Selective COX-2 Inhibitors as Neuroprotective Agents in Traumatic Brain Injury
Abstract
:1. Introduction
2. Current TBI Treatment Options
3. Inflammation Following TBI
4. Anti-Inflammatory Drugs for TBI
5. Preclinical Studies
5.1. Injury Administration and Assessment
5.2. Findings in Preclinical Studies of Selective COX-2 Inhibitors
5.3. Pathology
5.4. Functional Outcomes
5.5. Evaluation of Preclinical Studies
5.6. The Role of COX-1 in Brain Injury
6. Human Studies
7. Discussion and Future Perspectives
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- Sorby-Adams, A.J.; Marcoionni, A.M.; Dempsey, E.R.; Woenig, J.A.; Turner, R.J. The Role of Neurogenic Inflammation in Blood-Brain Barrier Disruption and Development of Cerebral Oedema Following Acute Central Nervous System (CNS) Injury. Int. J. Mol. Sci. 2017, 18, 1788. [Google Scholar] [CrossRef] [PubMed]
- Dewan, M.C.; Rattani, A.; Gupta, S.; Baticulon, R.E.; Hung, Y.C.; Punchak, M.; Agrawal, A.; Adeleye, A.O.; Shrime, M.G.; Rubiano, A.M.; et al. Estimating the global incidence of traumatic brain injury. J. Neurosurg. 2018, 130, 1080–1097. [Google Scholar] [CrossRef] [PubMed]
- Stocchetti, N.; Zanier, E.R. Chronic impact of traumatic brain injury on outcome and quality of life: A narrative review. Crit. Care 2016, 20, 148. [Google Scholar] [CrossRef] [PubMed]
- Norup, A.; Kruse, M.; Soendergaard, P.L.; Rasmussen, K.W.; Biering-Sørensen, F. Socioeconomic Consequences of Traumatic Brain Injury: A Danish Nationwide Register-Based Study. J. Neurotrauma 2020, 37, 2694–2702. [Google Scholar] [CrossRef]
- Miller, G.F.; DePadilla, L.; Xu, L. Costs of Nonfatal Traumatic Brain Injury in the United States, 2016. Med. Care 2021, 59, 451–455. [Google Scholar] [CrossRef]
- Leibson, C.L.; Brown, A.W.; Hall Long, K.; Ransom, J.E.; Mandrekar, J.; Osler, T.M.; Malec, J.F. Medical care costs associated with traumatic brain injury over the full spectrum of disease: A controlled population-based study. J. Neurotrauma 2012, 29, 2038–2049. [Google Scholar] [CrossRef]
- Peeters, W.; van den Brande, R.; Polinder, S.; Brazinova, A.; Steyerberg, E.W.; Lingsma, H.F.; Maas, A.I. Epidemiology of traumatic brain injury in Europe. Acta Neurochir. 2015, 157, 1683–1696. [Google Scholar] [CrossRef]
- Roozenbeek, B.; Maas, A.I.; Menon, D.K. Changing patterns in the epidemiology of traumatic brain injury. Nat. Reviews. Neurol. 2013, 9, 231–236. [Google Scholar] [CrossRef]
- Brazinova, A.; Rehorcikova, V.; Taylor, M.S.; Buckova, V.; Majdan, M.; Psota, M.; Peeters, W.; Feigin, V.; Theadom, A.; Holkovic, L.; et al. Epidemiology of Traumatic Brain Injury in Europe: A Living Systematic Review. J. Neurotrauma 2018, 38, 1411–1440. [Google Scholar] [CrossRef]
- Ahmed, S.; Venigalla, H.; Mekala, H.M.; Dar, S.; Hassan, M.; Ayub, S. Traumatic Brain Injury and Neuropsychiatric Complications. Indian J. Psychol. Med. 2017, 39, 114–121. [Google Scholar] [CrossRef]
- Gardner, A.J.; Zafonte, R. Neuroepidemiology of traumatic brain injury. Handb. Clin. Neurol. 2016, 138, 207–223. [Google Scholar] [CrossRef]
