Energy Metabolism and Metformin: Effects on Ischemia-Reperfusion Injury in Kidney Transplantation
Abstract
1. Introduction
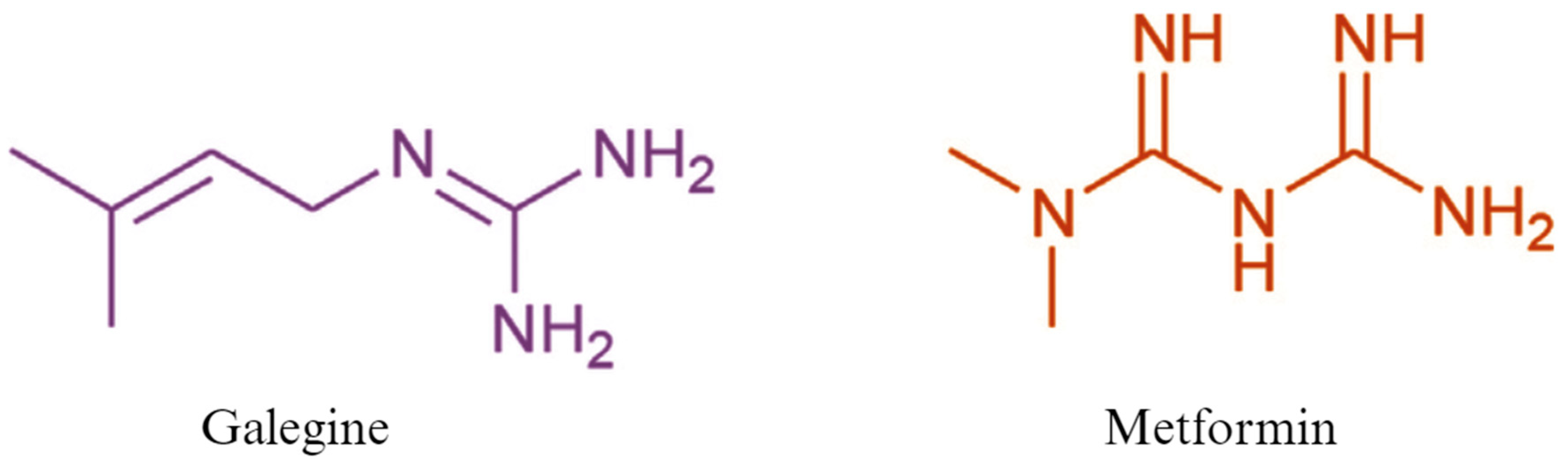
2. History and Uses of Metformin
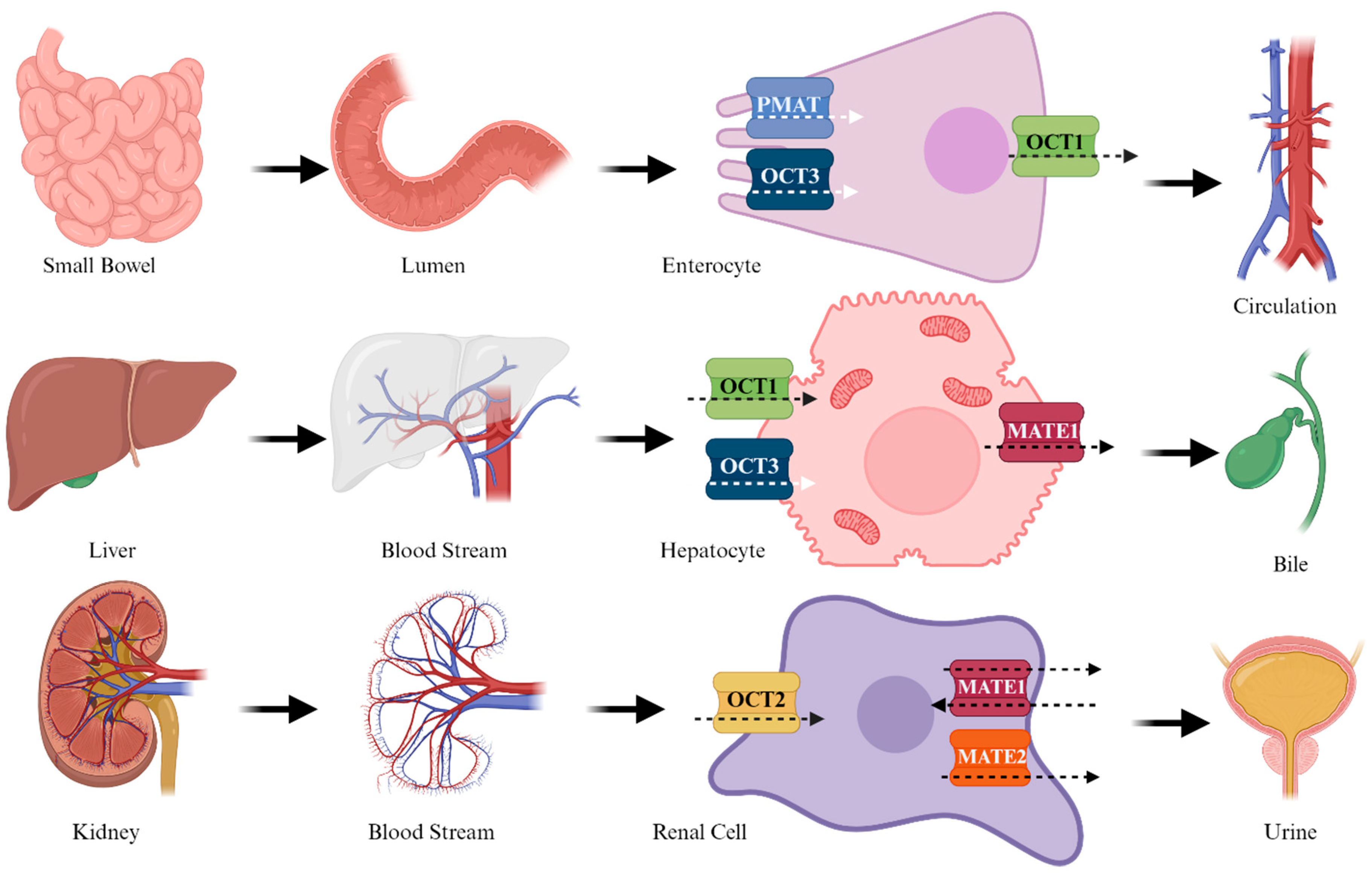
3. Pharmacokinetics of Metformin
4. Pharmacodynamics
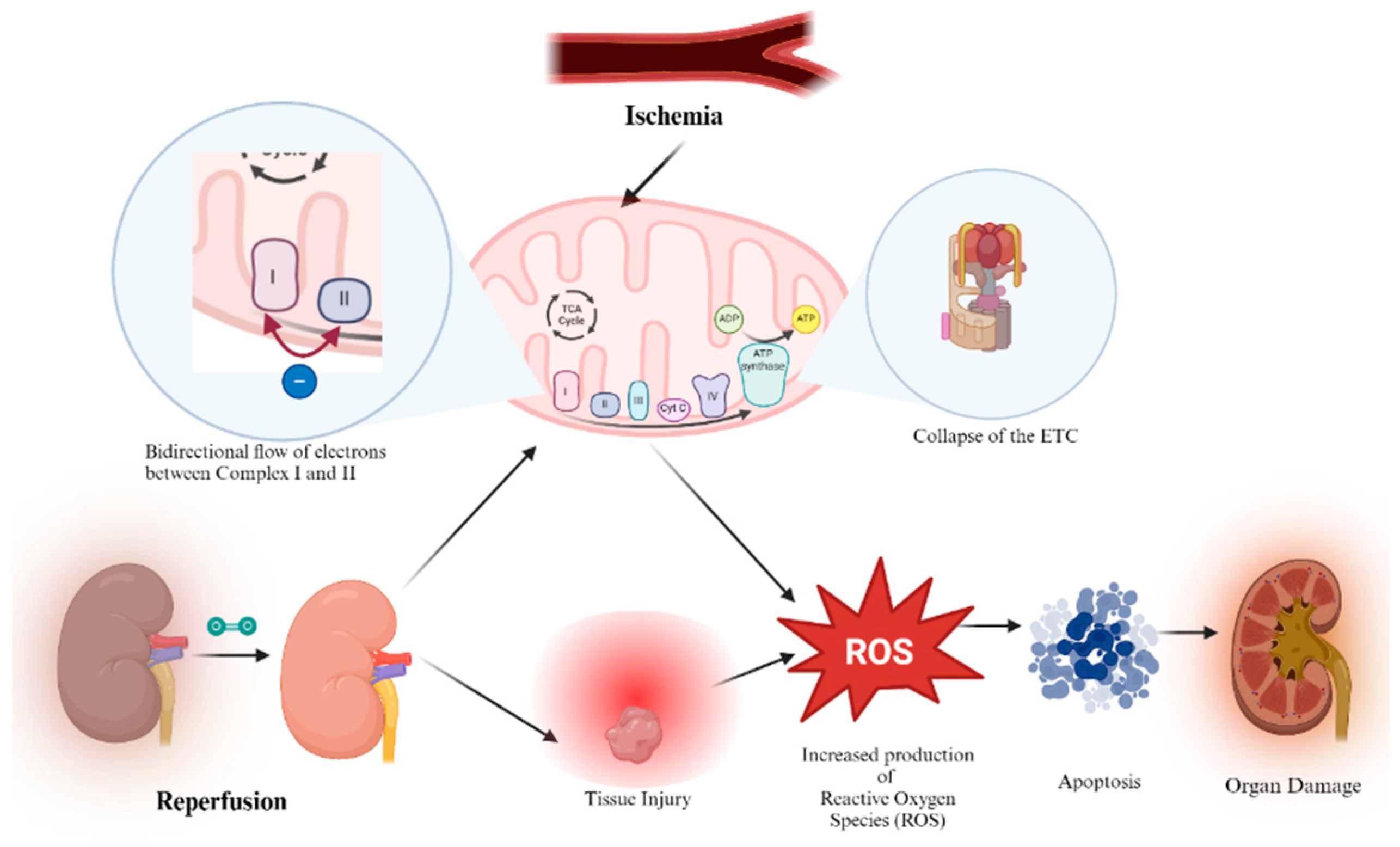
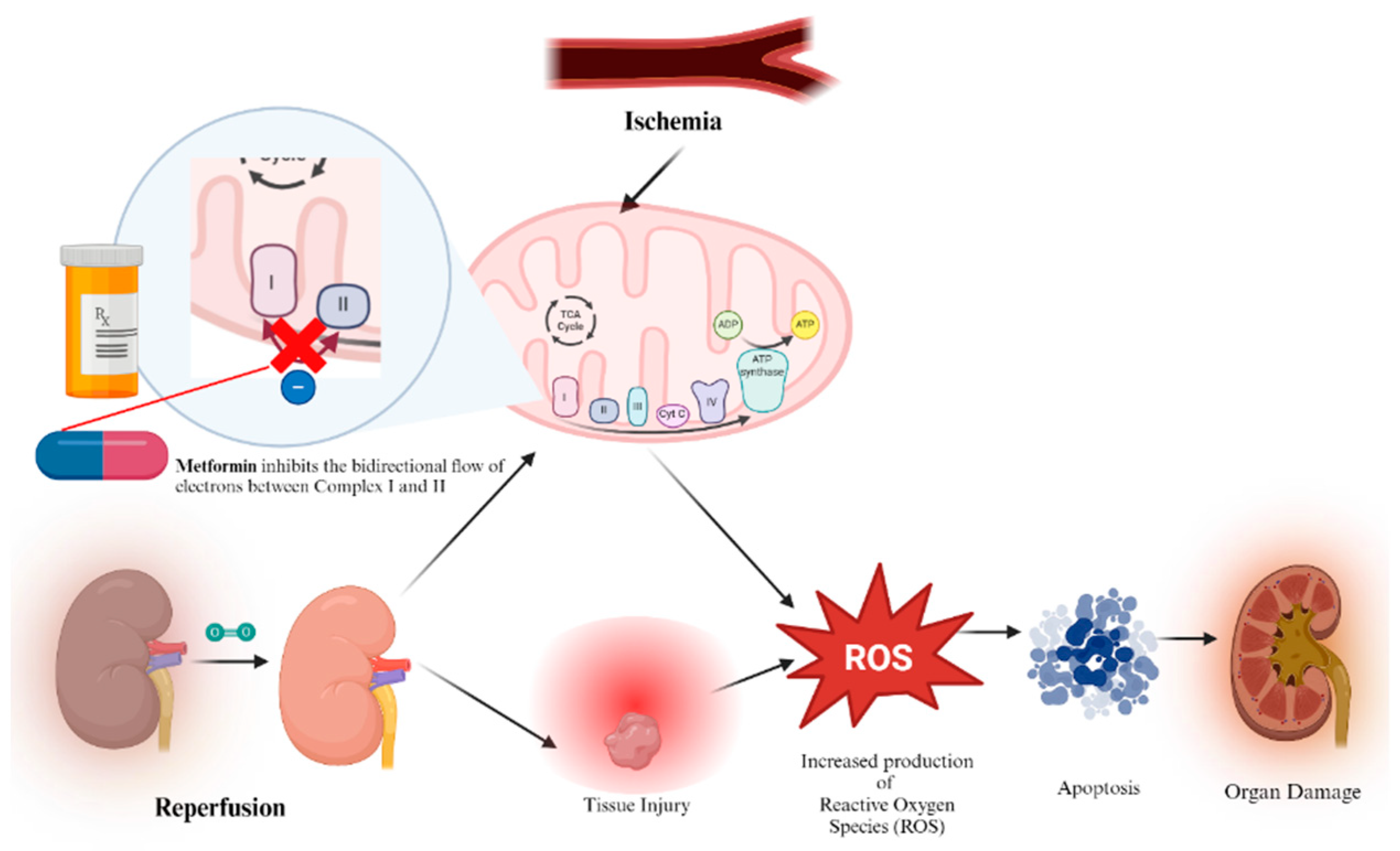
5. Metformin’s Role in Ischemia-Reperfusion Injury (IRI) in the Setting of Organ Transplantation
6. Conclusions
Funding
Conflicts of Interest
Abbreviations
| ACC | acetyl-CoA carboxylase |
| AMP | adenosine monophosphate |
| AMPK | adenosine monophosphate-activated protein kinase |
| ASBT | sodium-dependent bile acid transporter |
| ATP | adenosine triphosphate |
| CPT | carnitine palmitoyl transferase |
| ECD | extended criteria donor |
| FDA | Food and Drug Administration |
| GI | gastrointestinal |
| GLP | glucagon-like peptide |
| HbA1c | glycated hemoglobin |
| HMP | hypothermic machine perfusion |
| IRI | ischemia-reperfusion injury |
| LKB1 | liver kinase B1 |
| KDPI | Kidney Donor Profile Index |
| mGPD | glycerol phosphate dehydrogenase |
| MATE | multidrug and toxin extrusion |
| MPT | mitochondrial permeability transition pore |
| MTF | metformin |
| NADH | nicotinamide adenine dinucleotide + hydrogen |
| NMP | normothermic machine perfusion |
| mTORC1 | mechanistic target of rapamycin complex 1 |
| OCT | organic cation transporter |
| PMAT | plasma membrane monoamine transporter |
| RISK | Reperfusion injury salvage kinase |
| ROS | reactive oxygen species |
| SCD | Standard Criteria Donor |
| T2DM | type 2 diabetes mellitus |
| WHO | World Health Organization |
References
- Davies, M.J.; Aroda, V.R.; Collins, B.S.; Gabbay, R.A.; Green, J.; Maruthur, N.M.; Rosas, S.E.; Del Prato, S.; Mathieu, C.; Mingrone, G.; et al. Management of hyperglycemia in type 2 diabetes, 2022. A consensus report by the american diabetes association (ADA) and the european association for the study of diabetes (EASD). Diabetes Care 2022, 45, 2753–2786. [Google Scholar] [CrossRef]
- Web Annex A. World health organization model list of essential medicines—23rd list, 2023. In The Selection and Use of Essential Medicines 2023: Executive Summary of the Report of the 24th WHO Expert Committee on the Selection and Use of Essential Medicines, 24–28 April 2023; WHO/MHP/HPS/EML/2023.02; World Health Organization: Geneva, Switzerland, 2023. [Google Scholar]
- Hostalek, U.; Campbell, I. Metformin for diabetes prevention: Update of the evidence base. Curr. Med. Res. Opin. 2021, 37, 1705–1717. [Google Scholar] [CrossRef]
- Zhou, J.; Massey, S.; Story, D.; Li, L. Metformin: An old drug with new applications. Int. J. Mol. Sci. 2018, 19, 2863. [Google Scholar] [CrossRef]
