Blood-Derived Exosomal hTERT mRNA in Patients with Lung Cancer: Characterization and Correlation with Response to Therapy
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients’ Characteristics
2.2. Study Population and Procedures
2.3. Exosomes’ Purification
2.4. RNA Purification
2.5. cDNA Formation
2.6. hTERT Expression by Real-Time PCR
- hTERT: Forward, 5′-GTACTTTGTCAAGGTGGATGTGA-3′
- Reverse, 5′-GCTGGAGGTCTGTCAAGGTAGAG-3′.
- HPRT-1: Forward, 5′-TCAGGCAGTATAATCCAAAGATGGT-3′
- Reverse, 5′-CTTCGTGGGGTCCTTTTCAC-3′.
2.7. Statistical Analysis
3. Results
3.1. Patients
3.2. The Iolation of Exosomes
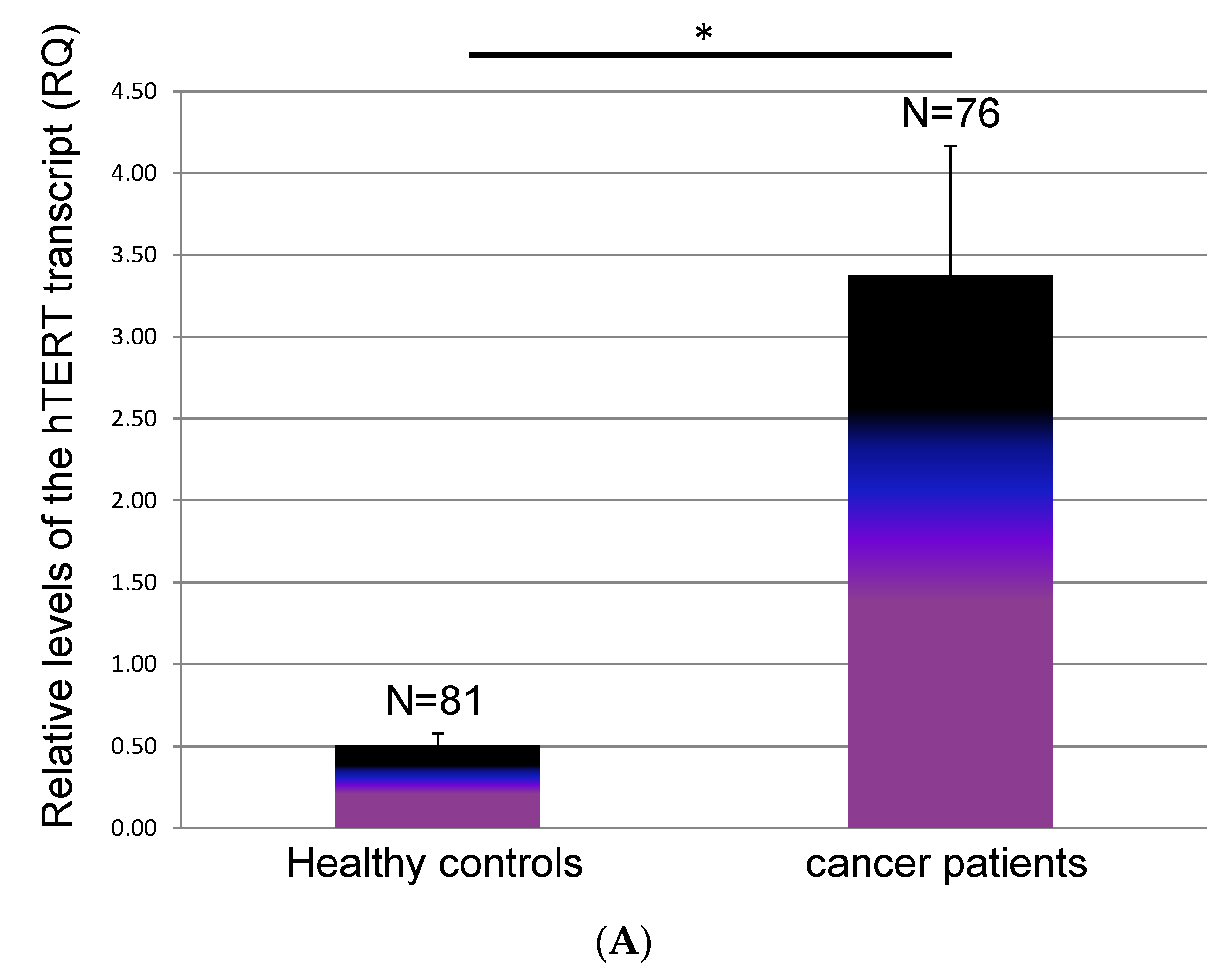
