Diabetic Kidney Disease in Post-Transplant Diabetes Mellitus: Causes, Treatment and Outcomes
Abstract
:1. Introduction
2. Review Protocol
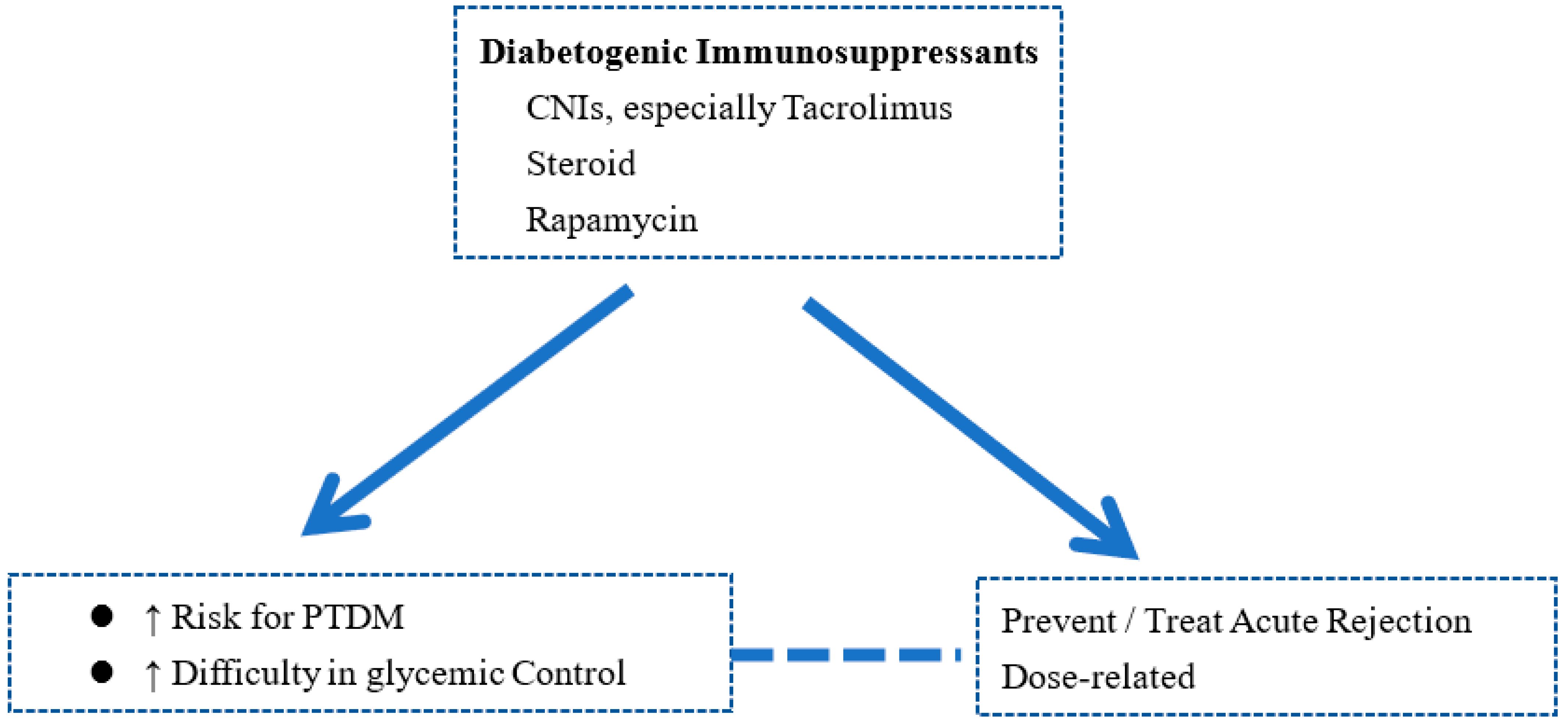
3. Risk Factors for PTDM
4. Pathophysiology of Diabetic Kidney Disease in PTDM
5. Diagnosis of DKD and PTDM
6. Prevention of PTDM
7. Management of DKD in Patients with PTDM
7.1. Lifestyle Modification
7.2. Medication Treatment
7.2.1. Insulin
7.2.2. Metformin
7.2.3. Dipeptidyl Peptidase 4 Inhibitors
7.2.4. Glucagon-like Peptide-1 Receptor Agonists
7.2.5. Sodium–Glucose Cotransporter 2 Inhibitors
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Carminatti, M.; Tedesco-Silva, H.; Silva Fernandes, N.M.; Sanders-Pinheiro, H. Chronic kidney disease progression in kidney transplant recipients: A focus on traditional risk factors. Nephrology 2019, 24, 141–147. [Google Scholar] [CrossRef] [PubMed]
- Au, E.; Wong, G.; Chapman, J.R. Cancer in kidney transplant recipients. Nat. Rev. Nephrol. 2018, 14, 508–520. [Google Scholar] [CrossRef]
- Lamb, K.E.; Lodhi, S.; Meier-Kriesche, H.U. Long-term renal allograft survival in the United States: A critical reappraisal. Am. J. Transpl. 2011, 11, 450–462. [Google Scholar] [CrossRef]
- Moroni, G.; Binda, V.; Quaglini, S.; Sacchi, L.; Raffiotta, F.; Cosa, F.; Montagnino, G.; Favi, E.; Messa, P.; Ponticelli, C. Causes of late transplant failure in cyclosporine-treated kidney allograft recipients. Clin. Exp. Nephrol. 2019, 23, 1076–1086. [Google Scholar] [CrossRef] [PubMed]
- Ponticelli, C.; Favi, E.; Ferraresso, M. New-Onset Diabetes after Kidney Transplantation. Medicina 2021, 57, 250. [Google Scholar] [CrossRef]
- Gomes, V.; Ferreira, F.; Guerra, J.; Bugalho, M.J. New-onset diabetes after kidney transplantation: Incidence and associated factors. World J. Diabetes 2018, 9, 132–137. [Google Scholar] [CrossRef]
- Sharif, A.; Hecking, M.; de Vries, A.P.; Porrini, E.; Hornum, M.; Rasoul-Rockenschaub, S.; Berlakovich, G.; Krebs, M.; Kautzky-Willer, A.; Schernthaner, G.; et al. Proceedings from an international consensus meeting on posttransplantation diabetes mellitus: Recommendations and future directions. Am. J. Transpl. 2014, 14, 1992–2000. [Google Scholar] [CrossRef] [PubMed]
- Kasiske, B.L.; Snyder, J.J.; Gilbertson, D.; Matas, A.J. Diabetes mellitus after kidney transplantation in the United States. Am. J. Transpl. 2003, 3, 178–185. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Ducloux, D.; Courivaud, C. Prevention of Post-Transplant Diabetes Mellitus: Towards a Personalized Approach. J. Pers. Med. 2022, 12, 116. [Google Scholar] [CrossRef]
- Kovesdy, C.P.; Furth, S.; Zoccali, C.; On behalf of the World Kidney Day Steering Committee. Obesity and kidney disease: Hidden consequences of the epidemic. J. Nephrol. 2017, 30, 1–10. [Google Scholar] [CrossRef]
- Wang, Y.; Chen, X.; Song, Y.; Caballero, B.; Cheskin, L.J. Association between obesity and kidney disease: A systematic review and meta-analysis. Kidney Int. 2008, 73, 19–33. [Google Scholar] [CrossRef]
- Martin-Moreno, P.L.; Shin, H.S.; Chandraker, A. Obesity and Post-Transplant Diabetes Mellitus in Kidney Transplantation. J. Clin. Med. 2021, 10, 2497. [Google Scholar] [CrossRef]
- Ahmed, B.; Sultana, R.; Greene, M.W. Adipose tissue and insulin resistance in obese. Biomed Pharm. 2021, 137, 111315. [Google Scholar] [CrossRef]
- Kuo, H.T.; Poommipanit, N.; Sampaio, M.; Reddy, P.; Cho, Y.W.; Bunnapradist, S. Risk factors for development of new-onset diabetes mellitus in pediatric renal transplant recipients: An analysis of the OPTN/UNOS database. Transplantation 2010, 89, 434–439. [Google Scholar] [CrossRef]
- Antonelli, A.; Ferrari, S.M.; Giuggioli, D.; Di Domenicantonio, A.; Ruffilli, I.; Corrado, A.; Fabiani, S.; Marchi, S.; Ferri, C.; Ferrannini, E.; et al. Hepatitis C virus infection and type 1 and type 2 diabetes mellitus. World J. Diabetes 2014, 5, 586–600. [Google Scholar] [CrossRef]
- Alzahrani, N. Hepatitis C virus, insulin resistance, and diabetes: A review. Microbiol. Immunol. 2022, 66, 453–459. [Google Scholar] [CrossRef]