- Kheniser, K.G.; Kashyap, S.R.; Kasumov, T. A systematic review: The appraisal of the effects of metformin on lipoprotein modification and function. Obes. Sci. Pract. 2019, 5, 36–45. [Google Scholar] [CrossRef]
- Rajaei, E.; Haybar, H.; Mowla, K.; Zayeri, Z.D. Metformin one in a million efficient medicines for rheumatoid arthritis complications: Inflammation, osteoblastogenesis, cardiovascular disease, malignancies. Curr. Rheumatol. Rev. 2019, 15, 116–122. [Google Scholar] [CrossRef]
- Lv, Z.; Guo, Y. Metformin and its benefits for various diseases. Front. Endocrinol. 2020, 11, 191. [Google Scholar] [CrossRef]
- Foretz, M.; Guigas, B.; Viollet, B. Metformin: Update on mechanisms of action and repurposing potential. Nat. Rev. Endocrinol. 2023, 19, 460–476. [Google Scholar] [CrossRef]
- Bramante, C.T.; Ingraham, N.E.; Murray, T.A.; Marmor, S.; Hovertsen, S.; Gronski, J.; McNeil, C.; Feng, R.; Guzman, G.; Abdelwahab, N.; et al. Metformin and risk of mortality in patients hospitalised with COVID-19: A retrospective cohort analysis. Lancet Healthy Longev. 2021, 2, e34–e41. [Google Scholar] [CrossRef]
- Barzilai, N.; Crandall, J.P.; Kritchevsky, S.B.; Espeland, M.A. Metformin as a tool to target aging. Cell Metab. 2016, 23, 1060–1065. [Google Scholar] [CrossRef]
- Witters, L.A. The blooming of the french lilac. J. Clin. Investig. 2001, 108, 1105–1107. [Google Scholar] [CrossRef]
- Usman, M.; Khan, W.R.; Yousaf, N.; Akram, S.; Murtaza, G.; Kudus, K.A.; Ditta, A.; Rosli, Z.; Rajpar, M.N.; Nazre, M. Exploring the phytochemicals and anti-cancer potential of the members of fabaceae family: A comprehensive review. Molecules 2022, 27, 3863. [Google Scholar] [CrossRef]
- Du, W.; Jiang, W.; Yi, D.; Pang, Y. The complete chloroplast genome of Galega officinalis L. Mitochondrial DNA B Resour. 2021, 6, 663–665. [Google Scholar] [CrossRef]
- Berlinck, R.G.S. 3.12—Ecological interactions mediated by guanidine secondary metabolites. In Comprehensive Natural Products III; Liu, H., Begley, T.P., Eds.; Elsevier: Oxford, UK, 2020; pp. 237–243. [Google Scholar]
- ACS Molecule of the Week Archive: Guanidine. American Chemical Society. Available online: https://www.acs.org/molecule-of-the-week/archive/g/guanidine.html (accessed on 30 April 2024).
- Y-conjugated compounds: The equilibrium geometries and electronic structures of guanidine, guanidinium cation, urea, and 1,1-diaminoethylene. J. Am. Chem. Soc. 1993, 115, 2362–2372. [CrossRef]
- Zeisel, S.H. A brief history of choline. Ann. Nutr. Metab. 2012, 61, 254–258. [Google Scholar] [CrossRef]
- Liu, J.; Li, X.; Guo, Y. Recent advances in the isolation, synthesis and biological activity of marine guanidine alkaloids. Mar. Drugs 2017, 15, 324. [Google Scholar] [CrossRef]
- Kim, S.; Semenya, D.; Castagnolo, D. Antimicrobial drugs bearing guanidine moieties: A review. Eur. J. Med. Chem. 2021, 216, 113293. [Google Scholar] [CrossRef]
