Endocardial Endothelial Dysfunction and Unknown Polymorphic Composite Accumulation in Heart Failure
Abstract
:1. Introduction
2. Materials and Methods
2.1. Heart Failure Animal Model
2.2. Scanning Electron Microscopy
2.3. Energy-Dispersive X-ray Spectroscopy (EDS)
2.4. Human Sample Collection
2.5. Immunohistochemistry Staining
2.6. Statistical Analysis
3. Results
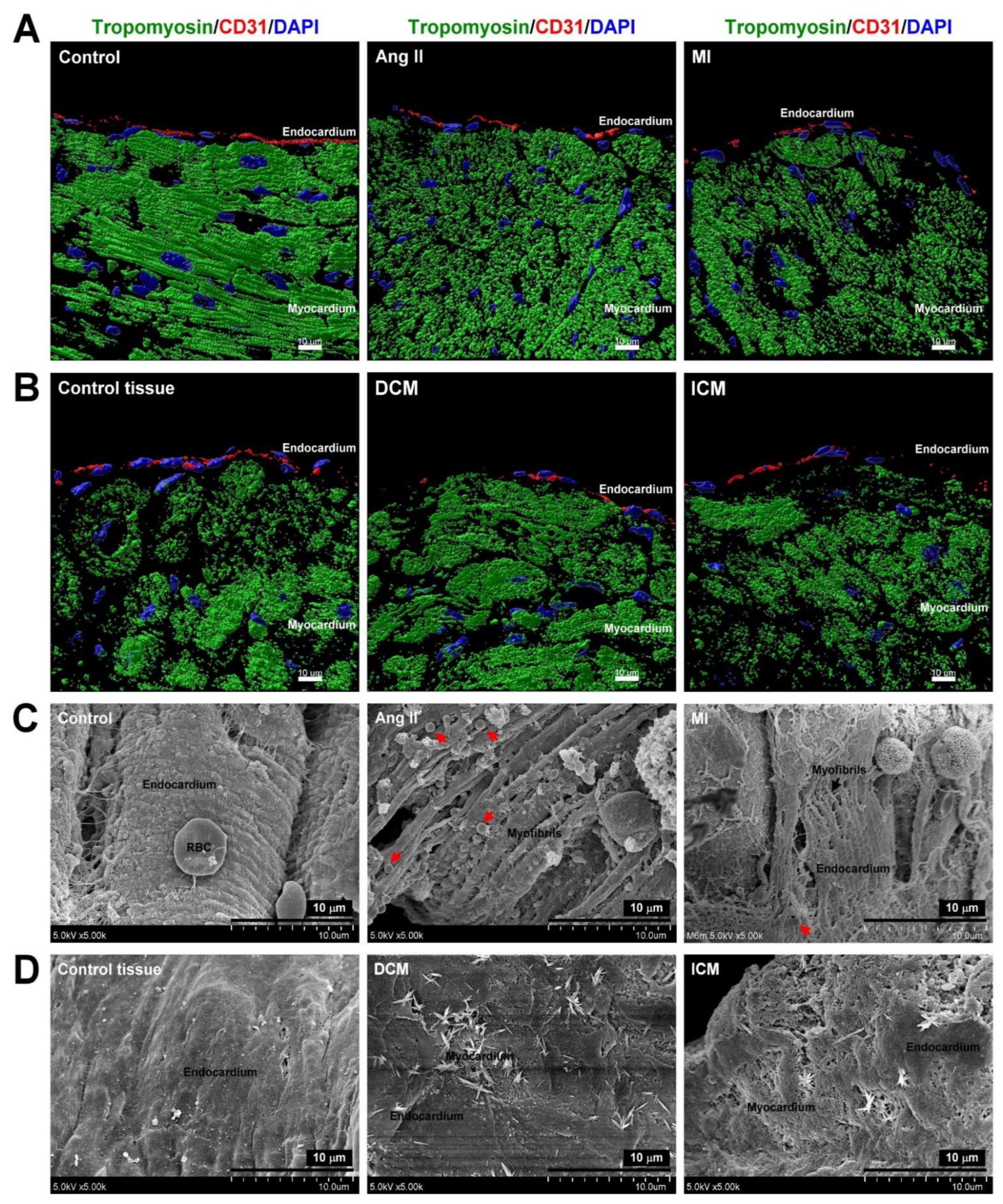
3.1. HF-Induced EE Injury Led to Myocardium Myofibril Fragmentation and Mitochondrial Rearrangement
3.2. HF-Induced Endothelial-to-Mesenchymal Transition in the Endocardium
3.3. Unknown Composite Accumulation in the Endocardium of the HF Model
3.4. Elemental Analysis of Unidentified Composite on the Endocardium in HF Models
3.5. Unidentified Composite Accumulation on Endocardium in Human HF
3.6. Elemental Analysis of Unidentified Composite on Endocardium in Human HF
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Malik, A.; Brito, D.; Chhabra, L. Congestive Heart Failure. In StatPearls, StatPearls Publishing Copyright © 2021; StatPearls Publishing LLC.: Treasure Island, FL, USA, 2021. [Google Scholar]
- Smiljic, S. The clinical significance of endocardial endothelial dysfunction. Medicina 2017, 53, 295–302. [Google Scholar] [CrossRef]
- Emam, M.A.; Abugherin, B. Histological study on the heart ventricle of Egyptian bovines (Bos aegyptiacus). Open Vet. J. 2020, 9, 281–286. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schoner, A.; Tyrrell, C.; Wu, M.; Gelow, J.M.; Hayes, A.A.; Lindner, J.R.; Thornburg, K.L.; Hasan, W. Endocardial Endothelial Dysfunction Progressively Disrupts Initially Anti then Pro-Thrombotic Pathways in Heart Failure Mice. PLoS ONE 2015, 10, e0142940. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Trochu, J.N.; Bouhour, J.B.; Kaley, G.; Hintze, T.H. Role of endothelium-derived nitric oxide in the regulation of cardiac oxygen metabolism: Implications in health and disease. Circ. Res. 2000, 87, 1108–1117. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jones, S.P.; Bolli, R. The ubiquitous role of nitric oxide in cardioprotection. J. Mol. Cell. Cardiol. 2006, 40, 16–23. [Google Scholar] [CrossRef] [PubMed]
- Noireaud, J.; Andriantsitohaina, R. Recent insights in the paracrine modulation of cardiomyocyte contractility by cardiac endothelial cells. BioMed Res. Int. 2014, 2014, 923805. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Münzel, T.; Camici, G.G.; Maack, C.; Bonetti, N.R.; Fuster, V.; Kovacic, J.C. Impact of Oxidative Stress on the Heart and Vasculature: Part 2 of a 3-Part Series. J. Am. Coll. Cardiol. 2017, 70, 212–229. [Google Scholar] [CrossRef]