- Hiskens, M.I.; Mengistu, T.S.; Hovinga, B.; Thornton, N.; Smith, K.B.; Mitchell, G. Epidemiology and management of traumatic brain injury in a regional Queensland Emergency Department. Australas. Emerg. Care 2023, 26, 314–320. [Google Scholar] [CrossRef] [PubMed]
- Fong, R.; Konakondla, S.; Schirmer, C.M.; Lacroix, M. Surgical interventions for severe traumatic brain injury. J. Emerg. Crit. Care Med. 2017, 1, 28. [Google Scholar] [CrossRef]
- Schäfer, M.K.; Pfeiffer, A.; Jaeckel, M.; Pouya, A.; Dolga, A.M.; Methner, A. Regulators of mitochondrial Ca(2+) homeostasis in cerebral ischemia. Cell Tissue Res. 2014, 357, 395–405. [Google Scholar] [CrossRef]
- Werner, C.; Engelhard, K. Pathophysiology of traumatic brain injury. Br. J. Anaesth. 2007, 99, 4–9. [Google Scholar] [CrossRef]
- Cash, A.; Theus, M.H. Mechanisms of Blood-Brain Barrier Dysfunction in Traumatic Brain Injury. Int. J. Mol. Sci. 2020, 21, 3344. [Google Scholar] [CrossRef] [PubMed]
- Dietvorst, S.; Depreitere, B.; Meyfroidt, G. Beyond intracranial pressure: Monitoring cerebral perfusion and autoregulation in severe traumatic brain injury. Curr. Opin. Crit. Care 2023, 29, 85–88. [Google Scholar] [CrossRef]
- Morganti-Kossmann, M.C.; Semple, B.D.; Hellewell, S.C.; Bye, N.; Ziebell, J.M. The complexity of neuroinflammation consequent to traumatic brain injury: From research evidence to potential treatments. Acta Neuropathol. 2019, 137, 731–755. [Google Scholar] [CrossRef]
- Simon, D.W.; McGeachy, M.J.; Bayir, H.; Clark, R.S.; Loane, D.J.; Kochanek, P.M. The far-reaching scope of neuroinflammation after traumatic brain injury. Nat. Rev. Neurol. 2017, 13, 171–191. [Google Scholar] [CrossRef]
- van Essen, T.A.; Lingsma, H.F.; Pisică, D.; Singh, R.D.; Volovici, V.; den Boogert, H.F.; Younsi, A.; Peppel, L.D.; Heijenbrok-Kal, M.H.; Ribbers, G.M.; et al. Surgery versus conservative treatment for traumatic acute subdural haematoma: A prospective, multicentre, observational, comparative effectiveness study. Lancet Neurol. 2022, 21, 620–631. [Google Scholar] [CrossRef]
- van Essen, T.A.; van Erp, I.A.M.; Lingsma, H.F.; Pisică, D.; Yue, J.K.; Singh, R.D.; van Dijck, J.; Volovici, V.; Younsi, A.; Kolias, A.; et al. Comparative effectiveness of decompressive craniectomy versus craniotomy for traumatic acute subdural hematoma (CENTER-TBI): An observational cohort study. EClinicalMedicine 2023, 63, 102161. [Google Scholar] [CrossRef] [PubMed]
- Gantner, D.; Wiegers, E.; Bragge, P.; Finfer, S.; Delaney, A.; van Essen, T.; Peul, W.; Maas, A.I.R.; Cooper, D.J. Decompressive Craniectomy Practice following Traumatic Brain Injury in Comparison with Randomized Trials: Harmonized, Multi-Center Cohort Studies in Europe, the United Kingdom, and Australia. J. Neurotrauma 2022, 39, 860–869. [Google Scholar] [CrossRef]
- Shah, A.; Almenawer, S.; Hawryluk, G. Timing of Decompressive Craniectomy for Ischemic Stroke and Traumatic Brain Injury: A Review. Front. Neurol. 2019, 10, 11. [Google Scholar] [CrossRef] [PubMed]
- Kolias, A.G.; Adams, H.; Timofeev, I.; Czosnyka, M.; Corteen, E.A.; Pickard, J.D.; Turner, C.; Gregson, B.A.; Kirkpatrick, P.J.; Murray, G.D.; et al. Decompressive craniectomy following traumatic brain injury: Developing the evidence base. Br. J. Neurosurg. 2016, 30, 246–250. [Google Scholar] [CrossRef]
