Brain Volumetric Analysis Using Artificial Intelligence Software in Premanifest Huntington’s Disease Individuals from a Colombian Caribbean Population
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Participants
2.2. Clinical Assessment
2.2.1. Diagnosis of Premanifestations of HD
Blood Samples and Genomic DNA Extraction
HTT CAG Repeat Quantification
MRI Volumetry
AI Software for Volumetric Imaging
2.3. Statistical Analysis
3. Results
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| HD | Huntington’s disease |
| HTT | Huntingtin gene (protein coding) |
| CAG | Cytosine, adenine, and guanine |
| VBM | Voxel-based morphometry |
| AI | Artificial intelligence |
References
- Stoker, T.B.; Mason, S.L.; Greenland, J.C.; Holden, S.T.; Santini, H.; Barker, R.A. Huntington’s disease: Diagnosis and management. Pract. Neurol. 2022, 22, 32–41. [Google Scholar] [CrossRef] [PubMed]
- National Center for Biotechnology Information. HTT Huntingtin [Homo Sapiens (Human)]—Gene—NCBI. 2021. Available online: https://www.ncbi.nlm.nih.gov/gene/3064 (accessed on 12 February 2024).
- Barnat, M.; Capizzi, M.; Aparicio, E.; Boluda, S.; Wennagel, D.; Kacher, R.; Kassem, R.; Lenoir, S.; Agasse, F.; Braz, B.Y.; et al. Huntington’s disease alters human neurodevelopment. Science 2020, 369, 787–793. [Google Scholar] [CrossRef] [PubMed]
- Aviner, R.; Lee, T.-T.; Masto, V.B.; Li, K.H.; Andino, R.; Frydman, J. Polyglutamine-mediated ribotoxicity disrupts proteostasis and stress responses in Huntington’s disease. Nat. Cell Biol. 2024, 26, 892–902. [Google Scholar] [CrossRef]
- Abeyasinghe, P.M.; Long, J.D.; Razi, A.; Pustina, D.; Paulsen, J.S.; Tabrizi, S.J.; Poudel, G.R.; Georgiou-Karistianis, N. Tracking Huntington’s Disease Progression Using Motor, Functional, Cognitive, and Imaging Markers. Mov. Disord. 2021, 36, 2282–2292. [Google Scholar] [CrossRef]
- Gusella, J.F.; MacDonald, M.E. Huntington’s disease: The case for genetic modifiers. Genome Med. 2009, 1, 80. [Google Scholar] [CrossRef]
- NIH. Enfermedad de Huntington|NINDS Español. INstituto Nacional de Trastornos Neurológicos y Accidentes Cerebrovasculares. 2022. Available online: https://espanol.ninds.nih.gov/es/trastornos/enfermedad-de-huntington (accessed on 12 February 2024).
- Waldvogel, H.J.; Kim, E.H.; Thu, D.C.V.; Tippett, L.J.; Faull, R.L.M. New Perspectives on the Neuropathology in Huntington’s Disease in the Human Brain and its Relation to Symptom Variation. J. Huntingt. Dis. 2012, 1, 143–153. [Google Scholar] [CrossRef] [PubMed]
- Pringsheim, T.; Wiltshire, K.; Day, L.; Dykeman, J.; Steeves, T.; Jette, N. The incidence and prevalence of Huntington’s disease: A systematic review and meta-analysis. Mov. Disord. 2012, 27, 1083–1091. [Google Scholar] [CrossRef]
- Daza, B.; Caiaffa, R.H.; Arteta, B.J.; Echeverría, R.V.; Ladrón de Guevara, Z.; Escamilla, M. Estudio neuroepidemiológico en Juan de Acosta, Atlántico, Colombia. ActaMédCoI 1991, 17, 324. [Google Scholar]
- Ganesh, S.; Chithambaram, T.; Krishnan, N.R.; Vincent, D.R.; Kaliappan, J.; Srinivasan, K. Exploring Huntington’s Disease Diagnosis via Artificial Intelligence Models: A Comprehensive Review. Diagnostics 2023, 13, 3592. [Google Scholar] [CrossRef]
