Abstract
Eosinophilic esophagitis (EoE) is an immune-mediated disease that manifests with dysphagia and is characterized by the predominantly eosinophilic infiltration of the esophageal mucosa. Several instruments have been developed to assess the symptoms of EoE: the Daily Symptom Questionnaire (DSQ), EoE Activity Index (EEsAI), Pediatric EoE Symptom Severity (PEESSv2), etc. The use of the EREFS is a gold standard for endoscopic diagnosis. The EoE histologic scoring system (EoEHSS) was elaborated for the assessment of histological features in EoE. However, the remission criteria are not clearly defined and vary greatly in different studies. Gastroenterologists establish the severity of EoE mainly based on endoscopic findings. At the same time, EoE requires a multidisciplinary approach. The recently developed Index of Severity of Eosinophilic Esophagitis (I-SEE) that is built on symptoms, endoscopic findings, and histological features is promising.
1. Introduction
Eosinophilic esophagitis (EoE) is an immune-mediated disease of the esophagus that manifests with dysphagia and is characterized by the predominantly eosinophilic infiltration of the esophageal mucosa (>15 eosinophils in high power field, eos/hpf) [1,2,3,4,5]. EoE is a chronic disease arising in predisposed individuals that often harbor one or several atopic conditions: bronchial asthma, atopic rhinitis, atopic dermatitis, eczema, etc. [6,7,8]. EoE may present with seasonal exacerbations due to aeroallergen exposure [9,10].
Almost half of the patients who were diagnosed in childhood do not have any symptoms 8 years after their diagnosis [11,12], though 2/3 of them did not receive drug therapy. At the same time, there is a risk of strictures increasing over time in patients who manifest in adulthood [13]. The more time that passes without treatment, the more the risk of strictures rises. Strictures were identified in 17% of patients that were diagnosed during 2 years from the first manifestation, in 31% of patients who were diagnosed 2–5 years after the first manifestation, in 38% patients with a delay in diagnosis for 8–11 years, in 64% of patients with a delay in diagnosis for 14–17 years, and in 71% of patients with a delay in diagnosis for more than 20 years. In another study, diagnostic delay for every year was associated with an increase in stricture presence for 9% [14]. Three phenotypes of the EoE were identified: inflammatory, mixed, and stenofibrotic [15]. The inflammatory phenotype was more common in young ages (13 vs. 29 vs. 39 years, respectively; p < 0.001), and dysphagia and food impaction were rare in this phenotype. Frequent symptoms included abdominal pain, vomiting, and failure to thrive. Individuals with the inflammatory phenotype more often reported atopy. The rate of stenosis increased with age (for every 10 years, the odds ratio of stenosis was 2.1 (95% CI, 1.7–2.7)). The risk of stenosis increased by 5% with every year of symptoms prior to the diagnosis. Therefore, EoE shows the progression from the inflammatory to stenofibrotic phenotype.
The treatment of EoE is focused on the induction of the sustained remission that implies not only the absence of symptoms, but the absence of histological features of the disease [16]. The management of EoE is based on diet and drug therapy that includes proton pump inhibitors (PPIs), topical steroids, and biological therapy (with antibodies to IL-4, IL-5, IL-13, etc.) [17,18,19,20,21]. Esophageal strictures can be successfully treated with dilation.
Diet therapy includes an elemental diet and empiric food elimination. An elemental diet represents drinking a special elemental formula consisting of amino acids, fats, sugars, vitamins, and nutrients. In a systematic review of six observational studies, an elemental diet was associated with histological remission (<15 eos/hpf) in 93.6% of patients compared to 13.3% in the placebo group (RR, 0.07; 95% CI, 0.05–0.12) [22]. The elemental diet intervention has the highest response rate compared to the other dietary interventions. However, this approach is costly, difficult to adhere to because of taste, and may be associated with the development of IgE-mediated food allergies during food reintroduction [23]. Empiric food elimination diets are based on the elimination of the most common foods causing the allergy-mediated inflammation of the esophagus in EoE. This approach includes a six-food elimination diet (SFED, with the elimination of milk, wheat, eggs, soy, peanuts/tree nuts, and fish/shellfish), a four-food elimination diet (restricting milk, wheat, legumes, and eggs), and other less restrictive diet regimes. SFED is the most studied approach, with a histological response in 67.9% of patients (<15 eos/hpf) compared to 13.3% in the placebo comparison group (RR 0.38; 95% CI, 0.32–0.43) in the systematic review [22]. Dietary adherence and the need for repeated endoscopies during food reintroduction are the main difficulties of this approach.
PPIs represent the first drug of choice in EoE because they are inexpensive, easy to administer, and have minimal side effects. High-dose PPI treatment led to the complete resolution of symptoms in 68% of patients, with EoE and histological remission (<15 eos/hpf) in 49% of patients [24]. In a systematic review of 23 observational studies with 1051 EoE patients, PPI therapy gave a histological response (<15 eos/hpf) in 41.7% of patients compared to 13.3% in the placebo group (RR, 0.66; 95% CI, 0.61–0.72) [22]. The mechanisms of action of PPIs in EoE are independent of gastric acid suppression and include the inhibition of immune cell function and the reduction in allergic Th2 inflammation, reduction in epithelial cell inflammatory cytokine expression, and the partial restoration of the integrity of the epithelial barrier [25,26,27,28].
Topical corticosteroids (TCS) are also widely used for the treatment of EoE. A systematic review of eight double-blind placebo-controlled clinical trials of TCS treatment that included 437 patients showed that TCS were associated with histologic remission in 64.9% of patients (<15 eos/hpf), compared to 13.3% in patients treated with the placebo (RR 0.39, 95% CI, 0.85–1.19) [22]. Budesonide orally disintegrating tablets (BOT) demonstrated the induction of histological and clinical remission in 90.1% and 75% of patients at 6 weeks, respectively [29]. Corticosteroids modulate the NF-kB inflammatory cascade and directly decrease the expression of eotaxin-3, thereby reducing the recruitment of eosinophils in the esophagus [30]. TCS are well tolerated. Side effects from TCS include oral or esophageal candidiasis [31] and exclusively rare adrenal insufficiency [32].
Severe esophageal structures and a narrow caliber esophagus need dilation. A meta-analysis of 27 studies with 845 EoE patients who underwent a total of 1820 esophageal dilations demonstrated that dilation improved dysphagia in 95% of patients following the procedure (95% CI = 90–98%) [33]. The complications included perforation, which occurred in 0.38% (95% CI: 0.18–0.85), hemorrhage, which occurred in 0.05% (95% CI: 0–0.3%), and hospitalization in 0.67% (95% CI: 0.3–1.1%). Another systematic review and meta-analysis of 37 studies including 977 patients with EoE that underwent 2034 dilations showed that dilation was associated with a perforation rate of 0.033% (95% CI, 0–0.226%), a bleeding rate of 0.028% (95% CI, 0–0.217%), and a hospitalization rate of 0.689% (95% CI 0–1.42%) [34]. At the same time, dilation does not have an impact of esophageal inflammation, but rather, it resolves dysphagia symptoms by widening the esophageal diameter. That is why ongoing esophageal inflammation and remodeling requires repeated dilations.
So, there are different therapeutic options to treat EoE. Nevertheless, the terms “clinical remission”, “endoscopic remission”, and “histological remission” define different entities and do not always coincide. For example, clinical symptoms may persist in patients with histological remission [35,36,37]. Currently, the medical community lacks a uniform definition and uniform criteria of the remission in EoE [18,38,39]. Different endpoints are used in different studies to detect the clinical efficacy of therapy. Different definitions of clinical, endoscopic, and histological remissions are reviewed in this article.
2. Clinical Symptom Assessment in EoE
The clinical symptoms of EoE vary in patients of different age groups [15,40,41,42]. In little children, they include feeding problems, food refusal, nausea, vomiting, and failure to thrive; older children complain of abdominal pain, vomiting/regurgitation, and heartburn and may present with weight loss. In children, pain may also lead to sleeping problems [43]. Dysphagia and food impaction prevail in teenagers and adults. Indeed, in adults, EoE is the most frequent reason for dysphagia and food impaction [44]. Food impaction requiring endoscopy is observed in 33–53% of adults with EoE [45].
It should be mentioned that EoE implies changes in eating behaviors that involves the use of coping mechanisms to avoid symptoms. Patients eat more slowly, chew excessively, take smaller pieces, imbibe fluids with meals, and avoid hard-textured foods [18]. The use of these coping mechanisms hampers the assessment of symptoms [39].
Several patient-reported outcomes were developed to evaluate the severity of symptoms of EoE and the response to the therapy [38]: Daily Symptom Questionnaire (DSQ) [32,46,47,48,49], EoE Activity Index (EEsAI) [50,51], Pediatric EoE Symptom Severity (PEESSv2) [52], etc. Dellon ES et al. [46] developed DSQ, which includes three questions for the identification of dysphagia: (1) did you eat solid food this day, (2) has food gone down slowly or been stuck, and (3) did you have to do anything to make the food go down or to get relief? The DSQ results showed a correlation with the number of dysphagia days (R = 0.96; p < 0.001) and the Straumann Dysphagia Instrument (SDI, R = 0.77; p < 0.001). The DSQ was successfully validated [47]. The treatment of the oral suspension of budesonide (BOS) resulted in a substantial decrease in DSQ (from 29.3 to 15.0 in the BOS group vs. from 29.0 to 21.5 in the placebo group, p = 0.0096) [48]. A decrease in DSQ ≥ 30% was a criterion of therapy efficacy [32,49]. The dysphagia symptom diary (DSD) [53] is a modification of the DSQ, which contains a fourth question about the presence and severity of pain during dysphagia. A decrease in the symptom score was more prominent in the group receiving 360 mg RPC4046 than in the placebo group.