- Hiskens, M.I. Targets of Neuroprotection and Review of Pharmacological Interventions in Traumatic Brain Injury. J. Pharmacol. Exp. Ther. 2022, 382, 149–166. [Google Scholar] [CrossRef]
- Finnie, J.W. Neuroinflammation: Beneficial and detrimental effects after traumatic brain injury. Inflammopharmacology 2013, 21, 309–320. [Google Scholar] [CrossRef] [PubMed]
- Johnson, V.E.; Meaney, D.F.; Cullen, D.K.; Smith, D.H. Animal models of traumatic brain injury. Handb. Clin. Neurol. 2015, 127, 115–128. [Google Scholar] [CrossRef]
- Kumar, A.; Loane, D.J. Neuroinflammation after traumatic brain injury: Opportunities for therapeutic intervention. Brain Behav. Immun. 2012, 26, 1191–1201. [Google Scholar] [CrossRef]
- Lozano, D.; Gonzales-Portillo, G.S.; Acosta, S.; de la Pena, I.; Tajiri, N.; Kaneko, Y.; Borlongan, C.V. Neuroinflammatory responses to traumatic brain injury: Etiology, clinical consequences, and therapeutic opportunities. Neuropsychiatr. Dis. Treat. 2015, 11, 97–106. [Google Scholar] [CrossRef]
- Woodcock, T.; Morganti-Kossmann, M.C. The role of markers of inflammation in traumatic brain injury. Front. Neurol. 2013, 4, 18. [Google Scholar] [CrossRef]
- Alam, A.; Thelin, E.P.; Tajsic, T.; Khan, D.Z.; Khellaf, A.; Patani, R.; Helmy, A. Cellular infiltration in traumatic brain injury. J. Neuroinflamm. 2020, 17, 328. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Wernersbach, I.; Strehle, J.; Li, S.; Appel, D.; Klein, M.; Ritter, K.; Hummel, R.; Tegeder, I.; Schafer, M.K.E. Early posttraumatic CSF1R inhibition via PLX3397 leads to time- and sex-dependent effects on inflammation and neuronal maintenance after traumatic brain injury in mice. Brain Behav. Immun. 2022, 106, 49–66. [Google Scholar] [CrossRef]
- Schäfer, M.K.E.; Tegeder, I. NG2/CSPG4 and progranulin in the posttraumatic glial scar. Matrix Biol. 2018, 68–69, 571–588. [Google Scholar] [CrossRef]
- Blobaum, A.L.; Marnett, L.J. Structural and functional basis of cyclooxygenase inhibition. J. Med. Chem. 2007, 50, 1425–1441. [Google Scholar] [CrossRef] [PubMed]
- Hakan, T.; Toklu, H.Z.; Biber, N.; Ozevren, H.; Solakoglu, S.; Demirturk, P.; Aker, F.V. Effect of COX-2 inhibitor meloxicam against traumatic brain injury-induced biochemical, histopathological changes and blood–brain barrier permeability. Neuro Res. 2010, 32, 629–635. [Google Scholar] [CrossRef] [PubMed]
- Shapira, Y.; Davidson, E.; Weidenfeld, Y.; Cotev, S.; Shohami, E. Dexamethasone and indomethacin do not affect brain edema following head injury in rats. J. Cereb. Blood Flow. Metab. 1988, 8, 395–402. [Google Scholar] [CrossRef]
- Edwards, P.; Arango, M.; Balica, L.; Cottingham, R.; El-Sayed, H.; Farrell, B.; Fernandes, J.; Gogichaisvili, T.; Golden, N.; Hartzenberg, B.; et al. Final results of MRC CRASH, a randomised placebo-controlled trial of intravenous corticosteroid in adults with head injury-outcomes at 6 months. Lancet 2005, 365, 1957–1959. [Google Scholar] [CrossRef]
