Usage of the Anemia Control Model Is Associated with Reduced Hospitalization Risk in Hemodialysis
Abstract
1. Introduction
2. Materials and Methods
2.1. The Anemia Control Model (ACM)
2.2. Study Design and Participants
2.3. Definition of Exposure Groups
2.3.1. ACM Adherent Patients
2.3.2. Reference Group
2.4. Covariates
2.5. Outcome Definition
2.6. Statistical Analysis
2.6.1. Primary Analysis
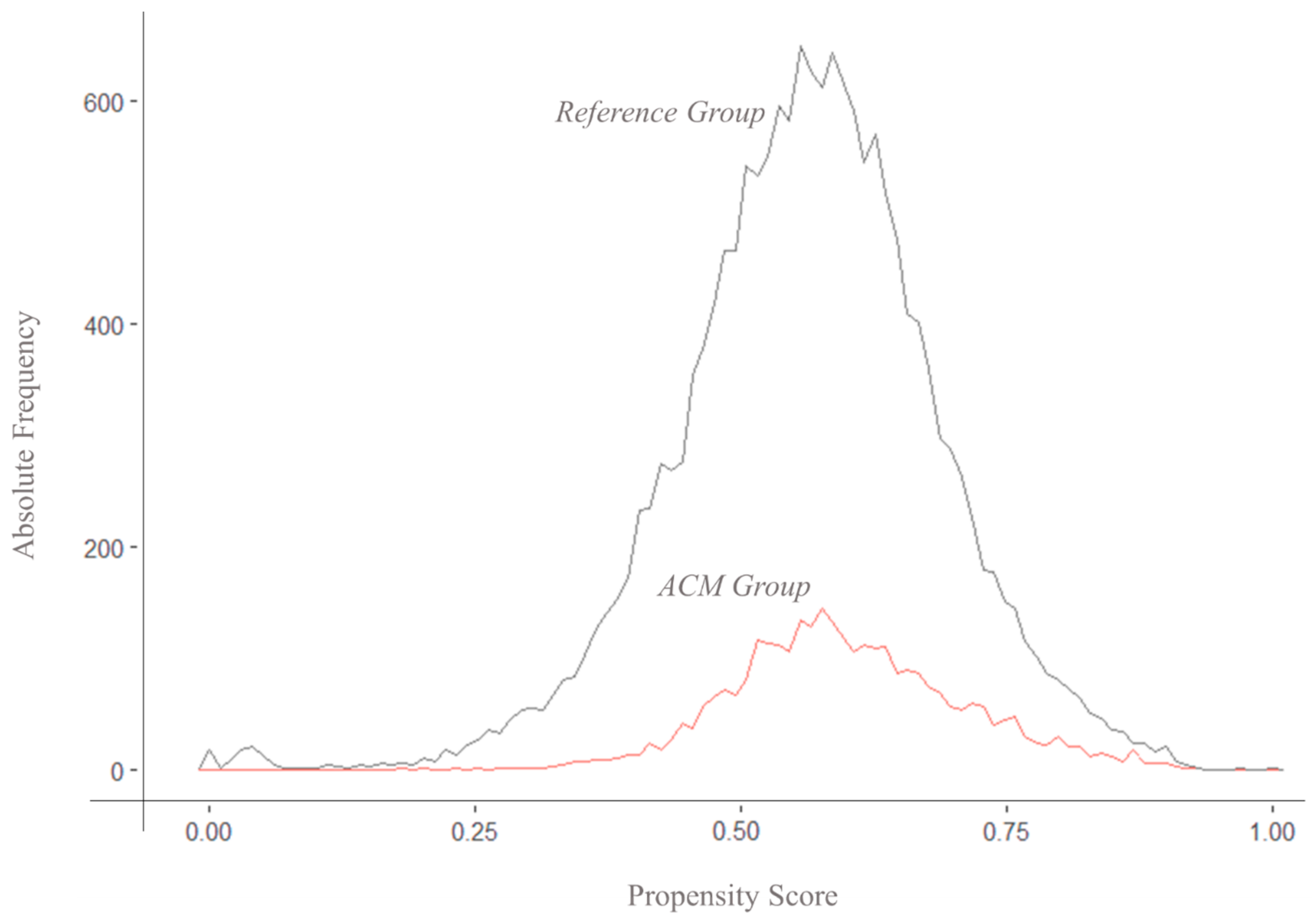
Propensity Score (PM) Estimation
Matching Strategy
Outcomes Estimation
2.6.2. Secondary Analysis
3. Results
3.1. Study Sample before Matching
3.2. Propensity Score Estimation
3.3. Study Sample after Matching
3.4. Hospitalization and Mortality Rate
3.5. Secondary Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- McMurray, J.J.V.; Parfrey, P.S.; Adamson, J.W.; Aljama, P.; Berns, J.S.; Bohlius, J.; Drüeke, T.B.; Finkelstein, F.O.; Fishbane, S.; Ganz, T.; et al. Kidney disease: Improving global outcomes (KDIGO) anemia work group. KDIGO clinical practice guideline for anemia in chronic kidney disease. Kidney Int. Suppl. 2012, 2, 279–335. [Google Scholar] [CrossRef]
- Hanna, R.M.; Streja, E.; Kalantar-Zadeh, K. Burden of Anemia in Chronic Kidney Disease: Beyond Erythropoietin. Adv. Ther. 2021, 38, 52–75. [Google Scholar] [CrossRef]
- KDOQI; National Kidney Foundation. KDOQI Clinical Practice Guidelines and Clinical Practice Recommendations for Anemia in Chronic Kidney Disease. Am. J. Kidney Dis. 2006, 47 (Suppl. S3), S1–S14. [Google Scholar]
- Toft, G.; Heide-Jørgensen, U.; van Haalen, H.; James, G.; Hedman, K.; Birn, H.; Christiansen, C.F. Anemia and clinical outcomes in patients with non-dialysis dependent or dialysis dependent severe chronic kidney disease: A Danish population-based study. J. Nephrol. 2020, 33, 147–156. [Google Scholar] [CrossRef]
- Quon, P.; Gitlin, M.; Isitt, J.J.; Mohan, S.; McClellan, W.M.; Javier, J.; de Lissovoy, G.; Hollenbeak, C.S. Cost-effectiveness of treating chronic anemia with epoetin alfa among hemodialysis patients in the United States. Health Outcomes Res. Med. 2012, 3, e79–e89. [Google Scholar] [CrossRef]
- Toida, T.; Iwakiri, T.; Sato, Y.; Komatsu, H.; Kitamura, K.; Fujimoto, S. Relationship between hemoglobin levels corrected by interdialytic weight gain and mortality in japanese hemodialysis patients: Miyazaki dialysis cohort study. PLoS ONE 2017, 12, e0169117. [Google Scholar] [CrossRef] [PubMed]
- Locatelli, F.; Nissenson, A.R.; Barrett, B.J.; Walker, R.G.; Wheeler, D.C.; Eckardt, K.U.; Lameire, N.H.; Eknoyan, G. Clinical practice guidelines for anemia in chronic kidney disease: Problems and solutions. A position statement from Kidney Disease: Improving Global Outcomes (KDIGO). Kidney Int. 2008, 74, 1237–1240. [Google Scholar] [CrossRef]
- Borawski, B.; Malyszko, J.S.; Kwiatkowska, M.; Malyszko, J. Current status of renal anemia pharmacotherapy—What can we offer today. J. Clin. Med. 2021, 10, 4149. [Google Scholar] [CrossRef]
- Drüeke, T.B.; Parfrey, P.S. Summary of the KDIGO guideline on anemia and comment: Reading between the (guide)line(s). Kidney Int. 2012, 82, 952–960. [Google Scholar] [CrossRef]
- UK Renal Registry (UKRR). Adults on In-Centre Haemodialysis (ICHD) in the UK at the End of 2020. Available online: https://ukkidney.org/sites/renal.org/files/24th_UKRR_ANNUAL_REPORT_ICHD_Ch5.pdf (accessed on 1 September 2024).
- Zhao, X.; Niu, Q.; Gan, L.; Hou, F.F.; Liang, X.; Ni, Z.; Chen, Y.; Zhao, J.; Bieber, B.; Robinson, B.; et al. Baseline data report of the China Dialysis Outcomes and Practice Patterns Study (DOPPS). Sci. Rep. 2021, 11, 873. [Google Scholar] [CrossRef]
