Rehabilitation: Neurogenic Bone Loss after Spinal Cord Injury
Abstract
:1. Introduction
2. Pathophysiology of Bone Loss after SCI
3. Disuse and Bone Loss after SCI
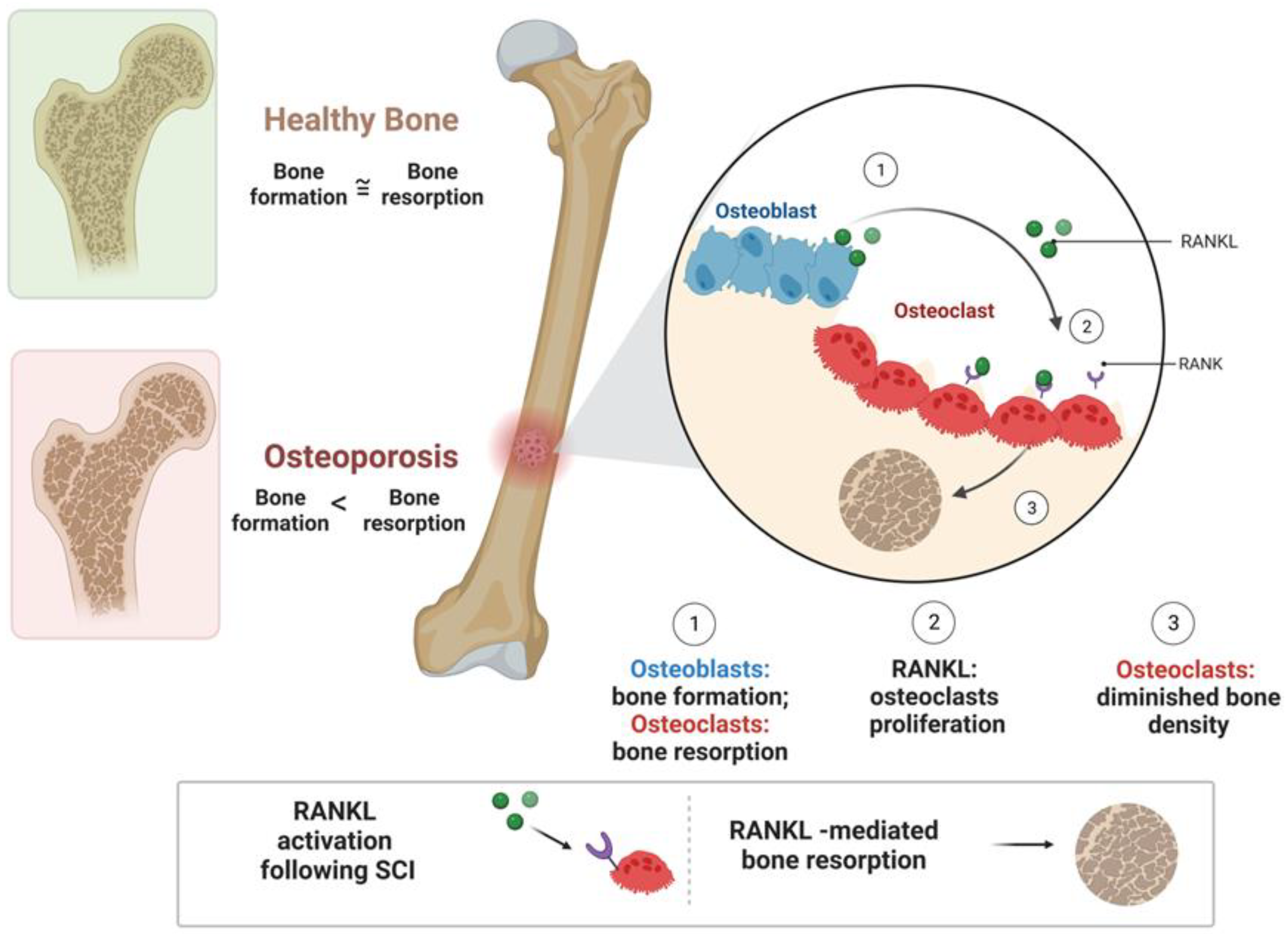
4. Risk Factors in SCI Individuals
5. Cellular and Molecular Events following SCI
5.1. 4-1BB Signaling after Acute SCI
5.2. RANKL Signaling after SCI
5.3. Wnt Signaling after SCI
6. Calcium-Regulated Hormones in Bone Loss after SCI
7. Bone Density and Fractures after SCI
8. Therapeutic Strategies for Neurogenic Bone Loss after SCI
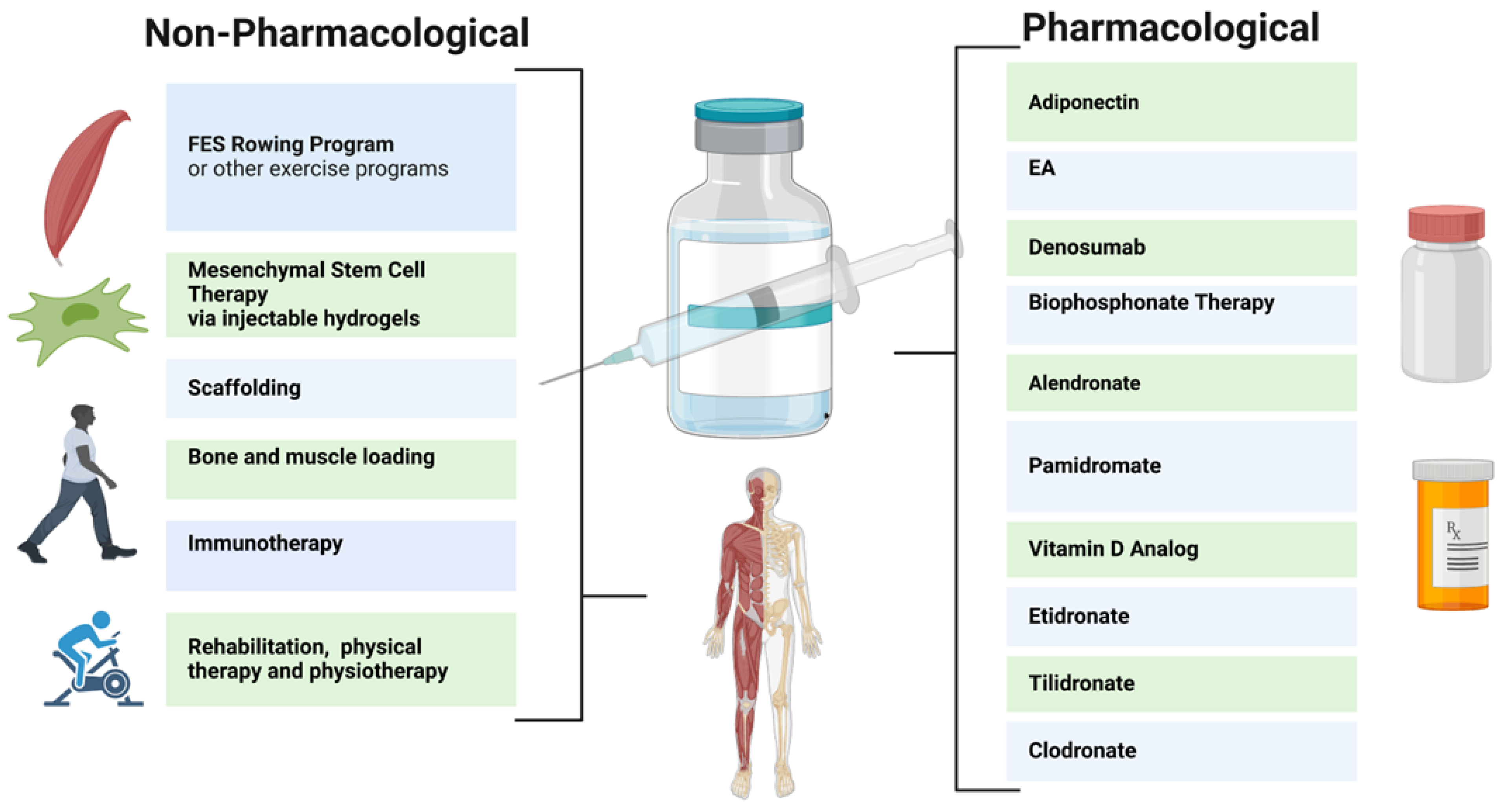
8.1. Pharmacological Therapy
8.2. Nonpharmacological Therapy
9. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Alizadeh, A.; Dyck, S.M.; Karimi-Abdolrezaee, S. Traumatic spinal cord injury: An overview of pathophysiology, models and acute injury mechanisms. Front. Neurol. 2019, 10, 282. [Google Scholar] [CrossRef]
- Ahuja, C.S.; Wilson, J.R.; Nori, S.; Kotter, M.; Druschel, C.; Curt, A.; Fehlings, M.G. Traumatic spinal cord injury. Nat. Rev. Dis. Primers 2017, 3, 17018. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Tang, Y.; Vogel, L.; DeVivo, M. Causes of spinal cord injury. Top. Spinal Cord Inj. Rehabil. 2013, 19, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Shams, R.; Drasites, K.P.; Zaman, V.; Matzelle, D.; Shields, D.C.; Garner, D.P.; Sole, C.J.; Haque, A.; Banik, N.L. The Pathophysiology of Osteoporosis after Spinal Cord Injury. Int. J. Mol. Sci. 2021, 22, 3057. [Google Scholar] [CrossRef]
- Chen, L.W.; Glinsky, J.V.; Islam, S.; Hossain, M.; Boswell-Ruys, C.L.; Kataria, C.; Redhead, J.; Xiong, Y.; Gollan, E.; Costa, P.D.; et al. The effects of 10,000 voluntary contractions over 8 weeks on the strength of very weak muscles in people with spinal cord injury: A randomised controlled trial. Spinal Cord 2020, 58, 857–864. [Google Scholar] [CrossRef]
- Fouad, K.; Popovich, P.G.; Kopp, M.A.; Schwab, J.M. The neuroanatomical–functional paradox in spinal cord injury. Nat. Rev. Neurol. 2021, 17, 53–62. [Google Scholar] [CrossRef]
- Zhu, S.; Bennett, S.; Kuek, V.; Xiang, C.; Xu, H.; Rosen, V.; Xu, J. Endothelial cells produce angiocrine factors to regulate bone and cartilage via versatile mechanisms. Theranostics 2020, 10, 5957–5965. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez, G.; Berri, M.; Lin, P.; Kamdar, N.; Mahmoudi, E.; Peterson, M.D. Musculoskeletal morbidity following spinal cord injury: A longitudinal cohort study of privately-insured beneficiaries. Bone 2021, 142, 115700. [Google Scholar] [CrossRef]
- Wang, S.; Deng, J.; Fu, H.; Guo, Z.; Zhang, L.; Tang, P. Astrocytes directly clear myelin debris through endocytosis pathways and followed by excessive gliosis after spinal cord injury. Biochem. Biophys. Res. Commun. 2020, 525, 20–26. [Google Scholar] [CrossRef]
- Yang, T.; Dai, Y.; Chen, G.; Cui, S. Dissecting the Dual Role of the Glial Scar and Scar-Forming Astrocytes in Spinal Cord Injury. Front. Cell. Neurosci. 2020, 14, 78. [Google Scholar] [CrossRef]
- Lin, C.-Y.; Androjna, C.; Rozic, R.; Nguyen, B.T.; Parsons, B.; Midura, R.J.; Lee, Y.-S. Differential Adaptations of the Musculoskeletal System after Spinal Cord Contusion and Transection in Rats. J. Neurotrauma 2018, 35, 1737–1744. [Google Scholar] [CrossRef] [PubMed]
- Marini, S.; Barone, G.; Masini, A.; Dallolio, L.; Bragonzoni, L.; Longobucco, Y.; Maffei, F. The Effect of Physical Activity on Bone Biomarkers in People with Osteoporosis: A Systematic Review. Front. Endocrinol. 2020, 11, 585689. [Google Scholar] [CrossRef] [PubMed]
- Craven, B.C.; Cirnigliaro, C.M.; Carbone, L.D.; Tsang, P.; Morse, L.R. The Pathophysiology, Identification and Management of Fracture Risk, Sublesional Osteoporosis and Fracture among Adults with Spinal Cord Injury. J. Pers. Med. 2023, 13, 966. [Google Scholar] [CrossRef] [PubMed]
