Non-Oncologic Applications of Nanomedicine-Based Phototherapy
Abstract
1. Introduction
2. Mechanisms of Nanomedicine-Based Phototherapy
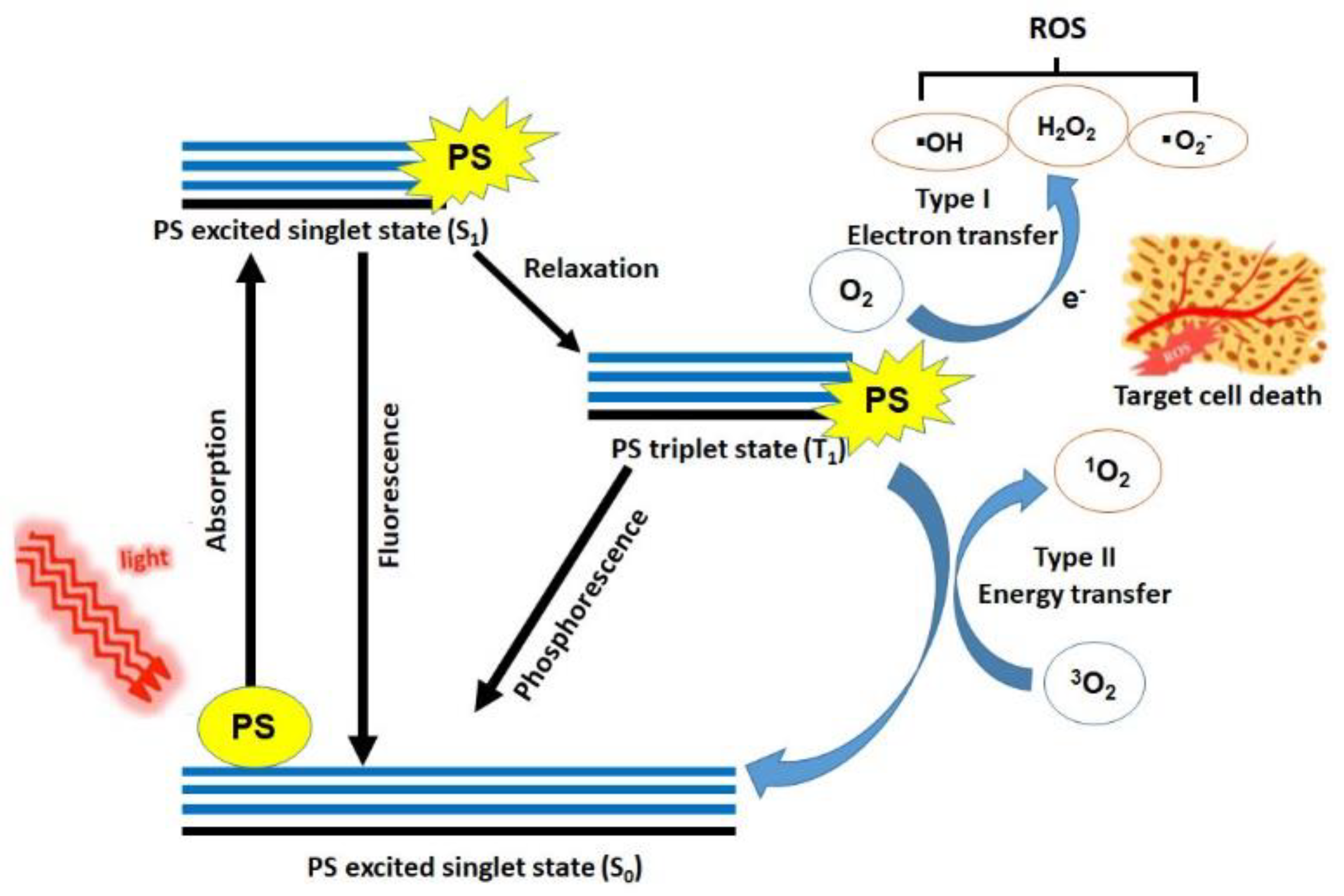
2.1. Mechanism of Photodynamic Therapy (PDT)
2.1.1. Light Sources for Photodynamic Therapy
2.1.2. The Role of Oxygen in Photodynamic Therapy
2.1.3. Photosensitizers Used in Photodynamic Therapy
2.2. Mechanism of Photothermal Therapy (PTT)
2.2.1. Phototherapeutic Mechanism in Photothermal Therapy
2.2.2. Photosensitizers Used in Photothermal Therapy
2.3. Nanocarriers for Phototherapy
3. Non-Oncologic Applications of Photodynamic Therapy
3.1. Dermatologic Disease
3.1.1. Acne
3.1.2. Warts
3.1.3. Photoaging
3.1.4. Psoriasis
3.1.5. Vascular Malformations
3.1.6. Cutaneous Leishmaniasis
3.1.7. Onychomycosis
3.1.8. Hirsutism
3.1.9. Keloid
3.1.10. Alopecia Areata
3.2. Ophthalmologic Disease
3.2.1. Central Serous Chorioretinopathy
3.2.2. Age-Related Macular Degeneration
3.2.3. Corneal Neovascularization
3.3. Cardiovascular Disease
3.3.1. Atherosclerosis
3.3.2. Esophageal Varix
3.4. Dental Disease
3.4.1. Periodontitis
3.4.2. Oral Lichen Planus
3.5. Neurologic Disease
3.5.1. Alzheimer’s Disease
3.5.2. Prion Disease
3.6. Skeletal Disease
3.6.1. Rheumatoid Arthritis
3.6.2. Synovitis
3.7. Gastrointestinal Disease
3.7.1. Crohn’s Disease
3.7.2. Bacteria-Mediated Gastritis or Colitis
3.8. Respiratory Disease
3.8.1. Ventilator-Associated Pneumonia
3.8.2. COVID-19
4. Non-Oncologic Applications of Photothermal Therapy
4.1. Atherosclerosis
4.2. Dry Eye Syndrome
5. Future Perspective of Nanomaterials for Non-Oncologic Disease
5.1. Multifunctional Nanomaterials for Phototherapy
5.2. Photoactivatable Nanomaterials for Phototherapy
5.3. Target-Specific Nanomaterials for Phototherapy
5.4. Deep Tissue Penetrating Nanomaterials for Phototherapy
6. Remaining Issues
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Roelandts, R. The history of phototherapy: Something new under the sun? J. Am. Acad. Dermatol. 2002, 46, 926–930. [Google Scholar] [CrossRef] [PubMed]
- Saleeby, C.W. Sunlight and Health, 3rd ed.; Nisbet & Co.: London, UK, 1926. [Google Scholar]
- Rathod, D.G.; Muneer, H.; Masood, S. Phototherapy. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2020. [Google Scholar]
- Nimbalkar, M.; Yawalkar, M.; Mahajan, N.; Dhoble, S.J. Potential of Luminescent Materials In Phototherapy. Photodiagn. Photodyn. Ther. 2020, 102082. [Google Scholar] [CrossRef] [PubMed]