- Rüb, U.; Seidel, K.; Heinsen, H.; Vonsattel, J.P.; den Dunnen, W.F.; Korf, H.W. Huntington’s disease (HD): The neuropathology of a multisystem neurodegenerative disorder of the human brain. Brain Pathol. 2016, 26, 726–740. [Google Scholar] [CrossRef]
- Liu, H.; Zhang, C.; Xu, J.; Jin, J.; Cheng, L.; Miao, X.; Wu, Q.; Wei, Z.; Liu, P.; Lu, H.; et al. Huntingtin silencing delays onset and slows progression of Huntington’s disease: A biomarker study. Brain 2021, 144, 3101–3113. [Google Scholar] [CrossRef] [PubMed]
- Saudou, F.; Humbert, S. The Biology of Huntingtin. Neuron 2016, 89, 910–926. [Google Scholar] [CrossRef] [PubMed]
- Gregory, S.; Scahill, R.I.; Rees, G.; Tabrizi, S. Magnetic resonance imaging in Huntington’s disease. In Huntington’s Disease; Precious, S.V., Rosser, A.E., Dunnett, S.B., Eds.; Methods in Molecular Biology; Humana Press: New York, NY, USA, 2018; Volume 1780, pp. 303–328. [Google Scholar] [CrossRef]
- Zeun, P.; Scahill, R.I.; Tabrizi, S.J.; Wild, E.J. Fluid and imaging biomarkers for Huntington’s disease. Mol. Cell. Neurosci. 2019, 97, 67–80. [Google Scholar] [CrossRef] [PubMed]
- Wijeratne, P.A.; Garbarino, S.; Gregory, S.; Johnson, E.B.; Scahill, R.I.; Paulsen, J.S.; Tabrizi, S.J.; Lorenzi, M.; Alexander, D.C. Revealing the Timeline of Structural MRI Changes in Premanifest to Manifest Huntington Disease. Neurol. Genet. 2021, 7, e617. [Google Scholar] [CrossRef] [PubMed]
- McColgan, P.; Gregory, S.; Seunarine, K.K.; Razi, A.; Papoutsi, M.; Johnson, E.; Durr, A.; Roos, R.A.C.; Leavitt, B.R.; Holmans, P.; et al. Brain Regions Showing White Matter Loss in Huntington’s Disease Are Enriched for Synaptic and Metabolic Genes. Biol. Psychiatry 2018, 83, 456–465. [Google Scholar] [CrossRef]
- Kumar, Y.; Koul, A.; Singla, R.; Ijaz, M.F. Artificial intelligence in disease diagnosis: A systematic literature review, synthesizing framework and future research agenda. J. Ambient. Intell. Humaniz. Comput. 2023, 14, 8459–8486. [Google Scholar] [CrossRef]
- De Natale, E.R.; Wilson, H.; Politis, M. Imaging BiomarkersBiomarkersin Huntington’s DiseaseHuntington’s Disease (HD) BT—Neurodegenerative Diseases Biomarkers: Towards Translating Research to Clinical Practice; Peplow, P.V., Martinez, B., Gennarelli, T.A., Eds.; Springer: New York, NY, USA, 2022; pp. 457–505. [Google Scholar] [CrossRef]
- Ashburner, J.; Friston, K.J. Unified segmentation. Neuroimage 2005, 26, 839–851. [Google Scholar] [CrossRef]
- Reuter, M.; Schmansky, N.J.; Rosas, H.D.; Fischl, B. Within-subject template estimation for unbiased longitudinal image analysis. Neuroimage 2012, 61, 1402–1418. [Google Scholar] [CrossRef]
- Ahmad, M.; Ríos-Anillo, M.R.; Acosta-López, J.E.; Cervantes-Henríquez, M.L.; Martínez-Banfi, M.; Pineda-Alhucema, W.; Puentes-Rozo, P.; Sánchez-Barros, C.; Pinzón, A.; Patel, H.R.; et al. Uncovering the Genetic and Molecular Features of Huntington’s Disease in Northern Colombia. Int. J. Mol. Sci. 2023, 24, 16154. [Google Scholar] [CrossRef]