The EEsAI [50] includes an evaluation of the following parameters: duration, frequency, and severity of dysphagia, pain when swallowing, a visual dysphagia question concerning food consistency, and behavioral adaptations (avoidance, modification, and slow eating of various foods). The optimal time of symptom recall was 7 days. The values of the EEsAI were greater in active EoE in terms of endoscopic and histological features. EEsAI ≤ 20 allowed for the identification of patients with endoscopic remission with an accuracy of 65.1% and for the identification of patients with histological remission (<20 eos/mm2, which corresponds with <5 eos/hpf) with an accuracy of 62.1% [37]. The EEsAI was successfully validated and was used in different studies [29,51,54,55,56,57,58].
The Straumann Dysphagia Instrument (SDI) is a nonvalidated questionnaire that rates the frequency and intensity of dysphagia from 0 to 9 points [59]. The SDI was used to show the efficacy of budesonide in EoE (SDI decreased from 5.61 to 2.22, p < 0.0001). The SDI was used to evaluate clinical response in other studies [54,60,61]. A decrease in the SDI > 3 points was the criterion of symptomatic remission.
The Dysphagia Symptom Score (DSS) is a nonvalidated questionnaire, reflecting the frequency, intensity, duration of symptoms, and presence of lifestyle changes [62,63]. The Mayo Dysphagia Questionnaire (MDQ) is a validated instrument for the assessment of dysphagia in esophageal diseases [64,65]. It was not developed for EoE, and in clinical studies [36,66], the assessment of symptoms using the MDQ did not show a correlation with the induction of histological remission. The results of dysphagia assessment using a visual analogous scale (VAS) demonstrated a correlation with the Likert scale (R = 0.77; p < 0.0001) and MDQ (R = 0.46, p = 0.001) [67].
PEESSv2 was developed for children and their parents [52], and it includes an assessment of the following parameters: chest pain, heartburn, abdominal pain, dysphagia/food impaction, vomiting, nausea, regurgitation, and poor appetite. The PEESSv2 dysphagia domain showed a correlation with biological signs of activity in EoE [68], with the expression of eosinophil peroxidase in both distal and proximal biopsies (ρ = 0.23–0.37, p = 0.019–0.17), and with the expression of the tryptase and chymase of mast cells (ρ = 0.34, p = 0.036 and ρ = 0.32, p = 0.041, respectively). Moreover, there was an association between dysphagia and the expression of CPA3 (ρ = 0.36, p = 0.02). A transcriptome analysis revealed that dysphagia was associated with the expression of genes related to eosinophilia, chemokines, mast cells, neurosensory, cytokines, and inflammation.
Other patient-reported outcomes include the symptom scoring tool (SST) [69,70] and clinical symptom score (CSS) [71]. The SST [69] represents seven questions for the identification of heartburn/regurgitation, abdominal pain, nocturnal awakening, nausea/vomiting, anorexia/early satiety, dysphagia/odynophagia, and gastrointestinal hemorrhage. Dysphagia and anorexia/early satiety were associated with EoE (odds ratio 15 (95% CI, 6–68), p < 0.001). Symptoms of dysphagia and anorexia/early satiety are also correlated with the average epithelial score (r = 0.32, p < 0.05). Dysphagia is correlated with the maximum lamina propria score (r = 0.45, p < 0.05). In a randomized placebo-controlled study, the use of oral viscous budesonide was associated with a decrease in the severity of symptoms measured by SST (p = 0.0007) [70].
The CSS [71] evaluates the following symptoms in points from 0 to 3: (1) heartburn, (2) abdominal pain, (3) nocturnal awakening due to the symptoms, (4) nausea, regurgitation, or vomiting, (5) anorexia or early satiety, and (6) dysphagia, odynophagia, or food impaction. The clinical response was defined as a decrease in CSS ≥ 50%, and clinical remission was defined as 0 points of CSS. An assessment of compensatory mechanisms is an advantage of CSS, although the use of CSS did not allow for the differentiation between the oral budesonide suspension group and the placebo group.
To sum up, there are different instruments to evaluate the symptoms of EoE (Table 1), but not all of them are responsive to treatment and correlate with histological remission. While the criteria of the response to treatment vary in different studies, an intuitive definition of remission should be the absence of symptoms. Nevertheless, the absence of symptoms does not designate the absence of biological activity of the disease [37]; therefore, there is a need for a complex evaluation of symptoms, endoscopic features, and histological findings.

Table 1.
Comparison of different instruments for symptom assessment in EoE.
3. Evaluation of Endoscopic Features in EoE
Endoscopic findings in EoE include linear furrows (in 48% of patients), esophageal rings (in 44% of patients), pallor/decreased vascularity (in 41% of patients), white plagues (in 27% of patients), strictures (in 21% of patients), and narrow-caliber esophagus (in 9% of patients) [72]. Rings and strictures are more often identified in adults (57% and 25%, respectively) than in children (11% and 8%, respectively, p < 0.05). Plagues and pallor/decreased vascularity are more often seen in children (36% and 58%, respectively) than in adults (19% and 18%, respectively, p < 0.05).
The gold standard of endoscopic evaluation in EoE implies the use of the Endoscopic Reference Score (EREFS), which includes the assessment of the following features: edema, rings, exudates, furrows, and strictures (Table 2) [73]. The EREFS showed a moderate level of interobserver agreement (κ for different features varies from 0.50 to 0.58, the proportion of pairwise agreement for experts and non-experts was 81% and 74% for exudates, 90% and 77% for edema, and 98% and 90% for crepe paper esophagus. In another study [74], interobserver agreement was substantial for rings (κ 0.70), white exudates (κ 0.63), and crepe paper esophagus (κ 0.62), moderate for furrows (κ 0.49) and strictures (κ 0.54), and slight for edema (κ 0.12). The EREFS classification system identifies patients with EoE in an area under the receiver operator characteristic curve of 0.934 [75]. The threshold of a score of 2 allowed for EoE to be diagnosed with a sensitivity of 88%, specificity of 92%, positive predictive value of 84%, negative predictive value of 94%, and accuracy of 91%. The EREFS score decreased after treatment, and a more prominent reduction was observed in patients with histological response (<15 eos/hpf).

Table 2.
EREFS score [73].
Rings, strictures, and crepe paper esophagus correspond to fibrotic lesions and exudates, while edema and furrows stand for inflammatory lesions [13,76]. Rodríguez-Sánchez J. et al. [63] showed that exudates (p = 0.03), furrows (p = 0.03), and inflammatory score (p < 0.001) predicted the histological activity of EoE, although only exudates correlated with histological response after treatment, while furrows and edema persisted in 50% and 70% patients with histological remission, respectively. Crepe paper esophagus, diffuse exudates, and severe rings correlated with a higher EREFS score.
Van Rhijn, 2016 [77] revealed that rings and furrows were more prominent in active EoE. Fibrotic scores (r = 0.28, p = 0.020), inflammatory scores (r = 0.27, p = 0.025), and total EREFS scores (r = 0.43, p < 0.001) correlated with the peak eosinophil count (PEC) in biopsies, although the reduction in PEC after treatment was not accompanied with the decrease in the EREFS score. Therefore, the predictive values of EREFS were not sufficient to predict the histological activity of the disease.
Chen J.W., 2016 [78] demonstrated that higher ring scores were associated with a lower distensibility plateau (rs = −0.46; p < 0.0001) and a higher risk of food impaction. Food impaction in anamnesis was observed in 20% patients with a ring score of 0, in 25% of patients with a ring score of 1, in 39% patients with a ring score of 2, and in 100% patients with a ring score of 3 (p = 0.002). The severity of exudates (r = 0.27; p = 0.02) and furrows (r = 0.49; p < 0.0001) correlated with the density of intraepithelial eosinophils in biopsies.
The detection of more than one EREFS feature identified children with EoE with 89.6% sensitivity and 87.9% [79]. The EREFS score correlated with PEC (p < 0.001). The EREFS score significantly reduced after treatment in children (2.4 vs. 0.7, p < 0.001) [79] and adults (3.88 vs. 2.01, p > 0.001) [75]. Therefore, EREFS is responsive to treatment. Moreover, the severity of endoscopic features is the main determinant of disease activity for gastroenterologists [80].
In most studies, the treatment results are described as a decrease in the EREFS score [32,48,49,53,54,57,58,60,75,79]. Safroneeva E. et al. [37] gave the following three definitions of endoscopic remission: endoscopic inflammatory remission, endoscopic fibrotic remission, and total endoscopic remission (inflammatory and fibrotic remission). Endoscopic inflammatory remission included the following: the absence of white exudates; furrows and edema may be present, but not in combination. Endoscopic fibrotic remission was defined as the absence of moderate and severe rings, and the absence of strictures. Total endoscopic remission included signs of both inflammatory and fibrotic remission. Greuter T. et al., 2019 [81] and Miehlke S. et al., 2022 [29] defined endoscopic remission as the absence of inflammatory features of EoE (exudates, furrows, and edema), while mild rings may be present. Thus, a uniform definition of endoscopic remission currently is not developed.
