Comparative Targeted Metabolomics of Ischemic Stroke: Thrombi and Serum Profiling for the Identification of Stroke-Related Metabolites
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Subjects
2.2. Clinical and Biochemical Measurements
2.3. Preparation of Stroke Thrombi for Targeted Metabolomics Analysis
2.4. Targeted Metabolomics Analysis
2.5. Statistical Analyses
3. Results
3.1. Clinical Features of the Study Population
3.2. Clinical Features of the Study Population
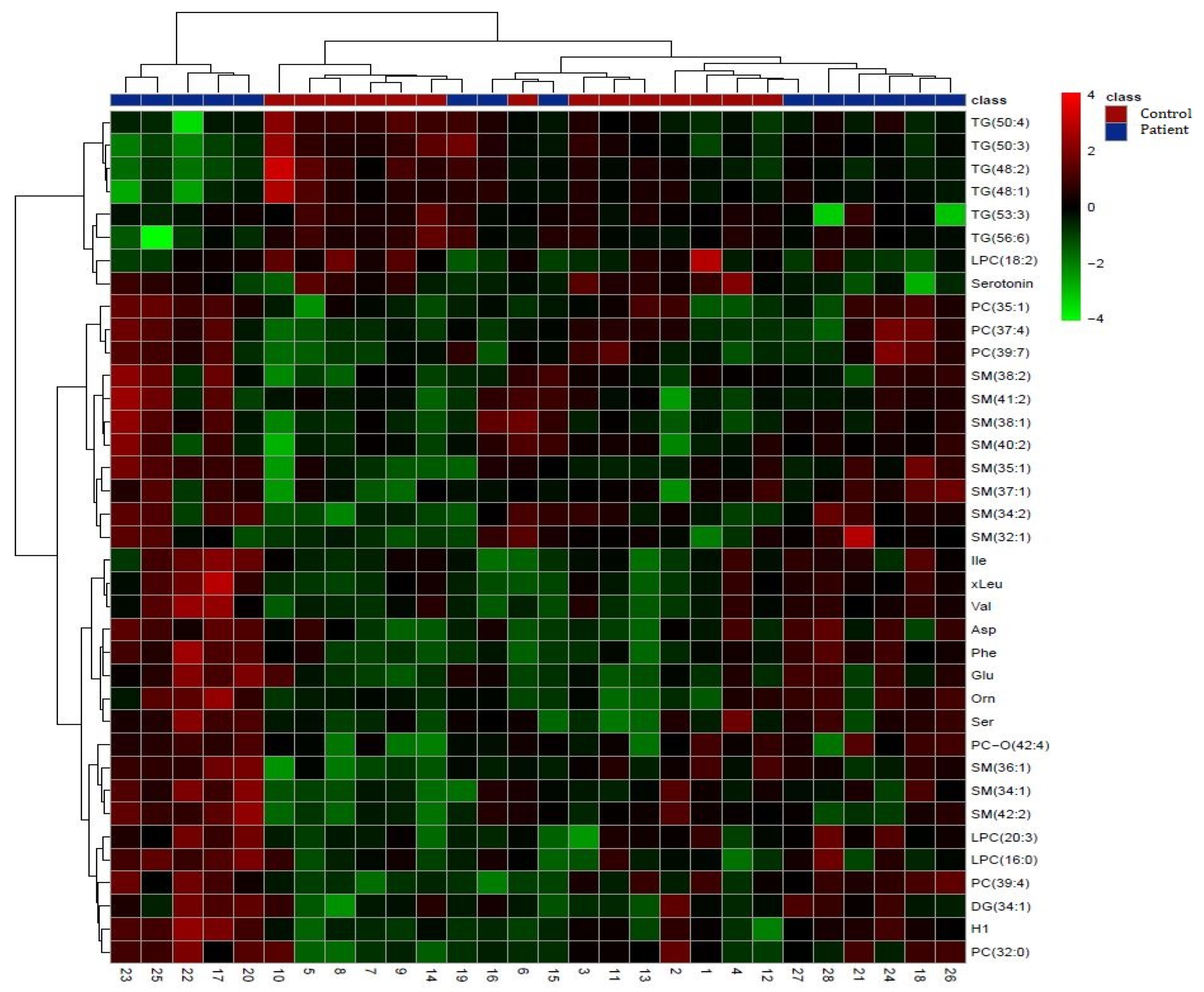
3.2.1. Comparison of Stroke Patient Serums vs. Control Serums
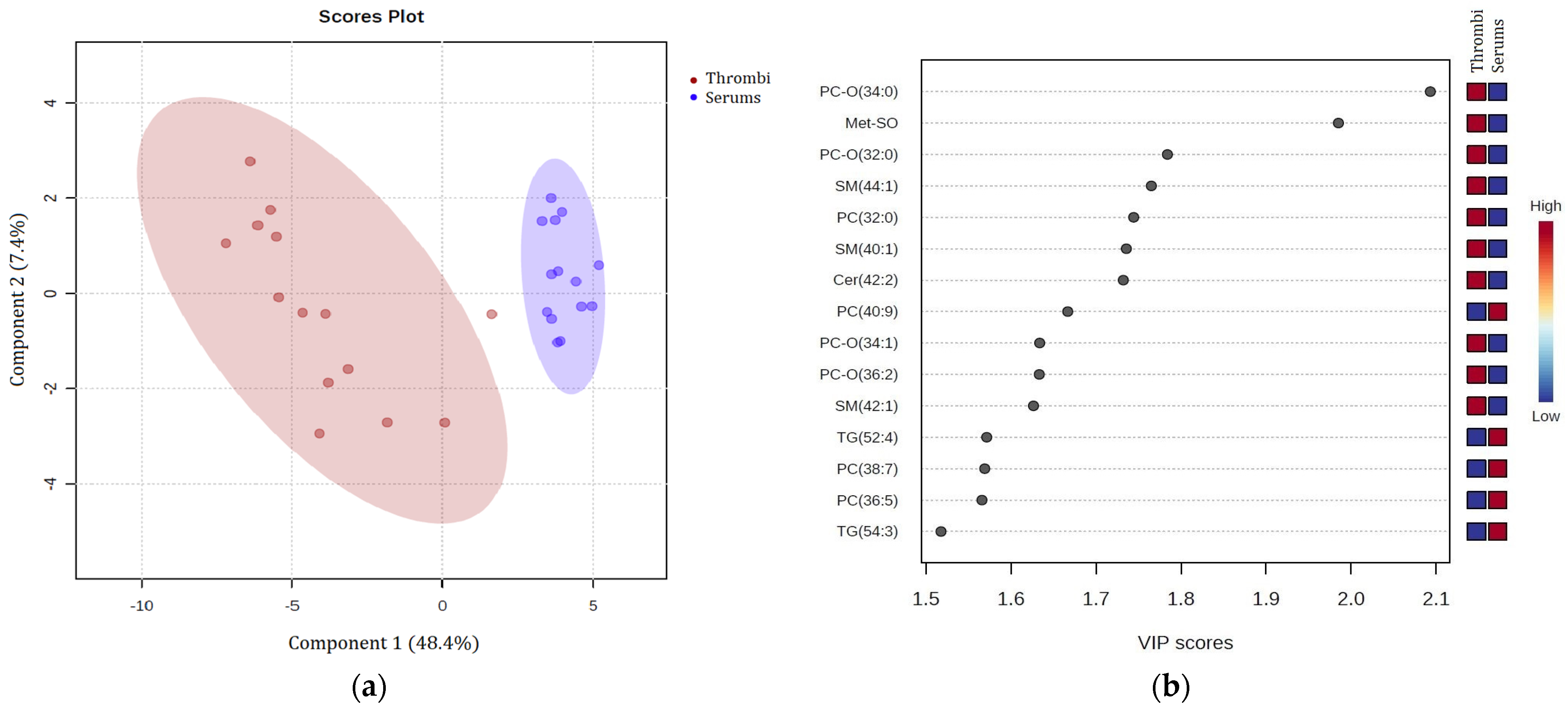
3.2.2. Comparison of Patient Stroke Thrombi vs. Stroke Patient Serum
4. Discussion
Study Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Feigin, V.L.; Brainin, M.; Norrving, B.; Martins, S.; Sacco, R.L.; Hacke, W.; Fisher, M.; Pandian, J.; Lindsay, P. World Stroke Organization (WSO): Global Stroke Fact Sheet 2022. Int. J. Stroke 2022, 17, 18–29. [Google Scholar] [CrossRef] [PubMed]
- Gorelick, P.B. The global burden of stroke: Persistent and disabling. Lancet Neurol. 2019, 18, 417–418. [Google Scholar] [CrossRef]
- Herpich, F.; Rincon, F. Management of Acute Ischemic Stroke. Crit. Care Med. 2020, 48, 1654. [Google Scholar] [CrossRef] [PubMed]
- Raha, O.; Hall, C.; Malik, A.; D’Anna, L.; Lobotesis, K.; Kwan, J.; Banerjee, S. Advances in mechanical thrombectomy for acute ischaemic stroke. BMJ Med. 2023, 2, e000407. [Google Scholar] [CrossRef]
- Meretoja, A.; Keshtkaran, M.; Saver, J.L.; Tatlisumak, T.; Parsons, M.W.; Kaste, M.; Davis, S.M.; Donnan, G.A.; Churilov, L. Stroke thrombolysis: Save a minute, save a day. Stroke 2014, 45, 1053–1058. [Google Scholar] [CrossRef] [PubMed]
- Han, T.S.; Gulli, G.; Fry, C.H.; Affley, B.; Robin, J.; Fluck, D.; Kakar, P.; Sharma, P. Adverse consequences of immediate thrombolysis-related complications: A multi-centre registry-based cohort study of acute stroke. J. Thromb. Thrombolysis 2022, 53, 218. [Google Scholar] [CrossRef] [PubMed]
- Jolugbo, P.; Ariëns, R.A.S. Thrombus Composition and Efficacy of Thrombolysis and Thrombectomy in Acute Ischemic Stroke. Stroke 2021, 52, 1131–1142. [Google Scholar] [CrossRef] [PubMed]
