Fibroblast Activation Protein (FAP)-Mediated Cleavage of Type III Collagen Reveals Serum Biomarker Potential in Non-Small Cell Lung Cancer and Spondyloarthritis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Target Identification
2.2. Antibody Development and Specificity
2.3. Assay Development and Evaluation
2.4. C3F Assay Protocol
2.5. Assessment of MMP Degraded Type III Collagen
2.6. Subjects
2.7. Statistics
3. Results
3.1. Technical Evaluation of the C3F ELISA Assay
3.2. C3F Antibody Binding Is Specific to the FAP-Cleaved Type III Collagen Fragment
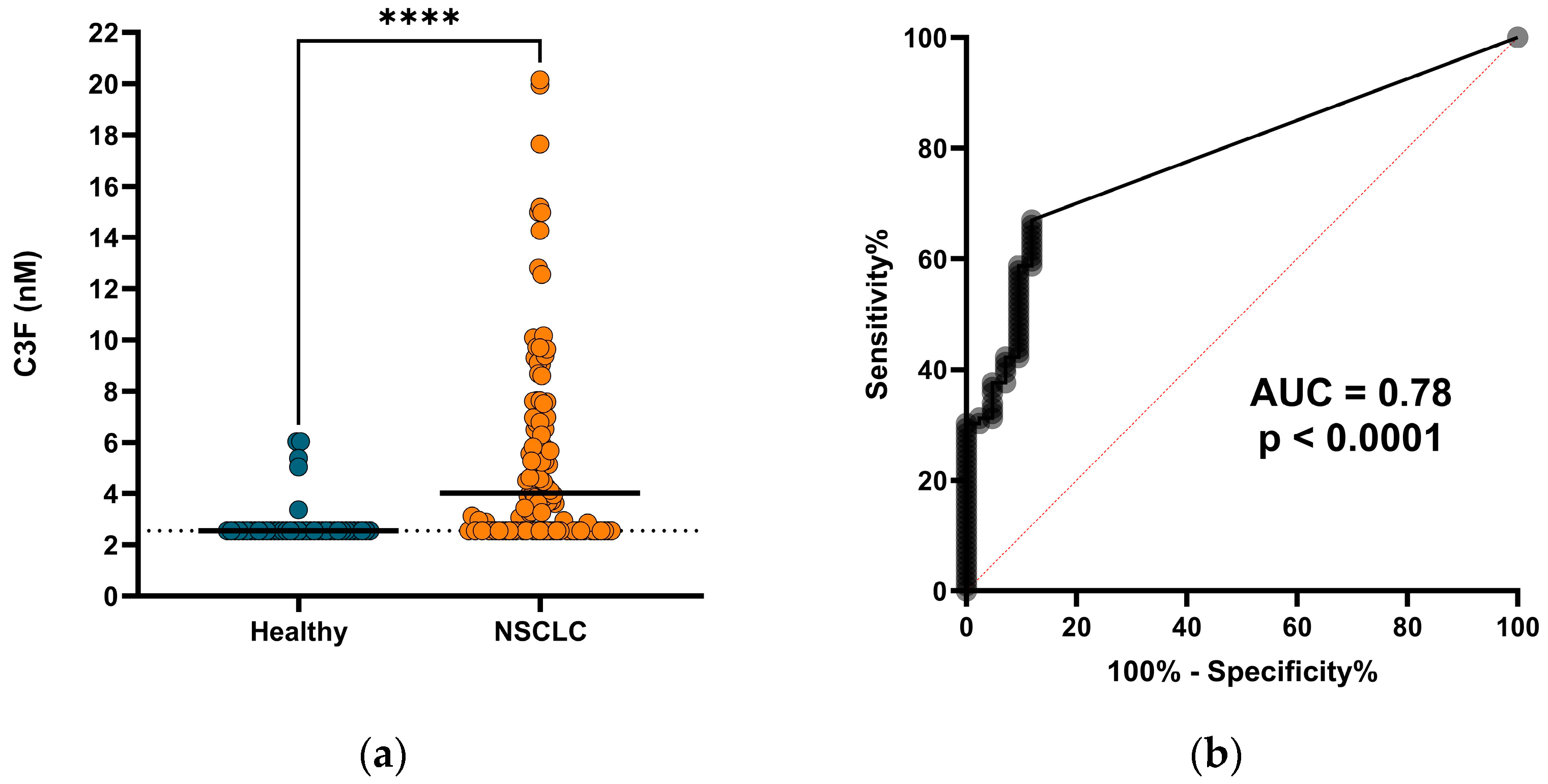
3.3. C3F Is Elevated in Serum from Patients with NSCLC
3.4. C3F Levels Are Elevated in Patients with SpA
4. Discussion
5. Conclusions
6. Patents
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Yang, P.; Luo, Q.; Wang, X.; Fang, Q.; Fu, Z.; Li, J.; Lai, Y.; Chen, X.; Xu, X.; Peng, X.; et al. Comprehensive Analysis of Fibroblast Activation Protein Expression in Interstitial Lung Diseases. Am. J. Respir. Crit. Care Med. 2023, 207, 160–172. [Google Scholar] [CrossRef] [PubMed]
- Hamson, E.J.; Keane, F.M.; Tholen, S.; Schilling, O.; Gorrell, M.D. Understanding Fibroblast Activation Protein (FAP): Substrates, Activities, Expression and Targeting for Cancer Therapy. Proteom. Clin. Appl. 2014, 8, 454–463. [Google Scholar] [CrossRef] [PubMed]
- Busek, P.; Balaziova, E.; Matrasova, I.; Hilser, M.; Tomas, R.; Syrucek, M.; Zemanova, Z.; Krepela, E.; Belacek, J.; Sedo, A. Fibroblast Activation Protein Alpha Is Expressed by Transformed and Stromal Cells and Is Associated with Mesenchymal Features in Glioblastoma. Tumor Biol. 2016, 37, 13961–13971. [Google Scholar] [CrossRef] [PubMed]
- Fitzgerald, A.A.; Weiner, L.M. The Role of Fibroblast Activation Protein in Health and Malignancy. Cancer Metastasis Rev. 2020, 39, 783–803. [Google Scholar] [CrossRef] [PubMed]
- Xin, L.; Gao, J.; Zheng, Z.; Chen, Y.; Lv, S.; Zhao, Z.; Yu, C.; Yang, X.; Zhang, R. Fibroblast Activation Protein-α as a Target in the Bench-to-Bedside Diagnosis and Treatment of Tumors: A Narrative Review. Front. Oncol. 2021, 11, 648187. [Google Scholar] [CrossRef]
- Antonova, D.V.; Gnatenko, D.A.; Kotova, E.S.; Pleshkan, V.V.; Kuzmich, A.I.; Didych, D.A.; Sverdlov, E.D.; Alekseenko, I.V. Cell-Specific Expression of the FAP Gene Is Regulated by Enhancer Elements. Front. Mol. Biosci. 2023, 10, 1111511. [Google Scholar] [CrossRef]
- Rauber, S.; Mohammadian, H.; Schmidkonz, C.; Atzinger, A.; Soare, A.; Maschauer, S.; Treutlein, C.; Angeli, M.; Raimondo, M.G.; Xu, C.; et al. Molecular Imaging with Fibroblast Activation Protein Tracers Depicts Inflammatory Joint Damage and Its Transition to Resolution of Inflammation. bioRxiv 2023. [Google Scholar] [CrossRef]
