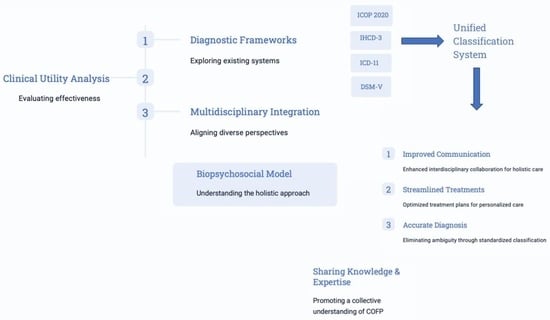
Advancements in Understanding and Classifying Chronic Orofacial Pain: Key Insights from Biopsychosocial Models and International Classifications (ICHD-3, ICD-11, ICOP)
Abstract
:1. Introduction
- exhaustive (including all clinical diseases or disorders within the field of interest);
- biologically plausible (symptoms and signs should correspond to known biological processes) and mutually exclusive (there should be no overlap between disease entities due to common symptoms);
- clinically useful (so that it can be used to aid in treatment and prognosis);
- reliable (applicable consistently and reproducibly among clinicians);
- simple for practical use.
- Chronic central neuropathic pain (MG 30.50);
- Chronic peripheral neuropathic pain (MG 30.51).
- NT: 8B82.0 under trigeminal disorders (Foundation ID in the ICD-11 browser: 1803581281);
- PIFP: 8B82.1 under trigeminal disorders (Foundation ID in the ICD-11 browser: 248232693);
- BMS: DA0F.0: sensory disturbances involving the orofacial region (Foundation ID in the ICD-11 browser: 618998878) (Figure 2).
2. Discussion and Future Directions
3. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A. Terminologies, Definitions, and Classifications Related to COFP
| Terminologies | Definitions |
| Allodynia | Pain evoked by a stimulus that is normally not harmful (mechanical, tactile) and does not cause tissue damage. Example: light brushing, light pressure, mild cold or heat. Note: the stimulus leads to an unexpectedly painful response. Lowered threshold—stimulus and mode of response differ. |
| Hyperalgesia | Increased sensitivity to pain, often disproportionate, produced by a harmful stimulus. Note: hyperalgesia reflects an increase in pain to above-threshold stimulation. Increased response: stimulus and mode of response are the same. |
| Hyperesthesia | Increased sensitivity to stimulation. The word is used to indicate both a decrease in the threshold to any stimulus and an increased response to normally recognized stimuli. It includes both allodynia and hyperalgesia, but more specific terms should be used wherever applicable. |
| Hyperapathia | Pain syndrome characterized by an abnormal painful reaction to a stimulus, especially a repetitive stimulus, as well as by an increased threshold. Note: it can occur with allodynia, hyperesthesia, hyperalgesia, or dysesthesia. There may be a delay in identifying the stimulus or incorrect localization with pain irradiation that can take on an explosive character. Increased threshold, increased response—stimulus and mode of response may be the same or different. |
| Hypoalgesia | Reduced sensitivity to pain produced by a normally painful stimulus. Relatively low pain in response to a stimulation that produces pain. Increased threshold, decreased response—stimulus and mode of response are the same. |
| Analgesia | Absence of pain in response to a harmful stimulus. |
| Hypoesthesia | Reduced sensitivity to stimulation that is normally painful. |
| Paresthesia | Spontaneous or provoked abnormal sensation that is not unpleasant. |
| Dysesthesia | Spontaneous or provoked abnormal sensation, unpleasant. |
| Trigeminal first neuron | First neuron of the somatosensory pathway that detects mechanical, thermal, or chemical stimuli at the peripheral end and transmits an action potential to the Gasser ganglion that synapses with the second-order neuron or projection neuron. |
| Nociceptor | Primary afferent (sensory) neuron that is exclusively activated by a painful stimulus. They are free nerve endings that may be thin myelinated Aδ fibers or unmyelinated C fibers. |
| Nociception | Process through which the nociceptor detects the painful stimulus and generates an action potential that propagates towards the higher centers. |
| Second-order neuron or projection neuron | Neuron that from the Gasser ganglion and/or the dorsal horn of the spinal cord that receives input from the primary afferent neuron and/or interneurons and projects it to the higher pain processing centers. |
| Interneuron | Neuron equipped with a cell body, axon, and dendrites present at the level of the Gasser ganglion and the spinal cord. It can be excitatory (glutamatergic) or inhibitory (GABAergic). |
| Spinothalamic tract | Tract of neurons that project from the Gasser ganglion and/or the spinal cord to the thalamus. |
| Central sensitization | Exaggerated or amplified response of the central nervous system to peripheral nociceptive and sensory stimuli. This amplified response and neuronal hyperexcitability contribute to the development of persistent pain characterized by hyperalgesia, allodynia, spontaneous pain, and referred pain. |
| Adaptation of terminology and definitions from the IASP. |
Appendix B. ICD-11 Extension Codes
- XS7G: Psychosocial factors present;
- XS8B: No psychosocial factors present;
- Determinants of severity:
- Intensity:
- XS5B: No pain;
- XS5D: Mild pain (NRS: 1–3; VAS: <31 mm);
- XS9Q: Moderate pain (NRS: 4–6; VAS: 31–54 mm);
- XS2E: Severe pain (NRS: 7–10; VAS: 55–100 mm);
- Discomfort:
- XS1J: No discomfort;
- XS3R: Mild discomfort (NRS: 1–3; VAS: <31 mm);
- XS7C: Moderate distress (NRS: 4–6; VAS: 31–54 mm);
- XS7N: Severe distress (NRS: 7–10; VAS: 55–100 mm);
- Interference:
- XS71: No pain-related interference;
- XS5R: Mild pain-related interference (NRS: 1–3; VAS: <31 mm);
- XS2L: Moderate pain-related interference (NRS: 4–6; VAS: 31–54 mm);
- XS2U: Severe pain-related interference (NRS: 7–10; VAS: 55–100 mm).
