Changes in Molar Tipping and Surrounding Alveolar Bone with Different Designs of Skeletal Maxillary Expanders
Abstract
:1. Introduction
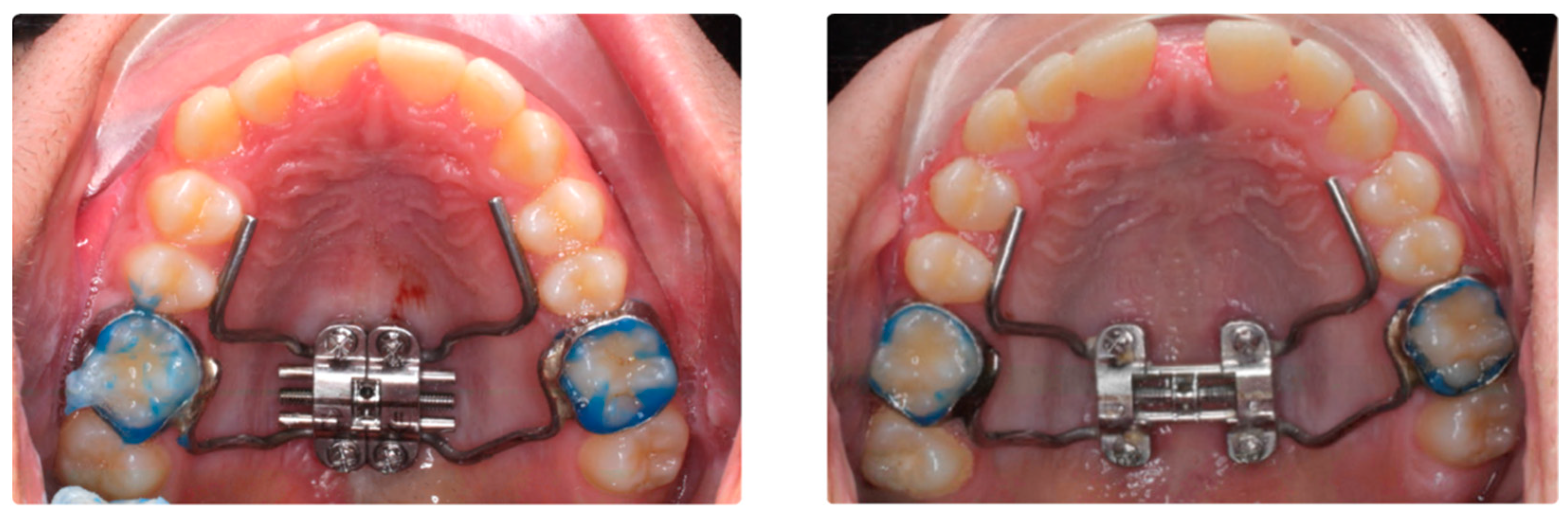
2. Materials and Methods
2.1. Design and Participants
2.2. Digital Procedure and Measurements in the CBCT
2.2.1. CBCT Data Acquisition
2.2.2. CBCT Measurement
2.3. Statistical Analysis
3. Results
3.1. General Descriptive Analysis
3.2. Evaluation of Variables Baseline
3.3. Changes in T1–T0 Bucolingual Angulation of First Molar
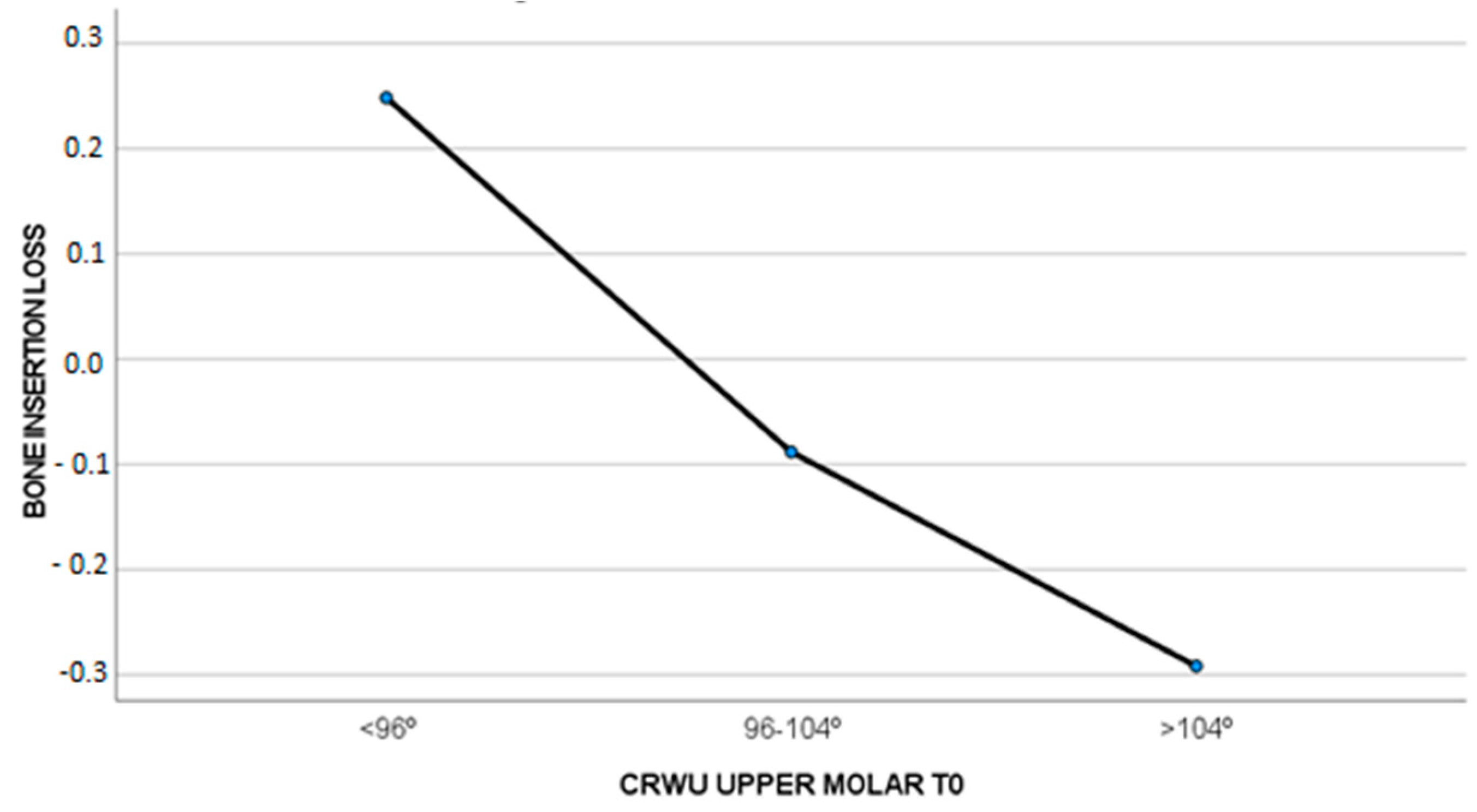
3.4. The Loss of CBI and CBW and Their Relationship with the CWRU at T0
4. Discussion
5. Conclusions
- Patients treated with MARPE show torque increases in the teeth selected to support the expansion appliance compared to cases treated with BAME.
- In cases where the upper molar torque was correct at the beginning of the treatment, a slight bone insertion gain was observed.
- In cases where the upper molar torque was negative or positive, a slight bone insertion loss was observed.
- Regarding the labial cortical bone loss, a slight gain of CBW was observed in all cases. This increase in labial cortical is higher in cases where posterior molar torque was negative before treatment.