- Ascione, A.; De Luca, M.; Tartaglione, M.T.; Lampasi, F.; Di Costanzo, G.G.; Lanza, A.G.; Picciotto, F.P.; Marino-Marsilia, G.; Fontanella, L.; Leandro, G. Peginterferon alfa-2a plus ribavirin is more effective than peginterferon alfa-2b plus ribavirin for treating chronic hepatitis C virus infection. Gastroenterology 2010, 138, 116–122. [Google Scholar] [CrossRef]
- Dai, C.Y.; Chuang, W.L.; Yu, M.L. EASL recommendations on treatment of hepatitis C: Final update of the series—Some issues. J. Hepatol. 2021, 74, 473–474. [Google Scholar] [CrossRef]
- Einollahi, B.; Motalebi, M.; Salesi, M.; Ebrahimi, M.; Taghipour, M. The impact of cytomegalovirus infection on new-onset diabetes mellitus after kidney transplantation: A review on current findings. J. Nephropathol. 2014, 3, 139–148. [Google Scholar] [CrossRef]
- Shivaswamy, V.; Boerner, B.; Larsen, J. Post-Transplant Diabetes Mellitus: Causes, Treatment, and Impact on Outcomes. Endocr. Rev. 2016, 37, 37–61. [Google Scholar] [CrossRef]
- Hellemans, R.; Abramowicz, D. Cytomegalovirus after kidney transplantation in 2020: Moving towards personalized prevention. Nephrol. Dial. Transpl. 2022, 37, 810–816. [Google Scholar] [CrossRef]
- van Raalte, D.H.; Nofrate, V.; Bunck, M.C.; van Iersel, T.; Elassaiss Schaap, J.; Nassander, U.K.; Heine, R.J.; Mari, A.; Dokter, W.H.; Diamant, M. Acute and 2-week exposure to prednisolone impair different aspects of beta-cell function in healthy men. Eur. J. Endocrinol. 2010, 162, 729–735. [Google Scholar] [CrossRef]
- Maes, B.D.; Kuypers, D.; Messiaen, T.; Evenepoel, P.; Mathieu, C.; Coosemans, W.; Pirenne, J.; Vanrenterghem, Y.F. Posttransplantation diabetes mellitus in FK-506-treated renal transplant recipients: Analysis of incidence and risk factors. Transplantation 2001, 72, 1655–1661. [Google Scholar] [CrossRef]
- Palepu, S.; Prasad, G.V. New-onset diabetes mellitus after kidney transplantation: Current status and future directions. World J. Diabetes 2015, 6, 445–455. [Google Scholar] [CrossRef]
- Johnston, O.; Rose, C.L.; Webster, A.C.; Gill, J.S. Sirolimus is associated with new-onset diabetes in kidney transplant recipients. J. Am. Soc. Nephrol. 2008, 19, 1411–1418. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.D.; Chang, J.Y.; Chung, B.H.; Kim, C.D.; Lee, S.H.; Kim, Y.H.; Yang, C.W. Effect of Everolimus with Low-Dose Tacrolimus on Development of New-Onset Diabetes After Transplantation and Allograft Function in Kidney Transplantation: A Multicenter, Open-Label, Randomized Trial. Ann. Transpl. 2021, 26, e927984. [Google Scholar] [CrossRef]
- Vincenti, F.; Friman, S.; Scheuermann, E.; Rostaing, L.; Jenssen, T.; Campistol, J.M.; Uchida, K.; Pescovitz, M.D.; Marchetti, P.; Tuncer, M.; et al. Results of an international, randomized trial comparing glucose metabolism disorders and outcome with cyclosporine versus tacrolimus. Am. J. Transpl. 2007, 7, 1506–1514. [Google Scholar] [CrossRef] [PubMed]
- Araki, M.; Flechner, S.M.; Ismail, H.R.; Flechner, L.M.; Zhou, L.; Derweesh, I.H.; Goldfarb, D.; Modlin, C.; Novick, A.C.; Faiman, C. Posttransplant diabetes mellitus in kidney transplant recipients receiving calcineurin or mTOR inhibitor drugs. Transplantation 2006, 81, 335–341. [Google Scholar] [CrossRef]
- Kotha, S.; Lawendy, B.; Asim, S.; Gomes, C.; Yu, J.; Orchanian-Cheff, A.; Tomlinson, G.; Bhat, M. Impact of immunosuppression on incidence of post-transplant diabetes mellitus in solid organ transplant recipients: Systematic review and meta-analysis. World J. Transpl. 2021, 11, 432–442. [Google Scholar] [CrossRef] [PubMed]
- Gheith, O.; Farouk, N.; Nampoory, N.; Halim, M.A.; Al-Otaibi, T. Diabetic kidney disease: World wide difference of prevalence and risk factors. J. Nephropharmacol. 2016, 5, 49–56. [Google Scholar] [CrossRef] [PubMed]
- Koye, D.N.; Magliano, D.J.; Nelson, R.G.; Pavkov, M.E. The Global Epidemiology of Diabetes and Kidney Disease. Adv. Chronic Kidney Dis. 2018, 25, 121–132. [Google Scholar] [CrossRef] [PubMed]
- Jamal Shahwan, M.; Hassan, N.A.G.; Shaheen, R.A. Assessment of kidney function and associated risk factors among type 2 diabetic patients. Diabetes Metab. Syndr. 2019, 13, 2661–2665. [Google Scholar] [CrossRef]
- Hu, X.; Liu, W.; Yan, Y.; Liu, H.; Huang, Q.; Xiao, Y.; Gong, Z.; Du, J. Vitamin D protects against diabetic nephropathy: Evidence-based effectiveness and mechanism. Eur. J. Pharm. 2019, 845, 91–98. [Google Scholar] [CrossRef]