References
- Mills, S.E.E.; Nicolson, K.P.; Smith, B.H. Chronic Pain: A Review of Its Epidemiology and Associated Factors in Population-Based Studies. Br. J. Anaesth. 2019, 123, e273–e283. [Google Scholar] [CrossRef]
- Elliott, A.M.; Smith, B.H.; Penny, K.I.; Smith, W.C.; Chambers, W.A. The Epidemiology of Chronic Pain in the Community. Lancet 1999, 354, 1248–1252. [Google Scholar] [CrossRef] [PubMed]
- Vartiainen, P.; Roine, R.P.; Kalso, E.; Heiskanen, T. Worse Health-Related Quality of Life, Impaired Functioning and Psychiatric Comorbidities Are Associated with Excess Mortality in Patients with Severe Chronic Pain. Eur. J. Pain 2022, 26, 1135–1146. [Google Scholar] [CrossRef]
- Hadi, M.A.; McHugh, G.A.; Closs, S.J. Impact of Chronic Pain on Patients’ Quality of Life: A Comparative Mixed-Methods Study. J. Patient Exp. 2019, 6, 133–141. [Google Scholar] [CrossRef] [PubMed]
- Rayner, L.; Hotopf, M.; Petkova, H.; Matcham, F.; Simpson, A.; McCracken, L.M. Depression in Patients with Chronic Pain Attending a Specialised Pain Treatment Centre: Prevalence and Impact on Health Care Costs. Pain 2016, 157, 1472–1479. [Google Scholar] [CrossRef]
- Kawai, K.; Kawai, A.T.; Wollan, P.; Yawn, B.P. Adverse Impacts of Chronic Pain on Health-Related Quality of Life, Work Productivity, Depression and Anxiety in a Community-Based Study. Fam. Pract. 2017, 34, 656–661. [Google Scholar] [CrossRef]
- Institute of Medicine (US) Committee on Advancing Pain Research, Care, and Education. Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research. In The National Academies Collection: Reports Funded by National Institutes of Health; National Academies Press (US): Washington, DC, USA, 2011. [Google Scholar]
- Koesling, D.; Bozzaro, C. Chronic Pain Patients’ Need for Recognition and Their Current Struggle. Med. Health Care Philos. 2021, 24, 563–572. [Google Scholar] [CrossRef] [PubMed]
- Varenna, M.; Crotti, C.; Ughi, N.; Zucchi, F.; Caporali, R. Determinants of Diagnostic Delay in Complex Regional Pain Syndrome Type 1: An Observational Study of 180 Consecutive New Cases. J. Clin. Rheumatol. 2021, 27, e491–e495. [Google Scholar] [CrossRef]
- Nicola, M.; Correia, H.; Ditchburn, G.; Drummond, P.D. Defining Pain-Validation: The Importance of Validation in Reducing the Stresses of Chronic Pain. Front. Pain Res. 2022, 3, 884335. [Google Scholar] [CrossRef]
- Chmieliauskaite, M.; Stelson, E.A.; Epstein, J.B.; Klasser, G.D.; Farag, A.; Carey, B.; Albuquerque, R.; Mejia, L.; Ariyawardana, A.; Nasri-Heir, C.; et al. Consensus Agreement to Rename Burning Mouth Syndrome and Improve ICD-11 Disease Criteria: An International Delphi Study. Pain 2021, 162, 2548–2557. [Google Scholar] [CrossRef]
- ICD-11 for Mortality and Morbidity Statistics. Available online: https://icd.who.int/browse/11/2018/mms/en (accessed on 11 November 2023).
- National Pain Strategy Overview|IPRCC. Available online: https://www.iprcc.nih.gov/national-pain-strategy-overview (accessed on 13 November 2023).
- The Lancet. ICD-11. Lancet 2019, 393, 2275. [Google Scholar] [CrossRef]
- Heath, L.; Philip, A. Chronic Pain Care: Time for Excellence. Fam. Med. Community Health 2020, 8, e000285. [Google Scholar] [CrossRef]
- Sessle, B.J. Chronic Orofacial Pain: Models, Mechanisms, and Genetic and Related Environmental Influences. Int. J. Mol. Sci. 2021, 22, 7112. [Google Scholar] [CrossRef]
- May, A.; Benoliel, R.; Imamura, Y.; Pigg, M.; Baad-Hansen, L.; Svensson, P.; Hoffmann, J. Orofacial Pain for Clinicians: A Review of Constant and Attack-like Facial Pain Syndromes. Cephalalgia 2023, 43, 03331024231187160. [Google Scholar] [CrossRef] [PubMed]
- Costa, Y.M.; De Koninck, B.P.; Elsaraj, S.M.; Exposto, F.G.; Herrero Babiloni, A.; Kapos, F.P.; Sharma, S.; Shimada, A. Orofacial Pain Education in Dentistry: A Path to Improving Patient Care and Reducing the Population Burden of Chronic Pain. J. Dent. Educ. 2021, 85, 349–358. [Google Scholar] [CrossRef] [PubMed]
- Kappesser, J. The Facial Expression of Pain in Humans Considered from a Social Perspective. Philos. Trans. R. Soc. B Biol. Sci. 2019, 374, 20190284. [Google Scholar] [CrossRef] [PubMed]
- Häggman-Henrikson, B.; Liv, P.; Ilgunas, A.; Visscher, C.M.; Lobbezoo, F.; Durham, J.; Lövgren, A. Increasing Gender Differences in the Prevalence and Chronification of Orofacial Pain in the Population. Pain 2020, 161, 1768–1775. [Google Scholar] [CrossRef] [PubMed]
- Benoliel, R.; Pertes, R.A.; Eliav, E. Chapter 17—OROFACIAL PAIN. In Current Therapy in Pain; Smith, H.S., Ed.; W.B. Saunders: Philadelphia, PA, USA, 2009. [Google Scholar] [CrossRef]
- Taheri, J.B.; Anbari, F.; Sani, S.K.; Mirmoezi, S.M.; Khalighi, H.R. A 10-Year Overview of Chronic Orofacial Pain in Patients at an Oral Medicine Center in Iran. J. Dent. Anesth. Pain. Med. 2022, 22, 289–294. [Google Scholar] [CrossRef]
- Kumar, A.; Brennan, M.T. Differential Diagnosis of Orofacial Pain and Temporomandibular Disorder. Dent. Clin. North Am. 2013, 57, 419–428. [Google Scholar] [CrossRef]
- Peng, K.-P.; Oppermann, T. Orofacial Pain Disorders: An Overview and Diagnostic Approach. Cephalalgia Rep. 2022, 5, 25158163221097349. [Google Scholar] [CrossRef]
- Adamo, D.; Spagnuolo, G. Burning Mouth Syndrome: An Overview and Future Perspectives. Int. J. Environ. Res. Public Health 2022, 20, 682. [Google Scholar] [CrossRef]
- Meints, S.M.; Edwards, R.R. Evaluating Psychosocial Contributions to Chronic Pain Outcomes. Prog. Neuropsychopharmacol. Biol. Psychiatry 2018, 87, 168–182. [Google Scholar] [CrossRef]