- Yun, E.; Kook, Y.; Yoo, K.H.; Kim, K.I.; Lee, M.S.; Kim, J.; Lee, A. Endothelial to Mesenchymal Transition in Pulmonary Vascular Diseases. Biomedicines 2020, 8, 639. [Google Scholar] [CrossRef]
- Kovacic, J.C.; Dimmeler, S.; Harvey, R.P.; Finkel, T.; Aikawa, E.; Krenning, G.; Baker, A.H. Endothelial to Mesenchymal Transition in Cardiovascular Disease: JACC State-of-the-Art Review. J. Am. Coll. Cardiol. 2019, 73, 190–209. [Google Scholar] [CrossRef]
- Hulshoff, M.S.; Xu, X.; Krenning, G.; Zeisberg, E.M. Epigenetic Regulation of Endothelial-to-Mesenchymal Transition in Chronic Heart Disease. Arterioscler Thromb. Vasc Biol. 2018, 38, 1986–1996. [Google Scholar] [CrossRef] [Green Version]
- Li, Y.; Lui, K.O.; Zhou, B. Reassessing endothelial-to-mesenchymal transition in cardiovascular diseases. Nat. Rev. Cardiol. 2018, 15, 445–456. [Google Scholar] [CrossRef]
- Mantziari, L.; Ziakas, A.; Ventoulis, I.; Kamperidis, V.; Lilis, L.; Katsiki, N.; Karavasiliadou, S.; Kiraklidis, K.; Pliakos, C.; Gemitzis, K.; et al. Differences in Clinical Presentation and Findings between Idiopathic Dilated and Ischaemic Cardiomyopathy in an Unselected Population of Heart Failure Patients. Open Cardiovasc. Med. J. 2012, 6, 98–105. [Google Scholar] [CrossRef] [PubMed]
- Piera-Velazquez, S.; Jimenez, S.A. Endothelial to Mesenchymal Transition: Role in Physiology and in the Pathogenesis of Human Diseases. Physiol. Rev. 2019, 99, 1281–1324. [Google Scholar] [CrossRef]
- Xie, Y.; Liao, J.; Yu, Y.; Guo, Q.; Yang, Y.; Ge, J.; Chen, H.; Chen, R. Endothelial-to-mesenchymal transition in human idiopathic dilated cardiomyopathy. Mol. Med. Rep. 2018, 17, 961–969. [Google Scholar] [CrossRef]
- Wirrig, E.E.; Yutzey, K.E. Conserved transcriptional regulatory mechanisms in aortic valve development and disease. Arterioscler Thromb. Vasc Biol. 2014, 34, 737–741. [Google Scholar] [CrossRef] [Green Version]
- Hjortnaes, J.; Shapero, K.; Goettsch, C.; Hutcheson, J.D.; Keegan, J.; Kluin, J.; Mayer, J.E.; Bischoff, J.; Aikawa, E. Valvular interstitial cells suppress calcification of valvular endothelial cells. Atherosclerosis 2015, 242, 251–260. [Google Scholar] [CrossRef] [Green Version]
- Ekmekcioglu, C.; Mehrabi, M.R.; Glogar, H.D.; Jucewicz, M.; Volf, I.; Spieckermann, P.G. Oxidized low-density lipoprotein is localized in the ventricles of hearts from patients with coronary heart disease. Int. J. Clin. Lab. Res. 2000, 30, 133–140. [Google Scholar] [CrossRef]
