Low Levels of Adropin Predict Adverse Clinical Outcomes in Outpatients with Newly Diagnosed Prediabetes after Acute Myocardial Infarction
Abstract
:1. Introduction
2. Materials and Methods
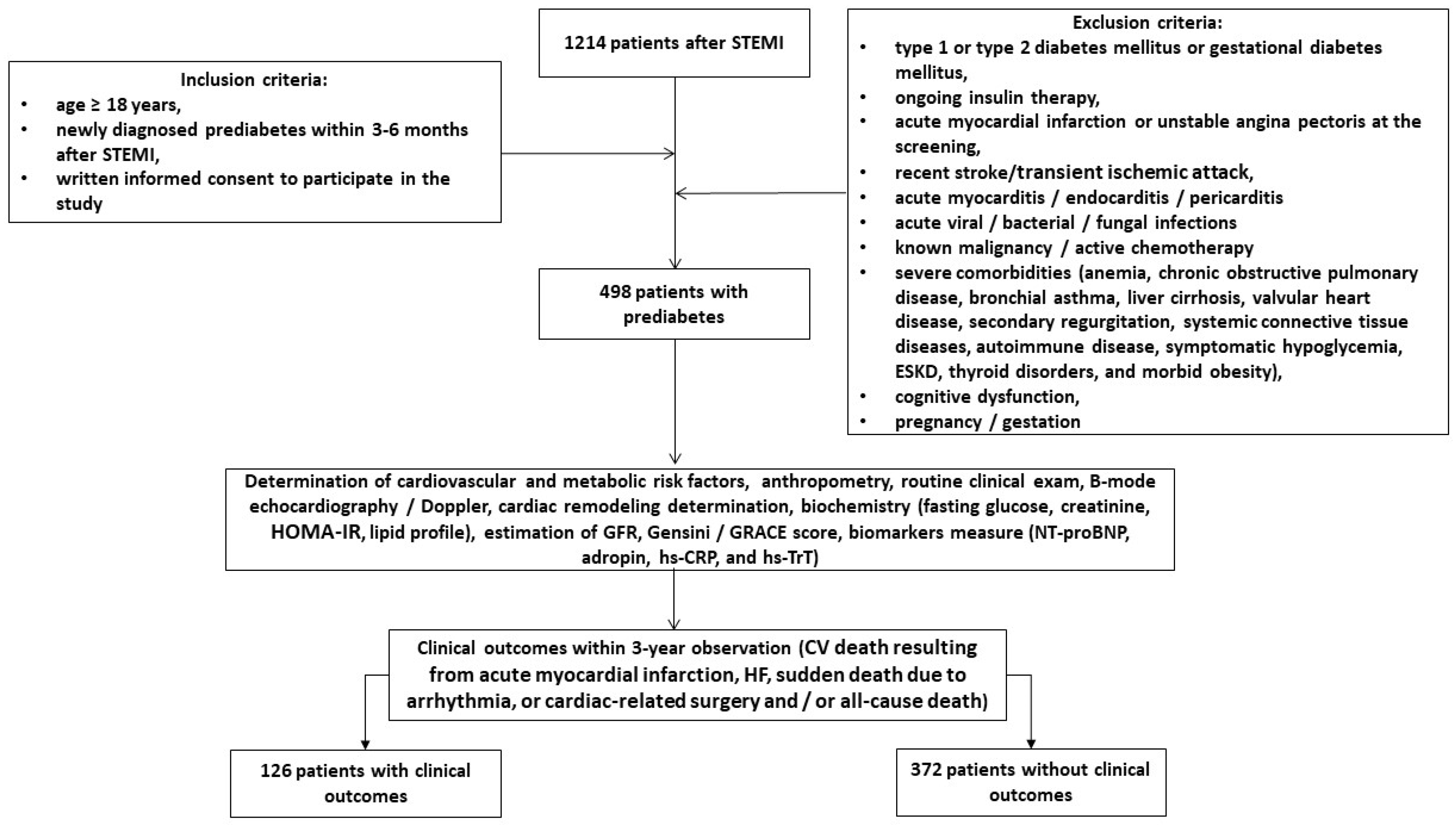
2.1. Patient Population and Study Design
2.2. Demographics and Anthropomorphic Data Collection
2.3. Clinical Outcomes Determination
2.4. Relevant Medical Data Collection
2.5. Determination of Prediabetes/Diabetes and Other Comorbidities
2.6. Echocardiography Examination
2.7. Glomerular Filtration Rate and Insulin Resistance Determination
2.8. Post-STEMI Risk Determination and Assessment of Atherosclerosis Severity
2.9. Blood Sampling
2.10. Biomarker Analysis
2.11. Statistics
3. Results
3.1. General Characteristics of the Patients
3.2. Spearman’s Correlation between the Levels of Biomarkers at Baseline and Other Parameters
3.3. The Reliability of the Predictive Ability of Adropin: The Results of the ROC Curve Analysis
3.4. Predictors for Clinical Events in Post-STEMI Patients with Prediabetes: Univariate and Multivariate Logistic Regression Analysis
3.5. Comparison of the Predictive Models
3.6. Survival of the Post-STEMI Patients with Newly Diagnosed Prediabetes Depending on Serum Levels of Adropin
4. Discussion
Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Tian, L.; Zhu, J.; Liu, L.; Liang, Y.; Li, J.; Yang, Y. Prediabetes and Short-Term Outcomes in Nondiabetic Patients after Acute ST-Elevation Myocardial Infarction. Cardiology 2013, 127, 55–61. [Google Scholar] [CrossRef]
- Pop-Busui, R.; Januzzi, J.L.; Bruemmer, D.; Butalia, S.; Green, J.B.; Horton, W.B.; Knight, C.; Levi, M.; Rasouli, N.; Richardson, C.R. Heart Failure: An Underappreciated Complication of Diabetes. A Consensus Report of the American Diabetes Association. Diabetes Care 2022, 45, 1670–1690. [Google Scholar] [CrossRef]
- Ritsinger, V.; Tanoglidi, E.; Malmberg, K.; Näsman, P.; Rydén, L.; Tenerz, Å.; Norhammar, A. Sustained prognostic implications of newly detected glucose abnormalities in patients with acute myocardial infarction: Long-term follow-up of the Glucose Tolerance in Patients with Acute Myocardial Infarction cohort. Diabetes Vasc. Dis. Res. 2014, 12, 23–32. [Google Scholar] [CrossRef]
- Norhammar, A.; Tenerz, A.; Nilsson, G.; Hamsten, A.; Efendíc, S.; Rydén, L.; Malmberg, K. Glucose metabolism in patients with acute myocardial infarction and no previous diagnosis of diabetes mellitus: A prospective study. Lancet 2002, 359, 2140–2144. [Google Scholar] [CrossRef]
- ElSayed, N.A.; Aleppo, G.; Aroda, V.R.; Bannuru, R.R.; Brown, F.M.; Bruemmer, D.; Collins, B.S.; Gaglia, J.L.; Hilliard, M.E.; Isaacs, D.; et al. 2. Classification and Diagnosis of Diabetes: Standards of Care in Diabetes—2023. Diabetes Care 2022, 46, S19–S40. [Google Scholar] [CrossRef]
- Davidson, M.B. Historical review of the diagnosis of prediabetes/intermediate hyperglycemia: Case for the international criteria. Diabetes Res. Clin. Pract. 2022, 185, 109219. [Google Scholar] [CrossRef]
- Hermanides, R.S.; Kennedy, M.W.; Kedhi, E.; van Dijk, P.R.; Timmer, J.R.; Ottervanger, J.P.; Dambrink, J.-H.; Gosselink, A.M.; Roolvink, V.; Miedema, K.; et al. Impact of elevated HbA1c on long-term mortality in patients presenting with acute myocardial infarction in daily clinical practice: Insights from a ‘real world’ prospective registry of the Zwolle Myocardial Infarction Study Group. Eur. Heart J. Acute Cardiovasc. Care 2020, 9, 616–625. [Google Scholar] [CrossRef]
- Karayiannides, S.; Djupsjö, C.; Kuhl, J.; Hofman-Bang, C.; Norhammar, A.; Holzmann, M.J.; Lundman, P. Long-term prognosis in patients with acute myocardial infarction and newly detected glucose abnormalities: Predictive value of oral glucose tolerance test and HbA1c. Cardiovasc. Diabetol. 2021, 20, 122. [Google Scholar] [CrossRef]