- Párraga, J.P.; Castellanos, A. A Manifesto in Defense of Pain Complexity: A Critical Review of Essential Insights in Pain Neuroscience. J. Clin. Med. 2023, 12, 7080. [Google Scholar] [CrossRef]
- Jensen, M.P.; Moore, M.R.; Bockow, T.B.; Ehde, D.M.; Engel, J.M. Psychosocial Factors and Adjustment to Chronic Pain in Persons with Physical Disabilities: A Systematic Review. Arch. Phys. Med. Rehabil. 2011, 92, 146–160. [Google Scholar] [CrossRef] [PubMed]
- Prego-Domínguez, J.; Skillgate, E.; Orsini, N.; Takkouche, B. Social Factors and Chronic Pain: The Modifying Effect of Sex in the Stockholm Public Health Cohort Study. Rheumatology 2022, 61, 1802–1809. [Google Scholar] [CrossRef] [PubMed]
- Borsook, D.; Kalso, E. Transforming Pain Medicine: Adapting to Science and Society. Eur. J. Pain 2013, 17, 1109–1125. [Google Scholar] [CrossRef]
- Ablin, J.N.; Buskila, D. Personalized Treatment of Pain. Curr. Rheumatol. Rep. 2013, 15, 298. [Google Scholar] [CrossRef] [PubMed]
- Hui, D.; Bruera, E. A Personalized Approach to Assessing and Managing Pain in Patients with Cancer. J. Clin. Oncol. 2014, 32, 1640–1646. [Google Scholar] [CrossRef]
- Scholz, J.; Finnerup, N.B.; Attal, N.; Aziz, Q.; Baron, R.; Bennett, M.I.; Benoliel, R.; Cohen, M.; Cruccu, G.; Davis, K.D.; et al. The IASP Classification of Chronic Pain for ICD-11: Chronic Neuropathic Pain. Pain 2019, 160, 53–59. [Google Scholar] [CrossRef]
- Cohen, M.; Quintner, J.; van Rysewyk, S. Reconsidering the International Association for the Study of Pain Definition of Pain. Pain. Rep. 2018, 3, e634. [Google Scholar] [CrossRef]
- Raja, S.N.; Carr, D.B.; Cohen, M.; Finnerup, N.B.; Flor, H.; Gibson, S.; Keefe, F.; Mogil, J.S.; Ringkamp, M.; Sluka, K.A.; et al. The Revised IASP Definition of Pain: Concepts, Challenges, and Compromises. Pain 2020, 161, 1976–1982. [Google Scholar] [CrossRef] [PubMed]
- Treede, R.-D.; Rief, W.; Barke, A.; Aziz, Q.; Bennett, M.I.; Benoliel, R.; Cohen, M.; Evers, S.; Finnerup, N.B.; First, M.B.; et al. Chronic Pain as a Symptom or a Disease: The IASP Classification of Chronic Pain for the International Classification of Diseases (ICD-11). Pain 2019, 160, 19–27. [Google Scholar] [CrossRef] [PubMed]
- Nicholas, M.; Vlaeyen, J.W.S.; Rief, W.; Barke, A.; Aziz, Q.; Benoliel, R.; Cohen, M.; Evers, S.; Giamberardino, M.A.; Goebel, A.; et al. IASP Taskforce for the Classification of Chronic Pain. The IASP classification of chronic pain for ICD-11: Chronic primary pain. Pain. 2019, 160, 28–37. [Google Scholar] [CrossRef] [PubMed]
- Fitzcharles, M.-A.; Cohen, S.P.; Clauw, D.J.; Littlejohn, G.; Usui, C.; Häuser, W. Nociplastic Pain: Towards an Understanding of Prevalent Pain Conditions. Lancet 2021, 397, 2098–2110. [Google Scholar] [CrossRef] [PubMed]
- St John Smith, E. Advances in Understanding Nociception and Neuropathic Pain. J. Neurol. 2018, 265, 231–238. [Google Scholar] [CrossRef]
- Dubin, A.E.; Patapoutian, A. Nociceptors: The Sensors of the Pain Pathway. J. Clin. Investig. 2010, 120, 3760–3772. [Google Scholar] [CrossRef]
- Eilers, H.; Schumacher, M.A. Mechanosensitivity of Primary Afferent Nociceptors in the Pain Pathway. In Mechanosensitivity in Cells and Tissues; Kamkin, A., Kiseleva, I., Eds.; Academia: Moscow, Russia, 2005. [Google Scholar]
- Tajti, J.; Szok, D.; Csáti, A.; Szabó, Á.; Tanaka, M.; Vécsei, L. Exploring Novel Therapeutic Targets in the Common Pathogenic Factors in Migraine and Neuropathic Pain. Int. J. Mol. Sci. 2023, 24, 4114. [Google Scholar] [CrossRef]
- Costigan, M.; Scholz, J.; Woolf, C.J. Neuropathic Pain. Annu. Rev. Neurosci. 2009, 32, 1–32. [Google Scholar] [CrossRef]
- Nie, L.; Jiang, L.; Quinn, J.P.; Grubb, B.D.; Wang, M. TRPA1-Mediated Src Family Kinases Activity Facilitates Cortical Spreading Depression Susceptibility and Trigeminovascular System Sensitization. Int. J. Mol. Sci. 2021, 22, 12273. [Google Scholar] [CrossRef]
- Raju, H.; Tadi, P. Neuroanatomy, Somatosensory Cortex. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2023. [Google Scholar]
- Spekker, E.; Tanaka, M.; Szabó, Á.; Vécsei, L. Neurogenic Inflammation: The Participant in Migraine and Recent Advancements in Translational Research. Biomedicines 2022, 10, 76. [Google Scholar] [CrossRef]
- Finnerup, N.B.; Haroutounian, S.; Kamerman, P.; Baron, R.; Bennett, D.L.H.; Bouhassira, D.; Cruccu, G.; Freeman, R.; Hansson, P.; Nurmikko, T.; et al. Neuropathic Pain: An Updated Grading System for Research and Clinical Practice. Pain 2016, 157, 1599–1606. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, M.; Török, N.; Tóth, F.; Szabó, Á.; Vécsei, L. Co-Players in Chronic Pain: Neuroinflammation and the Tryptophan-Kynurenine Metabolic Pathway. Biomedicines 2021, 9, 897. [Google Scholar] [CrossRef] [PubMed]
- Baron, R. Neuropathic Pain: A Clinical Perspective. In Handbook of Experimental Pharmacology; Springer: Berlin/Heidelberg, Germany, 2009; pp. 3–30. [Google Scholar] [CrossRef]
- Toraman, A.; Toraman, E.; Özkaraca, M.; Budak, H. Evaluated Periodontal Tissues and Oxidative Stress in Rats with Neuropathic Pain-like Behavior. Mol. Biol. Rep. 2023, 50, 9315–9322. [Google Scholar] [CrossRef] [PubMed]
- Attal, N.; Bouhassira, D.; Baron, R. Diagnosis and Assessment of Neuropathic Pain through Questionnaires. Lancet Neurol. 2018, 17, 456–466. [Google Scholar] [CrossRef]
- Kosek, E.; Cohen, M.; Baron, R.; Gebhart, G.F.; Mico, J.-A.; Rice, A.S.C.; Rief, W.; Sluka, A.K. Do We Need a Third Mechanistic Descriptor for Chronic Pain States? Pain 2016, 157, 1382–1386. [Google Scholar] [CrossRef]