The functional lumen imaging probe (FLIP) evaluating distensibility plateau represents a technique to simultaneously measure the esophageal luminal cross-sectional area and distensive pressure during volume-controlled esophageal distension. Distensibility plateau was reduced in patients with EoE compared with asymptomatic controls [82]. A greater reduction in DP in patients with EoE was associated with the future risk for food impaction and/or requirement for therapeutic dilation [83]. That is why the distensibility plateau may reflect disease severity in EoE, and its improvement can be used as a measurement of clinical outcome.
4. Histological Criteria of the Remission in EoE
The diagnosis of EoE requires the presence of >15 eos/hpf [1,2,3]. However, the transitional eosinophilia of the esophageal mucosa may be attributed to caffeine exposure [84]. Currently, there is no uniform definition of the histological response to the treatment of EoE, and the histological criteria of the remission vary in different studies. Meanwhile, the development of uniform histological criterion of remission will allow for the results of treatment to be evaluated more objectively and to compare the results of different studies.
In some studies, the histological criterion of the remission is PEC < 15 eos/hpf [32,49,63,77,81,85]. Wolf W.A. et al. [85] showed that PEC < 15 was associated with endoscopic response in 90% of patients, with the decrease in symptoms in 88% of patients and with both clinical and endoscopic responses in 81% of patients. The logistic regression showed that a more prominent decrease in the eosinophil count is associated with a higher probability of the symptomatic response; for every 10% decrease in the eosinophil count, the symptom response increased by approximately 7% (p = 0.04), the endoscopic response increased by 6% (p < 0.001), and combined symptomatic and endoscopic responses increased by 10% (p = 0.01) [86]. PEC < 15 eos/hpf was a criterion for including studies in a meta-analysis [87]. This meta-analysis has shown that observational studies more often used the threshold of <15 eos/hpf, while interventional studies used more stringent criteria: <6 [32,49,54,70,71], <5 eos/hpf, and even <1 eos/hpf [53,88]. Gupta S.K., 2015 [71] defined a histological response as <6 eos/hpf, and histological remission as <1 eos/hpf.
Nevertheless, a low PEC is accompanied by the alleviation of symptoms only in a fraction of patients. In 85% of children with histological remission (PEC 0–5 eos/hpf), symptoms persisted [35]. Alexander J.A. et al. [36] revealed a histological response (>90% decrease in eosinophil count from baseline) in 61.9% of adults with EoE on fluticasone therapy and a symptomatic response in 42.9% of patients. Histological remission (<1 eos/hpf) was reached in 76.1% of patients in the group using high doses of oral budesonide suspension, but symptoms were absent only in 17.6% of patients [71]. Safroneeva E. et al. [37] showed that the area under the curve for symptoms measured by EEsAI and histological remission comprised 0.60 for PEC < 20/мм2 (which is equivalent to <5 eos/hpf) and 0.61 for PEC <60/мм2 (which is equivalent to <15 eos/hpf), and the accuracy rates were 62.1% and 61.7%, respectively. Therefore, PEC is not a sufficient histological criterion to define remission. Moreover, PEC reflects only inflammatory changes and does not reflect remodeling and stenofibrosis.
Aceves S.S. et al. [69] evaluated not only PEC, but other parameters in epithelium (basal zone hyperplasia (BZH), dilated intercellular spaces (DIS), desquamation of epithelium, clusters of eosinophils, and eosinophil degranulation) and in lamia propria (eosinophil count and fibrosis). The difficulty in using this score is that lamina propria does not necessary present in biopsy specimens. The rate of identification of the lamina propria in biopsies range from 38% to 75% in different studies [89,90,91]. But the advantage of this score is the evaluation of both—inflammatory features and the remodeling of the esophagus. The histological parameters of this score correlated with endoscopic features and dysphagia symptoms [69]. The epithelial remodeling score [92] is based on the previous score and includes BZH, DIS, and desquamation. The severity of the peak epithelial eosinophilia over the entire disease duration correlated positively with epithelial remodeling (r = 0.76, p < 0.0001), lamina propria eosinophilia (r = 0.54, p < 0.0001), and fibrosis (r = 0.53, p < 0.0001). The severity of lamina propria fibrosis (LPF) over time was lower in patients with PEC < 15 eos/hpf. Patients with a clinical response to topical corticosteroids demonstrated less prominent features of remodeling than non-responders.
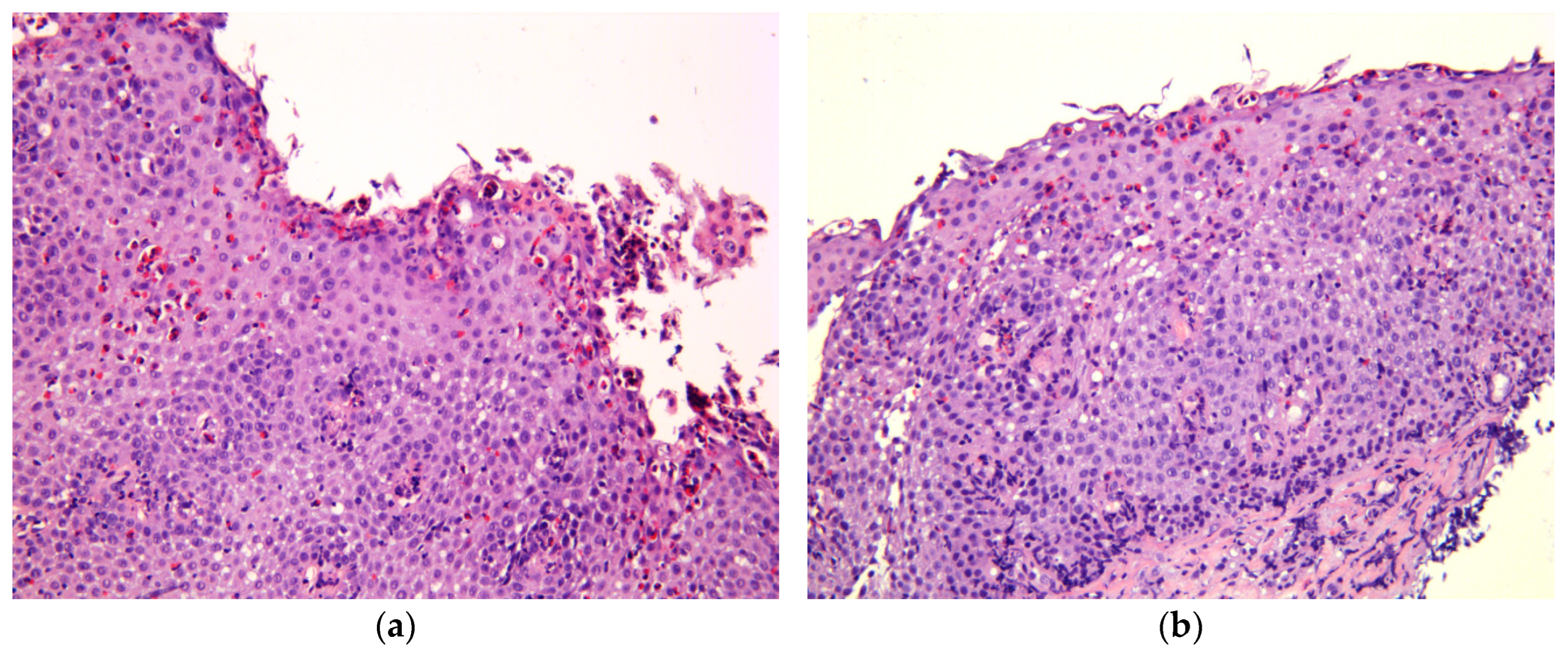
Collins M.H. et al. [93] developed an eosinophilic esophagitis histological scoring system (EoEHSS), which includes the following parameters (Table 3): PEC, DIS, BZH, eosinophilic abscesses (EA), eosinophil surface layering (SL), surface epithelial alteration (SEA), dyskeratotic epithelial cells (DEC), and LPF (Figure 1). EoEHSS evaluates not only the severity of features (grade), but also the extension of histological changes (stage). It allows for EoE to be diagnosed and for the discrimination between active EoE and treatment status. Moreover, logistic regression shows better results of EoEHSS compared with PEC in identifying treatment status. Distinct parameters of EoEHSS show a correlation with clinical symptoms given the low PEC. Whelan K.A. et al. [94] demonstrated that BZH persisted almost in 30% patients with PEC < 15 eos/hpf and was associated with ongoing symptoms of EoE (odds ratio 2.14; 95% CI, 1.03–4.42; p = 0.041) and endoscopic features of EoE (odds ratio 7.10; 95% CI, 3.12–16.18; p < 0.001). It can be explained by the elevated count of mast cells in patients with BZH and DIS that induce an IgE-mediated allergic response and are the component of Th2 inflammation in EoE [95]. Bolton S.M. et al. [95] identified BZH in 48.4% of distal biopsies and in 45.1% of biopsies from the mid-esophagus. In this study, BZH was associated both with an elevated count of mast cells and with their degranulation. Interestingly, in patients with EoE without symptoms, the count of mast cells was lower than in patients with active EoE.