- Lenzen, M.; Ryden, L.; Öhrvik, J.; Bartnik, M.; Malmberg, K.; Reimer, W.S.O.; Simoons, M.L.; on behalf of the Euro Heart Survey Investigators. Diabetes known or newly detected, but not impaired glucose regulation, has a negative influence on 1-year outcome in patients with coronary artery disease: A report from the Euro Heart Survey on diabetes and the heart. Eur. Heart J. 2006, 27, 2969–2974. [Google Scholar] [CrossRef]
- Mai, L.; Wen, W.; Qiu, M.; Liu, X.; Sun, L.; Zheng, H.; Cai, X.; Huang, Y. Association between prediabetes and adverse outcomes in heart failure. Diabetes Obes. Metab. 2021, 23, 2476–2483. [Google Scholar] [CrossRef]
- Einarson, T.R.; Acs, A.; Ludwig, C.; Panton, U.H. Prevalence of cardiovascular disease in type 2 diabetes: A systematic literature review of scientific evidence from across the world in 2007–2017. Cardiovasc. Diabetol. 2018, 17, 83. [Google Scholar] [CrossRef]
- Cai, X.; Liu, X.; Sun, L.; He, Y.; Zheng, S.; Zhang, Y.; Huang, Y. Prediabetes and the risk of heart failure: A meta-analysis. Diabetes Obes. Metab. 2021, 23, 1746–1753. [Google Scholar] [CrossRef]
- Sinha, A.; Ning, H.; Ahmad, F.S.; Bancks, M.P.; Carnethon, M.R.; O’brien, M.J.; Allen, N.B.; Wilkins, J.T.; Lloyd-Jones, D.M.; Khan, S.S. Association of fasting glucose with lifetime risk of incident heart failure: The Lifetime Risk Pooling Project. Cardiovasc. Diabetol. 2021, 20, 66. [Google Scholar] [CrossRef]
- Hsu, J.-C.; Yang, Y.-Y.; Chuang, S.-L.; Lin, L.-Y.; Chen, T.H.-H. Prediabetes as a risk factor for new-onset atrial fibrillation: The propensity-score matching cohort analyzed using the Cox regression model coupled with the random survival forest. Cardiovasc. Diabetol. 2023, 22, 35. [Google Scholar] [CrossRef]
- Ritchie, R.H.; Abel, E.D. Basic Mechanisms of Diabetic Heart Disease. Circ. Res. 2020, 126, 1501–1525. [Google Scholar] [CrossRef]
- Lind, V.; Hammar, N.; Lundman, P.; Friberg, L.; Talbäck, M.; Walldius, G.; Norhammar, A. Impaired fasting glucose: A risk factor for atrial fibrillation and heart failure. Cardiovasc. Diabetol. 2021, 20, 227. [Google Scholar] [CrossRef]
- Berezin, A.E.; Berezin, A.A.; Lichtenauer, M. Emerging Role of Adipocyte Dysfunction in Inducing Heart Failure Among Obese Patients with Prediabetes and Known Diabetes Mellitus. Front. Cardiovasc. Med. 2020, 7, 583175. [Google Scholar] [CrossRef]
- Brannick, B.; Dagogo-Jack, S. Prediabetes and Cardiovascular Disease. Endocrinol. Metab. Clin. N. Am. 2018, 47, 33–50. [Google Scholar] [CrossRef]
- Berezin, A. Metabolic memory phenomenon in diabetes mellitus: Achieving and perspectives. Diabetes Metab. Syndr. Clin. Res. Rev. 2016, 10, S176–S183. [Google Scholar] [CrossRef]
- Johansson, J.S.; Boström, K.B.; Hjerpe, P.; Mourtzinis, G.; Kahan, T.; Ljungman, C. Prediabetes and incident heart failure in hypertensive patients: Results from the Swedish Primary Care Cardiovascular Database. Nutr. Metab. Cardiovasc. Dis. 2022, 32, 2803–2810. [Google Scholar] [CrossRef]
- Berezin, A.A. Impaired function of fibroblast growth factor 23/Klotho protein axis in prediabetes and diabetes mellitus: Promising predictor of cardiovascular risk. Diabetes Metab. Syndr. Clin. Res. Rev. 2019, 13, 2549–2556. [Google Scholar] [CrossRef]