- Kostyunin, A.; Mukhamadiyarov, R.; Glushkova, T.; Bogdanov, L.; Shishkova, D.; Osyaev, N.; Ovcharenko, E.; Kutikhin, A. Ultrastructural Pathology of Atherosclerosis, Calcific Aortic Valve Disease, and Bioprosthetic Heart Valve Degeneration: Commonalities and Differences. Int. J. Mol. Sci. 2020, 21, 7434. [Google Scholar] [CrossRef] [PubMed]
- Murphy, C.J.; Oudit, G.Y. Iron-overload cardiomyopathy: Pathophysiology, diagnosis, and treatment. J. Card. Fail. 2010, 16, 888–900. [Google Scholar] [CrossRef] [PubMed]
- Kato, T.; Sekiguchi, A.; Sagara, K.; Tanabe, H.; Takamura, M.; Kaneko, S.; Aizawa, T.; Fu, L.T.; Yamashita, T. Endothelial-mesenchymal transition in human atrial fibrillation. J. Cardiol. 2017, 69, 706–711. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bergström, J.; Gustavsson, A.; Hellman, U.; Sletten, K.; Murphy, C.L.; Weiss, D.T.; Solomon, A.; Olofsson, B.O.; Westermark, P. Amyloid deposits in transthyretin-derived amyloidosis: Cleaved transthyretin is associated with distinct amyloid morphology. J. Pathol. 2005, 206, 224–232. [Google Scholar] [CrossRef]
- Birnie, D.H.; Nery, P.B.; Ha, A.C.; Beanlands, R.S. Cardiac Sarcoidosis. J. Am. Coll. Cardiol. 2016, 68, 411–421. [Google Scholar] [CrossRef]
- Palaniswamy, C.; Frishman, W.H.; Aronow, W.S. Carcinoid heart disease. Cardiol. Rev. 2012, 20, 167–176. [Google Scholar] [CrossRef] [PubMed]
- Kampmann, C. Enzyme replacement therapy and the heart. In Fabry Disease: Perspectives from 5 Years of FOS; Mehta, A., Beck, M., Sunder-Plassmann, G., Eds.; Oxford PharmaGenesis Copyright © 2021, Oxford PharmaGenesis™: Oxford, UK, 2006. [Google Scholar]
- Hsieh, C.C.; Li, C.Y.; Hsu, C.H.; Chen, H.L.; Chen, Y.H.; Liu, Y.P.; Liu, Y.R.; Kuo, H.F.; Liu, P.L. Mitochondrial protection by simvastatin against angiotensin II-mediated heart failure. Br. J. Pharmacol. 2019, 176, 3791–3804. [Google Scholar] [CrossRef] [Green Version]
- Wei, B.; Lin, Q.; Ji, Y.G.; Zhao, Y.C.; Ding, L.N.; Zhou, W.J.; Zhang, L.H.; Gao, C.Y.; Zhao, W. Luteolin ameliorates rat myocardial ischaemia-reperfusion injury through activation of peroxiredoxin II. Br. J. Pharmacol. 2018, 175, 3315–3332. [Google Scholar] [CrossRef]
- Andries, L.J.; Kaluza, G.; De Keulenaer, G.W.; Mebazaa, A.; Brutsaert, D.L.; Sys, S.U. Endocardial endothelial dysfunction and heart failure. J. Card. Fail. 1996, 2, S195–S202. [Google Scholar] [CrossRef]