- Sánchez-Rojas, M.; Puentes Rozo, P.; Pineda, D.A.; Acosta-López, J.; Mejía-Segura, E.; Cervantes-Henríquez, M.; Martínez-Banfi, M.; Ahmad, M.; Rosa Ríos Anillo, M.; Pineda-Alhucema, W.; et al. Enfermedad de Huntington una Aproximación Desde la Investigación; Universidad Simón Bolivar: Caracas, Venezuela, 2021. [Google Scholar]
- Huntington Study Group. Unified Huntington’s Disease Rating Scale: Reliability and consistency. Mov. Disord. 1996, 11, 136–142. [Google Scholar] [CrossRef]
- Myers, R.H.; Harris, J.D.; Shoulson, I. Physical disability rating scale. Clinical and neuropathologic assessment of severity in Huntington’s disease. Neurology 1988, 38, 341–347. [Google Scholar] [CrossRef] [PubMed]
- Ciosi, M.; Ciosi, M.; Cumming, S.A.; Mubarak, A.; Symeonidi, E.; Herzyk, P.; McGuinness, D.; Galbraith, J.; Hamilton, G.; Monckton, D.G. Library preparation and MiSeq sequencing for the genotyping-by-sequencing of the Huntington disease HTT exon one trinucleotide repeat and the quantification of somatic mosaicism. Protoc. Exch. 2018. [Google Scholar] [CrossRef]
- Free, S.L.; Bergin, P.S.; Fish, D.R.; Cook, M.J.; Shorvon, S.D.; Stevens, J.M. Methods for normalization of hippocampal volumes measured with MR. AJNR Am. J. Neuroradiol. 1995, 16, 637–643. [Google Scholar] [PubMed]
- Möhler, R.; Meyer, G. Development methods of guidelines and documents with recommendations on physical restraint reduction in nursing homes: A systematic review. BMC Geriatr. 2015, 15, 152. [Google Scholar] [CrossRef]
- Chew, R.; Wenger, M.; Guillory, J.; Nonnemaker, J.; Kim, A. Identifying Electronic Nicotine Delivery System Brands and Flavors on Instagram: Natural Language Processing Analysis. J. Med. Internet Res. 2022, 24, e30257. [Google Scholar] [CrossRef]
- Ceccarini, J.; Ahmad, R.; Van De Vliet, L.; Casteels, C.; Vandenbulcke, M.; Vandenberghe, W.; Van Laere, K. Behavioral symptoms in premanifest Huntington disease correlate with reduced frontal CB 1 R levels. J. Nucl. Med. 2019, 60, 115–121. [Google Scholar] [CrossRef]
- Podvin, S.; Reardon, H.T.; Yin, K.; Mosier, C.; Hook, V. Multiple clinical features of Huntington’s disease correlate with mutant HTT gene CAG repeat lengths and neurodegeneration. J. Neurol. 2019, 266, 551–564. [Google Scholar] [CrossRef]
- Valdés Hernández, M.D.C.; Abu-Hussain, J.; Qiu, X.; Priller, J.; Parra Rodríguez, M.; Pino, M.; Báez, S.; Ibáñez, A. Structural neuroimaging differentiates vulnerability from disease manifestation in colombian families with Huntington’s disease. Brain Behav. 2019, 9, e01343. [Google Scholar] [CrossRef]
- Tabrizi, S.J.; Langbehn, D.R.; Leavitt, B.R.; Roos, R.A.; Durr, A.; Craufurd, D.; Kennard, C.; Hicks, S.L.; Fox, N.C.; Scahill, R.I.; et al. Biological and clinical manifestations of Huntington’s disease in the longitudinal TRACK-HD study: Cross-sectional analysis of baseline data. Lancet Neurol. 2009, 8, 791–801. [Google Scholar] [CrossRef]
- Khan, W.; Alusi, S.; Tawfik, H.; Hussain, A. The relationship between non-motor features and weight-loss in the premanifest stage of Huntington’s disease. PLoS ONE 2021, 16, e0253817. [Google Scholar] [CrossRef]