- Chitgupi, U.; Qin, Y.; Lovell, J.F. Targeted Nanomaterials for Phototherapy. Nanotheranostics 2017, 1, 38–58. [Google Scholar] [CrossRef] [PubMed]
- Chung, E.; Vitkin, A. Photon mayhem: New directions in diagnostic and therapeutic photomedicine. Biomed. Eng. Lett. 2019, 9, 275–277. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Lovell, J.F.; Yoon, J.; Chen, X. Clinical development and potential of photothermal and photodynamic therapies for cancer. Nat. Rev. Clin. Oncol. 2020, 17, 657–674. [Google Scholar] [CrossRef] [PubMed]
- Dolmans, D.E.; Fukumura, D.; Jain, R.K. Photodynamic therapy for cancer. Nat. Rev. Cancer 2003, 3, 380–387. [Google Scholar] [CrossRef]
- Riley, R.S.; Day, E.S. Gold nanoparticle-mediated photothermal therapy: Applications and opportunities for multimodal cancer treatment. Wiley Interdiscip. Rev. Nanomed. Nanobiotechnol. 2017, 9. [Google Scholar] [CrossRef]
- Lipson, R.L.; Baldes, E.J. The photodynamic properties of particular hematoporphyrin derivatives. Arch. Dermatol. 1960, 82, 508–516. [Google Scholar] [CrossRef]
- Lipson, R.; Baldes, E.; Olsen, A. The use of haematoporphyrin derivative in tumour detection. J. Natl. Cancer Inst. 1961, 26, 1–8. [Google Scholar]
- Li, X.; Lee, S.; Yoon, J. Supramolecular photosensitizers rejuvenate photodynamic therapy. Chem. Soc. Rev. 2018, 47, 1174–1188. [Google Scholar] [CrossRef]
- Chan, W.; Lam, D.; Lai, T.; Tam, B.; Liu, D.; Chan, C. Choroidal vascular remodelling in central serous chorioretinopathy after indocyanine green guided photodynamic therapy with verteporfin: A novel treatment at the primary disease level. Br. J. Ophthalmol. 2003, 87, 1453–1458. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Bhattarai, P.; Dai, Z.; Chen, X. Photothermal therapy and photoacoustic imaging via nanotheranostics in fighting cancer. Chem. Soc. Rev. 2019, 48, 2053–2108. [Google Scholar] [CrossRef] [PubMed]
- Cheng, L.; Zhang, F.; Wang, S.; Pan, X.; Han, S.; Liu, S.; Ma, J.; Wang, H.; Shen, H.; Liu, H. Activation of prodrugs by NIR-triggered release of exogenous enzymes for locoregional chemo-photothermal therapy. Angew. Chem. Int. Ed. 2019, 58, 7728–7732. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Z.; Yan, Y.; Wang, L.; Zhang, Q.; Cheng, Y. Melanin-like nanoparticles decorated with an autophagy-inducing peptide for efficient targeted photothermal therapy. Biomaterials 2019, 203, 63–72. [Google Scholar] [CrossRef] [PubMed]
