1. Introduction
COVID-19, a highly contagious disease caused by SARS-CoV-2, is associated with clinical manifestations ranging from asymptomatic to severely diseased states such as pneumonia, acute respiratory distress syndrome (ARDS) and acute lung injury (ALI), multi-organ failure, and even death. COVID-19 has infected over 600 million people during the pandemic resulting in more than 6 million deaths.
The virus enters the cell by binding viral spike protein (S1) to the epithelial cells’ angiotensin-converting enzyme 2 (ACE2), one of the main components of the renin–angiotensin System (RAS) [
1]. Recent studies identified soluble ACE2 levels in plasma as a reliable biomarker of COVID-19 [
2,
3]. Similarly, plasma levels of angiotensin (Ang) peptides and anti-ACE2 auto-antibodies have been considered biomarkers of rheumatoid arthritis [
4]. The classical arm of RAS involves ACE/Ang II/Ang II type 1 receptor (AT1R) and controls a diverse range of biological effects through AT1R stimulation by Ang II. On the other hand, the RAS protective arm comprises ACE2/Ang 1–7/Mas receptor (MasR), which counteracts the effects of Ang II [
5,
6]. Ang II, initially produced by the enzymatic action of ACE on Ang I, plays a pivotal role in regulating blood pressure, electrolyte and fluid balance, and inflammatory pathogenesis. Overstimulation of the classical arm by excessive Ang II produces pro-inflammatory (e.g., ALI), proliferative, and fibrotic effects [
7]. ACE2 converts the pro-inflammatory peptide Ang II to the anti-inflammatory peptide Ang 1–7 [
8]. Ang 1–7 acts as the RAS’s counter-regulatory peptide, presenting anti-inflammatory, anti-proliferative, and anti-fibrotic effects, and maintaining the body’s hemostasis [
9]. The Ang 1–7/Ang II ratio is a critical factor in the activated RAS balance distortion (
Figure 1). The binding of the virus to ACE2 leads to its internalization, causing an imbalance between ACE/ACE2, resulting in an unopposed higher level of Ang II and changing Ang 1–7/Ang II, which overactivates the AT1R and by losing the protective effects of the Ang 1–7/Mas R, it starts an inflammatory process that leads to a so-called cytokine storm and initiation and progression of ALI and ARDS [
10]. Treatment with ACE inhibitors (ACEi) and Ang II receptor blockers (ARB) theoretically have the potential to prevent and maybe treat ALI and ARDS resulting from COVID-19 infection [
11].
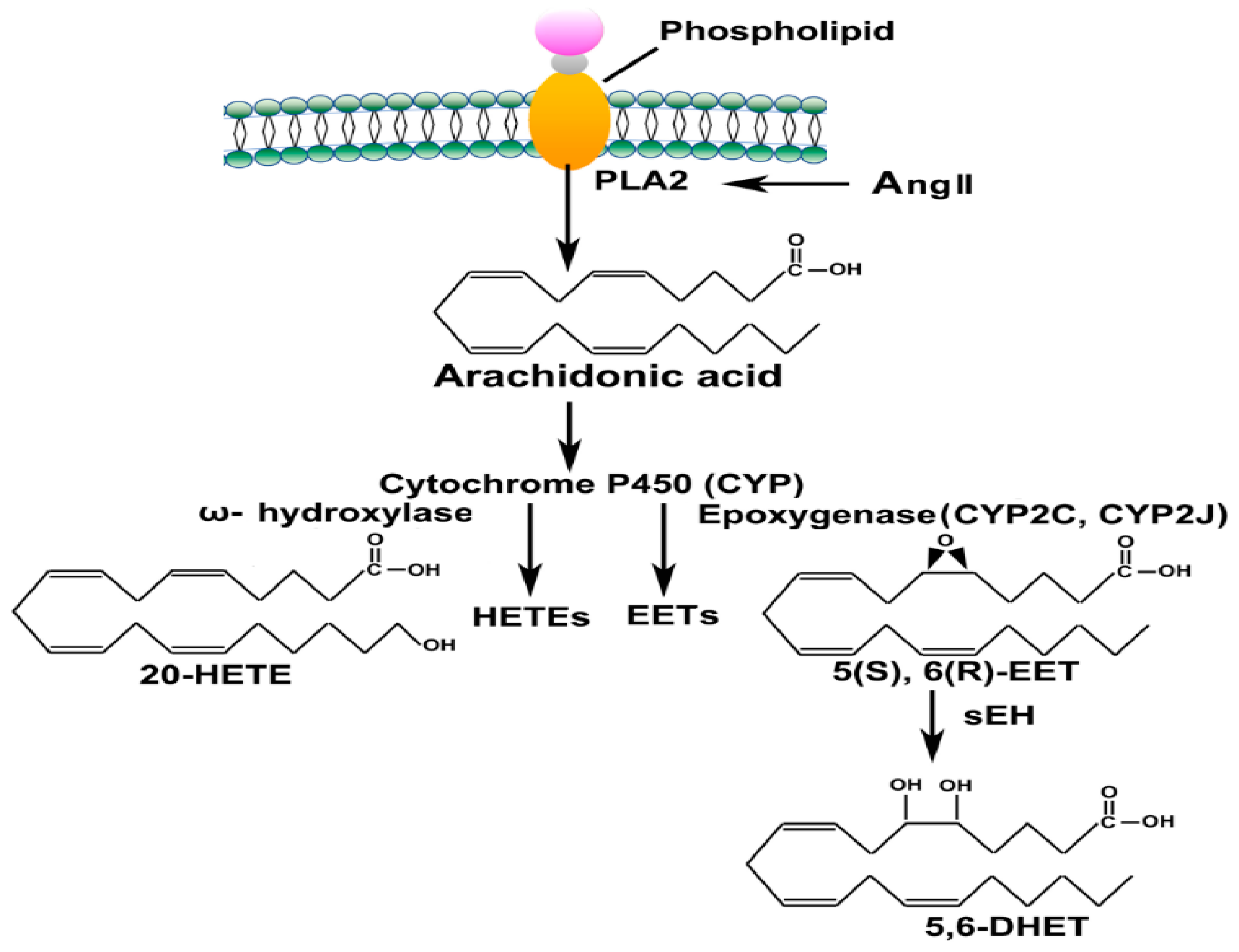
Arachidonic Acid (ArA) is released during an inflammatory response by action of phospholipase 2 (PLA2) and then metabolized by different CYP450 enzymes (ω-hydroxylase and epoxygenase) to convert into eicosanoids such as hydroxyeicosatetraenoic acids (HETEs) and epoxyeicosatrienoic acids (EETs), respectively (
Figure 2). These eicosanoids function in diverse physiological systems associated with inflammation processes [
12,
13,
