physiother. Res. Int. 2000, 5, 1–18. [Google Scholar] [CrossRef]
- Chen, C.-L.; Tang, F.-T.; Chen, H.-C.; Chung, C.-Y.; Wong, M.-K. Brain lesion size and location: Effects on motor recovery and functional outcome in stroke patients. Arch. Phys. Med. Rehabil. 2000, 81, 447–452. [Google Scholar] [CrossRef] [PubMed]
- Chilvers, M.J.; Rajashekar, D.; Low, T.A.; Scott, S.H.; Dukelow, S.P. Clinical, Neuroimaging and Robotic Measures Predict Long-Term Proprioceptive Impairments following Stroke. Brain Sci. 2023, 13, 953. [Google Scholar] [CrossRef] [PubMed]
- Carvalho, A.; Cunha, A.; Rodrigues, M.; Figueiredo, S.; Paredes, L.; Gregório, T.; Morais, H.; Pinheiro, J.; Cruz, V.T.; Roriz, J.M.; et al. Mechanical Thrombectomy in Acute Ischemic Stroke: Initial Single-Center Experience and Comparison with Randomized Controlled Trials. J. Stroke Cerebrovasc. Dis. 2017, 26, 589–594. [Google Scholar] [CrossRef]
- Raha, O.; Hall, C.; Malik, A.; D’Anna, L.; Lobotesis, K.; Kwan, J.; Banerjee, S. Advances in mechanical thrombectomy for acute ischaemic stroke. BMJ Med. 2023, 2, e000407. [Google Scholar] [CrossRef]
- Jadhav, A.P.; Desai, S.M.; Jovin, T.G. Indications for Mechanical Thrombectomy for Acute Ischemic Stroke: Current Guidelines and Beyond. Neurology 2021, 97, S126–S136. [Google Scholar] [CrossRef]
- Moskowitz, M.A.; Lo, E.H.; Iadecola, C. The Science of Stroke: Mechanisms in Search of Treatments. Neuron 2010, 67, 181–198. [Google Scholar] [CrossRef] [PubMed]
- Yoo, A.J.; Pulli, B.; Gonzalez, R.G. Imaging-based treatment selection for intravenous and intra-arterial stroke therapies: A comprehensive review. Expert Rev. Cardiovasc. Ther. 2011, 9, 857–876. [Google Scholar] [CrossRef]
- Zemgulyte, G.; Tanaka, S.; Hide, I.; Sakai, N.; Pampuscenko, K.; Borutaite, V.; Rastenyte, D. Evaluation of the Effectiveness of Post-Stroke Metformin Treatment Using Permanent Middle Cerebral Artery Occlusion in Rats. Pharmaceuticals 2021, 14, 312. [Google Scholar] [CrossRef]
- Elkins, J.S.; Friedmanbc, C.; Boden-Albala, B.; Sacco, R.L.; Hripcsakc, G. Coding Neuroradiology Reports for the Northern Manhattan Stroke Study: A Comparison of Natural Language Processing and Manual Review. Comput. Biomed. Res. 2000, 33, 1–10. [Google Scholar] [CrossRef]
- Rivas, R.; Montazeri, N.; Le, N.X.; Hristidis, V. Automatic Classification of Online Doctor Reviews: Evaluation of Text Classifier Algorithms. J. Med. Internet Res. 2018, 20, e11141. [Google Scholar] [CrossRef] [PubMed]
- Heo, T.S.; Kim, Y.S.; Choi, J.M.; Jeong, Y.S.; Seo, S.Y.; Lee, J.H.; Jeon, J.P.; Kim, C. Prediction of Stroke Outcome Using Natural Language Processing-Based Machine Learning of Radiology Report of Brain MRI. J. Pers. Med. 2020, 10, 286. [Google Scholar] [CrossRef]
- Vagal, A.; Wintermark, M.; Nael, K.; Bivard, A.; Parsons, M.; Grossman, A.W.; Khatri, P. Automated CT perfusion imaging for acute ischemic stroke: Pearls and pitfalls for real-world use. Neurology 2019, 93, 888–898. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.; Mlynash, M.; Christensen, S.; Jiang, B.; Wintermark, M.; Sträter, R.; Broocks, G.; Grams, A.; Nikoubashman, O.; Morotti, A.; et al. Hyperacute Perfusion Imaging Before Pediatric Thrombectomy: Analysis of the Save ChildS Study. Neurology 2023, 100, e1148–e1158. [Google Scholar] [CrossRef] [PubMed]
- Haggenmüller, B.; Kreiser, K.; Sollmann, N.; Huber, M.; Vogele, D.; Schmidt, S.A.; Beer, M.; Schmitz, B.; Ozpeynirci, Y.; Rosskopf, J.; et al. Pictorial Review on Imaging Findings in Cerebral CTP in Patients with Acute Stroke and Its Mimics: A Primer for General Radiologists. Diagnostics 2023, 13, 447. [Google Scholar] [CrossRef]
- Psychogios, K.; Tsivgoulis, G. Intravenous thrombolysis for acute ischemic stroke: Why not? Curr. Opin. Neurol. 2021, 35, 10–17. [Google Scholar] [CrossRef] [PubMed]
- Beyeler, M.; Weber, L.; Kurmann, C.C.; Piechowiak, E.I.; Mosimann, P.J.; Zibold, F.; Meinel, T.R.; Branca, M.; Goeldlin, M.; Pilgram-Pastor, S.M.; et al. Association of reperfusion success and emboli in new territories with long term mortality after mechanical thrombectomy. J. NeuroInt. Surg. 2021, 14, 326–332. [Google Scholar] [CrossRef]
- Popiela, T.J.; Krzyściak, W.; Pilato, F.; Ligęzka, A.; Bystrowska, B.; Bukowska-Strakova, K.; Brzegowy, P.; Muthusamy, K.; Kozicz, T. The Assessment of Endovascular Therapies in Ischemic Stroke: Management, Problems and Future Approaches. J. Clin. Med. 2022, 11, 1864. [Google Scholar] [CrossRef]
- Pawłowski, K.; Dziadkiewicz, A.; Podlasek, A.; Klaudel, J.; Mączkowiak, A.; Szołkiewicz, M. Thrombectomy-Capable Stroke Centre—A Key to Acute Stroke Care System Improvement? Retrospective Analysis of Safety and Efficacy of Endovascular Treatment in Cardiac Cathlab. Int. J. Environ. Res. Public Health 2023, 20, 2232. [Google Scholar] [CrossRef]
- Sato, H.; Mitsui, N.; Fujikawa, S.; Kinoshita, M.; Hori, K.; Uebayashi, M.; Kimura, T. Critical evaluation of the modified Rankin Scale for assessment of the efficacy of mechanical thrombectomy: A retrospective comparison between the modified Rankin Scale and functional independence measure. Interv. Neuroradiol. 2023. [Google Scholar] [CrossRef]
- Yeo, M.; Tahayori, B.; Kok, H.K.; Maingard, J.; Kutaiba, N.; Russell, J.; Thijs, V.; Jhamb, A.; Chandra, R.V.; Brooks, M.; et al. Evaluation of techniques to improve a deep learning algorithm for the automatic detection of intracranial haemorrhage on CT head imaging. Eur. Radiol. Exp. 2023, 7, 17. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.-T.; Chen, Y.-L.; Chen, Y.-Y.; Huang, Y.-T.; Wong, H.-F.; Yan, J.-L.; Wang, J.-J. Deep Learning–Based Brain Computed Tomography Image Classification with Hyperparameter Optimization through Transfer Learning for Stroke. Diagnostics 2022, 12, 807. [Google Scholar] [CrossRef] [PubMed]
- Aho, K.; Harmsen, P.; Hatano, S.; Marquardsen, J.; Smirnov, V.E.; Strasser, T. Cerebrovascular disease in the community: Results of a WHO collaborative study. Bull. World Health Organ. 1980, 58, 113–130. [Google Scholar]
- Sacco, R.L.; Kasner, S.E.; Broderick, J.P.; Caplan, L.R.; Connors, J.J.; Culebras, A.; Elkind, M.S.; George, M.G.; Hamdan, A.D.; Higashida, R.T.; et al. An Updated Definition of Stroke for the 21st Century: A statement for healthcare professionals from the American heart association/American stroke association. Stroke 2013, 44, 2064–2089. [Google Scholar] [CrossRef]