- Shi, J.; Hou, Z.; Yan, J.; Qiu, W.; Liang, L.; Meng, M.; Li, L.; Wang, X.; Xie, Y.; Jiang, L.; et al. The Prognostic Significance of Fibroblast Activation Protein-α in Human Lung Adenocarcinoma. Ann. Transl. Med. 2020, 8, 224. [Google Scholar] [CrossRef]
- Wikberg, M.L.; Edin, S.; Lundberg, I.V.; Van Guelpen, B.; Dahlin, A.M.; Rutegård, J.; Stenling, R.; Öberg, Å.; Palmqvist, R. High Intratumoral Expression of Fibroblast Activation Protein (FAP) in Colon Cancer Is Associated with Poorer Patient Prognosis. Tumor Biol. 2013, 34, 1013–1020. [Google Scholar] [CrossRef]
- Pellinen, T.; Sandeman, K.; Blom, S.; Turkki, R.; Hemmes, A.; Välimäki, K.; Eineluoto, J.; Kenttämies, A.; Nordling, S.; Kallioniemi, O.; et al. Stromal FAP Expression Is Associated with MRI Visibility and Patient Survival in Prostate Cancer. Cancer Res. Commun. 2022, 2, 172–181. [Google Scholar] [CrossRef]
- Vlachostergios, P.J.; Karathanasis, A.; Tzortzis, V. Expression of Fibroblast Activation Protein Is Enriched in Neuroendocrine Prostate Cancer and Predicts Worse Survival. Genes 2022, 13, 135. [Google Scholar] [CrossRef]
- Kawase, T.; Yasui, Y.; Nishina, S.; Hara, Y.; Yanatori, I.; Tomiyama, Y.; Nakashima, Y.; Yoshida, K.; Kishi, F.; Nakamura, M.; et al. Fibroblast Activation Protein-α-Expressing Fibroblasts Promote the Progression of Pancreatic Ductal Adenocarcinoma. BMC Gastroenterol. 2015, 15, 109. [Google Scholar] [CrossRef]
- Li, M.; Cheng, X.; Rong, R.; Gao, Y.; Tang, X.; Chen, Y. High Expression of Fibroblast Activation Protein (FAP) Predicts Poor Outcome in High-Grade Serous Ovarian Cancer. BMC Cancer 2020, 20, 1032. [Google Scholar] [CrossRef]
- Zhao, L.; Chen, J.; Pang, Y.; Fu, K.; Shang, Q.; Wu, H.; Sun, L.; Lin, Q.; Chen, H. Fibroblast Activation Protein-Based Theranostics in Cancer Research: A State-of-the-Art Review. Theranostics 2022, 12, 1557–1569. [Google Scholar] [CrossRef]
- Mori, Y.; Dendl, K.; Cardinale, J.; Kratochwil, C.; Giesel, F.L.; Haberkorn, U. FAPI PET: Fibroblast Activation Protein Inhibitor Use in Oncologic and Nononcologic Disease. Radiology 2023, 306, e220749. [Google Scholar] [CrossRef] [PubMed]
- Huang, R.; Pu, Y.; Huang, S.; Yang, C.; Yang, F.; Pu, Y.; Li, J.; Chen, L.; Huang, Y. FAPI-PET/CT in Cancer Imaging: A Potential Novel Molecule of the Century. Front. Oncol. 2022, 12, 854658. [Google Scholar] [CrossRef] [PubMed]