- Varacallo, M.; Davis, D.D.; Pizzutillo, P. Osteoporosis in Spinal Cord Injuries. In StatPearls; Ineligible Companies: Treasure Island, FL, USA, 2023. [Google Scholar]
- Edwards, W.B.; Schnitzer, T.J. Bone Imaging and Fracture Risk after Spinal Cord Injury. Curr. Osteoporos. Rep. 2015, 13, 310–317. [Google Scholar] [CrossRef] [PubMed]
- Maïmoun, L.; Gelis, A.; Serrand, C.; Mura, T.; Humbert, L.; Boudousq, V.; de Santa-Barbara, P.; Laux, D.; Fattal, C.; Mariano-Goulart, D. Alteration of Volumetric Bone Mineral Density Parameters in Men with Spinal Cord Injury. Calcif. Tissue Int. 2023, 113, 304–316. [Google Scholar] [CrossRef]
- Cirnigliaro, C.M.; La Fountaine, M.F.; Parrott, J.S.; Kirshblum, S.C.; Sauer, S.J.; Shapses, S.A.; McClure, I.A.; Bauman, W.A. Loss of lower extremity bone mineral density 1 year after denosumab is discontinued in persons with subacute spinal cord injury. Osteoporos. Int. 2023, 34, 741–748. [Google Scholar] [CrossRef]
- Zhang, L.; Yin, Y.; Guo, J.; Jin, L.; Hou, Z. Chronic intermittent hypobaric hypoxia ameliorates osteoporosis after spinal cord injury through balancing osteoblast and osteoclast activities in rats. Front. Endocrinol. 2023, 14, 1035186. [Google Scholar] [CrossRef]
- Ishimoto, R.; Mutsuzaki, H.; Shimizu, Y.; Kishimoto, H.; Takeuchi, R.; Hada, Y. Prevalence of Sarcopenic Obesity and Factors Influencing Body Composition in Persons with Spinal Cord Injury in Japan. Nutrients 2023, 15, 473. [Google Scholar] [CrossRef]
- Bitra, A.; Doukov, T.; Croft, M.; Zajonc, D.M. Crystal structures of the human 4-1BB receptor bound to its ligand 4-1BBL reveal covalent receptor dimerization as a potential signaling amplifier. J. Biol. Chem. 2018, 293, 9958–9969. [Google Scholar] [CrossRef]
- Wan, D.; Ai, S.; Ouyang, H.; Cheng, L. Activation of 4-1BB signaling in bone marrow stromal cells triggers bone loss via the p-38 MAPK-DKK1 axis in aged mice. Exp. Mol. Med. 2021, 53, 654–666. [Google Scholar] [CrossRef]
- Cheng, P.; Liao, H.-Y.; Zhang, H.-H. The role of Wnt/mTOR signaling in spinal cord injury. J. Clin. Orthop. Trauma 2022, 25, 101760. [Google Scholar] [CrossRef]
- Liu, J.; Xiao, Q.; Xiao, J.; Niu, C.; Li, Y.; Zhang, X.; Zhou, Z.; Shu, G.; Yin, G. Wnt/beta-catenin signalling: Function, biological mechanisms, and therapeutic opportunities. Signal Transduct. Target. Ther. 2022, 7, 3. [Google Scholar] [CrossRef] [PubMed]
- Gifre, L.; Vidal, J.; Carrasco, J.L.; Filella, X.; Ruiz-Gaspà, S.; Muxi, A.; Portell, E.; Monegal, A.; Guañabens, N.; Peris, P. Effect of Recent Spinal Cord Injury on Wnt Signaling Antagonists (Sclerostin and Dkk-1) and Their Relationship with Bone Loss. A 12-Month Prospective Study. J. Bone Miner. Res. 2015, 30, 1014–1021. [Google Scholar] [CrossRef]
- Sutor, T.W.; Kura, J.; Mattingly, A.J.; Otzel, D.M.; Yarrow, J.F. The Effects of Exercise and Activity-Based Physical Therapy on Bone after Spinal Cord Injury. Int. J. Mol. Sci. 2022, 23, 608. [Google Scholar] [CrossRef] [PubMed]
- Yarrow, J.F.; Wnek, R.D.; Conover, C.F.; Reynolds, M.C.; Buckley, K.H.; Kura, J.R.; Sutor, T.W.; Otzel, D.M.; Mattingly, A.J.; Croft, S.; et al. Bone loss after severe spinal cord injury coincides with reduced bone formation and precedes bone blood flow deficits. J. Appl. Physiol. 2021, 131, 1288–1299. [Google Scholar] [CrossRef] [PubMed]
- Morse, L.; Teng, Y.D.; Pham, L.; Newton, K.; Yu, D.; Liao, W.-L.; Kohler, T.; Müller, R.; Graves, D.; Stashenko, P.; et al. Spinal cord injury causes rapid osteoclastic resorption and growth plate abnormalities in growing rats (SCI-induced bone loss in growing rats). Osteoporos. Int. 2008, 19, 645–652. [Google Scholar] [CrossRef]