- Langbehn, D.R.; Stout, J.C.; Gregory, S.; Mills, J.A.; Durr, A.; Leavitt, B.R.; Roos, R.A.C.; Long, J.D.; Owen, G.; Johnson, H.J.; et al. Association of CAG Repeats With Long-term Progression in Huntington Disease. JAMA Neurol. 2019, 76, 1375–1385. [Google Scholar] [CrossRef] [PubMed]
- Casella, C.; Lipp, I.; Rosser, A.; Jones, D.K.; Metzler-Baddeley, C. A Critical Review of White Matter Changes in Huntington’s Disease. Mov. Disord. 2020, 35, 1302–1311. [Google Scholar] [CrossRef]
- Tan, B.; Shishegar, R.; Poudel, G.R.; Fornito, A.; Georgiou-Karistianis, N. Cortical morphometry and neural dysfunction in Huntington’s disease: A review. Eur. J. Neurol. 2021, 28, 1406–1419. [Google Scholar] [CrossRef]
- Gómez-Ansón, B.; Alegret, M.; Muñoz, E.; Monté, G.C.; Alayrach, E.; Sánchez, A.; Boada, M.; Tolosa, E. Prefrontal cortex volume reduction on MRI in preclinical Huntington’s disease relates to visuomotor performance and CAG number. Park. Relat. Disord. 2009, 15, 213–219. [Google Scholar] [CrossRef] [PubMed]
- Penney, J.B.J.; Vonsattel, J.P.; MacDonald, M.E.; Gusella, J.F.; Myers, R.H. CAG repeat number governs the development rate of pathology in Huntington’s disease. Ann. Neurol. 1997, 41, 689–692. [Google Scholar] [CrossRef]
- Aylward, E.H.; Anderson, N.B.; Bylsma, F.W.; Wagster, M.V.; Barta, P.E.; Sherr, M.; Feeney, J.; Davis, A.; Rosenblatt, A.; Pearlson, G.D.; et al. Frontal lobe volume in patients with Huntington’s disease. Neurology 1998, 50, 252–258. [Google Scholar] [CrossRef]
- Hobbs, N.Z.; Barnes, J.; Frost, C.; Henley, S.M.D.; Wild, E.J.; Macdonald, K.; Barker, R.A.; Scahill, R.I.; Fox, N.C.; Tabrizi, S.J. Onset and progression of pathologic atrophy in Huntington disease: A longitudinal MR imaging study. AJNR Am. J. Neuroradiol. 2010, 31, 1036–1041. [Google Scholar] [CrossRef] [PubMed]
- Squitieri, F.; Cannella, M.; Simonelli, M.; Sassone, J.; Martino, T.; Venditti, E.; Ciammola, A.; Colonnese, C.; Frati, L.; Ciarmiello, A. Distinct brain volume changes correlating with clinical stage, disease progression rate, mutation size, and age at onset prediction as early biomarkers of brain atrophy in Huntington’s disease. CNS Neurosci. Ther. 2009, 15, 1–11. [Google Scholar] [CrossRef]
- Vonsattel, J.P.; DiFiglia, M. Huntington disease. J. Neuropathol. Exp. Neurol. 1998, 57, 369–384. [Google Scholar] [CrossRef]
- Fennema-Notestine, C.; Archibald, S.L.; Jacobson, M.W.; Corey-Bloom, J.; Paulsen, J.S.; Peavy, G.M.; Gamst, A.C.; Hamilton, J.M.; Salmon, D.P.; Jernigan, T.L. In vivo evidence of cerebellar atrophy and cerebral white matter loss in Huntington disease. Neurology 2004, 63, 989–995. [Google Scholar] [CrossRef]
- Glangetas, C.; Espinosa, P.; Bellone, C. Deficit in motor skill consolidation-dependent synaptic plasticity at motor cortex to dorsolateral striatum synapses in a mouse model of Huntington’s disease. eNeuro 2020, 7, 0297-19. [Google Scholar] [CrossRef] [PubMed]
- Kim, A.; Lalonde, K.; Truesdell, A.; Gomes Welter, P.; Brocardo, P.S.; Rosenstock, T.R.; Gil-Mohapel, J. New Avenues for the Treatment of Huntington’s Disease. Int. J. Mol. Sci. 2021, 22, 8363. [Google Scholar] [CrossRef] [PubMed]