- Syed, M.; Flechsig, P.; Liermann, J.; Windisch, P.; Staudinger, F.; Akbaba, S.; Koerber, S.A.; Freudlsperger, C.; Plinkert, P.K.; Debus, J.; et al. Fibroblast Activation Protein Inhibitor (FAPI) PET for Diagnostics and Advanced Targeted Radiotherapy in Head and Neck Cancers. Eur. J. Nucl. Med. Mol. Imaging 2020, 47, 2836–2845. [Google Scholar] [CrossRef] [PubMed]
- Chen, M.; Xu, G.; Fan, M.; Jia, H.; Xiao, L.; Lang, J. Anti-Tumour Effects of a Xenogeneic Fibroblast Activation Protein-Based Whole Cell Tumour Vaccine in Murine Tumour Models. Artif. Cells Nanomed. Biotechnol. 2019, 47, 4182–4193. [Google Scholar] [CrossRef] [PubMed]
- Wen, Y.; Wang, C.-T.; Ma, T.-T.; Li, Z.-Y.; Zhou, L.-N.; Mu, B.; Leng, F.; Shi, H.-S.; Li, Y.-O.; Wei, Y.-Q. Immunotherapy Targeting Fibroblast Activation Protein Inhibits Tumor Growth and Increases Survival in a Murine Colon Cancer Model. Cancer Sci. 2010, 101, 2325–2332. [Google Scholar] [CrossRef] [PubMed]
- Kakarla, S.; Chow, K.K.H.; Mata, M.; Shaffer, D.R.; Song, X.-T.; Wu, M.-F.; Liu, H.; Wang, L.L.; Rowley, D.R.; Pfizenmaier, K.; et al. Antitumor Effects of Chimeric Receptor Engineered Human T Cells Directed to Tumor Stroma. Mol. Ther. 2013, 21, 1611–1620. [Google Scholar] [CrossRef] [PubMed]
- Huang, S.; Fang, R.; Xu, J.; Qiu, S.; Zhang, H.; Du, J.; Cai, S. Evaluation of the Tumor Targeting of a FAPα-Based Doxorubicin Prodrug. J. Drug Target. 2011, 19, 487–496. [Google Scholar] [CrossRef] [PubMed]
- Ye, G.; Huang, M.; Li, Y.; Ouyang, J.; Chen, M.; Wen, Q.; Li, X.; Zeng, H.; Long, P.; Fan, Z.; et al. The FAP -Activated Prodrug Z-GP-DAVLBH Inhibits the Growth and Pulmonary Metastasis of Osteosarcoma Cells by Suppressing the AXL Pathway. Acta Pharm. Sin. B 2022, 12, 1288–1304. [Google Scholar] [CrossRef] [PubMed]
- Claus, C.; Ferrara, C.; Xu, W.; Sam, J.; Lang, S.; Uhlenbrock, F.; Albrecht, R.; Herter, S.; Schlenker, R.; Hüsser, T.; et al. Tumor-Targeted 4-1BB Agonists for Combination with T Cell Bispecific Antibodies as off-the-Shelf Therapy. Sci. Transl. Med. 2019, 11, eaav5989. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.E.; Hamson, E.J.; Koczorowska, M.M.; Tholen, S.; Chowdhury, S.; Bailey, C.G.; Lay, A.J.; Twigg, S.M.; Lee, Q.; Roediger, B.; et al. Identification of Novel Natural Substrates of Fibroblast Activation Protein-Alpha by Differential Degradomics and Proteomics. Mol. Cell. Proteom. 2019, 18, 65–85. [Google Scholar] [CrossRef] [PubMed]
- Wu, M.; Wang, Y.; Yang, Q.; Wang, X.; Yang, X.; Xing, H.; Sang, X.; Li, X.; Zhao, H.; Huo, L. Comparison of Baseline 68 Ga-FAPI and 18 F-FDG PET/CT for Prediction of Response and Clinical Outcome in Patients with Unresectable Hepatocellular Carcinoma Treated with PD-1 Inhibitor and Lenvatinib. J. Nucl. Med. 2023, 64, 1532–1539. [Google Scholar] [CrossRef] [PubMed]