- Myhre, P.L.; Lyngbakken, M.N.; Berge, T.; Røysland, R.; Aagaard, E.N.; Pervez, O.; Kvisvik, B.; Brynildsen, J.; Norseth, J.; Tveit, A.; et al. Diagnostic Thresholds for Pre–Diabetes Mellitus and Diabetes Mellitus and Subclinical Cardiac Disease in the General Population: Data from the ACE 1950 Study. J. Am. Heart Assoc. 2021, 10, e020447. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, K.; Fan, W.; Bertoni, A.; Budoff, M.J.; Defilippi, C.; Lombardo, D.; Maisel, A.; Szklo, M.; Wong, N.D. N-terminal Pro B-type Natriuretic Peptide and High-sensitivity Cardiac Troponin as Markers for Heart Failure and Cardiovascular Disease Risks According to Glucose Status (from the Multi-Ethnic Study of Atherosclerosis [MESA]). Am. J. Cardiol. 2020, 125, 1194–1201. [Google Scholar] [CrossRef]
- Jia, X.; Al Rifai, M.; Hoogeveen, R.; Echouffo-Tcheugui, J.B.; Shah, A.M.; Ndumele, C.E.; Virani, S.S.; Bozkurt, B.; Selvin, E.; Ballantyne, C.M.; et al. Association of Long-term Change in N-Terminal Pro–B-Type Natriuretic Peptide with Incident Heart Failure and Death. JAMA Cardiol. 2023, 8, 222–230. [Google Scholar] [CrossRef]
- Bachmann, K.N.; Gupta, D.K.; Xu, M.; Brittain, E.; Farber-Eger, E.; Arora, P.; Collins, S.; Wells, Q.S.; Wang, T.J. Unexpectedly Low Natriuretic Peptide Levels in Patients with Heart Failure. JACC Heart Fail. 2021, 9, 192–200. [Google Scholar] [CrossRef] [PubMed]
- Tang, W.W.; Iqbal, N.; Wu, Y.; Hazen, S.L. Usefulness of Cardiac Biomarker Score for Risk Stratification in Stable Patients Undergoing Elective Cardiac Evaluation Across Glycemic Status. Am. J. Cardiol. 2012, 111, 465–470. [Google Scholar] [CrossRef] [PubMed]
- Buchan, T.A.; Ching, C.; Foroutan, F.; Malik, A.; Daza, J.F.; Hing, N.N.F.; Siemieniuk, R.; Evaniew, N.; Orchanian-Cheff, A.; Ross, H.J.; et al. Prognostic value of natriuretic peptides in heart failure: Systematic review and meta-analysis. Heart Fail. Rev. 2021, 27, 645–654. [Google Scholar] [CrossRef] [PubMed]
- Mushala, B.A.S.; Scott, I. Adropin: A hepatokine modulator of vascular function and cardiac fuel metabolism. Am. J. Physiol. Circ. Physiol. 2020, 320, H238–H244. [Google Scholar] [CrossRef] [PubMed]
- Lovren, F.; Pan, Y.; Quan, A.; Singh, K.K.; Shukla, P.C.; Gupta, M.; Al-Omran, M.; Teoh, H.; Verma, S. Adropin Is a Novel Regulator of Endothelial Function. Circulation 2010, 122, S185–S192. [Google Scholar] [CrossRef]
- Wu, L.; Fang, J.; Yuan, X.; Xiong, C.; Chen, L. Adropin reduces hypoxia/reoxygenation-induced myocardial injury via the reperfusion injury salvage kinase pathway. Exp. Ther. Med. 2019, 18, 3307–3314. [Google Scholar] [CrossRef]
- Altamimi, T.R.; Gao, S.; Karwi, Q.G.; Fukushima, A.; Rawat, S.; Wagg, C.S.; Zhang, L.; Lopaschuk, G.D. Adropin regulates cardiac energy metabolism and improves cardiac function and efficiency. Metabolism 2019, 98, 37–48. [Google Scholar] [CrossRef]
- Aydin, S.; Eren, M.; Yilmaz, M.; Kalayci, M.; Yardim, M.; Alatas, O.; Kuloglu, T.; Balaban, H.; Cakmak, T.; Kobalt, M.; et al. Adropin as a potential marker of enzyme-positive acute coronary syndrome. Cardiovasc. J. Afr. 2017, 28, 40–47. [Google Scholar] [CrossRef]
- Jasaszwili, M.; Billert, M.; Strowski, M.Z.; Nowak, K.W.; Skrzypski, M. Adropin as A Fat-Burning Hormone with Multiple Functions—Review of a Decade of Research. Molecules 2020, 25, 549. [Google Scholar] [CrossRef] [PubMed]
- Lian, W.; Gu, X.; Qin, Y.; Zheng, X. Elevated Plasma Levels of Adropin in Heart Failure Patients. Intern. Med. 2011, 50, 1523–1527. [Google Scholar] [CrossRef]
- Yu, H.-Y.; Zhao, P.; Wu, M.-C.; Liu, J.; Yin, W. Serum adropin levels are decreased in patients with acute myocardial infarction. Regul. Pept. 2014, 190–191, 46–49. [Google Scholar] [CrossRef] [PubMed]
- Zhao, L.-P.; Xu, W.-T.; Wang, L.; You, T.; Chan, S.-P.; Zhao, X.; Yang, X.-J. Serum Adropin Level in Patients with Stable Coronary Artery Disease. Heart Lung Circ. 2015, 24, 975–979. [Google Scholar] [CrossRef]