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bucci, R.; Montanaro, D.; Rongo, R.; Valletta, R.; Michelotti, A.; D’Antò, V. Effects of maxillary expansion on the upper airways: Evidence from systematic reviews and meta-analyses. J. Oral. Rehabil. 2019, 46, 377–387. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, H.; Moon, W.; Previdente, L.H.; Suzuki, S.S.; Garcez, A.S.; Consolaro, A. Miniscrew-assisted rapid palatal expander (MARPE): The quest for pure orthopedic movement. Dent. Press. J. Orthod. 2016, 21, 17–23. [Google Scholar] [CrossRef] [PubMed]
- Wilmes, B.; Tarraf, N.; Drescher, D. Treatment of maxillary transversal deficiency by using a mini-implant-borne rapid maxillary expander and aligners in combination. Am. J. Orthod. Dentofac. Orthop. 2021, 160, 147–154. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.J.; Park, Y.C.; Park, J.Y.; Hwang, W.S. Miniscrew-assisted nonsurgical palatal expansion before orthognathic surgery for a patient with severe mandibular prognathism. Am. J. Orthod. Dentofac. Orthop. 2010, 137, 830–839. [Google Scholar] [CrossRef]
- Moon, W. An interview with Won Moon. By André Wilson Machado, Barry Briss, Greg J Huang, Richard Kulbersh and Sergei Godeiro Fernandes Rabelo Caldas. Dent. Press. J. Orthod. 2013, 18, 12–28. [Google Scholar]
- Winsauer, H.; Vlachojannis, J.; Winsauer, C.; Ludwig, B.; Walter, A. A bone-borne appliance for rapid maxillary expansion. J. Clin. Orthod. 2013, 47, 375–381. [Google Scholar]
- Garib, D.G.; Henriques, J.F.; Janson, G.; de Freitas, M.R.; Fernandes, A.Y. Periodontal effects of rapid maxillary expansion with tooth-tissue-borne and tooth-borne expanders: A computed tomography evaluation. Am. J. Orthod. Dentofac. Orthop. 2006, 129, 749–758. [Google Scholar] [CrossRef]
- Kim, H.; Park, S.H.; Park, J.H.; Lee, K.J. Nonsurgical maxillary expansion in a 60-year-old patient with gingival recession and crowding. Korean J. Orthod. 2021, 51, 217–227. [Google Scholar] [CrossRef]
- Kapetanović, A.; Theodorou, C.I.; Bergé, S.; Schols, J.G.J.H.; Xi, T. Efficacy of miniscrew-assisted rapid palatal expansion (MARPE) in late adolescents and adults: A systematic review and meta-analysis. Eur. J. Orthod. 2021, 43, 313–323. [Google Scholar] [CrossRef]
- Lagravère, M.O.; Gamble, J.; Major, P.W.; Heo, G. Transverse dental changes after tooth-borne and bone-borne maxillary expansion. Int. Orthod. 2013, 11, 21–34. [Google Scholar] [CrossRef]
- Park, J.J.; Park, Y.C.; Lee, K.J.; Cha, J.Y.; Tahk, J.H.; Choi, Y.J. Skeletal and dentoalveolar changes after miniscrew-assisted rapid palatal expansion in young adults: A cone-beam computed tomography study. Korean J. Orthod. 2017, 47, 77–86. [Google Scholar] [CrossRef] [PubMed]
- Lim, H.M.; Park, Y.C.; Lee, K.J.; Kim, K.H.; Choi, Y.J. Stability of dental, alveolar, and skeletal changes after miniscrew-assisted rapid palatal expansion. Korean J. Orthod. 2017, 47, 313–322. [Google Scholar] [CrossRef] [PubMed]