- Iancu, A.; Buleu, F.; Chita, D.S.; Tutelca, A.; Tudor, R.; Brad, S. Early Hemorrhagic Transformation after Reperfusion Therapy in Patients with Acute Ischemic Stroke: Analysis of Risk Factors and Predictors. Brain Sci. 2023, 13, 840. [Google Scholar] [CrossRef] [PubMed]
- Ho-Tin-Noé, B.; Desilles, J.-P.; Mazighi, M. Thrombus composition and thrombolysis resistance in stroke. Res. Pr. Thromb. Haemost. 2023, 7, 100178. [Google Scholar] [CrossRef] [PubMed]
- Gurewich, V. The sequential, complementary and synergistic activation of fibrin-bound plasminogen by tissue plasminogen activator and pro-urokinase. Fibrinolysis 1989, 3, 59–66. [Google Scholar] [CrossRef]
- van der Ende, N.A.M.; Roozenbeek, B.; Smagge, L.E.M.; Luijten, S.P.R.; Aerden, L.A.M.; Kraayeveld, P.; Wijngaard, I.R.v.D.; Nijeholt, G.J.L.; Hertog, H.M.D.; Flach, H.Z.; et al. Dual thrombolytic therapy with mutant pro-urokinase and small bolus alteplase for ischemic stroke (DUMAS): Study protocol for a multicenter randomized controlled phase II trial. Trials 2022, 23, 1–10. [Google Scholar] [CrossRef]
- Gurewich, V. Activation of Fibrin-Bound Plasminogen by Pro-Urokinase and Its Complementariness with That by Tissue Plasminogen Activator. Enzyme 1988, 40, 97–108. [Google Scholar] [CrossRef]
- Yang, Y.; Gu, B.; Xu, X.Y. In Silico Study of Different Thrombolytic Agents for Fibrinolysis in Acute Ischemic Stroke. Pharmaceutics 2023, 15, 797. [Google Scholar] [CrossRef]
- Choi, H.-Y.; Cho, Y.; Kim, W.; Minn, Y.-K.; Kang, G.-H.; Jang, Y.-S.; Lee, Y.; Kim, J.-G.; Kim, J.; Cho, Y.; et al. Analysis of Mortality in Intracerebral Hemorrhage Patients with Hyperacute Ischemic Stroke Treated Using Thrombolytic Therapy: A Nationwide Population-based Cohort Study in South Korea. J. Pers. Med. 2022, 12, 1260. [Google Scholar] [CrossRef] [PubMed]
- Nisar, T.; Hanumanthu, R.; Khandelwal, P. Symptomatic Intracerebral Hemorrhage after Intravenous Thrombolysis: Predictive Factors and Validation of Prediction Models. J. Stroke Cerebrovasc. Dis. 2019, 28, 104360. [Google Scholar] [CrossRef] [PubMed]
- Aamir, R.; Fyffe, C.; Korin, N.; Lawrence, D.A.; Su, E.J.; Kanapathipillai, M. Heparin and Arginine Based Plasmin Nanoformulation for Ischemic Stroke Therapy. Int. J. Mol. Sci. 2021, 22, 11477. [Google Scholar] [CrossRef] [PubMed]
- Knowland, D.; Arac, A.; Sekiguchi, K.J.; Hsu, M.; Lutz, S.E.; Perrino, J.; Steinberg, G.K.; Barres, B.A.; Nimmerjahn, A.; Agalliu, D. Stepwise Recruitment of Transcellular and Paracellular Pathways Underlies Blood-Brain Barrier Breakdown in Stroke. Neuron 2014, 82, 603–617. [Google Scholar] [CrossRef] [PubMed]
- Shibata, K.; Hashimoto, T.; Miyazaki, T.; Miyazaki, A.; Nobe, K. Thrombolytic Therapy for Acute Ischemic Stroke: Past and Future. Curr. Pharm. Des. 2019, 25, 242–250. [Google Scholar] [CrossRef] [PubMed]
- National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group. Tissue Plasminogen Activator for Acute Ischemic Stroke. N. Engl. J. Med. 1995, 333, 1581–1588. [Google Scholar] [CrossRef]
- Lindley, R.I.; Wardlaw, J.M.; Whiteley, W.N.; Cohen, G.; Blackwell, L.; Murray, G.D.; Sandercock, P.A.; Baigent, C.; Chadwick, D.; Tyrrell, P.; et al. Alteplase for Acute Ischemic Stroke: Outcomes by clinically important subgroups in the Third International. Stroke 2015, 46, 746–756. [Google Scholar] [CrossRef]
- Parsons, M.; Spratt, N.; Bivard, A.; Campbell, B.; Chung, K.; Miteff, F.; O’Brien, B.; Bladin, C.; McElduff, P.; Allen, C.; et al. A Randomized Trial of Tenecteplase versus Alteplase for Acute Ischemic Stroke. N. Engl. J. Med. 2012, 366, 1099–1107. [Google Scholar] [CrossRef]
- Yamaguchi, T.; Mori, E.; Minematsu, K.; Nakagawara, J.; Hashi, K.; Saito, I.; Shinohara, Y. Alteplase at 0.6 mg/kg for Acute Ischemic Stroke Within 3 Hours of Onset: Japan Alteplase Clinical Trial (J-ACT). Stroke 2006, 37, 1810–1815. [Google Scholar] [CrossRef]
- Campbell, B.C.; Mitchell, P.J.; Churilov, L.; Yassi, N.; Kleinig, T.J.; Dowling, R.J.; Yan, B.; Bush, S.J.; Dewey, H.M.; Thijs, V.; et al. Tenecteplase versus Alteplase before Thrombectomy for Ischemic Stroke. N. Engl. J. Med. 2018, 378, 1573–1582. [Google Scholar] [CrossRef]
- Sommer, K.N.; Bhurwani, M.M.S.; Mokin, M.; Ionita, C.N. Evaluation of challenges and limitations of mechanical thrombectomy using 3D printed neurovascular phantoms. Proc. SPIE Int. Soc. Opt. Eng. 2021, 11601, 53–62. [Google Scholar] [CrossRef]
- Gu, B.; Piebalgs, A.; Huang, Y.; Longstaff, C.; Hughes, A.D.; Chen, R.; Thom, S.A.; Xu, X.Y. Mathematical Modelling of Intravenous Thrombolysis in Acute Ischaemic stroke: Effects of Dose Regimens on Levels of Fibrinolytic Proteins and Clot Lysis Time. Pharmaceutics 2019, 11, 111. [Google Scholar] [CrossRef] [PubMed]
- Endres, M.; Dirnagl, U.; Moskowitz, M.A. Chapter 2 The ischemic cascade and mediators of ischemic injury. In Handbook of Clinical Neurology, in Stroke; Elsevier: Amsterdam, The Netherlands, 2008; Volume 92, pp. 31–41. [Google Scholar] [CrossRef]
- Tong, X.; Wang, Y.; Fiehler, J.; Bauer, C.T.; Jia, B.; Zhang, X.; Huo, X.; Luo, G.; Wang, A.; Pan, Y.; et al. Thrombectomy Versus Combined Thrombolysis and Thrombectomy in Patients With Acute Stroke: A Matched-Control Study. Stroke 2021, 52, 1589–1600. [Google Scholar] [CrossRef] [PubMed]
- Rha, J.-H.; Saver, J.L. The Impact of Recanalization on Ischemic Stroke Outcome. Stroke 2007, 38, 967–973. [Google Scholar] [CrossRef]
- Bhatia, R.; Hill, M.D.; Shobha, N.; Menon, B.; Bal, S.; Kochar, P.; Watson, T.; Goyal, M.; Demchuk, A.M. Low Rates of Acute Recanalization With Intravenous Recombinant Tissue Plasminogen Activator in Ischemic Stroke: Real-world experience and a call for action. Stroke 2010, 41, 2254–2258. [Google Scholar] [CrossRef]
- González, R.G.; Furie, K.L.; Goldmacher, G.V.; Smith, W.S.; Kamalian, S.; Payabvash, S.; Harris, G.J.; Halpern, E.F.; Koroshetz, W.J.; Camargo, E.C.; et al. Good outcome rate of 35% in IV-tPA-treated patients with computed tomography angiography confirmed severe anterior circulation occlusive stroke. Stroke 2013, 44, 3109–3113. [Google Scholar] [CrossRef]
- Iglesias-Rey, R.; Rodríguez-Yáñez, M.; Rodríguez-Castro, E.; Pumar, J.M.; Arias, S.; Santamaría, M.; López-Dequidt, I.; Hervella, P.; Correa-Paz, C.; Sobrino, T.; et al. Worse Outcome in Stroke Patients Treated with rt-PA Without Early Reperfusion: Associated Factors. Transl. Stroke Res. 2017, 9, 347–355. [Google Scholar] [CrossRef]