14]. For instance, 20-HETE, a potent vasoconstrictor, regulates vascular tone, blood flow to specific organs, and sodium and fluid transport to the kidneys [
15]. EETs act as an endothelium-derived hyperpolarizing factor and present with potent vasodilatory and anti-inflammatory effects [
16].
Like ACE/ACE2 and Ang II/Ang 1–7 ratios, the balance between 20-HETE/EETs is critical for the body’s physiological homeostasis. Results from adjuvant arthritis animal studies demonstrate that the RAS and ArA pathways are affected, and the balance between their pro and anti-inflammatory axes is disturbed [
17,
18]. The two pathways are interrelated and directly correlated, demonstrating their significance in the inflammatory response process. Ang II up-regulates phospholipase A, causing ArA release from the cell membrane, propagating the inflammatory cascade furthermore through the ArA pathway [
19]. An imbalance between the vasoconstrictor and vasodilator ArA metabolites occurs due to inflammation impacting the RAS and increasing Ang II levels [
20]. COVID-19′s inflammatory response affects the RAS and ArA pathways [
21]. Given the systemic and local RAS and ArA pathways play essential roles in the homeostasis of vital organs such as lungs, heart, liver, and kidneys, we expect that the understanding and knowledge of the RAS and ArA pathways biomarkers’ status and their association with patient demographic variables (such as gender, age, body mass index (BMI), and underlying comorbidities) could help physicians to predict future complications in these organs and plan for better intervention.
The impact of sex difference is one of the unique traits seen in COVID-19 infections. Recent studies have shown that males are more affected by the disease than females, with higher mortality and hospitalization rate [
22,
23]. Although the mechanism for this discrepancy has not been elucidated, recent communication reports attributed it to an infectivity mechanism of COVID-19 involving the ACE2 receptor, Type II transmembrane Serine Protease (TMPRSS 2) and androgen receptor [
24]. TMPRSS 2 is vital in activating viral spike protein, a crucial step in viral entry. The androgen receptor is a known promoter of TMPRSS2 gene expression [
25]. The upregulation of this gene by the androgenic stimulation could explain the higher infectivity in males [
26]. In addition, lesser infectivity in children could be explained by the lower expression of the androgen receptors due to underdeveloped sex organs. The phenomenon has been reported for sex hormones’ influence on ACE2 expression and activity in the mouse adipose tissue, kidneys, and myocardium [
27,
28,
29]. While speculation, it seems reasonable that if the sex hormone modulator 17β-Oestradiol affects the expression and activity of the ACE2 receptor and increases Ang 1–7 levels; thus, hormone therapy offers a potential supportive treatment for female COVID-19 patients [
30].