- Berezina, T.A.; Fushtey, I.M.; Pavlov, S.V.; Berezin, A.E. Predictors of Kidney Function Outcomes and Their Relation to SGLT2 Inhibitor Dapagliflozin in Patients with Type 2 Diabetes Mellitus Who Had Chronic Heart Failure. Adv. Ther. 2023, 41, 292–314. [Google Scholar] [CrossRef]
- Berezin, A.A.; Obradovic, Z.; Novikov, E.V.; Boxhammer, E.; Lichtenauer, M.; Berezin, A.E. Interplay between Myokine Profile and Glycemic Control in Type 2 Diabetes Mellitus Patients with Heart Failure. Diagnostics 2022, 12, 2940. [Google Scholar] [CrossRef]
- Kalkan, A.K.; Cakmak, H.A.; Erturk, M.; Kalkan, K.E.; Uzun, F.; Tasbulak, O.; Diker, V.O.; Aydin, S.; Celik, A. Adropin and Irisin in Patients with Cardiac Cachexia. Arq. Bras. Cardiol. 2018, 111, 39–47. [Google Scholar] [CrossRef]
- American Diabetes Association. Standards of Care in Diabetes—2023 Abridged for Primary Care Providers. Clin. Diabetes 2023, 41, 4–31. [Google Scholar] [CrossRef]
- Stevens, P.E.; Ahmed, S.B.; Carrero, J.J.; Foster, B.; Francis, A.; Hall, R.K.; Herrington, W.G.; Hill, G.; Inker, L.A.; Kazancıoğlu, R.; et al. KDIGO 2024 Clinical Practice Guideline for the Evaluation and Management of Chronic Kidney Disease. Kidney Int. 2024, 105, S117–S314. [Google Scholar] [CrossRef]
- McDonagh, T.A.; Metra, M.; Adamo, M.; Gardner, R.S.; Baumbach, A.; Böhm, M.; Burri, H.; Butler, J.; Čelutkienė, J.; Chioncel, O.; et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur. Heart J. 2021, 42, 3599–3726, Erratum in Eur. Heart J. 2021, 42, 4901. [Google Scholar] [CrossRef]
- Williams, B.; Mancia, G.; Spiering, W.; Agabiti Rosei, E.; Azizi, M.; Burnier, M.; Clement, D.L.; Coca, A.; de Simone, G.; Dominiczak, A.; et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur. Heart J. 2018, 39, 3021–3104. [Google Scholar] [CrossRef]
- Mach, F.; Baigent, C.; Catapano, A.L.; Koskinas, K.C.; Casula, M.; Badimon, L.; Chapman, M.J.; De Backer, G.G.; Delgado, V.; Ference, B.A.; et al. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: Lipid modification to reduce cardiovascular risk: The Task Force for the management of dyslipidaemias of the European Society of Cardiology (ESC) and European Atherosclerosis Society (EAS). Eur. Heart J. 2020, 41, 111–188. [Google Scholar] [CrossRef]
- Mitchell, C.; Rahko, P.S.; Blauwet, L.A.; Canaday, B.; Finstuen, J.A.; Foster, M.C.; Horton, K.; Ogunyankin, K.O.; Palma, R.A.; Velazquez, E.J. Guidelines for Performing a Comprehensive Transthoracic Echocardiographic Examination in Adults: Recommendations from the American Society of Echocardiography. J. Am. Soc. Echocardiogr. 2018, 32, 1–64. [Google Scholar] [CrossRef] [PubMed]
- Levey, A.S.; Stevens, L.A.; Schmid, C.H.; Zhang, Y.L.; Castro, A.F., 3rd; Feldman, H.I.; Kusek, J.W.; Eggers, P.; Van Lente, F.; Greene, T.; et al. A New Equation to Estimate Glomerular Filtration Rate. Ann. Intern. Med. 2009, 150, 604–612. [Google Scholar] [CrossRef]
- Matthews, D.R.; Hosker, J.P.; Rudenski, A.S.; Naylor, B.A.; Treacher, D.F.; Turner, R.C. Homeostasis model assessment: Insulin resistance and β-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 1985, 28, 412–419. [Google Scholar] [CrossRef]
- Gensini, G.G. A more meaningful scoring system for determining the severity of coronary heart disease. Am. J. Cardiol. 1983, 51, 606. [Google Scholar] [CrossRef]
- Fox, K.A.A.; Dabbous, O.H.; Goldberg, R.J.; Pieper, K.S.; Eagle, K.A.; Van de Werf, F.; Avezum, A.; Goodman, S.G.; Flather, M.D.; Anderson, F.A.; et al. Prediction of risk of death and myocardial infarction in the six months after presentation with acute coronary syndrome: Prospective multinational observational study (GRACE). BMJ 2006, 333, 1091. [Google Scholar] [CrossRef] [PubMed]
