Comparative Analysis of Stromal Vascular Fraction and Alternative Mechanisms in Bone Fracture Stimulation to Bridge the Gap between Nature and Technological Advancement: A Systematic Review
Abstract
:1. Introduction
2. Materials and Methods
2.1. Literature Search Strategy
2.2. Quality Assessment
2.3. Ethical Considerations
3. Results
4. Discussion
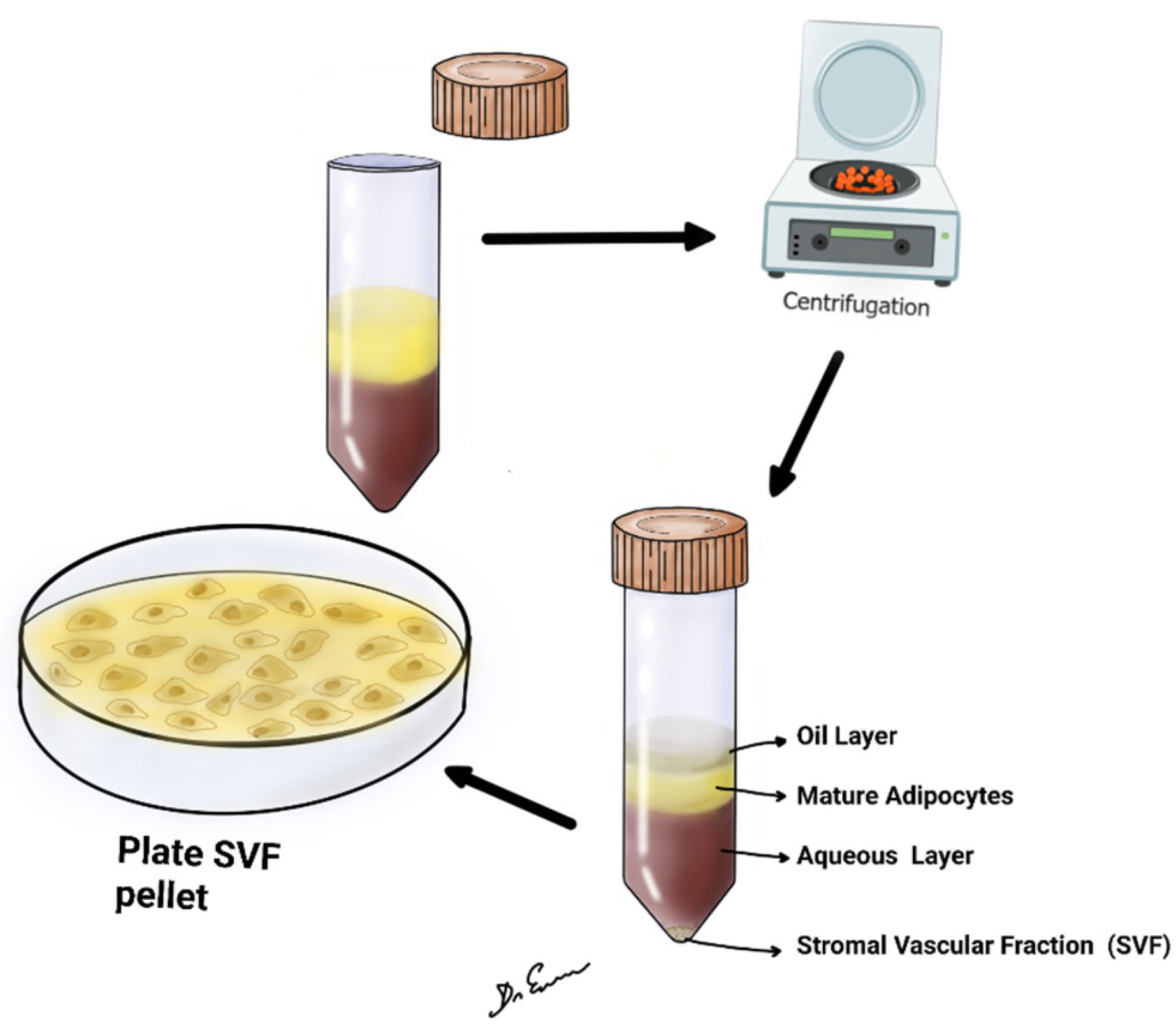
4.1. Steps of SVF
4.2. Limitations of the Study
4.2.1. Predominance of Alternative Methods in Literature
4.2.2. Scarcity of Human Studies on SVF
4.2.3. Potential Publication Bias and Generalizability Concerns
4.2.4. Developmental Stage of SVF Research
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Bolander, M.E. Regulation of fracture repair by growth factors. Proc. Soc. Exp. Biol. Med. 1992, 200, 165–170. [Google Scholar] [CrossRef]
- Byock, I. The Best Care Possible: A Physician’s Quest to Transform Care through the End of Life; Avery: New York, NY, USA, 2012; p. 1. [Google Scholar]
- Marsh, D.; Li, G. The biology of fracture healing: Optimizing outcome. Br. Med. Bull. 1999, 55, 856–869. [Google Scholar] [CrossRef]
- Schmidt, I.; Albert, J.; Ritthaler, M.; Papastavrou, A.; Steinmann, P. Bone fracture healing within a continuum bone remodelling framework. Comput. Methods Biomech. Biomed. Eng. 2022, 25, 1040–1050. [Google Scholar] [CrossRef] [PubMed]
- Marsell, R.; Einhorn, T.A. The biology of fracture healing. Injury 2011, 42, 551–555. [Google Scholar] [CrossRef] [PubMed]
- Yamagiwa, H.; Endo, N. Bone fracture and the healing mechanisms. Histological aspect of fracture healing. Primary and secondary healing. Clin. Calcium. 2009, 19, 627–633. [Google Scholar] [PubMed]
- Loi, F.; Córdova, L.A.; Pajarinen, J.; Lin, T.H.; Yao, Z.; Goodman, S.B. Inflammation, fracture and bone repair. Bone 2016, 86, 119–130. [Google Scholar] [CrossRef] [PubMed]
- Veis, D.J.; O’Brien, C.A. Osteoclasts, Master Sculptors of Bone. Annu. Rev. Pathol. 2023, 18, 257–281. [Google Scholar] [CrossRef]
- Goldstein, C.; Sprague, S.; Petrisor, B. Electrical Stimulation for Fracture Healing: Current Evidence. J. Orthop. Trauma 2010, 24, S62–S65. [Google Scholar] [CrossRef] [PubMed]
- Yoshida, T.; Kim, W.C.; Kubo, T. Bone fracture and the healing mechanisms. Fracture treatment using electrical stimulation. Clin. Calcium. 2009, 19, 709–717. [Google Scholar]
- Victoria, G.; Petrisor, B.; Drew, B.; Dick, D. Bone stimulation for fracture healing: What’s all the fuss? Indian J. Orthop. 2009, 43, 117–120. [Google Scholar] [CrossRef]
- Watanabe, Y.; Matsushita, T.; Bhandari, M.; Zdero, R.; Schemitsch, E.H. Ultrasound for fracture healing: Current evidence. J. Orthop. Trauma 2010, 24, S56–S61. [Google Scholar] [CrossRef]
- Ma, Q.; Miri, Z.; Haugen, H.J.; Moghanian, A.; Loca, D. Significance of mechanical loading in bone fracture healing, bone regeneration, and vascularization. J. Tissue Eng. 2023, 14, 20417314231172573. [Google Scholar] [CrossRef]
- Frost, H.M. Wolff’s Law and bone’s structural adaptations to mechanical usage: An overview for clinicians. Angle Orthod. 1994, 64, 175–188. [Google Scholar]
- Goodman, S.; Aspenberg, P. Effects of mechanical stimulation on the differentiation of hard tissues. Biomaterials 1993, 14, 563–569. [Google Scholar] [CrossRef]
- Komrakova, M.; Sehmisch, S.; Tezval, M.; Ammon, J.; Lieberwirth, P.; Sauerhoff, C.; Trautmann, L.; Wicke, M.; Dullin, C.; Stuermer, K.M.; et al. Identification of a vibration regime favorable for bone healing and muscle in estrogen-deficient rats. Calcif. Tissue Int. 2013, 92, 509–520. [Google Scholar] [CrossRef] [PubMed]
- Campos, M.S.; Volpon, J.B.; Ximenez, J.P.B.; Franttini, A.P.; Dalloul, C.E.; Sousa-Neto, M.D.; Silva, R.A.; Kacena, M.A.; Zamarioli, A. Vibration therapy as an effective approach to improve bone healing in diabetic rats. Front. Endocrinol. 2022, 13, 909317. [Google Scholar] [CrossRef] [PubMed]