Based on the data provided by the U.S. Centers for Disease Control (CDC), rates of hospitalization and death increase with age. Compared to the age group of 18–29 years, the hospitalization rate was 5× higher in the 65–74 and 9.1× more in the 75–84 age groups. Similarly, the mortality rate increased by 25× in the 50–64, 65× in the 65–74 and 140× in the 75–84 age groups [
31]. COVID-19 hospitalizations rate could also be correlated with obesity and BMI. A study from Johns Hopkins showed that the hospitalization rate increased in adults with obesity and underweight relative to the normal weight [
32]. Obesity is also linked to impaired immune function and reduction in lung capacity, thereby increasing the risk of infection and impairing ventilation. As reported by CDC, increased BMI could be related to an increased risk of ICU admission, invasive mechanical ventilation, and death [
33].
This study aims to analyze the effector RAS peptides (Ang II and Ang 1–7) and relate them with the metabolites of the CYP450-mediated ArA pathway. Additionally, we correlated these metabolites with the demographic variables known to worsen the prognosis of COVID-19 to understand how these variables play a role at the molecular level in the infection. The results of this study help explain how variability in biomarkers combined with individuals’ demographics and comorbidities correlate with COVID-19 disease intensity. Such knowledge could allow healthcare providers to predict future complications and plan for better interventions.
2. Materials and Methods
2.1. Materials
Ang 1–7 (Anaspec, AS-61039) and Ang II (Anaspec, AS-20633) were acquired from Anaspec Inc. (Fremont, CA, USA). (Asn1, Val5)-Ang II (IS), Sigma-Aldrich A6402-1MG, was obtained from Sigma Aldrich (St. Louis, MO, USA). Waters C18 SPE cartridges (Sep-Pak WAT020805) were purchased from Waters (Milford, MA, USA). The reference standards for ArA metabolites were procured from Cayman Chemical Company (Ann Arbor, MI, USA). These included 19-(R)-hydroxyeicosatetraenoic acid (19-HETE) (P/N,10007767), 20-hydroxyeicosatetraenoic acid (20-HETE) (P/N,90030), (±)-5,6-epoxyeicosatrienoic acid (5,6-EET) (P/N,50211), (±)8,9-epoxyeicosatrienoic acid (8,9-EET) (P/N,50351), (±)11,12-epoxyeicosatrienoic acid (11,12-EET) (P/N,50511), (±)14,15-epoxyeicosatrienoic Acid (14,15-EET) (P/N,50651), (±)-5,6-dihydroxyeicosatrienoic acid (5,6-DHET) (P/N, 51211), (±)8,9-dihydroxyeicosatrienoic acid (8,9-DiHT) (P/N,51351), (±)11,12-dihydroxyeicosatrienoic acid (11,12-DHET) (P/N,51511), and (±)14,15-dihydroxyeicosatrienoic acid (14,15-DHET) (P/N,51651). The deuterated internal standards (IS) listed below were also obtained from Cayman, with the deuterium atoms present at the carbons 16, 17, 18, 19, and 20 positions and an isotopic purity of ≥99% for 8,9-EET-d11. LC-MS grade water, acetonitrile, and formic acid were purchased from Fisher Scientific (Fair Lawn, NJ, USA).
2.2. LC-MS/MS System
LC-MS/MS system comprised of liquid chromatography (Shimadzu, MD, USA) with a binary pump (LC-30AD), an autosampler (SIL-30AC), a controller (CBM-20A), a degasser (DGU-20A5R), a column oven (CTO-20A), and an ABSciex QTRAP 5500 mass spectrometer (SCIEX, Foster City, CA, USA) with electron spray ionization (ESI) source. The chromatograms were monitored using Analyst 1.7 software, and the data were analyzed in MultiQuant 3.0 software (SCIEX, Foster City, CA, USA). The analytes were separated using Synergi™ Fusion-RP column (2.5 µm, 100 × 2 mm) obtained from Phenomenex (Torrance, CA, USA). All the analyses were performed in positive ion mode.