- Yamada, T.; Liu, X.; Englert, U.; Yamane, H.; Dronskowski, R. Solid-state structure of free base guanidine achieved at last. Chemistry 2009, 15, 5651–5655. [Google Scholar] [CrossRef]
- Watanabe, C.K. Studies in the Metabolism Changes Induced by Administration of Guanidine Bases. J. Biol. Chem. 1918, 33, 253–265. [Google Scholar] [CrossRef]
- Cameron, A.R.; Logie, L.; Patel, K.; Erhardt, S.; Bacon, S.; Middleton, P.; Harthill, J.; Forteath, C.; Coats, J.T.; Kerr, C.; et al. Metformin selectively targets redox control of complex I energy transduction. Redox Biol. 2018, 14, 187–197. [Google Scholar] [CrossRef]
- Mooney, M.H.; Fogarty, S.; Stevenson, C.; Gallagher, A.M.; Palit, P.; Hawley, S.A.; Hardie, D.G.; Coxon, G.D.; Waigh, R.D.; Tate, R.J.; et al. Mechanisms underlying the metabolic actions of galegine that contribute to weight loss in mice. Br. J. Pharmacol. 2008, 153, 1669–1677. [Google Scholar] [CrossRef]
- Wang, W.; Zhang, X. Antihypertensive effect of galegine from biebersteinia heterostemon in rats. Molecules 2021, 26, 4830. [Google Scholar] [CrossRef] [PubMed]
- Bertaccini, G.; Coruzzi, G. Extragastric H2-receptors. J. Clin. Gastroenterol. 1983, 5 (Suppl. S1), 57–70. [Google Scholar] [CrossRef] [PubMed]
- Powell, J.R.; Shamel, L.B. Characterization of vascular histamine receptors in the rat. Br. J. Pharmacol. 1979, 66, 517–520. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Müller, H.; Reinwein, H. Zur pharmakologie des galegins. Naunyn-Schmiedebergs Arch. Exp. Pathol. Pharmakol. 1927, 125, 212–228. [Google Scholar] [CrossRef]
- Bailey, C.J. Metformin: Historical overview. Diabetologia 2017, 60, 1566–1576. [Google Scholar] [CrossRef] [PubMed]
- Vera, I.M.; Ruivo MT, G.; Rocha LF, L.; Marques, S.; Bhatia, S.N.; Mota, M.M.; Mancio-Silva, L. Targeting liver stage malaria with metformin. JCI Insight 2019, 4, e127441. [Google Scholar] [CrossRef] [PubMed]
- Garcia, E.Y. Flumamine, a new synthetic analgesic and anti-flu drug. J. Philipp. Med. Assoc. 1950, 26, 287–293. [Google Scholar] [PubMed]
- Kinaan, M.; Ding, H.; Triggle, C.R. Metformin: An old drug for the treatment of diabetes but a new drug for the protection of the endothelium. Med. Princ. Pract. 2015, 24, 401–415. [Google Scholar] [CrossRef] [PubMed]
- DeFronzo, R.A.; Goodman, A.M. Efficacy of metformin in patients with non-insulin-dependent diabetes mellitus. the multicenter metformin study group. N. Engl. J. Med. 1995, 333, 541–549. [Google Scholar] [CrossRef]
- Nemeth, D.V.; Baldini, E.; Sorrenti, S.; D’Andrea, V.; Bellini, M.I. Cancer metabolism and ischemia-reperfusion injury: Two sides of the same coin. J. Clin. Med. 2022, 11, 5096. [Google Scholar] [CrossRef]
- Rosilio, C.; Ben-Sahra, I.; Bost, F.; Peyron, J. Metformin: A metabolic disruptor and anti-diabetic drug to target human leukemia. Cancer Lett. 2014, 346, 188–196. [Google Scholar] [CrossRef]