- Hoeeg, C.; Frljak, S.; Qayyum, A.A.; Vrtovec, B.; Kastrup, J.; Ekblond, A.; Follin, B. Efficacy and Mode of Action of Mesenchymal Stem Cells in Non-Ischemic Dilated Cardiomyopathy: A Systematic Review. Biomedicines 2020, 8, 570. [Google Scholar] [CrossRef] [PubMed]
- Brieler, J.; Breeden, M.A.; Tucker, J. Cardiomyopathy: An Overview. Am. Fam. Physician 2017, 96, 640–646. [Google Scholar] [PubMed]
- Argulian, E.; Sherrid, M.V.; Messerli, F.H. Misconceptions and Facts About Hypertrophic Cardiomyopathy. Am. J. Med. 2016, 129, 148–152. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Maron, B.J.; Towbin, J.A.; Thiene, G.; Antzelevitch, C.; Corrado, D.; Arnett, D.; Moss, A.J.; Seidman, C.E.; Young, J.B. Contemporary definitions and classification of the cardiomyopathies: An American Heart Association Scientific Statement from the Council on Clinical Cardiology, Heart Failure and Transplantation Committee; Quality of Care and Outcomes Research and Functional Genomics and Translational Biology Interdisciplinary Working Groups; and Council on Epidemiology and Prevention. Circulation 2006, 113, 1807–1816. [Google Scholar] [PubMed] [Green Version]
- Wu, Y.; Yin, X.; Wijaya, C.; Huang, M.H.; McConnell, B.K. Acute myocardial infarction in rats. J. Vis. Exp. 2011, 48, 2464. [Google Scholar] [CrossRef] [Green Version]
- Weinheimer, C.J.; Kovacs, A.; Evans, S.; Matkovich, S.J.; Barger, P.M.; Mann, D.L. Load-Dependent Changes in Left Ventricular Structure and Function in a Pathophysiologically Relevant Murine Model of Reversible Heart Failure. Circ. Heart Fail. 2018, 11, e004351. [Google Scholar] [CrossRef] [PubMed]
- Wang, G.; Cruz, A.S.; Youker, K.; Marcos-Abdala, H.G.; Thandavarayan, R.A.; Cooke, J.P.; Torre-Amione, G.; Chen, K.; Bhimaraj, A. Role of Endothelial and Mesenchymal Cell Transitions in Heart Failure and Recovery Thereafter. Front. Genet. 2020, 11, 609262. [Google Scholar] [CrossRef] [PubMed]
- Sun, X.; Sun, Y.; Jiang, P.; Qi, G.; Chen, X. Crosstalk between endothelial cell-specific calpain inhibition and the endothelial-mesenchymal transition via the HSP90/Akt signaling pathway. Biomed. Pharmacother. 2020, 124, 109822. [Google Scholar] [CrossRef] [PubMed]
- Piera-Velazquez, S.; Li, Z.; Jimenez, S.A. Role of endothelial-mesenchymal transition (EndoMT) in the pathogenesis of fibrotic disorders. Am. J. Pathol. 2011, 179, 1074–1080. [Google Scholar] [CrossRef] [PubMed]