- Plum, L.A.; Zella, J.B. Vitamin D compounds and diabetic nephropathy. Arch. Biochem. Biophys. 2012, 523, 87–94. [Google Scholar] [CrossRef] [PubMed]
- Said, S.M.; Nasr, S.H. Silent diabetic nephropathy. Kidney Int. 2016, 90, 24–26. [Google Scholar] [CrossRef]
- Drummond, K.N.; Kramer, M.S.; Suissa, S.; Levy-Marchal, C.; Dell’Aniello, S.; Sinaiko, A.; Mauer, M.; International Diabetic Nephropathy Study, G. Effects of duration and age at onset of type 1 diabetes on preclinical manifestations of nephropathy. Diabetes 2003, 52, 1818–1824. [Google Scholar] [CrossRef]
- Pourghasem, M.; Shafi, H.; Babazadeh, Z. Histological changes of kidney in diabetic nephropathy. Casp. J. Intern. Med. 2015, 6, 120–127. [Google Scholar]
- Caramori, M.L.; Kim, Y.; Huang, C.; Fish, A.J.; Rich, S.S.; Miller, M.E.; Russell, G.; Mauer, M. Cellular basis of diabetic nephropathy: 1. Study design and renal structural-functional relationships in patients with long-standing type 1 diabetes. Diabetes 2002, 51, 506–513. [Google Scholar] [CrossRef]
- Nosadini, R.; Velussi, M.; Brocco, E.; Bruseghin, M.; Abaterusso, C.; Saller, A.; Dalla Vestra, M.; Carraro, A.; Bortoloso, E.; Sambataro, M.; et al. Course of renal function in type 2 diabetic patients with abnormalities of albumin excretion rate. Diabetes 2000, 49, 476–484. [Google Scholar] [CrossRef]
- Tervaert, T.W.; Mooyaart, A.L.; Amann, K.; Cohen, A.H.; Cook, H.T.; Drachenberg, C.B.; Ferrario, F.; Fogo, A.B.; Haas, M.; de Heer, E.; et al. Pathologic classification of diabetic nephropathy. J. Am. Soc. Nephrol. 2010, 21, 556–563. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hong, D.; Zheng, T.; Jia-qing, S.; Jian, W.; Zhi-hong, L.; Lei-shi, L. Nodular glomerular lesion: A later stage of diabetic nephropathy? Diabetes Res. Clin. Pract. 2007, 78, 189–195. [Google Scholar] [CrossRef]
- Gilbert, R.E.; Cooper, M.E. The tubulointerstitium in progressive diabetic kidney disease: More than an aftermath of glomerular injury? Kidney Int. 1999, 56, 1627–1637. [Google Scholar] [CrossRef] [PubMed]
- Min, W.; Yamanaka, N. Three-dimensional analysis of increased vasculature around the glomerular vascular pole in diabetic nephropathy. Virchows Arch. A Pathol. Anat. Histopathol. 1993, 423, 201–207. [Google Scholar] [CrossRef] [PubMed]
- Valderhaug, T.G.; Hjelmesaeth, J.; Jenssen, T.; Roislien, J.; Leivestad, T.; Hartmann, A. Early posttransplantation hyperglycemia in kidney transplant recipients is associated with overall long-term graft losses. Transplantation 2012, 94, 714–720. [Google Scholar] [CrossRef] [PubMed]
- Matas, A.J.; Gillingham, K.J.; Humar, A.; Ibrahim, H.N.; Payne, W.D.; Gruessner, R.W.; Dunn, T.B.; Sutherland, D.E.; Najarian, J.S.; Kandaswamy, R. Posttransplant diabetes mellitus and acute rejection: Impact on kidney transplant outcome. Transplantation 2008, 85, 338–343. [Google Scholar] [CrossRef]
- Jenssen, T.; Hartmann, A. Post-transplant diabetes mellitus in patients with solid organ transplants. Nat. Rev. Endocrinol. 2019, 15, 172–188. [Google Scholar] [CrossRef]
- Eide, I.A.; Halden, T.A.; Hartmann, A.; Asberg, A.; Dahle, D.O.; Reisaeter, A.V.; Jenssen, T. Mortality risk in post-transplantation diabetes mellitus based on glucose and HbA1c diagnostic criteria. Transpl. Int. 2016, 29, 568–578. [Google Scholar] [CrossRef]
- Seoane-Pillado, M.T.; Pita-Fernandez, S.; Valdes-Canedo, F.; Seijo-Bestilleiro, R.; Pertega-Diaz, S.; Fernandez-Rivera, C.; Alonso-Hernandez, A.; Gonzalez-Martin, C.; Balboa-Barreiro, V. Incidence of cardiovascular events and associated risk factors in kidney transplant patients: A competing risks survival analysis. BMC Cardiovasc. Disord. 2017, 17, 72. [Google Scholar] [CrossRef]
- Jenssen, T.; Hartmann, A. Emerging treatments for post-transplantation diabetes mellitus. Nat. Rev. Nephrol. 2015, 11, 465–477. [Google Scholar] [CrossRef]
- Heldal, T.F.; Ueland, T.; Jenssen, T.; Hartmann, A.; Reisaeter, A.V.; Aukrust, P.; Michelsen, A.; Asberg, A. Inflammatory and related biomarkers are associated with post-transplant diabetes mellitus in kidney recipients: A retrospective study. Transpl. Int. 2018, 31, 510–519. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ekstrand, A.V.; Eriksson, J.G.; Gronhagen-Riska, C.; Ahonen, P.J.; Groop, L.C. Insulin resistance and insulin deficiency in the pathogenesis of posttransplantation diabetes in man. Transplantation 1992, 53, 563–569. [Google Scholar] [CrossRef] [PubMed]