Table 3.
Eosinophilic esophagitis histological scoring system (EoEHSS) [93].
Figure 1.
Histological features of EoE, hematoxylin, and eosin staining; magnification ×200. (a) Marked eosinophil surface layering (SL) with surface epithelial alteration (SEA), eosinophilic abscesses (EA). (b) Intraepithelial eosinophilic infiltration, pronounced basal zone hyperplasia (BZH), lamina propria fibrosis (LPF).
Even though lamina propria may not present in biopsies, the following combination of parameters can be an indirect indicator of the presence (but not stage) of LPF: age, BZH, DEC, and SEA [96]. The accuracy of this model for the identification of LPF comprised 84%. In other study, the strongest correlation was identified between LPF and two parameters of EoEHSS—DEC (r = 0.75; p < 0.001) and CEA (r = 0.70; p < 0.001) [91]. In logistic regression, the presence of DEC and CEA predicted LPF with an area under the curve of 0.91 (0.85–0.98) for CEA and 0.90 (0.83–0.97) for DEC.
Based on EoEHSS, Collins M.H. et al. [97] proposed the EoE histology remission score (EoEHRS) that includes two criteria: (1) PEC < 15 eos/hpf and (2) EoEHSS grade < 3 and EoEHSS stage < 3. The authors give the reason for their approach that PEC is not the only hallmark and component of inflammation in EoE and the evaluation of biopsies with EoEHSS may better define the remission. Moreover, the authors demonstrated a moderate correlation of EoEHRS with a decrease in symptoms of dysphagia (0.39–0.30, p ≤ 0.01), pain (0.48–0.34, p ≤ 0.01), and GERD symptoms (0.51–0.32, p ≤ 0.01) evaluated by PEESSv2.0. The correlation of PEC with symptom severity was weaker compared with EoEHRS. Moreover, biopsies that reached remission refined by EoEHRS showed a low expression of CPA3 (p = 0.0022) and thryptase (p = 0.0088), which confirms the low biological activity of EoE.
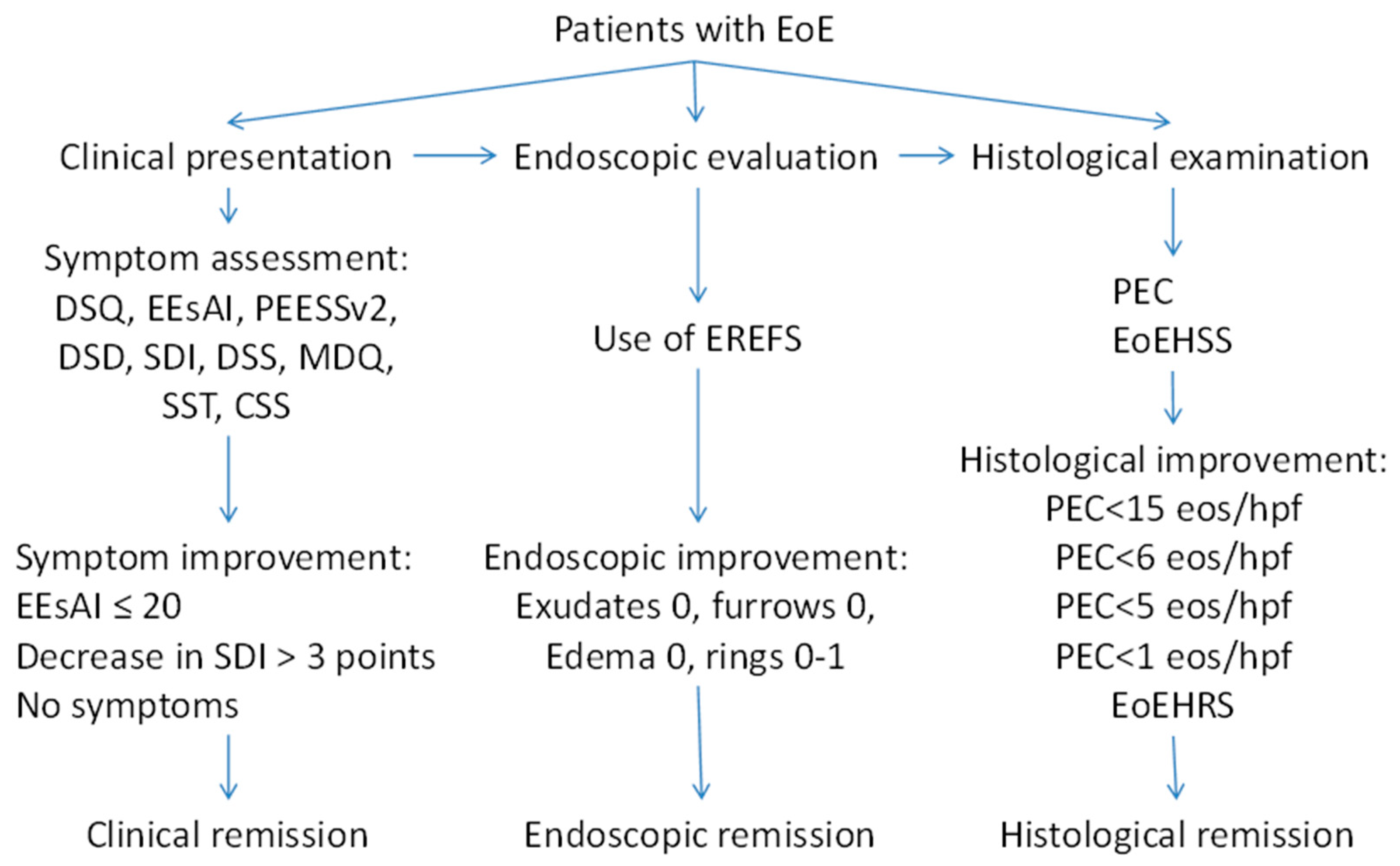
5. Multidisciplinary Approach to Estimate Severity of EoE
As it is shown in our review, there are different methods to evaluate clinical symptoms and different criteria of endoscopic and histological remission (Figure 2). Meanwhile, the data suggest that the evaluation of severity and the definition of the remission in EoE should be built on a combination of symptoms, endoscopic findings, and histology. Therefore, an instrument for the evaluation of EoE severity should be developed based on a multidisciplinary approach, using clinical, endoscopic, and histological features. A multidisciplinary international research group recently developed the Index of Severity of Eosinophilic Esophagitis (I-SEE) [98], grading the severity of EoE in points, where 0–6 correspond to mild EoE, 7–14 points correspond to moderate EoE, and ≥15 points correspond to severe EoE (Table 4). The I-SEE needs further validation and will be doubtlessly applied in clinical practice.
Figure 2.
Different criteria of the remission in EoE.

Table 4.
Eosinophilic Esophagitis Severity Index [97].
6. Conclusions
Currently, there is no uniform definition of the term “remission” in EoE. An assessment of the severity of EoE implies the evaluation of clinical, endoscopic, and histological features. EREFS is a gold standard for endoscopic examination in patients with EoE. EoEHSS is the most reliable histologic system for the evaluation of biopsies with EoE. The Multidisciplinary Severity Index for Eosinophilic Esophagitis (I-SEE) is promising but needs further validation.