- Jeong, Y.; Jo, Y.K.; Kim, B.J.; Yang, B.; Joo, K.I.; Cha, H.J. Sprayable Adhesive Nanotherapeutics: Mussel-Protein-Based Nanoparticles for Highly Efficient Locoregional Cancer Therapy. ACS Nano 2018, 12, 8909–8919. [Google Scholar] [CrossRef] [PubMed]
- Guo, L.; Liu, W.; Niu, G.; Zhang, P.; Zheng, X.; Jia, Q.; Zhang, H.; Ge, J.; Wang, P. Polymer nanoparticles with high photothermal conversion efficiency as robust photoacoustic and thermal theranostics. J. Mater. Chem B 2017, 5, 2832–2839. [Google Scholar] [CrossRef]
- Calixto, G.M.; Bernegossi, J.; de Freitas, L.M.; Fontana, C.R.; Chorilli, M. Nanotechnology-Based Drug Delivery Systems for Photodynamic Therapy of Cancer: A Review. Molecules 2016, 21, 342. [Google Scholar] [CrossRef]
- Moghissi, K.; Dixon, K.; Gibbins, S. A Surgical View of Photodynamic Therapy in Oncology: A Review. Surg. J. N. Y. 2015, 1, e1–e15. [Google Scholar] [CrossRef]
- Allison, R.R.; Bagnato, V.S.; Cuenca, R.; Downie, G.H.; Sibata, C.H. The future of photodynamic therapy in oncology. Future Oncol. 2006, 2, 53–71. [Google Scholar] [CrossRef]
- Meimandi, M.; Talebi Ardakani, M.R.; Esmaeil Nejad, A.; Yousefnejad, P.; Saebi, K.; Tayeed, M.H. The Effect of Photodynamic Therapy in the Treatment of Chronic Periodontitis: A Review of Literature. J. Lasers Med. Sci. 2017, 8, S7–S11. [Google Scholar] [CrossRef]
- Zhu, T.C.; Finlay, J.C. The role of photodynamic therapy (PDT) physics. Med. Phys. 2008, 35, 3127–3136. [Google Scholar] [CrossRef] [PubMed]
- Karamanolis, G.; Mallas, E. Role of Photodynamic Therapy in Gastroenterology. Ann. Gastroenterol. 2005, 18, 141–147. [Google Scholar]
- Stacey, O.J.; Pope, S.J. New avenues in the design and potential application of metal complexes for photodynamic therapy. Rsc Adv. 2013, 3, 25550–25564. [Google Scholar] [CrossRef]
- Choi, Y.H.; Han, H.-K. Nanomedicines: Current status and future perspectives in aspect of drug delivery and pharmacokinetics. J. Pharm. Investig. 2018, 48, 43–60. [Google Scholar] [CrossRef]
- Borgia, F.; Giuffrida, R.; Caradonna, E.; Vaccaro, M.; Guarneri, F.; Cannavò, S.P. Early and late onset side effects of photodynamic therapy. Biomedicines 2018, 6, 12. [Google Scholar] [CrossRef]