- Ruocco, H.H.; Lopes-Cendes, I.; Li, L.M.; Santos-Silva, M.; Cendes, F. Striatal and extrastriatal atrophy in Huntington’s disease and its relationship with length of the CAG repeat. Braz. J. Med. Biol. Res. 2006, 39, 1129–1136. [Google Scholar] [CrossRef]
- Brown, T.; Chen, L. Neuropathology of Huntington’s Disease; IntechOpen: London, UK, 2022. [Google Scholar] [CrossRef]
- Escudero-Cabarcas, J.; Pineda-Alhucema, W.; Martinez-Banfi, M.; Acosta-López, J.E.; Cervantes-Henriquez, M.L.; Mejía-Segura, E.; Jiménez-Figueroa, G.; Sánchez-Barros, C.; Puentes-Rozo, P.J.; Noguera-Machacón, L.M.; et al. Theory of Mind in Huntington’s Disease: A Systematic Review of 20 Years of Research. J. Huntingt. Dis. 2024, 13, 15–31. [Google Scholar] [CrossRef]
- Tan, B.; Shishegar, R.; Fornito, A.; Poudel, G.; Georgiou-Karistianis, N. Longitudinal mapping of cortical surface changes in Huntington’s Disease. Brain Imaging Behav. 2022, 16, 1381–1391. [Google Scholar] [CrossRef] [PubMed]
- Seto-Ohshima, A.; Emson, P.C.; Lawson, E.; Mountjoy, C.Q.; Carrasco, L.H. Loss of matrix calcium-binding protein-containing neurons in Huntington’s disease. Lancet 1988, 1, 1252–1255. [Google Scholar] [CrossRef]
- Tippett, L.J.; Waldvogel, H.J.; Snell, R.G.; Vonsattel, J.-P.; Young, A.B.; Faull, R.L.M. The Complexity of Clinical Huntington’s Disease: Developments in Molecular Genetics, Neuropathology and Neuroimaging Biomarkers. Adv. Neurobiol. 2017, 15, 129–161. [Google Scholar] [CrossRef]
- Kassubek, J.; Juengling, F.D.; Ecker, D.; Landwehrmeyer, G.B. Thalamic atrophy in Huntington’s disease co-varies with cognitive performance: A morphometric MRI analysis. Cereb. Cortex 2005, 15, 846–853. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Rüb, U.; Hoche, F.; Brunt, E.R.; Heinsen, H.; Seidel, K.; Del Turco, D.; Paulson, H.L.; Bohl, J.; von Gall, C.; Vonsattel, J.-P.; et al. Degeneration of the cerebellum in Huntington’s disease (HD): Possible relevance for the clinical picture and potential gateway to pathological mechanisms of the disease process. Brain Pathol. 2013, 23, 165–177. [Google Scholar] [CrossRef]
- Drouin-Ouellet, J.; Sawiak, S.J.; Cisbani, G.; Lagacé, M.; Kuan, W.-L.; Saint-Pierre, M.; Dury, R.J.; Alata, W.; St-Amour, I.; Mason, S.L.; et al. Cerebrovascular and blood–brain barrier impairments in Huntington’s disease: Potential implications for its pathophysiology. Ann. Neurol. 2015, 78, 160–177. [Google Scholar] [CrossRef]
- Rocha, N.P.; Ribeiro, F.M.; Furr-Stimming, E.; Teixeira, A.L. Neuroimmunology of Huntington’s Disease: Revisiting Evidence from Human Studies. Mediat. Inflamm. 2016, 2016, 8653132. [Google Scholar] [CrossRef] [PubMed]



| Inclusion Criteria | Exclusion Criteria |
|---|---|
| Accepting and signing the informed consent form | Not accepting and signing the informed consent form |
| Belonging to a family with a record of at least one member with Huntington’s disease | Not being affiliated to the General Health Social Security System |
| Confirming the anomalous expansion of cytosine, adenine, and guanine triplets in the IT15 gene | Patients with movement disorders and/or a history of psychiatric disorders other than Huntington’s disease |