- Ghoneima, A.; Abdel-Fattah, E.; Hartsfield, J.; El-Bedwehi, A.; Kamel, A.; Kula, K. Effects of rapid maxillary expansion on the craial and circummaxillary sutures. Am. J. Orthod. Dentofac. Orthop. 2011, 140, 510–519. [Google Scholar] [CrossRef]
- Cantarella, D.; Dominguez-Mompell, R.; Moschik, C.; Sfogliano, L.; Elkenawy, I.; Pan, H.C.; Mallya, S.M.; Moon, W. Zygomaticomaxillary modifications in the horizontal plane induced by micro-implant-supported skeletal expander, analyzed with CBCT images. Prog. Orthod. 2018, 19, 1–8. [Google Scholar] [CrossRef]
- Lee, S.C.; Park, J.H.; Bayome, M.; Kim, K.B.; Araujo, E.A.; Kook, Y.A. Effect of bone-borne rapid maxillary expanders with and without surgical assistance on the craniofacial structures using finite element analysis. Am. J. Orthod. Dentofac. Orthop. 2014, 145, 638–648. [Google Scholar] [CrossRef]
- Hayes, J. A Clinical Approach to Identify Transverse Discrepancies. In Proceedings of the Pennsylvania Association of Orthodontists, Philadelphia, PA, USA, 8 March 2003. [Google Scholar]
- Tamburrino, R.K.; Boucher, N.S.; Vanarsdall, R.L.; Secchi, A. The transverse dimension: Diagnosis and relevance to functional occlusion. RWISO J. 2010, 13–22. [Google Scholar]
- Gioka, C.; Eliades, T. Materials-induced variation in the torque expression of preadjusted appliances. Am. J. Orthod. Dentofac. Orthop. 2004, 125, 323–328. [Google Scholar] [CrossRef] [PubMed]
- Mestriner, M.A.; Enoki, C.; Mucha, J.N. Normal torque of the buccal surface of mandibular teeth and its relationship with bracket positioning: A study in normal occlusion. Braz. Dent. J. 2006, 17, 155–160. [Google Scholar] [CrossRef]
- McLaughlin, R.P.; Bennett, J.C. Finishing with the preadjusted orthodontic appliance. Semin. Orthod. 2003, 9, 165–183. [Google Scholar] [CrossRef]
- Lucchese, A.; Manuelli, M.; Albertini, P.; Ghislanzoni, L.H. Transverse and torque dental changes after passive self-ligating fixed therapy: A two-year follow-up study. Am. J. Orthod. Dentofac. Orthop. 2019, 156, 94–103. [Google Scholar] [CrossRef]
- Goh, S.; Dreyer, C.; Weir, T. The predictability of the mandibular curve of Wilson, buccolingual crown inclination, and transverse expansion expression with Invisalign treatment. Am. J. Orthod. Dentofac. Orthop. 2023, 163, 109–116. [Google Scholar] [CrossRef] [PubMed]
- Canan, S.; Şenışık, N.E. Comparison of the treatment effects of different rapid maxillary expansion devices on the maxilla and the mandible. Part 1: Evaluation of dentoalveolar changes. Am. J. Orthod. Dentofac. Orthop. 2017, 151, 1125–1138. [Google Scholar] [CrossRef]
- Moon, H.W.; Kim, M.J.; Ahn, H.W.; Kim, S.J.; Kim, S.H.; Chung, K.R.; Nelson, G. Molar inclination and surrounding alveolar bone change relative to the design of bone-borne maxillary expanders: A CBCT study. Angle Orthod. 2020, 90, 13–22. [Google Scholar] [CrossRef]