- Moore, J.V.; West, C.M.; Whitehurst, C. The biology of photodynamic therapy. Phys. Med. Biol. 1997, 42, 913. [Google Scholar] [CrossRef]
- Mallidi, S.; Anbil, S.; Bulin, A.L.; Obaid, G.; Ichikawa, M.; Hasan, T. Beyond the Barriers of Light Penetration: Strategies, Perspectives and Possibilities for Photodynamic Therapy. Theranostics 2016, 6, 2458–2487. [Google Scholar] [CrossRef]
- Tegos, G.; Dai, T.; Fuchs, B.B.; Coleman, J.J.; Prates, R.A.; Astrakas, C.; St Denis, T.G.; Ribeiro, M.S.; Mylonakis, E.; Hamblin, M.R. Concepts and principles of photodynamic therapy as an alternative antifungal discovery platform. Front. Microbiol. 2012, 3, 120. [Google Scholar]
- Baskaran, R.; Lee, J.; Yang, S.-G. Clinical development of photodynamic agents and therapeutic applications. Biomater. Res. 2018, 22, 1–8. [Google Scholar] [CrossRef]
- Brancaleon, L.; Moseley, H. Laser and non-laser light sources for photodynamic therapy. Lasers Med. Sci. 2002, 17, 173–186. [Google Scholar] [CrossRef]
- Wilson, B.C.; Patterson, M.S.; Lilge, L. Implicit and explicit dosimetry in photodynamic therapy: A New paradigm. Lasers Med. Sci. 1997, 12, 182–199. [Google Scholar] [CrossRef] [PubMed]
- Georgakoudi, I.; Nichols, M.G.; Foster, T.H. The mechanism of Photofrin photobleaching and its consequences for photodynamic dosimetry. Photochem. Photobiol. 1997, 65, 135–144. [Google Scholar] [CrossRef] [PubMed]
- Star, W.M. Light delivery and light dosimetry for photodynamic therapy. Laser Med. Sci. 1990, 5, 107–113. [Google Scholar] [CrossRef][Green Version]
- Moan, J.; Berg, K. The photodegradation of porphyrins in cells can be used to estimate the lifetime of singlet oxygen. Photochem. Photobiol. 1991, 53, 549–553. [Google Scholar] [CrossRef]
- Dougherty, T.J.; Gomer, C.J.; Henderson, B.W.; Jori, G.; Kessel, D.; Korbelik, M.; Moan, J.; Peng, Q. Photodynamic therapy. J. Natl. Cancer Inst. 1998, 90, 889–905. [Google Scholar] [CrossRef]
- Abbas, M.; Zou, Q.; Li, S.; Yan, X. Self-Assembled Peptide- and Protein-Based Nanomaterials for Antitumor Photodynamic and Photothermal Therapy. Adv. Mater. 2017, 29. [Google Scholar] [CrossRef]
- Kim, K.S.; Kim, J.; Kim, D.H.; Hwang, H.S.; Na, K. Multifunctional trastuzumab-chlorin e6 conjugate for the treatment of HER2-positive human breast cancer. Biomater. Sci. 2018, 6, 1217–1226. [Google Scholar] [CrossRef]