- Yang, X.; Li, G.; Ruan, C.; Hu, K.; Tang, G. Formulation and Preclinical Testing of Tc-99m-Labeled HYNIC-Glc-FAPT as a FAP-Targeting Tumor Radiotracer. Bioconjug. Chem. 2023, 34, 2133–2143. [Google Scholar] [CrossRef] [PubMed]
- Lai, C.; Cao, R.; Li, R.; He, C.; Wang, X.; Shi, H.; Qu, C.; Qian, K.; Song, S.; Chen, W.-H.; et al. Fibroblast Activation Protein Targeting Probe with Gly–Pro Sequence for PET of Glioblastoma. Mol. Pharm. 2023, 20, 4120–4128. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.-O.; Mullins, S.R.; Franco-Barraza, J.; Valianou, M.; Cukierman, E.; Cheng, J.D. FAP-Overexpressing Fibroblasts Produce an Extracellular Matrix That Enhances Invasive Velocity and Directionality of Pancreatic Cancer Cells. BMC Cancer 2011, 11, 245. [Google Scholar] [CrossRef]
- Basalova, N.; Alexandrushkina, N.; Grigorieva, O.; Kulebyakina, M.; Efimenko, A. Fibroblast Activation Protein Alpha (FAPα) in Fibrosis: Beyond a Perspective Marker for Activated Stromal Cells? Biomolecules 2023, 13, 1718. [Google Scholar] [CrossRef]
- Christiansen, V.J.; Jackson, K.W.; Lee, K.N.; McKee, P.A. Effect of Fibroblast Activation Protein and A2-Antiplasmin Cleaving Enzyme on Collagen Types I, III, and IV. Arch. Biochem. Biophys. 2007, 457, 177–186. [Google Scholar] [CrossRef]
- Nissen, N.I.; Johansen, A.Z.; Chen, I.; Johansen, J.S.; Pedersen, R.S.; Hansen, C.P.; Karsdal, M.A.; Willumsen, N. Collagen Biomarkers Quantify Fibroblast Activity In Vitro and Predict Survival in Patients with Pancreatic Ductal Adenocarcinoma. Cancers 2022, 14, 819. [Google Scholar] [CrossRef]
- Thorlacius-Ussing, J.; Jensen, C.; Nissen, N.I.; Cox, T.R.; Kalluri, R.; Karsdal, M.; Willumsen, N. The Collagen Landscape in Cancer: Profiling Collagens in Tumors and in Circulation Reveals Novel Markers of Cancer-associated Fibroblast Subtypes. J. Pathol. 2024, 262, 22–36. [Google Scholar] [CrossRef]
- Pehrsson, M.; Manon-Jensen, T.; Sun, S.; Villesen, I.F.; Castañé, H.; Joven, J.; Patel, K.; Goodman, Z.; Nielsen, M.J.; Bay-Jensen, A.; et al. An MMP-degraded and Cross-linked Fragment of Type III Collagen as a Non-invasive Biomarker of Hepatic Fibrosis Resolution. Liver Int. 2022, 42, 1605–1617. [Google Scholar] [CrossRef]
- Gudmann, N.S.; Siebuhr, A.S.; Christensen, A.F.; Ejstrup, L.; Sørensen, G.L.; Loft, A.G.; Karsdal, M.A.; Bay-Jensen, A.-C.; Munk, H.L.; Junker, P. Type I and III Collagen Turnover Is Increased in Axial Spondyloarthritis and Psoriatic Arthritis. Associations with Disease Activity and Diagnostic Capacity. Clin. Exp. Rheumatol. 2017, 35, 653–659. [Google Scholar]