2.3. Human Subject
The Institutional Review Board approved this study through the IRB-FY2020-273 protocol to analyze de-identified COVID-19 patients’ plasma samples provided by the University of Utah Hospital under a signed Material Transfer Agreement. These patients were recruited for another study at the University of Utah which the institution’s IRB also reviewed and approved all study recruitment materials, educational information, participant instructions for self-collection of specimens, surveys, and the informed consent documents (IRB-00102638) and (IRB-00093575).
The University of Utah research group inclusion criteria for healthy volunteers were consenting male and female subjects of any self-identified race/ethnicity without acute or chronic illnesses aged 18 and older, and exclusion criteria were the use of any prescription medication, pregnancy, suffering from any acute or chronic medical condition or disease, having been hospitalized or had surgery within the preceding 6 weeks, or having any prior history of stroke. The inclusion criteria for COVID patients were ICU admission with confirmed infection and organ dysfunction as defined by a Sequential Organ Failure Assessment (SOFA) ≥ 2 above baseline (if baseline data are unavailable, baseline SOFA is assumed to be 0). All patients were enrolled in the study within 72 h of ICU admission. Additionally, individuals diagnosed with COVID and hospitalized with acute COVID infection were enrolled in the study. The exclusion criteria were admission to the ICU for longer than 72 h, hemoglobin level < 7 gm/dL, or clinically significant bleeding.
After the patient met inclusion criteria and no exclusion criteria were indicated, subjects provided consent using approved IRB protocols. Once subjects consented, a whole blood sample was drawn within 48 (±24) h (study day 0) of a COVID-19 diagnosis. Aliquots of blood samples were mixed with a protease inhibitor cocktail solution containing 1.0 mM p-hydroxy mercury benzoate, 30 mM 1,10-phenanthroline, 1.0 mM phenylmethylsulphonyl fluoride, 1.0 mM Pepstatin A, and 7.5% EDTA (all from Sigma Aldrich, St. Louis, MO, USA), and treated with 1% Triton X (to inactivate the virus). Plasma was harvested after centrifugation for 10 min at 2500× g and 4 °C and stored at −80 °C until assayed.
2.4. Sample Preparation Procedures
2.4.1. Solid-Phase Extraction (SPE)
Angiotensin peptides (Ang 1–7 and Ang II) were extracted from the plasma samples using solid phase extraction (SPE). SPE was carried out based on a previously established method by Cui et al. with minor changes in the process [
34]. Briefly, 200 μL of plasma samples was mixed with 100 μL of the internal standard (50 ng/mL). Then, 1.5 μL of formic Acid was added to make the final concentration of 0.5%. The samples were mixed and loaded onto the Waters C18 SPE cartridges previously preconditioned with 3 mL ethanol and 3 mL deionized water. Samples were then loaded onto the cartridge and allowed to interact with the column by application of a positive nitrogen flow from a positive pressure manifold (Agilent Technologies Inc., Santa Clara, CA, USA). It was then washed with 3 mL of deionized water and eluted with 3 mL of methanol containing 5% formic acid. The eluted solutions were collected and dried using a Savant 200 SpeedVac system (Thermo Fisher Scientific, Waltham, MA, USA). The dried samples were reconstituted in 100 µL of acidified water containing 0.1% formic acid, and 10 µL of samples were injected into the LC-MS/MS to quantify the Ang peptides concentrations.
2.4.2. Liquid–Liquid Extraction (LLE)
A liquid–liquid extraction (LLE) method using ethyl acetate was utilized to extract the ArA metabolites from the plasma samples. This method was previously validated in our lab [
35]. Briefly, 300 µL of plasma sample was mixed with 100 µL of 10,11-EET d11 (IS, 100 ng/mL), and 2 µL of FA was added. The samples were vortexed, and 500 µL of ethyl acetate was added. The resulting biphasic solutions were mixed thoroughly by vortexing for 1 min and centrifuged at 15,000×
g, 4 °C, for 15 min. After centrifugation, 400 µL of the supernatant layer was taken, and for a second extraction step, 500 µL of the ethyl acetate was added again. The organic supernatant phase was mixed with the previous step extract, dried under nitrogen gas, and reconstituted in methanol for LC-MS/MS analysis. A volume of 30 µL of the sample was injected into the LC-MS/MS.
2.4.3. LC-MS/MS Method for Ang Peptides
Ang 1–7 and Ang II levels in the patients’ plasma samples were analyzed using the LC-MS/MS method described in a published study [
34]. Minor modifications and validation were performed before applying the analytical method for plasma sample analysis. Separation of Ang peptides was achieved using a Synergi RP column (2 × 100 mm) with a particle size of 2.5 μm from Phenomenex (Torrance, CA, USA). The column was maintained at ambient temperature. The mobile phase contained water with 0.1% formic acid (A) and ACN (B).