- Dowling, R.J.O.; Niraula, S.; Stambolic, V.; Goodwin, P.J. Metformin in cancer: Translational challenges. J. Mol. Endocrinol. 2012, 48, 31. [Google Scholar] [CrossRef]
- Coyle, C.; Cafferty, F.H.; Vale, C.; Langley, R.E. Metformin as an adjuvant treatment for cancer: A systematic review and meta-analysis. Ann. Oncol. 2016, 27, 2184–2195. [Google Scholar] [CrossRef]
- Marshall, S.M. 60 years of metformin use: A glance at the past and a look to the future. Diabetologia 2017, 60, 1561–1565. [Google Scholar] [CrossRef]
- Drzewoski, J.; Hanefeld, M. The current and potential therapeutic use of metformin-the good old drug. Pharmaceuticals 2021, 14, 122. [Google Scholar] [CrossRef]
- Mikulic, M. Statista. Available online: https://www.statista.com/statistics/780332/metformin-hydrochloride-prescriptions-number-in-the-us/#:~:text=Number%20of%20metformin%20prescriptions%20in%20the%20U.S.%202004%2D2021&text=In%202004%2C%20metformin%20was%20prescribed,treatment%20of%20type%202%20diabetes (accessed on 20 April 2024).
- IDF Diabetes Atlas, 10th ed.; IDF: Brussels, Belgium, 2021.
- Davies, M.J.; D’Alessio, D.A.; Fradkin, J.; Kernan, W.N.; Mathieu, C.; Mingrone, G.; Rossing, P.; Tsapas, A.; Wexler, D.J.; Buse, J.B. Management of hyperglycemia in type 2 diabetes, 2018. A consensus report by the american diabetes association (ADA) and the european association for the study of diabetes (EASD). Diabetes Care 2018, 41, 2669–2701. [Google Scholar] [CrossRef]
- Aggarwal, N.; Singla, A.; Mathieu, C.; Montanya, E.; Pfeiffer, A.F.H.; Johnsson, E.; Zhao, J.; Iqbal, N.; Bailey, C. Metformin extended-release versus immediate-release: An international, randomized, double-blind, head-to-head trial in pharmacotherapy-naïve patients with type 2 diabetes. Diabetes Obes. Metab. 2018, 20, 463–467. [Google Scholar] [CrossRef]
- Extended versus immediate-release metformin. Drug Ther. Bull. 2022, 60, 38. [CrossRef]
- Jabbour, S.; Ziring, B. Advantages of extended-release metformin in patients with type 2 diabetes mellitus. Postgrad. Med. 2011, 123, 15–23. [Google Scholar] [CrossRef] [PubMed]
- Xu, L.; Huang, Z.; He, X.; Wan, X.; Fang, D.; Li, Y. Adverse effect of metformin therapy on serum vitamin B12 and folate: Short-term treatment causes disadvantages? Med. Hypotheses. 2013, 81, 149–151. [Google Scholar] [CrossRef] [PubMed]
- Graham, G.G.; Punt, J.; Arora, M.; Day, R.O.; Doogue, M.P.; Duong, J.; Furlong, T.J.; Greenfield, J.R.; Greenup, L.C.; Kirkpatrick, C.M.; et al. Clinical pharmacokinetics of metformin. Clin. Pharmacokinet. 2011, 50, 81–98. [Google Scholar] [CrossRef]
- Wilcock, C.; Bailey, C.J. Accumulation of metformin by tissues of the normal and diabetic mouse. Xenobiotica 1994, 24, 49–57. [Google Scholar] [CrossRef]