- Le, B.; Ray, C.; Gonzalez, B.; Miskevics, S.; Weaver, F.M.; Priebe, M.; Carbone, L.D. Laboratory evaluation of secondary causes of bone loss in Veterans with spinal cord injury and disorders. Osteoporos. Int. 2019, 30, 2241–2248. [Google Scholar] [CrossRef]
- Ma, Z.; Ma, M.; He, Y.; Sun, H.; Yang, B.; Dong, H.; Wang, Y. Bisphosphonates Alleviate Bone Loss in People with Acute Spinal Cord Injury: A Systematic Review and Meta-Analysis. World Neurosurg. 2023, 170, e584–e595. [Google Scholar] [CrossRef]
- Ducher, G.; Courteix, D.; Même, S.; Magni, C.; Viala, J.; Benhamou, C. Bone geometry in response to long-term tennis playing and its relationship with muscle volume: A quantitative magnetic resonance imaging study in tennis players. Bone 2005, 37, 457–466. [Google Scholar] [CrossRef]
- Zhu, S.; Chen, M.; Ying, Y.; Wu, Q.; Huang, Z.; Ni, W.; Wang, X.; Xu, H.; Bennett, S.; Xiao, J.; et al. Versatile subtypes of pericytes and their roles in spinal cord injury repair, bone development and repair. Bone Res. 2022, 10, 30. [Google Scholar] [CrossRef]
- Zheng, X.; Qi, Y.; Zhou, H.; Kang, H.; Tong, Y.; Bi, L. Bone Mineral Density at the Distal Femur and Proximal Tibia and Related Factors During the First Year of Spinal Cord Injury. Int. J. Gen. Med. 2021, 14, 1121–1129. [Google Scholar] [CrossRef] [PubMed]
- Alexandre, C.; Vico, L. Pathophysiology of bone loss in disuse osteoporosis. Jt. Bone Spine 2011, 78, 572–576. [Google Scholar] [CrossRef] [PubMed]
- Tan, C.O.; Battaglino, R.A.; Doherty, A.L.; Gupta, R.; Lazzari, A.A.; Garshick, E.; Zafonte, R.; Morse, L.R. Adiponectin is associated with bone strength and fracture history in paralyzed men with spinal cord injury. Osteoporos. Int. 2014, 25, 2599–2607. [Google Scholar] [CrossRef] [PubMed]
- Williams, J.A.; Huesa, C.; Turunen, M.J.; Oo, J.A.; Radzins, O.; Gardner, W.; Windmill, J.F.C.; Isaksson, H.; Tanner, K.E.; Riddell, J.S.; et al. Time course changes to structural, mechanical and material properties of bone in rats after complete spinal cord injury. J. Musculoskelet. Neuronal Interact. 2022, 22, 212–234. [Google Scholar]
- Jackson, A.B.; Dijkers, M.; DeVivo, M.J.; Poczatek, R.B. A demographic profile of new traumatic spinal cord injuries: Change and stability over 30 years. Arch. Phys. Med. Rehabil. 2004, 85, 1740–1748. [Google Scholar] [CrossRef]
- Dharnipragada, R.; Ahiarakwe, U.; Gupta, R.; Abdilahi, A.; Butterfield, J.; Naik, A.; Parr, A.; Morse, L.R. Pharmacologic and Nonpharmacologic Treatment Modalities for Bone Loss in SCI—Proposal for Combined Approach. J. Clin. Densitom. 2023, 26, 101359. [Google Scholar] [CrossRef]
- Babaie, M.; Joulani, M.; Hameghavandi, M.H.R.; Asgardoon, M.H.; Nojomi, M.; O'Reilly, G.M.; Gholami, M.; Ghodsi, Z.; Rahimi-Movaghar, V. Risk of permanent medical impairment after road traffic crashes: A systematic review. Chin. J. Traumatol. 2022, 22, 115–118. [Google Scholar] [CrossRef]
- Spinal cord injury facts and figures at a glance. J. Spinal Cord Med. 2013, 36, 170–171. [CrossRef]
- Gifre, L.; Vidal, J.; Carrasco, J.L.; Muxi, A.; Portell, E.; Monegal, A.; Guañabens, N.; Peris, P. Risk factors for the development of osteoporosis after spinal cord injury. A 12-month follow-up study. Osteoporos. Int. 2015, 26, 2273–2280. [Google Scholar] [CrossRef]
- New, P.W.; Simmonds, F.; Stevermuer, T. A population-based study comparing traumatic spinal cord injury and non-traumatic spinal cord injury using a national rehabilitation database. Spinal Cord 2011, 49, 397–403. [Google Scholar] [CrossRef]
- Dalle, D.U.; Sriram, S.; Bandyopadhyay, S.; Egiz, A.; Kotecha, J.; Kanmounye, U.S.; Higginbotham, G.; Ooi, S.Z.Y.; Bankole, N.D.A. Management and Outcomes of Traumatic Pediatric Spinal Cord Injuries in Low- and Middle-Income Countries: A Scoping Review. World Neurosurg. 2022, 165, 180–187. [Google Scholar] [CrossRef] [PubMed]