- Alonso-Alonso, M.L.; Pérez-Mato, M.; Sampedro-Viana, A.; Correa-Paz, C.; Ávila-Gómez, P.; Sobrino, T.; Campos, F.; Castillo, J.; Iglesias-Rey, R.; Hervella, P. Fibrin-Targeted Nanoparticles for Finding, Visualizing and Characterizing Blood Clots in Acute Ischemic Stroke. Pharmaceutics 2022, 14, 2156. [Google Scholar] [CrossRef]
- Adams, H.P.; Brott, T.G.; Furlan, A.J.; Gomez, C.R.; Grotta, J.; Helgason, C.M.; Kwiatkowski, T.; Lyden, P.D.; Marler, J.R.; Torner, J.; et al. Guidelines for Thrombolytic Therapy for Acute Stroke: A Supplement to the Guidelines for the Management of Patients With Acute Ischemic Stroke. A statement for healthcare professionals from a Special Writing Group of the Stroke Council, American Heart Association. Circulation 1996, 94, 1167–1174. [Google Scholar] [CrossRef]
- Frank, D.; Zlotnik, A.; Boyko, M.; Gruenbaum, B.F. The Development of Novel Drug Treatments for Stroke Patients: A Review. Int. J. Mol. Sci. 2022, 23, 5796. [Google Scholar] [CrossRef]
- Shah, P.P.; Szaflarski, J.P.; Allendorfer, J.; Hamilton, R.H. Induction of neuroplasticity and recovery in post-stroke aphasia by non-invasive brain stimulation. Front. Hum. Neurosci. 2013, 7, 888. [Google Scholar] [CrossRef] [PubMed]
- Cichon, N.; Wlodarczyk, L.; Saluk-Bijak, J.; Bijak, M.; Redlicka, J.; Gorniak, L.; Miller, E. Novel Advances to Post-Stroke Aphasia Pharmacology and Rehabilitation. J. Clin. Med. 2021, 10, 3778. [Google Scholar] [CrossRef] [PubMed]
- Chieffo, R.; Giatsidis, F.; Santangelo, R.; Alyagon, U.; Comola, M.; Zangen, A.; Comi, G.; Leocani, L. Repetitive Transcranial Magnetic Stimulation With H-Coil Coupled With Cycling for Improving Lower Limb Motor Function After Stroke: An Exploratory Study. Neuromodul. Technol. Neural Interface 2020, 24, 916–922. [Google Scholar] [CrossRef]
- Kim, W.-S.; Kwon, B.S.; Gil Seo, H.; Park, J.; Paik, N.-J. Low-Frequency Repetitive Transcranial Magnetic Stimulation Over Contralesional Motor Cortex for Motor Recovery in Subacute Ischemic Stroke: A Randomized Sham-Controlled Trial. Neurorehabilit. Neural Repair 2020, 34, 856–867. [Google Scholar] [CrossRef]
- Liu, Y.; Yin, M.; Luo, J.; Huang, L.; Zhang, S.; Pan, C.; Hu, X. Effects of transcranial magnetic stimulation on the performance of the activities of daily living and attention function after stroke: A randomized controlled trial. Clin. Rehabil. 2020, 34, 1465–1473. [Google Scholar] [CrossRef]
- Zanardi, R.; Poletti, S.; Prestifilippo, D.; Attanasio, F.; Barbini, B.; Colombo, C. Transcranial direct current stimulation: A novel approach in the treatment of vascular depression. Brain Stimul. 2020, 13, 1559–1565. [Google Scholar] [CrossRef]
- Power, J.D.; Schlaggar, B.L. Neural plasticity across the lifespan. Wiley Interdiscip. Rev. Dev. Biol. 2016, 6, e216. [Google Scholar] [CrossRef] [PubMed]
- Alia, C.; Spalletti, C.; Lai, S.; Panarese, A.; Lamola, G.; Bertolucci, F.; Vallone, F.; Di Garbo, A.; Chisari, C.; Micera, S.; et al. Neuroplastic Changes Following Brain Ischemia and their Contribution to Stroke Recovery: Novel Approaches in Neurorehabilitation. Front. Cell Neurosci. 2017, 11, 76. [Google Scholar] [CrossRef]
- Hatcher, J.F.; Dempsey, R.J. Citicoline: Neuroprotective mechanisms in cerebral ischemia. J. Neurochem. 2002, 80, 12–23. [Google Scholar] [CrossRef]
- Lim, C.-M.; Kim, S.-W.; Park, J.-Y.; Kim, C.; Yoon, S.H.; Lee, J.-K. Fluoxetine affords robust neuroprotection in the postischemic brain via its anti-inflammatory effect. J. Neurosci. Res. 2009, 87, 1037–1045. [Google Scholar] [CrossRef]
- Szelenberger, R.; Kostka, J.; Saluk-Bijak, J.; Miller, E. Pharmacological Interventions and Rehabilitation Approach for Enhancing Brain Self-repair and Stroke Recovery. Curr. Neuropharmacol. 2019, 18, 51–64. [Google Scholar] [CrossRef] [PubMed]
- O’Collins, V.E.; Macleod, M.R.; Donnan, G.A.; Horky, L.L.; van der Worp, B.H.; Howells, D.W. 1026 Experimental treatments in acute stroke. Ann. Neurol. 2006, 59, 467–477. [Google Scholar] [CrossRef] [PubMed]
- Goenka, L.; Satyanarayana, C.R.U.; George, M. Neuroprotective agents in Acute Ischemic Stroke—A Reality Check. BioMed. Pharmacother. 2018, 109, 2539–2547. [Google Scholar] [CrossRef] [PubMed]
- Ford, G.A. Clinical pharmacological issues in the development of acute stroke therapies. Br. J. Pharmacol. 2008, 153, S112–S119. [Google Scholar] [CrossRef]
- Frese, A.; Husstedt, I.; Ringelstein, E.; Evers, S. Pharmacologic Treatment of Central Post-Stroke Pain. Clin. J. Pain 2006, 22, 252–260. [Google Scholar] [CrossRef] [PubMed]
- Greener, J.; Enderby, P.; Whurr, R. Pharmacological treatment for aphasia following stroke. Cochrane Database Syst. Rev. 2001, 2001, CD000424. [Google Scholar] [CrossRef]
- Hackett, M.L.; Anderson, C.S.; House, A.O. Management of Depression After Stroke. Stroke 2005, 36, 1092–1097. [Google Scholar] [CrossRef]
- Ghozy, S.; Reda, A.; Varney, J.; Elhawary, A.S.; Shah, J.; Murry, K.; Sobeeh, M.G.; Nayak, S.S.; Azzam, A.Y.; Brinjikji, W.; et al. Neuroprotection in Acute Ischemic Stroke: A Battle Against the Biology of Nature. Front. Neurol. 2022, 13, 870141. [Google Scholar] [CrossRef]
- Cramer, S.C. Repairing the human brain after stroke. II. Restorative therapies. Ann. Neurol. 2008, 63, 549–560. [Google Scholar] [CrossRef]
- Chollet, F.; Tardy, J.; Albucher, J.-F.; Thalamas, C.; Berard, E.; Lamy, C.; Bejot, Y.; Deltour, S.; Jaillard, A.; Niclot, P.; et al. Fluoxetine for motor recovery after acute ischaemic stroke (FLAME): A randomised placebo-controlled trial. Lancet Neurol. 2011, 10, 123–130. [Google Scholar] [CrossRef]
- Chollet, F.; Albucher, J.-F. Strategies to Augment Recovery After Stroke. Curr. Treat. Opt. Neurol. 2012, 14, 531–540. [Google Scholar] [CrossRef] [PubMed]
- Miyauchi, J.T.; Tsirka, S.E. Advances in immunotherapeutic research for glioma therapy. J. Neurol. 2017, 265, 741–756. [Google Scholar] [CrossRef] [PubMed]
- Lattanzi, S.; Norata, D.; Divani, A.A.; Di Napoli, M.; Broggi, S.; Rocchi, C.; Ortega-Gutierrez, S.; Mansueto, G.; Silvestrini, M. Systemic Inflammatory Response Index and Futile Recanalization in Patients with Ischemic Stroke Undergoing Endovascular Treatment. Brain Sci. 2021, 11, 1164. [Google Scholar] [CrossRef] [PubMed]
- Rabinstein, A.A. Update on Treatment of Acute Ischemic Stroke. Contin. Lifelong Learn. Neurol. 2020, 26, 268–286. [Google Scholar] [CrossRef]
- Pagiola, I.; Chassin, O.; Gallas, S.; Riviere, M.S.; Legris, N.; Mihalea, C.; Caroff, J.; Ikka, L.; Chalumeau, V.; de Aguiar, G.B.; et al. Extending the stroke treatment window beyond DAWN in patients with very slow progressor type collaterals: How far can we go? J. Cerebrovasc. Endovasc. Neurosurg. 2021, 23, 354–358. [Google Scholar] [CrossRef]