- Chait, Y.; Nathanson, B.H.; Germain, M.J. Individualized anemia management enhanced by ferric pyrophosphate citrate protocol. Sci. Rep. 2022, 12, 20122. [Google Scholar] [CrossRef] [PubMed]
- United States Renal Data System. Clinical indicators & preventive care. In 2022 USRDS Annual Data Report: Epidemiology of Kidney Disease in the United States; National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases: Stapleton, NY, USA, 2022. Available online: https://usrds-adr.niddk.nih.gov/2022/end-stage-renal-disease/3-clinical-indicators-and-preventive-care (accessed on 1 September 2024).
- Gilbertson, D.T.; Ebben, J.P.; Foley, R.N.; Weinhandl, E.D.; Bradbury, B.D.; Collins, A.J. Hemoglobin level variability: Associations with mortality. Clin. J. Am. Soc. Nephrol. 2008, 3, 133–138. [Google Scholar] [CrossRef]
- Ishani, A.; Solid, C.A.; Weinhandl, E.D.; Gilbertson, D.T.; Foley, R.N.; Collins, A.J. Association between number of months below K/DOQI haemoglobin target and risk of hospitalization and death. Nephrol. Dial. Transplant. 2008, 23, 1682–1689. [Google Scholar] [CrossRef] [PubMed]
- Phrommintikul, A.; Haas, S.J.; Elsik, M.; Krum, H. Mortality and target haemoglobin concentrations in anaemic patients with chronic kidney disease treated with erythropoietin: A meta-analysis. Lancet 2007, 369, 381–388. [Google Scholar] [CrossRef] [PubMed]
- Parfrey, P.S.; Foley, R.N.; Wittreich, B.H.; Sullivan, D.J.; Zagari, M.J.; Frei, D. Double-blind comparison of full and partial anemia correction in incident hemodialysis patients without symptomatic heart disease. J. Am. Soc. Nephrol. 2005, 16, 2180–2189. [Google Scholar] [CrossRef]
- Singh, A.K.; Szczech, L.; Tang, K.L.; Barnhart, H.; Sapp, S.; Wolfson, M.; Reddan, D. Correction of Anemia with Epoetin Alfa in Chronic Kidney Disease. N. Engl. J. Med. 2006, 355, 2085–2098. [Google Scholar] [CrossRef] [PubMed]
- Lau, J.H.; Gangji, A.S.; Rabbat, C.G.; Brimble, K.S. Impact of haemoglobin and erythropoietin dose changes on mortality: A secondary analysis of results from a randomized anaemia management trial. Nephrol. Dial. Transplant. 2010, 25, 4002–4009. [Google Scholar] [CrossRef] [PubMed]
- Besarab, A.; Bolton, W.K.; Browne, J.K.; Egrie, J.C.; Nissenson, A.R.; Okamoto, D.M.; Schwab, S.J.; Goodkin, D.A. The Effects of Normal as Compared with Low Hematocrit Values in Patients with Cardiac Disease Who Are Receiving Hemodialysis and Epoetin. N. Engl. J. Med. 1998, 339, 584–590. [Google Scholar] [CrossRef] [PubMed]
- Pfeffer, M.A.; Burdmann, E.A.; Chen, C.Y.; Cooper, M.E.; De Zeeuw, D.; Eckardt, K.U.; Feyzi, J.M.; Ivanovich, P.; Kewalramani, R.; Levey, A.S.; et al. A Trial of Darbepoetin Alfa in Type 2 Diabetes and Chronic Kidney Disease. N. Engl. J. Med. 2009, 361, 2019–2032. [Google Scholar] [CrossRef]
- Solomon, S.D.; Uno, H.; Lewis, E.F.; Eckardt, K.U.; Lin, J.; Burdmann, E.A.; De Zeeuw, D.; Ivanovich, P.; Levey, A.S.; Parfrey, P.; et al. Erythropoietic Response and Outcomes in Kidney Disease and Type 2 Diabetes. N. Engl. J. Med. 2010, 363, 1146–1155. [Google Scholar] [CrossRef]
- Szczech, L.A.; Barnhart, H.X.; Inrig, J.K.; Reddan, D.N.; Sapp, S.; Califf, R.M.; Patel, U.D.; Singh, A.K. Secondary analysis of the CHOIR trial epoetin-α dose and achieved hemoglobin outcomes. Kidney Int. 2008, 74, 791–798. [Google Scholar] [CrossRef] [PubMed]