- Bazzani, M.; Cevidanes, L.H.S.; al Turkestani, N.N.; Annarumma, F.; McMullen, C.; Ruellas, A.C.O.; Massaro, C.; Rego, M.V.N.N.; Yatabe, M.S.; Kim-Berman, H.; et al. Three-dimensional comparison of bone-borne and tooth-bone-borne maxillary expansion in young adults with maxillary skeletal deficiency. Orthod. Craniofac Res. 2022, 26, 151–162. [Google Scholar] [CrossRef] [PubMed]
- Ronsivalle, V.; Venezia, P.; Bennici, O.; D’Antò, V.; Giudice, A. Accuracy of digital workfloe for placing orthodontic miniscrews using generic and licensed open systems. A 3d imaging analysis of non-native.stl files for guided protocols. BMC Oral Health 2023, 494, 23. [Google Scholar]
- Shewinvanakitkul, W. A New Method to Measure Buccolingual Inclination Using Cbct. Master’s Thesis, Case Western Reserve University, Cleveland, OH, USA, 2009. [Google Scholar]
- Yehya Mostafa, R.; Bous, R.M.; Hans, M.G.; Valiathan, M.; Copeland, G.E.; Palomo, J.M. Effects of Case Western Reserve University’s transverse analysis on the quality of orthodontic treatment. Am. J. Orthod. Dentofac. Orthop. 2019, 152, 178–192, Erratum in: Am. J. Orthod. Dentofac. Orthop. 2019, 155, 618. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Lawrence Erlbaum Associates: Hillsdale, NJ, USA, 1988. [Google Scholar]
- Evangelinakis, N. Changes in Buccolingual Inclination of Mandibular Canines and First Molars after Orthodontic Treatment using CBCT. Ph.D. Thesis, Case Western Reserve University, Cleveland, OH, USA, 2010. [Google Scholar]
- Shewinvanakitkul, W.; Hans, M.G.; Narendran, S.; Martin Palomo, J. Measuring Buccolingual Inclination of Mandibular Canines and First Molars using CBCT. Orthod. Craniofac Res. 2011, 14, 168–174. [Google Scholar] [CrossRef] [PubMed]
- Karamitsou, E. Pretreatment Buccolingual Inclination of Maxillary Canines and First Molars. Master’s Thesis, Case Western Reserve University, Cleveland, OH, USA, 2011. [Google Scholar]
- Miyamoto, M.J. Changes in Buccolingual Inclination of Maxillary Canines and First Molars after Orthodontic Treatment Using CBCT. Ph.D. Thesis, Case Western Reserve University, Cleveland, OH, USA, 2011. [Google Scholar]
- Copeland, G. Case Western Reserve University Transverse Analysis: Clinical Application. Ph.D. Thesis, Case Western Reserve University, Cleveland, OH, USA, 2012. [Google Scholar]
- Streit, L. Case Western Reserve University Transverse Analysis—Developing Norms. Ph.D. Thesis, Case Western Reserve University, Cleveland, OH, USA, 2012. [Google Scholar]
- Palomo, J.M.; Valiathan, M.; Hans, G.M. 3D Orthodontic Diagnosis and Treatment Planning. In Cone Beam Computed Tomography in Orthodontics: Indications, Insights, and Innovations; Kapila, S.D., Ed.; John Wiley & Sons Inc.: Ames, IA, USA; Hoboken, NJ, USA, 2014; pp. 221–246. [Google Scholar]