- Genovese, F.; Akhgar, A.; Lim, S.S.; Farris, A.B.; Battle, M.; Cobb, J.; Sinibaldi, D.; Karsdal, M.A.; White, W.I. Collagen Type III and VI Remodeling Biomarkers Are Associated with Kidney Fibrosis in Lupus Nephritis. Kidney360 2021, 2, 1473–1481. [Google Scholar] [CrossRef]
- Williams, K.E.; Olsen, D.R. Matrix Metalloproteinase-1 Cleavage Site Recognition and Binding in Full-Length Human Type III Collagen. Matrix Biol. 2009, 28, 373–379. [Google Scholar] [CrossRef]
- Bigg, H.F.; Rowan, A.D.; Barker, M.D.; Cawston, T.E. Activity of Matrix Metalloproteinase-9 against Native Collagen Types I and III. FEBS J. 2007, 274, 1246–1255. [Google Scholar] [CrossRef]
- Taddese, S.; Jung, M.C.; Ihling, C.; Heinz, A.; Neubert, R.H.H.; Schmelzer, C.E.H. MMP-12 Catalytic Domain Recognizes and Cleaves at Multiple Sites in Human Skin Collagen Type I and Type III. Biochim. Biophys. Acta—Proteins Proteom. 2010, 1804, 731–739. [Google Scholar] [CrossRef]
- Gefter, M.L.; Margulies, D.H.; Scharff, M.D. A Simple Method for Polyethylene Glycol-Promoted Hybridization of Mouse Myeloma Cells. Somat. Cell Genet. 1977, 3, 231–236. [Google Scholar] [CrossRef]
- Rudwaleit, M.; Van Der Heijde, D.; Landewé, R.; Listing, J.; Akkoc, N.; Brandt, J.; Braun, J.; Chou, C.T.; Collantes-Estevez, E.; Dougados, M.; et al. The development of Assessment of Spondyloarthritis international Society classification criteria for axial spondyloarthritis (part II): Validation and final selection. Ann. Rheum. Dis. 2009, 68, 777–783. [Google Scholar] [CrossRef]
- Van Rymenant, Y.; Tanc, M.; Van Elzen, R.; Bracke, A.; De Wever, O.; Augustyns, K.; Lambeir, A.-M.; Kockx, M.; De Meester, I.; Van Der Veken, P. In Vitro and In Situ Activity-Based Labeling of Fibroblast Activation Protein with UAMC1110-Derived Probes. Front. Chem. 2021, 9, 640566. [Google Scholar] [CrossRef] [PubMed]
- Cheng, J.D.; Valianou, M.; Canutescu, A.A.; Jaffe, E.K.; Lee, H.-O.; Wang, H.; Lai, J.H.; Bachovchin, W.W.; Weiner, L.M. Abrogation of Fibroblast Activation Protein Enzymatic Activity Attenuates Tumor Growth. Mol. Cancer Ther. 2005, 4, 351–360. [Google Scholar] [CrossRef] [PubMed]
- Winkler, J.; Abisoye-Ogunniyan, A.; Metcalf, K.J.; Werb, Z. Concepts of Extracellular Matrix Remodelling in Tumour Progression and Metastasis. Nat. Commun. 2020, 11, 5120. [Google Scholar] [CrossRef] [PubMed]