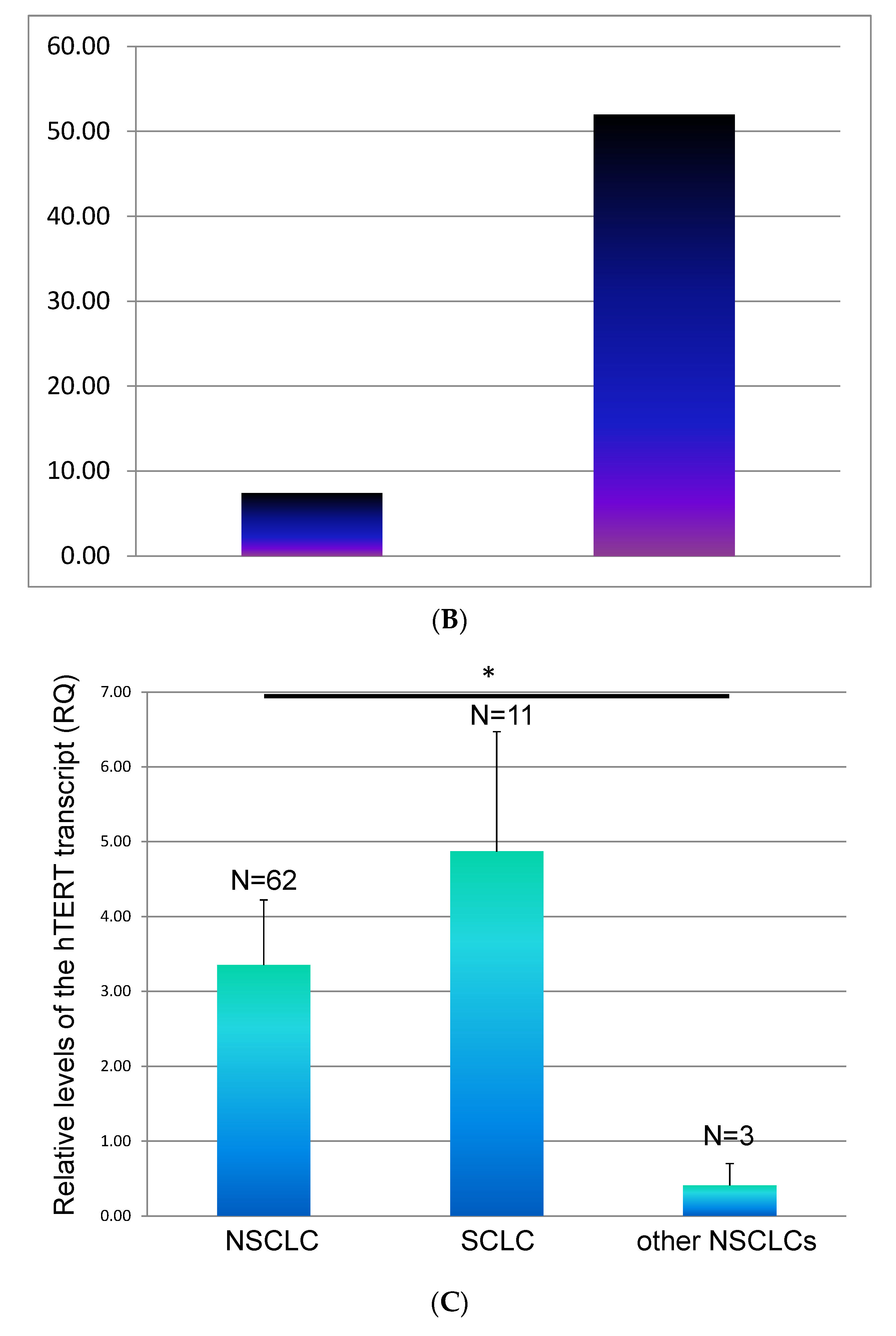
3.3. The Dynamics of hTERT at Time of Evaluation Regarding the Status of Metastasis
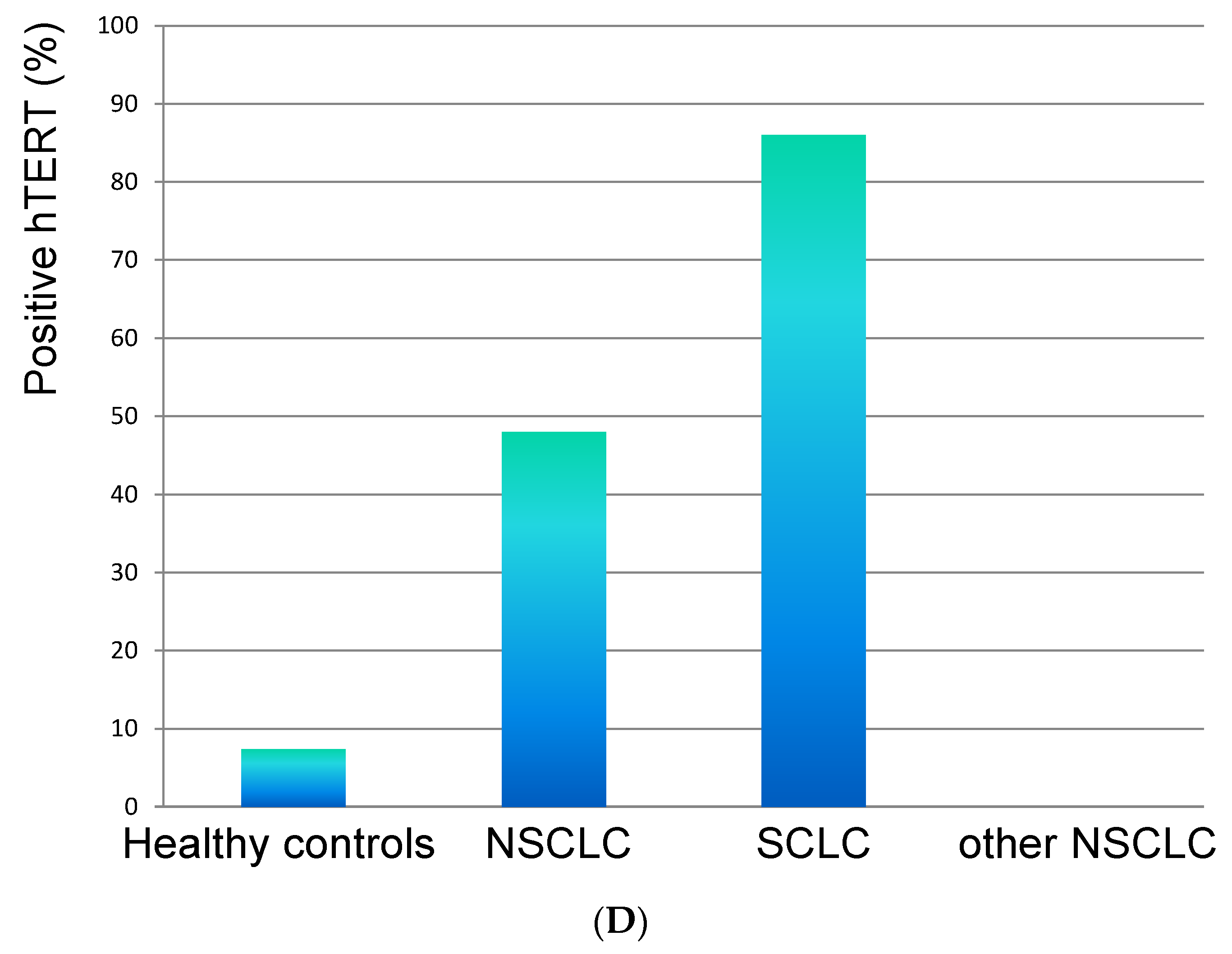
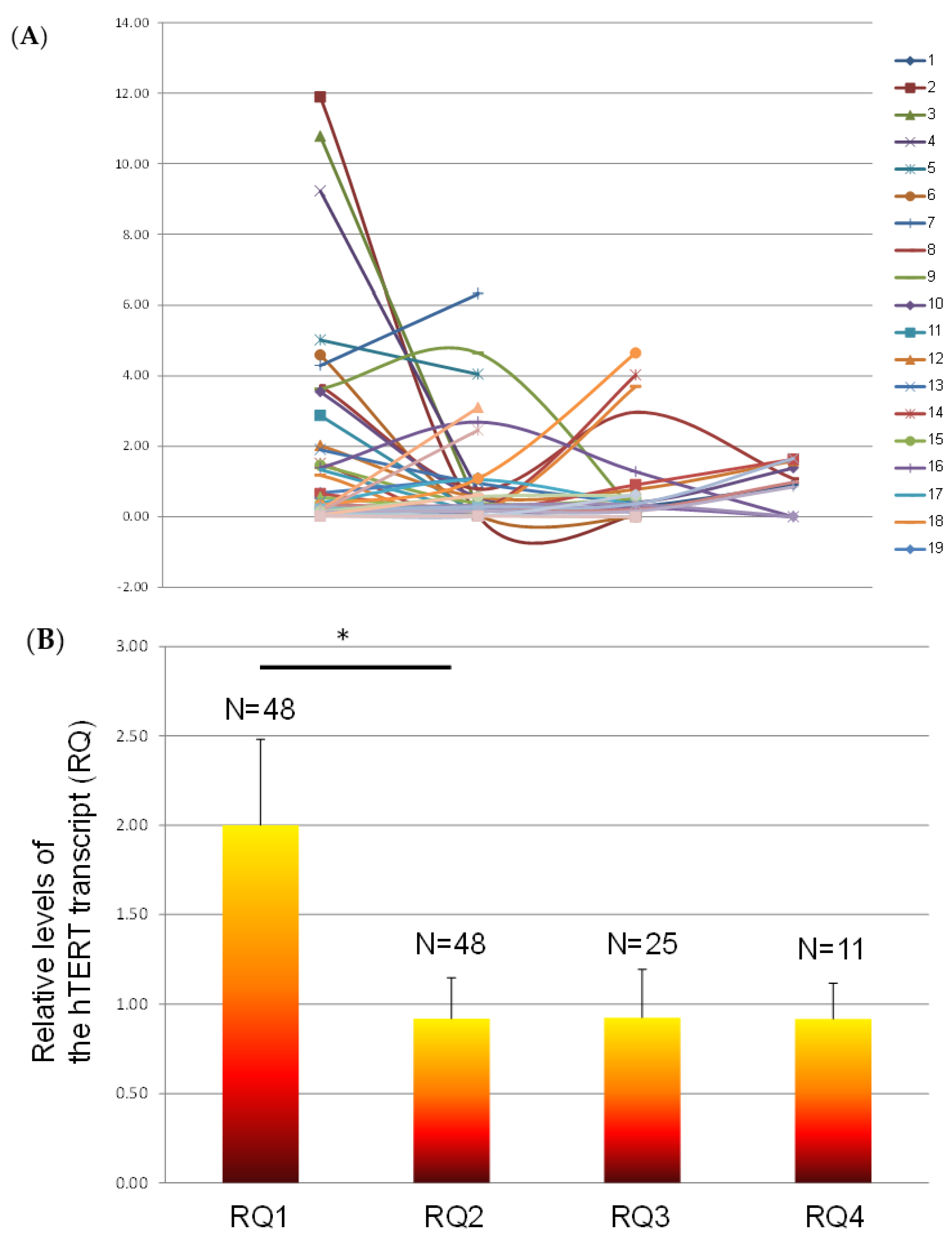
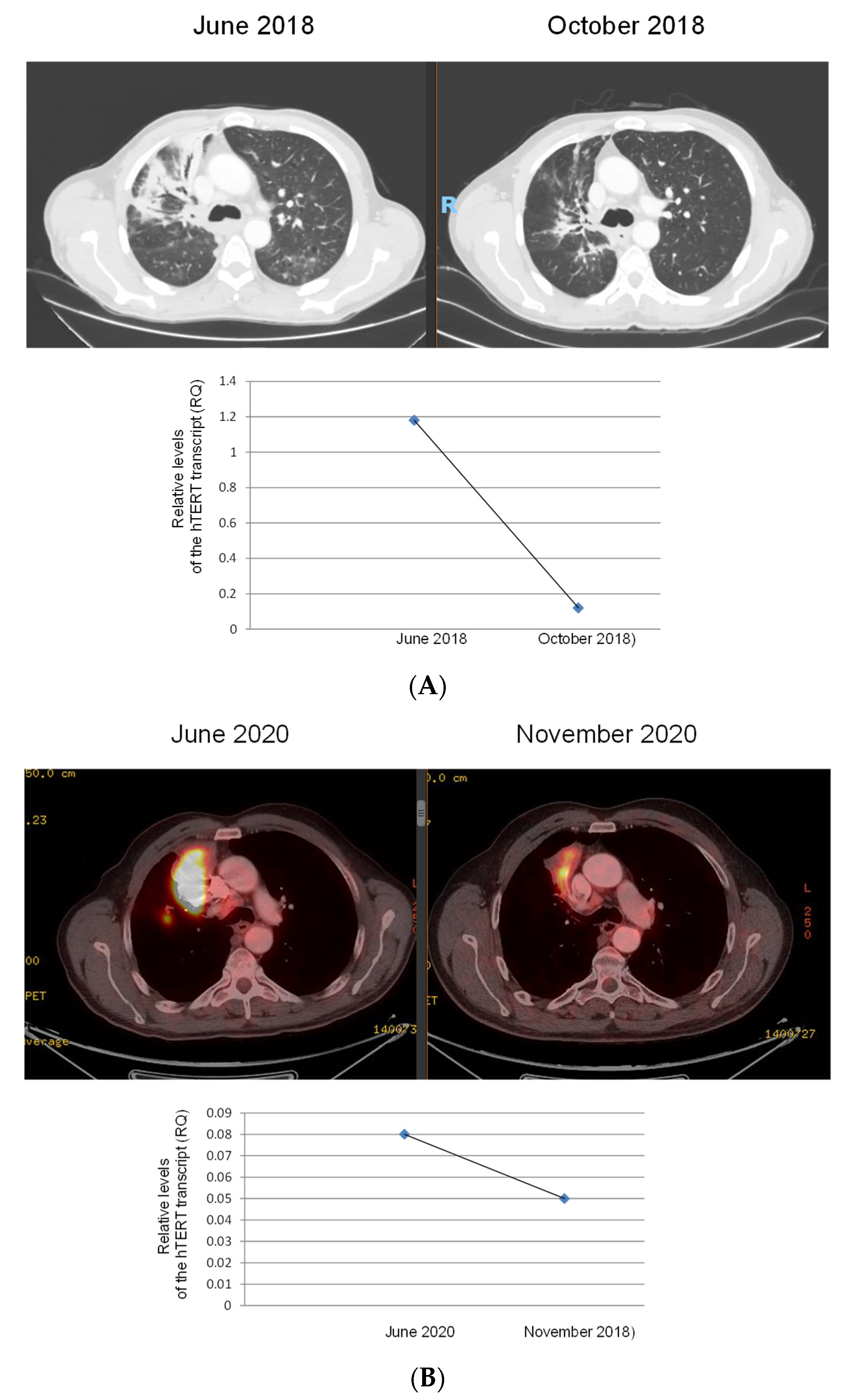
3.4. The Levels of Exosomal hTERT Transcript throughout Follow-Up of the Disease
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization International Agency for Research on Cancer. Globocan 2020: Lung Cancer. International Agency for Research on Cancer. Available online: http://gco.iarc.fr/today/data/factsheets/cancers/15-Lung-fact-sheet.pdf (accessed on 2 March 2021).
- Choi, S.H.; Yoo, S.S.; Lee, S.Y.; Park, J.Y. Anti-angiogenesis revisited: Reshaping the treatment landscape of advanced non-small cell lung cancer. Arch. Pharmacal Res. 2022, 45, 263–279. [Google Scholar] [CrossRef] [PubMed]
- The Cancer Atlas. Lung Cancer Remains the Most Commonly Diagnosed Cancer and the Leading Cause of Cancer Death Worldwide because of Inadequate Tobacco Control Policies. Available online: https://canceratlas.cancer.org/the-burden/lung-cancer/ (accessed on 1 April 2023).
- NCCN Guidelines. Treatment by Cancer Type. Available online: https://www.nccn.org/guidelines/category_1 (accessed on 1 April 2023).