- Food and Drug Administration. FDA Drug Safety Communication: Modified Dosing Recommendations to Improve the Safe Use of Erythropoiesis-Stimulating Agents in Chronic Kidney Disease; Food and Drug Administration: Silver Spring, MD, USA, 2011.
- Koulouridis, I.; Alfayez, M.; Trikalinos, T.A.; Balk, E.M.; Jaber, B.L. Dose of Erythropoiesis-Stimulating Agents and Adverse Outcomes in CKD: A metaregression analysis. Am. J. Kidney Dis. 2013, 61, 44–56. [Google Scholar] [CrossRef] [PubMed]
- Jeong, H.Y.; Ko, E.J.; Kim, S.H.; Lee, M.J.; Cho, H.J.; Yang, D.H.; Lee, S.Y. Administration of a high-dose erythropoietin-stimulating agent in hemodialysis patients is associated with late arteriovenous fistula failure. Yonsei Med. J. 2017, 58, 793–799. [Google Scholar] [CrossRef] [PubMed]
- Kuragano, T.; Matsumura, O.; Matsuda, A.; Hara, T.; Kiyomoto, H.; Murata, T.; Kitamura, K.; Fujimoto, S.; Hase, H.; Joki, N.; et al. Association between hemoglobin variability, serum ferritin levels, and adverse events/mortality in maintenance hemodialysis patients. Kidney Int. 2014, 86, 845–854. [Google Scholar] [CrossRef]
- Pérez-García, R.; Varas, J.; Cives, A.; Martín-Malo, A.; Aljama, P.; Ramos, R.; Pascual, J.; Stuard, S.; Canaud, B.; Merello, J.I.; et al. Increased mortality in haemodialysis patients administered high doses of erythropoiesis-stimulating agents: A propensity score-matched analysis. Nephrol. Dial. Transplant. 2018, 33, 690–699. [Google Scholar] [CrossRef]
- Salgado Filho, N.; Lages, J.S.; Brito, D.J.D.A.; Santos, E.J.F.; Dos Santos, A.M.; de Souza, F.L.; Mendes, V.G.G.; Silva, G.A.D.S.; Carneiro, E.C.R.D.L.; Muniz, M.P.R.; et al. Variability in hemoglobin levels and the factors associated with mortality in hemodialysis patients: A 78-month follow-up study. Int. J. Environ. Res. Public Health 2021, 18, 1078. [Google Scholar] [CrossRef] [PubMed]
- Streja, E.; Park, J.; Chan, T.Y.; Lee, J.; Soohoo, M.; Rhee, C.M.; Arah, O.A.; Kalantar-Zadeh, K. Erythropoietin Dose and Mortality in Hemodialysis Patients: Marginal Structural Model to Examine Causality. Int. J. Nephrol. 2016, 2016, 6087134. [Google Scholar] [CrossRef]
- Cizman, B.; Smith, H.T.; Camejo, R.R.; Casillas, L.; Dhillon, H.; Mu, F.; Wu, E.; Xie, J.; Zuckerman, P.; Coyne, D. Clinical and Economic Outcomes of Erythropoiesis-Stimulating Agent Hyporesponsiveness in the Post-Bundling Era. Kidney Med. 2020, 2, 589–599.e1. [Google Scholar] [CrossRef] [PubMed]
- Ebben, J.P.; Gilbertson, D.T.; Foley, R.N.; Collins, A.J. Hemoglobin level variability: Associations with comorbidity, intercurrent events, and hospitalizations. Clin. J. Am. Soc. Nephrol. 2006, 1, 1205–1210. [Google Scholar] [CrossRef]
- Lin, F.J.; Zhang, X.; Huang, L.S.; Ji, G.; Huang, H.D.; Xie, Y.; Jiang, G.R.; Zhou, X.; Lu, W. Impact of hemoglobin variability on cardiovascular mortality in maintenance hemodialysis patients. Int. Urol. Nephrol. 2018, 50, 1703–1712. [Google Scholar] [CrossRef]
- Zhao, L.; Hu, C.; Cheng, J.; Zhang, P.; Jiang, H.; Chen, J. Haemoglobin variability and all-cause mortality in haemodialysis patients: A systematic review and meta-analysis. Nephrology 2019, 24, 1265–1272. [Google Scholar] [CrossRef] [PubMed]
- Yang, W.; Israni, R.K.; Brunelli, S.M.; Joffe, M.M.; Fishbane, S.; Feldman, H.I. Hemoglobin variability and mortality in ESRD. J. Am. Soc. Nephrol. 2007, 18, 3164–3170. [Google Scholar] [CrossRef] [PubMed]
- Fishbane, S.; Berns, J.S. Evidence and implications of haemoglobin cycling in anaemia management. Nephrol. Dial. Transplant. 2007, 22, 2129–2132. [Google Scholar] [CrossRef] [PubMed]