- Seo, J.-Y.; Park, J.-S.; Seo, K.-W.; Yang, H.-M.; Lim, H.-S.; Choi, B.-J.; Choi, S.-Y.; Yoon, M.-H.; Hwang, G.-S.; Tahk, S.-J.; et al. Impact of new-onset diabetes on clinical outcomes after ST segment-elevated myocardial infarction. Scand. Cardiovasc. J. 2019, 53, 379–384. [Google Scholar] [CrossRef]
- Mehta, S.R.; Wood, D.A.; Storey, R.F.; Mehran, R.; Bainey, K.R.; Nguyen, H.; Meeks, B.; Di Pasquale, G.; López-Sendón, J.; Faxon, D.P.; et al. Complete Revascularization with Multivessel PCI for Myocardial Infarction. N. Engl. J. Med. 2019, 381, 1411–1421. [Google Scholar] [CrossRef] [PubMed]
- Bainey, K.R.; Mehta, S.R.; Lai, T.; Welsh, R.C. Complete vs culprit-only revascularization for patients with multivessel disease undergoing primary percutaneous coronary intervention for ST-segment elevation myocardial infarction: A systematic review and meta-analysis. Am. Heart J. 2013, 167, 1–14.e2. [Google Scholar] [CrossRef] [PubMed]
- Ploumen, E.H.; Pinxterhuis, T.H.; Zocca, P.; Roguin, A.; Anthonio, R.L.; Schotborgh, C.E.; Benit, E.; Aminian, A.; Danse, P.W.; Doggen, C.J.M.; et al. Impact of prediabetes and diabetes on 3-year outcome of patients treated with new-generation drug-eluting stents in two large-scale randomized clinical trials. Cardiovasc. Diabetol. 2021, 20, 217. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.H.; Her, A.-Y.; Jeong, M.H.; Kim, B.-K.; Hong, S.-J.; Kim, S.; Ahn, C.-M.; Kim, J.-S.; Ko, Y.-G.; Choi, D.; et al. Effects of prediabetes on long-term clinical outcomes of patients with acute myocardial infarction who underwent PCI using new-generation drug-eluting stents. Diabetes Res. Clin. Pract. 2019, 160, 107994. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.H.; Her, A.-Y.; Jeong, M.H.; Kim, B.-K.; Hong, S.-J.; Kim, S.; Ahn, C.-M.; Kim, J.-S.; Ko, Y.-G.; Choi, D.; et al. Two-Year Clinical Outcomes Between Prediabetic and Diabetic Patients with STEMI and Multivessel Disease Who Underwent Successful PCI Using Drug-Eluting Stents. Angiology 2020, 72, 50–61. [Google Scholar] [CrossRef]
- Oqab, Z.; Kunadian, V.; Wood, D.A.; Storey, R.F.; Rao, S.V.; Mehran, R.; Pinilla-Echeverri, N.; Mani, T.; Boone, R.H.; Kassam, S.; et al. Complete Revascularization Versus Culprit-Lesion-Only PCI in STEMI Patients with Diabetes and Multivessel Coronary Artery Disease: Results from the COMPLETE Trial. Circ. Cardiovasc. Interv. 2023, 16, e012867. [Google Scholar] [CrossRef] [PubMed]
- Cueva-Recalde, J.F.; Ruiz-Arroyo, J.R.; Roncalés García-Blanco, F. Prediabetes and coronary artery disease: Outcome after revascularization procedures. Endocrinol. Nutr. 2016, 63, 106–112. [Google Scholar] [CrossRef] [PubMed]
- Ahsan, M.J.; Latif, A.; Ahmad, S.; Willman, C.; Lateef, N.; Shabbir, M.A.; Ahsan, M.Z.; Yousaf, A.; Riasat, M.; Ghali, M.; et al. Outcomes of Prediabetes Compared with Normoglycaemia and Diabetes Mellitus in Patients Undergoing Percutaneous Coronary Intervention: A Systematic Review and Meta-analysis. Heart Int. 2023, 17, 45–53. [Google Scholar] [CrossRef] [PubMed]
- Behnoush, A.H.; Maleki, S.; Arzhangzadeh, A.; Khalaji, A.; Pezeshki, P.S.; Vaziri, Z.; Esmaeili, Z.; Ebrahimi, P.; Ashraf, H.; Masoudkabir, F.; et al. Prediabetes and major adverse cardiac events after acute coronary syndrome: An overestimated concept. Clin. Cardiol. 2024, 47. [Google Scholar] [CrossRef]
- Hosseini, K.; Khalaji, A.; Behnoush, A.H.; Soleimani, H.; Mehrban, S.; Amirsardari, Z.; Najafi, K.; Sabet, M.F.; Mohammadi, N.S.H.; Shojaei, S.; et al. The association between metabolic syndrome and major adverse cardiac and cerebrovascular events in patients with acute coronary syndrome undergoing percutaneous coronary intervention. Sci. Rep. 2024, 14, 697. [Google Scholar] [CrossRef]