- Kanakaris, N.K.; Paliobeis, C.; Nlanidakis, N.; Giannoudis, P.V. Biological enhancement of tibial diaphyseal aseptic non-unions: The efficacy of autologous bone grafting, BMPs and reaming by-products. Injury 2007, 38 (Suppl. S2), S65–S75, Erratum in Injury 2007, 38, 1224. [Google Scholar] [CrossRef] [PubMed]
- Van Lieshout, E.M.M.; Den Hartog, D. Effect of platelet-rich plasma on fracture healing. Injury 2021, 52, S58–S66. [Google Scholar] [CrossRef] [PubMed]
- Wojda, S.J.; Donahue, S.W. Parathyroid hormone for bone regeneration. J. Orthop. Res. 2018, 36, 2586–2594. [Google Scholar] [CrossRef] [PubMed]
- Agaverdiev, M.; Shamsov, B.; Mirzoev, S.; Vardikyan, A.; Ramirez, M.E.; Nurmukhametov, R.; Beilerli, A.; Zhang, B.; Gareev, I.; Pavlov, V. MiRNA regulated therapeutic potential of the stromal vascular fraction: Current clinical applications—A systematic review. Noncoding RNA Res. 2022, 8, 146–154. [Google Scholar] [CrossRef] [PubMed]
- Bora, P.; Majumdar, A.S. Adipose tissue-derived stromal vascular fraction in regenerative medicine: A brief review on biology and translation. Stem Cell Res. Ther. 2017, 8, 145. [Google Scholar] [CrossRef] [PubMed]
- Montemurro, N.; Ortenzi, V.; Naccarato, G.A.; Perrini, P. Angioleiomyoma of the knee: An uncommon cause of leg pain. A systematic review of the literature. Interdiscip. Neurosurg. 2020, 22, 10087. [Google Scholar] [CrossRef]
- Onoi, Y.; Matsumoto, T.; Sobajima, S.; Tsubosaka, M.; Hayashi, S.; Matsushita, T.; Iwaguro, H.; Kuroda, R. Clinical use of autologous adipose-derived stromal vascular fraction cell injections for hip osteoarthritis. Regen. Ther. 2023, 24, 94–102. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.S.; Oh, S.M.; Suh, D.S.; Tak, D.H.; Kwon, Y.B.; Koh, Y.G. Cartilage lesion size and number of stromal vascular fraction (SVF) cells strongly influenced the SVF implantation outcomes in patients with knee osteoarthritis. J. Exp. Orthop. 2023, 10, 28. [Google Scholar] [CrossRef] [PubMed]
- Saxer, F.; Scherberich, A.; Todorov, A.; Studer, P.; Miot, S.; Schreiner, S.; Güven, S.; Tchang, L.A.; Haug, M.; Heberer, M.; et al. Implantation of Stromal Vascular Fraction Progenitors at Bone Fracture Sites: From a Rat Model to a First-in-Man Study. Stem Cells 2016, 34, 2956–2966. [Google Scholar] [CrossRef]
- Urlaub, K.M.; Ranganathan, K.; Lynn, J.V.; Luby, A.O.; Patrick, L.N.; Nelson, N.S.; Donneys, A.M.; Buchman, S.R. Intraoperative Stromal Vascular Fraction Therapy Improves Histomorphometric and Vascular Outcomes in Irradiated Mandibular Fracture Repair. Plast. Reconstr. Surg. 2021, 147, 865–874. [Google Scholar] [CrossRef]
- Sananta, P.; Dradjat, R.S.; Rosandi, R.D.; Siahaan, L.D. TGF-1 biomarker level evaluation on fracture healing in a murine model with a bone defect after stromal vascular fraction application. Med. Glas 2022, 19, 63–67. [Google Scholar]
- Dradjat, R.S.; Sananta, P.; Rosandi, R.D.; Siahaan, L.D. Osteocalcin biomarker level evaluation on fracture healing with bone defect after stromal vascular fraction application in murine model. Ann. Med. Surg. 2021, 71, 103020. [Google Scholar] [CrossRef] [PubMed]
- Kamenaga, T.; Kuroda, Y.; Nagai, K.; Tsubosaka, M.; Takashima, Y.; Kikuchi, K.; Fujita, M.; Ikuta, K.; Anjiki, K.; Maeda, T.; et al. Cryopreserved human adipose-derived stromal vascular fraction maintains fracture healing potential via angiogenesis and osteogenesis in an immunodeficient rat model. Stem Cell Res. Ther. 2021, 12, 110. [Google Scholar] [CrossRef] [PubMed]
- Dykstra, J.A.; Facile, T.; Patrick, R.J.; Francis, K.R.; Milanovich, S.; Weimer, J.M.; Kota, D.J. Concise Review: Fat and Furious: Harnessing the Full Potential of Adipose-Derived Stromal Vascular Fraction. Stem Cells Transl. Med. 2017, 6, 1096–1108. [Google Scholar] [CrossRef] [PubMed]