Author Contributions
K.M., L.M. and A.M.—conceptualization, investigation, visualization, writing—original draft preparation, writing—review and editing, and supervision. V.K., D.A., E.M., I.B. and M.T.—review and editing. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data presented in this study are openly available in PubMed database.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Lucendo, A.J.; Molina-Infante, J.; Arias, A.; von Arnim, U.; Bredenoord, A.J.; Bussmann, C.; Amil Dias, J.; Bove, M.; Gonzalez-Cervera, J.; Larsson, H.; et al. Guidelines on eosinophilic esophagitis: Evidence-based statements and recommendations for diagnosis and management in children and adults. United Eur. Gastroenterol. J. 2017, 5, 335–358. [Google Scholar] [CrossRef] [PubMed]
- Dellon, E.S.; Liacouras, C.A.; Molina-Infante, J.; Furuta, G.T.; Spergel, J.M.; Zevit, N.; Spechler, S.J.; Attwood, S.E.; Straumann, A.; Aceves, S.S.; et al. Updated International Consensus Diagnostic Criteria for Eosinophilic Esophagitis: Proceedings of the AGREE Conference. Gastroenterology 2018, 155, 1022–1033.e10. [Google Scholar] [CrossRef] [PubMed]
- Dellon, E.S.; Gonsalves, N.; Hirano, I.; Furuta, G.T.; Liacouras, C.A.; Katzka, D.A. ACG clinical guideline: Evidenced based approach to the diagnosis and management of esophageal eosinophilia and eosinophilic esophagitis (EoE). Am. J. Gastroenterol. 2013, 108, 679–692; quiz 693. [Google Scholar] [CrossRef] [PubMed]
- Kaibysheva, V.O.; Mikhaleva, L.M.; Nikonov, E.L.; Shapovalyants, S.G. Epidemiology, etiology and pathogenesis of eosinophilic esophagitis. The latest data. Russ. J. Evid.-Based Gastroenterol. = Dokazatel’naya Gastroenterol. 2019, 8, 50–72. [Google Scholar] [CrossRef]
- Maslenkina, K.S.; Mikhaleva, L.M.; Motylev, E.N.; Gushchin, M.U.; Kaibysheva, V.O.; Atyakshin, D.A.; Kudryavtseva, Y.Y.; Kudryavtsev, G.Y. Clinical and morphological diagnosis of eosinophilic esophagitis. Clin. Exp. Morphol. 2023, 12, 5–18. [Google Scholar] [CrossRef]
- Gonzalez-Cervera, J.; Arias, A.; Redondo-Gonzalez, O.; Cano-Mollinedo, M.M.; Terreehorst, I.; Lucendo, A.J. Association between atopic manifestations and eosinophilic esophagitis: A systematic review and meta-analysis. Ann. Allergy Asthma Immunol. 2017, 118, 582–590.e2. [Google Scholar] [CrossRef]
- Capucilli, P.; Hill, D.A. Allergic Comorbidity in Eosinophilic Esophagitis: Mechanistic Relevance and Clinical Implications. Clin. Rev. Allergy Immunol. 2019, 57, 111–127. [Google Scholar] [CrossRef]
- Hill, D.A.; Grundmeier, R.W.; Ramos, M.; Spergel, J.M. Eosinophilic Esophagitis Is a Late Manifestation of the Allergic March. J. Allergy Clin. Immunol. Pract. 2018, 6, 1528–1533. [Google Scholar] [CrossRef]
- Ram, G.; Lee, J.; Ott, M.; Brown-Whitehorn, T.F.; Cianferoni, A.; Shuker, M.; Wang, M.L.; Verma, R.; Liacouras, C.A.; Spergel, J.M. Seasonal exacerbation of esophageal eosinophilia in children with eosinophilic esophagitis and allergic rhinitis. Ann. Allergy Asthma Immunol. 2015, 115, 224–228.e1. [Google Scholar] [CrossRef]
- Reed, C.C.; Iglesia, E.G.A.; Commins, S.P.; Dellon, E.S. Seasonal exacerbation of eosinophilic esophagitis histologic activity in adults and children implicates role of aeroallergens. Ann. Allergy Asthma Immunol. 2019, 122, 296–301. [Google Scholar] [CrossRef]
- Bohm, M.; Jacobs, J.W., Jr.; Gupta, A.; Gupta, S.; Wo, J.M. Most children with eosinophilic esophagitis have a favorable outcome as young adults. Dis. Esophagus 2017, 30, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Dellon, E.S.; Hirano, I. Epidemiology and Natural History of Eosinophilic Esophagitis. Gastroenterology 2018, 154, 319–332.e3. [Google Scholar] [CrossRef] [PubMed]
- Schoepfer, A.M.; Safroneeva, E.; Bussmann, C.; Kuchen, T.; Portmann, S.; Simon, H.U.; Straumann, A. Delay in diagnosis of eosinophilic esophagitis increases risk for stricture formation in a time-dependent manner. Gastroenterology 2013, 145, 1230–1236.e2. [Google Scholar] [CrossRef] [PubMed]
- Warners, M.J.; Oude Nijhuis, R.A.B.; de Wijkerslooth, L.R.H.; Smout, A.; Bredenoord, A.J. The natural course of eosinophilic esophagitis and long-term consequences of undiagnosed disease in a large cohort. Am. J. Gastroenterol. 2018, 113, 836–844. [Google Scholar] [CrossRef] [PubMed]
- Dellon, E.S.; Kim, H.P.; Sperry, S.L.; Rybnicek, D.A.; Woosley, J.T.; Shaheen, N.J. A phenotypic analysis shows that eosinophilic esophagitis is a progressive fibrostenotic disease. Gastrointest. Endosc. 2014, 79, 577–585.e4. [Google Scholar] [CrossRef] [PubMed]
- Lyons, E.; Donohue, K.; Lee, J.J. Developing Pharmacologic Treatments for Eosinophilic Esophagitis: Draft Guidance from the United States Food and Drug Administration. Gastroenterology 2019, 157, 275–277. [Google Scholar] [CrossRef]
- Franciosi, J.P.; Gordon, M.; Sinopoulou, V.; Dellon, E.S.; Gupta, S.K.; Reed, C.C.; Gutierrez-Junquera, C.; Venkatesh, R.D.; Erwin, E.A.; Egiz, A.; et al. Medical treatment of eosinophilic esophagitis. Cochrane Database Syst. Rev. 2023, 7, CD004065. [Google Scholar] [CrossRef]
- Hirano, I.; Furuta, G.T. Approaches and Challenges to Management of Pediatric and Adult Patients with Eosinophilic Esophagitis. Gastroenterology 2020, 158, 840–851. [Google Scholar] [CrossRef]
- Greuter, T.; Hirano, I.; Dellon, E.S. Emerging therapies for eosinophilic esophagitis. J. Allergy Clin. Immunol. 2020, 145, 38–45. [Google Scholar] [CrossRef]
- Racca, F.; Pellegatta, G.; Cataldo, G.; Vespa, E.; Carlani, E.; Pelaia, C.; Paoletti, G.; Messina, M.R.; Nappi, E.; Canonica, G.W.; et al. Type 2 Inflammation in Eosinophilic Esophagitis: From Pathophysiology to Therapeutic Targets. Front. Physiol. 2021, 12, 815842. [Google Scholar] [CrossRef]
- Feo-Ortega, S.; Lucendo, A.J. Evidence-based treatments for eosinophilic esophagitis: Insights for the clinician. Ther. Adv. Gastroenterol. 2022, 15, 1–19. [Google Scholar] [CrossRef] [PubMed]
- Rank, M.A.; Sharaf, R.N.; Furuta, G.T.; Aceves, S.S.; Greenhawt, M.; Spergel, J.M.; Falck-Ytter, Y.T.; Dellon, E.S.; Chachu, K.A.; Day, L.; et al. Technical Review on the Management of Eosinophilic Esophagitis: A Report from the AGA Institute and the Joint Task Force on Allergy-Immunology Practice Parameters. Gastroenterology 2020, 158, 1789–1810.e15. [Google Scholar] [CrossRef] [PubMed]
- Muir, A.; Falk, G.W. Eosinophilic Esophagitis: A Review. JAMA 2021, 326, 1310–1318. [Google Scholar] [CrossRef] [PubMed]
- Frandsen, L.T.; Westmark, S.; Melgaard, D.; Krarup, A.L. Effectiveness of PPI treatment and guideline adherence in 236 patients with eosinophilic oesophagitis-Results from the population-based DanEoE cohort shows a low complication rate. United Eur. Gastroenterol. J. 2021, 9, 910–918. [Google Scholar] [CrossRef] [PubMed]
- Wen, T.; Dellon, E.S.; Moawad, F.J.; Furuta, G.T.; Aceves, S.S.; Rothenberg, M.E. Transcriptome analysis of proton pump inhibitor-responsive esophageal eosinophilia reveals proton pump inhibitor-reversible allergic inflammation. J. Allergy Clin. Immunol. 2015, 135, 187–197. [Google Scholar] [CrossRef] [PubMed]
- Cheng, E.; Zhang, X.; Huo, X.; Yu, C.; Zhang, Q.; Wang, D.H.; Spechler, S.J.; Souza, R.F. Omeprazole blocks eotaxin-3 expression by oesophageal squamous cells from patients with eosinophilic oesophagitis and GORD. Gut 2013, 62, 824–832. [Google Scholar] [CrossRef] [PubMed]