- Lu, T.; Yang, X.; Huang, Y.; Zhao, M.; Li, M.; Ma, K.; Yin, J.; Zhan, C.; Wang, Q. Trends in the incidence, treatment, and survival of patients with lung cancer in the last four decades. Cancer Manag. Res. 2019, 11, 943–953. [Google Scholar] [CrossRef] [PubMed]
- Jonas, D.E.; Reuland, D.S.; Reddy, S.M.; Nagle, M.; Clark, S.D.; Weber, R.P.; Enyioha, C.; Malo, T.L.; Brenner, A.T.; Armstrong, C.; et al. Screening for Lung Cancer with Low-Dose Computed Tomography. JAMA 2021, 325, 971–987. [Google Scholar] [CrossRef] [PubMed]
- Cainap, C.; Pop, L.A.; Balacescu, O.; Cainap, S.S. Early diagnosis and screening in lung cancer. Am. J. Cancer Res. 2020, 10, 1993–2009. [Google Scholar] [PubMed]
- Wadowska, K.; Bil-Lula, I.; Trembecki, Ł.; Śliwińska-Mossoń, M. Genetic Markers in Lung Cancer Diagnosis: A Review. Int. J. Mol. Sci. 2020, 21, 4569. [Google Scholar] [CrossRef] [PubMed]
- El-Zein, R.A.; Abdel-Rahman, S.; Santee, K.J.; Yu, R.; Shete, S. Identification of Small and Non-Small Cell Lung Cancer Markers in Peripheral Blood Using Cytokinesis-Blocked Micronucleus and Spectral Karyotyping Assays. Cytogenet. Genome Res. 2017, 152, 122–131. [Google Scholar] [CrossRef]
- Van Mastrigt, E.; De Jongste, J.C.; Pijnenburg, M.W. The analysis of volatile organic compounds in exhaled breath and biomarkers in exhaled breath condensate in children—Clinical tools or scientific toys? Clin. Exp. Allergy 2015, 45, 1170–1188. [Google Scholar] [CrossRef]
- Aksenova, A.Y.; Mirkin, S.M. At the Beginning of the End and in the Middle of the Beginning: Structure and Maintenance of Telomeric DNA Repeats and Interstitial Telomeric Sequences. Genes 2019, 10, 118. [Google Scholar] [CrossRef]
- Chan, S.R.W.L.; Blackburn, E.H. Telomeres and telomerase. Philos. Trans. R. Soc. B Biol. Sci. 2004, 359, 109–122. [Google Scholar] [CrossRef]
- Phatak, P.; Burger, A.M. Telomerase and its potential for therapeutic intervention. Br. J. Pharmacol. 2007, 152, 1003–1011. [Google Scholar] [CrossRef]
- Low, K.C.; Tergaonkar, V. Telomerase: Central regulator of all of the hallmarks of cancer. Trends Biochem. Sci. 2013, 38, 426–434. [Google Scholar] [CrossRef]
- Lantuejoul, S.; Salon, C.; Soria, J.-C.; Brambilla, E. Telomerase expression in lung preneoplasia and neoplasia. Int. J. Cancer 2007, 120, 1835–1841. [Google Scholar] [CrossRef] [PubMed]
- Kawai, T.; Hiroi, S.; Nakanishi, K.; Meeker, A.K. Telomere length and telomerase expression in atypical adenomatous hyperplasia and small bronchioloalveolar carcinoma of the lung. Am. J. Clin. Pathol. 2007, 127, 254–262. [Google Scholar] [CrossRef] [PubMed]
- Mavrogiannou, E.; Strati, A.; Stathopoulou, A.; Tsaroucha, E.G.; Kaklamanis, L.; Lianidou, E.S. Real-Time RT-PCR Quantification of Human Telomerase Reverse Transcriptase Splice Variants in Tumor Cell Lines and Non–Small Cell Lung Cancer. Clin. Chem. 2007, 53, 53–61. [Google Scholar] [CrossRef]
- Kumaki, F.; Kawai, T.; Hiroi, S.; Shinomiya, N.; Ozeki, Y.; Ferrans, V.J.; Torikata, C. Telomerase activity and expression of human telomerase RNA component and human telomerase reverse transcriptase in lung carcinomas. Hum. Pathol. 2001, 32, 188–195. [Google Scholar] [CrossRef]
- Frías, C.; García-Aranda, C.; De Juan, C.; Morán, A.; Ortega, P.; Gómez, A.; Hernando, F.; López-Asenjo, J.-A.; Torres, A.-J.; Benito, M.; et al. Telomere shortening is associated with poor prognosis and telomerase activity correlates with DNA repair impairment in non-small cell lung cancer. Lung Cancer 2008, 60, 416–425. [Google Scholar] [CrossRef]
- Fan, Y.-B.; Ye, L.; Wang, T.-Y.; Wu, G.-P. Correlation between morphology and human telomerase gene amplification in bronchial brushing cells for the diagnosis of lung cancer. Diagn. Cytopathol. 2009, 38, 402–406. [Google Scholar] [CrossRef]
- Hashim, M.; Sayed, M.; Samy, N.; Elshazly, S. Prognostic significance of telomerase activity and some tumor markers in non-small cell lung cancer. Med. Oncol. 2010, 28, 322–330. [Google Scholar] [CrossRef] [PubMed]
- Targowski, T.; Jahnz-Różyk, K.; Owczarek, W.; Raczka, A.; Janda, P.; Szkoda, T.; Płusa, T. Telomerase activity and serum levels of p53 protein as prognostic factors of survival in patients with advanced non-small cell lung cancer. Respir. Med. 2010, 104, 1356–1361. [Google Scholar] [CrossRef]
- Wang, L.; Wang, L.E.; Mao, L.; Spitz, M.R.; Wei, Q. A functional variant of tandem repeats in human telomerase gene was associated with survival of patients with early stages of non-small cell lung cancer. Clin. Cancer Res. 2010, 16, 3779–3785. [Google Scholar] [CrossRef]
- Catarino, R.; Araújo, A.; Coelho, A.; Gomes, M.; Nogueira, A.; Lopes, C.; Medeiros, R.M. Prognostic Significance of Telomerase Polymorphism in Non–Small Cell Lung Cancer. Clin. Cancer Res. 2010, 16, 3706–3712. [Google Scholar] [CrossRef] [PubMed]
- Aras, G.; Kanmaz, D.; Ürer, N.; Purisa, S.; Kadakal, F.; Yentürk, E.; Tuncay, E. Immunohistochemical expression of telomerase in patients with non-small cell lung cancer: Prediction of metastasis and prognostic significance. Anticancer Res. 2013, 33, 2643–2650. [Google Scholar] [PubMed]
- Yuan, P.; Huang, S.; Bao, F.C.; Cao, J.L.; Sheng, H.X.; Shi, L.; Lv, W.; Hu, J. Discriminating association of a common telomerase reverse transcriptase promoter polymorphism with telomere parameters in non-small cell lung cancer with or without epidermal growth factor receptor mutation. Eur. J. Cancer 2019, 120, 10–19. [Google Scholar] [CrossRef] [PubMed]