- de Castro-Afonso, L.H.; Abud, T.G.; Pontes-Neto, O.M.; Monsignore, L.M.; Nakiri, G.S.; Cougo-Pinto, P.T.; de Oliveira, L.; dos Santos, D.; Dias, F.A.; Fábio, S.C.R.; et al. Mechanical thrombectomy with solitaire stent retrieval for acute ischemic stroke in a Brazilian population. Clinics 2012, 67, 1379–1386. [Google Scholar] [CrossRef]
- Gupta, V.; Parthasarathy, R. Mechanical Thrombectomy: Answering Unanswered. Ann. Indian Acad. Neurol. 2019, 23, 13–19. [Google Scholar] [CrossRef]
- Derex, L.; Cho, T.-H. Mechanical thrombectomy in acute ischemic stroke. Rev. Neurol. 2017, 173, 106–113. [Google Scholar] [CrossRef]
- Krishnan, R.; Mays, W.; Elijovich, L. Complications of Mechanical Thrombectomy in Acute Ischemic Stroke. Neurology 2021, 97, S115–S125. [Google Scholar] [CrossRef]
- Kim, H.Y.; Bin Back, D.; Choi, B.-R.; Choi, D.-H.; Kwon, K.J. Rodent Models of Post-Stroke Dementia. Int. J. Mol. Sci. 2022, 23, 10750. [Google Scholar] [CrossRef]
- Chin, Y.; Kishi, M.; Sekino, M.; Nakajo, F.; Abe, Y.; Terazono, Y.; Hiroyuki, O.; Kato, F.; Koizumi, S.; Gachet, C.; et al. Involvement of glial P2Y1 receptors in cognitive deficit after focal cerebral stroke in a rodent model. J. Neuroinflamm. 2013, 10, 95. [Google Scholar] [CrossRef] [PubMed]
- Ward, R.; Valenzuela, J.P.; Li, W.; Dong, G.; Fagan, S.C.; Ergul, A. Poststroke cognitive impairment and hippocampal neurovascular remodeling: The impact of diabetes and sex. Am. J. Physiol. Circ. Physiol. 2018, 315, H1402–H1413. [Google Scholar] [CrossRef] [PubMed]
- Lin, J.; Frontera, J.A. Decompressive Hemicraniectomy for Large Hemispheric Strokes. Stroke 2021, 52, 1500–1510. [Google Scholar] [CrossRef] [PubMed]
- Scott, R.M.; Smith, E.R. Moyamoya Disease and Moyamoya Syndrome. N. Engl. J. Med. 2009, 360, 1226–1237. [Google Scholar] [CrossRef] [PubMed]
- Canavero, I.; Vetrano, I.G.; Zedde, M.; Pascarella, R.; Gatti, L.; Acerbi, F.; Nava, S.; Ferroli, P.; Parati, E.A.; Bersano, A. Clinical Management of Moyamoya Patients. J. Clin. Med. 2021, 10, 3628. [Google Scholar] [CrossRef]
- Fukui, M. Guidelines for the diagnosis and treatment of spontaneous occlusion of the circle of Willis (‘moyamoya’ disease). Research Committee on Spontaneous Occlusion of the Circle of Willis (Moyamoya Disease) of the Ministry of Health and Welfare, Japan. Clin. Neurol. Neurosurg. 1997, 99 (Suppl. 2), S238–S240. [Google Scholar] [CrossRef]
- Miyamoto, S.; Yoshimoto, T.; Hashimoto, N.; Okada, Y.; Tsuji, I.; Tominaga, T.; Nakagawara, J.; Takahashi, J.C.; Yamada, K.; Tomata, Y.; et al. Effects of Extracranial–Intracranial Bypass for Patients With Hemorrhagic Moyamoya Disease: Results of the Japan Adult Moyamoya Trial. Stroke 2014, 45, 1415–1421. [Google Scholar] [CrossRef]
- Takahashi, J.C.; Funaki, T.; Houkin, K.; Inoue, T.; Ogasawara, K.; Nakagawara, J.; Kuroda, S.; Yamada, K.; Miyamoto, S.; Yoshimoto, T.; et al. Significance of the Hemorrhagic Site for Recurrent Bleeding: Prespecified Analysis in the Japan Adult Moyamoya Trial. Stroke 2016, 47, 37–43. [Google Scholar] [CrossRef]
- Haynes, M.S.; Alder, K.D.; Bellamkonda, K.; Kuzomunhu, L.; Grauer, J.N. Incidence, predictors, and timing of post-operative stroke following elective total hip arthroplasty and total knee arthroplasty. PLoS ONE 2020, 15, e0239239. [Google Scholar] [CrossRef]
- Somnuke, P.; Kattiyawittayakul, K.; Wongyingsinn, M.; Raksakietisak, M. Incidence, risk factors and outcomes of early post-operative stroke in a university-based, tertiary care hospital: A 7-year retrospective case-control study. Medicine 2023, 102, e34363. [Google Scholar] [CrossRef]
- Powers, W.J.; Rabinstein, A.A.; Ackerson, T.; Adeoye, O.M.; Bambakidis, N.C.; Becker, K.; Biller, J.; Brown, M.; Demaerschalk, B.M.; Hoh, B.; et al. Guidelines for the Early Management of Patients With Acute Ischemic Stroke: 2019 Update to the 2018 Guidelines for the Early Management of Acute Ischemic Stroke: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke 2019, 50, e344–e418, Correction in Stroke 2019, 50, e440–e441. [Google Scholar] [CrossRef] [PubMed]
- Turc, G.; Bhogal, P.; Fischer, U.; Khatri, P.; Lobotesis, K.; Mazighi, M.; Schellinger, P.D.; Toni, D.; de Vries, J.; White, P.; et al. European Stroke Organisation (ESO)—European Society for Minimally Invasive Neurological Therapy (ESMINT) Guidelines on Mechanical Thrombectomy in Acute Ischaemic StrokeEndorsed by Stroke Alliance for Europe (SAFE). Eur. Stroke J. 2019, 4, 6–12. [Google Scholar] [CrossRef] [PubMed]
- Ansari, J.; Triay, R.; Kandregula, S.; Adeeb, N.; Cuellar, H.; Sharma, P. Endovascular Intervention in Acute Ischemic Stroke: History and Evolution. Biomedicines 2022, 10, 418. [Google Scholar] [CrossRef] [PubMed]
- Roaldsen, M.B.; Lindekleiv, H.; Mathiesen, E.B. Intravenous thrombolytic treatment and endovascular thrombectomy for ischaemic wake-up stroke. Cochrane Database Syst. Rev. 2021, 2021, CD010995. [Google Scholar] [CrossRef]
- Hankey, G.J. Stroke. Lancet 2016, 389, 641–654. [Google Scholar] [CrossRef]
- Savitz, S.I.; Baron, J.-C.; Fisher, M.; Albers, G.W.; Arbe-Barnes, S.; Boltze, J.; Broderick, J.; Broschat, K.O.; Elkind, M.S.V.; En’wezoh, D.; et al. Stroke Treatment Academic Industry Roundtable X: Brain Cytoprotection Therapies in the Reperfusion Era. Stroke 2019, 50, 1026–1031. [Google Scholar] [CrossRef]
- Fisher, M.; Savitz, S.I. Pharmacological brain cytoprotection in acute ischaemic stroke—Renewed hope in the reperfusion era. Nat. Rev. Neurol. 2022, 18, 193–202. [Google Scholar] [CrossRef]
- Chen, F.; Qi, Z.; Luo, Y.; Hinchliffe, T.; Ding, G.; Xia, Y.; Ji, X. Non-pharmaceutical therapies for stroke: Mechanisms and clinical implications. Prog. Neurobiol. 2014, 115, 246–269. [Google Scholar] [CrossRef]
- Wang, Y.; Meng, R.; Liu, G.; Cao, C.; Chen, F.; Jin, K.; Ji, X.; Cao, G. Intracranial atherosclerotic disease. Neurobiol. Dis. 2018, 124, 118–132. [Google Scholar] [CrossRef]
- Molina, C.A.; Montaner, J.; Abilleira, S.; Ibarra, B.; Romero, F.; Arenillas, J.F.; Alvarez-Sabín, J. Timing of Spontaneous Recanalization and Risk of Hemorrhagic Transformation in Acute Cardioembolic Stroke. Stroke 2001, 32, 1079–1084. [Google Scholar] [CrossRef]
- García-Cobos, R.; Frank-García, A.; Gutiérrez-Fernández, M.; Díez-Tejedor, E. Citicoline, use in cognitive decline: Vascular and degenerative. J. Neurol. Sci. 2010, 299, 188–192. [Google Scholar] [CrossRef] [PubMed]