- Fialová, M.; Dlugošová, K.; Okruhlicová, L.; Kristek, F.; Manoach, M.; Tribulová, N. Adaptation of the heart to hypertension is associated with maladaptive gap junction connexin-43 remodeling. Physiol. Res. 2008, 57, 7–11. [Google Scholar] [CrossRef] [PubMed]
- Xu, A.; Deng, F.; Chen, Y.; Kong, Y.; Pan, L.; Liao, Q.; Rao, Z.; Xie, L.; Yao, C.; Li, S.; et al. NF-κB pathway activation during endothelial-to-mesenchymal transition in a rat model of doxorubicin-induced cardiotoxicity. Biomed. Pharmacother. 2020, 130, 110525. [Google Scholar] [CrossRef]
- Xiao, L.; Dudley, A.C. Fine-tuning vascular fate during endothelial-mesenchymal transition. J. Pathol. 2017, 241, 25–35. [Google Scholar] [CrossRef]
- Wang, B.; Ge, Z.; Wu, Y.; Zha, Y.; Zhang, X.; Yan, Y.; Xie, Y. MFGE8 is down-regulated in cardiac fibrosis and attenuates endothelial-mesenchymal transition through Smad2/3-Snail signalling pathway. J. Cell. Mol. Med. 2020, 24, 12799–12812. [Google Scholar] [CrossRef]
- Bayoumi, A.S.; Teoh, J.P.; Aonuma, T.; Yuan, Z.; Ruan, X.; Tang, Y.; Su, H.; Weintraub, N.L.; Kim, I.M. MicroRNA-532 protects the heart in acute myocardial infarction, and represses prss23, a positive regulator of endothelial-to-mesenchymal transition. Cardiovasc. Res. 2017, 113, 1603–1614. [Google Scholar] [CrossRef]
- Zhang, Y.; Wu, X.; Li, Y.; Zhang, H.; Li, Z.; Zhang, Y.; Zhang, L.; Ju, J.; Liu, X.; Chen, X.; et al. Endothelial to mesenchymal transition contributes to arsenic-trioxide-induced cardiac fibrosis. Sci. Rep. 2016, 6, 33787. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, S.J.; Lee, I.K.; Jeon, J.H. Vascular Calcification-New Insights Into Its Mechanism. Int. J. Mol. Sci. 2020, 21, 2685. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wu, M.; Rementer, C.; Giachelli, C.M. Vascular calcification: An update on mechanisms and challenges in treatment. Calcif. Tissue Int. 2013, 93, 365–373. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez, M.; Hernandez, M.; Cheungpasitporn, W.; Kashani, K.B.; Riaz, I.; Rangaswami, J.; Herzog, E.; Guglin, M.; Krittanawong, C. Hyponatremia in Heart Failure: Pathogenesis and Management. Curr. Cardiol. Rev. 2019, 15, 252–261. [Google Scholar] [CrossRef] [PubMed]
- Holland-Bill, L.; Christiansen, C.F.; Heide-Jørgensen, U.; Ulrichsen, S.P.; Ring, T.; Jørgensen, J.O.; Sørensen, H.T. Hyponatremia and mortality risk: A Danish cohort study of 279 508 acutely hospitalized patients. Eur. J. Endocrinol. 2015, 173, 71–81. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Donzé, J.D.; Beeler, P.E.; Bates, D.W. Impact of Hyponatremia Correction on the Risk for 30-Day Readmission and Death in Patients with Congestive Heart Failure. Am. J. Med. 2016, 129, 836–842. [Google Scholar] [CrossRef] [Green Version]