- Chiu, W.-T.; Lin, H.-C.; Lam, C.; Chu, S.-F.; Chiang, Y.-H.; Tsai, S.-H. Review Paper: Epidemiology of Traumatic Spinal Cord Injury: Comparisons Between Developed and Developing Countries. Asia Pac. J. Public Health. 2010, 22, 9–18. [Google Scholar] [CrossRef] [PubMed]
- Ashe, M.; Craven, C.; Eng, J.; Krassioukov, A. Prevention and Treatment of Bone Loss After a Spinal Cord Injury: A Systematic Review. Top. Spinal Cord Inj. Rehabil. 2007, 13, 123–145. [Google Scholar] [CrossRef]
- Alazzam, A.M.; Goldsmith, J.A.; Khalil, R.E.; Khan, M.R.; Gorgey, A.S. Denervation impacts muscle quality and knee bone mineral density after spinal cord injury. Spinal Cord 2023, 61, 276–284. [Google Scholar] [CrossRef]
- Morse, L.R.; Battaglino, R.A.; Stolzmann, K.L.; Hallett, L.D.; Waddimba, A.; Gagnon, D.; Lazzari, A.A.; Garshick, E. Osteoporotic fractures and hospitalization risk in chronic spinal cord injury. Osteoporos. Int. 2009, 20, 385–392. [Google Scholar] [CrossRef] [PubMed]
- Ibarra, A.; Alcántar-Garibay, O.; Incontri-Abraham, D. Spinal cord injury-induced cognitive impairment: A narrative review. Neural Regen. Res. 2022, 17, 2649–2654. [Google Scholar] [CrossRef]
- Drenkard, D.; Becke, F.M.; Langstein, J.; Spruss, T.; Kunz-Schughart, L.A.; Tan, T.E.; Lim, Y.C.; Schwarz, H. CD137 is expressed on blood vessel walls at sites of inflammation and enhances monocyte migratory activity. FASEB J. 2006, 21, 456–463. [Google Scholar] [CrossRef]
- Reali, C.; Curto, M.; Sogos, V.; Scintu, F.; Pauly, S.; Schwarz, H.; Gremo, F. Expression of CD137 and its ligand in human neurons, astrocytes, and microglia: Modulation by FGF-2. J. Neurosci. Res. 2003, 74, 67–73. [Google Scholar] [CrossRef]
- Kim, C.-S.; Kim, J.G.; Lee, B.-J.; Choi, M.-S.; Choi, H.-S.; Kawada, T.; Lee, K.-U.; Yu, R. Deficiency for Costimulatory Receptor 4-1BB Protects Against Obesity-Induced Inflammation and Metabolic Disorders. Diabetes 2011, 60, 3159–3168. [Google Scholar] [CrossRef]
- Shao, Z.; Schwarz, H. CD137 ligand, a member of the tumor necrosis factor family, regulates immune responses via reverse signal transduction. J. Leukoc. Biol. 2011, 89, 21–29. [Google Scholar] [CrossRef]
- Tu, T.H.; Kim, C.-S.; Goto, T.; Kawada, T.; Kim, B.-S.; Yu, R. 4-1BB/4-1BBL Interaction Promotes Obesity-Induced Adipose Inflammation by Triggering Bidirectional Inflammatory Signaling in Adipocytes/Macrophages. Mediat. Inflamm. 2012, 2012, 972629. [Google Scholar] [CrossRef]
- Saito, K.; Ohara, N.; Hotokezaka, H.; Fukumoto, S.; Yuasa, K.; Naito, M.; Fujiwara, T.; Nakayama, K. Infection-induced Up-regulation of the Costimulatory Molecule 4-1BB in Osteoblastic Cells and Its Inhibitory Effect on M-CSF/RANKL-induced in Vitro Osteoclastogenesis. J. Biol. Chem. 2004, 279, 13555–13563. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Park, O.J.; Lee, Y.J.; Jung, H.-M.; Woo, K.M.; Choi, Y. The 4-1BB ligand and 4-1BB expressed on osteoclast precursors enhance RANKL-induced osteoclastogenesis via bi-directional signaling. Eur. J. Immunol. 2008, 38, 1598–1609. [Google Scholar] [CrossRef] [PubMed]
- Wakley, A.A.; Leeming, R.; Malon, J.; Arabatzis, T.J.; Koh, W.Y.; Cao, L. Contribution of CD137L to Sensory Hypersensitivity in a Murine Model of Neuropathic Pain. eNeuro 2018, 5, 218. [Google Scholar] [CrossRef] [PubMed]
- Sanchez-Paulete, A.R.; Labiano, S.; Rodriguez-Ruiz, M.E.; Azpilikueta, A.; Etxeberria, I.; Bolaños, E.; Lang, V.; Rodriguez, M.; Aznar, M.A.; Jure-Kunkel, M.; et al. Deciphering CD137 (4-1BB) signaling in T-cell costimulation for translation into successful cancer immunotherapy. Eur. J. Immunol. 2016, 46, 513–522. [Google Scholar] [CrossRef]