The gradient time program was initiated with 5% ACN and increased to 30% ACN over a 4-min period. The composition was held steady from 4 to 8 min, then decreased to 5% ACN at 9 min and maintained for 10 min. The flow rate was set at 0.3 mL/min, and the injection volume was 30 μL. Electrospray ionization was employed, and the analytes were detected using multiple reaction monitoring (MRM) in positive mode. The optimized parameters for the source/gas were as follows: curtain gas, 30; collision gas, medium; ion spray voltage, 5500 V; temperature, 300 °C; ion source gas 1 (nebulizer gas), 20 psi; and ion source gas 2 (turbo gas), 25 psi.
LC-MS analysis was conducted using the single ion recording (SIR) mode, with specific m/z values: 300.5 for Ang 1–7, 349.6 for Ang II, and 516.6 for the internal standard (IS). For LC-MS/MS, the MRM transitions used were m/z 300.6→136 for Ang 1–7, m/z 349.6→136 for Ang II, and m/z 516→769.4 for the internal standard.
2.4.4. LC-MS/MS Method for ArA Metabolites
The experimental protocol and assay conditions were conducted with minor optimization to analyze ArA metabolites, following a previously described method [
35]. In summary, these metabolites were separated using a Synergi
TM RP column (2 × 100 mm) with a particle size of 2.5 μm from Phenomenex (Torrance, CA, USA). The separation was carried out at ambient temperature. The mobile phase contained water with 0.1% formic acid (A) and ACN (B).
The gradient time program for the mobile phase began with 5% ACN and increased to 20% ACN within 2 min. It was then raised to 55% ACN and maintained for 2.5 to 6 min before rising to 100% ACN at 8 min. The method continued until 9 min, after which the mobile phase was reduced to 5% ACN over a total run time of 10.5 min. The flow rate was set at 0.3 mL/min, and the injection volume was 10 μL.
For mass spectrometric analysis, a triple quadrupole was utilized to monitor the m/z transitions using the Analyst® 1.7.2 software. Electrospray ionization was employed, and the analytes were detected using multiple reaction monitoring (MRM) in the negative mode. The optimized parameters for the source/gas were as follows: curtain gas, 20 psi; collision gas, medium; ion spray voltage, approximately 4500 V; temperature, 400 °C; ion source gas 1 (nebulizer gas), 20 psi; and ion source gas 2 (turbo gas), 25 psi.
2.5. Statistical Analysis
Patients’ demographic data are presented as mean ± standard deviation (SD). The biomarkers data are expressed as mean ± standard error of means (SEM) and analyzed by a standard computer program, GraphPad Prism Software PC software, version 9.3.1, and Statistical Package for Social Sciences (SPSS) version 28 for Windows (SPSS Inc., Chicago, IL, USA). The plasma concentrations of some of the ArA metabolites in some patients were lower than the LC-MS/MS method detection limit. In addition, the level of Ang II (in three cases) fell outside the 3 standard deviations threshold based on the Z-score method and were considered outliers. Therefore, those patients were excluded in the statistical comparison case by case. Data were tested for normal distribution using the Kolmogorov–Smirnov test and homogeneity of variance using Levene’s test before proceeding with the non-parametric statistical tests. Group comparisons were made using the Mann–Whitney U test, and the correlation for the continuous variables was analyzed using Pearson’s correlation coefficient. The confidence interval was set at 95%, and p < 0.05 was considered statistically significant.
4. Discussion
In this study, we evaluated and compared the RAS components (Ang 1–7, Ang II plasma levels, Ang 1–7/Ang II ratio) and ArA metabolites (HETEs, EETs and DHETs) between healthy controls and COVID-19 patients to determine whether the RAS axes were unbalanced in COVID-19 patients and impacted on the ArA pathway and its metabolites profiles.