- Zuk, P.A.; Zhu, M.; Mizuno, H.; Huang, J.; Futrell, J.W.; Katz, A.J.; Benhaim, P.; Lorenz, H.P.; Hedrick, M.H. Multilineage cells from human adipose tissue: Implications for cell-based therapies. Tissue Eng. 2001, 7, 211–228. [Google Scholar] [CrossRef] [PubMed]
- Ghigliotti, G.; Barisione, C.; Garibaldi, S.; Fabbi, P.; Brunelli, C.; Spallarossa, P.; Altieri, P.; Rosa, G.; Spinella, G.; Palombo, D.; et al. Adipose Tissue Immune Response: Novel Triggers and Consequences for Chronic Inflammatory Conditions. Inflammation 2014, 37, 1337–1353. [Google Scholar] [CrossRef]
- Gornitsky, J.; Viezel-Mathieu, A.; Alnaif, N.; Azzi, A.J.; Gilardino, M.S. A systematic review of the effectiveness and complications of fat grafting in the facial region. JPRAS Open 2019, 19, 87–97. [Google Scholar] [CrossRef] [PubMed]
- Duhoux, A.; Chennoufi, M.; Lantieri, L.; Hivelin, M. Complications of fat grafts growth after weight gain: Report of a severe diplopia. J. Plast. Reconstr. Aesthetic Surg. 2013, 66, 987–990. [Google Scholar]
- Mitchell, J.B.; McIntosh, K.; Zvonic, S.; Garrett, S.; Floyd, Z.E.; Kloster, A. Immunophenotype of human adipose derived cells: Temporal changes in stromal-associated and stem cell-associated markers. Stem Cells 2006, 24, 376–385. [Google Scholar] [CrossRef] [PubMed]
- Saeed, K.; Khan, F.A.; Qudus, S.B.A.; Javed, S. Autologous Fat Grafting—A Step Forward in Wound Management. Int. J. Low. Extrem. Wounds 2022, 21, 647–650. [Google Scholar] [CrossRef] [PubMed]
- Kao, Y.; Chen, K.; Lee, K.; Hsu, C.; Chien, Y. Pulmonary Fat Embolism following Liposuction and Fat Grafting: A Review of Published Cases. Healthcare 2022, 11, 1391. [Google Scholar] [CrossRef]
- Debnath, T.; Chelluri, L.K. Standardization and quality assessment for clinical grade mesenchymal stem cells from human adipose tissue. Hematol. Transfus. Cell Ther. 2019, 41, 7–16. [Google Scholar] [CrossRef]
- Haack-Sørensen, M.; Follin, B.; Juhl, M.; Brorsen, S.K.; Søndergaard, R.H.; Kastrup, J.; Ekblond, A. Culture expansion of adipose derived stromal cells. A closed automated Quantum Cell Expansion System compared with manual flask-based culture. J. Transl. Med. 2016, 14, 319. [Google Scholar] [CrossRef]
- Khalifeh, J.M.; Zohny, Z.; MacEwan, M.; Stephen, M.; Johnston, W.; Gamble, P.; Zeng, Y.; Yan, Y.; Ray, W.Z. Electrical Stimulation and Bone Healing: A Review of Current Technology and Clinical Applications. IEEE Rev. Biomed. Eng. 2018, 11, 217–232. [Google Scholar] [CrossRef]
- Barbosa, F.; Garrudo, F.F.F.; Marques, A.C.; Cabral, J.M.S.; Morgado, J.; Ferreira, F.C.; Silva, J.C. Novel Electroactive Mineralized Polyacrylonitrile/PEDOT:PSS Electrospun Nanofibers for Bone Repair Applications. Int. J. Mol. Sci. 2023, 24, 13203. [Google Scholar] [CrossRef]
- Palanisamy, P.; Alam, M.; Li, S.; Chow, S.K.; Zheng, Y.P. Low-Intensity Pulsed Ultrasound Stimulation for Bone Fractures Healing: A Review. J. Ultrasound Med. 2022, 41, 547–563. [Google Scholar] [CrossRef]
- Song, L. Effects of Exercise or Mechanical Stimulation on Bone Development and Bone Repair. Stem Cells Int. 2022, 28, 5372229. [Google Scholar] [CrossRef]
- Singh, N.A.; Quine, S.; Clemson, L.M.; Williams, E.J.; Williamson, D.A.; Stavrinos, T.M.; Grady, J.N.; Perry, T.J.; Lloyd, B.D.; Smith, E.U.R. Effects of high-intensity progressive resistance training and targeted multidisciplinary treatment of frailty on mortality and nursing home admissions after hip fracture: A randomized controlled trial. J. Am. Med. Dir. Assoc. 2012, 13, 24–30. [Google Scholar] [CrossRef]
- Massari, L.; Benazzo, F.; Falez, F.; Perugia, D.; Pietrogrande, L.; Setti, S.; Osti, R.; Vaienti, E.; Ruosi, C.; Cadossi, R. Biophysical stimulation of bone and cartilage: State of the art and future perspectives. Int. Orthop. 2019, 43, 539–551. [Google Scholar] [CrossRef] [PubMed]