- Álvarez-Sabín, J.; Román, G.C. The Role of Citicoline in Neuroprotection and Neurorepair in Ischemic Stroke. Brain Sci. 2013, 3, 1395–1414. [Google Scholar] [CrossRef] [PubMed]
- Stroke Unit Trialists’ Collaboration. Collaborative systematic review of the randomised trials of organised inpatient (stroke unit) care after stroke. BMJ 1997, 314, 1151–1159. [Google Scholar] [CrossRef]
- Campbell, B.C.V.; De Silva, D.A.; Macleod, M.R.; Coutts, S.B.; Schwamm, L.H.; Davis, S.M.; Donnan, G.A. Ischaemic stroke. Nat. Rev. Dis. Prim. 2019, 5, 70. [Google Scholar] [CrossRef]
- Hsieh, H.-C.; Liao, R.-D.; Yang, T.-H.; Leong, C.-P.; Tso, H.-H.; Wu, J.-Y.; Huang, Y.-C. The clinical effect of Kinesio taping and modified constraint-induced movement therapy on upper extremity function and spasticity in patients with stroke: A randomized controlled pilot study. Eur. J. Phys. Rehabil. Med. 2021, 57, 511–519. [Google Scholar] [CrossRef] [PubMed]
- Stoll, G.; Nieswandt, B. Thrombo-inflammation in acute ischaemic stroke—Implications for treatment. Nat. Rev. Neurol. 2019, 15, 473–481. [Google Scholar] [CrossRef] [PubMed]
- Schnieder, M.; Bähr, M.; Kirsch, M.; Maier, I.; Behme, D.; Riedel, C.H.; Psychogios, M.-N.; Brehm, A.; Liman, J.; von Arnim, C.A.F. Analysis of Frailty in Geriatric Patients as a Prognostic Factor in Endovascular Treated Patients with Large Vessel Occlusion Strokes. J. Clin. Med. 2021, 10, 2171. [Google Scholar] [CrossRef]
- Liu, X.; Dai, Q.; Ye, R.; Zi, W.; Liu, Y.; Wang, H.; Zhu, W.; Ma, M.; Yin, Q.; Li, M.; et al. Endovascular treatment versus standard medical treatment for vertebrobasilar artery occlusion (BEST): An open-label, randomised controlled trial. Lancet Neurol. 2020, 19, 115–122. [Google Scholar] [CrossRef]
- Levy, E.I.; Siddiqui, A.H.; Crumlish, A.; Snyder, K.V.; Hauck, E.F.; Fiorella, D.J.; Hopkins, L.N.; Mocco, J. First Food and Drug Administration-Approved Prospective Trial of Primary Intracranial Stenting for Acute Stroke: SARIS (stent-assisted recanalization in acute ischemic. Stroke 2009, 40, 3552–3556. [Google Scholar] [CrossRef]
- Hasan, T.F.; Hasan, H.; Kelley, R.E. Overview of Acute Ischemic Stroke Evaluation and Management. Biomedicines 2021, 9, 1486. [Google Scholar] [CrossRef]
- Meisel, C.; Schwab, J.M.; Prass, K.; Meisel, A.; Dirnagl, U. Central nervous system injury-induced immune deficiency syndrome. Nat. Rev. Neurosci. 2005, 6, 775–786. [Google Scholar] [CrossRef] [PubMed]
- Chamorro, A.; Urra, X.; Planas, A.M. Infection After Acute Ischemic Stroke: A manifestation of brain-induced immunodepression. Stroke 2007, 38, 1097–1103. [Google Scholar] [CrossRef] [PubMed]
- Vogelgesang, A.; Grunwald, U.; Langner, S.; Jack, R.; Bröker, B.M.; Kessler, C.; Dressel, A. Analysis of Lymphocyte Subsets in Patients With Stroke and Their Influence on Infection After Stroke. Stroke 2008, 39, 237–241. [Google Scholar] [CrossRef]
- Urra, X.; Cervera, Á.; Villamor, N.; Planas, A.; Chamorro, A. Harms and benefits of lymphocyte subpopulations in patients with acute stroke. Neuroscience 2009, 158, 1174–1183. [Google Scholar] [CrossRef] [PubMed]
- Brait, V.H.; Arumugam, T.V.; Drummond, G.R.; Sobey, C.G. Importance of T Lymphocytes in Brain Injury, Immunodeficiency, and Recovery after Cerebral Ischemia. J. Cereb. Blood Flow Metab. 2012, 32, 598–611. [Google Scholar] [CrossRef]
- Bi, Y.; Shen, J.; Chen, S.-C.; Chen, J.-X.; Xia, Y.-P. Prognostic value of neutrophil to lymphocyte ratio in acute ischemic stroke after reperfusion therapy. Sci. Rep. 2021, 11, 6177. [Google Scholar] [CrossRef]
- Lattanzi, S.; Cagnetti, C.; Provinciali, L.; Silvestrini, M. Neutrophil-to-lymphocyte ratio and neurological deterioration following acute cerebral hemorrhage. Oncotarget 2017, 8, 57489–57494. [Google Scholar] [CrossRef]
- de Mendivil, A.O.; Alcalá-Galiano, A.; Ochoa, M.; Salvador, E.; Millán, J.M. Brainstem Stroke: Anatomy, Clinical and Radiological Findings. Semin. Ultrasound CT MRI 2013, 34, 131–141. [Google Scholar] [CrossRef]
- Haddad, J.J.; Saadé, N.E.; Safieh-Garabedian, B. Cytokines and neuro–immune–endocrine interactions: A role for the hypothalamic–pituitary–adrenal revolving axis. J. Neuroimmunol. 2002, 133, 1–19. [Google Scholar] [CrossRef]
- Yeh, S.-J.; Huang, K.-Y.; Wang, T.-G.; Chen, Y.-C.; Chen, C.-H.; Tang, S.-C.; Tsai, L.-K.; Yip, P.-K.; Jeng, J.-S. Dysphagia screening decreases pneumonia in acute stroke patients admitted to the stroke intensive care unit. J. Neurol. Sci. 2011, 306, 38–41. [Google Scholar] [CrossRef]
- Shim, R.; Wong, C.H.Y. Ischemia, Immunosuppression and Infection—Tackling the Predicaments of Post-Stroke Complications. Int. J. Mol. Sci. 2016, 17, 64. [Google Scholar] [CrossRef] [PubMed]
- Suri, R.; Rodriguez-Porcel, F.; Donohue, K.; Jesse, E.; Lovera, L.; Dwivedi, A.K.; Espay, A.J. Post-stroke Movement Disorders: The Clinical, Neuroanatomic, and Demographic Portrait of 284 Published Cases. J. Stroke Cerebrovasc. Dis. 2018, 27, 2388–2397. [Google Scholar] [CrossRef]
- Thieme, H.; Mehrholz, J.; Pohl, M.; Behrens, J.; Dohle, C.; Morkisch, N.; Borgetto, B.; Winter, J.; Hunter, S.M.; Sim, J.; et al. Mirror Therapy for Improving Motor Function After Stroke. Stroke 2013, 44, e1–e2. [Google Scholar] [CrossRef] [PubMed]
- Lindenberg, R.; Renga, V.; Zhu, L.L.; Nair, D.; Schlaug, G. Bihemispheric brain stimulation facilitates motor recovery in chronic stroke patients. Neurology 2010, 75, 2176–2184. [Google Scholar] [CrossRef]
- Lo, A.C.; Guarino, P.D.; Richards, L.G.; Haselkorn, J.K.; Wittenberg, G.F.; Federman, D.G.; Ringer, R.J.; Wagner, T.H.; Krebs, H.I.; Volpe, B.T.; et al. Robot-Assisted Therapy for Long-Term Upper-Limb Impairment after Stroke. N. Engl. J. Med. 2010, 362, 1772–1783. [Google Scholar] [CrossRef]
- Wang, L.E.; Fink, G.R.; Diekhoff, S.; Rehme, A.K.; Eickhoff, S.B.; Grefkes, C. Noradrenergic enhancement improves motor network connectivity in stroke patients. Ann. Neurol. 2010, 69, 375–388. [Google Scholar] [CrossRef]
- Acler, M.; Robol, E.; Fiaschi, A.; Manganotti, P. A double blind placebo RCT to investigate the effects of serotonergic modulation on brain excitability and motor recovery in stroke patients. J. Neurol. 2009, 256, 1152–1158. [Google Scholar] [CrossRef] [PubMed]
- Pollock, A.; Baer, G.; Langhorne, P.; Pomeroy, V. Physiotherapy treatment approaches for the recovery of postural control and lower limb function following stroke: A systematic review. Clin. Rehabil. 2007, 21, 395–410. [Google Scholar] [CrossRef]