- Foretz, M.; Guigas, B.; Bertrand, L.; Pollak, M.; Viollet, B. Metformin: From mechanisms of action to therapies. Cell. Metab. 2014, 20, 953–966. [Google Scholar] [CrossRef]
- Liang, X.; Giacomini, K.M. Transporters involved in metformin pharmacokinetics and treatment response. J. Pharm. Sci. 2017, 106, 2245–2250. [Google Scholar] [CrossRef]
- LaMoia, T.E.; Shulman, G.I. Cellular and molecular mechanisms of metformin action. Endocr. Rev. 2021, 42, 77–96. [Google Scholar] [CrossRef]
- Wang, D.; Jonker, J.W.; Kato, Y.; Kusuhara, H.; Schinkel, A.H.; Sugiyama, Y. Involvement of organic cation transporter 1 in hepatic and intestinal distribution of metformin. J. Pharmacol. Exp. Ther. 2002, 302, 510–515. [Google Scholar] [CrossRef]
- Shu, Y.; Sheardown, S.A.; Brown, C.; Owen, R.P.; Zhang, S.; Castro, R.A.; Ianculescu, A.G.; Yue, L.; Lo, J.C.; Burchard, E.G.; et al. Effect of genetic variation in the organic cation transporter 1 (OCT1) on metformin action. J. Clin. Investig. 2007, 117, 1422–1431. [Google Scholar] [CrossRef]
- Matsuzaki, S.; Humphries, K.M. Selective inhibition of deactivated mitochondrial complex I by biguanides. Biochemistry 2015, 54, 2011–2021. [Google Scholar] [CrossRef]
- Hirst, J. Mitochondrial complex I. Annu. Rev. Biochem. 2013, 82, 551–575. [Google Scholar] [CrossRef] [PubMed]
- Foretz, M.; Guigas, B.; Viollet, B. Understanding the glucoregulatory mechanisms of metformin in type 2 diabetes mellitus. Nat. Rev. Endocrinol. 2019, 15, 569–589. [Google Scholar] [CrossRef] [PubMed]
- Hardie, D.G. AMPK—Sensing energy while talking to other signaling pathways. Cell. Metab. 2014, 20, 939–952. [Google Scholar] [CrossRef]
- Zhang, Y.; Meng, Q.; Sun, Q.; Xu, Z.; Zhou, H.; Wang, Y. LKB1 deficiency-induced metabolic reprogramming in tumorigenesis and non-neoplastic diseases. Mol. Metab. 2021, 44, 101131. [Google Scholar] [CrossRef]
- Filippov, S.; Pinkosky, S.L.; Lister, R.J.; Pawloski, C.; Hanselman, J.C.; Cramer, C.T.; Srivastava, R.A.K.; Hurley, T.R.; Bradshaw, C.D.; Spahr, M.A.; et al. ETC-1002 regulates immune response, leukocyte homing, and adipose tissue inflammation via LKB1-dependent activation of macrophage AMPK. J. Lipid Res. 2013, 54, 2095–2108. [Google Scholar] [CrossRef]
- Wang, X.; Liang, Z.; Xiang, H.; Li, Y.; Chen, S.; Lu, H. LKB1 regulates vascular macrophage functions in atherosclerosis. Front. Pharmacol. 2021, 12, 810224. [Google Scholar] [CrossRef]
- He, L.; Sabet, A.; Djedjos, S.; Miller, R.; Sun, X.; Hussain, M.A.; Radovick, S.; Wondisford, F.E. Metformin and insulin suppress hepatic gluconeogenesis through phosphorylation of CREB binding protein 1. Cell 2009, 137, 635–646. [Google Scholar] [CrossRef]
- Boudaba, N.; Marion, A.; Huet, C.; Pierre, R.; Viollet, B.; Foretz, M. AMPK re-activation suppresses hepatic steatosis but its downregulation does not promote fatty liver development. EBioMedicine 2018, 28, 194–209. [Google Scholar] [CrossRef]