- Yang, X.; Zhu, P.; Xie, R.-X.; Chen, P.-F.; Liu, H.; Cheng, X.-M.; Zhu, Z.-Q.; Peng, X.-M.; Liu, H.-B.; Yang, Q.-Y.; et al. Tracking Tumor Alteration in Glioma through Serum Fibroblast Activation Protein Combined with Image. BMC Cancer 2023, 23, 1012. [Google Scholar] [CrossRef] [PubMed]
- Ping, Q.; Yan, R.; Cheng, X.; Wang, W.; Zhong, Y.; Hou, Z.; Shi, Y.; Wang, C.; Li, R. Cancer-Associated Fibroblasts: Overview, Progress, Challenges, and Directions. Cancer Gene Ther. 2021, 28, 984–999. [Google Scholar] [CrossRef] [PubMed]
- Lavie, D.; Ben-Shmuel, A.; Erez, N.; Scherz-Shouval, R. Cancer-Associated Fibroblasts in the Single-Cell Era. Nat. Cancer 2022, 3, 793–807. [Google Scholar] [CrossRef]
- Desbois, M.; Wang, Y. Cancer-Associated Fibroblasts: Key Players in Shaping the Tumor Immune Microenvironment. Immunol. Rev. 2021, 302, 241–258. [Google Scholar] [CrossRef]
- Han, C.; Liu, T.; Yin, R. Biomarkers for Cancer-Associated Fibroblasts. Biomark. Res. 2020, 8, 64. [Google Scholar] [CrossRef]
- Bu, L.; Baba, H.; Yasuda, T.; Uchihara, T.; Ishimoto, T. Functional Diversity of Cancer-associated Fibroblasts in Modulating Drug Resistance. Cancer Sci. 2020, 111, 3468–3477. [Google Scholar] [CrossRef]
- Bager, C.L.; Willumsen, N.; Leeming, D.J.; Smith, V.; Karsdal, M.A.; Dornan, D.; Bay-Jensen, A.C. Collagen Degradation Products Measured in Serum Can Separate Ovarian and Breast Cancer Patients from Healthy Controls: A Preliminary Study. Cancer Biomark. 2015, 15, 783–788. [Google Scholar] [CrossRef]
- Karsdal, M.A.; Nielsen, M.J.; Sand, J.M.; Henriksen, K.; Genovese, F.; Bay-Jensen, A.-C.; Smith, V.; Adamkewicz, J.I.; Christiansen, C.; Leeming, D.J. Extracellular Matrix Remodeling: The Common Denominator in Connective Tissue Diseases Possibilities for Evaluation and Current Understanding of the Matrix as More Than a Passive Architecture, but a Key Player in Tissue Failure. Assay Drug Dev. Technol. 2013, 11, 70–92. [Google Scholar] [CrossRef]
- Karsdal, M.A.; Woodworth, T.; Henriksen, K.; Maksymowych, W.P.; Genant, H.; Vergnaud, P.; Christiansen, C.; Schubert, T.; Qvist, P.; Schett, G.; et al. Biochemical Markers of Ongoing Joint Damage in Rheumatoid Arthritis—Current and Future Applications, Limitations and Opportunities. Arthritis Res. Ther. 2011, 13, 215. [Google Scholar] [CrossRef] [PubMed]
- Bay-Jensen, A.C.; Kjelgaard-Petersen, C.F.; Petersen, K.K.; Arendt-Nielsen, L.; Quasnichka, H.L.; Mobasheri, A.; Karsdal, M.A.; Leeming, D.J. Aggrecanase Degradation of Type III Collagen Is Associated with Clinical Knee Pain. Clin. Biochem. 2018, 58, 37–43. [Google Scholar] [CrossRef]