- O’Callaghan, J.P.; Brinton, R.E.; McEwen, B.S. Glucocorticoids regulate the synthesis of glial fibrillary acidic protein in intact and adrenalectomized rats but do not affect its expression following brain injury. J. Neurochem. 1991, 57, 860–869. [Google Scholar] [CrossRef]
- Tran, N.; Kim, S.J.; Vincent, H.K.; Rodriguez, A.; Hinton, D.R.; Bullock, M.R.; Young, H.F. Aquaporin-1–mediated cerebral edema following traumatic brain injury: Effects of acidosis and corticosteroid administration. J. Neurosurg. 2010, 112, 1095–1104. [Google Scholar] [CrossRef]
- Zhang, Z.; Zhang, Z.; Artelt, M.; Burnet, M.; Schluesener, H.J. Dexamethasone attenuates early expression of three molecules associated with microglia/macrophages activation following rat traumatic brain injury. Acta Neuropathol. 2007, 113, 675–682. [Google Scholar] [CrossRef]
- Carney, N.; Totten, A.M.; O’Reilly, C.; Ullman, J.S.; Hawryluk, G.W.; Bell, M.J.; Bratton, S.L.; Chesnut, R.; Harris, O.A.; Kissoon, N.; et al. Guidelines for the Management of Severe Traumatic Brain Injury, Fourth Edition. Neurosurgery 2017, 80, 6–15. [Google Scholar] [CrossRef]
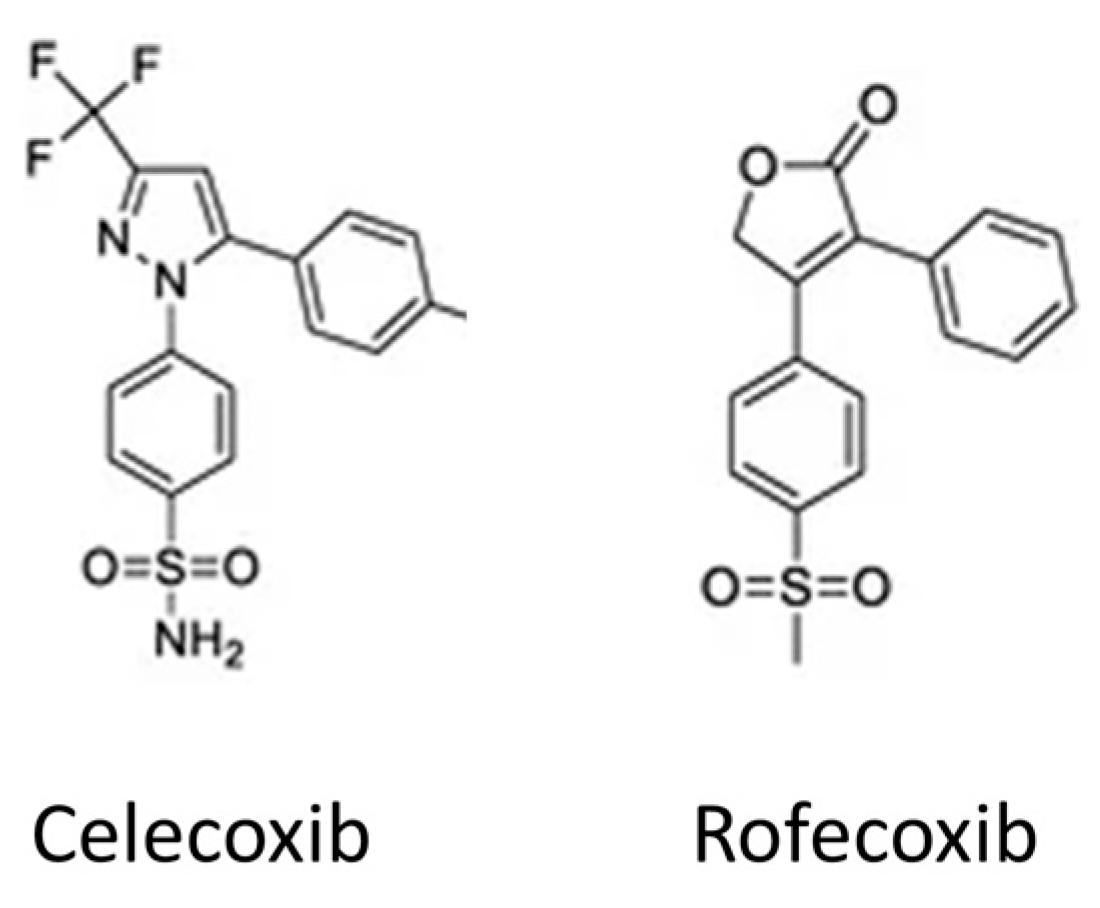
- Chakraborti, A.K.; Garg, S.K.; Kumar, R.; Motiwala, H.F.; Jadhavar, P.S. Progress in COX-2 inhibitors: A journey so far. Curr. Med. Chem. 2010, 17, 1563–1593. [Google Scholar] [CrossRef]
- Kelso, M.L.; Scheff, S.W.; Pauly, J.R.; Loftin, C.D. Effects of genetic deficiency of cyclooxygenase-1 or cyclooxygenase-2 on functional and histological outcomes following traumatic brain injury in mice. BMC Neurosci. 2009, 10, 108. [Google Scholar] [CrossRef] [PubMed]
- Allison, M.C.; Howatson, A.G.; Torrance, C.J.; Lee, F.D.; Russell, R.I. Gastrointestinal damage associated with the use of nonsteroidal antiinflammatory drugs. N. Engl. J. Med. 1992, 327, 749–754. [Google Scholar] [CrossRef] [PubMed]
- Clive, D.M.; Stoff, J.S. Renal syndromes associated with nonsteroidal antiinflammatory drugs. N. Engl. J. Med. 1984, 310, 563–572. [Google Scholar] [CrossRef] [PubMed]
- Bally, M.; Dendukuri, N.; Rich, B.; Nadeau, L.; Helin-Salmivaara, A.; Garbe, E.; Brophy, J.M. Risk of acute myocardial infarction with NSAIDs in real world use: Bayesian meta-analysis of individual patient data. BMJ 2017, 357, j1909. [Google Scholar] [CrossRef] [PubMed]
- Rogers, J.; Kirby, L.C.; Hempelman, S.R.; Berry, D.L.; McGeer, P.L.; Kaszniak, A.W.; Zalinski, J.; Cofield, M.; Mansukhani, L.; Willson, P.; et al. Clinical trial of indomethacin in Alzheimer’s disease. Neurology 1993, 43, 1609–1611. [Google Scholar] [CrossRef]
- Scharf, S.; Mander, A.; Ugoni, A.; Vajda, F.; Christophidis, N. A double-blind, placebo-controlled trial of diclofenac/misoprostol in Alzheimer’s disease. Neurology 1999, 53, 197–201. [Google Scholar] [CrossRef]
- Blasko, I.; Apochal, A.; Boeck, G.; Hartmann, T.; Grubeck-Loebenstein, B.; Ransmayr, G. Ibuprofen decreases cytokine-induced amyloid beta production in neuronal cells. Neurobiol. Dis. 2001, 8, 1094–1101. [Google Scholar] [CrossRef]
- Pompl, P.N.; Ho, L.; Bianchi, M.; McManus, T.; Qin, W.; Pasinetti, G.M. A therapeutic role for cyclooxygenase-2 inhibitors in a transgenic mouse model of amyotrophic lateral sclerosis. FASEB J. 2003, 17, 725–727. [Google Scholar] [CrossRef]