- Gunyuz Toklu, M.; Germec-Cakan, D.; Tozlu, M. Periodontal, dentoalveolar, and skeletal effects of tooth-borne and tooth-bone-borne expansion appliances. Am. J. Orthod. Dentofac. Orthop. 2015, 148, 97–109. [Google Scholar] [CrossRef]
- Jia, H.; Zhuang, L.; Zhang, N.; Bian, Y.; Li, S. Comparison of skeletal maxillary transverse deficiency treated by microimplant-assisted rapid palatal expansion and tooth-borne expansion during the post-pubertal growth spurt stage: A prospective cone beam computed tomography study. Angle Orthod. 2021, 91, 36–45. [Google Scholar] [CrossRef]
- De Oliveira, C.B.; Ayub, P.; Ledra, I.M.; Murata, W.H.; Suzuki, S.S.; Ravelli, D.B.; Santos-Pinto, A. Microimplant assisted rapid palatal expansion vs surgically assisted rapid palatal expansion for maxillary transverse discrepancy treatment. Am. J. Orthod. Dentofac. Orthop. 2021, 159, 733–742. [Google Scholar] [CrossRef]
- Khosravi, M.; Ugolini, A.; Miresmaeili, A.; Mirzaei, H.; Shahidi-Zandi, V.; Soheilifar, S.; Karami, M.; Mahmoudzadeh, M. Tooth-borne versus bone-borne rapid maxillary expansion for transverse maxillary deficiency: A systematic review. Int. Orthod. 2019, 17, 425–436. [Google Scholar] [CrossRef] [PubMed]
- Baysal, A.; Uysal, T.; Veli, I.; Ozer, T.; Karadede, I.; Hekimoglu, S. Evaluation of alveolar bone loss following rapid maxillary expansion using cone-beam computed tomography. Korean J. Orthod. 2013, 43, 83–95. [Google Scholar] [CrossRef] [PubMed]
- Leonardi, R.; Ronsivalle, V.; Barbato, E.; Lagravère, M.; Flores-Mir, C.; Lo Giudice, A. External root resorption (ERR) and rapid maxillary expansion (RME) at post-retention stage: A comparison between tooth-borne and bone-borne RME. Prog. Orthod. 2022, 23, 1–9. [Google Scholar] [CrossRef]
- Leonardi, R.; Ronsisvalle, V.; Isola, G.; Cicciù, M.; Lagravère, M.; Flores-Mir, C.; Lo Giudice, A. External root resorption and rapid maxillary expansion in the short-term: A CBCT comparative study between tooth-borne and bone-borne appliances, using 3D imaging digital technology. BMC Oral. Health 2023, 558, 23. [Google Scholar] [CrossRef] [PubMed]

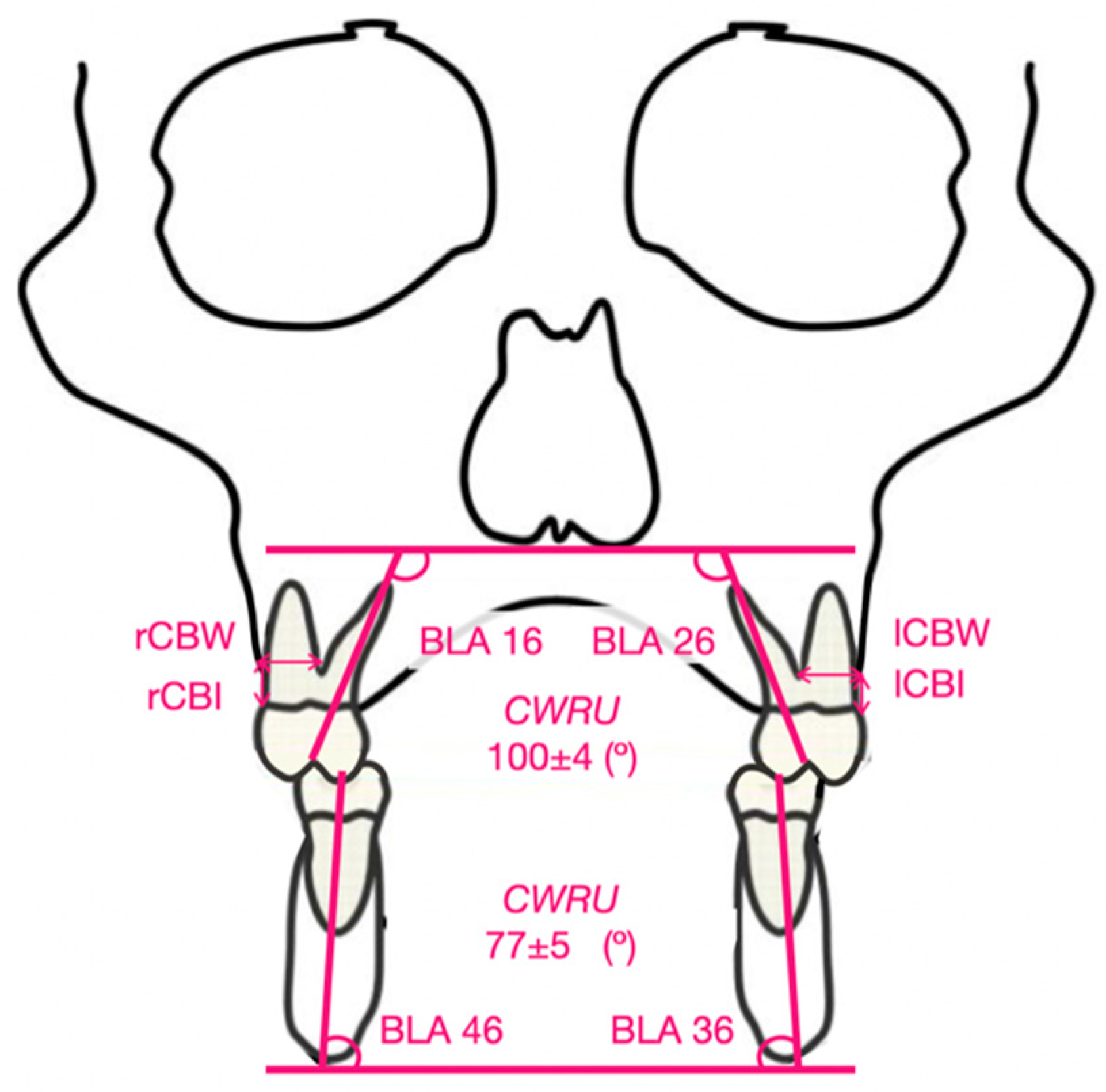

| Measurements | Description |
|---|---|
| Bucolingual angulation of the first right upper molar (BLA 16) | Angle between the line passing through the palatal cusp and the root apex of the palatal root of the right upper first molar and the tangent line to the floor of the nostrils. |
| Bucolingual angulation of the first left upper molar (BLA 26) | Angle between the line passing through the palatal cusp and the root apex of the palatal root of the left upper first molar and the line tangent to the floor of the nostrils. |
| Bucolingual angulation of the first left lower molar (BLA 36) | Angle between the line passing through the central fossa and the root apex of the lingual root of the first right lower molar and the line tangent to the lower edge of the mandibular corpus. |