- Zhang, X.; Jozic, A.; Song, P.; Xu, Q.; Shi, X.; Wang, H.; Bishop, L.; Struthers, H.M.; Rutledge, J.; Chen, S.; et al. MRNA Vaccine against Fibroblast Activation Protein Ameliorates Murine Models of Inflammatory Arthritis. Rheumatol. Immunol. Res. 2023, 4, 90–97. [Google Scholar] [CrossRef]
- Tillmanns, J.; Widera, C.; Habbaba, Y.; Galuppo, P.; Kempf, T.; Wollert, K.C.; Bauersachs, J. Circulating Concentrations of Fibroblast Activation Protein α in Apparently Healthy Individuals and Patients with Acute Coronary Syndrome as Assessed by Sandwich ELISA. Int. J. Cardiol. 2013, 168, 3926–3931. [Google Scholar] [CrossRef] [PubMed]
- Dorst, D.N.; Rijpkema, M.; Buitinga, M.; Walgreen, B.; Helsen, M.M.A.; Brennan, E.; Klein, C.; Laverman, P.; Ramming, A.; Schmidkonz, C.; et al. Targeting of Fibroblast Activation Protein in Rheumatoid Arthritis Patients: Imaging and Ex Vivo Photodynamic Therapy. Rheumatology 2022, 61, 2999–3009. [Google Scholar] [CrossRef]
- Lavis, P.; Pingitore, J.; Doumont, G.; Garabet, A.; Van Simaeys, G.; Lacroix, S.; Passon, N.; Van Heymbeek, C.; De Maeseneire, C.; Allard, J.; et al. Usefulness of FAPα Assessment in Bronchoalveolar Lavage as a Marker of Fibrogenesis: Results of a Preclinical Study and First Report in Patients with Idiopathic Pulmonary Fibrosis. Respir. Res. 2023, 24, 254. [Google Scholar] [CrossRef] [PubMed]
- Kalaei, Z.; Manafi-Farid, R.; Rashidi, B.; Kiani, F.K.; Zarei, A.; Fathi, M.; Jadidi-Niaragh, F. The Prognostic and Therapeutic Value and Clinical Implications of Fibroblast Activation Protein-α as a Novel Biomarker in Colorectal Cancer. Cell Commun. Signal. 2023, 21, 139. [Google Scholar] [CrossRef]
- Warli, S.M.; Putrantyo, I.I.; Laksmi, L.I. Correlation Between Tumor-Associated Collagen Signature and Fibroblast Activation Protein Expression With Prognosis of Clear Cell Renal Cell Carcinoma Patient. World J. Oncol. 2023, 14, 145–149. [Google Scholar] [CrossRef]
- Zhao, Y.; Liu, Y.; Jia, Y.; Wang, X.; He, J.; Zhen, S.; Wang, J.; Liu, L. Fibroblast Activation Protein in the Tumor Microenvironment Predicts Outcomes of PD-1 Blockade Therapy in Advanced Non-Small Cell Lung Cancer. J. Cancer Res. Clin. Oncol. 2023, 149, 3469–3483. [Google Scholar] [CrossRef]


| Clinical Variables | Patients with NSCLC (n = 109) | Healthy Individuals (n = 42) |
|---|---|---|
| Age (years) | ||
| Median (min–max) | 62 (37–81) | 54 (37–69) |
| Sex, n (%) | ||
| Male | 77 (71%) | 30 (71%) |
| Female | 32 (29%) | 12 (29%) |
| NSCLC subtype, n (%) | ||
| Adenocarcinoma | 66 (61%) | |
| Squamous cell carcinoma | 43 (39%) | |
| Body mass index (BMI) | ||