- Wu, V.; Bravenboer, N.; Ten Bruggenkate, C.M.; Helder, M.N.; Schulten, E.A. Long-Term Safety of Bone Regeneration Using Autologous Stromal Vascular Fraction and Calcium Phosphate Ceramics: A 10-Year Prospective Cohort Study. Stem Cells Transl. Med. 2023, 12, 617–630. [Google Scholar] [CrossRef]
- Tarantino, U.; Cerocchi, I.; Celi, M.; Scialdoni, A.; Saturnino, L.; Gasbarra, E. Pharmacological agents and bone healing. Clin. Cases Miner. Bone Metab. 2009, 6, 144–148. [Google Scholar] [PubMed]
- AI-Aql, Z.S.; Alagl, A.S.; Graves, D.T.; Gerstenfeld, L.C.; Einhorn, T.A. Molecular mechanisms controlling bone formation during fracture healing and distraction osteogenesis. J. Dent. Res. 2008, 87, 107–118. [Google Scholar] [CrossRef] [PubMed]
- Pountos, I.; Georgouli, T.; Blokhuis, T.J.; Pape, H.C.; Giannoudis, P.V. Pharmacological agents and impairment of fracture healing: What is the evidence? Injury 2008, 39, 384–394. [Google Scholar] [CrossRef]
- Karamian, B.A.; Schroeder, G.D.; Lambrechts, M.J.; Canseco, J.A.; Oner, C.; Vialle, E.; Rajasekaran, S.; Dvorak, M.R.; Benneker, L.M.; Kandziora, F.; et al. An international validation of the AO spine subaxial injury classification system. Eur. Spine J. 2023, 32, 46–54. [Google Scholar] [CrossRef]
- Copcu, H.E.; Oztan, S. Not Stromal Vascular Fraction (SVF) or Nanofat, but Total Stromal-Cells (TOST): A New Definition. Systemic Review of Mechanical Stromal-Cell Extraction Techniques. Tissue Eng. Regen. Med. 2021, 18, 25–36. [Google Scholar] [CrossRef]
- Pak, J.; Lee, J.H.; Pak, N.J.; Park, K.S.; Jeon, J.H.; Jeong, B.C.; Lee, S.H. Clinical Protocol of Producing Adipose Tissue-Derived Stromal Vascular Fraction for Potential Cartilage Regeneration. J. Vis. Exp. 2018, 139, 58363. [Google Scholar]
- Francis, S.L.; Duchi, S.; Onofrillo, C.; Di Bella, C.; Choong, P.F.M. Adipose-Derived Mesenchymal Stem Cells in the Use of Cartilage Tissue Engineering: The Need for a Rapid Isolation Procedure. Stem Cells Int. 2018, 2018, 8947548. [Google Scholar] [CrossRef] [PubMed]
- Busato, A.; De Francesco, F.; Biswas, R.; Mannucci, S.; Conti, G.; Fracasso, G.; Conti, A.; Riccio, V.; Riccio, M.; Sbarbati, A. Simple and Rapid Non-Enzymatic Procedure Allows the Isolation of Structurally Preserved Connective Tissue Micro-Fragments Enriched with SVF. Cells 2020, 10, 36. [Google Scholar] [CrossRef] [PubMed]
- Matsuo, F.S.; Cavalcanti de Araújo, P.H.; Mota, R.F.; Carvalho, A.J.R.; de Queiroz, M.S.; de Almeida, B.B.; Ferreira, K.C.d.O.S.; Metzner, R.J.M.; Ferrari, G.D.; Alberici, L.C.; et al. RANKL induces beige adipocyte differentiation in preadipocytes. Am. J. Physiol. Endocrinol. Metab. 2020, 318, E866–E877. [Google Scholar] [CrossRef] [PubMed]
- Contreras, G.A.; Kabara, E.; Brester, J.; Neuder, L.; Kiupel, M. Macrophage infiltration in the omental and subcutaneous adipose tissues of dairy cows with displaced abomasum. J. Dairy Sci. 2015, 98, 6176–6187. [Google Scholar] [CrossRef]
- Dey, A.; Ni, Z.; Johnson, M.S.; Sedger, L.M. A multi-colour confocal microscopy method for identifying and enumerating macrophage subtypes and adherent cells in the stromal vascular fraction of human adipose. J. Immunol. Methods 2021, 491, 112988. [Google Scholar] [CrossRef]
- Dulong, J.; Loisel, S.; Rossille, D.; Léonard, S.; Bescher, N.; Bezier, I.; Latour, M.; Monvoisin, C.; Monnier, D.; Bertheuil, N.; et al. CD40L-expressing CD4+ T cells prime adipose-derived stromal cells to produce inflammatory chemokines. Cytotherapy 2022, 24, 500–507. [Google Scholar] [CrossRef]
- Gulyaeva, O.; Dempersmier, J.; Sul, H.S. Genetic and epigenetic control of adipose development. Biochim. Biophys. Acta Mol. Cell Biol. Lipids 2019, 1864, 3–12. [Google Scholar] [CrossRef] [PubMed]
- Zhu, H.; Ge, J.; Chen, X.; Lu, F.; Cai, J. Mechanical Micronization of Lipoaspirates for Regenerative Therapy. J. Vis. Exp. 2019, 15, 145. [Google Scholar]