- Alcántara Montero, A. Importance of Nociplastic Pain in Patients with Rheumatic Diseases. Clinics 2023, 78, 100309. [Google Scholar] [CrossRef]
- Kosek, E.; Clauw, D.; Nijs, J.; Baron, R.; Gilron, I.; Harris, R.E.; Mico, J.-A.; Rice, A.S.C.; Sterling, M. Chronic Nociplastic Pain Affecting the Musculoskeletal System: Clinical Criteria and Grading System. Pain 2021, 162, 2629. [Google Scholar] [CrossRef] [PubMed]
- Baliki, M.N.; Mansour, A.R.; Baria, A.T.; Apkarian, A.V. Functional Reorganization of the Default Mode Network across Chronic Pain Conditions. PLoS ONE 2014, 9, e106133. [Google Scholar] [CrossRef] [PubMed]
- Woolf, C.J.; Mannion, R.J. Neuropathic Pain: Aetiology, Symptoms, Mechanisms, and Management. Lancet 1999, 353, 1959–1964. [Google Scholar] [CrossRef]
- Bonezzi, C.; Fornasari, D.; Cricelli, C.; Magni, A.; Ventriglia, G. Not All Pain Is Created Equal: Basic Definitions and Diagnostic Work-Up. Pain Ther. 2020, 9, 1–15. [Google Scholar] [CrossRef]
- Gatchel, R.J.; Peng, Y.B.; Peters, M.L.; Fuchs, P.N.; Turk, D.C. The Biopsychosocial Approach to Chronic Pain: Scientific Advances and Future Directions. Psychol. Bull. 2007, 133, 581–624. [Google Scholar] [CrossRef]
- Gevers-Montoro, C.; Liew, B.X.W.; Deldar, Z.; Conesa-Buendia, F.M.; Ortega-De Mues, A.; Falla, D.; Khatibi, A. A Network Analysis on Biopsychosocial Factors and Pain-Related Outcomes Assessed during a COVID-19 Lockdown. Sci. Rep. 2023, 13, 4399. [Google Scholar] [CrossRef]
- Johnson, K.B.; Wei, W.; Weeraratne, D.; Frisse, M.E.; Misulis, K.; Rhee, K.; Zhao, J.; Snowdon, J.L. Precision Medicine, AI, and the Future of Personalized Health Care. Clin. Transl. Sci. 2021, 14, 86–93. [Google Scholar] [CrossRef]
- Abramson, L.; Petranker, R.; Marom, I.; Aviezer, H. Social Interaction Context Shapes Emotion Recognition through Body Language, Not Facial Expressions. Emotion 2021, 21, 557–568. [Google Scholar] [CrossRef] [PubMed]
- Frith, C. Role of Facial Expressions in Social Interactions. Philos. Trans. R. Soc. Lond. B Biol. Sci. 2009, 364, 3453–3458. [Google Scholar] [CrossRef]
- Langeslag, S.J.; Gootjes, L.; van Strien, J.W. The Effect of Mouth Opening in Emotional Faces on Subjective Experience and the Early Posterior Negativity Amplitude. Brain Cogn. 2018, 127, 51–59. [Google Scholar] [CrossRef]
- Hargreaves, K.M. CONGRESS Orofacial Pain. Pain 2011, 152, S25–S32. [Google Scholar] [CrossRef] [PubMed]
- Zimet, G.D.; Dahlem, N.W.; Zimet, S.G.; Farley, G.K. The Multidimensional Scale of Perceived Social Support. J. Personal. Assess. 1988, 52, 30–41. [Google Scholar] [CrossRef]
- Canfora, F.; Calabria, E.; Pecoraro, G.; D′Aniello, L.; Aria, M.; Marenzi, G.; Sammartino, P.; Mignogna, M.D.; Adamo, D. The Use of Self-Report Questionnaires in an Analysis of the Multidimensional Aspects of Pain and a Correlation with the Psychological Profile and Quality of Life in Patients with Burning Mouth Syndrome: A Case-Control Study. J. Oral Rehabil. 2022, 49, 890–914. [Google Scholar] [CrossRef] [PubMed]
- Gobel, H.; The International Classification of Headache Disorders. ICHD-3. Available online: https://ichd-3.org/ (accessed on 9 February 2022).
- Weiss, A.L.; Ehrhardt, K.P.; Tolba, R. Atypical Facial Pain: A Comprehensive, Evidence-Based Review. Curr. Pain Headache Rep. 2017, 21, 8. [Google Scholar] [CrossRef] [PubMed]
- Ziegeler, C.; Beikler, T.; Gosau, M.; May, A. Idiopathic Facial Pain Syndromes–An Overview and Clinical Implications. Dtsch. Arztebl. Int. 2021, 118, 81–87. [Google Scholar] [CrossRef]
- Van Deun, L.; de Witte, M.; Goessens, T.; Halewyck, S.; Ketelaer, M.-C.; Matic, M.; Moens, M.; Vaes, P.; Van Lint, M.; Versijpt, J. Facial Pain: A Comprehensive Review and Proposal for a Pragmatic Diagnostic Approach. Eur. Neurol. 2020, 83, 5–16. [Google Scholar] [CrossRef] [PubMed]
- International Classification of Orofacial Pain, 1st Edition (ICOP). Cephalalgia 2020, 40, 129–221. [CrossRef] [PubMed]
- Labanca, M.; Gianò, M.; Franco, C.; Rezzani, R. Orofacial Pain and Dentistry Management: Guidelines for a More Comprehensive Evidence-Based Approach. Diagnostics 2023, 13, 2854. [Google Scholar] [CrossRef] [PubMed]
- Crandall, J.A. An Introduction to Orofacial Pain. Dent. Clin. North Am. 2018, 62, 511–523. [Google Scholar] [CrossRef] [PubMed]
- Ghurye, S.; McMillan, R. Orofacial Pain—An Update on Diagnosis and Management. Br. Dent. J. 2017, 223, 639–647. [Google Scholar] [CrossRef]
- Ananthan, S.; Benoliel, R. Chronic Orofacial Pain. J. Neural Transm. 2020, 127, 575–588. [Google Scholar] [CrossRef]
- Hadlaq, E.M.; Khan, H.; Mubayrik, A.B.; Almuflehi, N.S.; Mawardi, H. Dentists’ Knowledge of Chronic Orofacial Pain. Niger. J. Clin. Pract. 2019, 22, 1365–1371. [Google Scholar] [CrossRef]
- Tomoyasu, Y.; Higuchi, H.; Mori, M.; Takaya, K.; Honda, Y.; Yamane, A.; Yabuki, A.; Hayashi, T.; Ishii-Maruyama, M.; Jinzenji, A.; et al. Chronic Orofacial Pain in Dental Patients: Retrospective Investigation over 12 Years. Acta Med. Okayama 2014, 68, 269–275. [Google Scholar] [CrossRef]
- Sarlani, E.; Balciunas, B.A.; Grace, E.G. Orofacial Pain—Part I: Assessment and Management of Musculoskeletal and Neuropathic Causes. AACN Clin. Issues 2005, 16, 333–346. [Google Scholar] [CrossRef]
- Adamo, D.; Mignogna, M.D.; Wang, X.-Q.; Femminella, G.D. Editorial: Chronic Pain in Neuropsychiatric Diseases. Front. Hum. Neurosci. 2023, 17, 1213217. [Google Scholar] [CrossRef]
- Veerapaneni, K.D.; Kapoor, N.; Veerapaneni, P.; Nalleballe, K. Trigeminal Neuropathy. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2023. [Google Scholar]