Our results indicate that Ang 1–7 levels were significantly lower, whereas Ang II levels were prominently higher in the COVID-19 patients than in the healthy control individuals (
Figure 3 and
Table 2). The ratio of Ang 1–7/Ang II as an indicator of the balance between the RAS classical and protective arms was dramatically lower in COVID-19 patients. Such imbalance is attributed to the deactivation of the ACE2 enzyme by the SARS-CoV-2 virus and matched with measured higher Ang II plasma levels in these patients. Our study’s results agree with most of the previous reports that showed that the protective arm of the RAS is downregulated due to the infection [
36,
37,
38,
39]. In concert with our findings, these studies found significantly lower circulating Ang 1–7 levels in COVID-19 patients than in the control group. They also reported that the Ang II levels were lower in the patients that recovered from the disease than those who succumbed to the infection, and, similarly, concluded that the elevated ratio of Ang II/Ang 1–7 is an indication that the balance of the RAS shifted towards the classical axis with increasing hospitalization, disease severity, and mortality [
36]. In another study, Lieu et al. found plasma Ang II levels to be elevated in the COVID-19-infected groups compared to healthy controls [
38]. Additionally, the study of Wu et al. determined that the circulating plasma concentration of Ang II increased with the severity of the disease [
39].
Although our study results align with most recently reported literature [
36,
37,
38,
39], few studies have reported that Ang 1–7 levels were elevated in the infected group rather than in the controls [
40,
41,
42]. The observed controversy could be explained by different methodological approaches in patient enrolment or sample collection and analysis, among other possible explanations. Martins et al. analyzed plasma samples from individuals already taking ACEi or ARBs [
40]. These classes of drugs are known to increase ACE2 activity, elevate Ang 1–7, and reduce Ang II plasma levels. Such an effect is expected to be more pronounced in healthy controls as no virus is present to inhibit ACE2 enzyme activity, somehow explaining the observations of Martins et al. [
40]. A comprehensive meta-analysis showed that the levels of Ang 1–7 in some studies were approximately 11-fold higher in the infected group than in the control group. It also included other controversial studies that reported the other way around. Interestingly, this meta-analysis founds that the level of Ang II was also elevated in the COVID-19-infected group [
40]. The observed contradiction could have occurred due to including a range of studies that utilized different sample collection and processing methods. Some of those studies did not consider the enzymes and peptide stability, and some used nonspecific analytical methods, as highlighted by Martins et al. [
40]. In another small study (enrolling 10 patients and 5 healthy control subjects), authors looked at equilibrium analysis reflecting overall plasmatic RAS activity instead of its actual status as they did not consider adding protease inhibitors to plasma samples [
41]. That means the reported results are not representing the actual status of the RAS components at the time of sample collection. Therefore, it is not a direct measure of RAS peptides, but measures the ongoing activity of RAS proteases which could make a significant difference in the level of peptides. It is worth mentioning that the RAS is a complex system comprised of non-ACE pathways that could impact the Ang II and Ang1–7 levels when ACE2 activity was influenced by COVID-19 infection [
41].
It is worth mentioning the observed results indicate that both arms of the RAS are affected by this viral infection. The binding of the virus to ACE2 leads to its down-regulation, causing an imbalance between ACE/ACE2 and consequently resulting in a lower Ang 1–7/Ang II ratio and a surge of an unopposed Ang II and cytokine storm to impose tissue injury depicted in
Figure 1, signifying the lung as a typically impacted primary tissue by the virus. The RAS is closely linked to cardiovascular function, and its dysregulation in COVID-19 can have cardiovascular implications. Ang II can promote vasoconstriction, oxidative stress, and prothrombotic effects, increasing the risk of cardiovascular complications reported in infected individuals. The inflammatory response triggered by the dysregulated RAS can damage endothelial cells, disrupt the integrity of blood vessels, and contribute to cardiovascular dysfunction. Such phenomenon has been supported by an animal model of arthritis, where an imbalance of the cardiac and renal RAS components explains the cardio-renal toxicity [
17]. Treatment with ACE inhibitors (ACEi) and Ang II receptor blockers (ARB), which are commonly used to manage hypertension, could be beneficial in COVID-19 by potentially mitigating the harmful effects of an imbalanced RAS [
42]. However, more research is needed to fully understand the complex interactions between RAS and COVID-19 and determine the optimal therapeutic approaches.
We also observed that in COVID-19 patients, there was no significant increase in inflammatory 19-HETE and 20-HETE; however, there was a remarkable change in anti-inflammatory EETs and DHETs profiles (
Table 2). The level of EETs was dramatically increased in COVID-19 patients, whereas the DHETs concentration was repressed. ArA metabolism is a complex process involving several enzymes, including CYP450 enzymes, which play a role in converting ArA into various bioactive metabolites, such as HETEs, EETs, and DHETs. Research on the specific impacts of COVID-19 on ArA metabolites through CYP enzymes is limited; however, it is known that COVID-19 can lead to a dysregulated immune response and excessive inflammation in some individuals. Inflammatory processes, including the production of ArA metabolites, are tightly regulated by various factors, such as cytokines and other inflammatory mediators. It is plausible that COVID-19-induced inflammation could indirectly impact the ArA pathway by altering the expression or activity of enzymes involved in its metabolism, including CYP enzymes. It has been reported that CYP enzyme expression was affected by the excessive inflammatory response due to COVID-19 viral infection [
43]. For example, CYP4A1 and CYP4A2 enzymes convert ArA to HETEs and promote the expression of inflammatory cytokines and adhesion molecules [
44].