- Goncharov, E.N.; Koval, O.A.; Nikolaevich Bezuglov, E.; Ramirez, M.d.J.E.; Engelgard, M.; Igorevich, E.I.; Saporiti, A.; Kotenko, K.V.; Montemurro, N. Stromal Vascular Fraction Therapy for Knee Osteoarthritis: A Systematic Review. Medicina 2023, 59, 2090. [Google Scholar] [CrossRef]
- Goncharov, E.N.; Koval, O.A.; Igorevich, E.I.; Encarnacion Ramirez, M.D.J.; Nurmukhametov, R.; Valentinovich, K.K.; Montemurro, N. Analyzing the Clinical Potential of Stromal Vascular Fraction: A Comprehensive Literature Review. Medicina 2024, 60, 221. [Google Scholar] [CrossRef]
- Hachem, L.D.; Ahuja, C.S.; Fehlings, M.G. Assessment and management of acute spinal cord injury: From point of injury to rehabilitation. J. Spinal Cord Med. 2017, 40, 665–675. [Google Scholar] [CrossRef]
- Montemurro, N.; Murrone, D.; Romanelli, B.; Ierardi, A. Postoperative Textiloma Mimicking Intracranial Rebleeding in a Patient with Spontaneous Hemorrhage: Case Report and Review of the Literature. Case Rep. Neurol. 2020, 12, 7–12. [Google Scholar] [CrossRef] [PubMed]
- Viola, A.; Appiah, J.; Donnally, C.J.; Kim, Y.H.; Shenoy, K. Bone Graft Options in Spinal Fusion: A Review of Current Options and the Use of Mesenchymal Cellular Bone Matrices. World Neurosurg. 2022, 158, 182–188. [Google Scholar] [CrossRef] [PubMed]
- Montemurro, N.; Pierozzi, E.; Inchingolo, A.M.; Pahwa, B.; De Carlo, A.; Palermo, A.; Scarola, R.; Dipalma, G.; Corsalini, M.; Inchingolo, A.D.; et al. New biograft solution, growth factors and bone regenerative approaches in neurosurgery, dentistry, and orthopedics: A review. Eur. Rev. Med. Pharmacol. Sci. 2023, 27, 7653–7664. [Google Scholar]
- Bhattacharjee, M.; Escobar Ivirico, J.L.; Kan, H.M.; Shah, S.; Otsuka, T.; Bordett, R.; Barajaa, M.; Nagiah, N.; Pandey, R.; Nair, L.S.; et al. Injectable amnion hydrogel-mediated delivery of adipose-derived stem cells for osteoarthritis treatment. Proc. Natl. Acad. Sci. USA 2022, 119, e2120968119. [Google Scholar] [CrossRef]
- Navarro, A.; Marín, S.; Riol, N.; Carbonell-Uberos, F.; Miñana, M.D. Fibroblast-Negative CD34-Negative Cells from Human Adipose Tissue Contain Mesodermal Precursors for Endothelial and Mesenchymal Cells. Stem Cells Dev. 2015, 24, 2280–2296. [Google Scholar] [CrossRef]
- Montemurro, N.; Cocciaro, A.; Liberti, G.; Cosottini, M.; Perrini, P. The internal trabecular bone structure of the odontoid process of the axis. A retrospective single-center comparative study in patients following cervical trauma. J. Neurol. Surg. A Cent. Eur. Neurosurg. 2022, 8, 1. [Google Scholar] [CrossRef]


| Authors | Objectives | Methodology | Sample Size | Main Findings | Following Time (Months) |
|---|---|---|---|---|---|
| Saxer et al. [26] | To explore the efficacy of SVF in enhancing bone regeneration in fractures | Prospective | 8 | SVF significantly improves bone regeneration speed | 12 |
| Urlaub et al. [27] | To examine the efficacy of SVF to enhance healing outcomes in a murine model of irradiated mandibular fracture | Prospective | 35 | SVF therapy significantly improved all metrics of bone vascularization compared to the irradiated fracture group and was not statistically different from fracture. Bone cellularity and maturity were restored to non-irradiated levels in the irradiated fracture with SVF group despite preoperative radiation. | NA |
| Sananta et al. [28] | To determine the effect of SVF from adipose tissue in the process of bone defect healing, measured by TGF-β1 biomarker. | Randomized controlled trial | 12 | TGF- β1 biomarker expressions were higher in the group with SVF application than in the group without SVF application. All comparisons of the SVF group and positive control group showed significant differences (p = 0.000), respectively. | 3 |
| Dradjat et al. [29] | Randomized controlled trial | 12 | Osteocalcin biomarker expressions were higher in the group treated with SVF application than those without using SVF. All comparisons of the SVF group and positive control group showed significant differences (p < 0.05). | 3 | |