- Jorgensen, M.B.; Hornum, M.; van Hall, G.; Bistrup, C.; Hansen, J.M.; Mathiesen, E.R.; Feldt-Rasmussen, B. The impact of kidney transplantation on insulin sensitivity. Transpl. Int. 2017, 30, 295–304. [Google Scholar] [CrossRef] [PubMed]
- Hecking, M.; Kainz, A.; Werzowa, J.; Haidinger, M.; Doller, D.; Tura, A.; Karaboyas, A.; Horl, W.H.; Wolzt, M.; Sharif, A.; et al. Glucose metabolism after renal transplantation. Diabetes Care 2013, 36, 2763–2771. [Google Scholar] [CrossRef]
- Halden, T.A.; Egeland, E.J.; Asberg, A.; Hartmann, A.; Midtvedt, K.; Khiabani, H.Z.; Holst, J.J.; Knop, F.K.; Hornum, M.; Feldt-Rasmussen, B.; et al. GLP-1 Restores Altered Insulin and Glucagon Secretion in Posttransplantation Diabetes. Diabetes Care 2016, 39, 617–624. [Google Scholar] [CrossRef]
- Davidson, J.; Wilkinson, A.; Dantal, J.; Dotta, F.; Haller, H.; Hernandez, D.; Kasiske, B.L.; Kiberd, B.; Krentz, A.; Legendre, C.; et al. New-onset diabetes after transplantation: 2003 International consensus guidelines. Proceedings of an international expert panel meeting. Barcelona, Spain, 19 February 2003. Transplantation 2003, 75 (Suppl. S10), SS3–SS24. [Google Scholar] [CrossRef]
- American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care 2011, 34 (Suppl. S1), S62–S69. [Google Scholar] [CrossRef]
- Hare, M.J.; Shaw, J.E.; Zimmet, P.Z. Current controversies in the use of haemoglobin A1c. J. Intern. Med. 2012, 271, 227–236. [Google Scholar] [CrossRef]
- Cosio, F.G.; Pesavento, T.E.; Osei, K.; Henry, M.L.; Ferguson, R.M. Post-transplant diabetes mellitus: Increasing incidence in renal allograft recipients transplanted in recent years. Kidney. Int. 2001, 59, 732–737. [Google Scholar] [CrossRef]
- Porrini, E.; Delgado, P.; Alvarez, A.; Cobo, M.; Perez, L.; Gonzalez-Posada, J.M.; Hortal, L.; Gallego, R.; Garcia, J.J.; Checa, M.; et al. The combined effect of pre-transplant triglyceride levels and the type of calcineurin inhibitor in predicting the risk of new onset diabetes after renal transplantation. Nephrol. Dial. Transpl. 2008, 23, 1436–1441. [Google Scholar] [CrossRef]
- Bergrem, H.A.; Valderhaug, T.G.; Hartmann, A.; Bergrem, H.; Hjelmesaeth, J.; Jenssen, T. Glucose tolerance before and after renal transplantation. Nephrol. Dial. Transpl. 2010, 25, 985–992. [Google Scholar] [CrossRef] [Green Version]
- Baid, S.; Cosimi, A.B.; Farrell, M.L.; Schoenfeld, D.A.; Feng, S.; Chung, R.T.; Tolkoff-Rubin, N.; Pascual, M. Posttransplant diabetes mellitus in liver transplant recipients: Risk factors, temporal relationship with hepatitis C virus allograft hepatitis, and impact on mortality. Transplantation 2001, 72, 1066–1072. [Google Scholar] [CrossRef]
- Chen, T.; Jia, H.; Li, J.; Chen, X.; Zhou, H.; Tian, H. New onset diabetes mellitus after liver transplantation and hepatitis C virus infection: Meta-analysis of clinical studies. Transpl. Int. 2009, 22, 408–415. [Google Scholar] [CrossRef]
- Hornum, M.; Lindahl, J.P.; von Zur-Muhlen, B.; Jenssen, T.; Feldt-Rasmussen, B. Diagnosis, management and treatment of glucometabolic disorders emerging after kidney transplantation: A position statement from the Nordic Transplantation Societies. Transpl. Int. 2013, 26, 1049–1060. [Google Scholar] [CrossRef]
- Jenssen, T.; Hartmann, A. Prevention and management of transplant-associated diabetes. Expert Opin. Pharm. 2011, 12, 2641–2655. [Google Scholar] [CrossRef]
- Markell, M. New-onset diabetes mellitus in transplant patients: Pathogenesis, complications, and management. Am. J. Kidney Dis. 2004, 43, 953–965. [Google Scholar] [CrossRef]
- Torres, A.; Hernandez, D.; Moreso, F.; Seron, D.; Burgos, M.D.; Pallardo, L.M.; Kanter, J.; Diaz Corte, C.; Rodriguez, M.; Diaz, J.M.; et al. Randomized Controlled Trial Assessing the Impact of Tacrolimus Versus Cyclosporine on the Incidence of Posttransplant Diabetes Mellitus. Kidney Int. Rep. 2018, 3, 1304–1315. [Google Scholar] [CrossRef]