- Zhou, G.; Myers, R.; Li, Y.; Chen, Y.; Shen, X.; Fenyk-Melody, J.; Wu, M.; Ventre, J.; Doebber, T.; Fujii, N.; et al. Role of AMP-activated protein kinase in mechanism of metformin action. J. Clin. Investig. 2001, 108, 1167–1174. [Google Scholar] [CrossRef]
- Foretz, M.; Hébrard, S.; Leclerc, J.; Zarrinpashneh, E.; Soty, M.; Mithieux, G.; Sakamoto, K.; Andreelli, F.; Viollet, B. Metformin inhibits hepatic gluconeogenesis in mice independently of the LKB1/AMPK pathway via a decrease in hepatic energy state. J. Clin. Investig. 2010, 120, 2355–2369. [Google Scholar] [CrossRef]
- Madiraju, A.K.; Erion, D.M.; Rahimi, Y.; Zhang, X.-M.; Braddock, D.T.; Albright, R.A.; Prigaro, B.J.; Wood, J.L.; Bhanot, S.; MacDonald, M.J.; et al. Metformin suppresses gluconeogenesis by inhibiting mitochondrial glycerophosphate dehydrogenase. Nature 2014, 510, 542–546. [Google Scholar] [CrossRef]
- Bahne, E.; Sun, E.W.L.; Young, R.L.; Hansen, M.; Sonne, D.P.; Hansen, J.S.; Rohde, U.; Liou, A.P.; Jackson, M.L.; de Fontgalland, D.; et al. Metformin-induced glucagon-like peptide-1 secretion contributes to the actions of metformin in type 2 diabetes. JCI Insight 2018, 3, e93936. [Google Scholar] [CrossRef] [PubMed]
- Holst, J.J. The physiology of glucagon-like peptide. Physiol. Rev. 2007, 87, 1409–1439. [Google Scholar] [CrossRef] [PubMed]
- Hansen, M.; Scheltema, M.J.; Sonne, D.P.; Hansen, J.S.; Sperling, M.; Rehfeld, J.F.; Holst, J.J.; Vilsbøll, T.; Knop, F.K. Effect of chenodeoxycholic acid and the bile acid sequestrant colesevelam on glucagon-like peptide-1 secretion. Diabetes Obes. Metab. 2016, 18, 571–580. [Google Scholar] [CrossRef] [PubMed]
- Qin, J.; Li, Y.; Cai, Z.; Li, S.; Zhu, J.; Zhang, F.; Liang, S.; Zhang, W.; Guan, Y.; Shen, D.; et al. A metagenome-wide association study of gut microbiota in type 2 diabetes. Nature 2012, 490, 55–60. [Google Scholar] [CrossRef] [PubMed]
- Wu, H.; Esteve, E.; Tremaroli, V.; Khan, M.T.; Caesar, R.; Mannerås-Holm, L.; Ståhlman, M.; Olsson, L.M.; Serino, M.; Planas-Fèlix, M.; et al. Metformin alters the gut microbiome of individuals with treatment-naive type 2 diabetes, contributing to the therapeutic effects of the drug. Nat. Med. 2017, 23, 850–858. [Google Scholar] [CrossRef] [PubMed]
- Stratta, R.J.; Rohr, M.S.; Sundberg, A.K.; Armstrong, G.; Hairston, G.; Hartmann, E.; Farney, A.C.; Roskopf, J.P.; Iskandar, S.S.M.; Adams, P.L. Increased kidney transplantation utilizing expanded criteria deceased organ donors with results comparable to standard criteria donor transplant. Ann. Surg. 2004, 239, 688–697. [Google Scholar] [CrossRef]
- Mandal, A.K.; Kalligonis, A.N.; Ratner, L.E. Expanded criteria donors: Attempts to increase the renal transplant donor pool. Adv. Ren. Replace. Ther. 2000, 7, 117–130. [Google Scholar] [CrossRef]