- Jacob, M.; Lopata, A.L.; Dasouki, M.; Abdel Rahman, A.M. Metabolomics toward personalized medicine. Mass Spectrom. Rev. 2019, 38, 221–238. [Google Scholar] [CrossRef] [PubMed]
- Daneman, R. The blood–brain barrier in health and disease. Ann. Neurol. 2012, 72, 648–672. [Google Scholar] [CrossRef] [PubMed]
- Costamagna, G.; Bonato, S.; Corti, S.; Meneri, M. Advancing Stroke Research on Cerebral Thrombi with Omic Technologies. Int. J. Mol. Sci. 2023, 24, 3419. [Google Scholar] [CrossRef]
- Khan, A.; Shin, M.S.; Jee, S.H.; Park, Y.H. Global metabolomics analysis of serum from humans at risk of thrombotic stroke. Analyst 2020, 145, 1695–1705. [Google Scholar] [CrossRef]
- Sun, D.; Tiedt, S.; Yu, B.; Jian, X.; Gottesman, R.F.; Mosley, T.H.; Boerwinkle, E.; Dichgans, M.; Fornage, M. A prospective study of serum metabolites and risk of ischemic stroke. Neurology 2019, 92, E1890–E1898. [Google Scholar] [CrossRef] [PubMed]
- Li, W.; Shao, C.; Li, C.; Zhou, H.; Yu, L.; Yang, J.; Wan, H.; He, Y. Metabolomics: A useful tool for ischemic stroke research. J. Pharm. Anal. 2023, 13, 968–983. [Google Scholar] [CrossRef] [PubMed]
- Chumachenko, M.S.; Waseem, T.V.; Fedorovich, S. V Metabolomics and metabolites in ischemic stroke. Rev. Neurosci. 2022, 33, 181–205. [Google Scholar] [CrossRef] [PubMed]
- Lee, E.J.; Kim, D.J.; Kang, D.W.; Yang, W.; Jeong, H.Y.; Kim, J.M.; Ko, S.B.; Lee, S.H.; Yoon, B.W.; Cho, J.Y.; et al. Targeted Metabolomic Biomarkers for Stroke Subtyping. Transl. Stroke Res. 2023, 15, 422–432. [Google Scholar] [CrossRef] [PubMed]
- Sidorov, E.; Sanghera, D.K.; Vanamala, J.K.P. Biomarker for Ischemic Stroke Using Metabolome: A Clinician Perspective. J. Stroke 2019, 21, 31. [Google Scholar] [CrossRef] [PubMed]
- Arul, S.; Ghozy, S.; Mereuta, O.M.; Senol, Y.C.; Orscelik, A.; Kobeissi, H.; Gupta, R.; Brinjikji, W.; Kallmes, D.F.; Kadirvel, R. Metabolite signature in acute ischemic stroke thrombi: A systematic review. J. Thromb. Thrombolysis 2023, 56, 594–602. [Google Scholar] [CrossRef] [PubMed]