- Grinyo, J.M.; Del Carmen Rial, M.; Alberu, J.; Steinberg, S.M.; Manfro, R.C.; Nainan, G.; Vincenti, F.; Jones-Burton, C.; Kamar, N. Safety and Efficacy Outcomes 3 Years After Switching to Belatacept From a Calcineurin Inhibitor in Kidney Transplant Recipients: Results From a Phase 2 Randomized Trial. Am. J. Kidney Dis. 2017, 69, 587–594. [Google Scholar] [CrossRef]
- de Graav, G.N.; van der Zwan, M.; Baan, C.C.; Janssen, J.; Hesselink, D.A. Improved Glucose Tolerance in a Kidney Transplant Recipient with Type 2 Diabetes Mellitus after Switching from Tacrolimus to Belatacept: A Case Report and Review of Potential Mechanisms. Transpl. Direct 2018, 4, e350. [Google Scholar] [CrossRef]
- Santos, A.H., Jr.; Chen, C.; Casey, M.J.; Womer, K.L.; Wen, X. New-onset diabetes after kidney transplantation: Can the risk be modified by choosing immunosuppression regimen based on pretransplant viral serology? Nephrol. Dial. Transpl. 2018, 33, 177–184. [Google Scholar] [CrossRef]
- Santoro, D.; Lucisano, S.; Gagliostro, G.; Alibrandi, A.; Benvenga, S.; Ientile, R.; Bellinghieri, G.; Buemi, M.; Caccamo, D. Vitamin D receptor polymorphism in chronic kidney disease patients with complicated cardiovascular disease. J. Ren. Nutr. 2015, 25, 187–193. [Google Scholar] [CrossRef]
- Gembillo, G.; Cernaro, V.; Salvo, A.; Siligato, R.; Laudani, A.; Buemi, M.; Santoro, D. Role of Vitamin D Status in Diabetic Patients with Renal Disease. Medicina 2019, 55, 273. [Google Scholar] [CrossRef]
- Aranow, C. Vitamin D and the immune system. J. Investig. Med. 2011, 59, 881–886. [Google Scholar] [CrossRef] [PubMed]
- Norman, P.E.; Powell, J.T. Vitamin D and cardiovascular disease. Circ. Res. 2014, 114, 379–393. [Google Scholar] [CrossRef] [PubMed]
- Ponticelli, C.; Sala, G. Vitamin D: A new player in kidney transplantation? Expert Rev. Clin. Immunol. 2014, 10, 1375–1383. [Google Scholar] [CrossRef] [PubMed]
- Messa, P.; Regalia, A.; Alfieri, C.M. Nutritional Vitamin D in Renal Transplant Patients: Speculations and Reality. Nutrients 2017, 9, 550. [Google Scholar] [CrossRef]
- Quach, K.; Abdelmasih, M.; Chen, P.X.; Li, Y.; Famure, O.; Nash, M.; Prasad, R.; Perkins, B.A.; Yip, P.M.; Kim, S.J. Vitamin D Levels and the Risk of Posttransplant Diabetes Mellitus After Kidney Transplantation. Prog. Transpl. 2021, 31, 133–141. [Google Scholar] [CrossRef]
- Dedinska, I.; Laca, L.; Miklusica, J.; Palkoci, B.; Skalova, P.; Kantarova, D.; Galajda, P.; Mokan, M. The role of proteinuria, paricalcitol and vitamin D in the development of post-transplant diabetes mellitus. Bratisl. Lek. Listy 2018, 119, 401–407. [Google Scholar] [CrossRef]
- Le Fur, A.; Fournier, M.C.; Gillaizeau, F.; Masson, D.; Giral, M.; Cariou, B.; Cantarovich, D.; Dantal, J. Vitamin D deficiency is an independent risk factor for PTDM after kidney transplantation. Transpl. Int. 2016, 29, 207–215. [Google Scholar] [CrossRef]
- Chakkera, H.A.; Pham, P.T.; Pomeroy, J.; Weil, E.J.; Knowler, W.C. Can New-Onset Diabetes After Kidney Transplant Be Prevented? Diabetes Care 2013, 36, 1406–1412. [Google Scholar] [CrossRef]
- Knowler, W.C.; Barrett-Connor, E.; Fowler, S.E.; Hamman, R.F.; Lachin, J.M.; Walker, E.A.; Nathan, D.M.; Diabetes Prevention Program Research, G. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N. Engl. J. Med. 2002, 346, 393–403. [Google Scholar] [CrossRef] [PubMed]
- Taheri, S.; Zaghloul, H.; Chagoury, O.; Elhadad, S.; Ahmed, S.H.; El Khatib, N.; Amona, R.A.; El Nahas, K.; Suleiman, N.; Alnaama, A.; et al. Effect of intensive lifestyle intervention on bodyweight and glycaemia in early type 2 diabetes (DIADEM-I): An open-label, parallel-group, randomised controlled trial. Lancet Diabetes Endocrinol. 2020, 8, 477–489. [Google Scholar] [CrossRef]
- Kuningas, K.; Driscoll, J.; Mair, R.; Smith, H.; Dutton, M.; Day, E.; Sharif, A.A. Comparing Glycaemic Benefits of Active Versus Passive Lifestyle Intervention in Kidney Allograft Recipients: A Randomized Controlled Trial. Transplantation 2020, 104, 1491–1499. [Google Scholar] [CrossRef] [PubMed]
- Byambasukh, O.; Oste, M.C.J.; Gomes-Neto, A.W.; van den Berg, E.; Navis, G.; Bakker, S.J.L.; Corpeleijn, E. Physical Activity and the Development of Post-Transplant Diabetes Mellitus, and Cardiovascular- and All-Cause Mortality in Renal Transplant Recipients. J. Clin. Med. 2020, 9, 415. [Google Scholar] [CrossRef]