- Salzberg-Brenhouse, H.; Chen, E.; Emerich, D.; Baldwin, S.; Hogeland, K.; Ranelli, S.; Lafreniere, D.; Perdomo, B.; Novak, L.; Kladis, T. Inhibitors of cyclooxygenase-2, but not cyclooxygenase-1 provide structural and functional protection against quinolinic acid-induced neurodegeneration. J. Pharmacol. Exp. Ther. 2003, 306, 218–228. [Google Scholar] [CrossRef] [PubMed]
- Shibata, H.; Katsuki, H.; Nishiwaki, M.; Kume, T.; Kaneko, S.; Akaike, A. Lipopolysaccharide-induced dopaminergic cell death in rat midbrain slice cultures: Role of inducible nitric oxide synthase and protection by indomethacin. J. Neurochem. 2003, 86, 1201–1212. [Google Scholar] [CrossRef] [PubMed]
- Rawat, C.; Kukal, S.; Dahiya, U.R.; Kukreti, R. Cyclooxygenase-2 (COX-2) inhibitors: Future therapeutic strategies for epilepsy management. J. Neuroinflamm. 2019, 16, 197. [Google Scholar] [CrossRef] [PubMed]
- Mhillaj, E.; Morgese, M.G.; Tucci, P.; Furiano, A.; Luongo, L.; Bove, M.; Maione, S.; Cuomo, V.; Schiavone, S.; Trabace, L. Celecoxib Prevents Cognitive Impairment and Neuroinflammation in Soluble Amyloid beta-treated Rats. Neuroscience 2018, 372, 58–73. [Google Scholar] [CrossRef]
- Borre, Y.; Lemstra, S.; Westphal, K.G.; Morgan, M.E.; Olivier, B.; Oosting, R.S. Celecoxib delays cognitive decline in an animal model of neurodegeneration. Behav. Brain Res. 2012, 234, 285–291. [Google Scholar] [CrossRef]
- Teismann, P.; Tieu, K.; Choi, D.; Wu, D.; Naini, A.; Hunot, S.; Vila, M.; Jackson-Lewis, V.; Przedborski, S. Cyclooxygenase-2 is instrumental in Parkinson’s disease neurodegeneration. Proc. Natl. Acad. Sci. USA 2003, 100, 5473–5478. [Google Scholar] [CrossRef]
- Pearn, M.L.; Niesman, I.R.; Egawa, J.; Sawada, A.; Almenar-Queralt, A.; Shah, S.B.; Duckworth, J.L.; Head, B.P. Pathophysiology Associated with Traumatic Brain Injury: Current Treatments and Potential Novel Therapeutics. Cell Mol. Neurobiol. 2017, 37, 571–585. [Google Scholar] [CrossRef]
- Bergold, P.J. Treatment of traumatic brain injury with anti-inflammatory drugs. Exp. Neurol. 2016, 275 Pt 3, 367–380. [Google Scholar] [CrossRef]
- Russo, M.V.; McGavern, D.B. Inflammatory neuroprotection following traumatic brain injury. Science 2016, 353, 783–785. [Google Scholar] [CrossRef]
- Strauss, K.I. Antiinflammatory and neuroprotective actions of COX2 inhibitors in the injured brain. Brain Behav. Immun. 2008, 22, 285–298. [Google Scholar] [CrossRef]
- Hurley, S.D.; Olschowka, J.A.; O’Banion, M.K. Cyclooxygenase Inhibition as a Strategy to Ameliorate Brain Injury. J. Neurotraum 2002, 19, 1–15. [Google Scholar] [CrossRef]
- Hiskens, M.I.; Angoa-Pérez, M.; Schneiders, A.G.; Vella, R.K.; Fenning, A.S. Modeling sports-related mild traumatic brain injury in animals-A systematic review. J. Neurosci. Res. 2019, 97, 1194–1222. [Google Scholar] [CrossRef]
- Xiong, Y.; Mahmood, A.; Chopp, M. Animal models of traumatic brain injury. Nat. Rev. Neurosci. 2013, 14, 128–142. [Google Scholar] [CrossRef]