Furthermore, the CYP epoxygenase enzyme families of CYP2C and CYP2J generate EETs from ArA, resulting in anti-inflammation, vasodilation, and proangiogenic effects [
45]. Multiple studies demonstrated that both EETs and HETEs play a role in lung and kidney injury [
46,
47,
48]. These reports suggested that the dysregulation of these enzymes may contribute to the inflammatory response observed in COVID-19 patients. In the current study, the observed increase in EETs and decrease in DHETs levels could be attributed to the body’s defense mechanism in resolving the inflammation by up-regulation of CYP epoxygenase enzymes and down-regulation of the sEH. It is possible that other enzymatic mechanisms could also be responsible for this phenomenon, and the proposed claim needs further investigation to be confirmed.
Evidence elucidates that the cross-talk between the RAS and CYP-mediated ArA pathway can significantly affect inflammatory disease manifestations [
18] and explain vascular complications observed in COVID-19 patients. A possible link between ArA metabolites level and ACE enzyme induction has been reported [
49]. Consequently, the elevated 20-HETE level and low EETs plasma concentrations in patients associated with renal and vascular complications were correlated with plasma renin activity [
50]. Additionally, investigation of the association between 20-HETE and the RAS components in rats has shown similar patterns on increased blood pressure and over-expression of CYP4A2 cDNA, which was normalized by the administration of lisinopril, losartan, or a 20-HETE antagonist [
51]. The different results on the ArA metabolites observed in this study could be explained by the activation of AT2R by the high concentration of Ang II in COVID-19 patients. It has been reported that AT2R activation favors EETs production, inhibits pro-inflammatory cytokine intracellular signaling [
52], and probably helps patients to recover from this viral infection. The anti-inflammatory effects of direct AT2R stimulation have been reported using selective peptide [
35] and nonpeptide [
53] AT2R agonists. These anti-inflammatory effects do not counteract Ang II-induced, AT1R-mediated pro-inflammatory actions. AT2R- stimulation antagonizes the effects of TNF-α or other non-RAS stimuli, such as growth factors and has been reported previously [
54,
55,
56]. The Ang II signaling through AT2R activation seems to interfere with other non-RAS signaling cascades coupled with harmful stimuli, and ARBs seem unable to block cytokine-induced IL-6 expression [
57]. AT2R stimulation reduces TNF-α–induced IL-6 expression by activating protein phosphatases, increasing EETs synthesis and inhibiting NF-κB activity [
52]. The observed higher concentration of Ang II in COVID-19 patients due to internalization and inactivation of the ACE 2 could explain the elevated EETs levels and their positive correlation with Ang II levels (
Table 2,
Table 3,
Table 4,
Table 5 and
Table 6). Previous reports on the protective effects of AT2R in other inflammatory conditions support this finding [
58,
59].
Additionally, it has been reported that in an in vitro study, Ang 1–7, through activation of the Mas receptor, increased the release of ArA, which the Mas antagonist abolished. Neither AT1R nor AT2R antagonists could block this effect [
60]. The current study’s results indicate a negative trend of correlations between EETs and Ang 1–7 or Ang 1–7/Ang II in COVID-19 patients is in concert with that report (
Table 3 and
Table 5).
Arachidonic acid is a polyunsaturated fatty acid generated by membrane phospholipids under inflammatory conditions facilitated by PLA2. It has been proposed that ArA possesses antiviral properties and can contribute to the inactivation of enveloped viruses such as SARS-CoV-2 [
61]. ArA can serve as a substrate for various pathways, including cyclooxygenase (COX), lipoxygenase (LOX), and CYP-mediated epoxygenation and hydroxylation pathways, leading to the production of diverse metabolites. These metabolites play a role in regulating inflammation, immune responses, and vascular function. The dysregulation of ArA metabolites has been implicated in multiple diseases, including respiratory disorders. The COX pathway generates pro-inflammatory lipid mediators such as prostaglandins (PGs) and thromboxane (TXA2). The LOX pathway, on the other hand, produces leukotrienes and lipoxins, which exhibit both pro- and anti-inflammatory activities. In contrast to the pro-inflammatory lipid mediators, certain ArA mediators, such as lipoxins, contribute to inflammation resolution and possess potent anti-inflammatory effects [
61]. Among the various PGs, PGE2 has been suggested to play a significant role in COVID-19 pathophysiology by promoting hyperinflammatory and immune responses [
62].