| Kamenaga et al. [30] | To evaluate the therapeutic effect of (SVF) cells on fracture healing in a rat non-healing fracture model and comparing the effects between freshly isolated (F) and cryopreserved (C)-SVFs. | Prospective | 5 | SVF cells can enhance bone healing and cryopreserved cells have almost equal potential as fresh cells. SVF cells can be used for improving nonunion bone fracture healing as an alternative to other mesenchymal stem cells and the effect of SVF cells can be maintained under cryopreservation. | 2 |
| Stimulation Technique | Mechanism of Action | Application Method | Primary Benefit |
|---|---|---|---|
| Electrical stimulation [9,10] | Utilizes electric fields or currents to stimulate cellular processes involved in bone repair. | Varies depending on the type; can involve surgical insertion of electrodes or external application. | Promotes bone healing through cellular activation and biochemical reactions. |
| Ultrasound stimulation [10,12] | Employs sound waves of specific frequencies and intensities to influence cellular activities. | External application focusing on the fracture site. | Enhances osteoblast activities, hastening bone healing. |
| Mechanical stimulation [13,14] | Applies measured forces to synchronize with the body’s reparative responses. | Use of specialized devices to apply forces directly or indirectly on the fracture. | Rekindles cellular processes for bone formation and supports bone density improvement. |
| Biological intervention [10,19,20] | Uses natural accelerators like BMPs to speed up bone growth. | Direct application to the fracture zone. | Accelerates bone growth and regeneration. |
| SVF [22,23,24] | Harvested from adipose tissue; packed with cellular entities to facilitate healing. | Injection or application at the fracture site. | Enhances bone formation, immune modulation, vascular integration, and creates an optimized cellular environment for healing. |
| Nutritional and pharmacological stimulation [10] | Involve essential elements and medications to bolster bone’s recovery. | Oral intake or injection, as per the advised dosage. | Fortifies bones, enhances bone density, and accelerates bone repair mechanisms. |
| Criterion | Electrical Stimulation [11] | Ultrasound Stimulation [12] | Mechanical Stimulation [13,16] | Biological Intervention [19] | SVF [22,26] | Nutritional and Pharmacological Stimulation [20] |
|---|---|---|---|---|---|---|
| Invasiveness | Varies | Non-invasive | Varies | Invasive | Invasive | Non-invasive |
| Ease of application | Moderate | Easy | Moderate | Complex | Moderate | Easy |
| Targeted outcome | Bone repair | Bone formation | Bone formation/density | Bone growth/regeneration | Multi-functional | Bone fortification |
| Potential side effects | Minimal | Minimal | Minimal | Varies | Minimal | Minimal, dose-dependent |
| Applicability | Broad | Specific | Broad | Specific | Broad | Broad |
| Complication | Description | Potential Impact | Mitigation Strategies |
|---|---|---|---|
| Invasiveness of procedure [31] | Surgical extraction of adipose tissue is required. | Risks like infection, bleeding, and anesthesia reactions. | Use sterile techniques; skilled surgical procedures. |
| Risk of infection [32,33] | Introduction of pathogens during the procedure. | Local or systemic infections. | Adhere to aseptic techniques; prophylactic antibiotics. |
| Immune reaction [33,34,35] | Body may react to reintroduced cells. | Inflammation, rejection, or adverse immune response. | Close monitoring; use autologous cells to reduce risk. |
| Pain and discomfort [36,37] | At the adipose tissue harvesting site. | Swelling, bruising, and discomfort. | Pain management; post-procedure care. |