- Schneider, A.; Asmus, G.; Biggar, P.; Braun, J.; Dellanna, F.; Fiedler, R.; Galle, J.; Girndt, M.; Gondolf, K.; Hahn, K.; et al. Hemoglobin Cycling in Hemodialysis Patients. Nephrol. Res Rev. 2010, 2, 1–5. [Google Scholar] [CrossRef]
- Barbieri, C.; Mari, F.; Stopper, A.; Gatti, E.; Escandell-Montero, P.; Martínez-Martínez, J.M.; Martín-Guerrero, J.D. A new machine learning approach for predicting the response to anemia treatment in a large cohort of End Stage Renal Disease patients undergoing dialysis. Comput Biol Med. 2015, 61, 56–61. [Google Scholar] [CrossRef]
- Barbieri, C.; Molina, M.; Ponce, P.; Tothova, M.; Cattinelli, I.; Titapiccolo, J.I.; Mari, F.; Amato, C.; Leipold, F.; Wehmeyer, W.; et al. An international observational study suggests that artificial intelligence for clinical decision support optimizes anemia management in hemodialysis patients. Kidney Int. 2016, 90, 422–429. [Google Scholar] [CrossRef] [PubMed]
- Bucalo, M.L.; Barbieri, C.; Roca, S.; Titapiccolo, J.I.; Romero, M.S.R.; Ramos, R.; Albaladejo, M.; Manzano, D.; Mari, F.; Molina, M. The anaemia control model: Does it help nephrologists in therapeutic decision-making in the management of anaemia? Nefrologia 2018, 38, 491–502. [Google Scholar] [CrossRef] [PubMed]
- Garbelli, M.; Bellocchio, F.; Baro Salvador, M.E.; Chermisi, M.; Rincon Bello, A.; Godoy, I.B.; Perez, S.O.; Shkolenko, K.; Perez, A.S.; Toro, D.S.; et al. The use of Anemia Control Model is Associated with Improved Hemoglobin Target Achievement, Lower Rates of Inappropriate Erythropoietin Stimulating Agents, and Severe Anemia among Dialysis Patients. Blood Purif. 2024, 53, 405–417. [Google Scholar] [CrossRef]
- Barbieri, C.; Bolzoni, E.; Mari, F.; Cattinelli, I.; Bellocchio, F.; Martin, J.D.; Amato, C.; Stopper, A.; Gatti, E.; Macdougall, I.C.; et al. Performance of a predictive model for long-Term hemoglobin response to darbepoetin and iron administration in a large cohort of hemodialysis patients. PLoS ONE 2016, 11, e0148938. [Google Scholar] [CrossRef]
- Escandell-Montero, P.; Chermisi, M.; Martinez-Martinez, J.M.; Gomez-Sanchis, J.; Barbieri, C.; Soria-Olivas, E.; Mari, F.; Vila-Francés, J.; Stopper, A.; Gatti, E.; et al. Optimization of anemia treatment in hemodialysis patients via reinforcement learning. Artif. Intell. Med. 2014, 62, 47–60. [Google Scholar] [CrossRef] [PubMed]
- Garbelli, M.; Ion Titapiccolo, J.; Bellocchio, F.; Stuard, S.; Brancaccio, D.; Neri, L. Prolonged patient survival after implementation of a continuous quality improvement programme empowered by digital transformation in a large dialysis network. Nephrol. Dial. Transplant. 2022, 37, 469–476. [Google Scholar] [CrossRef] [PubMed]
- Pellicer-Valero, O.J.; Cattinelli, I.; Neri, L.; Mari, F.; Martín-Guerrero, J.D.; Barbieri, C. Enhanced prediction of hemoglobin concentration in a very large cohort of hemodialysis patients by means of deep recurrent neural networks. Artif. Intell. Med. 2020, 107, 101898. [Google Scholar] [CrossRef] [PubMed]
- Palmer, S.C.; Navaneethan, S.D.; Craig, J.C.; Johnson, D.W.; Tonelli, M.; Garg, A.X.; Pellegrini, F.; Ravani, P.; Jardine, M.; Perkovic, V.; et al. Meta-analysis: Erythropoiesis-stimulating agents in patients with chronic kidney disease. Ann. Intern. Med. 2010, 153, 23–33. [Google Scholar] [CrossRef] [PubMed]