- Turc, G.; Bhogal, P.; Fischer, U.; Khatri, P.; Lobotesis, K.; Mazighi, M.; Schellinger, P.D.; Toni, D.; de Vries, J.; White, P.; et al. European Stroke Organisation (ESO)—European Society for MinimallyInvasive Neurological Therapy (ESMINT) Guidelines on Mechanical Thrombectomy inAcute Ischaemic StrokeEndorsed by Stroke Alliance for Europe(SAFE). Eur. Stroke J. 2019, 4, 6. [Google Scholar] [CrossRef]
- Berge, E.; Whiteley, W.; Audebert, H.; de Marchis, G.M.; Fonseca, A.C.; Padiglioni, C.; de la Ossa, N.P.; Strbian, D.; Tsivgoulis, G.; Turc, G. European Stroke Organisation (ESO) guidelines on intravenousthrombolysis for acute ischaemic stroke. Eur. Stroke J. 2021, 6, I–LXII. [Google Scholar] [CrossRef]
- Turc, G.; Tsivgoulis, G.; Audebert, H.J.; Boogaarts, H.; Bhogal, P.; De Marchis, G.M.; Fonseca, A.C.; Khatri, P.; Mazighi, M.; Pérez de la Ossa, N.; et al. European Stroke Organisation—European Society for Minimally Invasive Neurological Therapy expedited recommendation on indication for intravenous thrombolysis before mechanical thrombectomy in patients with acute ischaemic stroke and anterior circulation large vessel occlusion. Eur. Stroke J. 2022, 7, I. [Google Scholar]
- Hrvatska Komora Medicinskih Biokemičara Priručnik o Preporučenim Metodama u Medicinsko-Biokemijskim Laboratorijima; HKMB: Zagreb, Croatia, 1998.
- Friedewald, W.T.; Levy, R.I.; Fredrickson, D.S. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin. Chem. 1972, 18, 499–502. [Google Scholar] [CrossRef] [PubMed]
- Fritsche-Guenther, R.; Gloaguen, Y.; Eisenberger, A.; Kirwan, J.A. Analysis of adherent cell culture lysates with low metabolite concentrations using the Biocrates AbsoluteIDQ p400 HR kit. Sci. Rep. 2022, 12, 7933. [Google Scholar] [CrossRef] [PubMed]
- Rubić, I.; Burchmore, R.; Weidt, S.; Regnault, C.; Kuleš, J.; Rafaj, R.B.; Mašek, T.; Horvatić, A.; Crnogaj, M.; Eckersall, P.D.; et al. Multi Platforms Strategies and Metabolomics Approaches for the Investigation of Comprehensive Metabolite Profile in Dogs with Babesia canis Infection. Int. J. Mol. Sci. 2022, 23, 1575. [Google Scholar] [CrossRef] [PubMed]
- Kuleš, J.; Rubić, I.; Beer Ljubić, B.; Bilić, P.; Barić Rafaj, R.; Brkljačić, M.; Burchmore, R.; Eckersall, D.; Mrljak, V. Combined Untargeted and Targeted Metabolomics Approaches Reveal Urinary Changes of Amino Acids and Energy Metabolism in Canine Babesiosis With Different Levels of Kidney Function. Front. Microbiol. 2021, 12, 715701. [Google Scholar] [CrossRef]