- Cheng, E.; Zhang, X.; Wilson, K.S.; Wang, D.H.; Park, J.Y.; Huo, X.; Yu, C.; Zhang, Q.; Spechler, S.J.; Souza, R.F. JAK-STAT6 Pathway Inhibitors Block Eotaxin-3 Secretion by Epithelial Cells and Fibroblasts from Esophageal Eosinophilia Patients: Promising Agents to Improve Inflammation and Prevent Fibrosis in EoE. PLoS ONE 2016, 11, e0157376. [Google Scholar] [CrossRef]
- van Rhijn, B.D.; Weijenborg, P.W.; Verheij, J.; van den Bergh Weerman, M.A.; Verseijden, C.; van den Wijngaard, R.M.; de Jonge, W.J.; Smout, A.J.; Bredenoord, A.J. Proton pump inhibitors partially restore mucosal integrity in patients with proton pump inhibitor-responsive esophageal eosinophilia but not eosinophilic esophagitis. Clin. Gastroenterol. Hepatol. 2014, 12, 1815–1823.e2. [Google Scholar] [CrossRef]
- Miehlke, S.; Schlag, C.; Lucendo, A.J.; Biedermann, L.; Vaquero, C.S.; Schmoecker, C.; Hayat, J.; Hruz, P.; Ciriza de Los Rios, C.; Bredenoord, A.J.; et al. Budesonide orodispersible tablets for induction of remission in patients with active eosinophilic oesophagitis: A 6-week open-label trial of the EOS-2 Programme. United Eur. Gastroenterol. J. 2022, 10, 330–343. [Google Scholar] [CrossRef]
- Massironi, S.; Mulinacci, G.; Gallo, C.; Elvevi, A.; Danese, S.; Invernizzi, P.; Vespa, E. Mechanistic Insights into Eosinophilic Esophagitis: Therapies Targeting Pathophysiological Mechanisms. Cells 2023, 12, 2473. [Google Scholar] [CrossRef]
- Dellon, E.S.; Woosley, J.T.; Arrington, A.; McGee, S.J.; Covington, J.; Moist, S.E.; Gebhart, J.H.; Tylicki, A.E.; Shoyoye, S.O.; Martin, C.F.; et al. Efficacy of Budesonide vs Fluticasone for Initial Treatment of Eosinophilic Esophagitis in a Randomized Controlled Trial. Gastroenterology 2019, 157, 65–73.e5. [Google Scholar] [CrossRef]
- Hirano, I.; Collins, M.H.; Katzka, D.A.; Mukkada, V.A.; Falk, G.W.; Morey, R.; Desai, N.K.; Lan, L.; Williams, J.; Dellon, E.S.; et al. Budesonide Oral Suspension Improves Outcomes in Patients with Eosinophilic Esophagitis: Results from a Phase 3 Trial. Clin. Gastroenterol. Hepatol. 2022, 20, 525–534.e10. [Google Scholar] [CrossRef] [PubMed]
- Moawad, F.J.; Molina-Infante, J.; Lucendo, A.J.; Cantrell, S.E.; Tmanova, L.; Douglas, K.M. Systematic review with meta-analysis: Endoscopic dilation is highly effective and safe in children and adults with eosinophilic oesophagitis. Aliment. Pharmacol. Ther. 2017, 46, 96–105. [Google Scholar] [CrossRef] [PubMed]
- Dougherty, M.; Runge, T.M.; Eluri, S.; Dellon, E.S. Esophageal dilation with either bougie or balloon technique as a treatment for eosinophilic esophagitis: A systematic review and meta-analysis. Gastrointest. Endosc. 2017, 86, 581–591.e3. [Google Scholar] [CrossRef] [PubMed]
- Pentiuk, S.; Putnam, P.E.; Collins, M.H.; Rothenberg, M.E. Dissociation between symptoms and histological severity in pediatric eosinophilic esophagitis. J. Pediatr. Gastroenterol. Nutr. 2009, 48, 152–160. [Google Scholar] [CrossRef] [PubMed]
- Alexander, J.A.; Jung, K.W.; Arora, A.S.; Enders, F.; Katzka, D.A.; Kephardt, G.M.; Kita, H.; Kryzer, L.A.; Romero, Y.; Smyrk, T.C.; et al. Swallowed fluticasone improves histologic but not symptomatic response of adults with eosinophilic esophagitis. Clin. Gastroenterol. Hepatol. 2012, 10, 742–749.e1. [Google Scholar] [CrossRef] [PubMed]
- Safroneeva, E.; Straumann, A.; Coslovsky, M.; Zwahlen, M.; Kuehni, C.E.; Panczak, R.; Haas, N.A.; Alexander, J.A.; Dellon, E.S.; Gonsalves, N.; et al. Symptoms Have Modest Accuracy in Detecting Endoscopic and Histologic Remission in Adults with Eosinophilic Esophagitis. Gastroenterology 2016, 150, 581–590.e4. [Google Scholar] [CrossRef]
- Dellon, E.S.; Gupta, S.K. A Conceptual Approach to Understanding Treatment Response in Eosinophilic Esophagitis. Clin. Gastroenterol. Hepatol. 2019, 17, 2149–2160. [Google Scholar] [CrossRef]
- Hirano, I.; Spechler, S.; Furuta, G.; Dellon, E.S. White Paper AGA: Drug Development for Eosinophilic Esophagitis. Clin. Gastroenterol. Hepatol. 2017, 15, 1173–1183. [Google Scholar] [CrossRef]
- Reed, C.C.; Dellon, E.S. Eosinophilic Esophagitis. Med. Clin. N. Am. 2019, 103, 29–42. [Google Scholar] [CrossRef]
- Kaibysheva, V.O.; Kashin, S.V.; Mikhaleva, L.M.; Vidyayeva, N.S.; Kuvaev, R.O.; Galkova, Z.V.; Ilchishina, T.A.; Pechnikova, V.V.; Nikonov, E.L.; Shapovalyants, S.G. Eosinophilic esophagitis: Current view on the problem and own clinical observations. Russ. J. Evid.-Based Gastroenterol. = Dokazatel’naya Gastroenterol. 2019, 8, 58–83. [Google Scholar] [CrossRef]
- Laserna-Mendieta, E.J.; Navarro, P.; Casabona-Frances, S.; Savarino, E.V.; Perez-Martinez, I.; Guagnozzi, D.; Barrio, J.; Perello, A.; Guardiola-Arevalo, A.; Betore-Glaria, M.E.; et al. Differences between childhood- and adulthood-onset eosinophilic esophagitis: An analysis from the EoE connect registry. Dig Liver Dis. 2023, 55, 350–359. [Google Scholar] [CrossRef] [PubMed]
- Lynch, M.K.; Avis, K.T.; Dimmitt, R.A.; Goodin, B.R. Topical Review: Eosinophilic Esophagitis in Children: Implications for Health-Related Quality of Life and Potential Avenues for Future Research. J. Pediatr. Psychol. 2015, 40, 727–732. [Google Scholar] [CrossRef] [PubMed]
- Kidambi, T.; Toto, E.; Ho, N.; Taft, T.; Hirano, I. Temporal trends in the relative prevalence of dysphagia etiologies from 1999–2009. World J. Gastroenterol. 2012, 18, 4335–4341. [Google Scholar] [CrossRef] [PubMed]
- Desai, T.K.; Stecevic, V.; Chang, C.H.; Goldstein, N.S.; Badizadegan, K.; Furuta, G.T. Association of eosinophilic inflammation with esophageal food impaction in adults. Gastrointest. Endosc. 2005, 61, 795–801. [Google Scholar] [CrossRef]
- Dellon, E.S.; Irani, A.M.; Hill, M.R.; Hirano, I. Development and field testing of a novel patient-reported outcome measure of dysphagia in patients with eosinophilic esophagitis. Aliment. Pharmacol. Ther. 2013, 38, 634–642. [Google Scholar] [CrossRef]
- Hudgens, S.; Evans, C.; Phillips, E.; Hill, M. Psychometric validation of the Dysphagia Symptom Questionnaire in patients with eosinophilic esophagitis treated with budesonide oral suspension. J. Patient. Rep. Outcomes 2017, 1, 3. [Google Scholar] [CrossRef]
- Dellon, E.S.; Katzka, D.A.; Collins, M.H.; Hamdani, M.; Gupta, S.K.; Hirano, I.; Investigators, M.P. Budesonide Oral Suspension Improves Symptomatic, Endoscopic, and Histologic Parameters Compared with Placebo in Patients with Eosinophilic Esophagitis. Gastroenterology 2017, 152, 776–786.e5. [Google Scholar] [CrossRef]
- Dellon, E.S.; Collins, M.H.; Katzka, D.A.; Mukkada, V.A.; Falk, G.W.; Morey, R.; Goodwin, B.; Eisner, J.D.; Lan, L.; Desai, N.K.; et al. Long-Term Treatment of Eosinophilic Esophagitis with Budesonide Oral Suspension. Clin. Gastroenterol. Hepatol. 2022, 20, 1488–1498.e11. [Google Scholar] [CrossRef]
- Schoepfer, A.M.; Straumann, A.; Panczak, R.; Coslovsky, M.; Kuehni, C.E.; Maurer, E.; Haas, N.A.; Romero, Y.; Hirano, I.; Alexander, J.A.; et al. Development and validation of a symptom-based activity index for adults with eosinophilic esophagitis. Gastroenterology 2014, 147, 1255–1266.e21. [Google Scholar] [CrossRef]
- Albinsson, S.; Tuomi, L.; Wenneras, C.; Larsson, H. Patient-Reported Dysphagia in Adults with Eosinophilic Esophagitis: Translation and Validation of the Swedish Eosinophilic Esophagitis Activity Index. Dysphagia 2022, 37, 286–296. [Google Scholar] [CrossRef] [PubMed]