| Bucolingual angulation of the first right lower molar (BLA 46) | Angle between the line passing through the central fossa and the root apex of the lingual root of the first lower left molar and the line tangent to the lower edge of the mandibular body. |
| Cortical bone insertion (CBI) | Labial cortical bone insertion with respect to the cementoenamel junction of the upper first molars |
| Cortical bone width (CBW) | Labial cortical bone thickness. The distance from the furca of the upper first molars to the most external point of the labial cortical bone was taken. |
| ICC | ME | |
|---|---|---|
| BLA 16 | 0.972 | 0.26° ± 0.56 |
| BLA 26 | 0.912 | 0.19° ± 0.42 |
| BLA 36 | 0.998 | 0.37° ± 0.67 |
| BLA 46 | 0.986 | 0.25° ± 0.55 |
| MARPE T0 M (SD) | MARPE T1 M (SD) | MARPE T1–T0 M (SD) | p Value T1–T0 | |
|---|---|---|---|---|
| BLA 16 (°) | 99.52 (7.35) | 103.94 (8.02) | 4.42 (10.25) | 0.085 |
| BLA 26 (°) | 97.47 (7.89) | 101.14 (7.69) | 3.67 (9.56) | 0.122 |
| BLA 36 (°) | 76.01 (5.50) | 77.26 (5.95) | 1.02 (4.21) | 0.222 |
| BLA 46 (°) | 76.46 (8.13) | 77.58 (6.93) | 1.12 (6.04) | 0.440 |
| BAME T0 | BAME T1 | BAME T1–T0 | p value T1–T0 | |
| BLA 16 (°) | 101.44 (5.88) | 100.93 (8.82) | − 0.51 (4.61) | 0.644 |
| BLA 26 (°) | 102.88 (10.16) | 105.22 (8.75) | 2.34 (4.51) | 0.042 * |
| BLA 36 (°) | 77.06(5.81) | 75.96 (6.41)) | − 1.10 (6.71) | 0.496 |
| BLA 46 (°) | 77.57(7.61) | 78.36 (6.51) | 0.79 (4.17) | 0.434 |
| MARPE T1–T0 | BAME T1–T0 | p Value | Cohen’s d | |
|---|---|---|---|---|
| BLA 16 (°) | 4.42 (10.25) | − 0.51 (4.61) | 0.071 | 0.620 |
| BLA 26 (°) | 3.67 (9.56) | 2.34 (4.51) | 0.594 | 0.177 |
| BLA 36 (°) | 1.02 (4.21) | − 1.10 (6.71) | 0.274 | 0.378 |
| BLA 46 (°) | 1.12 (6.04) | 0.79 (4.17) | 0.847 | 0.063 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Echarri-Nicolás, J.; González-Olmo, M.J.; Echarri-Labiondo, P.; Romero, M. Changes in Molar Tipping and Surrounding Alveolar Bone with Different Designs of Skeletal Maxillary Expanders. Biomedicines 2023, 11, 2380. https://doi.org/10.3390/biomedicines11092380
Echarri-Nicolás J, González-Olmo MJ, Echarri-Labiondo P, Romero M. Changes in Molar Tipping and Surrounding Alveolar Bone with Different Designs of Skeletal Maxillary Expanders. Biomedicines. 2023; 11(9):2380. https://doi.org/10.3390/biomedicines11092380
Chicago/Turabian StyleEcharri-Nicolás, Javier, María José González-Olmo, Pablo Echarri-Labiondo, and Martín Romero. 2023. "Changes in Molar Tipping and Surrounding Alveolar Bone with Different Designs of Skeletal Maxillary Expanders" Biomedicines 11, no. 9: 2380. https://doi.org/10.3390/biomedicines11092380
APA StyleEcharri-Nicolás, J., González-Olmo, M. J., Echarri-Labiondo, P., & Romero, M. (2023). Changes in Molar Tipping and Surrounding Alveolar Bone with Different Designs of Skeletal Maxillary Expanders. Biomedicines, 11(9), 2380. https://doi.org/10.3390/biomedicines11092380