- Bachmann, F.; Koch, G.; Pfister, M.; Szinnai, G.; Schropp, J. OptiDose: Computing the Individualized Optimal Drug Dosing Regimen Using Optimal Control. J. Optim. Theory Appl. 2021, 189, 46–65. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.Y.; Lee, T.C.; Liao, W.T.; Hsu, C.C. Multi-head self-attention mechanism enabled individualized hemoglobin prediction and treatment recommendation systems in anemia management for hemodialysis patients. Heliyon 2023, 9, e12613. [Google Scholar] [CrossRef]
- Rogg, S.; Fuertinger, D.H.; Volkwein, S.; Kappel, F.; Kotanko, P. Optimal EPO dosing in hemodialysis patients using a non-linear model predictive control approach. J. Math. Biol. 2019, 79, 2281–2313. [Google Scholar] [CrossRef]
- Jörg, D.J.; Fuertinger, D.H.; Kotanko, P. Mechanisms of hemoglobin cycling in anemia patients treated with erythropoiesisstimulating agents. PLoS Comput. Biol. 2023, 19, e1010850. [Google Scholar] [CrossRef] [PubMed]
- Kalicki, R.M.; Uehlinger, D.E. Red Cell Survival in Relation to Changes in the Hematocrit: More Important than You Think. Blood Purif. 2008, 26, 355–360. [Google Scholar] [CrossRef]
- Gilbertson, D.T.; Hu, Y.; Peng, Y.; Maroni, B.J.; Wetmore, J.B. Variability in hemoglobin levels in hemodialysis patients in the current era: A retrospective cohort study. Clin. Nephrol. 2017, 88, 254–263. [Google Scholar] [CrossRef] [PubMed]
- Portolés, J.; Martín, L.; Broseta, J.J.; Cases, A. Anemia in Chronic Kidney Disease: From Pathophysiology and Current Treatments, to Future Agents. Front. Med. 2021, 8, 642296. [Google Scholar] [CrossRef]
- Gaweda, A.E.; Goldsmith, L.J.; Brier, M.E.; Aronoff, G.R. Iron, inflammation, dialysis adequacy, nutritional status, and hyperparathyroidism modify erythropoietic response. Clin. J. Am. Soc. Nephrol. 2010, 5, 576–581. [Google Scholar] [CrossRef] [PubMed]
- Karimi, Z.; Raeisi Shahraki, H.; Mohammadian-Hafshejani, A. Erythropoiesis-stimulating agents and cardiovascular mortality: A systematic review and meta-analysis of 17 studies and 372,156 hemodialysis patients. Int. J. Cardiol. Cardiovasc. Risk Prev. 2023, 19, 200220. [Google Scholar] [CrossRef] [PubMed]
- Suttorp, M.M.; Hoekstra, T.; Mittelman, M.; Ott, I.; Krediet, R.T.; Dekker, F.W.; Putter, H. Treatment with high dose of erythropoiesis-stimulating agents and mortality: Analysis with a sequential Cox approach and a marginal structural model. Pharmacoepidemiol. Drug Saf. 2015, 24, 1068–1075. [Google Scholar] [CrossRef]
- Weinhandl, E.D.; Gilbertson, D.T.; Collins, A.J. Association of mean weekly epoetin alfa dose with mortality risk in a retrospective cohort study of medicare hemodialysis patients. Am. J. Nephrol. 2011, 34, 298–308. [Google Scholar] [CrossRef] [PubMed]
- Handelman, G.J.; Kotanko, P.; Cisternas, M.G.; Hoenich, N.; Usvyat, L.; Kuhlmann, M.; Levin, N.W. Hospitalization and mortality in hemodialysis patients: Association with hemoglobin variability. Blood Purif. 2013, 35, 247–257. [Google Scholar] [CrossRef] [PubMed]
- Eckardt, K.U.; Kim, J.; Kronenberg, F.; Aljama, P.; Anker, S.D.; Canaud, B.; Molemans, B.; Stenvinkel, P.; Schernthaner, G.; Ireland, E.; et al. Hemoglobin variability does not predict mortality in european hemodialysis patients. J. Am. Soc. Nephrol. 2010, 21, 1765–1775. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Goodkin, D.A.; Fuller, D.S.; Robinson, B.M.; Combe, C.; Fluck, R.; Mendelssohn, D.; Akizawa, T.; Pisoni, R.L.; Port, F.K. Naturally occurring higher hemoglobin concentration does not increase mortality among hemodialysis patients. J. Am. Soc. Nephrol. 2011, 22, 358–365. [Google Scholar] [CrossRef]