- Argani, H. Expanded criteria donors. Exp. Clin. Transplant. 2022, 20 (Suppl. S4), 13–19. [Google Scholar] [CrossRef]
- Dahmen, M.; Becker, F.; Pavenstädt, H.; Suwelack, B.; Schütte-Nütgen, K.; Reuter, S. Validation of the kidney donor profile index (KDPI) to assess a deceased donor’s kidneys’ outcome in a european cohort. Sci. Rep. 2019, 9, 11234. [Google Scholar] [CrossRef]
- Kidney Donor Profile Index (KDPI) Guide for Clinicians. Available online: https://optn.transplant.hrsa.gov/professionals/by-topic/guidance/kidney-donor-profile-index-kdpi-guide-for-clinicians/#:~:text=The%20KDPI%20tells%20you%20how,associated%20with%20shorter%20estimated%20function (accessed on 20 April 2024).
- Bellini, M.I.; Courtney, A.E.; McCaughan, J.A. Living Donor Kidney Transplantation Improves Graft and Recipient Survival in Patients with Multiple Kidney Transplants. J. Clin. Med. 2020, 9, 2118. [Google Scholar] [CrossRef]
- Bachmann, Q.; Haberfellner, F.; Büttner-Herold, M.; Torrez, C.; Haller, B.; Assfalg, V.; Renders, L.; Amann, K.; Heemann, U.; Schmaderer, C.; et al. The kidney donor profile index (KDPI) correlates with histopathologic findings in post-reperfusion baseline biopsies and predicts kidney transplant outcome. Front. Med. 2022, 9, 875206. [Google Scholar] [CrossRef]
- Molinari, M.; Kaltenmeier, C.; Liu, H.; Ashwat, E.; Jorgensen, D.; Puttarajappa, C.; Wu, C.M.; Mehta, R.; Sood, P.; Shah, N.; et al. Function and longevity of renal grafts from high-KDPI donors. Clin. Transplant. 2022, 36, e14759. [Google Scholar] [CrossRef]
- van Ittersum, F.J.; Hemke, A.C.; Dekker, F.W.; Hilbrands, L.B.; Christiaans, M.H.L.; Roodnat, J.I.; Hoitsma, A.J.; van Diepen, M. Increased risk of graft failure and mortality in dutch recipients receiving an expanded criteria donor kidney transplant. Transpl. Int. 2017, 30, 14–28. [Google Scholar] [CrossRef]
- Micó-Carnero, M.; Zaouali, M.A.; Rojano-Alfonso, C.; Maroto-Serrat, C.; Ben Abdennebi, H.; Peralta, C. A potential route to reduce ischemia/reperfusion injury in organ preservation. Cells 2022, 11, 2763. [Google Scholar] [CrossRef]
- Delaura, I.F.; Gao, Q.; Anwar, I.J.; Abraham, N.; Kahan, R.; Hartwig, M.G.; Barbas, A.S. Complement-targeting therapeutics for ischemia-reperfusion injury in transplantation and the potential for ex vivo delivery. Front. Immunol. 2022, 13, 1000172. [Google Scholar] [CrossRef]
- Fard, A.; Pearson, R.; Lathan, R.; Mark, P.B.; Clancy, M.J. Perfusate composition and duration of ex-vivo normothermic perfusion in kidney transplantation: A systematic review. Transpl. Int. 2022, 35, 10236. [Google Scholar] [CrossRef]
- Cowled, P.F.R. Pathophysiology of Reperfusion Injury. 2011, 18. Available online: https://www.ncbi.nlm.nih.gov/books/NBK534267/ (accessed on 1 July 2024).