- Tao, S.; Xiao, X.; Li, X.; Na, F.; Na, G.; Wang, S.; Zhang, P.; Hao, F.; Zhao, P.; Guo, D.; et al. Targeted metabolomics reveals serum changes of amino acids in mild to moderate ischemic stroke and stroke mimics. Front. Neurol. 2023, 14, 1153193. [Google Scholar] [CrossRef] [PubMed]
- Aliprandi, A.; Longoni, M.; Stanzani, L.; Tremolizzo, L.; Vaccaro, M.; Begni, B.; Galimberti, G.; Garofolo, R.; Ferrarese, C. Increased Plasma Glutamate in Stroke Patients Might Be Linked to Altered Platelet Release and Uptake. J. Cereb. Blood Flow Metab. 2005, 25, 513–519. [Google Scholar] [CrossRef]
- Ishizaki, F. A follow-up study of platelet-rich plasma serotonin in clinical subtypes of cerebral infarction. J. Neural Transm. 1987, 69, 123–129. [Google Scholar] [CrossRef] [PubMed]
- Ban, Y.; Watanabe, T.; Miyazaki, A.; Nakano, Y.; Tobe, T.; Idei, T.; Iguchi, T.; Ban, Y.; Katagiri, T. Impact of increased plasma serotonin levels and carotid atherosclerosis on vascular dementia. Atherosclerosis 2007, 195, 153–159. [Google Scholar] [CrossRef]
- Golimbet, V.E.; Brusov, O.S.; Faktor, M.I.; Zlobina, G.P.; Lezheiko, T.V.; Lavrushina, O.M.; Petrova, E.A.; Savina, M.A.; Skvortsova, V.I. Effects of the interaction of variants of the serotonin transporter and brain-derived neurotrophic factor on platelet serotonin levels in stroke patients. Neurosci. Behav. Physiol. 2011, 41, 554–557. [Google Scholar] [CrossRef]
- Berger, M.; Gray, J.A.; Roth, B.L. The Expanded Biology of Serotonin. Annu. Rev. Med. 2009, 60, 355–366. [Google Scholar] [CrossRef]
- de Abajo, F.J. Effects of Selective Serotonin Reuptake Inhibitors on Platelet Function. Drugs Aging 2011, 28, 345–367. [Google Scholar] [CrossRef]
- Nogueira, R.G.; Qureshi, M.M.; Abdalkader, M.; Martins, S.O.; Yamagami, H.; Qiu, Z.; Mansour, O.Y.; Sathya, A.; Czlonkowska, A.; Tsivgoulis, G.; et al. Global Impact of COVID-19 on Stroke Care and IV Thrombolysis. Neurology 2021, 96, E2824–E2838. [Google Scholar] [CrossRef] [PubMed]