| Being affiliated to the General Health Social Security System |
| Variables | Triplet Expansion ≤26 | Triplet Expansion 27–35 | Triplet Expansion ≥40 | Fail/NA | Total |
|---|---|---|---|---|---|
| Age | 34.53 (σ10.40) | 27.50 (σ10.60) | 39.25 (σ12.44) | - | - |
| Gender | |||||
| Female (26) | 18 | 1 | 4 | 3 | 26 |
| Male (13) | 10 | 1 | 2 | 0 | 13 |
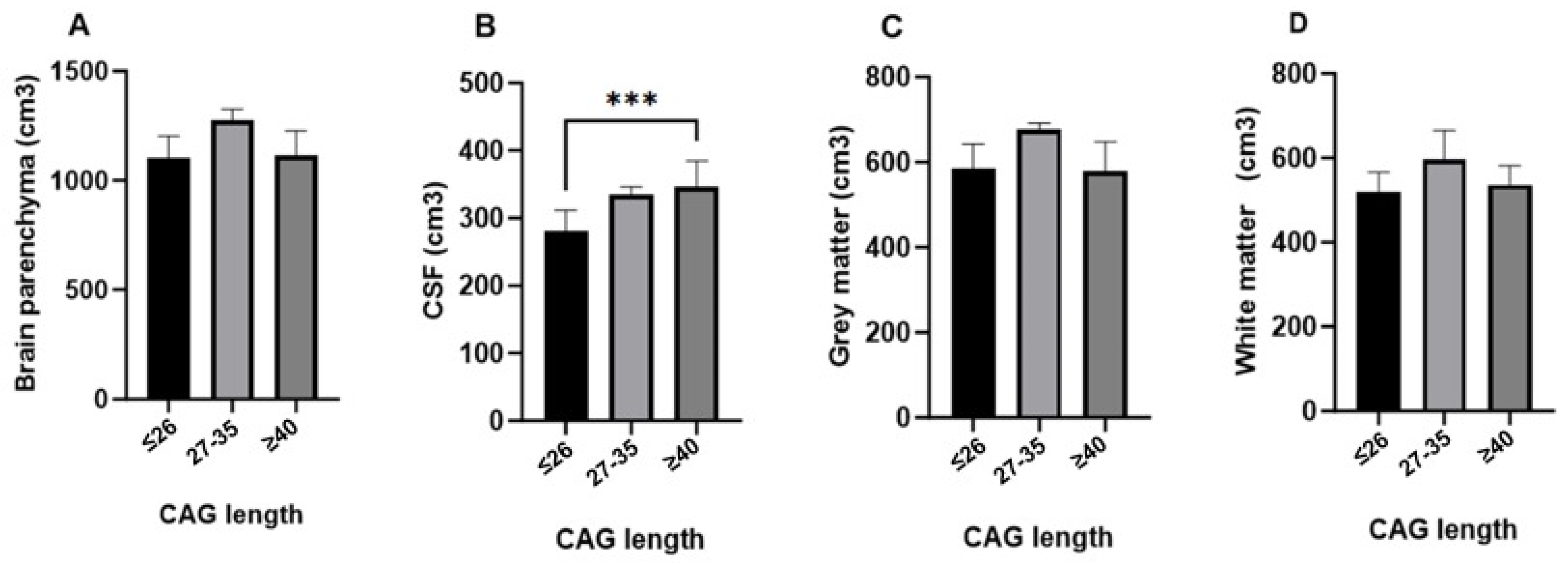
| Structures | Substructures | CAG | N | Average Range | Mean | Standard. Deviation | Minimum | Maximum | Kruskal–Wallis’s H Test | p |
|---|---|---|---|---|---|---|---|---|---|---|
| Global volumes | Brain parenchyma | ≤26 | 28 | 17.21 | 1115.14 | 105.204 | 918 | 1350 | 4.526 | 0.104 |
| 27–35 | 2 | 33.50 | ||||||||
| ≥40 | 6 | 19.50 | ||||||||
| CSF | ≤26 | 28 | 15.09 | 294.92 | 40.353 | 230 | 411 | 13.216 | 0.001 | |
| 27–35 | 2 | 30.00 | ||||||||
| ≥40 | 6 | 30.58 | ||||||||
| Gray matter | ≤26 | 28 | 17.39 | 589.78 | 59.892 | 456 | 722 | 4.366 | 0.113 | |
| 27–35 | 2 | 33.50 | ||||||||
| ≥40 | 6 | 18.67 | ||||||||
| White matter | ≤26 | 28 | 16.98 | 525.36 | 50.749 | 445 | 645 | 3.773 | 0.152 | |
| 27–35 | 2 | 30.75 | ||||||||
| ≥40 | 6 | 21.50 | ||||||||
| White matter, left hemisphere | ≤26 | 28 | 16.84 | 239.64 | 23.411 | 202 | 295 | 4.209 | 0.122 | |
| 27–35 | 2 | 31.00 | ||||||||
| ≥40 | 6 | 22.08 | ||||||||
| White matter, right hemisphere | ≤26 | 28 | 17.18 | 240.39 | 23.369 | 204 | 298 | 2.885 | 0.236 | |
| 27–35 | 2 | 29.25 | ||||||||
| ≥40 | 6 | 21.08 |
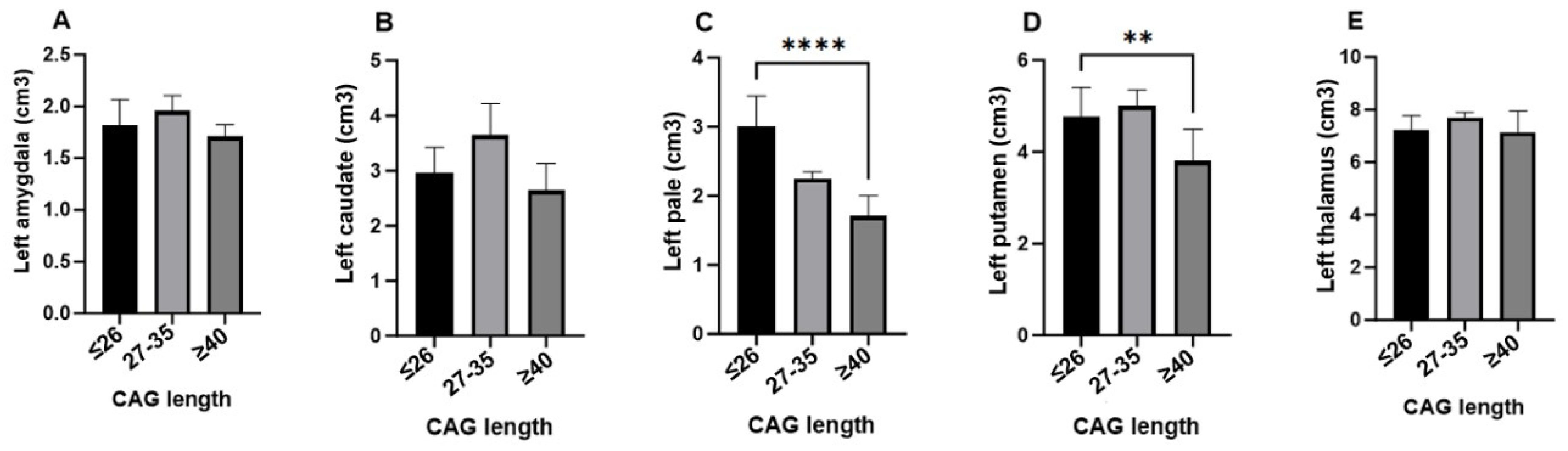
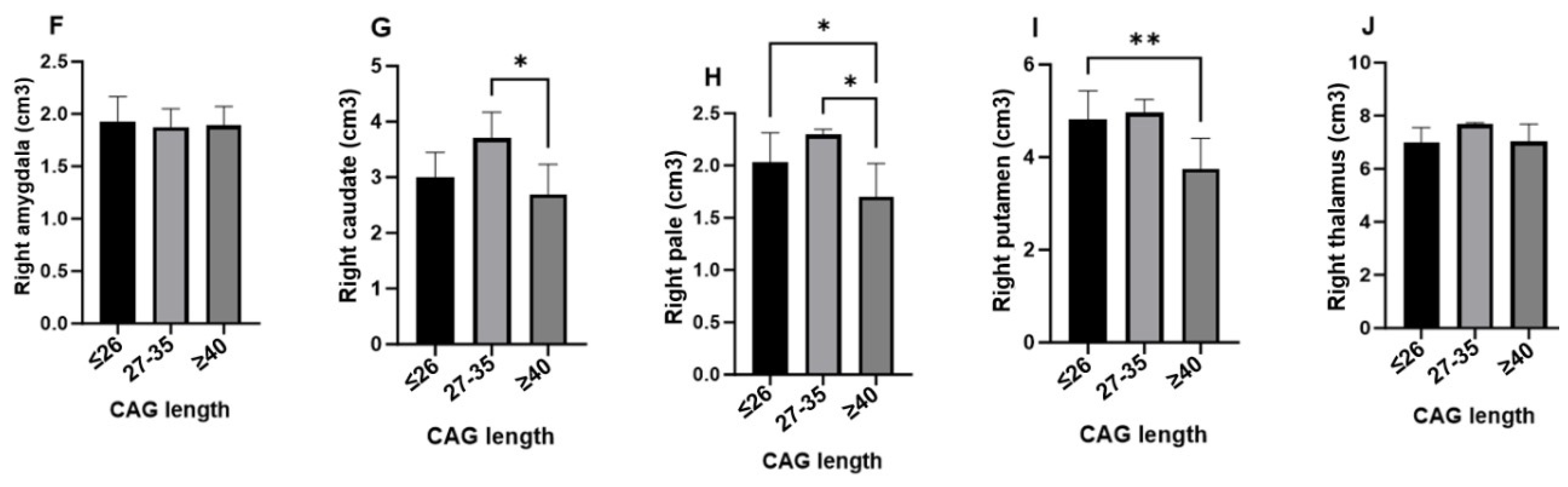
| Structures | Substructures | CAG | N | Average Range | Mean | Standard Deviation | Minimum | Maximum | Kruskal–Wallis H Test | p |
|---|---|---|---|---|---|---|---|---|---|---|
| Subcortical structures | Left amygdala | ≤26 | 28 | 18.91 | 1.8069 | 0.23091 | 1.40 | 2.41 | 2.811 | 0.245 |
| 27–35 | 2 | 27.50 | ||||||||
| ≥40 | 6 | 13.58 | ||||||||
| Right amygdala | ≤26 | 28 | 18.86 | 1.9189 | 0.22147 | 1.56 | 2.38 | 0.158 | 0.924 | |
| 27–35 | 2 | 18.00 | ||||||||
| ≥40 | 6 | 17.00 | ||||||||
| Left caudate | ≤26 | 28 | 18.98 | 2.9500 | 0.49608 | 1.69 | 4.05 | 5.449 | 0.066 | |
| 27–35 | 2 | 31.50 | ||||||||
| ≥40 | 6 | 11.92 | ||||||||
| Right caudate | ≤26 | 28 | 18.89 | 2.9908 | 0.49358 | 1.78 | 4.03 | 5.494 | 0.064 | |
| 27–35 | 2 | 32.00 | ||||||||
| ≥40 | 6 | 12.17 | ||||||||
| Left pallidum | ≤26 | 28 | 19.52 | 1.9750 | 0.30807 | 1.30 | 2.64 | 6.998 | 0.030 | |
| 27–35 | 2 | 30.50 | ||||||||
| ≥40 | 6 | 9.75 | ||||||||
| Right pallidum | ≤26 | 28 | 19.50 | 1.9883 | 0.31310 | 1.19 | 2.65 | 8.082 | 0.018 | |
| 27–35 | 2 | 32.00 | ||||||||
| ≥40 | 6 | 9.33 | ||||||||
| Left putamen | ≤26 | 28 | 20.52 | 4.6286 | 0.71912 | 2.85 | 5.64 | 9.043 | 0.011 | |
| 27–35 | 2 | 25.00 | ||||||||
| ≥40 | 6 | 6.92 | ||||||||
| Right putamen | ≤26 | 28 | 20.73 | 4.6425 | 0.72777 | 2.78 | 5.66 | 9.915 | 0.007 | |
| 27–35 | 2 | 24.00 | ||||||||
| ≥40 | 6 | 6.25 | ||||||||
| Left thalamus | ≤26 | 28 | 17.71 | 7.2292 | 0.59440 | 5.73 | 8.60 | 1.964 | 0.375 | |
| 27–35 | 2 | 28.50 | ||||||||
| ≥40 | 6 | 18.83 | ||||||||
| Right thalamus | ≤26 | 28 | 17.41 | 7.0389 | 0.57174 | 5.92 | 8.27 | 3.376 | 0.185 | |