- Xing, Y.-L.; Liu, F.; Li, J.-F.; Lin, J.-C.; Zhu, G.-D.; Li, M.; Zhang, C.-R.; Niu, Y.-Y. Case-Control Study on Impact of the Telomerase Reverse Transcriptase Gene Polymorphism and Additional Single Nucleotide Polymorphism (SNP)- SNP Interaction on Non-Small Cell Lung Cancers Risk in Chinese Han Population. J. Clin. Lab. Anal. 2016, 30, 1071–1077. [Google Scholar] [CrossRef] [PubMed]
- Fernández-Marcelo, T.; Gómez, A.; Pascua, I.; de Juan, C.; Head, J.; Hernando, F.; Jarabo, J.R.; Calatayud, J.; Torres-García, A.J.; Iniesta, P. Telomere length and telomerase activity in non-small cell lung cancer prognosis: Clinical usefulness of a specific telomere status. J. Exp. Clin. Cancer Res. 2015, 34, 78. [Google Scholar] [CrossRef]
- Flacco, A.; Ludovini, V.; Bianconi, F.; Ragusa, M.; Bellezza, G.; Tofanetti, F.R.; Pistola, L.; Siggillino, A.; Vannucci, J.; Cagini, L.; et al. MYC and Human Telomerase Gene (TERC) Copy Number Gain in Early-stage Non–small Cell Lung Cancer. Am. J. Clin. Oncol. 2015, 38, 152–158. [Google Scholar] [CrossRef]
- Wu, H.; Qiao, N.; Wang, Y.; Jiang, M.; Wang, S.; Wang, C.; Hu, L. Association between the telomerase reverse transcriptase (TERT) rs2736098 polymorphism and cancer risk: Evidence from a case-control study of non-small-cell lung cancer and a meta-analysis. PLoS ONE 2013, 8, e76372. [Google Scholar] [CrossRef]
- Antoniou, K.M.; Samara, K.D.; Lasithiotaki, I.; Margaritopoulos, G.A.; Soufla, G.; Lambiri, I.; Giannarakis, I.; Drositis, I.; Spandidos, D.A.; Siafakas, N.M. Differential telomerase expression in idiopathic pulmonary fibrosis and non-small cell lung cancer. Oncol. Rep. 2013, 30, 2617–2624. [Google Scholar] [CrossRef]
- Beisner, J.; Dong, M.; Taetz, S.; Piotrowska, K.; Kleideiter, E.; Friedel, G.; Schaefer, U.; Lehr, C.M.; Klotz, U.; Mürdter TEBeisner, J.; et al. Efficient telomerase inhibition in human non-small cell lung cancer cells by liposomal delivery of, 2′-O-methyl-RNA. J Pharm. Sci. 2009, 98, 1765–1774. [Google Scholar] [CrossRef]
- Liu, D.; Kojima, T.; Ouchi, M.; Kuroda, S.; Watanabe, Y.; Hashimoto, Y.; Onimatsu, H.; Urata, Y.; Fujiwara, T. Preclinical evaluation of synergistic effect of telomerase-specific oncolytic virotherapy and gemcitabine for human lung cancer. Mol. Cancer Ther. 2009, 8, 980–987. [Google Scholar] [CrossRef]
- Park, S.E.; Yoo, H.S.; Jin, C.-Y.; Hong, S.H.; Lee, Y.-W.; Kim, B.W.; Lee, S.H.; Kim, W.-J.; Cho, C.K.; Choi, Y.H. Induction of apoptosis and inhibition of telomerase activity in human lung carcinoma cells by the water extract of Cordyceps militaris. Food Chem. Toxicol. 2009, 47, 1667–1675. [Google Scholar] [CrossRef] [PubMed]
- Beisner, J.; Dong, M.; Taetz, S.; Nafee, N.; Griese, E.U.; Schaefer, U.; Lehr, C.M.; Klotz, U.; Mürdter, T.E. Nanoparticle mediated delivery of 2’-O-methyl-RNA leads to efficient telomerase inhibition and telomere shortening in human lung cancer cells. Lung Cancer 2010, 68, 346–354. [Google Scholar] [CrossRef] [PubMed]
- Wei, C.-W.; Lin, C.-C.; Yu, Y.-L.; Lin, P.-C.; Wu, M.-T.; Chen, C.-J.; Chang, W.; Lin, S.-Z.; Chen, Y.-L.S.; Harn, H.-J. n-Butylidenephthalide induced apoptosis in the A549 human lung adenocarcinoma cell line by coupled down-regulation of AP-2α and telomerase activity. Acta Pharmacol. Sin. 2009, 30, 1297–1306. [Google Scholar] [CrossRef]
- Zhang, J.F.; Wei, F.; Wang, H.P.; Li, H.M.; Qiu, W.; Ren, P.K.; Chen, X.F.; Huang, Q. Potent anti-tumor activity of telomerase-dependent and HSV-TK armed oncolytic adenovirus for non-small cell lung cancer in vitro and in vivo. J. Exp. Clin. Cancer Res. 2010, 29, 52. [Google Scholar] [CrossRef]
- Rao, Y.K.; Kao, T.-Y.; Wu, M.-F.; Ko, J.-L.; Tzeng, Y.-M. Identification of small molecule inhibitors of telomerase activity through transcriptional regulation of hTERT and calcium induction pathway in human lung adenocarcinoma A549 cells. Bioorganic Med. Chem. 2010, 18, 6987–6994. [Google Scholar] [CrossRef] [PubMed]
- Tuntiwechapikul, W.; Taka, T.; Songsomboon, C.; Kaewtunjai, N.; Imsumran, A.; Makonkawkeyoon, L.; Pompimon, W.; Lee, T.R.; Yaswen, P.; MacKenzie, K.L.; et al. Ginger Extract Inhibits Human Telomerase Reverse Transcriptase and c-Myc Expression in A549 Lung Cancer Cells. J. Med. Food 2010, 13, 1347–1354. [Google Scholar] [CrossRef]
- Dong, M.; Philippi, C.; Loretz, B.; Nafee, N.; Schaefer, U.F.; Friedel, G.; Ammon-Treiber, S.; Griese, E.U.; Lehr, C.M.; Klotz, U.; et al. Tissue slice model of human lung cancer to investigate telomerase inhibition by nanoparticle delivery of antisense 2′-O-methyl-RNA. Int. J. Pharm. 2011, 419, 33–42. [Google Scholar] [CrossRef]
- Serrano, D.; Bleau, A.-M.; Fernandez-Garcia, I.; Fernandez-Marcelo, T.; Iniesta, P.; Ortiz-De-Solorzano, C.; Calvo, A. Inhibition of telomerase activity preferentially targets aldehyde dehydrogenase-positive cancer stem-like cells in lung cancer. Mol. Cancer 2011, 10, 96. [Google Scholar] [CrossRef]
- Nafee, N.; Schneider, M.; Friebel, K.; Dong, M.; Schaefer, U.F.; Mürdter, T.E.; Lehr CMNafee, N. Treatment of lung cancer via telomerase inhibition: Self-assembled nanoplexes versus polymeric nanoparticles as vectors for 2′-O-methyl-RNA. Eur. J. Pharm. Biopharm. 2012, 80, 478–489. [Google Scholar] [CrossRef]
- Zhang, P.; Tan, J.; Yang, D.-B.; Luo, Z.-C.; Luo, S.; Chen, P.; Sun, P.; Zhou, Y.; Chen, X.-C.; Wei, Y.-Q.; et al. Gene therapy using the human telomerase catalytic subunit gene promoter enables targeting of the therapeutic effects of vesicular stomatitis virus matrix protein against human lung adenocarcinoma. Exp. Ther. Med. 2012, 4, 859–864. [Google Scholar] [CrossRef]