- Sütbeyaz, S.; Yavuzer, G.; Sezer, N.; Koseoglu, B.F. Mirror Therapy Enhances Lower-Extremity Motor Recovery and Motor Functioning After Stroke: A Randomized Controlled Trial. Arch. Phys. Med. Rehabil. 2007, 88, 555–559. [Google Scholar] [CrossRef]
- Doyle, S.; Bennett, S.; Fasoli, S.E.; McKenna, K.T. Interventions for sensory impairment in the upper limb after stroke. Cochrane Database Syst. Rev. 2010, 2010, CD006331. [Google Scholar] [CrossRef]
- Almekhlafi, M.; Kuczynski, A.; Demchuk, A. Therapeutic hypothermia: Applications in adults with acute ischemic stroke. Brain Circ. 2019, 5, 43–54. [Google Scholar] [CrossRef] [PubMed]
- Woodruff, T.M.; Thundyil, J.; Tang, S.-C.; Sobey, C.G.; Taylor, S.M.; Arumugam, T.V. Pathophysiology, treatment, and animal and cellular models of human ischemic stroke. Mol. Neurodegener. 2011, 6, 11. [Google Scholar] [CrossRef] [PubMed]
- Lees, T.; Shad-Kaneez, F.; Simpson, A.M.; Nassif, N.T.; Lin, Y.; Lal, S. Heart Rate Variability as a Biomarker for Predicting Stroke, Post-stroke Complications and Functionality. Biomark. Insights 2018, 13, 1177271918786931. [Google Scholar] [CrossRef] [PubMed]
- Hussain, I.; Park, S.-J. Quantitative Evaluation of Task-Induced Neurological Outcome after Stroke. Brain Sci. 2021, 11, 900. [Google Scholar] [CrossRef]
- Hussain, I.; Park, S.-J. Prediction of Myoelectric Biomarkers in Post-Stroke Gait. Sensors 2021, 21, 5334. [Google Scholar] [CrossRef]
- Onose, G.; Anghelescu, A.; Blendea, D.; Ciobanu, V.; Daia, C.; Firan, F.C.; Oprea, M.; Spinu, A.; Popescu, C.; Ionescu, A.; et al. Cellular and Molecular Targets for Non-Invasive, Non-Pharmacological Therapeutic/Rehabilitative Interventions in Acute Ischemic Stroke. Int. J. Mol. Sci. 2022, 23, 907. [Google Scholar] [CrossRef]
- Saunders, D.H.; Sanderson, M.; Hayes, S.; Johnson, L.; Kramer, S.; Carter, D.D.; Jarvis, H.; Brazzelli, M.; Mead, G.E. Physical fitness training for stroke patients. Cochrane Database Syst. Rev. 2020, 2020, CD003316. [Google Scholar] [CrossRef]
- Winstein, C.J.; Rose, D.K.; Tan, S.M.; Lewthwaite, R.; Chui, H.C.; Azen, S.P. A randomized controlled comparison of upper-extremity rehabilitation strategies in acute stroke: A pilot study of immediate and long-term outcomes. Arch. Phys. Med. Rehabil. 2004, 85, 620–628. [Google Scholar] [CrossRef]
- Kendall, B.J.; Gothe, N.P. Effect of Aerobic Exercise Interventions on Mobility among Stroke Patients: A Systematic Review. Am. J. Phys. Med. Rehabil. 2016, 95, 214–224. [Google Scholar] [CrossRef]
- Brunelli, S.; Iosa, M.; Fusco, F.R.; Pirri, C.; Di Giunta, C.; Foti, C.; Traballesi, M. Early body weight-supported overground walking training in patients with stroke in subacute phase compared to conventional physiotherapy: A randomized controlled pilot study. Int. J. Rehabil. Res. 2019, 42, 309–315. [Google Scholar] [CrossRef]
- Shahid, J.; Kashif, A.; Shahid, M.K. A Comprehensive Review of Physical Therapy Interventions for Stroke Rehabilitation: Impairment-Based Approaches and Functional Goals. Brain Sci. 2023, 13, 717. [Google Scholar] [CrossRef] [PubMed]
- Rost, N.S.; Brodtmann, A.; Pase, M.P.; van Veluw, S.J.; Biffi, A.; Duering, M.; Hinman, J.D.; Dichgans, M. Post-Stroke Cognitive Impairment and Dementia. Circ. Res. 2022, 130, 1252–1271. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.-Y.; Chen, S.-D.; Leng, X.-Y.; Kuo, K.; Wang, Z.-T.; Cui, M.; Tan, L.; Wang, K.; Dong, Q.; Yu, J.-T. Post-Stroke Cognitive Impairment: Epidemiology, Risk Factors, and Management. J. Alzheimer’s Dis. 2022, 86, 983–999. [Google Scholar] [CrossRef] [PubMed]
- Kalaria, R.N.; Akinyemi, R.; Ihara, M. Stroke injury, cognitive impairment and vascular dementia. Biochim. Biophys. Acta (BBA) Mol. Basis Dis. 2016, 1862, 915–925. [Google Scholar] [CrossRef]
- Hussain, A.; Lee, M.; Rana, J.; Virani, S.S. Epidemiology and risk factors for stroke in young individuals: Implications for prevention. Curr. Opin. Cardiol. 2021, 36, 565–571. [Google Scholar] [CrossRef]
- Furie, K. Epidemiology and Primary Prevention of Stroke. Contin. Lifelong Learn. Neurol. 2020, 26, 260–267. [Google Scholar] [CrossRef]
- Wu, S.; Wu, B.; Liu, M.; Chen, Z.; Wang, W.; Anderson, C.S.; Sandercock, P.; Wang, Y.; Huang, Y.; Cui, L.; et al. Stroke in China: Advances and challenges in epidemiology, prevention, and management. Lancet Neurol. 2019, 18, 394–405. [Google Scholar] [CrossRef]
- Caprio, F.Z.; Sorond, F.A. Cerebrovascular Disease: Primary and Secondary Stroke Prevention. Med. Clin. N. Am. 2018, 103, 295–308. [Google Scholar] [CrossRef]
- Feigin, V.L.; Krishnamurthi, R.V.; Parmar, P.; Norrving, B.; Mensah, G.A.; Bennett, D.A.; Barker-Collo, S.; Moran, A.E.; Sacco, R.L.; Truelsen, T.; et al. Update on the Global Burden of Ischemic and Hemorrhagic Stroke in 1990-2013: The GBD 2013 Study. Neuroepidemiology 2015, 45, 161–176. [Google Scholar] [CrossRef]
- Pandian, J.D.; Gall, S.L.; Kate, M.P.; Silva, G.S.; Akinyemi, R.O.; Ovbiagele, B.I.; Lavados, P.M.; Gandhi, D.B.C.; Thrift, A.G. Prevention of stroke: A global perspective. Lancet 2018, 392, 1269–1278. [Google Scholar] [CrossRef]
- Smith, A.C.; Bensink, M.; Armfield, N.; Stillman, J.; Caffery, L. Telemedicine and rural health care applications. J. Postgrad. Med. 2006, 51, 286–293. [Google Scholar]
- Matusitz, J.; Breen, G.-M. Telemedicine: Its Effects on Health Communication. Health Commun. 2007, 21, 73–83. [Google Scholar] [CrossRef] [PubMed]
- Baratloo, A.; Rahimpour, L.; Abushouk, A.I.; Safari, S.; Lee, C.W.; Abdalvand, A. Effects of Telestroke on Thrombolysis Times and Outcomes: A Meta-analysis. Prehospital Emerg. Care 2018, 22, 472–484. [Google Scholar] [CrossRef] [PubMed]
- Tchero, H.; Teguo, M.T.; Lannuzel, A.; Rusch, E. Telerehabilitation for Stroke Survivors: Systematic Review and Meta-Analysis. J. Med. Internet Res. 2018, 20, e10867. [Google Scholar] [CrossRef]
- Chae, S.H.; Kim, Y.; Lee, K.-S.; Park, H.-S. Development and Clinical Evaluation of a Web-Based Upper Limb Home Rehabilitation System Using a Smartwatch and Machine Learning Model for Chronic Stroke Survivors: Prospective Comparative Study. JMIR mHealth uHealth 2020, 8, e17216. [Google Scholar] [CrossRef]
- Donkor, E.S. Stroke in the21stCentury: A Snapshot of the Burden, Epidemiology, and Quality of Life. Stroke Res. Treat. 2018, 2018, 3238165. [Google Scholar] [CrossRef]
- Duncan, P.W.; Bushnell, C.; Sissine, M.; Coleman, S.; Lutz, B.J.; Johnson, A.M.; Radman, M.; Bettger, J.P.; Zorowitz, R.D.; Stein, J. Comprehensive Stroke Care and Outcomes: Time for a Paradigm Shift. Stroke 2021, 52, 385–393. [Google Scholar] [CrossRef]