- Fisher, R.; Clarkson, E. Medication Management of Neuropathic Pain Disorders. Dent. Clin. North Am. 2024, 68, 121–131. [Google Scholar] [CrossRef]
- Heir, G.M.; Ananthan, S.; Kalladka, M.; Kuchukulla, M.; Renton, T. Persistent Idiopathic Dentoalveolar Pain: Is It a Central Pain Disorder? Dent. Clin. North Am. 2023, 67, 71–83. [Google Scholar] [CrossRef] [PubMed]
- Ayoub, L.J.; Seminowicz, D.A.; Moayedi, M. A Meta-Analytic Study of Experimental and Chronic Orofacial Pain Excluding Headache Disorders. NeuroImage Clin. 2018, 20, 901–912. [Google Scholar] [CrossRef]
- Lovette, B.C.; Bannon, S.M.; Spyropoulos, D.C.; Vranceanu, A.-M.; Greenberg, J. “I Still Suffer Every Second of Every Day”: A Qualitative Analysis of the Challenges of Living with Chronic Orofacial Pain. J. Pain Res. 2022, 15, 2139–2148. [Google Scholar] [CrossRef]
- Vickers, E.R.; Boocock, H. Chronic Orofacial Pain Is Associated with Psychological Morbidity and Negative Personality Changes: A Comparison to the General Population. Aust. Dent. J. 2005, 50, 21–30. [Google Scholar] [CrossRef] [PubMed]
- Foreman, P.A. Chronic Orofacial Pain: A Clinical Challenge. N. Z. Dent. J. 2008, 104, 44–48. [Google Scholar] [PubMed]
- Setty, S.; David, J. Classification and Epidemiology of Orofacial Pain. In Orofacial Pain: A Clinician’s Guide; Vadivelu, N., Vadivelu, A., Kaye, A.D., Eds.; Springer International Publishing: Cham, Switzerland, 2014. [Google Scholar] [CrossRef]
- Derafshi, R.; Rezazadeh, F.; Ghapanchi, J.; Basandeh Sharif, D.; Farzin, M. Prevalence of Chronic Orofacial Pain in Elderly Patients Referred to Shiraz Dental School From 2005 to 2017. Anesth. Pain Med. 2019, 9, e91182. [Google Scholar] [CrossRef] [PubMed]
- Isong, U.; Gansky, S.A.; Plesh, O. Temporomandibular Joint and Muscle Disorder-Type Pain in US Adults: The National Health Interview Survey. J. Orofac. Pain 2008, 22, 317–322. [Google Scholar]
- Khawaja, S.N.; Alaswaiti, O.F.; Scrivani, S.J. Burning Mouth Syndrome. Dent. Clin. North. Am. 2023, 67, 49–60. [Google Scholar] [CrossRef]
- Wu, S.; Zhang, W.; Yan, J.; Noma, N.; Young, A.; Yan, Z. Worldwide Prevalence Estimates of Burning Mouth Syndrome: A Systematic Review and Meta-Analysis. Oral Dis. 2021, 28, 1431–1440. [Google Scholar] [CrossRef]
- Kohorst, J.J.; Bruce, A.J.; Torgerson, R.R.; Schenck, L.A.; Davis, M.D.P. The Prevalence of Burning Mouth Syndrome: A Population-Based Study. Br. J. Dermatol. 2015, 172, 1654–1656. [Google Scholar] [CrossRef]
- Adamo, D.; Canfora, F.; Calabria, E.; Coppola, N.; Sansone, M.; Spagnuolo, G.; Pecoraro, G.; Aria, M.; D’Aniello, L.; Mignogna, M.D.; et al. Burning Mouth Syndrome and Hypertension: Prevalence, Gender Differences and Association with Pain and Psycho-Social Characteristics-A Case Control Study. Int. J. Environ. Res. Public Health 2023, 20, 2040. [Google Scholar] [CrossRef]
- Araya, E.I.; Claudino, R.F.; Piovesan, E.J.; Chichorro, J.G. Trigeminal Neuralgia: Basic and Clinical Aspects. Curr. Neuropharmacol. 2020, 18, 109–119. [Google Scholar] [CrossRef] [PubMed]
- Khawaja, S.N.; Scrivani, S.J. Trigeminal Neuralgia. Dent. Clin. North Am. 2023, 67, 99–115. [Google Scholar] [CrossRef] [PubMed]
- Mungoven, T.J.; Meylakh, N.; Marciszewski, K.K.; Macefield, V.G.; Macey, P.M.; Henderson, L.A. Microstructural Changes in the Trigeminal Nerve of Patients with Episodic Migraine Assessed Using Magnetic Resonance Imaging. J. Headache Pain 2020, 21, 59. [Google Scholar] [CrossRef] [PubMed]
- Laakso, S.M.; Hekali, O.; Kurdo, G.; Martola, J.; Sairanen, T.; Atula, S. Trigeminal Neuralgia in Multiple Sclerosis: Prevalence and Association with Demyelination. Acta Neurol. Scand. 2020, 142, 139–144. [Google Scholar] [CrossRef] [PubMed]
- Schweiger, V.; Nocini, R.; De Santis, D.; Procacci, P.; Zanette, G.; Secchettin, E.; Del Balzo, G.; Fior, A.; Martini, A.; Nizzero, M.; et al. Persistent Idiopathic Facial Pain (PIFP) in Patients Referred to a Multidisciplinary Centre in Italy: A Retrospective Observational Study. J. Clin. Med. 2022, 11, 3821. [Google Scholar] [CrossRef] [PubMed]
- Haendel, M.A.; Chute, C.G.; Robinson, P.N. Classification, Ontology, and Precision Medicine. N. Engl. J. Med. 2018, 379, 1452–1462. [Google Scholar] [CrossRef]
- Fillingim, R.B.; Bruehl, S.; Dworkin, R.H.; Dworkin, S.F.; Loeser, J.D.; Turk, D.C.; Widerstrom-Noga, E.; Arnold, L.; Bennett, R.; Edwards, R.R.; et al. The ACTTION-American Pain Society Pain Taxonomy (AAPT): An Evidence-Based and Multidimensional Approach to Classifying Chronic Pain Conditions. J. Pain 2014, 15, 241–249. [Google Scholar] [CrossRef]
- Headache Classification Committee of the International Headache Society (IHS). The International Classification of Headache Disorders, 3rd Edition (Beta Version). Cephalalgia 2013, 33, 629–808. [Google Scholar] [CrossRef] [PubMed]
- Manzoni, G.C.; Grisendi, I.; Torelli, P. ICHD-3: What Changes Do We Need Regarding Migraine? Curr. Pain Headache Rep. 2011, 15, 170–176. [Google Scholar] [CrossRef] [PubMed]
- Göbel, C.H.; Karstedt, S.C.; Münte, T.F.; Göbel, H.; Wolfrum, S.; Lebedeva, E.R.; Olesen, J.; Royl, G. ICHD-3 Is Significantly More Specific than ICHD-3 Beta for Diagnosis of Migraine with Aura and with Typical Aura. J. Headache Pain 2020, 21, 2. [Google Scholar] [CrossRef]
- Gobel, H.; 13.11 Burning Mouth Syndrome (BMS). ICHD-3. Available online: https://ichd-3.org/13-painful-cranial-neuropathies-and-other-facial-pains/13-11-persistent-idiopathic-facial-pain-pifp/ (accessed on 9 February 2022).