- Soltani, S.; Kolahdouz-Mohammadi, R.; Aydin, S.; Yosaee, S.; Clark, C.C.T.; Abdollahi, S. Circulating levels of adropin and overweight/obesity: A systematic review and meta-analysis of observational studies. Hormones 2021, 21, 15–22. [Google Scholar] [CrossRef]
- Soltani, S.; Beigrezaei, S.; Malekahmadi, M.; Clark, C.C.T.; Abdollahi, S. Circulating levels of adropin and diabetes: A systematic review and meta-analysis of observational studies. BMC Endocr. Disord. 2023, 23, 73. [Google Scholar] [CrossRef]
- Yosaee, S.; Khodadost, M.; Esteghamati, A.; Speakman, J.R.; Shidfar, F.; Nazari, M.N.; Bitarafan, V.; Djafarian, K. Metabolic Syndrome Patients Have Lower Levels of Adropin When Compared with Healthy Overweight/Obese and Lean Subjects. Am. J. Men’s Health 2016, 11, 426–434. [Google Scholar] [CrossRef]
- Butler, A.A.; Tam, C.S.; Stanhope, K.L.; Wolfe, B.M.; Ali, M.R.; O’Keeffe, M.; St-Onge, M.-P.; Ravussin, E.; Havel, P.J. Low Circulating Adropin Concentrations with Obesity and Aging Correlate with Risk Factors for Metabolic Disease and Increase after Gastric Bypass Surgery in Humans. J. Clin. Endocrinol. Metab. 2012, 97, 3783–3791. [Google Scholar] [CrossRef]
- Niepolski, L.; Grzegorzewska, A.E. Salusins and adropin: New peptides potentially involved in lipid metabolism and atherosclerosis. Adv. Med. Sci. 2016, 61, 282–287. [Google Scholar] [CrossRef]
- Sato, K.; Yamashita, T.; Shirai, R.; Shibata, K.; Okano, T.; Yamaguchi, M.; Mori, Y.; Hirano, T.; Watanabe, T. Adropin Contributes to Anti-Atherosclerosis by Suppressing Monocyte-Endothelial Cell Adhesion and Smooth Muscle Cell Proliferation. Int. J. Mol. Sci. 2018, 19, 1293. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Xie, W. LncRNA HDAC11-AS1 Suppresses Atherosclerosis by Inhibiting HDAC11-Mediated Adropin Histone Deacetylation. J. Cardiovasc. Transl. Res. 2022, 15, 1256–1269. [Google Scholar] [CrossRef]
- Ying, T.; Wu, L.; Lan, T.; Wei, Z.; Hu, D.; Ke, Y.; Jiang, Q.; Fang, J. Adropin inhibits the progression of atherosclerosis in ApoE-/-/Enho-/- mice by regulating endothelial-to-mesenchymal transition. Cell Death Discov. 2023, 9, 402. [Google Scholar] [CrossRef]
- Močnik, M.; Varda, N.M. Current Knowledge of Selected Cardiovascular Biomarkers in Pediatrics: Kidney Injury Molecule-1, Salusin-α and -β, Uromodulin, and Adropin. Children 2022, 9, 102. [Google Scholar] [CrossRef] [PubMed]
- Rooban, S.; Senghor, K.A.; Vinodhini, V.; Kumar, J. Adropin: A crucial regulator of cardiovascular health and metabolic balance. Metab. Open 2024, 23, 100299. [Google Scholar] [CrossRef]
- A Berezina, T.; Hoppe, U.C.; Lichtenauer, M.; Berezin, A.A. Methods to predict heart failure in diabetes patients. Expert Rev. Endocrinol. Metab. 2024, 241–256. [Google Scholar] [CrossRef] [PubMed]


| Variables | Entire Group (n = 498) | Clinical Outcomes Group (n = 126) | Clinical Outcomes Free Group (n = 372) | p Value |
|---|---|---|---|---|
| Demographics/anthropometric parameters and comorbid conditions | ||||
| Age, year | 63 (51–75) | 65 (52–77) | 62 (50–75) | 0.228 |
| Male/female, n (%) | 263 (52.8)/235 (47.2) | 77 (61.1)/49 (38.9) | 186 (50.0)/186 (50.0) | 0.050 |
| BMI, kg/m2 | 26.8 ± 3.76 | 26.9 ± 3.65 | 25.5 ± 3.90 | 0.720 |
| Waist circumference, cm | 99.1 ± 5.22 | 101.2 ± 5.70 | 95.3 ± 6.17 | 0.160 |
| WHR, units | 0.92 ± 0.11 | 0.92 ± 0.10 | 0.91 ± 0.09 | 0.880 |
| Dyslipidemia, n (%) | 425 (85.3) | 113 (89.7) | 312 (83.9) | 0.254 |
| Hypertension, n (%) | 353 (70.8) | 88 (69.8) | 265 (71.2) | 0.640 |
| Chronic HF, n (%) | 216 (43.4) | 55 (43.7) | 161 (43.3) | 0.782 |
| HFpEF, n (%) | 43 (19.9) | 11 (20.0) | 32 (19.9) | 0.838 |