- Bonaventura, A.; Liberale, L.; Vecchié, A.; Casula, M.; Carbone, F.; Dallegri, F.; Montecucco, F. Update on Inflammatory Biomarkers and Treatments in Ischemic Stroke. Int. J. Mol. Sci. 2016, 17, 1967. [Google Scholar] [CrossRef]
- Satani, N.; Savitz, S.I. Is Immunomodulation a Principal Mechanism Underlying How Cell-Based Therapies Enhance Stroke Recovery? Neurotherapeutics 2016, 13, 775–782. [Google Scholar] [CrossRef]
- Azodi, S.; Jacobson, S. Cytokine Therapies in Neurological Disease. Neurotherapeutics 2016, 13, 555–561. [Google Scholar] [CrossRef]
- Goyal, M.; Sutherland, G.R.; Lama, S.; Cimflova, P.; Kashani, N.; Mayank, A.; Psychogios, M.-N.; Spelle, L.; Costalat, V.; Sakai, N.; et al. Neurointerventional Robotics: Challenges and Opportunities. Clin. Neuroradiol. 2020, 30, 203–208. [Google Scholar] [CrossRef] [PubMed]
- Patel, T.M.; Shah, S.C.; Pancholy, S.B. Long Distance Tele-Robotic-Assisted Percutaneous Coronary Intervention: A Report of First-in-Human Experience. EClinicalMedicine 2019, 14, 53–58. [Google Scholar] [CrossRef] [PubMed]
- Zeleňák, K.; Krajina, A.; Meyer, L.; Fiehler, J.; ESMINT Artificial Intelligence and Robotics Ad hoc Committee; Behme, D.; Bulja, D.; Caroff, J.; Chotai, A.A.; Da Ros, V.; et al. How to Improve the Management of Acute Ischemic Stroke by Modern Technologies, Artificial Intelligence, and New Treatment Methods. Life 2021, 11, 488. [Google Scholar] [CrossRef]
- Liu, T.; Fan, W.; Wu, C. A hybrid machine learning approach to cerebral stroke prediction based on imbalanced medical dataset. Artif. Intell. Med. 2019, 101, 101723. [Google Scholar] [CrossRef]
- Kokkotis, C.; Giarmatzis, G.; Giannakou, E.; Moustakidis, S.; Tsatalas, T.; Tsiptsios, D.; Vadikolias, K.; Aggelousis, N. An Explainable Machine Learning Pipeline for Stroke Prediction on Imbalanced Data. Diagnostics 2022, 12, 2392. [Google Scholar] [CrossRef] [PubMed]
- Poona, N.K.; van Niekerk, A.; Nadel, R.L.; Ismail, R. Random Forest (RF) Wrappers for Waveband Selection and Classification of Hyperspectral Data. Appl. Spectrosc. 2016, 70, 322–333. [Google Scholar] [CrossRef]
- Yu, D.; Liu, Z.; Su, C.; Han, Y.; Duan, X.; Zhang, R.; Liu, X.; Yang, Y.; Xu, S. Copy number variation in plasma as a tool for lung cancer prediction using Extreme Gradient Boosting (XGBoost) classifier. Thorac. Cancer 2019, 11, 95–102. [Google Scholar] [CrossRef]
- Gkantzios, A.; Kokkotis, C.; Tsiptsios, D.; Moustakidis, S.; Gkartzonika, E.; Avramidis, T.; Aggelousis, N.; Vadikolias, K. Evaluation of Blood Biomarkers and Parameters for the Prediction of Stroke Survivors’ Functional Outcome upon Discharge Utilizing Explainable Machine Learning. Diagnostics 2023, 13, 532. [Google Scholar] [CrossRef]
- Sarvestany, S.S.; Kwong, J.C.; Azhie, A.; Dong, V.; Cerocchi, O.; Ali, A.F.; Karnam, R.S.; Kuriry, H.; Shengir, M.; Candido, E.; et al. Development and validation of an ensemble machine learning framework for detection of all-cause advanced hepatic fibrosis: A retrospective cohort study. Lancet Digit. Health 2022, 4, e188–e199. [Google Scholar] [CrossRef]
- Bos, J.M.; Attia, Z.I.; Albert, D.E.; Noseworthy, P.A.; Friedman, P.A.; Ackerman, M.J. Use of Artificial Intelligence and Deep Neural Networks in Evaluation of Patients With Electrocardiographically Concealed Long QT Syndrome From the Surface 12-Lead Electrocardiogram. JAMA Cardiol. 2021, 6, 532–538. [Google Scholar] [CrossRef]
- Chandrabhatla, A.S.; Pomeraniec, I.J.; Ksendzovsky, A. Co-evolution of machine learning and digital technologies to improve monitoring of Parkinson’s disease motor symptoms. Npj Digit. Med. 2022, 5, 32. [Google Scholar] [CrossRef] [PubMed]
- Thompson, A.C.; Jammal, A.A.; Berchuck, S.I.; Mariottoni, E.B.; Medeiros, F.A. Assessment of a Segmentation-Free Deep Learning Algorithm for Diagnosing Glaucoma From Optical Coherence Tomography Scans. JAMA Ophthalmol. 2020, 138, 333–339. [Google Scholar] [CrossRef] [PubMed]
- Sirsat, M.S.; Fermé, E.; Câmara, J. Machine Learning for Brain Stroke: A Review. J. Stroke Cerebrovasc. Dis. 2020, 29, 105162. [Google Scholar] [CrossRef] [PubMed]
- Mainali, S.; Darsie, M.E.; Smetana, K.S. Machine Learning in Action: Stroke Diagnosis and Outcome Prediction. Front. Neurol. 2021, 12, 734345. [Google Scholar] [CrossRef]
- Chavva, I.R.; Crawford, A.L.; Mazurek, M.H.; Yuen, M.M.; Prabhat, A.M.; Payabvash, S.; Sze, G.; Falcone, G.J.; Matouk, C.C.; de Havenon, A.; et al. Deep Learning Applications for Acute Stroke Management. Ann. Neurol. 2022, 92, 574–587. [Google Scholar] [CrossRef]
- Zhu, S.; Gilbert, M.; Chetty, I.; Siddiqui, F. The 2021 landscape of FDA-approved artificial intelligence/machine learning-enabled medical devices: An analysis of the characteristics and intended use. Int. J. Med. Inform. 2022, 165, 104828. [Google Scholar] [CrossRef]
- Chandrabhatla, A.S.; Kuo, E.A.; Sokolowski, J.D.; Kellogg, R.T.; Park, M.; Mastorakos, P. Artificial Intelligence and Machine Learning in the Diagnosis and Management of Stroke: A Narrative Review of United States Food and Drug Administration-Approved Technologies. J. Clin. Med. 2023, 12, 3755. [Google Scholar] [CrossRef]
- Suri, J.S.; Agarwal, S.; Gupta, S.K.; Puvvula, A.; Viskovic, K.; Suri, N.; Alizad, A.; El-Baz, A.; Saba, L.; Fatemi, M.; et al. Systematic Review of Artificial Intelligence in Acute Respiratory Distress Syndrome for COVID-19 Lung Patients: A Biomedical Imaging Perspective. IEEE J. Biomed. Health Inform. 2021, 25, 4128–4139. [Google Scholar] [CrossRef]
- Pal, D.; Reddy, P.B.; Roy, S. Attention UW-Net: A fully connected model for automatic segmentation and annotation of chest X-ray. Comput. Biol. Med. 2022, 150, 106083. [Google Scholar] [CrossRef]
- Jain, P.K.; Dubey, A.; Saba, L.; Khanna, N.N.; Laird, J.R.; Nicolaides, A.; Fouda, M.M.; Suri, J.S.; Sharma, N. Attention-Based UNet Deep Learning Model for Plaque Segmentation in Carotid Ultrasound for Stroke Risk Stratification: An Artificial Intelligence Paradigm. J. Cardiovasc. Dev. Dis. 2022, 9, 326. [Google Scholar] [CrossRef]
- Kaplan, P.W.; Rossetti, A.O. EEG Patterns and Imaging Correlations in Encephalopathy: Encephalopathy part II. J. Clin. Neurophysiol. 2011, 28, 233–251. [Google Scholar] [CrossRef]
- Islam, M.S.; Hussain, I.; Rahman, M.; Park, S.J.; Hossain, A. Explainable Artificial Intelligence Model for Stroke Prediction Using EEG Signal. Sensors 2022, 22, 9859. [Google Scholar] [CrossRef] [PubMed]