- Benoliel, R.; Svensson, P.; Evers, S.; Wang, S.-J.; Barke, A.; Korwisi, B.; Rief, W.; Treede, R.-D. IASP Taskforce for the Classification of Chronic Pain. The IASP Classification of Chronic Pain for ICD-11: Chronic Secondary Headache or Orofacial Pain. Pain 2019, 160, 60–68. [Google Scholar] [CrossRef] [PubMed]
- Peng, K.-P.; Benoliel, R.; May, A. A Review of Current Perspectives on Facial Presentations of Primary Headaches. J. Pain Res. 2022, 15, 1613–1621. [Google Scholar] [CrossRef]
- Üstün Özek, S. A Study on the Correlation between Pain Frequency and Severity and Vitamin B12 Levels in Episodic and Chronic Migraine. Arq. Neuropsiquiatr. 2022, 80, 586–592. [Google Scholar] [CrossRef] [PubMed]
- Akgün, N.; Acıman Demirel, E.; Açıkgöz, M.; Çelebi, U.; Köktürk, F.; Atasoy, H.T. The Effect of Weather Variables on the Severity, Duration, and Frequency of Headache Attacks in the Cases of Episodic Migraine and Episodic Tension-Type Headache. Turk. J. Med. Sci. 2021, 51, 1406–1412. [Google Scholar] [CrossRef]
- Regier, D.A.; Kuhl, E.A.; Kupfer, D.J. The DSM-5: Classification and Criteria Changes. World Psychiatry 2013, 12, 92–98. [Google Scholar] [CrossRef] [PubMed]
- Parolini, F.; Goethel, M.; Becker, K.; Fernandes, C.; Fernandes, R.J.; Ervilha, U.F.; Santos, R.; Vilas-Boas, J.P. Breaking Barriers: Artificial Intelligence Interpreting the Interplay between Mental Illness and Pain as Defined by the International Association for the Study of Pain. Biomedicines 2023, 11, 2042. [Google Scholar] [CrossRef]
- Chen, C.; Nakagawa, S. Recent Advances in the Study of the Neurobiological Mechanisms behind the Effects of Physical Activity on Mood, Resilience and Emotional Disorders. Adv. Clin. Exp. Med. 2023, 32, 937–942. [Google Scholar] [CrossRef]
- Brady, R.E.; Braz, A.N. Challenging Interactions Between Patients With Severe Health Anxiety and the Healthcare System: A Qualitative Investigation. J. Prim. Care Community Health 2023, 14, 21501319231214876. [Google Scholar] [CrossRef] [PubMed]
- Pai, A.; Suris, A.M.; North, C.S. Posttraumatic Stress Disorder in the DSM-5: Controversy, Change, and Conceptual Considerations. Behav. Sci. 2017, 7, 7. [Google Scholar] [CrossRef]
- Stein, D.J.; Palk, A.C.; Kendler, K.S. What Is a Mental Disorder? An Exemplar-Focused Approach. Psychol. Med. 2021, 51, 894–901. [Google Scholar] [CrossRef] [PubMed]
- Katz, J.; Rosenbloom, B.N.; Fashler, S. Chronic Pain, Psychopathology, and DSM-5 Somatic Symptom Disorder. Can. J. Psychiatry 2015, 60, 160–167. [Google Scholar] [CrossRef]
- Henningsen, P. Management of Somatic Symptom Disorder. Dialogues Clin. Neurosci. 2018, 20, 23–31. [Google Scholar] [CrossRef] [PubMed]
- Löwe, B.; Levenson, J.; Depping, M.; Hüsing, P.; Kohlmann, S.; Lehmann, M.; Shedden-Mora, M.; Toussaint, A.; Uhlenbusch, N.; Weigel, A. Somatic Symptom Disorder: A Scoping Review on the Empirical Evidence of a New Diagnosis. Psychol. Med. 2021, 52, 632–648. [Google Scholar] [CrossRef]
- Engle, R.L.; Mohr, D.C.; Holmes, S.K.; Seibert, M.N.; Afable, M.; Leyson, J.; Meterko, M. Evidence-Based Practice and Patient-Centered Care: Doing Both Well. Health Care Manag. Rev. 2021, 46, 174–184. [Google Scholar] [CrossRef] [PubMed]
- Greene, S.M.; Tuzzio, L.; Cherkin, D. A Framework for Making Patient-Centered Care Front and Center. Perm. J. 2012, 16, 49–53. [Google Scholar] [CrossRef]
- Zeh, S.; Christalle, E.; Zill, J.M.; Härter, M.; Block, A.; Scholl, I. What Do Patients Expect? Assessing Patient-Centredness from the Patients’ Perspective: An Interview Study. BMJ Open 2021, 11, e047810. [Google Scholar] [CrossRef]
- Priyank, H.; Shankar Prasad, R.; Shivakumar, S.; Sayed Abdul, N.; Pathak, A.; Cervino, G.; Cicciù, M.; Minervini, G. Management Protocols of Chronic Orofacial Pain: A Systematic Review. Saudi Dent. J. 2023, 35, 395–402. [Google Scholar] [CrossRef]
- Kopruszinski, C.M.; Porreca, F.; Chichorro, J.G. Editorial: Chronic Orofacial Pain. Front. Pain Res. 2023, 3, 1086256. [Google Scholar] [CrossRef]
- Fillingim, R.B. Individual Differences in Pain: Understanding the Mosaic That Makes Pain Personal. Pain 2017, 158, S11–S18. [Google Scholar] [CrossRef]
- McGrath, P.A. Psychological Aspects of Pain Perception. Arch. Oral. Biol. 1994, 39, 55S–62S. [Google Scholar] [CrossRef]
- Lang-Illievich, K.; Rumpold-Seitlinger, G.; Szilagyi, I.S.; Dorn, C.; Sailer, M.; Schittek, G.A.; Klivinyi, C.; Bornemann-Cimenti, H. Biological, Psychological, and Social Factors Associated with Worsening of Chronic Pain during the First Wave of the COVID-19 Pandemic: A Cross-Sectional Survey. Br. J. Anaesth. 2021, 127, e37–e39. [Google Scholar] [CrossRef] [PubMed]
- Klasser, G.D.; Manfredini, D.; Goulet, J.-P.; De Laat, A. Oro-Facial Pain and Temporomandibular Disorders Classification Systems: A Critical Appraisal and Future Directions. J. Oral Rehabil. 2018, 45, 258–268. [Google Scholar] [CrossRef]
- Sessle, B.J. Fifty Years of Development of Neuroscientific Insights into Oro-Facial Pain and Its Control. J. Oral Rehabil. 2023, 50, 860–876. [Google Scholar] [CrossRef] [PubMed]
- Yao, A.L.; Barad, M. Diagnosis and Management of Chronic Facial Pain. BJA Educ. 2020, 20, 120–125. [Google Scholar] [CrossRef] [PubMed]
- Raman, S.; Ikutame, D.; Okura, K.; Matsuka, Y. Targeted Therapy for Orofacial Pain: A Novel Perspective for Precision Medicine. J. Pers. Med. 2023, 13, 565. [Google Scholar] [CrossRef]
- Von Piekartz, H.; Geitner, G.; Möller, D.; Braun, R.; Hall, T. Does Combined Individualized Orofacial Manual Therapy, Pain Neuroscience Education, and Brain Training Change Orofacial Pain, Chronic Face Dysfunction, (Facial) Body Perception and Pain? An Observational Mixed Methods Case Series Study. J. Man. Manip. Ther. 2022, 30, 180–191. [Google Scholar] [CrossRef]
- Wolf, E. Chronic Orofacial Pain. Understanding Patients from Two Perspectives: The Clinical View and the Patient’s Experience. Swed. Dent. J. Suppl. 2006, 9–69. [Google Scholar]
- Woda, A.; Pionchon, P. A Unified Concept of Idiopathic Orofacial Pain: Clinical Features. J. Orofac. Pain 1999, 13, 172–184. [Google Scholar]