- Petersen, A.; Soderstrom, M.; Saha, B.; Sharma, P. Animal models of traumatic brain injury: A review of pathophysiology to biomarkers and treatments. Exp. Brain Res. 2021, 239, 2939–2950. [Google Scholar] [CrossRef]
- Thau-Zuchman, O.; Shohami, E.; Alexandrovich, A.G.; Trembovler, V.; Leker, R.R. The anti-inflammatory drug carprofen improves long-term outcome and induces gliogenesis after traumatic brain injury. J. Neurotrauma 2012, 29, 375–384. [Google Scholar] [CrossRef]
- Dash, P.K.; Mach, S.A.; Moore, A.N. Regional expression and role of cyclooxygenase-2 following experimental traumatic brain injury. J. Neurotrauma 2000, 17, 69–81. [Google Scholar] [CrossRef]
- Hiskens, M.; Vella, R.; Schneiders, A.; Fenning, A. Celecoxib in a preclinical model of repetitive mild traumatic brain injury: Hippocampal learning deficits persist with inflammatory and excitotoxic neuroprotection. Trauma Care 2021, 1, 23–37. [Google Scholar] [CrossRef]
- Khaksari, M.; Razmi, Z.; Hekmat, A.S.; Naderi, V.; Rostami, S. The effects of cyclooxygenase inhibitors on the brain inflammatory response following traumatic brain injury in rats. Iran. J. Basic Med. Sci. 2012, 15, 1102. [Google Scholar]
- Dehlaghi Jadid, K.; Davidsson, J.; Lidin, E.; Hånell, A.; Angéria, M.; Mathiesen, T.; Risling, M.; Günther, M. COX-2 inhibition by diclofenac is associated with decreased apoptosis and lesion area after experimental focal penetrating traumatic brain injury in rats. Front. Neurol. 2019, 10, 811. [Google Scholar] [CrossRef]
- Gopez, J.J.; Yue, H.; Vasudevan, R.; Malik, A.S.; Fogelsanger, L.N.; Lewis, S.; Panikashvili, D.; Shohami, E.; Jansen, S.A.; Narayan, R.K.; et al. Cyclooxygenase-2-specific inhibitor improves functional outcomes, provides neuroprotection, and reduces inflammation in a rat model of traumatic brain injury. Neurosurgery 2005, 56, 590–604. [Google Scholar] [CrossRef]
- Girgis, H.; Palmier, B.; Croci, N.; Soustrat, M.; Plotkine, M.; Marchand-Leroux, C. Effects of selective and non-selective cyclooxygenase inhibition against neurological deficit and brain oedema following closed head injury in mice. Brain Res. 2013, 1491, 78–87. [Google Scholar] [CrossRef]
- Cernak, I.; O’Connor, C.; Vink, R. Activation of cyclo-oxygenase-2 contributes to motor and cognitive dysfunction following diffuse traumatic brain injury in rats. Clin. Exp. Pharmacol. Physiol. 2001, 28, 922–925. [Google Scholar] [CrossRef]
- Kunz, T.; Marklund, N.; Hillered, L.; Oliw, E.H. Effects of the selective cyclooxygenase-2 inhibitor rofecoxib on cell death following traumatic brain injury in the rat. Restor. Neurol. Neurosci. 2006, 24, 55–63. [Google Scholar]
- Hickey, R.W.; Adelson, P.D.; Johnnides, M.J.; Davis, D.S.; Yu, Z.; Rose, M.E.; Chang, Y.F.; Graham, S.H. Cyclooxygenase-2 activity following traumatic brain injury in the developing rat. Pediatr. Res. 2007, 62, 271–276. [Google Scholar] [CrossRef]
- Deshpande, L.S.; Sun, D.A.; Sombati, S.; Baranova, A.; Wilson, M.S.; Attkisson, E.; Hamm, R.J.; DeLorenzo, R.J. Alterations in neuronal calcium levels are associated with cognitive deficits after traumatic brain injury. Neurosci. Lett. 2008, 441, 115–119. [Google Scholar] [CrossRef]