- Ofsthun, N.; LaBrecque, J.; Lacson, E.; Keen, M.; Lazarus, J.M. The effects of higher hemoglobin levels on mortality and hospitalization in hemodialysis patients. Kidney Int. 2003, 63, 1908–1914. [Google Scholar] [CrossRef]
- Weinhandl, E.D.; Peng, Y.; Gilbertson, D.T.; Bradbury, B.D.; Collins, A.J. Hemoglobin variability and mortality: Confounding by disease severity. Am. J. Kidney Dis. 2011, 57, 255–265. [Google Scholar] [CrossRef]
- Ng, L.J.; Chen, F.; Pisoni, R.L.; Krishnan, M.; Mapes, D.; Keen, M.; Bradbury, B.D. Hospitalization risks related to vascular access type among incident US hemodialysis patients. Nephrol. Dial. Transplant. 2011, 26, 3659–3666. [Google Scholar] [CrossRef]
- Morena, M.; Jaussent, A.; Chalabi, L.; Leray-Moragues, H.; Chenine, L.; Debure, A.; Thibaudin, D.; Azzouz, L.; Patrier, L.; Maurice, F.; et al. Treatment tolerance and patient-reported outcomes favor online hemodiafiltration compared to high-flux hemodialysis in the elderly. Kidney Int. 2017, 91, 1495–1509. [Google Scholar] [CrossRef]
- Ok, E.; Asci, G.; Toz, H.; Ok, E.S.; Kircelli, F.; Yilmaz, M.; Hur, E.; Demirci, M.S.; Demirci, C.; Duman, S.; et al. Mortality and cardiovascular events in online haemodiafiltration (OL-HDF) compared with high-flux dialysis: Results from the Turkish OL-HDF Study. Nephrol. Dial. Transplant. 2013, 28, 192–202. [Google Scholar] [CrossRef] [PubMed]
- Blankestijn, P.J.; Vernooij, R.W.; Hockham, C.; Strippoli, G.F.; Canaud, B.; Hegbrant, J.; Barth, C.; Covic, A.; Cromm, K.; Cucui, A.; et al. Effect of Hemodiafiltration or Hemodialysis on Mortality in Kidney Failure. N. Engl. J. Med. 2023, 389, 700–709. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, C.R.; Hornig, C.; Canaud, B. Systematic review to compare the outcomes associated with the modalities of expanded hemodialysis (HDx) versus high-flux hemodialysis and/or hemodiafiltration (HDF) in patients with end-stage kidney disease (ESKD). Semin. Dial. 2023, 36, 86–106. [Google Scholar] [CrossRef] [PubMed]


| Exposure Groups | Significance * | ||||
|---|---|---|---|---|---|
| Characteristics | Whole Sample (n = 20,209) | ACM Group (n = 3108) | Reference Group (n = 17,101) | p-Value | Effect Size |
| n (%), Mean (St.D.), or Median (IQR) | |||||
| Age | 65.3 (14.5) | 67.8 (14.4) | 64.8 (14.4) | <0.001 | 0.0107 |
| Men | 11,962 (59.2) | 1945 (62.6) | 10,017 (58.6) | <0.001 | 0.0234 |
| BMI | 26.8 (6.5) | 26.4 (5.4) | 26.9 (6.7) | <0.001 | 0.0015 |
| Dialysis vintage (years) | 2.03 (4.7) | 2.8 (5.26) | 1.87 (4.59) | <0.001 | 0.2672 |
| Vascular access | <0.001 | 0.1280 | |||
| Catheter or graft | 5578 (28.2) | 592 (19.0) | 4986 (29.9) | ||
| Arteriovenous fistula | 14,188 (71.8) | 2517 (81.0) | 11,671 (70.1) | ||
| Missing | 419 (2.1) | 0 (0) | 419 (2.5) | ||
| Kt/V | 1.6 (0.4) | 1.9 (0.4) | 1.6 (0.4) | <0.001 | 0.2554 |
| Treatment time (minutes) | 241.8 (13.1) | 243.7 (13.1) | 241.5 (13.1) | <0.001 | 0.0169 |
| Hemoglobin (g/dL) | 11.1 (1.2) | 11.4 (1.1) | 11.0 (1.2) | <0.001 | 0.0188 |
| Albumin (g/dL) | 3.9 (0.4) | 4.0 (0.5) | 3.9 (0.4) | <0.001 | 0.0075 |
| Ferritin (ng/mL) | 558.8 (436.5) | 567.0 (349.7) | 557.3 (450.8) | 0.176 | 0.0037 |
| Phosphate (mg/dL) | 4.7 (1.4) | 4.3 (1.1) | 4.8 (1.4) | <0.001 | 0.0269 |
| Leukocytes (103/µL) | 7883.2 (41,545.4) | 6582.5 (1824.9) | 8123.0 (45,203.6) | <0.001 | 0.0286 |
| C-reactive protein (mg/L) | 13.6 (22.3) | 12.1 (17.0) | 13.8 (23.1) | <0.001 | 0.0030 |
| Transferrin saturation (%) | 29.9 (12.8) | 32.2 (11.9) | 29.5 (12.9) | <0.001 | 0.0007 |