- Miedema, I.; Horvath, K.M.; Uyttenboogaart, M.; Koopman, K.; Lahr, M.M.H.; De Keyser, J.; Luijckx, G.J. Effect of selective serotonin re-uptake inhibitors (SSRIs) on functional outcome in patients with acute ischemic stroke treated with tPA. J. Neurol. Sci. 2010, 293, 65–67. [Google Scholar] [CrossRef] [PubMed]
- Jauhiainen, R.; Vangipurapu, J.; Laakso, A.; Kuulasmaa, T.; Kuusisto, J.; Laakso, M. The Association of 9 Amino Acids With Cardiovascular Events in Finnish Men in a 12-Year Follow-up Study. J. Clin. Endocrinol. Metab. 2021, 106, 3448. [Google Scholar] [CrossRef] [PubMed]
- Ormstad, H.; Verkerk, R.; Sandvik, L. Serum Phenylalanine, Tyrosine, and their Ratio in Acute Ischemic Stroke: On the Trail of a Biomarker? J. Mol. Neurosci. 2016, 58, 102–108. [Google Scholar] [CrossRef] [PubMed]
- Gao, J.; Yang, H.; Chen, J.; Fang, J.; Chen, C.; Liang, R.; Yang, G.; Wu, H.; Wu, C.; Li, S. Analysis of serum metabolites for the discovery of amino acid biomarkers and the effect of galangin on cerebral ischemia. Mol. Biosyst. 2013, 9, 2311–2321. [Google Scholar] [CrossRef] [PubMed]
- Cigdem, B.; Bolayir, A.; Celik, V.K.; Kapancik, S.; Kilicgun, H.; Gokce, S.F.; Gulunay, A. The Role of Reduced Polyamine Synthesis in Ischemic Stroke. Neurochem. J. 2020, 14, 243–250. [Google Scholar] [CrossRef]
- Das, A.; Fröhlich, D.; Achanta, L.B.; Rowlands, B.D.; Housley, G.D.; Klugmann, M.; Rae, C.D. L-Aspartate, L-Ornithine and L-Ornithine-L-Aspartate (LOLA) and Their Impact on Brain Energy Metabolism. Neurochem. Res. 2020, 45, 1438–1450. [Google Scholar] [CrossRef]
- Balasubramanian, R.; Hu, J.; Guasch-Ferre, M.; Li, J.; Sorond, F.; Zhao, Y.; Shutta, K.H.; Salas-Salvado, J.; Hu, F.; Clish, C.B.; et al. Metabolomic Profiles Associated With Incident Ischemic Stroke. Neurology 2022, 98, e483–e492. [Google Scholar] [CrossRef]
- Djite, M.; Chao de la Barca, J.M.; Bocca, C.; Gaye, N.M.; Barry, N.O.; Mbacke, M.N.; Cissé, O.; Kandji, P.M.; Thioune, N.M.; Coly-Gueye, N.F.; et al. A Metabolomic Signature of Ischemic Stroke Showing Acute Oxidative and Energetic Stress. Antioxidants 2024, 13, 60. [Google Scholar] [CrossRef]
- Yong, M.; Kaste, M. Dynamic of Hyperglycemia as a Predictor of Stroke Outcome in the ECASS-II Trial. Stroke 2008, 39, 2749–2755. [Google Scholar] [CrossRef] [PubMed]