| 27–35 | 2 | 31.50 | ||||||||
| ≥40 | 6 | 19.25 |
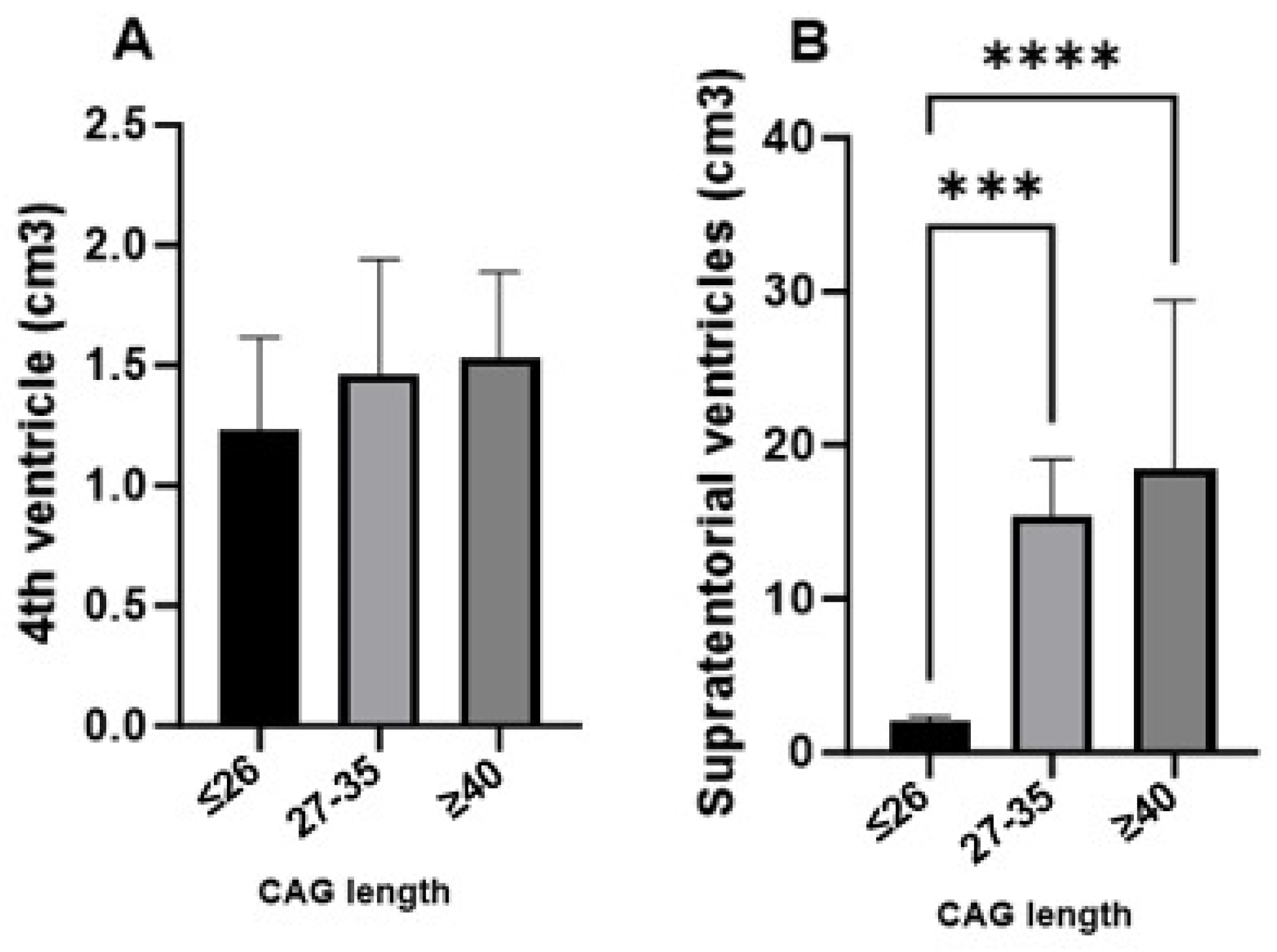
| Structures | Substructures | CAG | N | Average Range | Mean | Standard Deviation | Mini- mum | Maxi- mum | Kruskal–Wallis H Test | p |
|---|---|---|---|---|---|---|---|---|---|---|
| Ventricular system | 4th ventricle | ≤26 | 28 | 16.82 | 1.2939 | 0.39211 | 0.60 | 2.07 | 3.245 | 0.197 |
| 27–35 | 2 | 23.00 | ||||||||
| ≥40 | 6 | 24.83 | ||||||||
| Supratentorial ventricles | ≤26 | 28 | 15.29 | 11.0939 | 6.48371 | 3.73 | 39.10 | 11.765 | 0.003 | |
| 27–35 | 2 | 31.00 | ||||||||
| ≥40 | 6 | 29.33 |
| Structures | Substructures | CAG | N | Average Range | Mean | Standard Deviation | Minimum | Maximum | Kruskal–Wallis H Test | p |
|---|---|---|---|---|---|---|---|---|---|---|
| Infratentorial structures | White matter, left cerebellum | ≤26 | 28 | 17.04 | 12.7117 | 1.72630 | 8.92 | 15.60 | 4.551 | 0.103 |
| 27–35 | 2 | 33.00 | ||||||||
| ≥40 | 6 | 20.50 | ||||||||
| White matter, right cerebellum | ≤26 | 28 | 16.95 | 12.3500 | 1.61168 | 8.74 | 15.30 | 4.607 | 0.100 | |
| 27–35 | 2 | 32.75 | ||||||||
| ≥40 | 6 | 21.00 | ||||||||
| Gray matter, left cerebellum | ≤26 | 28 | 17.00 | 53.575 | 6.9595 | 42.2 | 75.1 | 4.397 | 0.111 | |
| 27–35 | 2 | 32.50 | ||||||||
| ≥40 | 6 | 20.83 | ||||||||
| Gray matter, right cerebellum | ≤26 | 28 | 16.96 | 52.783 | 6.8373 | 42.3 | 73.4 | 3.732 | 0.155 | |
| 27–35 | 2 | 30.50 | ||||||||
| ≥40 | 6 | 21.67 | ||||||||
| Brainstem | ≤26 | 28 | 17.79 | 20.197 | 2.3384 | 15.6 | 24.9 | 2.421 | 0.298 | |
| 27–35 | 2 | 29.75 | ||||||||
| ≥40 | 6 | 18.08 |
| Structures | Substructures | CAG | N | Average Range | Mean | Standard Deviation | Minimum | Maximum | Kruskal–Wallis H Test | p |
|---|---|---|---|---|---|---|---|---|---|---|
| Cortical areas | Frontal cortex | ≤26 | 28 | 17.66 | 136.736 | 16.6920 | 99.5 | 178.0 | 3.484 | 0.175 |
| 27–35 | 2 | 32.00 | ||||||||
| ≥40 | 6 | 17.92 | ||||||||
| Left frontal cortex | ≤26 | 28 | 17.79 | 68.853 | 8.4647 | 50.2 | 88.8 | 3.228 | 0.199 | |
| 27–35 | 2 | 31.50 | ||||||||
| ≥40 | 6 | 17.50 | ||||||||
| Right frontal cortex | ≤26 | 28 | 17.48 | 68.164 | 8.3325 | 49.3 | 89.3 | 4.327 | 0.115 | |
| 27–35 | 2 | 33.50 | ||||||||
| ≥40 | 6 | 18.25 | ||||||||
| Insular cortex | ≤26 | 28 | 18.04 | 11.1517 | 1.45717 | 8.42 | 14.50 | 1.222 | 0.543 | |
| 27–35 | 2 | 26.50 | ||||||||
| ≥40 | 6 | 18.00 | ||||||||
| Left insular cortex | ≤26 | 28 | 18.11 | 5.5375 | 0.75031 | 4.11 | 7.17 | 1.572 | 0.456 | |
| 27–35 | 2 | 27.50 | ||||||||
| ≥40 | 6 | 17.33 | ||||||||
| Right insular cortex | ≤26 | 28 | 17.73 | 5.6142 | 0.71584 | 4.30 | 7.35 | 1.481 | 0.477 | |
| 27–35 | 2 | 27.00 | ||||||||
| ≥40 | 6 | 19.25 | ||||||||
| Occipital cortex | ≤26 | 28 | 17.07 | 48.203 | 4.6208 | 34.8 | 59.3 | 2.981 | 0.225 | |
| 27–35 | 2 | 28.75 | ||||||||
| ≥40 | 6 | 21.75 | ||||||||
| Left occipital cortex | ≤26 | 28 | 17.52 | 23.686 | 2.3424 | 17.3 | 28.2 | 1.982 | 0.371 | |
| 27–35 | 2 | 28.00 | ||||||||
| ≥40 | 6 | 19.92 | ||||||||
| Right occipital cortex | ≤26 | 28 | 16.75 | 24.511 | 2.5215 | 17.5 | 31.1 | 4.534 | 0.104 | |