Epoxyeicosatrienoic acids (EETs) and their metabolite, dihydroxyeicosatrienoic acid (DHET), exert various biological effects on the vascular system and interact with other ArA metabolites (e.g., prostanoids) and pathways such as the renin–angiotensin system (RAS). A recent study reported that EETs and prostanoids interact at the receptor level, with EETs antagonizing the actions of vasoconstrictor lipids [
63]. Therefore, the higher levels of EETs, as observed in our study, could be considered the body’s defense mechanism in the fight against COVID-19.
Regarding gender differences, it has been observed that the expression of COX-2 and PGE2 increased more in males compared to females during acute inflammation in humans [
64]. Based on this finding, elevated PGE2 levels in males may contribute to more severe COVID-19 infections in this group [
62]. Considering that COVID-19 patients with comorbidities, including obesity, face a higher risk of disease aggravation, PGE2 could also contribute to the severity of the disease in these patients, as increased PGE2 levels have been reported in obese individuals [
65]. Although the results of this study showed differences in the RAS component and ArA metabolites levels based on age, sex, BMI, and comorbidities, such distinctions did not reach a significant level (
Figure 4 and
Figure 5). The lack of detection of such differences could be related to our study’s limitation on enrolling a small number of patients. It is most likely that such a distinction could be made in more extensive studies.
It has been reported that the SOFA score can be used as a tool in combination with other disease severity scores in predicting mortality in COVID-19 patients [
66]. Our observed association can explain the potential and positive correlation of the SOFA score with Ang II, 19- and total-HETE, indicating that these RAS components and ArA metabolites directly or indirectly impact COVID-19 patients’ organ function.
The evolving landscape of breakthrough infections, variants of concern, and vaccination can have potential implications for the efficacy of the components of the RAS and ArA metabolites as identified biomarkers. Addressing these considerations can enhance the practical impact of the associations between the RAS, ArA metabolites, and these infections. This goal can be achieved by considering the specific variants of concern and their effects on these biomarkers through more extensive studies to establish the associations that can be better contextualized in the evolving landscape. The validation of our findings and understanding of how these biomarkers relate to specific variants or breakthrough cases can help identify individuals at higher risk for severe infection or who may respond differently to particular treatments. This knowledge enhances risk stratification, treatment guidance, and long-term health management strategies, enabling more personalized and practical approaches in the context of the evolving landscape of these infections and vaccination efforts.
Based on the current study’s findings, it may be reasonable to consider the potential use of NSAIDs in the early treatment of COVID-19 when there are no apparent contraindications. However, this issue has been a subject of considerable debate and research [
67,
68,
69]. One factor that sparked interest in using NSAIDs is the imbalance of the RAS in favor of the proinflammatory peptide Ang II in COVID-19 patients, and these anti-inflammatory agents could restore it, as was shown in animal and human studies [
17,
70,
71]. Ang II promotes inflammation and vasoconstriction, and its increased levels have been associated with severe lung injury and acute respiratory distress syndrome in COVID-19 patients. Early treatment with NSAIDs aims to modulate the immune response [
72]. It may impact the pro-inflammatory mediators such as Ang II, ArA metabolites, and cytokine storm triggered by the viral infection, potentially preventing disease progression and the need for hospitalization [
18,
73]. Although ample evidence supports such beneficial effects of NSAIDs on the management of inflammatory conditions, studies have shown that using these agents may have negative or no outcome at all [
68,
69]. However, using NSAIDs with or without other anti-inflammatory drugs may be beneficial in reducing hospitalization and mortality if intervened in the early stage of the viral infection [
74,
75]. To conclusively elucidate the effect of NSAIDs, further extensive clinical trials are required to confirm the same findings in managing COVID-19.
Limitations
One significant limitation of this pilot study was the small number of patients, limiting its potential for generalizability. This study’s findings and conclusions may not apply to a larger population or diverse demographics, as the sample size may not adequately represent the variations and complexities present in the broader population. However, increasing the study’s statistical power by enrolling a larger population could enhance the ability to detect significant correlations accurately, as some trends have already been seen.