- Gomes-Neto, A.W.; Oste, M.C.J.; Sotomayor, C.G.; Berg, E.V.D.; Geleijnse, J.M.; Gans, R.O.B.; Bakker, S.J.L.; Navis, G.J. Fruit and Vegetable Intake and Risk of Posttransplantation Diabetes in Renal Transplant Recipients. Diabetes Care 2019, 42, 1645–1652. [Google Scholar] [CrossRef] [PubMed]
- Oste, M.C.; Corpeleijn, E.; Navis, G.J.; Keyzer, C.A.; Soedamah-Muthu, S.S.; van den Berg, E.; Postmus, D.; de Borst, M.H.; Kromhout, D.; Bakker, S.J. Mediterranean style diet is associated with low risk of new-onset diabetes after renal transplantation. BMJ Open Diabetes Res. Care 2017, 5, e000283. [Google Scholar] [CrossRef]
- Chakkera, H.A.; Weil, E.J.; Castro, J.; Heilman, R.L.; Reddy, K.S.; Mazur, M.J.; Hamawi, K.; Mulligan, D.C.; Moss, A.A.; Mekeel, K.L.; et al. Hyperglycemia during the immediate period after kidney transplantation. Clin. J. Am. Soc. Nephrol. 2009, 4, 853–859. [Google Scholar] [CrossRef]
- Thomas, M.C.; Mathew, T.H.; Russ, G.R.; Rao, M.M.; Moran, J. Early peri-operative glycaemic control and allograft rejection in patients with diabetes mellitus: A pilot study. Transplantation 2001, 72, 1321–1324. [Google Scholar] [CrossRef]
- Hecking, M.; Haidinger, M.; Doller, D.; Werzowa, J.; Tura, A.; Zhang, J.; Tekoglu, H.; Pleiner, J.; Wrba, T.; Rasoul-Rockenschaub, S.; et al. Early basal insulin therapy decreases new-onset diabetes after renal transplantation. J. Am. Soc. Nephrol. 2012, 23, 739–749. [Google Scholar] [CrossRef]
- Schwaiger, E.; Krenn, S.; Kurnikowski, A.; Bergfeld, L.; Perez-Saez, M.J.; Frey, A.; Topitz, D.; Bergmann, M.; Hodlmoser, S.; Bachmann, F.; et al. Early Postoperative Basal Insulin Therapy versus Standard of Care for the Prevention of Diabetes Mellitus after Kidney Transplantation: A Multicenter Randomized Trial. J. Am. Soc. Nephrol. 2021, 32, 2083–2098. [Google Scholar] [CrossRef]
- Tahseen, A.C.; Mallik, R.; Javeria, P.; Mona, W.; Adnan, S. Association of British Clinical Diabetologists and Renal Association guidelines on the detection and management of diabetes post solid organ transplantation. Diabet Med. 2021, 38, e14523. Available online: https://www.diabetes.org.uk/resources-s3/public/2020-07/ABCD-RA%20PTDM%20v12.pdf (accessed on 3 October 2022).
- Stephen, J.; Anderson-Haag, T.L.; Gustafson, S.; Snyder, J.J.; Kasiske, B.L.; Israni, A.K. Metformin use in kidney transplant recipients in the United States: An observational study. Am. J. Nephrol. 2014, 40, 546–553. [Google Scholar] [CrossRef] [PubMed]
- Vest, L.S.; Koraishy, F.M.; Zhang, Z.; Lam, N.N.; Schnitzler, M.A.; Dharnidharka, V.R.; Axelrod, D.; Naik, A.S.; Alhamad, T.A.; Kasiske, B.L.; et al. Metformin use in the first year after kidney transplant, correlates, and associated outcomes in diabetic transplant recipients: A retrospective analysis of integrated registry and pharmacy claims data. Clin. Transpl. 2018, 32, e13302. [Google Scholar] [CrossRef] [PubMed]
- Alnasrallah, B.; Goh, T.L.; Chan, L.W.; Manley, P.; Pilmore, H. Transplantation and diabetes (Transdiab): A pilot randomised controlled trial of metformin in impaired glucose tolerance after kidney transplantation. BMC Nephrol. 2019, 20, 147. [Google Scholar] [CrossRef]
- Richter, B.; Bandeira-Echtler, E.; Bergerhoff, K.; Lerch, C.L. Dipeptidyl peptidase-4 (DPP-4) inhibitors for type 2 diabetes mellitus. Cochrane Database Syst. Rev. 2008, 2008, CD006739. [Google Scholar] [CrossRef] [PubMed]
- Vaghasiya, J.; Sheth, N.; Bhalodia, Y.; Manek, R. Sitagliptin protects renal ischemia reperfusion induced renal damage in diabetes. Regul. Pept. 2011, 166, 48–54. [Google Scholar] [CrossRef] [PubMed]
- Wajchenberg, B.L. Beta-cell failure in diabetes and preservation by clinical treatment. Endocr. Rev. 2007, 28, 187–218. [Google Scholar] [CrossRef]
- Shivaswamy, V.; Bennett, R.G.; Clure, C.C.; Ottemann, B.; Davis, J.S.; Larsen, J.L.; Hamel, F.G. Tacrolimus and sirolimus have distinct effects on insulin signaling in male and female rats. Transl. Res. 2014, 163, 221–231. [Google Scholar] [CrossRef]
- Strom Halden, T.A.; Asberg, A.; Vik, K.; Hartmann, A.; Jenssen, T. Short-term efficacy and safety of sitagliptin treatment in long-term stable renal recipients with new-onset diabetes after transplantation. Nephrol. Dial. Transpl. 2014, 29, 926–933. [Google Scholar] [CrossRef]