- Chatterjee, S.; Nieman, G.F.; Christie, J.D.; Fisher, A.B. Shear stress-related mechanosignaling with lung ischemia: Lessons from basic research can inform lung transplantation. Am. J. Physiol. Lung Cell. Mol. Physiol. 2014, 307, 668. [Google Scholar] [CrossRef]
- Bellini, M.I.; Yiu, J.; Nozdrin, M.; Papalois, V. The Effect of Preservation Temperature on Liver, Kidney, and Pancreas Tissue ATP in Animal and Preclinical Human Models. J. Clin. Med. 2019, 8, 1421. [Google Scholar] [CrossRef]
- Bellini, M.I.; Tortorici, F.; Amabile, M.I.; D’Andrea, V. Assessing kidney graft viability and its cells metabolism during machine perfusion. Int. J. Mol. Sci. 2021, 22, 1121. [Google Scholar] [CrossRef]
- Vial, G.; Detaille, D.; Guigas, B. Role of mitochondria in the mechanism(s) of action of metformin. Front. Endocrinol. 2019, 10, 294. [Google Scholar] [CrossRef]
- Chance, B.; Hollunger, G. The interaction of energy and electron transfer reactions in mitochondria. I. general properties and nature of the products of succinate-linked reduction of pyridine nucleotide. J. Biol. Chem. 1961, 236, 1534–1543. [Google Scholar] [CrossRef]
- Kelly, B.; Tannahill, G.M.; Murphy, M.P.; O’Neill, L.A.J. Metformin inhibits the production of reactive oxygen species from NADH:Ubiquinone oxidoreductase to limit induction of interleukin-1β (IL-1β) and boosts interleukin-10 (IL-10) in lipopolysaccharide (LPS)-activated macrophages. J. Biol. Chem. 2015, 290, 20348–20359. [Google Scholar] [CrossRef] [PubMed]
- Batandier, C.; Guigas, B.; Detaille, D.; El-Mir, M.; Fontaine, E.; Rigoulet, M.; Leverve, X.M. The ROS production induced by a reverse-electron flux at respiratory-chain complex 1 is hampered by metformin. J. Bioenerg. Biomembr. 2006, 38, 33–42. [Google Scholar] [CrossRef] [PubMed]
- Mohsin, A.A.; Chen, Q.; Quan, N.; Rousselle, T.; Maceyka, M.W.; Samidurai, A.; Thompson, J.; Hu, Y.; Li, J.; Lesnefsky, E.J. Mitochondrial complex I inhibition by metformin limits reperfusion injury. J. Pharmacol. Exp. Ther. 2019, 369, 282–290. [Google Scholar] [CrossRef] [PubMed]
- Ding, R.; Wu, W.; Sun, Z.; Li, Z. AMP-activated protein kinase: An attractive therapeutic target for ischemia-reperfusion injury. Eur. J. Pharmacol. 2020, 888, 173484. [Google Scholar] [CrossRef] [PubMed]
- Erpicum, P.; Krzesinski, J.; Jouret, F. Role of AMP-activated protein kinase in renal ischemic preconditioning. Nephrol. Ther. 2014, 10, 17–24. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Liu, X.; Wang, M.; Jiang, G.; Qiu, T.; Chen, Z.; Wang, L. Metformin attenuated the inflammation after renal ischemia/reperfusion and suppressed apoptosis of renal tubular epithelial cell in rats. Acta Cir. Bras. 2015, 30, 617–623. [Google Scholar] [CrossRef] [PubMed]
- Osorio-Llanes, E.; Villamizar-Villamizar, W.; Ospino Guerra, M.C.; Díaz-Ariza, L.A.; Castiblanco-Arroyave, S.C.; Medrano, L.; Mengual, D.; Belón, R.; Castellar-López, J.; Sepúlveda, Y.; et al. Effects of metformin on ischemia/reperfusion injury: New evidence and mechanisms. Pharmaceuticals 2023, 16, 1121. [Google Scholar] [CrossRef] [PubMed]
- Huijink, T.M.; Venema, L.H.; Posma, R.A.; de Vries, N.J.; Westerkamp, A.C.; Ottens, P.J.; Touw, D.J.; Nijsten, M.W.; Leuvenink, H.G.D. Metformin preconditioning and postconditioning to reduce ischemia reperfusion injury in an isolated ex vivo rat and porcine kidney normothermic machine perfusion model. Clin. Transl. Sci. 2021, 14, 222–230. [Google Scholar] [CrossRef] [PubMed]
- Yu, H.; Wang, J.; Liu, M.; Hu, C.; Sun, J.; Xu, B.; Lu, S.; Huang, D.; Pang, Q.; Hu, C. Metformin alleviates lung ischemia-reperfusion injury in a rat lung transplantation model. Exp. Lung Res. 2024, 50, 15–24. [Google Scholar] [CrossRef]
- Wang, M.; Liu, Y.; Liang, Y.; Naruse, K.; Takahashi, K. Systematic understanding of pathophysiological mechanisms of oxidative stress-related conditions-diabetes mellitus, cardiovascular diseases, and ischemia-reperfusion injury. Front. Cardiovasc. Med. 2021, 8, 649785. [Google Scholar] [CrossRef]
- Westerkamp, A.C.; Fujiyoshi, M.; Ottens, P.J.; Nijsten, M.W.; Touw, D.J.; de Meijer, V.E.; Lisman, T.; Leuvenink, H.G.D.; Moshage, H.; Berendsen, T.A.; et al. Metformin preconditioning improves hepatobiliary function and reduces injury in a rat model of normothermic machine perfusion and orthotopic transplantation. Transplantation 2020, 104, e271–e280. [Google Scholar] [CrossRef] [PubMed]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nemeth, D.V.; Iannelli, L.; Gangitano, E.; D’Andrea, V.; Bellini, M.I. Energy Metabolism and Metformin: Effects on Ischemia-Reperfusion Injury in Kidney Transplantation. Biomedicines 2024, 12, 1534. https://doi.org/10.3390/biomedicines12071534
Nemeth DV, Iannelli L, Gangitano E, D’Andrea V, Bellini MI. Energy Metabolism and Metformin: Effects on Ischemia-Reperfusion Injury in Kidney Transplantation. Biomedicines. 2024; 12(7):1534. https://doi.org/10.3390/biomedicines12071534
Chicago/Turabian StyleNemeth, Denise V., Leonardo Iannelli, Elena Gangitano, Vito D’Andrea, and Maria Irene Bellini. 2024. "Energy Metabolism and Metformin: Effects on Ischemia-Reperfusion Injury in Kidney Transplantation" Biomedicines 12, no. 7: 1534. https://doi.org/10.3390/biomedicines12071534
APA StyleNemeth, D. V., Iannelli, L., Gangitano, E., D’Andrea, V., & Bellini, M. I. (2024). Energy Metabolism and Metformin: Effects on Ischemia-Reperfusion Injury in Kidney Transplantation. Biomedicines, 12(7), 1534. https://doi.org/10.3390/biomedicines12071534