- Hafez, S.; Coucha, M.; Bruno, A.; Fagan, S.C.; Ergul, A. Hyperglycemia, Acute Ischemic Stroke, and Thrombolytic Therapy. Transl. Stroke Res. 2014, 5, 442–453. [Google Scholar] [CrossRef] [PubMed]
- Robbins, N.M.; Swanson, R.A. Opposing Effects of Glucose on Stroke and Reperfusion Injury. Stroke 2014, 45, 1881–1886. [Google Scholar] [CrossRef] [PubMed]
- Udagawa, J.; Hino, K. Plasmalogen in the brain: Effects on cognitive functions and behaviors attributable to its properties. Brain Res. Bull. 2022, 188, 197–202. [Google Scholar] [CrossRef] [PubMed]
- Sagaro, G.G.; Amenta, F. Choline-Containing Phospholipids in Stroke Treatment: A Systematic Review and Meta-Analysis. J. Clin. Med. 2023, 12, 2875. [Google Scholar] [CrossRef] [PubMed]
- Holmes, M.V.; Millwood, I.Y.; Kartsonaki, C.; Hill, M.R.; Bennett, D.A.; Boxall, R.; Guo, Y.; Xu, X.; Bian, Z.; Hu, R.; et al. Lipids, Lipoproteins, and Metabolites and Risk of Myocardial Infarction and Stroke. J. Am. Coll. Cardiol. 2018, 71, 620–632. [Google Scholar] [CrossRef] [PubMed]
- Purroy, F.; Ois, A.; Jove, M.; Arque, G.; Sol, J.; Mauri-Capdevila, G.; Rodriguez-Campello, A.; Pamplona, R.; Portero, M.; Roquer, J. Lipidomic signature of stroke recurrence after transient ischemic attack. Sci. Rep. 2023, 13, 13706. [Google Scholar] [CrossRef] [PubMed]
- Romiti, E.; Vasta, V.; Meacci, E.; Farnararo, M.; Linke, T.; Ferlinz, K.; Sandhoff, K.; Bruni, P. Characterization of sphingomyelinase activity released by thrombin-stimulated platelets. Mol. Cell. Biochem. 2000, 205, 75–81. [Google Scholar] [CrossRef] [PubMed]
- Tian, H.P.; Qiu, T.Z.; Zhao, J.; Li, L.X.; Guo, J. Sphingomyelinase-induced ceramide production stimulate calcium-independent JNK and PP2A activation following cerebral ischemia. Brain Inj. 2009, 23, 1073–1080. [Google Scholar] [CrossRef]
- Gui, Y.K.; Li, Q.; Liu, L.; Zeng, P.; Ren, R.F.; Guo, Z.F.; Wang, G.H.; Song, J.G.; Zhang, P. Plasma levels of ceramides relate to ischemic stroke risk and clinical severity. Brain Res. Bull. 2020, 158, 122–127. [Google Scholar] [CrossRef]