- Scheff, S.W.; Baldwin, S.A.; Brown, R.W.; Kraemer, P.J. Morris water maze deficits in rats following traumatic brain injury: Lateral controlled cortical impact. J. Neurotrauma 1997, 14, 615–627. [Google Scholar] [CrossRef]
- Schwab, J.M.; Beschorner, R.; Meyermann, R.; Gözalan, F.; Schluesener, H.J. Persistent accumulation of cyclooxygenase-1—Expressing microglial cells and macrophages and transient upregulation by endothelium in human brain injury. J. Neurosurg. 2002, 96, 892–899. [Google Scholar] [CrossRef]
- Karabekir, H.S.; Balci, C.; Aktepe, F.; Tokyol, C.; Dilek, H. Which is more effective in reducing secondary brain damage resulting from cyclooxygenase expression following traumatic brain injury: Calcium channel blockers or cox inhibitors? Neurosci. J. 2008, 13, 239–243. [Google Scholar]
- Shang, J.L.; Cheng, Q.; Yang, W.F.; Zhang, M.; Cui, Y.; Wang, Y.F. Possible roles of COX-1 in learning and memory impairment induced by traumatic brain injury in mice. Braz. J. Med. Biol. Res. 2014, 47, 1050–1056. [Google Scholar] [CrossRef]
- Chao, P.K.; Lu, K.T.; Jhu, J.Y.; Wo, Y.Y.P.; Huang, T.C.; Ro, L.S.; Yang, Y.L. Indomethacin protects rats from neuronal damage induced by traumatic brain injury and suppresses hippocampal IL-1β release through the inhibition of Nogo-A expression. J. Neuroinflamm. 2012, 9, 121. [Google Scholar] [CrossRef]
- Bisri, D.Y.; Arifin, Z.; Redjeki, I.S.; Listianto, H.; Bisri, T. The effect of selective COX-2 inhibitor on blood glutamate in moderate traumatic brain injury. Crit. Care Shock 2017, 20, 30. [Google Scholar]
- Bhanja, D.; Hallan, D.R.; Staub, J.; Rizk, E.; Zacko, J.C. Early Celecoxib use in Patients with Traumatic Brain Injury. Neurocrit. Care 2023, 40, 886–897. [Google Scholar] [CrossRef] [PubMed]
- Blais, V.; Turrin, N.P.; Rivest, S. Cyclooxygenase 2 (COX-2) inhibition increases the inflammatory response in the brain during systemic immune stimuli. J. Neurochem. 2005, 95, 1563–1574. [Google Scholar] [CrossRef]
- Cherry, J.D.; Olschowka, J.A.; O’Banion, M.K. Neuroinflammation and M2 microglia: The good, the bad, and the inflamed. J. Neuroinflamm. 2014, 11, 98. [Google Scholar] [CrossRef] [PubMed]
- Hanisch, U.K. Functional diversity of microglia—How heterogeneous are they to begin with? Front. Cell Neurosci. 2013, 7, 65. [Google Scholar] [CrossRef] [PubMed]
- Lourbopoulos, A.; Erturk, A.; Hellal, F. Microglia in action: How aging and injury can change the brain’s guardians. Front. Cell Neurosci. 2015, 9, 54. [Google Scholar] [CrossRef]
- Gupte, R.P.; Brooks, W.M.; Vukas, R.R.; Pierce, J.D.; Harris, J.L. Sex differences in traumatic brain injury: What we know and what we should know. J. Neurotrauma 2019, 36, 3063–3091. [Google Scholar] [CrossRef]
- Gunther, M.; Plantman, S.; Davidsson, J.; Angeria, M.; Mathiesen, T.; Risling, M. COX-2 regulation and TUNEL-positive cell death differ between genders in the secondary inflammatory response following experimental penetrating focal brain injury in rats. Acta Neurochir. 2015, 157, 649–659. [Google Scholar] [CrossRef]