- Sun, L.; Pan, J.; Peng, Y.; Wu, Y.; Li, J.; Liu, X.; Qin, Y.; Bauman, W.A.; Cardozo, C.; Zaidi, M.; et al. Anabolic steroids reduce spinal cord injury-related bone loss in rats associated with increased Wnt signaling. J. Spinal Cord Med. 2013, 36, 616–622. [Google Scholar] [CrossRef]
- Tian, Y.; Chen, J.; Yan, X.; Ren, D.; Liu, M.; Zhang, Q.; Zhang, Q.; Yuan, X. Overloaded Orthopedic Force Induces Condylar Subchondral Bone Absorption by Stimulating Rat Mesenchymal Stem Cells Differentiating into Osteoclasts via mTOR-Regulated RANKL/OPG Secretion in Osteoblasts. Stem Cells Dev. 2021, 30, 29–38. [Google Scholar] [CrossRef]
- Cao, X. RANKL-RANK signaling regulates osteoblast differentiation and bone formation. Bone Res. 2018, 6, 35. [Google Scholar] [CrossRef]
- Xu, H.; Chen, F.; Liu, T.; Xu, J.; Li, J.; Jiang, L.; Wang, X.; Sheng, J. Ellagic acid blocks RANKL–RANK interaction and suppresses RANKL-induced osteoclastogenesis by inhibiting RANK signaling pathways. Chem. Biol. Interact. 2020, 331, 109235. [Google Scholar] [CrossRef]
- Gao, K.; Zhang, T.; Wang, F.; Lv, C. Therapeutic Potential of Wnt-3a in Neurological Recovery after Spinal Cord Injury. Eur. Neurol. 2019, 81, 197–204. [Google Scholar] [CrossRef]
- Herman, P.E.; Papatheodorou, A.; Bryant, S.A.; Waterbury, C.K.M.; Herdy, J.R.; Arcese, A.A.; Buxbaum, J.D.; Smith, J.J.; Morgan, J.R.; Bloom, O. Highly conserved molecular pathways, including Wnt signaling, promote functional recovery from spinal cord injury in lampreys. Sci. Rep. 2018, 8, 742. [Google Scholar] [CrossRef] [PubMed]
- Yin, H.; Price, F.; Rudnicki, M.A. Satellite Cells and the Muscle Stem Cell Niche. Physiol. Rev. 2013, 93, 23–67. [Google Scholar] [CrossRef] [PubMed]
- Tang, Z.; Yang, C.; He, Z.; Deng, Z.; Li, X. Notoginsenoside R1 alleviates spinal cord injury through the miR-301a/KLF7 axis to activate Wnt/beta-catenin pathway. Open Med. 2022, 17, 741–755. [Google Scholar] [CrossRef] [PubMed]
- Rudnicki, M.A.; Williams, B.O. Wnt signaling in bone and muscle. Bone 2015, 80, 60–66. [Google Scholar] [CrossRef]
- Nedergaard, A.; Henriksen, K.; Karsdal, M.A.; Christiansen, C. Musculoskeletal ageing and primary prevention. Best Pr. Res. Clin. Obstet. Gynaecol. 2013, 27, 673–688. [Google Scholar] [CrossRef] [PubMed]
- Kirk, B.; Zanker, J.; Duque, G. Osteosarcopenia: Epidemiology, diagnosis, and treatment-facts and numbers. J. Cachexia Sarcopenia Muscle 2020, 11, 609–618. [Google Scholar] [CrossRef]
- LeBoff, M.S.; Chou, S.H.; Ratliff, K.A.; Cook, N.R.; Khurana, B.; Kim, E.; Cawthon, P.M.; Bauer, D.C.; Black, D.; Gallagher, J.C.; et al. Supplemental Vitamin D and Incident Fractures in Midlife and Older Adults. N. Engl. J. Med. 2022, 387, 299–309. [Google Scholar] [CrossRef] [PubMed]
- Dawson-Hughes, B.; Harris, S.S.; Krall, E.A.; Dallal, G.E. Effect of Calcium and Vitamin D Supplementation on Bone Density in Men and Women 65 Years of Age or Older. N. Engl. J. Med. 1997, 337, 670–676. [Google Scholar] [CrossRef]
- Bauman, W.A.; Zhang, R.-L.; Morrison, N.; Spungen, A.M. Acute Suppression of Bone Turnover with Calcium Infusion in Persons With Spinal Cord Injury. J. Spinal Cord Med. 2009, 32, 398–403. [Google Scholar] [CrossRef]
- Flueck, J.L.; Perret, C. Vitamin D deficiency in individuals with a spinal cord injury: A literature review. Spinal Cord 2017, 55, 428–434. [Google Scholar] [CrossRef]
- del Rivero, T.; Bethea, J.R. The effects of spinal cord injury on bone loss and dysregulation of the calcium/parathyroid hormone loop in mice. Osteoporos. Sarcopenia 2016, 2, 164–169. [Google Scholar] [CrossRef] [PubMed]
- Ung, R.-V.; Lapointe, N.P.; Guertin, P.A. Early adaptive changes in chronic paraplegic mice: A model to study rapid health degradation after spinal cord injury. Spinal Cord 2008, 46, 176–180. [Google Scholar] [CrossRef] [PubMed]