| MCV (fL) | 94.3 (6.5) | 95.1 (5.9) | 94.1 (6.6) | <0.001 | 0.0288 |
| MCH (pg/cell) | 32.9 (43.1) | 32.9 (0.8) | 32.9 (46.9) | 0.874 | 0.0044 |
| Serum sodium (mmol/L) | 138.1 (4.0) | 138.3 (2.6) | 138.1 (4.1) | 0.0042 | 0.0042 |
| Serum potassium (meq/L) | 4.9 (0.9) | 5.0 (0.6) | 4.9 (0.9) | 0.0066 | 0.0066 |
| Serum calcium (mg/dL) | 8.8 (1.3) | 9.0 (0.6) | 8.8 (1.4) | 0.0060 | 0.0059 |
| Cerebrovascular disease | 2750 (13.6) | 486 (15.6) | 2264 (13.2) | <0.001 | 0.0401 |
| Chronic pulmonary disease | 2197 (10.9) | 398 (12.8) | 1799 (10.5) | <0.001 | 0.0417 |
| Congestive heart failure | 4376 (21.7) | 696 (22.4) | 3680 (21.5) | 0.287 | 0.0075 |
| Connective tissue disorder | 332 (1.6) | 43 (1.4) | 289 (1.7) | 0.246 | 0.0105 |
| Coronary artery disease | 4199 (20.8) | 621 (20.0) | 3578 (20.9) | 0.243 | 0.0152 |
| Dementia | 313 (1.5) | 53 (1.7) | 260 (1.5) | 0.491 | 0.0115 |
| Diabetes without complication | 6155 (30,5) | 214 (6.9) | 871 (5.1) | <0.001 | 0.0052 |
| Diabetes with organ damage | 5070 (25.1) | 921 (29.6) | 4149 (24.3) | <0.001 | 0.0560 |
| Hemiplegia | 157 (0.8) | 20 (0.6) | 137 (0.8) | 0.418 | 0.0157 |
| Mild liver disease | 2002 (9.9) | 385 (12.4) | 1617 (9.5) | <0.001 | 0.0419 |
| Moderate/severe liver disease | 111 (0.5) | 16 (0.5) | 95 (0.6) | 0.880 | 0.0179 |
| Peptic ulcer disease | 1026 (5.1) | 152 (4.9) | 874 (5.1) | 0.638 | 0.0125 |
| Peripheral Vascular Disease | 3769 (18.7) | 740 (23.8) | 3029 (17.7) | <0.001 | 0.0506 |
| Exposure Groups | Significance * | |||||
|---|---|---|---|---|---|---|
| Characteristics | Whole Sample (n = 5071) | ACM Group (n = 1952) | ACM Unmatched (n = 1167) | Reference Group (n = 1952) | p-Value | Effect Size |
| N (%) or Mean (St.D.) | ||||||
| Age | 66.1 (14.7) | 67.6 (14.5) | 68.3 (14.3) | 63.3 (14.8) | <0.001 | 0.0413 |
| Men | 3165 (62.7) | 1243 (64.0) | 701 (60.1) | 1221 (62.9) | 0.09 | 0.0111 |
| BMI | 26.7 (5.6) | 26.4 (5.3) | 26.3 (5.5) | 27.2 (6.0) | <0.001 | 0.0010 |
| Dialysis vintage | 2.03 (4.59) | 1.25 (2.98) | 5.29 (5.51) | 1.05 (3.28) | <0.001 | 0.0004 |
| Vascular access | <0.001 | 0.1410 | ||||
| Catheter or graft | 1241 (24.8) | 420 (21.6) | 172 (14.7) | 649 (34.2) | ||
| Arteriovenous fistula | 3766 (75.2) | 1522 (78.4) | 995 (85.3) | 1249 (65.8) | ||
| Missing | 44 (0.9) | 0 (0) | 0 (0) | 44 (2.3) | ||
| Kt/V | 1.8 (0.4) | 1.9 (0.4) | 1.9 (0.4) | 1.5 (0.4) | <0.001 | 0.3300 |
| Treatment time (minutes) | 242.2 (13.3) | 243.9 (11.8) | 243.2 (15.0) | 239.8 (13.2) | <0.001 | 0.0170 |
| Hemoglobin (g/dL) | 11.3 (1.0) | 11.3 (0.9) | 11.6 (1.2) | 11.2 (0.9) | <0.001 | 0.0061 |
| Albumin (g/dL) | 3.9 (0.4) | 3.9 (0.5) | 4.0 (0.4) | 3.9 (0.4) | <0.001 | 0.0000 |
| Ferritin (ng/mL) | 520.5 (371.9) | 561.0 (362.0) | 577.0 (328.2) | 443.4 (394.3) | <0.001 | 0.0460 |
| Phosphate (mg/dL) | 4.4 (1.1) | 4.3 (1.1) | 4.2 (1.1) | 4.6 (1.1) | <0.001 | 0.0358 |
| Leukocytes (103/µL) | 6738.9 (2148.4) | 6685.2 (1833.5) | 6411.6 (1798.3) | 6992.9 (2569.3) | <0.001 | 0.0094 |
| C-reactive protein (mg/L) | 11.8 (16.6) | 12.4 (18.0) | 11.8 (15.2) | 11.3 (16.1) | 0.213 | 0.0020 |
| Transferrin saturation (%) | 30.3 (11.8) | 31.8 (11.6) | 32.9 (12.3) | 27.6 (11.1) | <0.001 | 0.0641 |
| MCV (fL) | 94.3 (6.1) | 95.2 (5.9) | 94.9 (5.9) | 92.9 (6.3) | <0.001 | 0.0663 |
| MCH (pg/cell) | 32.8 (1.0) | 32.9 (0.9) | 32.9 (0.8) | 32.8 (1.1) | <0.001 | 0.0049 |
| Serum sodium (mmol/L) | 138.1 (3.1) | 138.2 (2.6) | 138.4 (2.7) | 137.9 (3.7) | <0.001 | 0.0044 |