- Xue, J.; Yu, Y.; Zhang, X.; Zhang, C.; Zhao, Y.; Liu, B.; Zhang, L.; Wang, L.; Chen, R.; Gao, X.; et al. Sphingomyelin Synthase 2 Inhibition Ameliorates Cerebral Ischemic Reperfusion Injury Through Reducing the Recruitment of Toll-Like Receptor 4 to Lipid Rafts. J. Am. Heart Assoc. 2019, 8, e012885. [Google Scholar] [CrossRef] [PubMed]




| Patient | Control | p-Value | |
|---|---|---|---|
| Age | 70.36 ± 12.82 | 52.29 ± 15.09 | 0.002 |
| Sex M/F | 8/6 | 8/6 | - |
| DTPT (min) | 202.70 ± 114.19 | - | - |
| HST (days) | 16.90 ± 9.46 | - | - |
| BMI (kg/m2) | 26.34 ± 4.07 | 23.79 ± 5.35 | 0.192 |
| DBP (mmHg) | 79.71 ± 9.21 | 83.79 ± 14.46 | 0.382 |
| SBP (mmHg) | 146.43 ± 16.70 | 135.50 ± 14.31 | 0.074 |
| TG (mmol/L) | 1.51 ± 0.47 | 1.49 ± 0.73 | 0.907 |
| tCH (mmol/L) | 5.17 ± 0.67 | 5.11 ± 1.10 | 0.874 |
| LDL-CH (mmol/L) | 3.07 ± 1.16 | 3.09 ± 1.08 | 0.962 |
| HDL-CH (mmol/L) | 1.02 ± 0.19 | 1.22 ± 0.37 | 0.079 |
| Glucose (mmol/L) | 8.12 ± 1.26 | 5.73 ± 0.85 | <0.0001 |
| PV | 0.91 ± 0.17 | 0.98 ± 0.14 | 0.251 |
| aPTT | 24.37 ± 1.79 | 23.79 ± 2.48 | 0.485 |
| INR | 1.07 ± 0.10 | 1.04 ± 0.06 | 0.464 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Karmelić, I.; Rubić, I.; Starčević, K.; Ozretić, D.; Poljaković, Z.; Sajko, M.J.; Kalousek, V.; Kalanj, R.; Rešetar Maslov, D.; Kuleš, J.; et al. Comparative Targeted Metabolomics of Ischemic Stroke: Thrombi and Serum Profiling for the Identification of Stroke-Related Metabolites. Biomedicines 2024, 12, 1731. https://doi.org/10.3390/biomedicines12081731
Karmelić I, Rubić I, Starčević K, Ozretić D, Poljaković Z, Sajko MJ, Kalousek V, Kalanj R, Rešetar Maslov D, Kuleš J, et al. Comparative Targeted Metabolomics of Ischemic Stroke: Thrombi and Serum Profiling for the Identification of Stroke-Related Metabolites. Biomedicines. 2024; 12(8):1731. https://doi.org/10.3390/biomedicines12081731
Chicago/Turabian StyleKarmelić, Ivana, Ivana Rubić, Katarina Starčević, David Ozretić, Zdravka Poljaković, Mia Jurilj Sajko, Vladimir Kalousek, Rafaela Kalanj, Dina Rešetar Maslov, Josipa Kuleš, and et al. 2024. "Comparative Targeted Metabolomics of Ischemic Stroke: Thrombi and Serum Profiling for the Identification of Stroke-Related Metabolites" Biomedicines 12, no. 8: 1731. https://doi.org/10.3390/biomedicines12081731