- Yalla, N.; Bobba, G.; Guo, G.; Stankiewicz, A.; Ostlund, R. Parathyroid hormone reference ranges in healthy individuals classified by vitamin D status. J. Endocrinol. Investig. 2019, 42, 1353–1360. [Google Scholar] [CrossRef] [PubMed]
- Maïmoun, L.; Couret, I.; Mariano-Goulart, D.; Dupuy, A.M.; Micallef, J.-P.; Peruchon, E.; Ohanna, F.; Cristol, J.-P.; Rossi, M.; Leroux, J.-L. Changes in Osteoprotegerin/RANKL System, Bone Mineral Density, and Bone Biochemicals Markers in Patients with Recent Spinal Cord Injury. Calcif. Tissue Int. 2005, 76, 404–411. [Google Scholar] [CrossRef] [PubMed]
- Voor, M.J.; Brown, E.H.; Xu, Q.; Waddell, S.W.; Burden, R.L.; Burke, D.A.; Magnuson, D.S.; Bramlett, H.M.; Dietrich, W.D.; Marcillo, A.; et al. Bone Loss following Spinal Cord Injury in a Rat Model. J. Neurotrauma 2012, 29, 1676–1682. [Google Scholar] [CrossRef]
- Zehnder, Y.; Michel, D.; Knecht, H.; Perrelet, R.; Neto, I.; Kraenzlin, M.; Lippuner, K.; Lüthi, M.; Zäch, G. Long-term changes in bone metabolism, bone mineral density, quantitative ultrasound parameters, and fracture incidence after spinal cord injury: A cross-sectional observational study in 100 paraplegic men. Osteoporos. Int. 2004, 15, 180–189. [Google Scholar] [CrossRef]
- Jang, E.J.; Lee, Y.-K.; Choi, H.J.; Ha, Y.-C.; Jang, S.; Shin, C.S.; Cho, N.H. Osteoporotic Fracture Risk Assessment Using Bone Mineral Density in Korean: A Community-based Cohort Study. J. Bone Metab. 2016, 23, 34–39. [Google Scholar] [CrossRef]
- Dorado, M.T.F.; Merino, M.d.S.D.; Marco, D.G.; Boy, R.C.; Samper, B.B.; Dhier, L.M.; Bertol, C.L. Preventive treatment with alendronate of loss of bone mineral density in acute traumatic spinal cord injury. Randomized controlled clinical trial. Spinal Cord 2022, 60, 687–693. [Google Scholar] [CrossRef]
- Naot, D.; Musson, D.S.; Cornish, J. The Activity of Adiponectin in Bone. Calcif. Tissue Int. 2017, 100, 486–499. [Google Scholar] [CrossRef]
- Haugen, S.; He, J.; Sundaresan, A.; Stunes, A.K.; Aasarød, K.M.; Tiainen, H.; Syversen, U.; Skallerud, B.; Reseland, J.E. Adiponectin Reduces Bone Stiffness: Verified in a Three-Dimensional Artificial Human Bone Model In Vitro. Front. Endocrinol. 2018, 9, 236. [Google Scholar] [CrossRef]
- Otzel, D.M.; Conover, C.F.; Ye, F.; Phillips, E.G.; Bassett, T.; Wnek, R.D.; Flores, M.; Catter, A.; Ghosh, P.; Balaez, A.; et al. Longitudinal Examination of Bone Loss in Male Rats After Moderate–Severe Contusion Spinal Cord Injury. Calcif. Tissue Int. 2019, 104, 79–91. [Google Scholar] [CrossRef] [PubMed]
- Carbone, L.D.; Chin, A.S.; Burns, S.P.; Svircev, J.N.; Hoenig, H.; Heggeness, M.; Bailey, L.; Weaver, F. Mortality After Lower Extremity Fractures in Men with Spinal Cord Injury. J. Bone Miner. Res. 2014, 29, 432–439. [Google Scholar] [CrossRef] [PubMed]
- Cheng, C.-H.; Chen, L.-R.; Chen, K.-H. Osteoporosis Due to Hormone Imbalance: An Overview of the Effects of Estrogen Deficiency and Glucocorticoid Overuse on Bone Turnover. Int. J. Mol. Sci. 2022, 23, 1376. [Google Scholar] [CrossRef] [PubMed]
- Mills, E.G.; Yang, L.; Nielsen, M.F.; Kassem, M.; Dhillo, W.S.; Comninos, A.N. The Relationship Between Bone and Reproductive Hormones Beyond Estrogens and Androgens. Endocr. Rev. 2021, 42, 691–719. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Cheng, J.; Wei, D.; Wu, H.; Zhao, J. Causal relationships between sex hormone traits, lifestyle factors, and osteoporosis in men: A Mendelian randomization study. PLoS ONE 2022, 17, e0271898. [Google Scholar] [CrossRef] [PubMed]
- Khosla, S.; Amin, S.; Orwoll, E. Osteoporosis in men. Endocr. Rev. 2008, 29, 441–464. [Google Scholar] [CrossRef]
- Bauman, W.A.; Emmons, R.R.; Cirnigliaro, C.M.; Kirshblum, S.C.; Spungen, A.M. An effective oral vitamin D replacement therapy in persons with spinal cord injury. J. Spinal Cord Med. 2011, 34, 455–460. [Google Scholar] [CrossRef]