| Median (min–max) | 26 (16–36) | |
| Stage | ||
| 3 | 40 (37%) | |
| 4 | 69 (63%) |
| Clinical Variables | Patients with SpA (n = 17) | Healthy Individuals (n = 19) |
|---|---|---|
| Age (years) | ||
| Median (min–max) | 49 (27–69) | 51 (38–69) |
| Sex, n (%) | ||
| Male | 10 (59%) | 11 (58%) |
| Female | 7 (41%) | 8 (42%) |
| SpA subtype, n (%) | ||
| Axial spondyloarthritis | 7 (41%) | |
| Psoriatic arthritis | 10 (59%) | |
| Have received treatment, n (%) | ||
| No | 9 (53%) | |
| Yes | 7 (41%) | |
| Unknown | 1 (6%) |
| Test | Results |
|---|---|
| IC50 | 10.4 nM |
| Quantification range (LLOQ-ULOQ) | 1.27–250 nM |
| Lower limit of detection | 0.96 nM |
| Dilution recovery (1:2→1:4) | 93% |
| Spiking recovery (serum in serum) | 90% |
| Interference (hemoglobin, low/high conc.) | 102%/106% |
| Interference (biotin, low/high conc.) | 107%/109% |
| Interference (lipids, low/high conc.) | 103%/108% |
| Inter-assay variation | 13% |
| Intra-assay variation | 7% |
| Freeze/thaw stability up to four cycles | 84% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pedersen, R.S.; Thorlacius-Ussing, J.; Raimondo, M.G.; Langholm, L.L.; Schett, G.; Ramming, A.; Karsdal, M.; Willumsen, N. Fibroblast Activation Protein (FAP)-Mediated Cleavage of Type III Collagen Reveals Serum Biomarker Potential in Non-Small Cell Lung Cancer and Spondyloarthritis. Biomedicines 2024, 12, 545. https://doi.org/10.3390/biomedicines12030545
Pedersen RS, Thorlacius-Ussing J, Raimondo MG, Langholm LL, Schett G, Ramming A, Karsdal M, Willumsen N. Fibroblast Activation Protein (FAP)-Mediated Cleavage of Type III Collagen Reveals Serum Biomarker Potential in Non-Small Cell Lung Cancer and Spondyloarthritis. Biomedicines. 2024; 12(3):545. https://doi.org/10.3390/biomedicines12030545
Chicago/Turabian StylePedersen, Rasmus S., Jeppe Thorlacius-Ussing, Maria G. Raimondo, Lasse L. Langholm, Georg Schett, Andreas Ramming, Morten Karsdal, and Nicholas Willumsen. 2024. "Fibroblast Activation Protein (FAP)-Mediated Cleavage of Type III Collagen Reveals Serum Biomarker Potential in Non-Small Cell Lung Cancer and Spondyloarthritis" Biomedicines 12, no. 3: 545. https://doi.org/10.3390/biomedicines12030545
APA StylePedersen, R. S., Thorlacius-Ussing, J., Raimondo, M. G., Langholm, L. L., Schett, G., Ramming, A., Karsdal, M., & Willumsen, N. (2024). Fibroblast Activation Protein (FAP)-Mediated Cleavage of Type III Collagen Reveals Serum Biomarker Potential in Non-Small Cell Lung Cancer and Spondyloarthritis. Biomedicines, 12(3), 545. https://doi.org/10.3390/biomedicines12030545