- Marsh, J.D.; Keyrouz, S.G. Stroke Prevention and Treatment. J. Am. Coll. Cardiol. 2010, 56, 683–691. [Google Scholar] [CrossRef] [PubMed]
- Shrestha, S.; Coy, S.; Bekelis, K. Oral Antiplatelet and Anticoagulant Agents in the Prevention and Management of Ischemic Stroke. Curr. Pharm. Des. 2017, 23, 1377–1391. [Google Scholar] [CrossRef] [PubMed]
- Hopkins, L.N. Blazing the Frontiers of Stroke Therapy. Neurosurgery 2019, 85, S1–S2. [Google Scholar] [CrossRef]
- Saqqur, M.; Uchino, K.; Demchuk, A.M.; Molina, C.A.; Garami, Z.; Calleja, S.; Akhtar, N.; Orouk, F.O.; Salam, A.; Shuaib, A.; et al. Site of Arterial Occlusion Identified by Transcranial Doppler Predicts the Response to Intravenous Thrombolysis for Stroke. Stroke 2007, 38, 948–954. [Google Scholar] [CrossRef] [PubMed]
- Sweid, A.; Hammoud, B.; Ramesh, S.; Wong, D.; Alexander, T.D.; Weinberg, J.H.; Deprince, M.; Dougherty, J.; Maamari, D.J.-M.; Tjoumakaris, S.; et al. Acute ischaemic stroke interventions: Large vessel occlusion and beyond. Stroke Vasc. Neurol. 2019, 5, 80–85. [Google Scholar] [CrossRef]
- Ma, Z.; Ding, N.; Yu, Y.; Ma, Y.; Yuan, X.; Wang, Y.; Zhao, Y.; Luan, J.; Liu, J. Quantification of cerebral vascular perfusion density via optical coherence tomography based on locally adaptive regional growth. Appl. Opt. 2018, 57, 10117–10124. [Google Scholar] [CrossRef]
- Yang, S.; Liu, K.; Ding, H.; Gao, H.; Zheng, X.; Ding, Z.; Xu, K.; Li, P. Longitudinal in vivo intrinsic optical imaging of cortical blood perfusion and tissue damage in focal photothrombosis stroke model. J. Cereb. Blood Flow Metab. 2018, 39, 1381–1393. [Google Scholar] [CrossRef]
- Liu, K.; Yin, M.; Cai, Z. Research and application advances in rehabilitation assessment of stroke. J. Zhejiang Univ. B 2022, 23, 625–641. [Google Scholar] [CrossRef]
- Kleinschnitz, C.; Fluri, F.; Schuhmann, M. Animal models of ischemic stroke and their application in clinical research. Drug Des. Dev. Ther. 2015, 9, 3445–3454. [Google Scholar] [CrossRef] [PubMed]
- Dichgans, M.; Pulit, S.L.; Rosand, J. Stroke genetics: Discovery, biology, and clinical applications. Lancet Neurol. 2019, 18, 587–599. [Google Scholar] [CrossRef] [PubMed]
- Herpich, F.; Rincon, F.M. Management of Acute Ischemic Stroke. Crit. Care Med. 2020, 48, 1654–1663. [Google Scholar] [CrossRef]
- Chidambaram, S.B.; Rathipriya, A.G.; Mahalakshmi, A.M.; Sharma, S.; Hediyal, T.A.; Ray, B.; Sunanda, T.; Rungratanawanich, W.; Kashyap, R.S.; Qoronfleh, M.W.; et al. The Influence of Gut Dysbiosis in the Pathogenesis and Management of Ischemic Stroke. Cells 2022, 11, 1239. [Google Scholar] [CrossRef]
- Kuriakose, D.; Xiao, Z. Pathophysiology and Treatment of Stroke: Present Status and Future Perspectives. Int. J. Mol. Sci. 2020, 21, 7609. [Google Scholar] [CrossRef] [PubMed]
- Guruswamy, R.; ElAli, A. Complex Roles of Microglial Cells in Ischemic Stroke Pathobiology: New Insights and Future Directions. Int. J. Mol. Sci. 2017, 18, 496. [Google Scholar] [CrossRef]
- Bonfanti, L.; Charvet, C.J. Brain Plasticity in Humans and Model Systems: Advances, Challenges, and Future Directions. Int. J. Mol. Sci. 2021, 22, 9358. [Google Scholar] [CrossRef]
- Harpaz, D.; Eltzov, E.; Seet, R.C.; Marks, R.S.; Tok, A.I. Point-of-Care-Testing in Acute Stroke Management: An Unmet Need Ripe for Technological Harvest. Biosensors 2017, 7, 30. [Google Scholar] [CrossRef]
- Ganesh, A.; Barber, P.A. The Cognitive Sequelae of Transient Ischemic Attacks—Recent Insights and Future Directions. J. Clin. Med. 2022, 11, 2637. [Google Scholar] [CrossRef]
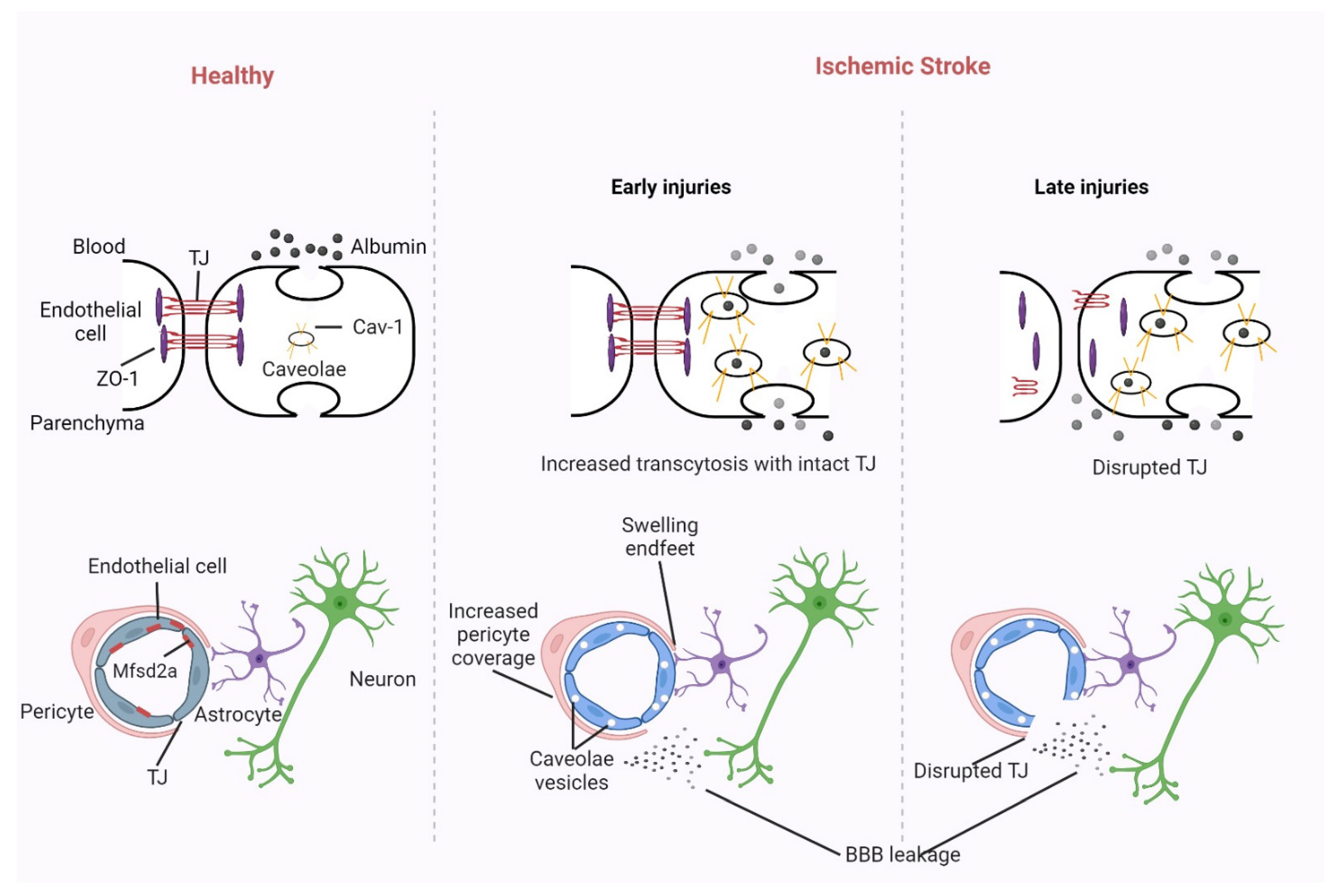

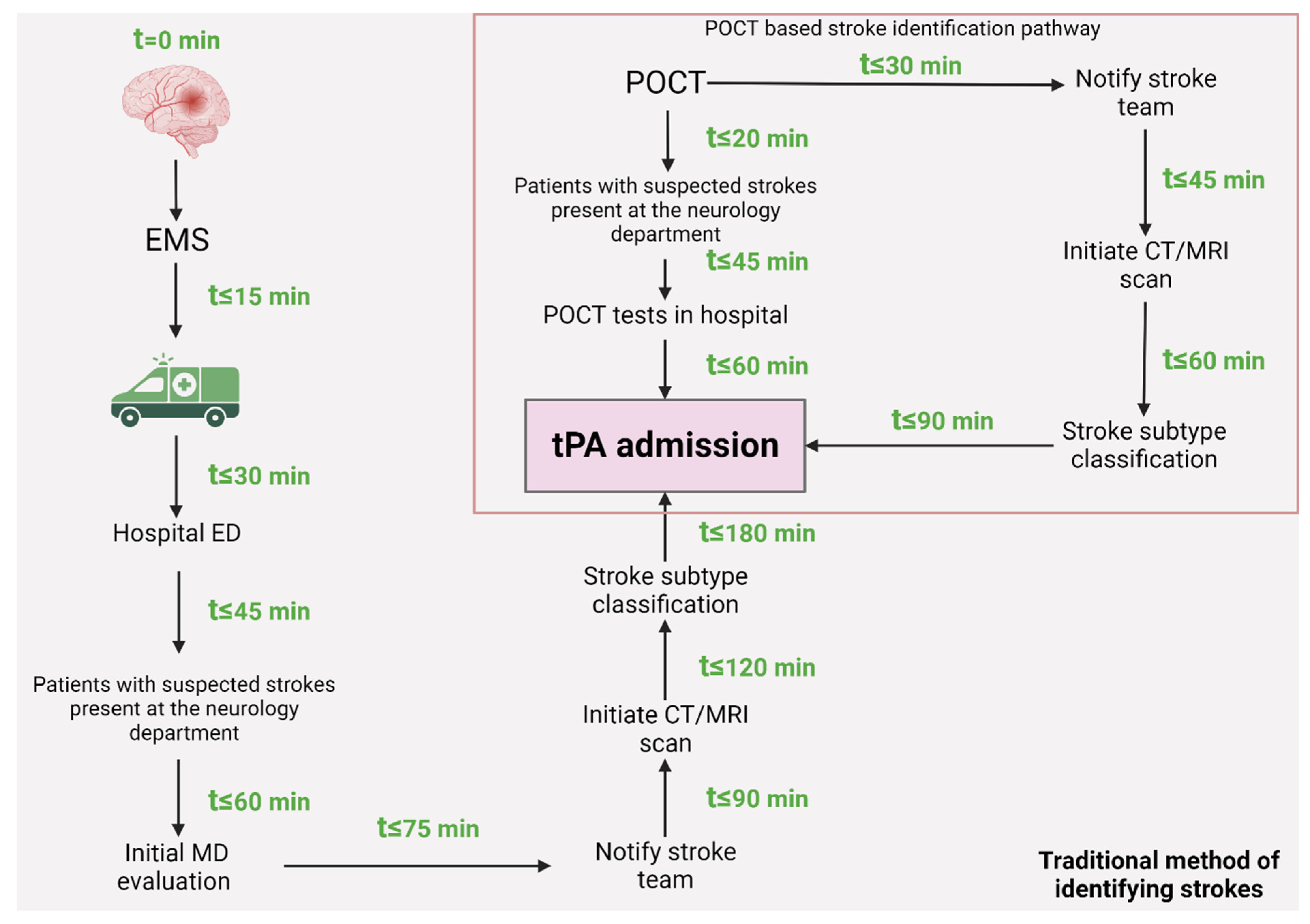
| Criteria/Stage | Cognitive Stage | Associative Stage | Automatic Stage | Citations |
|---|---|---|---|---|
| Primary Focus | In this stage of motor learning, the therapist helps the patient learn a piece of work. | Therapist assists the patient in task performance. | Patient is skilled and can perform tasks. | [280] |
| Decision Making | Decision making is based on “What to do?” | Decision making is based on “How to do a task?” | Decision making is based on “How to succeed?” | [281] |
| Task Execution | Learner constructs a motor program. | Patient performs and corrects errors; self-evaluation is promoted. | Complex and challenging tasks are performed to gain retention. | [254,280] |
| Self-evaluation and Feedback | Examine the task’s demands and his ability to complete it. | Continuity proven when error becomes consistent. | Select appropriate feedback. | [280,281] |
| Task Perception and Memory Recall | Identify the elements and recall the memory. | Emphasize the proprioception “feel of movement”. | Organize practice, self-evaluation and correction, gain retention. | [254,282] |
| Practice and Problem-solving | The patient then begins practicing the task, identifying and resolving problems. | Assist the learner with self-evaluation and decision-making skills. | Focus on the competitive aspect of the skills. | [280,281,282] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Saceleanu, V.M.; Toader, C.; Ples, H.; Covache-Busuioc, R.-A.; Costin, H.P.; Bratu, B.-G.; Dumitrascu, D.-I.; Bordeianu, A.; Corlatescu, A.D.; Ciurea, A.V. Integrative Approaches in Acute Ischemic Stroke: From Symptom Recognition to Future Innovations. Biomedicines 2023, 11, 2617. https://doi.org/10.3390/biomedicines11102617
Saceleanu VM, Toader C, Ples H, Covache-Busuioc R-A, Costin HP, Bratu B-G, Dumitrascu D-I, Bordeianu A, Corlatescu AD, Ciurea AV. Integrative Approaches in Acute Ischemic Stroke: From Symptom Recognition to Future Innovations. Biomedicines. 2023; 11(10):2617. https://doi.org/10.3390/biomedicines11102617
Chicago/Turabian StyleSaceleanu, Vicentiu Mircea, Corneliu Toader, Horia Ples, Razvan-Adrian Covache-Busuioc, Horia Petre Costin, Bogdan-Gabriel Bratu, David-Ioan Dumitrascu, Andrei Bordeianu, Antonio Daniel Corlatescu, and Alexandru Vlad Ciurea. 2023. "Integrative Approaches in Acute Ischemic Stroke: From Symptom Recognition to Future Innovations" Biomedicines 11, no. 10: 2617. https://doi.org/10.3390/biomedicines11102617
APA StyleSaceleanu, V. M., Toader, C., Ples, H., Covache-Busuioc, R.-A., Costin, H. P., Bratu, B.-G., Dumitrascu, D.-I., Bordeianu, A., Corlatescu, A. D., & Ciurea, A. V. (2023). Integrative Approaches in Acute Ischemic Stroke: From Symptom Recognition to Future Innovations. Biomedicines, 11(10), 2617. https://doi.org/10.3390/biomedicines11102617