- Tobeiha, M.; Moghadasian, M.H.; Amin, N.; Jafarnejad, S. RANKL/RANK/OPG Pathway: A Mechanism Involved in Exercise-Induced Bone Remodeling. BioMed Res. Int. 2020, 2020, 6910312. [Google Scholar] [CrossRef]
- Liu, F.-L.; Chen, C.-L.; Lee, C.-C.; Wu, C.-C.; Hsu, T.-H.; Tsai, C.-Y.; Huang, H.-S.; Chang, D.-M. The Simultaneous Inhibitory Effect of Niclosamide on RANKL-Induced Osteoclast Formation and Osteoblast Differentiation. Int. J. Med. Sci. 2017, 14, 840–852. [Google Scholar] [CrossRef]
- McDonald, C.L.; Lemme, N.J.; Testa, E.J.; Aaron, R.; Hartnett, D.A.; Cohen, E.M. Bisphosphonates in Total Joint Arthroplasty: A Review of Their Use and Complications. Arthroplast. Today 2022, 14, 133–139. [Google Scholar] [CrossRef]
- Nardone, V.; D'Asta, F.; Brandi, M.L. Pharmacological management of osteogenesis. Clinics 2014, 69, 438–446. [Google Scholar] [CrossRef]
- Bauman, W.A. Pharmacological approaches for bone health in persons with spinal cord injury. Curr. Opin. Pharmacol. 2021, 60, 346–359. [Google Scholar] [CrossRef] [PubMed]
- Russell, R.G.G. Bisphosphonates: Mode of Action and Pharmacology. Pediatrics 2007, 119 (Suppl. 2), S150–S162. [Google Scholar] [CrossRef] [PubMed]
- Drake, M.T.; Clarke, B.L.; Khosla, S. Bisphosphonates: Mechanism of Action and Role in Clinical Practice. Mayo Clin. Proc. 2008, 83, 1032–1045. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Liu, M.; Turner, R.; Iwaniec, U.; Kim, H.; Halloran, B. Dried plum mitigates spinal cord injury-induced bone loss in mice. JOR Spine 2020, 3, e1113. [Google Scholar] [CrossRef] [PubMed]
- Edwards, W.B.; Simonian, N.; Haider, I.T.; Anschel, A.S.; Chen, D.; Gordon, K.E.; Gregory, E.K.; Kim, K.H.; Parachuri, R.; Troy, K.L.; et al. Effects of Teriparatide and Vibration on Bone Mass and Bone Strength in People with Bone Loss and Spinal Cord Injury: A Randomized, Controlled Trial. J. Bone Miner. Res. 2018, 33, 1729–1740. [Google Scholar] [CrossRef]
- Kostenuik, P.J.; Nguyen, H.Q.; McCabe, J.; Warmington, K.S.; Kurahara, C.; Sun, N.; Chen, C.; Li, L.; Cattley, R.C.; Van, G.; et al. Denosumab, a Fully Human Monoclonal Antibody to RANKL, Inhibits Bone Resorption and Increases BMD in Knock-In Mice That Express Chimeric (Murine/Human) RANKL*. J. Bone Miner. Res. 2009, 24, 182–195. [Google Scholar] [CrossRef]
- Guo, Y.; Guo, T.; Di, Y.; Xu, W.; Hu, Z.; Xiao, Y.; Yu, H.; Hou, J. Pharmacokinetics, pharmacodynamics, safety and immunogenicity of recombinant, fully human anti-RANKL monoclonal antibody (MW031) versus denosumab in Chinese healthy subjects: A single-center, randomized, double-blind, single-dose, parallel-controlled trial. Expert Opin. Biol. Ther. 2023, 23, 705–715. [Google Scholar] [CrossRef]
- Won, K.Y.; Kalil, R.K.; Kim, Y.W.; Park, Y.-K. RANK signalling in bone lesions with osteoclast-like giant cells. Pathology 2011, 43, 318–321. [Google Scholar] [CrossRef]
- Miyagawa, K.; Ohata, Y.; Delgado-Calle, J.; Teramachi, J.; Zhou, H.; Dempster, D.D.; Subler, M.A.; Windle, J.J.; Chirgwin, J.M.; Roodman, G.D.; et al. Osteoclast-derived IGF1 is required for pagetic lesion formation in vivo. JCI Insight 2020, 5. [Google Scholar] [CrossRef]
- Song, R.; Gu, J.; Liu, X.; Zhu, J.; Wang, Q.; Gao, Q.; Zhang, J.; Cheng, L.; Tong, X.; Qi, X.; et al. Inhibition of osteoclast bone resorption activity through osteoprotegerin-induced damage of the sealing zone. Int. J. Mol. Med. 2014, 34, 856–862. [Google Scholar] [CrossRef] [PubMed]
- Liau, L.L.; Looi, Q.H.; Chia, W.C.; Subramaniam, T.; Ng, M.H.; Law, J.X. Treatment of spinal cord injury with mesenchymal stem cells. Cell Biosci. 2020, 10, 112. [Google Scholar] [CrossRef] [PubMed]
- Abo-Aziza, F.A.; Zaki, A.K.A.; El-Maaty, A.M.A. Bone marrow-derived mesenchymal stem cell (BM-MSC): A tool of cell therapy in hydatid experimentally infected rats. Cell Regen. 2019, 8, 58–71. [Google Scholar] [CrossRef] [PubMed]