- Chiappori, A.A.; Kolevska, T.; Spigel, D.R.; Hager, S.; Rarick, M.; Gadgeel, S.; Blais, N.; Von Pawel, J.; Hart, L.; Reck, M.; et al. A randomized phase II study of the telomerase inhibitor imetelstat as maintenance therapy for advanced non-small-cell lung cancer. Ann. Oncol. 2015, 26, 354–362. [Google Scholar] [CrossRef] [PubMed]
- Chen, T.W.; Tsai, K.D.; Yang, S.M.; Wong, H.Y.; Liu, Y.H.; Cherng, J.; Chou, K.S.; Wang, Y.T.; Cuizon, J.; Cherng, J.M. Discovery of a Novel Anti-Cancer Agent Targeting Both Topoisomerase I & II as Well as Telomerase Activities in Human Lung Adenocarcinoma A549 Cells In Vitro and In Vivo: Cinnamomum verum Component Cuminaldehyde. Curr. Cancer Drug Targets 2016, 16, 796–806. [Google Scholar] [PubMed]
- Frink, R.E.; Peyton, M.; Schiller, J.H.; Gazdar, A.F.; Shay, J.W.; Minna, J.D. Telomerase inhibitor imetelstat has preclinical activity across the spectrum of non-small cell lung cancer oncogenotypes in a telomere length dependent manner. Oncotarget 2016, 7, 31639–31651. [Google Scholar] [CrossRef]
- Hu, W.; Jia, Y.; Xiao, X.; Lv, K.; Chen, Y.; Wang, L.; Luo, X.; Liu, T.; Li, W.; Li, Y.; et al. KLF4 downregulates hTERT expression and telomerase activity to inhibit lung carcinoma growth. Oncotarget 2016, 7, 52870–52887. [Google Scholar] [CrossRef] [PubMed]
- Ding, X.; Cheng, J.; Pang, Q.; Wei, X.; Zhang, X.; Wang, P.; Yuan, Z.; Qian, D. BIBR1532, a Selective Telomerase Inhibitor, Enhances Radiosensitivity of Non-Small Cell Lung Cancer Through Increasing Telomere Dysfunction and ATM/CHK1 Inhibition. Int. J. Radiat. Oncol. Biol. Phys. 2019, 105, 861–874. [Google Scholar] [CrossRef] [PubMed]
- Mender, I.; LaRanger, R.; Luitel, K.; Peyton, M.; Girard, L.; Lai, T.-P.; Batten, K.; Cornelius, C.; Dalvi, M.P.; Ramirez, M.; et al. Telomerase-Mediated Strategy for Overcoming Non–Small Cell Lung Cancer Targeted Therapy and Chemotherapy Resistance. Neoplasia 2018, 20, 826–837. [Google Scholar] [CrossRef]
- Chen, R.-J.; Wu, P.-H.; Ho, C.-T.; Way, T.-D.; Pan, M.-H.; Chen, H.-M.; Ho, Y.-S.; Wang, Y.-J. P53-dependent downregulation of hTERT protein expression and telomerase activity induces senescence in lung cancer cells as a result of pterostilbene treatment. Cell Death Dis. 2017, 8, e2985. [Google Scholar] [CrossRef]
- Brunsvig, P.F.; Guren, T.K.; Nyakas, M.; Steinfeldt-Reisse, C.H.; Rasch, W.; Kyte, J.A.; Juul, H.V.; Aamdal, S.; Gaudernack, G.; Inderberg, E.M. Long-Term Outcomes of a Phase I Study with UV1, a Second Generation Telomerase Based Vaccine, in Patients With Advanced Non-Small Cell Lung Cancer. Front. Immunol. 2020, 115, 72172. [Google Scholar] [CrossRef]
- Cong, Y.-S.; Wright, W.E.; Shay, J.W. Human Telomerase and Its Regulation. Microbiol. Mol. Biol. Rev. 2002, 66, 407–425. [Google Scholar] [CrossRef]
- Zhang, Y.; Liu, Y.; Liu, H.; Tang, W.H. Exosomes: Biogenesis, biologic function and clinical potential. Cell Biosci. 2019, 9, 19. [Google Scholar] [CrossRef]
- Goldvaser, H.; Gutkin, A.; Beery, E.; Edel, Y.; Nordenberg, J.; Wolach, O.; Rabizadeh, E.; Uziel, O.; Lahav, M. Characterisation of blood-derived exosomal hTERT mRNA secretion in cancer patients: A potential pan-cancer marker. Br. J. Cancer 2017, 117, 353–357. [Google Scholar] [CrossRef]
- Gutkin, A.; Uziel, O.; Beery, E.; Nordenberg, J.; Pinchasi, M.; Goldvaser, H.; Henick, S.; Goldberg, M.; Lahav, M. Tumor cells derived exosomes contain hTERT mRNA and transform nonmalignant fibroblasts into telomerase positive cells. Oncotarget 2016, 7, 59173–59188. [Google Scholar] [CrossRef] [PubMed]
- Filipska, M.; Rosell, R. Mutated circulating tumor DNA as a liquid biopsy in lung cancer detection and treatment. Mol. Oncol. 2021, 15, 1667–1682. [Google Scholar] [CrossRef] [PubMed]
- Li, W.; Liu, J.-B.; Hou, L.-K.; Yu, F.; Zhang, J.; Wu, W.; Tang, X.-M.; Sun, F.; Lu, H.-M.; Deng, J.; et al. Liquid biopsy in lung cancer: Significance in diagnostics, prediction, and treatment monitoring. Mol. Cancer 2022, 21, 25. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.-B.; Chen, D.-D.; He, Q.-J.; Li, L.; Zhou, G.; Fu, Y.-M.; Deng, Y.; Niu, X.-X.; Chu, F.; Gao, X.-P.; et al. The LAC Score Indicates Significant Fibrosis in Patients with Chronic Drug-Induced Liver Injury: A Large Biopsy-Based Study. Front. Pharmacol. 2021, 12, 34090. [Google Scholar] [CrossRef]
- Szpechcinski, A.; Chorostowska-Wynimko, J.; Struniawski, R.; Kupis, W.; Rudzinski, P.; Langfort, R.; Puscinska, E.; Bielen, P.; Sliwinski, P.; Orlowski, T. Cell-free DNA levels in plasma of patients with non-small-cell lung cancer and inflammatory lung disease. Br. J. Cancer 2015, 113, 476–483. [Google Scholar] [CrossRef]
- Rothwell, D.G.; Ayub, M.; Cook, N.; Thistlethwaite, F.; Carter, L.; Dean, E.; Smith, N.; Villa, S.; Dransfield, J.; Clipson, A.; et al. Utility of ctDNA to support patient selection for early phase clinical trials: The TARGET study. Nat. Med. 2019, 25, 738–743. [Google Scholar] [CrossRef]
- Wu, Y.-L.; Sequist, L.V.; Hu, C.-P.; Feng, J.; Lu, S.; Huang, Y.; Li, W.; Hou, M.; Schuler, M.; Mok, T.; et al. EGFR mutation detection in circulating cell-free DNA of lung adenocarcinoma patients: Analysis of LUX-Lung 3 and 6. Br. J. Cancer 2016, 116, 175–185. [Google Scholar] [CrossRef]
- Nardo, G.; Carlet, J.; Marra, L.; Bonanno, L.; Boscolo, A.; Maso, A.D.; Bragadin, A.B.; Indraccolo, S.; Zulato, E. Detection of Low-Frequency KRAS Mutations in cfDNA from EGFR-Mutated NSCLC Patients After First-Line EGFR Tyrosine Kinase Inhibitors. Front. Oncol. 2021, 10, 607840. [Google Scholar] [CrossRef]