| Element | Control | Ang II | MI | |
|---|---|---|---|---|
| C | Weight% | 61.83 ± 4.81 | 53.8 ± 1.61 * | 4.47 ± 0.59 ** |
| Atomic% | 71.31 ± 4.38 | 63.27 ± 1.26 * | 6.48 ± 0.85 ** | |
| O | Weight% | 25.27 ± 4.24 | 33.236 ± 0.31 * | 59.31 ± 1.39 ** |
| Atomic% | 21.93 ± 3.98 | 29.35 ± 0.34 * | 64.52 ± 1.46 ** | |
| Na | Weight% | 6.88 ± 0.56 | 9.51± 1.30 * | 25.72 ± 3.2 ** |
| Atomic% | 4.554 ± 0.4 | 6.713 ± 0.85 * | 21.884 ± 2.41 ** | |
| S | Weight% | 6 ± 0.9 | 3.44 ± 0.47 * | 5.03 ± 2.06 |
| Atomic% | 2.59 ± 0.42 | 1.52 ± 0.21 * | 2.73 ± 1.13 | |
| N | Weight% | ND | ND | 5.46 ± 1.1 ** |
| Atomic% | ND | ND | 6.79 ± 0.77 ** | |
| Element | Control Tissue | DCM | ICM | |
|---|---|---|---|---|
| O | Weight% | 20.22 ± 4.75 | 30.08 ± 3.42 * | 30.79 ± 3.99 * |
| Atomic% | 17.25 ± 4.29 | 29.13 ± 3.69 * | 27.66 ± 3.91 * | |
| C | Weight% | 54.96 ± 5.8 | 34.29 ± 2.53 ** | 42.77 ± 1.73 * |
| Atomic% | 62.32 ± 5.86 | 44.15 ± 2.59 ** | 51.23 ± 1.28 * | |
| Na | Weight% | 4.3 ± 0.67 | 13.17± 1.04 ** | 7.29 ± 0.93 ** |
| Atomic% | 2.94 ± 0.39 | 9.69 ± 0.81 ** | 5.19 ± 0.63 ** | |
| S | Weight% | 3.82 ± 0.73 | 11.15 ± 1.63 ** | 5.03 ± 2.24 * |
| Atomic% | 1.62 ± 0.31 | 5.38 ± 0.35 ** | 2.26 ± 0.13 * | |
| N | Weight% | 16.69 ± 4.63 | 11.29 ± 3.97 | 14.06 ± 6.17 |
| Atomic% | 16 ± 2.51 | 12.45 ± 2.22 | 14.38 ± 3.27 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kuo, H.-F.; Liu, I.-F.; Li, C.-Y.; Tsai, C.-S.; Chen, Y.-H.; Lian, W.-S.; Lin, T.-C.; Liu, Y.-R.; Lee, T.-Y.; Huang, C.-Y.; et al. Endocardial Endothelial Dysfunction and Unknown Polymorphic Composite Accumulation in Heart Failure. Biomedicines 2021, 9, 1465. https://doi.org/10.3390/biomedicines9101465
Kuo H-F, Liu I-F, Li C-Y, Tsai C-S, Chen Y-H, Lian W-S, Lin T-C, Liu Y-R, Lee T-Y, Huang C-Y, et al. Endocardial Endothelial Dysfunction and Unknown Polymorphic Composite Accumulation in Heart Failure. Biomedicines. 2021; 9(10):1465. https://doi.org/10.3390/biomedicines9101465
Chicago/Turabian StyleKuo, Hsuan-Fu, I-Fan Liu, Chia-Yang Li, Chien-Sung Tsai, Yung-Hsiang Chen, Wei-Shiung Lian, Tzu-Chieh Lin, Yu-Ru Liu, Tsung-Ying Lee, Chi-Yuan Huang, and et al. 2021. "Endocardial Endothelial Dysfunction and Unknown Polymorphic Composite Accumulation in Heart Failure" Biomedicines 9, no. 10: 1465. https://doi.org/10.3390/biomedicines9101465