| Serum potassium (meq/L) | 4.9 (0.6) | 4.9 (0.6) | 5.0 (0.6) | 4.8 (0.6) | <0.001 | 0.0137 |
| Serum calcium (mg/dL) | 8.9 (0.6) | 8.9 (0.6) | 9.0 (0.7) | 8.8 (0.6) | <0.001 | 0.0137 |
| Cerebrovascular disease | 736 (14.6) | 296 (15.2) | 192 (16.5) | 248 (12.8) | 0.011 | 0.0348 |
| Chronic pulmonary disease | 594 (11.8) | 261 (13.4) | 140 (12.0) | 193 (9.9) | 0.003 | 0.0535 |
| Congestive heart failure | 1117 (22.1) | 425 (21.9) | 275 (23.6) | 417 (21.5) | 0.377 | 0.0043 |
| Connective tissue disorder | 74 (1.5) | 25 (1.3) | 18 (1.5) | 31 (1.6) | 0.703 | 0.0108 |
| Coronary artery disease | 964 (19.1) | 362 (18.6) | 260 (22.3) | 342 (17.6) | 0.005 | 0.0127 |
| Dementia | 84 (1.7) | 37 (1.9) | 16 (1.4) | 31 (1.6) | 0.507 | 0.0098 |
| Diabetes without complication | 332 (6.6) | 141 (7.3) | 73 (6.3) | 118 (6.1) | 0.291 | 0.0226 |
| Diabetes with organ damage | 1454 (28.8) | 612 (31.5) | 311 (26.6) | 531 (27.3) | 0.003 | 0.0450 |
| Hemiplegia | 31 (0.6) | 9 (0.5) | 11 (0.9) | 11 (0.6) | 0.239 | 0.0036 |
| Mild liver disease | 549 (10.9) | 204 (10.5) | 179 (15.3) | 166 (8.5) | <0.001 | 0.0324 |
| Moderate/severe liver disease | 30 (0.6) | 11 (0.6) | 5 (0.4) | 14 (0.7) | 0.578 | 0.0064 |
| Peptic ulcer disease | 239 (4.7) | 88 (4.5) | 66 (5.7) | 85 (4.4) | 0.232 | 0.0025 |
| Peripheral vascular disease | 1087 (21.5) | 424 (21.8) | 318 (27.2) | 345 (17.8) | <0.001 | 0.0502 |
| Group | Incidence Rate (Events/100 Person/Years) | Incidence Rate Difference (Events/100 Person/Years) | p-Value |
|---|---|---|---|
| Before matching | |||
| Whole sample | 80.9 (95% CI: 79.6–82.3) | - | - |
| ACM group | 71.3 (95% CI: 68.0–74.6) | - | - |
| Reference group | 82.6 (95% CI: 81.2–84.2) | 11.4 (95% CI: 7.6–15.2) | <0.001 |
| After matching | |||
| Matched sample | 80.9 (95% CI: 77.8–84.1) | - | - |
| ACM group | 74.3 (95% CI: 70.2–78.7) | - | - |
| Reference group | 86.7 (95% CI: 82.4–91.6) | 12.6 (95% CI: 6.3–18.9) | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Garbelli, M.; Baro Salvador, M.E.; Rincon Bello, A.; Samaniego Toro, D.; Bellocchio, F.; Fumagalli, L.; Chermisi, M.; Apel, C.; Petrovic, J.; Kendzia, D.; et al. Usage of the Anemia Control Model Is Associated with Reduced Hospitalization Risk in Hemodialysis. Biomedicines 2024, 12, 2219. https://doi.org/10.3390/biomedicines12102219
Garbelli M, Baro Salvador ME, Rincon Bello A, Samaniego Toro D, Bellocchio F, Fumagalli L, Chermisi M, Apel C, Petrovic J, Kendzia D, et al. Usage of the Anemia Control Model Is Associated with Reduced Hospitalization Risk in Hemodialysis. Biomedicines. 2024; 12(10):2219. https://doi.org/10.3390/biomedicines12102219
Chicago/Turabian StyleGarbelli, Mario, Maria Eva Baro Salvador, Abraham Rincon Bello, Diana Samaniego Toro, Francesco Bellocchio, Luca Fumagalli, Milena Chermisi, Christian Apel, Jovana Petrovic, Dana Kendzia, and et al. 2024. "Usage of the Anemia Control Model Is Associated with Reduced Hospitalization Risk in Hemodialysis" Biomedicines 12, no. 10: 2219. https://doi.org/10.3390/biomedicines12102219
APA StyleGarbelli, M., Baro Salvador, M. E., Rincon Bello, A., Samaniego Toro, D., Bellocchio, F., Fumagalli, L., Chermisi, M., Apel, C., Petrovic, J., Kendzia, D., Ion Titapiccolo, J., Yeung, J., Barbieri, C., Mari, F., Usvyat, L., Larkin, J., Stuard, S., & Neri, L. (2024). Usage of the Anemia Control Model Is Associated with Reduced Hospitalization Risk in Hemodialysis. Biomedicines, 12(10), 2219. https://doi.org/10.3390/biomedicines12102219