- Aisen, P.S.; Schafer, K.A.; Grundman, M.; Pfeiffer, E.; Sano, M.; Davis, K.L.; Farlow, M.R.; Jin, S.; Thomas, R.G.; Thal, L.J.; et al. Effects of rofecoxib or naproxen vs placebo on Alzheimer disease progression: A randomized controlled trial. JAMA 2003, 289, 2819–2826. [Google Scholar] [CrossRef]
- Reines, S.A.; Block, G.A.; Morris, J.C.; Liu, G.; Nessly, M.L.; Lines, C.R.; Norman, B.A.; Baranak, C.C.; Rofecoxib Protocol 091 Study, G. Rofecoxib: No effect on Alzheimer’s disease in a 1-year, randomized, blinded, controlled study. Neurology 2004, 62, 66–71. [Google Scholar] [CrossRef]
- Turner, R.C.; Lucke-Wold, B.P.; Logsdon, A.F.; Robson, M.J.; Dashnaw, M.L.; Huang, J.H.; Smith, K.E.; Huber, J.D.; Rosen, C.L.; Petraglia, A.L. The Quest to Model Chronic Traumatic Encephalopathy: A Multiple Model and Injury Paradigm Experience. Front. Neurol. 2015, 6, 222. [Google Scholar] [CrossRef] [PubMed]

| Drug | Animal | Mechanism | Dosage Timeframe | Inflammation | Pathology | Neurological Outcome | Reference |
|---|---|---|---|---|---|---|---|
| Carprofen | Mouse | WD | 5 min post | ⇓ Iba-1 ⇓ Il-1β ⇨ IL-4 ⇓ IL-6 ⇨ IL-10 | ⇓ Edema ⇑ Gliogenesis ⇓ Lesion area | ⇓ NSS | Thau-Zuchman et al. (2012) [65] |
| Celecoxib | Rat | CCI | Pre-injury | - | - | ⇓ Motor ⇨ MWM ⇨ Conditioned emotional response | Dash et al. (2000) [66] |
| Celecoxib | Mouse | M-WD | Pre-injury | ⇓ Gfap ⇓ Iba-1 ⇓ TNF | ⇓ MAPT | ⇓ MWM | Hiskens et al. (2021) [67] |
| Celecoxib | Rat | WD | Pre-injury | ⇓ Il-1β ⇨ IL-10 | - | - | Khaksari et al. (2012) [68] |
| Diclofenac | Rat | CCI | Immediate | - | ⇓ Apoptosis ⇓ Lesion area ⇨ Neuronal degeneration | - | Dehlaghi et al. (2019) [69] |
| DFU | Rat | CCI | 10 min pre or 6 h post | - | ⇓ PGE2 ⇓ Caspase-3 ⇑ 2-AG | ⇓ Neuro score ⇨ Beam walk ⇨ Open-field ⇓ MWM | Gopez et al. (2005) [70] |
| Meloxicam | Rat | M-WD | 30 min post | ⇓ Lipid peroxidation ⇓ GSH ⇨ Na K ATPase | ⇓ Edema ⇓ BBB | ⇓ NSS | Hakan et al. (2010) [35] |
| Meloxicam | Mouse | WD | 10 min post | - | ⇓ 6-keto PGF1α ⇨ Edema | ⇨ Neuro score | Girgis et al. (2013) [71] |
| Nimesulide | Rat | M-WD | 30 min post | - | - | ⇓ Barnes maze ⇓ Rotarod | Cernak et al. (2001) [72] |
| Nimesulide | Mouse | WD | 10 min post | - | ⇓ 6-keto PGF1α ⇨ Edema | ⇨ Neuro score | Grigis et al. (2013) [71] |
| Roficoxib | Rat | LFP | 5 min post | - | ⇨ Neuronal degeneration | - | Kunz et al. (2006) [73] |
| SC58125 | Rat | CCI | 15 min post or 24 h post | ⇓ PGE2 ⇨ Lesion area | ⇑ MWM | Hickey et al. (2007) [74] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hiskens, M.I.; Schneiders, A.G.; Fenning, A.S. Selective COX-2 Inhibitors as Neuroprotective Agents in Traumatic Brain Injury. Biomedicines 2024, 12, 1930. https://doi.org/10.3390/biomedicines12081930
Hiskens MI, Schneiders AG, Fenning AS. Selective COX-2 Inhibitors as Neuroprotective Agents in Traumatic Brain Injury. Biomedicines. 2024; 12(8):1930. https://doi.org/10.3390/biomedicines12081930
Chicago/Turabian StyleHiskens, Matthew I., Anthony G. Schneiders, and Andrew S. Fenning. 2024. "Selective COX-2 Inhibitors as Neuroprotective Agents in Traumatic Brain Injury" Biomedicines 12, no. 8: 1930. https://doi.org/10.3390/biomedicines12081930