| Risk of embolism [38] | Fat droplets entering the bloodstream. | Blockage in blood vessels; potentially life-threatening. | Careful handling; monitoring during and after procedure. |
| Quality and purity of SVF [39,40] | Isolation process must be controlled. | Reduced efficacy; introduction of other complications. | Rigorous processing protocols; quality control measures. |
| Stimulation Technique | Electrical Stimulation [41,42] | Ultrasound Stimulation [12,43] | Mechanical Stimulation [15,44,45] | Biological Intervention [46] | SVF (Stroma Vascular Fraction) [32,37,39,40,47] | Nutritional and Pharmacological Stimulation [48,49,50] |
|---|---|---|---|---|---|---|
| Invasiveness and surgical risks | Non-invasive, no surgical risks | Non-invasive, no surgical risks | May be non-invasive or invasive | Often invasive (surgical implantation) | Invasive (adipose tissue harvesting) | Non-invasive |
| Risk of infection | Low, at electrode sites | Low, at application site | Higher with invasive methods | High due to surgery | High due to surgery | Low, unless injections are involved |
| Immune and tissue reaction | Possible irritation or allergic reaction to electrodes | Minimal, possible skin irritation | Variable; higher with invasive methods | Possible immune reaction to biological materials | Potential immune reaction to reintroduced cells | Rare, mainly hypersensitivity to supplements |
| Pain and discomfort | Mild discomfort at application sites | Mild discomfort at application sites | Can vary; significant with invasive methods | Post-surgical pain and discomfort | Pain and swelling at harvesting site | Generally minimal |
| Procedure-specific complications | Skin irritation, electrical burns (rare) | Thermal injury to tissues (rare) | Joint stiffness, aggravation of injury | Rejection, inflammation, overgrowth of tissue | Embolism, variable healing efficacy, tissue damage | Side effects specific to medications or supplements |
| Long-term complications | Rare | Rare | Depends on method and patient response | Depends on type of biological material used | Limited long-term data available | Depends on long-term effects of medications |
| Need for repeat procedures | Rarely required | Rarely required | May require follow-up adjustments | May need additional treatments | Possible need for repeat procedures | Depends on treatment regimen |
| Efficacy and predictability | Generally predictable, efficacy varies | Efficacy can be variable | Efficacy varies widely with technique | Varies based on biological material and patient response | Unpredictable efficacy, varies by individual | Efficacy varies, dependent on condition and supplement |
| Other risks and considerations | Device dependency and maintenance | Inefficacy in certain cases | Dependency on device or mechanical application | Risk of over- or under-stimulation of tissue growth | Quality and purity of SVF, technique sensitivity | Nutrient imbalances, interactions with other medications |
| Type of Cells | Functions | Authors, Year [Ref.] |
|---|---|---|
| Mesenchymal progenitor/stem cells | Capacity to perform self-renewal, differentiation into specific cell lineages, and support maintenance of other cells via paracrine secretion. | Francis et al., 2018 [54] |
| Lymphocytes | Participate in both innate and adaptive immune responses with multiple effects or functions. Produce antibodies, direct cell-mediated killing of virus-infected and/or tumor cells and regulate immune responses. | Busato et al., 2020 [55] |
| Smooth muscle cells | Display involuntary contractile activity to control the diameter, wall movement, and wall stiffness of specific organs. | Busato et al., 2020 [55] |
| Adipose tissue-derived stem cells | Secrete growth factors, cytokines, and antioxidant factors into a microenvironment, regulating intracellular signaling pathways in neighboring cells. Protective outcome via inflammatory and immunomodulatory effects. | Bora et al., 2017 [22] |