- Boldrin, E.; Nardo, G.; Zulato, E.; Bonanno, L.; Polo, V.; Frega, S.; Pavan, A.; Indraccolo, S.; Saggioro, D. Detection of Loss of Heterozygosity in cfDNA of Advanced EGFR- or KRAS-Mutated Non-Small-Cell Lung Cancer Patients. Int. J. Mol. Sci. 2019, 21, 66. [Google Scholar] [CrossRef]
- Almodovar, K.; Iams, W.T.; Meador, C.B.; Zhao, Z.; York, S.; Horn, L.; Yan, Y.; Hernandez, J.; Chen, H.; Shyr, Y.; et al. Longitudinal Cell-Free DNA Analysis in Patients with Small Cell Lung Cancer Reveals Dynamic Insights into Treatment Efficacy and Disease Relapse. J. Thorac. Oncol. 2017, 13, 112–123. [Google Scholar] [CrossRef] [PubMed]
- Mayo-de-Las-Casas, C.; Jordana-Ariza, N.; Garzón-Ibañez, M.; Balada-Bel, A.; Bertrán-Alamillo, J.; Viteri-Ramírez, S.; Reguart, N.; Muñoz-Quintana, M.A.; Lianes-Barragan, P.; Camps, C.; et al. Large scale, prospective screening of EGFR mutations in the blood of advanced NSCLC patients to guide treatment decisions. Ann. Oncol. 2017, 28, 2248–2255. [Google Scholar] [CrossRef] [PubMed]
- Blakely, C.M.; Watkins, T.B.K.; Wu, W.; Gini, B.; Chabon, J.J.; E McCoach, C.; McGranahan, N.; A Wilson, G.; Birkbak, N.J.; Olivas, V.R.; et al. Evolution and clinical impact of co-occurring genetic alterations in advanced-stage EGFR-mutant lung cancers. Nat. Genet. 2017, 49, 1693–1704. [Google Scholar] [CrossRef]
- Chabon, J.J.; Hamilton, E.G.; Kurtz, D.M.; Esfahani, M.S.; Moding, E.J.; Stehr, H.; Schroers-Martin, J.; Nabet, B.Y.; Chen, B.; Chaudhuri, A.A.; et al. Integrating genomic features for non-invasive early lung cancer detection. Nature 2020, 580, 245–251. [Google Scholar] [CrossRef] [PubMed]
- Schoenfeld, A.J.; Chan, J.M.; Kubota, D.; Sato, H.; Rizvi, H.; Daneshbod, Y.; Chang, J.C.; Paik, P.K.; Offin, M.; Arcila, M.E.; et al. Tumor Analyses Reveal Squamous Transformation and Off-Target Alterations as Early Resistance Mechanisms to First-line Osimertinib in EGFR-Mutant Lung Cancer. Clin. Cancer Res. 2020, 26, 2654–2663. [Google Scholar] [CrossRef] [PubMed]
- Beagan, J.J.; Bach, S.; van Boerdonk, R.A.; van Dijk, E.; Thunnissen, E.; van den Broek, D.; Weiss, J.; Kazemier, G.; Pegtel, D.M.; Bahce, I.; et al. Circulating tumor DNA analysis of EGFR-mutant non-small cell lung cancer patients receiving simertinib following previous tyrosine kinase inhibitor treatment. Lung Cancer 2020, 145, 173–180. [Google Scholar] [CrossRef]
- Cheng, Y.; Ma, L.; Liu, Y.; Zhu, J.; Xin, Y.; Liu, X.; Wang, Y.; Zhang, T.; Yang, C.; Wang, S.; et al. Comprehensive characterization and clinical impact of concomitant genomic alterations in EGFR-mutant NSCLCs treated with EGFR kinase inhibitors. Lung Cancer 2020, 145, 63–70. [Google Scholar] [CrossRef]
- Liu, H.E.; Vuppalapaty, M.; Wilkerson, C.; Renier, C.; Chiu, M.; Lemaire, C.; Che, J.; Matsumoto, M.; Carroll, J.; Crouse, S.; et al. Detection of EGFR Mutations in cfDNA and CTCs, and Comparison to Tumor Tissue in Non-Small-Cell-Lung-Cancer (NSCLC) Patients. Front. Oncol. 2020, 10, 572895. [Google Scholar] [CrossRef]
- Zhou, Q.; Geng, Q.; Wang, L.; Huang, J.; Liao, M.; Li, Y.; Ding, Z.; Yang, S.; Zhao, H.; Shen, Q.; et al. Value of folate receptor-positive circulating tumour cells in the clinical management of indeterminate lung nodules: A non-invasive biomarker for predicting malignancy and tumour invasiveness. Ebiomedicine 2019, 41, 236–243. [Google Scholar] [CrossRef]
- Lim, M.; Park, J.; Lowe, A.C.; Jeong, H.O.; Lee, S.; Park, H.C.; Lee, K.; Kim, G.H.; Kim, M.-H.; Cho, Y.-K. A lab-on-a-disc platform enables serial monitoring of individual CTCs associated with tumor progression during EGFR-targeted therapy for patients with NSCLC. Theranostics 2020, 10, 5181–5194. [Google Scholar] [CrossRef]
- Zhang, Z.; Eramnath, N.; Enagrath, S. Current Status of CTCs as Liquid Biopsy in Lung Cancer and Future Directions. Front. Oncol. 2015, 5, 209. [Google Scholar] [CrossRef]
- Hofman, P. ALK Status Assessment with Liquid Biopsies of Lung Cancer Patients. Cancers 2017, 9, 106. [Google Scholar] [CrossRef]
- Cazzoli, R.; Buttitta, F.; Di Nicola, M.; Malatesta, S.; Marchetti, A.; Rom, W.N.; Pass, H.I. microRNAs Derived from Circulating Exosomes as Noninvasive Biomarkers for Screening and Diagnosing Lung Cancer. J. Thorac. Oncol. 2013, 8, 1156–1162. [Google Scholar] [CrossRef]
- Cristiano, S.; Leal, A.; Phallen, J.; Fiksel, J.; Adleff, V.; Bruhm, D.C.; Jensen, S.Ø.; Medina, J.E.; Hruban, C.; White, J.R.; et al. Genome-wide cell-free DNA fragmentation in patients with cancer. Nature 2019, 570, 385–389. [Google Scholar] [CrossRef]
- Jin, X.; Chen, Y.; Chen, H.; Fei, S.; Chen, D.; Cai, X.; Liu, L.; Lin, B.; Su, H.; Zhao, L.; et al. Evaluation of tumor-derived Exosomal miRNA as potential diagnostic biomarkers for early-stage non-small cell lung Cancer using next-generation sequencing. Clin. Cancer Res. 2017, 23, 5311–5319. [Google Scholar] [CrossRef] [PubMed]
- Qin, X.; Yu, S.; Zhou, L.; Shi, M.; Hu, Y.; Xu, X.; Shen, B.; Liu, S.; Yan, D.; Feng, J. Cisplatin-resistant lung cancer cell–derived exosomes increase cisplatin resistance of recipient cells in exosomal miR-100–5p-dependent manner. Int. J. Nanomed. 2017, 12, 3721–3733. [Google Scholar] [CrossRef]
- Liu, A.; Xie, H.; Li, R.; Ren, L.; Yang, B.; Dai, L.; Lu, W.; Liu, B.; Ren, D.; Zhang, X.; et al. Silencing ZIC2 abrogates tumorigenesis and anoikis resistance of non-small cell lung cancer cells by inhibiting Src/FAK signaling. Mol. Ther. Oncolytics 2021, 22, 195–208. [Google Scholar] [CrossRef] [PubMed]
- Yang, D.; Feng, W.; Zhuang, Y.; Liu, J.; Feng, Z.; Xu, T.; Wang, W.; Zhu, Y.; Wang, Z. Long non-coding RNA linc00665 inhibits CDKN1C expression by binding to EZH2 and affects cisplatin sensitivity of NSCLC cells. Mol. Ther. Nucleic Acids 2021, 23, 1053–1065. [Google Scholar] [CrossRef]