- Thiruvengadam, S.; Hutchison, B.; Lim, W.; Bennett, K.; Daniels, G.; Cusack, N.; Jacques, A.; Cawley, B.; Thiruvengadam, S.; Chakera, A. Intensive monitoring for post-transplant diabetes mellitus and treatment with dipeptidyl peptidase-4 inhibitor therapy. Diabetes Metab. Syndr. 2019, 13, 1857–1863. [Google Scholar] [CrossRef]
- Lane, J.T.; Odegaard, D.E.; Haire, C.E.; Collier, D.S.; Wrenshall, L.E.; Stevens, R.B. Sitagliptin therapy in kidney transplant recipients with new-onset diabetes after transplantation. Transplantation 2011, 92, e56–e57. [Google Scholar] [CrossRef]
- Boerner, B.P.; Miles, C.D.; Shivaswamy, V. Efficacy and safety of sitagliptin for the treatment of new-onset diabetes after renal transplantation. Int. J. Endocrinol. 2014, 2014, 617638. [Google Scholar] [CrossRef]
- Bae, J.; Lee, M.J.; Choe, E.Y.; Jung, C.H.; Wang, H.J.; Kim, M.S.; Kim, Y.S.; Park, J.Y.; Kang, E.S. Effects of Dipeptidyl Peptidase-4 Inhibitors on Hyperglycemia and Blood Cyclosporine Levels in Renal Transplant Patients with Diabetes: A Pilot Study. Endocrinol. Metab. 2016, 31, 161–167. [Google Scholar] [CrossRef] [PubMed]
- Anderson, S.; Cotiguala, L.; Tischer, S.; Park, J.M.; McMurry, K. Review of Newer Antidiabetic Agents for Diabetes Management in Kidney Transplant Recipients. Ann. Pharm. 2021, 55, 496–508. [Google Scholar] [CrossRef] [PubMed]
- Krishna, R.; Bergman, A.; Larson, P.; Cote, J.; Lasseter, K.; Dilzer, S.; Wang, A.; Zeng, W.; Chen, L.; Wagner, J.; et al. Effect of a single cyclosporine dose on the single-dose pharmacokinetics of sitagliptin (MK-0431), a dipeptidyl peptidase-4 inhibitor, in healthy male subjects. J. Clin. Pharm. 2007, 47, 165–174. [Google Scholar] [CrossRef]
- MacDonald, P.E.; El-Kholy, W.; Riedel, M.J.; Salapatek, A.M.; Light, P.E.; Wheeler, M.B. The multiple actions of GLP-1 on the process of glucose-stimulated insulin secretion. Diabetes 2002, 51 (Suppl. S3), S434–S442. [Google Scholar] [CrossRef]
- Garber, A.J. Long-acting glucagon-like peptide 1 receptor agonists: A review of their efficacy and tolerability. Diabetes Care 2011, 34 (Suppl. S2), S279–S284. [Google Scholar] [CrossRef]
- DeFronzo, R.A.; Ratner, R.E.; Han, J.; Kim, D.D.; Fineman, M.S.; Baron, A.D. Effects of exenatide (exendin-4) on glycemic control and weight over 30 weeks in metformin-treated patients with type 2 diabetes. Diabetes Care 2005, 28, 1092–1100. [Google Scholar] [CrossRef] [PubMed]
- Garber, A.; Henry, R.; Ratner, R.; Garcia-Hernandez, P.A.; Rodriguez-Pattzi, H.; Olvera-Alvarez, I.; Hale, P.M.; Zdravkovic, M.; Bode, B.; Group, L.-S. Liraglutide versus glimepiride monotherapy for type 2 diabetes (LEAD-3 Mono): A randomised, 52-week, phase III, double-blind, parallel-treatment trial. Lancet 2009, 373, 473–481. [Google Scholar] [CrossRef]
- Fruhbeck, G. Overview of adipose tissue and its role in obesity and metabolic disorders. Methods Mol. Biol. 2008, 456, 1–22. [Google Scholar] [CrossRef]
- Perna, S.; Mainardi, M.; Astrone, P.; Gozzer, C.; Biava, A.; Bacchio, R.; Spadaccini, D.; Solerte, S.B.; Rondanelli, M. 12-month effects of incretins versus SGLT2-Inhibitors on cognitive performance and metabolic profile. A randomized clinical trial in the elderly with Type-2 diabetes mellitus. Clin. Pharmacol. 2018, 10, 141–151. [Google Scholar] [CrossRef]
- Rondanelli, M.; Perna, S.; Astrone, P.; Grugnetti, A.; Solerte, S.B.; Guido, D. Twenty-four-week effects of liraglutide on body composition, adherence to appetite, and lipid profile in overweight and obese patients with type 2 diabetes mellitus. Patient Prefer Adherence 2016, 10, 407–413. [Google Scholar] [CrossRef] [Green Version]
- Ertuglu, L.A.; Porrini, E.; Hornum, M.; Demiray, A.; Afsar, B.; Ortiz, A.; Covic, A.; Rossing, P.; Kanbay, M. Glucagon-like peptide-1 receptor agonists and sodium-glucose cotransporter 2 inhibitors for diabetes after solid organ transplantation. Transpl. Int. 2021, 34, 1341–1359. [Google Scholar] [CrossRef]
- Singh, P.; Taufeeq, M.; Pesavento, T.E.; Washburn, K.; Walsh, D.; Meng, S. Comparison of the glucagon-like-peptide-1 receptor agonists dulaglutide and liraglutide for the management of diabetes in solid organ transplant: A retrospective study. Diabetes Obes. Metab. 2020, 22, 879–884. [Google Scholar] [CrossRef] [PubMed]