- Boido, M.; Ghibaudi, M.; Gentile, P.; Favaro, E.; Fusaro, R.; Tonda-Turo, C. Chitosan-based hydrogel to support the paracrine activity of mesenchymal stem cells in spinal cord injury treatment. Sci. Rep. 2019, 9, 6402. [Google Scholar] [CrossRef]
- Ning, Z.; Gu, P.; Zhang, J.; Cheung, C.W.; Lao, L.; Chen, H.; Zhang, Z.-J. Adiponectin regulates electroacupuncture-produced analgesic effects in association with a crosstalk between the peripheral circulation and the spinal cord. Brain Behav. Immun. 2021, 99, 43–52. [Google Scholar] [CrossRef]
- Hook, M.A.; Falck, A.; Dundumulla, R.; Terminel, M.; Cunningham, R.; Sefiani, A.; Callaway, K.; Gaddy, D.; Geoffroy, C.G. Osteopenia in a Mouse Model of Spinal Cord Injury: Effects of Age, Sex and Motor Function. Biology 2022, 11, 189. [Google Scholar] [CrossRef]
- Bergmann, P.; Body, J.J.; Boonen, S.; Boutsen, Y.; Devogelaer, J.P.; Goemaere, S.; Kaufman, J.; Reginster, J.Y.; Rozenberg, S. Loading and Skeletal Development and Maintenance. J. Osteoporos. 2010, 2011, 786752. [Google Scholar] [CrossRef]
- Seo, B.R.; Mooney, D.J. Recent and Future Strategies of Mechanotherapy for Tissue Regenerative Rehabilitation. ACS Biomater. Sci. Eng. 2022, 8, 4639–4642. [Google Scholar] [CrossRef]
- Takemura, Y.; Moriyama, Y.; Ayukawa, Y.; Kurata, K.; Rakhmatia, Y.D.; Koyano, K. Mechanical loading induced osteocyte apoptosis and connexin 43 expression in three-dimensional cell culture and dental implant model. J. Biomed. Mater. Res. Part A 2018, 107, 815–827. [Google Scholar] [CrossRef]
- Harkema, S.J.; Ferreira, C.K.; Brand, R.J.v.D.; Krassioukov, A.V.; Jeffries, E.C.; Hoffman, S.M.; de Leon, R.; Dominguez, J.F.; Semerjian, T.Z.; Melgar, I.A.; et al. Improvements in Orthostatic Instability with Stand Locomotor Training in Individuals with Spinal Cord Injury. J. Neurotrauma 2008, 25, 1467–1475. [Google Scholar] [CrossRef]
- Braaksma, J.M.; Vegter, R.J.; Leving, M.T.; van der Scheer, J.W.; Tepper, M.; Woldring, F.A.; van der Woude, L.H.; Houdijk, H.; de Groot, S. Handrim wheelchair propulsion technique in individuals with spinal cord injury with and without shoulder pain—A cross-sectional comparison. Am. J. Phys. Med. Rehabil. 2023, 102, 886–895. [Google Scholar] [CrossRef] [PubMed]
- Lambach, R.L.; Stafford, N.E.; Kolesar, J.A.; Kiratli, B.J.; Creasey, G.H.; Gibbons, R.S.; Andrews, B.J.; Beaupre, G.S. Bone changes in the lower limbs from participation in an FES rowing exercise program implemented within two years after traumatic spinal cord injury. J. Spinal Cord Med. 2018, 43, 306–314. [Google Scholar] [CrossRef] [PubMed]
- Bickel, C.S.; Yarar-Fisher, C.; Mahoney, E.T.; McCully, K.K. Neuromuscular Electrical Stimulation–Induced Resistance Training After SCI: A Review of the Dudley Protocol. Top. Spinal Cord Inj. Rehabil. 2015, 21, 294–302. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Leone, G.E.; Shields, D.C.; Haque, A.; Banik, N.L. Rehabilitation: Neurogenic Bone Loss after Spinal Cord Injury. Biomedicines 2023, 11, 2581. https://doi.org/10.3390/biomedicines11092581
Leone GE, Shields DC, Haque A, Banik NL. Rehabilitation: Neurogenic Bone Loss after Spinal Cord Injury. Biomedicines. 2023; 11(9):2581. https://doi.org/10.3390/biomedicines11092581
Chicago/Turabian StyleLeone, Giovanna E., Donald C. Shields, Azizul Haque, and Narendra L. Banik. 2023. "Rehabilitation: Neurogenic Bone Loss after Spinal Cord Injury" Biomedicines 11, no. 9: 2581. https://doi.org/10.3390/biomedicines11092581
APA StyleLeone, G. E., Shields, D. C., Haque, A., & Banik, N. L. (2023). Rehabilitation: Neurogenic Bone Loss after Spinal Cord Injury. Biomedicines, 11(9), 2581. https://doi.org/10.3390/biomedicines11092581