- Huber, M.; Kepesidis, K.V.; Voronina, L.; Fleischmann, F.; Fill, E.; Hermann, J.; Koch, I.; Milger-Kneidinger, K.; Kolben, T.; Schulz, G.B.; et al. Author response: Infrared molecular fingerprinting of blood-based liquid biopsies for the detection of cancer. eLife 2021, 10, e68758. [Google Scholar] [CrossRef] [PubMed]
- Wu, S.H.; Hsieh, C.C.; Hsu, S.C.; Yao, M.; Hsiao, J.K.; Wang, S.W.; Lin, C.P.; Huang, D.M. RBC-derived vesicles as a systemic delivery system of doxorubicin for lysosomal- mitochondrial axis-improved cancer therapy. J. Adv. Res. 2020, 301, 85–96. [Google Scholar] [CrossRef] [PubMed]
- Laish, I.; Levi, Z.; Mahajna, H.; Albshesh, A.; Horesh, N.; Katz, E.; Feldman, D.; Shinar, N.; Picard, O.; Yavzori, M.; et al. Characterization of blood-derived exosomal hTERT mRNA as a biomarker for colon cancer and Lynch syndrome. Front. Oncol. 2022, 12, 62473. [Google Scholar] [CrossRef]
- Xia, Z.; Qing, B.; Wang, W.; Gu, L.; Chen, H.; Yuan, Y. Formation, contents, functions of exosomes and their potential in lung cancer diagnostics and therapeutics. Thorac. Cancer 2021, 12, 3088–3100. [Google Scholar] [CrossRef]
- Li, M.-Y.; Liu, L.-Z.; Dong, M. Progress on pivotal role and application of exosome in lung cancer carcinogenesis, diagnosis, therapy and prognosis. Mol. Cancer 2021, 20, 22. [Google Scholar] [CrossRef] [PubMed]
- Jiang, C.; Zhang, N.; Hu, X.; Wang, H. Tumor-associated exosomes promote lung cancer metastasis through multiple mechanisms. Mol. Cancer 2021, 20, 117. [Google Scholar] [CrossRef]
- Zhang, W.; Qin, T.; Yang, Z.; Yin, L.; Zhao, C.; Feng, L.; Lin, S.; Liu, B.; Cheng, S.; Zhang, K. Telomerase-positive circulating tumor cells are associated with poor prognosis via a neutrophil-mediated inflammatory immune environment in glioma. BMC Med. 2021, 19, 277. [Google Scholar] [CrossRef] [PubMed]
- Chen, R.; Xu, X.; Qian, Z.; Zhang, C.; Niu, Y.; Wang, Z.; Sun, J.; Zhang, X.; Yu, Y. The biological functions and clinical applications of exosomes in lung cancer. Cell Mol. Life Sci. 2019, 76, 4613–4633. [Google Scholar] [CrossRef]
- Jeon, H.-S.; Choi, J.E.; Jung, D.K.; Choi, Y.Y.; Kang, H.G.; Lee, W.-K.; Yoo, S.S.; Lim, J.-O.; Park, J.Y. Telomerase Activity and the Risk of Lung Cancer. J. Korean Med. Sci. 2012, 27, 141–145. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.; Duan, X.; Zhang, Z.; Yang, Z.; Zhao, C.; Liang, C.; Liu, Z.; Cheng, S.; Zhang, K. Combination of CT and telomerase-positive circulating tumor cells improves diagnosis of small pulmonary nodules. J. Clin. Investig. 2021, 6, e148182. [Google Scholar] [CrossRef] [PubMed]
- Ha, D.; Yang, N.; Nadithe, V. Exosomes as therapeutic drug carriers and delivery vehicles across biological membranes: Current perspectives and future challenges. Acta Pharm. Sin. B 2016, 6, 287–296. [Google Scholar] [CrossRef]
- Karpov, O.; Lahav, M.; Wolach, O.; Raanani, P.; Peer, D.; Kaplan, T.; Uziel, O. Identification of Cancer Cells in the Human Body by Anti-Telomerase Peptide Antibody: Towards the Isolation of Circulating Tumor Cells. Int. J. Mol. Sci. 2022, 23, 12872. [Google Scholar] [CrossRef]
- Han, H.; He, C.; Chen, X.; Luo, Y.; Yang, M.; Wen, Z.; Hu, J.; Lin, F.; Han, M.; Yin, T.; et al. Shikonin N-benzyl matrinic acid ester derivatives as novel telomerase inhibitors with potent activity against lung cancer cell lines. Bioorganic Med. Chem. Lett. 2021, 57, 128503. [Google Scholar] [CrossRef] [PubMed]
- Prasad, R.R.; Mishra, D.K.; Kumar, M.; Yadava, P.K. Human telomerase reverse transcriptase promotes the epithelial to mesenchymal transition in lung cancer cells by enhancing c-MET upregulation. Heliyon 2021, 8, e08673. [Google Scholar] [CrossRef] [PubMed]
| Age | Gender | RQ | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Median | Range | F | M | Mean RQ | SEM | Median | Range | Type | Stage | |
| positives | 40 | 66.5 | 46–85 | 28 | 12 | 6.45 | 1.44 | 3.67 | 1.23–44.61 | NSCLC-30, SCLC-10 | IIIa-2, IIIb-3, IV-35 |
| negatives | 36 | 67 | 38–88 | 22 | 14 | 0.36 | 0.05 | 0.33 | 0–1.18 | NSCLC-30, SCLC-3, others-3 | IIIb-10, IV-26 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rotem, O.; Zer, A.; Yosef, L.; Beery, E.; Goldvaser, H.; Gutkin, A.; Levin, R.; Dudnik, E.; Berger, T.; Feinmesser, M.; et al. Blood-Derived Exosomal hTERT mRNA in Patients with Lung Cancer: Characterization and Correlation with Response to Therapy. Biomedicines 2023, 11, 1730. https://doi.org/10.3390/biomedicines11061730
Rotem O, Zer A, Yosef L, Beery E, Goldvaser H, Gutkin A, Levin R, Dudnik E, Berger T, Feinmesser M, et al. Blood-Derived Exosomal hTERT mRNA in Patients with Lung Cancer: Characterization and Correlation with Response to Therapy. Biomedicines. 2023; 11(6):1730. https://doi.org/10.3390/biomedicines11061730
Chicago/Turabian StyleRotem, Ofer, Alona Zer, Lilach Yosef, Einat Beery, Hadar Goldvaser, Anna Gutkin, Ron Levin, Elizabeth Dudnik, Tamar Berger, Meora Feinmesser, and et al. 2023. "Blood-Derived Exosomal hTERT mRNA in Patients with Lung Cancer: Characterization and Correlation with Response to Therapy" Biomedicines 11, no. 6: 1730. https://doi.org/10.3390/biomedicines11061730
APA StyleRotem, O., Zer, A., Yosef, L., Beery, E., Goldvaser, H., Gutkin, A., Levin, R., Dudnik, E., Berger, T., Feinmesser, M., Levy-Barda, A., Lahav, M., Raanani, P., & Uziel, O. (2023). Blood-Derived Exosomal hTERT mRNA in Patients with Lung Cancer: Characterization and Correlation with Response to Therapy. Biomedicines, 11(6), 1730. https://doi.org/10.3390/biomedicines11061730