| 27–35 | 2 | 31.25 | ||||||||
| ≥40 | 6 | 22.42 | ||||||||
| Parietal cortex | ≤26 | 28 | 18.41 | 124.433 | 11.9950 | 95.6 | 152.0 | 4.523 | 0.104 | |
| 27–35 | 2 | 32.50 | ||||||||
| ≥40 | 6 | 14.25 | ||||||||
| Left parietal cortex | ≤26 | 28 | 18.36 | 61.4975 | 5.90719 | 48.00 | 76.20 | 4.085 | 0.130 | |
| 27–35 | 2 | 32.00 | ||||||||
| ≥40 | 6 | 14.67 | ||||||||
| Right parietal cortex | ≤26 | 28 | 18.39 | 62.892 | 6.2177 | 47.7 | 76.2 | 5.154 | 0.076 | |
| 27–35 | 2 | 33.50 | ||||||||
| ≥40 | 6 | 14.00 | ||||||||
| Temporal cortex | ≤26 | 28 | 17.63 | 108.156 | 13.1853 | 84.8 | 137.0 | 3.244 | 0.197 | |
| 27–35 | 2 | 31.50 | ||||||||
| ≥40 | 6 | 18.25 | ||||||||
| Left temporal cortex | ≤26 | 28 | 17.46 | 55.164 | 6.6123 | 43.5 | 69.9 | 3.330 | 0.189 | |
| 27–35 | 2 | 31.50 | ||||||||
| ≥40 | 6 | 19.00 | ||||||||
| Right temporal cortex | ≤26 | 28 | 17.61 | 52.906 | 6.6293 | 41.3 | 66.9 | 3.248 | 0.197 | |
| 27–35 | 2 | 31.50 | ||||||||
| ≥40 | 6 | 18.33 | ||||||||
| Left hippocampus | ≤26 | 28 | 17.23 | 4.1364 | 0.27691 | 3.58 | 4.69 | 1.897 | 0.387 | |
| 27–35 | 2 | 21.25 | ||||||||
| ≥40 | 6 | 23.50 | ||||||||
| Right hippocampus | ≤26 | 28 | 18.00 | 4.2328 | 0.29162 | 3.74 | 4.88 | 0.622 | 0.733 | |
| 27–35 | 2 | 16.50 | ||||||||
| ≥40 | 6 | 21.50 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ríos-Anillo, M.R.; Ahmad, M.; Acosta-López, J.E.; Cervantes-Henríquez, M.L.; Henao-Castaño, M.C.; Morales-Moreno, M.T.; Espitia-Almeida, F.; Vargas-Manotas, J.; Sánchez-Barros, C.; Pineda, D.A.; et al. Brain Volumetric Analysis Using Artificial Intelligence Software in Premanifest Huntington’s Disease Individuals from a Colombian Caribbean Population. Biomedicines 2024, 12, 2166. https://doi.org/10.3390/biomedicines12102166
Ríos-Anillo MR, Ahmad M, Acosta-López JE, Cervantes-Henríquez ML, Henao-Castaño MC, Morales-Moreno MT, Espitia-Almeida F, Vargas-Manotas J, Sánchez-Barros C, Pineda DA, et al. Brain Volumetric Analysis Using Artificial Intelligence Software in Premanifest Huntington’s Disease Individuals from a Colombian Caribbean Population. Biomedicines. 2024; 12(10):2166. https://doi.org/10.3390/biomedicines12102166
Chicago/Turabian StyleRíos-Anillo, Margarita R., Mostapha Ahmad, Johan E. Acosta-López, Martha L. Cervantes-Henríquez, Maria C. Henao-Castaño, Maria T. Morales-Moreno, Fabián Espitia-Almeida, José Vargas-Manotas, Cristian Sánchez-Barros, David A. Pineda, and et al. 2024. "Brain Volumetric Analysis Using Artificial Intelligence Software in Premanifest Huntington’s Disease Individuals from a Colombian Caribbean Population" Biomedicines 12, no. 10: 2166. https://doi.org/10.3390/biomedicines12102166
APA StyleRíos-Anillo, M. R., Ahmad, M., Acosta-López, J. E., Cervantes-Henríquez, M. L., Henao-Castaño, M. C., Morales-Moreno, M. T., Espitia-Almeida, F., Vargas-Manotas, J., Sánchez-Barros, C., Pineda, D. A., & Sánchez-Rojas, M. (2024). Brain Volumetric Analysis Using Artificial Intelligence Software in Premanifest Huntington’s Disease Individuals from a Colombian Caribbean Population. Biomedicines, 12(10), 2166. https://doi.org/10.3390/biomedicines12102166