| HFmrEF, n (%) | 173 (80.1) | 44 (80.0) | 129 (80.1) | 0.840 |
| Atrial fibrillation, n (%) | 90 (18.1) | 24 (19.0) | 66 (17.7) | 0.060 |
| Smoking, n (%) | 211 (42.4) | 57 (45.2) | 154 (41.4) | 0.054 |
| Abdominal obesity, n (%) | 194 (39.0) | 53 (42.1) | 141 (37.9) | 0.051 |
| Left ventricular hypertrophy, n (%) | 467 (93.8) | 118 (93.7) | 349 (93.8) | 0.880 |
| CKD grades 1–3, n (%) | 131 (26.3) | 37 (29.4) | 94 (25.3) | 0.554 |
| Culprit lesion of coronary arteries and MI localization | ||||
| Left main coronary artery, n (%) | 36 (7.3) | 14 (11.1) | 22 (6.0) | 0.044 |
| Left anterior descending artery, n (%) | 218 (43.7) | 57 (45.2) | 161 (43.3) | 0.722 |
| Right coronary artery, n (%) | 190 (38.2) | 42 (33.3) | 106 (28.5) | 0.049 |
| Circumflex artery, n (%) | 54 (10.8) | 13 (10.3) | 41 (11.0) | 0.860 |
| Anterior localization, n (%) | 301 (60.4) | 80 (63.5) | 221 (59.4) | 0.050 |
| Posterior localization, n (%) | 197 (39.6) | 46 (36.5) | 151 (40.6) | 0.050 |
| Post-STEMI risk determination and severity of atherosclerosis | ||||
| GRACE score | 144 ± 37 | 148 ± 31 | 141 ± 41 | 0.620 |
| Gensini score | 32 (16–45) | 35 (18–46) | 31 (14–43) | 0.144 |
| Hemodynamic features | ||||
| Systolic BP, mm Hg | 141 ± 8 | 140 ± 8 | 139 ± 9 | 0.664 |
| Diastolic BP, mm Hg | 84 ± 7 | 87 ± 6 | 81 ± 8 | 0.612 |
| LVEDV, mL | 159 (138–167) | 162 (144–172) | 156 (137–166) | 0.474 |
| LVESV, mL | 83 (74–94) | 89 (82–100) | 81 (73–92) | 0.680 |
| LVEF, % | 48 (42–53) | 45 (41–51) | 47 (43–52) | 0.854 |
| LVMMI, g/m2 | 138 ± 11 | 140 ± 13 | 136 ± 10 | 0.442 |
| LAVI, mL/m2 | 44 (35–55) | 45 (36–56) | 42 (34–53) | 0.124 |
| E/e’, unit | 17 ± 7 | 18 ± 6 | 15 ± 5 | 0.412 |
| GLS, % | −14.9 (−12.1; −16.7) | −15.1 (−13.2; −16.9) | −14.2 (−11.9; −16.1) | 0.354 |
| Biomarkers | ||||
| eGFR, mL/min/1.73 m2 | 73 ± 15 | 66 ± 13 | 81 ± 15 | 0.126 |
| HOMA-IR, units | 7.34 ± 2.9 | 7.35 ± 2.8 | 7.22 ± 2.5 | 0.740 |
| Fasting glucose, mmol/L | 6.10 ± 0.6 | 6.11 ± 0.5 | 6.08 ± 0.7 | 0.880 |
| HbA1c, % | 5.92 ± 0.30 | 5.91 ± 0.24 | 5.90 ± 0.29 | 0.845 |
| Creatinine, µmol/L | 100.8 ± 15.1 | 116.9 ± 14.7 | 99.1 ± 15.3 | 0.412 |
| SUA, mcmol/L | 321 ± 109 | 361 ± 111 | 303 ± 78 | 0.662 |
| Total cholesterol, mmol/L | 4.92 ± 1.15 | 5.05 ± 1.13 | 4.77 ± 1.18 | 0.486 |
| HDL-C, mmol/L | 0.93 ± 0.60 | 0.94 ± 0.43 | 0.93 ± 0.60 | 0.752 |
| LDL-C, mmol/L | 3.38± 0.46 | 3.47± 0.25 | 3.24 ± 0.22 | 0.650 |
| Triglycerides, mmol/L | 1.35 ± 0.31 | 1.40 ± 0.27 | 1.33 ± 0.29 | 0.774 |
| hs-CRP, mg/L | 4.32 (2.15–6.70) | 4.60 (2.15–7.30) | 4.12 (2.10–6.56) | 0.120 |
| Adropin, pg/mL | 2.96 (1.92–4.30) | 2.14 (1.80–2.83) | 3.64 (2.70–5.58) | 0.001 |
| NT-proBNP, pmol/mL | 623 (172–1160) | 691 (210–1250) | 611 (170–1088) | 0.420 |
| hs-TnT, ng/mL | 0.06 (0.02–0.10) | 0.06 (0.01–0.08) | 0.05 (0.01–0.10) | 0.742 |
| Concomitant medications | ||||
| ACE inhibitors, n (%) | 316 (63.5) | 80 (63.5) | 236 (63.4) | 0.892 |
| Angiotensin-II receptor blockers, n (%) | 78 (15.7) | 21 (16.7) | 57 (15.3) | 0.524 |
| Beta-blockers, n (%) | 456 (91.6) | 115 (91.3) | 341 (91.7) | 0.832 |
| Ivabradine, n (%) | 82 (16.5) | 21 (16.7) | 61 (16.4) | 0.840 |
| Calcium channel blockers, n (%) | 61 (12.2) | 16 (12.7) | 45 (12.1) | 0.828 |
| Thiazide-like diuretics, n (%) | 43 (8.6) | 11 (8.7) | 32 (8.6) | 0.866 |
| Loop diuretics, n (%) | 216 (43.4) | 55 (43.7) | 161 (43.3) | 0.782 |
| MRA, n (%) | 173 (80.1) | 39 (70.9) | 134 (83.2) | 0.040 |
| Antiplatelet agents, n (%) | 429 (86.4) | 112 (88.9) | 317 (85.2) | 0.820 |
| Anticoagulants, n (%) | 90 (18.1) | 24 (19.0) | 66 (17.7) | 0.060 |
| Metformin, n (%) | 116 (23.3) | 28 (22.2) | 88 (23.7) | 0.760 |
| GLP-1 receptor agonist, n (%) | 95 (19.1) | 18 (14.3) | 77 (20.7) | 0.044 |