- Ren, K.; Vickers, R.; Murillo, J.; Ruparel, N.B. Revolutionizing Orofacial Pain Management: The Promising Potential of Stem Cell Therapy. Front. Pain Res. 2023, 4, 1239633. [Google Scholar] [CrossRef]
- Chamani, G.; Zarei, M.R.; Rad, M.; Mafi, S. Comparison of Low-Level Laser Therapy and Standard Treatment for Temporomandibular Disorders: An Assessment of Therapeutic and Placebo Effects. J. Oral Rehabil. 2023. [CrossRef] [PubMed]
- Sangalli, L.; Alessandri-Bonetti, A.; Kapos, F.P.; Boggero, I.A. Occupations Associated with Treatment Seeking and Biopsychosocial Functioning at a Tertiary Orofacial Pain Clinic: A Cross-Sectional Study. J. Am. Dent. Assoc. 2023. Online ahead of print. [Google Scholar] [CrossRef]
- Clark, T.S. Interdisciplinary Treatment for Chronic Pain: Is It Worth the Money? In Baylor University Medical Center Proceedings; Taylor & Francis: Abingdon, UK, 2000; Volume 13, pp. 240–243. [Google Scholar]
- Danilov, A.; Danilov, A.; Barulin, A.; Kurushina, O.; Latysheva, N. Interdisciplinary Approach to Chronic Pain Management. Postgrad. Med. 2020, 132, 5–9. [Google Scholar] [CrossRef] [PubMed]
- Jangwan, N.S.; Ashraf, G.M.; Ram, V.; Singh, V.; Alghamdi, B.S.; Abuzenadah, A.M.; Singh, M.F. Brain Augmentation and Neuroscience Technologies: Current Applications, Challenges, Ethics and Future Prospects. Front. Syst. Neurosci. 2022, 16, 1000495. [Google Scholar] [CrossRef]
- Black, J.E.; Kueper, J.K.; Williamson, T.S. An Introduction to Machine Learning for Classification and Prediction. Fam. Pract. 2023, 40, 200–204. [Google Scholar] [CrossRef]
- Xu, X.; Huang, Y. Objective Pain Assessment: A Key for the Management of Chronic Pain. F1000Res 2020, 9, F1000. [Google Scholar] [CrossRef]
- Lee, J.; Park, S.-H.; Ju, J.H.; Cho, J.H. Application of a Real-Time Pain Monitoring System in Korean Fibromyalgia Patients: A Pilot Study. Int. J. Rheum. Dis. 2019, 22, 934–939. [Google Scholar] [CrossRef] [PubMed]
- Eldabe, S.; Obara, I.; Panwar, C.; Caraway, D. Biomarkers for Chronic Pain: Significance and Summary of Recent Advances. Pain Res. Manag. 2022, 2022, 1940906. [Google Scholar] [CrossRef]
- Strand, N.; Maloney, J.; Tieppo Francio, V.; Murphy, M.; Turkiewicz, M.; El Helou, A.; Maita, M.; Covington, S.; Singh, N.; Peck, J.; et al. Advances in Pain Medicine: A Review of New Technologies. Curr. Pain Headache Rep. 2022, 26, 605–616. [Google Scholar] [CrossRef]
- Stoumpos, A.I.; Kitsios, F.; Talias, M.A. Digital Transformation in Healthcare: Technology Acceptance and Its Applications. Int. J. Environ. Res. Public Health 2023, 20, 3407. [Google Scholar] [CrossRef]
- Shrivastava, M.; Ye, L. A Review on Autophagy in Orofacial Neuropathic Pain. Cells 2022, 11, 3842. [Google Scholar] [CrossRef] [PubMed]
- Bonomini, F.; Favero, G.; Castrezzati, S.; Borsani, E. Role of Neurotrophins in Orofacial Pain Modulation: A Review of the Latest Discoveries. Int. J. Mol. Sci. 2023, 24, 12438. [Google Scholar] [CrossRef] [PubMed]
- Ferrillo, M.; Giudice, A.; Marotta, N.; Fortunato, F.; Di Venere, D.; Ammendolia, A.; Fiore, P.; de Sire, A. Pain Management and Rehabilitation for Central Sensitization in Temporomandibular Disorders: A Comprehensive Review. Int. J. Mol. Sci. 2022, 23, 12164. [Google Scholar] [CrossRef]
- Hill, J.E.; Stephani, A.-M.; Sapple, P.; Clegg, A.J. The Effectiveness of Continuous Quality Improvement for Developing Professional Practice and Improving Health Care Outcomes: A Systematic Review. Implement. Sci. 2020, 15, 23. [Google Scholar] [CrossRef]
- Vahdat, S.; Hamzehgardeshi, L.; Hessam, S.; Hamzehgardeshi, Z. Patient Involvement in Health Care Decision Making: A Review. Iran. Red Crescent Med. J. 2014, 16, e12454. [Google Scholar] [CrossRef] [PubMed]
- Junaid, S.B.; Imam, A.A.; Balogun, A.O.; De Silva, L.C.; Surakat, Y.A.; Kumar, G.; Abdulkarim, M.; Shuaibu, A.N.; Garba, A.; Sahalu, Y.; et al. Recent Advancements in Emerging Technologies for Healthcare Management Systems: A Survey. Healthcare 2022, 10, 1940. [Google Scholar] [CrossRef]



| Part 1: Primary Headache | |
|---|---|
| 1. Migraine | |
| 2. Tension-type headache | |
| 3. Trigeminal autonomic cephalalgias | |
| 4. Other primary headache disorders | |
| PART 2: SECONDARY HEADACHE | |
| 5. Headache attributed to trauma or injury to the head and/or neck | |
| 6. Headache attributed to cranial or cervical vascular disorder | |
| 7. Headache attributed to non-vascular intracranial disorder | |
| 8. Headache attributed to a substance or its withdrawal | |
| 9. Headache attributed to infection | |
| 10. Headache attributed to homeostasis disorders | |
| 11. Headache or facial pain attributed to disorders of the skull, neck, eyes, ears, nose, paranasal sinuses, teeth, mouth, or other facial or cervical structures | |
| 12. Headache attributed to psychiatric disorder | |
| PART 3: CRANIAL NEUROPATHIES, AND OTHER FACIAL PAINS | |
| 13. Painful cranial neuropathies and other facial pains | |
| 14. Other headache disorders | |
| 13. Painful cranial neuropathies and other facial pains | |
| ICHD code | Types of Pain |
| 13.1 | Trigeminal neuralgia |
| 13.1.1 | Classical trigeminal neuralgia |
| 13.1.1.1 | Purely paroxysmal classical trigeminal neuralgia |
| 13.1.1.2 | Classical trigeminal neuralgia with concurrent persistent facial pain |
| 13.1.2 | Painful trigeminal neuropathy |
| 13.1.2.1 | Painful trigeminal neuropathy attributed to acute herpes zoster |
| 13.1.2.2 | Post-herpetic trigeminal neuropathy |
| 13.1.2.3 | Painful post-traumatic trigeminal neuropathy |
| 13.1.2.4 | Painful trigeminal neuropathy attributed to multiple sclerosis (MS) plaques |
| 13.1.2.5 | Painful trigeminal neuropathy attributed to space-occupying lesion |
| 13.1.2.6 | Painful trigeminal neuropathy attributed to other disorders |
| 13.11 | Burning mouth syndrome (BMS) |
| 13.12 | Persistent idiopathic facial pain (PIFP) |
| Types of Pain | ICD-11 Code |
|---|---|
| Primary chronic pain | MG 30.0 |
| Chronic cancer pain | MG 30.1 |
| Chronic post-surgical and post-traumatic pain | MG 30.2 |
| Chronic musculoskeletal pain | MG 30.3 |
| Secondary chronic visceral pain | MG 30.4 |
| Chronic neuropathic pain | MG 30.5 |
| Secondary chronic headache or orofacial pain | MG 30.6 |
| Other specified chronic neuropathic pain | MG 30.Y |