- Franciosi, J.P.; Hommel, K.A.; DeBrosse, C.W.; Greenberg, A.B.; Greenler, A.J.; Abonia, J.P.; Rothenberg, M.E.; Varni, J.W. Development of a validated patient-reported symptom metric for pediatric eosinophilic esophagitis: Qualitative methods. BMC Gastroenterol. 2011, 11, 126. [Google Scholar] [CrossRef] [PubMed]
- Hirano, I.; Collins, M.H.; Assouline-Dayan, Y.; Evans, L.; Gupta, S.; Schoepfer, A.M.; Straumann, A.; Safroneeva, E.; Grimm, M.; Smith, H.; et al. RPC4046, a Monoclonal Antibody Against IL13, Reduces Histologic and Endoscopic Activity in Patients with Eosinophilic Esophagitis. Gastroenterology 2019, 156, 592–603.e10. [Google Scholar] [CrossRef] [PubMed]
- Hirano, I.; Dellon, E.S.; Hamilton, J.D.; Collins, M.H.; Peterson, K.; Chehade, M.; Schoepfer, A.M.; Safroneeva, E.; Rothenberg, M.E.; Falk, G.W.; et al. Efficacy of Dupilumab in a Phase 2 Randomized Trial of Adults with Active Eosinophilic Esophagitis. Gastroenterology 2020, 158, 111–122.e10. [Google Scholar] [CrossRef] [PubMed]
- Safroneeva, E.; Pan, Z.; King, E.; Martin, L.J.; Collins, M.H.; Yang, G.Y.; Capocelli, K.E.; Arva, N.C.; Abonia, J.P.; Atkins, D.; et al. Long-Lasting Dissociation of Esophageal Eosinophilia and Symptoms After Dilation in Adults with Eosinophilic Esophagitis. Clin. Gastroenterol. Hepatol. 2022, 20, 766–775.e4. [Google Scholar] [CrossRef] [PubMed]
- Masuda, M.Y.; LeSuer, W.E.; Horsley-Silva, J.L.; Putikova, A.; Buras, M.R.; Gibson, J.B.; Pyon, G.C.; Simmons, T.D.; Doyle, A.D.; Wright, B.L. Food-Specific IgG4 Is Elevated Throughout the Upper Gastrointestinal Tract in Eosinophilic Esophagitis. Dig Dis. Sci. 2023, 68, 2406–2413. [Google Scholar] [CrossRef] [PubMed]
- Dellon, E.S.; Collins, M.H.; Rothenberg, M.E.; Assouline-Dayan, Y.; Evans, L.; Gupta, S.; Schoepfer, A.; Straumann, A.; Safroneeva, E.; Rodriguez, C.; et al. Long-term Efficacy and Tolerability of RPC4046 in an Open-Label Extension Trial of Patients with Eosinophilic Esophagitis. Clin. Gastroenterol. Hepatol. 2021, 19, 473–483.e17. [Google Scholar] [CrossRef]
- Dellon, E.S.; Peterson, K.A.; Mitlyng, B.L.; Iuga, A.; Bookhout, C.E.; Cortright, L.M.; Walker, K.B.; Gee, T.S.; McGee, S.J.; Cameron, B.A.; et al. Mepolizumab for treatment of adolescents and adults with eosinophilic oesophagitis: A multicentre, randomised, double-blind, placebo-controlled clinical trial. Gut 2023, 72, 1828–1837. [Google Scholar] [CrossRef]
- Straumann, A.; Conus, S.; Degen, L.; Felder, S.; Kummer, M.; Engel, H.; Bussmann, C.; Beglinger, C.; Schoepfer, A.; Simon, H.U. Budesonide is effective in adolescent and adult patients with active eosinophilic esophagitis. Gastroenterology 2010, 139, 1526–1537.e1. [Google Scholar] [CrossRef]
- Miehlke, S.; Hruz, P.; Vieth, M.; Bussmann, C.; von Arnim, U.; Bajbouj, M.; Schlag, C.; Madisch, A.; Fibbe, C.; Wittenburg, H.; et al. A randomised, double-blind trial comparing budesonide formulations and dosages for short-term treatment of eosinophilic oesophagitis. Gut 2016, 65, 390–399. [Google Scholar] [CrossRef]
- Lorenz, N.J.; Link, A.; Czapiewski, P.; Arnim, U.V. Eosinophilic esophagitis: Comparison of clinical, endoscopic and histological scoring systems. Z. Gastroenterol. 2022, 60, 1779–1786. [Google Scholar] [CrossRef] [PubMed]
- Gonsalves, N.; Yang, G.Y.; Doerfler, B.; Ritz, S.; Ditto, A.M.; Hirano, I. Elimination diet effectively treats eosinophilic esophagitis in adults; food reintroduction identifies causative factors. Gastroenterology 2012, 142, 1451–1459.e1; quiz e1414–1455. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez-Sanchez, J.; Barrio-Andres, J.; Nantes Castillejo, O.; Valdivieso-Cortazar, E.; Perez-Martinez, I.; Boumidi, A.; Olmos-Jerez, J.A.; Payeras-Llodra, G.; Alcaide-Suarez, N.; Ruiz-Rebollo, L.; et al. The Endoscopic Reference Score shows modest accuracy to predict either clinical or histological activity in adult patients with eosinophilic oesophagitis. Aliment. Pharmacol. Ther. 2017, 45, 300–309. [Google Scholar] [CrossRef] [PubMed]
- Grudell, A.B.; Alexander, J.A.; Enders, F.B.; Pacifico, R.; Fredericksen, M.; Wise, J.L.; Locke, G.R., 3rd; Arora, A.; Zais, T.; Talley, N.J.; et al. Validation of the Mayo Dysphagia Questionnaire. Dis. Esophagus 2007, 20, 202–205. [Google Scholar] [CrossRef] [PubMed]
- McElhiney, J.; Lohse, M.R.; Arora, A.S.; Peloquin, J.M.; Geno, D.M.; Kuntz, M.M.; Enders, F.B.; Fredericksen, M.; Abdalla, A.A.; Khan, Y.; et al. The Mayo Dysphagia Questionnaire-30: Documentation of reliability and validity of a tool for interventional trials in adults with esophageal disease. Dysphagia 2010, 25, 221–230. [Google Scholar] [CrossRef] [PubMed]
- Dellon, E.S.; Sheikh, A.; Speck, O.; Woodward, K.; Whitlow, A.B.; Hores, J.M.; Ivanovic, M.; Chau, A.; Woosley, J.T.; Madanick, R.D.; et al. Viscous topical is more effective than nebulized steroid therapy for patients with eosinophilic esophagitis. Gastroenterology 2012, 143, 321–324.e1. [Google Scholar] [CrossRef] [PubMed]
- Reed, C.C.; Wolf, W.A.; Cotton, C.C.; Dellon, E.S. A visual analogue scale and a Likert scale are simple and responsive tools for assessing dysphagia in eosinophilic oesophagitis. Aliment. Pharmacol. Ther. 2017, 45, 1443–1448. [Google Scholar] [CrossRef]
- Martin, L.J.; Franciosi, J.P.; Collins, M.H.; Abonia, J.P.; Lee, J.J.; Hommel, K.A.; Varni, J.W.; Grotjan, J.T.; Eby, M.; He, H.; et al. Pediatric Eosinophilic Esophagitis Symptom Scores (PEESS v2.0) identify histologic and molecular correlates of the key clinical features of disease. J. Allergy Clin. Immunol. 2015, 135, 1519–1528.e8. [Google Scholar] [CrossRef]
- Aceves, S.S.; Newbury, R.O.; Dohil, M.A.; Bastian, J.F.; Dohil, R. A symptom scoring tool for identifying pediatric patients with eosinophilic esophagitis and correlating symptoms with inflammation. Ann. Allergy Asthma Immunol. 2009, 103, 401–406. [Google Scholar] [CrossRef]
- Dohil, R.; Newbury, R.; Fox, L.; Bastian, J.; Aceves, S. Oral viscous budesonide is effective in children with eosinophilic esophagitis in a randomized, placebo-controlled trial. Gastroenterology 2010, 139, 418–429. [Google Scholar] [CrossRef]
- Gupta, S.K.; Vitanza, J.M.; Collins, M.H. Efficacy and safety of oral budesonide suspension in pediatric patients with eosinophilic esophagitis. Clin. Gastroenterol. Hepatol. 2015, 13, 66–76.e3. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.P.; Vance, R.B.; Shaheen, N.J.; Dellon, E.S. The prevalence and diagnostic utility of endoscopic features of eosinophilic esophagitis: A meta-analysis. Clin. Gastroenterol. Hepatol. 2012, 10, 988–996.e5. [Google Scholar] [CrossRef] [PubMed]
- Hirano, I.; Moy, N.; Heckman, M.G.; Thomas, C.S.; Gonsalves, N.; Achem, S.R. Endoscopic assessment of the oesophageal features of eosinophilic oesophagitis: Validation of a novel classification and grading system. Gut 2013, 62, 489–495. [Google Scholar] [CrossRef] [PubMed]
- van Rhijn, B.D.; Warners, M.J.; Curvers, W.L.; van Lent, A.U.; Bekkali, N.L.; Takkenberg, R.B.; Kloek, J.J.; Bergman, J.J.; Fockens, P.; Bredenoord, A.J. Evaluating the endoscopic reference score for eosinophilic esophagitis: Moderate to substantial intra- and interobserver reliability. Endoscopy 2014, 46, 1049–1055. [Google Scholar] [CrossRef] [PubMed]