| Preadipocytes | Promote growth of adipose tissue by differentiating into mature and metabolically active adipocytes. Proliferating preadipocytes may also exhibit phagocytic activity towards microorganisms and behave similarly to macrophage-like cells. | Matsuo et al., 2020 [56] |
| Mφ2 macrophage | The type 2 macrophage (Mφ2) is produced by the type 2 T helper immune response and takes on an anti-inflammatory role, typically characterized by an increase in the production of interleukins (IL-4, IL-5, IL-9 and IL-13). It is also directly involved in regenerative and tissue repair processes that occur after injuries. | Contreras et al., 2015 [57]; Dey et al., 2021 [58] |
| T cells | As components of the adaptive immune system with major importance, these cells are responsible for eliminating infected host cells, activating other immune cells, and secreting cytokines that further regulate immune responses. | Dulong et al., 2022 [59] |
| Endothelial precursor cells and endothelial cells | Differentiate into functional endothelial cells and sustain vasculo genesis by incorporating themselves into the injured endothelium with the formation of functional blood vessels and through the local secretion of pro-angiogenic factors with a paracrine effect on the cells that form the vessel. Play a critical role in vascular homeostasis as well as physiological or pathological processes such as thrombosis, inflammation, and vascular wall remodeling. Resting endothelial cells control blood flow and the passage of protein from blood into tissues, as well as inhibiting inflammation and preventing coagulation | Gulyaeva et al., 2019 [60] |
| Conventional | Modified Approach | |
|---|---|---|
| Obtaining adipose tissue |
|
|
| Mechanical separation/shredding |
|
|
| Pre-filtration |
|
|
| Washing | [–] |
|
| Final filtration |
|
|
| Collection of SVF/adipose tissue |
|
|
| Cell counting and characterization |
|
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Goncharov, E.N.; Koval, O.A.; Nikolaevich Bezuglov, E.; Engelgard, M.; Igorevich, E.I.; Velentinovich Kotenko, K.; Encarnacion Ramirez, M.D.J.; Montemurro, N. Comparative Analysis of Stromal Vascular Fraction and Alternative Mechanisms in Bone Fracture Stimulation to Bridge the Gap between Nature and Technological Advancement: A Systematic Review. Biomedicines 2024, 12, 342. https://doi.org/10.3390/biomedicines12020342
Goncharov EN, Koval OA, Nikolaevich Bezuglov E, Engelgard M, Igorevich EI, Velentinovich Kotenko K, Encarnacion Ramirez MDJ, Montemurro N. Comparative Analysis of Stromal Vascular Fraction and Alternative Mechanisms in Bone Fracture Stimulation to Bridge the Gap between Nature and Technological Advancement: A Systematic Review. Biomedicines. 2024; 12(2):342. https://doi.org/10.3390/biomedicines12020342
Chicago/Turabian StyleGoncharov, Evgeniy Nikolaevich, Oleg Aleksandrovich Koval, Eduard Nikolaevich Bezuglov, Mikhail Engelgard, Eremin Ilya Igorevich, Konstantin Velentinovich Kotenko, Manuel De Jesus Encarnacion Ramirez, and Nicola Montemurro. 2024. "Comparative Analysis of Stromal Vascular Fraction and Alternative Mechanisms in Bone Fracture Stimulation to Bridge the Gap between Nature and Technological Advancement: A Systematic Review" Biomedicines 12, no. 2: 342. https://doi.org/10.3390/biomedicines12020342
APA StyleGoncharov, E. N., Koval, O. A., Nikolaevich Bezuglov, E., Engelgard, M., Igorevich, E. I., Velentinovich Kotenko, K., Encarnacion Ramirez, M. D. J., & Montemurro, N. (2024). Comparative Analysis of Stromal Vascular Fraction and Alternative Mechanisms in Bone Fracture Stimulation to Bridge the Gap between Nature and Technological Advancement: A Systematic Review. Biomedicines, 12(2), 342. https://doi.org/10.3390/biomedicines12020342