| Chronic neuropathic pain, unspecified | MG 30.Z |
| Types of OFP | ICOP 2020 | ICHD-3 v. Beta | IASP for ICD-11 |
|---|---|---|---|
| Trigeminal neuralgia | 4.1.1 | 13.1 | 8B82.0 |
| Purely paroxysmal classical trigeminal neuralgia | 4.1.1.1.1 | 13.1.1.1 | N.D |
| Classical trigeminal neuralgia with concomitant continuous pain | 4.1.1.1.2 | 13.1.1.2 | N.D |
| Trigeminal neuralgia attributed to multiple sclerosis | 4.1.1.2.1 | 13.1.2.4 | MG 30.50 |
| Trigeminal neuralgia attributed to space-occupying lesion | 4.1.1.2.2 | 13.1.2.5 | MG 30.50 |
| Trigeminal neuropathic pain attributed to herpes zoster | 4.1.2.1 | 13.1.2.1 | 1E91.4 |
| Post-herpetic trigeminal neuralgia | 4.1.2.2 | 13.1.2.2 | 1E91.5 |
| Post-traumatic trigeminal neuropathic pain | 4.1.2.3 | 13.1.2.3 | N.D |
| Trigeminal neuralgia attributed to another cause | 4.1.1.2.3 | 13.1.2.6 | 8B82.Z |
| Burning mouth syndrome | 6.1 | 13.11 | DA0F.0 |
| Persistent idiopathic facial pain | 6.2 | 13.12 | 8B82.1 |
| Persistent idiopathic dento-alveolar pain | 6.3 | N.D | N.D |
| Abbreviations | Questionnaires | |
|---|---|---|
| Pain | ||
| Pain drawing | / | Evaluate the extent of the pain |
| GCPS | Graded Chronic Pain Scale | Scale of pain intensity and disability |
| JFLS | Jaw Functional Limitation Scale | Scale of functional limitation (specific to TMD) |
| OBC | Oral Behaviors Checklist | Checklist of dysfunctional behaviors (specific to TMD) |
| Depression and anxiety | ||
| GAD7 | General Anxiety Disorders | Scale for the evaluation of generalized anxiety disorder |
| PHQ-9 | Patient Health Questionnaire-9 | Depression evaluation |
| PHQ-15 | Patient Health Questionnaire-15 | Scale for the evaluation of the severity of somatic symptoms |
| PCS | Pain Catastrophizing Scale | Scale for the evaluation of catastrophizing |
| Coping strategies | ||
| CSQ | Coping Strategies Questionnaires | Scale for the evaluation of coping strategies |
| TSK | Tampa Scale for Kinesiophobia | Scale of pain avoidance |
| Orofacial Pain | |
|---|---|
| 1. Orofacial pain attributed to disorders of the dento-alveolar and anatomically related structures | |
| 2. Myofascial orofacial pain | |
| 3. Temporomandibular joint (TMJ) pain | |
| 4. Orofacial pain attributed to lesion or disease of cranial nerves | |
| 5. Orofacial pains with presentations similar to primary headaches | |
| 6. Idiopathic orofacial pain | |
| ICOP Code | Types of Pain |
| 4.1 | Pain attributed to lesion or disease of the trigeminal nerve |
| 4.1.1 | Trigeminal neuralgia |
| 4.1.1.1 | Classical trigeminal neuralgia |
| 4.1.1.1.1 | Purely paroxysmal classical trigeminal neuralgia |
| 4.1.1.1.2 | Classical trigeminal neuralgia with concomitant continuous pain |
| 4.1.1.2 | Secondary trigeminal neuralgia |
| 4.1.1.2.1 | Trigeminal neuralgia attributed to multiple sclerosis |
| 4.1.1.2.2 | Trigeminal neuralgia attributed to space-occupying lesion |
| 4.1.1.2.3 | Trigeminal neuralgia attributed to another cause |
| 4.1.1.3 | Idiopathic trigeminal neuralgia |
| 4.1.1.3.1 | Idiopathic trigeminal neuralgia, purely paroxysmal |
| 4.1.1.3.2 | Idiopathic trigeminal neuralgia with concomitant continuous pain |
| 4.1.2 | Other trigeminal neuropathic pain |
| 4.1.2.1 | Trigeminal neuropathic pain attributed to herpes zoster |
| 4.1.2.2 | Post-herpetic trigeminal neuralgia |
| 4.1.2.3 | Post-traumatic trigeminal neuropathic pain |
| 4.1.2.3.1 | Probable post-traumatic trigeminal neuropathic pain |
| 4.1.2.4 | Trigeminal neuropathic pain attributed to another disorder |
| 4.1.2.4.1 | Probable trigeminal neuropathic pain attributed to another disorder |
| 4.1.2.5 | Idiopathic trigeminal neuropathic pain |
| ICOP Code | Types of Pain |
| 6.1 | Burning mouth syndrome (BMS) |
| 6.1.1 | Burning mouth syndrome without somatosensory alterations |
| 6.1.2 | Burning mouth syndrome with somatosensory alterations |
| 6.1.3 | Probable burning mouth syndrome |
| 6.2 | Persistent idiopathic facial pain (PIFP) |
| 6.2.1 | Persistent idiopathic facial pain without somatosensory alterations |
| 6.2.2 | Persistent idiopathic facial pain with somatosensory alterations |
| 6.2.3 | Probable persistent idiopathic facial pain |
| 6.3 | Persistent idiopathic dento-alveolar pain (PIDP) |
| 6.3.1 | Persistent idiopathic dento-alveolar pain without somatosensory alterations |
| 6.3.2 | Persistent idiopathic dento-alveolar pain with somatosensory alterations |
| 6.3.3 | Probable persistent idiopathic dento-alveolar pain |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Canfora, F.; Ottaviani, G.; Calabria, E.; Pecoraro, G.; Leuci, S.; Coppola, N.; Sansone, M.; Rupel, K.; Biasotto, M.; Di Lenarda, R.; et al. Advancements in Understanding and Classifying Chronic Orofacial Pain: Key Insights from Biopsychosocial Models and International Classifications (ICHD-3, ICD-11, ICOP). Biomedicines 2023, 11, 3266. https://doi.org/10.3390/biomedicines11123266
Canfora F, Ottaviani G, Calabria E, Pecoraro G, Leuci S, Coppola N, Sansone M, Rupel K, Biasotto M, Di Lenarda R, et al. Advancements in Understanding and Classifying Chronic Orofacial Pain: Key Insights from Biopsychosocial Models and International Classifications (ICHD-3, ICD-11, ICOP). Biomedicines. 2023; 11(12):3266. https://doi.org/10.3390/biomedicines11123266
Chicago/Turabian StyleCanfora, Federica, Giulia Ottaviani, Elena Calabria, Giuseppe Pecoraro, Stefania Leuci, Noemi Coppola, Mattia Sansone, Katia Rupel, Matteo Biasotto, Roberto Di Lenarda, and et al. 2023. "Advancements in Understanding and Classifying Chronic Orofacial Pain: Key Insights from Biopsychosocial Models and International Classifications (ICHD-3, ICD-11, ICOP)" Biomedicines 11, no. 12: 3266. https://doi.org/10.3390/biomedicines11123266
APA StyleCanfora, F., Ottaviani, G., Calabria, E., Pecoraro, G., Leuci, S., Coppola, N., Sansone, M., Rupel, K., Biasotto, M., Di Lenarda, R., Mignogna, M. D., & Adamo, D. (2023). Advancements in Understanding and Classifying Chronic Orofacial Pain: Key Insights from Biopsychosocial Models and International Classifications (ICHD-3, ICD-11, ICOP). Biomedicines, 11(12), 3266. https://doi.org/10.3390/biomedicines11123266