- Dellon, E.S.; Cotton, C.C.; Gebhart, J.H.; Higgins, L.L.; Beitia, R.; Woosley, J.T.; Shaheen, N.J. Accuracy of the Eosinophilic Esophagitis Endoscopic Reference Score in Diagnosis and Determining Response to Treatment. Clin. Gastroenterol. Hepatol. 2016, 14, 31–39. [Google Scholar] [CrossRef] [PubMed]
- Kuchen, T.; Straumann, A.; Safroneeva, E.; Romero, Y.; Bussmann, C.; Vavricka, S.; Netzer, P.; Reinhard, A.; Portmann, S.; Schoepfer, A.M. Swallowed topical corticosteroids reduce the risk for long-lasting bolus impactions in eosinophilic esophagitis. Allergy 2014, 69, 1248–1254. [Google Scholar] [CrossRef]
- van Rhijn, B.D.; Verheij, J.; Smout, A.J.; Bredenoord, A.J. The Endoscopic Reference Score shows modest accuracy to predict histologic remission in adult patients with eosinophilic esophagitis. Neurogastroenterol. Motil. 2016, 28, 1714–1722. [Google Scholar] [CrossRef]
- Chen, J.W.; Pandolfino, J.E.; Lin, Z.; Ciolino, J.D.; Gonsalves, N.; Kahrilas, P.J.; Hirano, I. Severity of endoscopically identified esophageal rings correlates with reduced esophageal distensibility in eosinophilic esophagitis. Endoscopy 2016, 48, 794–801. [Google Scholar] [CrossRef]
- Wechsler, J.B.; Bolton, S.M.; Amsden, K.; Wershil, B.K.; Hirano, I.; Kagalwalla, A.F. Eosinophilic Esophagitis Reference Score Accurately Identifies Disease Activity and Treatment Effects in Children. Clin. Gastroenterol. Hepatol. 2018, 16, 1056–1063. [Google Scholar] [CrossRef]
- Schoepfer, A.M.; Panczak, R.; Zwahlen, M.; Kuehni, C.E.; Coslovsky, M.; Maurer, E.; Haas, N.A.; Alexander, J.A.; Dellon, E.S.; Gonsalves, N.; et al. How do gastroenterologists assess overall activity of eosinophilic esophagitis in adult patients? Am. J. Gastroenterol. 2015, 110, 402–414. [Google Scholar] [CrossRef]
- Greuter, T.; Safroneeva, E.; Bussmann, C.; Biedermann, L.; Vavricka, S.R.; Katzka, D.A.; Schoepfer, A.M.; Straumann, A. Maintenance Treatment of Eosinophilic Esophagitis with Swallowed Topical Steroids Alters Disease Course over a 5-Year Follow-Up Period in Adult Patients. Clin. Gastroenterol. Hepatol. 2019, 17, 419–428.e6. [Google Scholar] [CrossRef] [PubMed]
- Kwiatek, M.A.; Hirano, I.; Kahrilas, P.J.; Rothe, J.; Luger, D.; Pandolfino, J.E. Mechanical properties of the esophagus in eosinophilic esophagitis. Gastroenterology 2011, 140, 82–90. [Google Scholar] [CrossRef] [PubMed]
- Nicodeme, F.; Hirano, I.; Chen, J.; Robinson, K.; Lin, Z.; Xiao, Y.; Gonsalves, N.; Kwasny, M.J.; Kahrilas, P.J.; Pandolfino, J.E. Esophageal distensibility as a measure of disease severity in patients with eosinophilic esophagitis. Clin. Gastroenterol. Hepatol. 2013, 11, 1101–1107.e1. [Google Scholar] [CrossRef] [PubMed]
- Nasi, M.; De Gaetano, A.; Carnevale, G.; Bertoni, L.; Selleri, V.; Zanini, G.; Pisciotta, A.; Caramaschi, S.; Reggiani Bonetti, L.; Farinetti, A.; et al. Effects of Energy Drink Acute Assumption in Gastrointestinal Tract of Rats. Nutrients 2022, 14, 1928. [Google Scholar] [CrossRef] [PubMed]
- Wolf, W.A.; Cotton, C.C.; Green, D.J.; Hughes, J.T.; Woosley, J.T.; Shaheen, N.J.; Dellon, E.S. Evaluation of Histologic Cutpoints for Treatment Response in Eosinophilic Esophagitis. J. Gastroenterol. Hepatol. Res. 2015, 4, 1780–1787. [Google Scholar] [CrossRef]
- Reed, C.C.; Wolf, W.A.; Cotton, C.C.; Rusin, S.; Perjar, I.; Hollyfield, J.; Woosley, J.T.; Shaheen, N.J.; Dellon, E.S. Optimal Histologic Cutpoints for Treatment Response in Patients with Eosinophilic Esophagitis: Analysis of Data from a Prospective Cohort Study. Clin. Gastroenterol. Hepatol. 2018, 16, 226–233.e2. [Google Scholar] [CrossRef]
- Eke, R.; Li, T.; White, A.; Tariq, T.; Markowitz, J.; Lenov, A. Systematic review of histological remission criteria in eosinophilic esophagitis. JGH Open 2018, 2, 158–165. [Google Scholar] [CrossRef]
- Konikoff, M.R.; Noel, R.J.; Blanchard, C.; Kirby, C.; Jameson, S.C.; Buckmeier, B.K.; Akers, R.; Cohen, M.B.; Collins, M.H.; Assa’ad, A.H.; et al. A randomized, double-blind, placebo-controlled trial of fluticasone propionate for pediatric eosinophilic esophagitis. Gastroenterology 2006, 131, 1381–1391. [Google Scholar] [CrossRef]
- Andreae, D.A.; Hanna, M.G.; Magid, M.S.; Malerba, S.; Andreae, M.H.; Bagiella, E.; Chehade, M. Swallowed Fluticasone Propionate Is an Effective Long-Term Maintenance Therapy for Children with Eosinophilic Esophagitis. Am. J. Gastroenterol. 2016, 111, 1187–1197. [Google Scholar] [CrossRef]
- Dellon, E.S.; Speck, O.; Woodward, K.; Covey, S.; Rusin, S.; Shaheen, N.J.; Woosley, J.T. Distribution and variability of esophageal eosinophilia in patients undergoing upper endoscopy. Mod. Pathol. 2015, 28, 383–390. [Google Scholar] [CrossRef]
- Hiremath, G.; Choksi, Y.A.; Acra, S.; Correa, H.; Dellon, E.S. Factors Associated with Adequate Lamina Propria Sampling and Presence of Lamina Propria Fibrosis in Children with Eosinophilic Esophagitis. Clin. Gastroenterol. Hepatol. 2021, 19, 1814–1823.e1811. [Google Scholar] [CrossRef]
- Rajan, J.; Newbury, R.O.; Anilkumar, A.; Dohil, R.; Broide, D.H.; Aceves, S.S. Long-term assessment of esophageal remodeling in patients with pediatric eosinophilic esophagitis treated with topical corticosteroids. J. Allergy Clin. Immunol. 2016, 137, 147–156.e148. [Google Scholar] [CrossRef] [PubMed]
- Collins, M.H.; Martin, L.J.; Alexander, E.S.; Boyd, J.T.; Sheridan, R.; He, H.; Pentiuk, S.; Putnam, P.E.; Abonia, J.P.; Mukkada, V.A.; et al. Newly developed and validated eosinophilic esophagitis histology scoring system and evidence that it outperforms peak eosinophil count for disease diagnosis and monitoring. Dis. Esophagus 2017, 30, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Whelan, K.A.; Godwin, B.C.; Wilkins, B.; Elci, O.U.; Benitez, A.; DeMarshall, M.; Sharma, M.; Gross, J.; Klein-Szanto, A.J.; Liacouras, C.A.; et al. Persistent Basal Cell Hyperplasia Is Associated with Clinical and Endoscopic Findings in Patients With Histologically Inactive Eosinophilic Esophagitis. Clin. Gastroenterol. Hepatol. 2020, 18, 1475–1482.e1. [Google Scholar] [CrossRef] [PubMed]
- Bolton, S.M.; Kagalwalla, A.F.; Arva, N.C.; Wang, M.Y.; Amsden, K.; Melin-Aldana, H.; Dellon, E.S.; Bryce, P.J.; Wershil, B.K.; Wechsler, J.B. Mast Cell Infiltration Is Associated with Persistent Symptoms and Endoscopic Abnormalities Despite Resolution of Eosinophilia in Pediatric Eosinophilic Esophagitis. Am. J. Gastroenterol. 2020, 115, 224–233. [Google Scholar] [CrossRef]
- Hiremath, G.; Sun, L.; Correa, H.; Acra, S.; Collins, M.H.; Bonis, P.; Arva, N.C.; Capocelli, K.E.; Falk, G.W.; King, E.; et al. Development and Validation of Web-Based Tool to Predict Lamina Propria Fibrosis in Eosinophilic Esophagitis. Am. J. Gastroenterol. 2022, 117, 272–279. [Google Scholar] [CrossRef]
- Collins, M.H.; Martin, L.J.; Wen, T.; Abonia, J.P.; Putnam, P.E.; Mukkada, V.A.; Rothenberg, M.E. Eosinophilic Esophagitis Histology Remission Score: Significant Relations to Measures of Disease Activity and Symptoms. J. Pediatr. Gastroenterol. Nutr. 2020, 70, 598–603. [Google Scholar] [CrossRef]
- Dellon, E.S.; Khoury, P.; Muir, A.B.; Liacouras, C.A.; Safroneeva, E.; Atkins, D.; Collins, M.H.; Gonsalves, N.; Falk, G.W.; Spergel, J.M.; et al. A Clinical Severity Index for Eosinophilic Esophagitis: Development, Consensus, and Future Directions. Gastroenterology 2022, 163, 59–76. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).