- Srinivas, N.; Sarnaik, M.K.; Modi, S.; Pisipati, Y.; Vaidya, S.; Syed Gaggatur, N.; Sange, A.H.; Sange, I. Sodium-Glucose Cotransporter 2 (SGLT-2) Inhibitors: Delving Into the Potential Benefits of Cardiorenal Protection Beyond the Treatment of Type-2 Diabetes Mellitus. Cureus 2021, 13, e16868. [Google Scholar] [CrossRef]
- Novikov, A.; Vallon, V. Sodium glucose cotransporter 2 inhibition in the diabetic kidney: An update. Curr. Opin. Nephrol. Hypertens. 2016, 25, 50–58. [Google Scholar] [CrossRef] [PubMed]
- Heerspink, H.J.L.; Kosiborod, M.; Inzucchi, S.E.; Cherney, D.Z.I. Renoprotective effects of sodium-glucose cotransporter-2 inhibitors. Kidney Int. 2018, 94, 26–39. [Google Scholar] [CrossRef]
- Zinman, B.; Wanner, C.; Lachin, J.M.; Fitchett, D.; Bluhmki, E.; Hantel, S.; Mattheus, M.; Devins, T.; Johansen, O.E.; Woerle, H.J.; et al. Empagliflozin, Cardiovascular Outcomes, and Mortality in Type 2 Diabetes. N. Engl. J. Med. 2015, 373, 2117–2128. [Google Scholar] [CrossRef]
- McGuire, D.K.; Shih, W.J.; Cosentino, F.; Charbonnel, B.; Cherney, D.Z.I.; Dagogo-Jack, S.; Pratley, R.; Greenberg, M.; Wang, S.; Huyck, S.; et al. Association of SGLT2 Inhibitors with Cardiovascular and Kidney Outcomes in Patients With Type 2 Diabetes: A Meta-analysis. JAMA Cardiol. 2021, 6, 148–158. [Google Scholar] [CrossRef] [PubMed]
- Hisadome, Y.; Mei, T.; Noguchi, H.; Ohkuma, T.; Sato, Y.; Kaku, K.; Okabe, Y.; Nakamura, M. Safety and Efficacy of Sodium-glucose Cotransporter 2 Inhibitors in Kidney Transplant Recipients With Pretransplant Type 2 Diabetes Mellitus: A Retrospective, Single-center, Inverse Probability of Treatment Weighting Analysis of 85 Transplant Patients. Transpl. Direct 2021, 7, e772. [Google Scholar] [CrossRef]
- Mahling, M.; Schork, A.; Nadalin, S.; Fritsche, A.; Heyne, N.; Guthoff, M. Sodium-Glucose Cotransporter 2 (SGLT2) Inhibition in Kidney Transplant Recipients with Diabetes Mellitus. Kidney Blood Press Res. 2019, 44, 984–992. [Google Scholar] [CrossRef] [PubMed]
- Chewcharat, A.; Prasitlumkum, N.; Thongprayoon, C.; Bathini, T.; Medaura, J.; Vallabhajosyula, S.; Cheungpasitporn, W. Efficacy and Safety of SGLT-2 Inhibitors for Treatment of Diabetes Mellitus among Kidney Transplant Patients: A Systematic Review and Meta-Analysis. Med. Sci. 2020, 8, 47. [Google Scholar] [CrossRef] [PubMed]
- Ujjawal, A.; Schreiber, B.; Verma, A. Sodium-glucose cotransporter-2 inhibitors (SGLT2i) in kidney transplant recipients: What is the evidence? Ther. Adv. Endocrinol. Metab. 2022, 13, 20420188221090001. [Google Scholar] [CrossRef] [PubMed]
| Modifiable | Strategy of PTDM Prevention | |
|---|---|---|
| Traditional risk factors for DM | ||
| Family history | No | |
| Old age | No | |
| Obesity | Yes | Body weight control |
| Black race | No | |
| Virus | ||
| Hepatitis C | Yes | DAA treatment before transplant |
| CMV | Yes | CMV prophylaxis |
| Transplant-associated factors | ||
| Retransplant | No | |
| High level of HLA mismatch | No | |
| Acute rejection | Yes |
|
| ||
| Immunosuppressive agent | Yes | |
| No induction | Induction in risky patient | |
| CNI, especially tacrolimus | CNI minimization/elimination | |
| Steroid | Steroid withdrawal | |
| mTORi? |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lim, L.-M.; Chang, J.-M.; Kuo, H.-T. Diabetic Kidney Disease in Post-Transplant Diabetes Mellitus: Causes, Treatment and Outcomes. Biomedicines 2023, 11, 470. https://doi.org/10.3390/biomedicines11020470
Lim L-M, Chang J-M, Kuo H-T. Diabetic Kidney Disease in Post-Transplant Diabetes Mellitus: Causes, Treatment and Outcomes. Biomedicines. 2023; 11(2):470. https://doi.org/10.3390/biomedicines11020470
Chicago/Turabian StyleLim, Lee-Moay, Jer-Ming Chang, and Hung-Tien Kuo. 2023. "Diabetic Kidney Disease in Post-Transplant Diabetes Mellitus: Causes, Treatment and Outcomes" Biomedicines 11, no. 2: 470. https://doi.org/10.3390/biomedicines11020470
APA StyleLim, L. -M., Chang, J. -M., & Kuo, H. -T. (2023). Diabetic Kidney Disease in Post-Transplant Diabetes Mellitus: Causes, Treatment and Outcomes. Biomedicines, 11(2), 470. https://doi.org/10.3390/biomedicines11020470