| SGLT2 inhibitors, n (%) | 297 (59.6) | 59 (43.7) | 238 (64.0) | 0.010 |
| Statins, n (%) | 498 (100.0) | 126 (100.0) | 372 (100.0) | 1.000 |
| Variables | NT-proBNP | Adropin | hs-CRP | |||
|---|---|---|---|---|---|---|
| r Coefficient | p Value | r Coefficient | p Value | r Coefficient | p Value | |
| LVH | 0.28 | 0.001 | −0.160 | 0.122 | 0.20 | 0.054 |
| LAVI | 0.32 | 0.001 | −0.32 | 0.001 | 0.30 | 0.001 |
| E/e’ | 0.32 | 0.001 | −0.19 | 0.062 | 0.11 | 0.246 |
| GLS | −0.37 | 0.001 | 0.32 | 0.001 | −0.07 | 0.366 |
| LVEF | −0.36 | 0.001 | 0.34 | 0.001 | −0.041 | 0.622 |
| eGFR | −0.34 | 0.001 | −0.16 | 0.060 | −0.13 | 0.255 |
| Gensini score | 0.10 | 0.058 | −0.34 | 0.001 | −0.28 | 0.001 |
| GRACE score | 0.13 | 0.054 | 0.26 | 0.001 | 0.28 | 0.001 |
| Fasting plasma glucose | 0.063 | 0.774 | −0.32 | 0.001 | 0.009 | 0.811 |
| HOMA-IR | 0.140 | 0.226 | −0.29 | 0.001 | 0.061 | 0.770 |
| HbA1c | 0.080 | 0.516 | −0.26 | 0.001 | 0.104 | 0.623 |
| Variables | Dependent Variables: Clinical Events | |||||
|---|---|---|---|---|---|---|
| Univariate Log Regression | Multivariate Log Regression | |||||
| OR | 95% CI | p Value | OR | 95% CI | p Value | |
| GRACE score ≥ 144 vs. <144 | 1.06 | 1.00–1.12 | 0.064 | - | ||
| Gensini score ≥ 32 vs. <32 | 1.10 | 1.02–2.12 | 0.001 | 1.07 | 1.04–2.10 | 0.001 |
| NT-proBNP at baseline ≥ 623 pmol/mL vs. <690 pmol/mL | 1.05 | 0.98–1.15 | 0.810 | - | ||
| Adropin ≤ 2.15 ng/mL vs. >2.15 ng/mL | 1.14 | 1.04–1.52 | 0.001 | 1.18 | 1.03–1.36 | 0.001 |
| Culprit lesion in left main coronary artery | 1.04 | 1.02–1.08 | 0.042 | 1.04 | 1.00–1.09 | 0.052 |
| Localization of MI, anterior vs. posterior | 1.03 | 1.00–1.07 | 0.168 | - | ||
| Administration of SGLT2i vs. unused SGLT2i | 0.93 | 0.89–0.98 | 0.016 | 0.94 | 0.89–0.97 | 0.010 |
| Administration of GLP-1 receptor agonist vs. unused GLP-1 receptor agonist | 0.95 | 0.92–0.99 | 0.048 | 0.95 | 0.90–0.99 | 0.040 |
| Predictive Models | Dependent Variable: Clinical Outcome | |||||
|---|---|---|---|---|---|---|
| AUC | NRI | IDI | ||||
| M (95% CI) | p Value | M (95% CI) | p Value | M (95% CI) | p Value | |
| Model 1 (Gensini score ≥ 32) | 0.802 (0.732–0.877) | - | Reference | - | Reference | - |
| Model 2 (Adropin ≤ 2.15 ng/mL) | 0.836 (0.745–0.928) | 0.012 | 0.45 (0.37–0.54) | 0.010 | 0.50 (0.44–0.57) | 0.010 |
| Model 3 (Administration of SGLT2i) | 0.815 (0.738–0.886) | 0.724 | 0.14 (0.11–0.19) | 0.266 | 0.16 (0.12–0.21) | 0.442 |
| Model 4 (Administration of GLP-1 receptor agonist) | 0.811 (0.740–0.875) | 0.760 | 0.13 (0.10–0.16) | 0.460 | 0.15 (0.10–0.21) | 0.514 |
| Model 1 + Model 2 | 0.936 (0.885–0.987) | 0.040 | 0.52 (0.46–0.61) | 0.044 | 0.54 (0.41–0.66) | 0.020 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Berezina, T.A.; Berezin, O.O.; Hoppe, U.C.; Lichtenauer, M.; Berezin, A.E. Low Levels of Adropin Predict Adverse Clinical Outcomes in Outpatients with Newly Diagnosed Prediabetes after Acute Myocardial Infarction. Biomedicines 2024, 12, 1857. https://doi.org/10.3390/biomedicines12081857
Berezina TA, Berezin OO, Hoppe UC, Lichtenauer M, Berezin AE. Low Levels of Adropin Predict Adverse Clinical Outcomes in Outpatients with Newly Diagnosed Prediabetes after Acute Myocardial Infarction. Biomedicines. 2024; 12(8):1857. https://doi.org/10.3390/biomedicines12081857
Chicago/Turabian StyleBerezina, Tetiana A., Oleksandr O. Berezin, Uta C. Hoppe, Michael Lichtenauer, and Alexander E. Berezin. 2024. "Low Levels of Adropin Predict Adverse Clinical Outcomes in Outpatients with Newly Diagnosed Prediabetes after Acute Myocardial Infarction" Biomedicines 12, no. 8: 1857. https://doi.org/10.3390/biomedicines12081857