- Kim, J.; Jo, Y.U.; Na, K. Photodynamic therapy with smart nanomedicine. Arch. Pharm. Res. 2020, 43, 22–31. [Google Scholar] [CrossRef]
- Beik, J.; Abed, Z.; Ghoreishi, F.S.; Hosseini-Nami, S.; Mehrzadi, S.; Shakeri-Zadeh, A.; Kamrava, S.K. Nanotechnology in hyperthermia cancer therapy: From fundamental principles to advanced applications. J. Control. Release 2016, 235, 205–221. [Google Scholar] [CrossRef]
- Ray, P.C.; Khan, S.A.; Singh, A.K.; Senapati, D.; Fan, Z. Nanomaterials for targeted detection and photothermal killing of bacteria. Chem. Soc. Rev. 2012, 41, 3193–3209. [Google Scholar] [CrossRef]
- Huang, X.; Jain, P.K.; El-Sayed, I.H.; El-Sayed, M.A. Plasmonic photothermal therapy (PPTT) using gold nanoparticles. Lasers Med. Sci. 2008, 23, 217–228. [Google Scholar] [CrossRef] [PubMed]
- Gai, S.; Yang, G.; Yang, P.; He, F.; Lin, J.; Jin, D.; Xing, B. Recent advances in functional nanomaterials for light–triggered cancer therapy. Nano Today 2018, 19, 146–187. [Google Scholar] [CrossRef]
- Eskiizmir, G.; Baskın, Y.; Yapıcı, K. Graphene-based nanomaterials in cancer treatment and diagnosis. In Fullerens, Graphenes and Nanotubes; William Andrew Publishing, Elsvier: Amsterdam, The Netherlands, 2018. [Google Scholar]
- Chen, J.-L.; Zhang, H.; Huang, X.-Q.; Wan, H.-Y.; Li, J.; Fan, X.-X.; Luo, K.Q.; Wang, J. Antiangiogenesis-combined photothermal therapy in the second near-infrared window at laser powers below the skin tolerance threshold. Nano Micro Lett. 2019, 11, 93. [Google Scholar] [CrossRef]
- Vines, J.B.; Yoon, J.H.; Ryu, N.E.; Lim, D.J.; Park, H. Gold Nanoparticles for Photothermal Cancer Therapy. Front. Chem. 2019, 7, 167. [Google Scholar] [CrossRef] [PubMed]
- Decuzzi, P.; Mitragotri, S. Introduction to special issue on “Nanoparticles in Medicine: Targeting, Optimization and Clinical Applications”. Bioeng. Transl. Med. 2016, 1, 8–9. [Google Scholar] [CrossRef]
- Chen, W.R.; Adams, R.L.; Bartels, K.E.; Nordquist, R.E. Chromophore-enhanced in vivo tumor cell destruction using an 808-nm diode laser. Cancer Lett. 1995, 94, 125–131. [Google Scholar] [CrossRef]
- Jori, G.; Spikes, J.D. Photothermal sensitizers: Possible use in tumor therapy. J. Photochem. Photobiol. B 1990, 6, 93–101. [Google Scholar] [CrossRef]
- Huang, X.; El-Sayed, I.H.; Qian, W.; El-Sayed, M.A. Cancer cell imaging and photothermal therapy in the near-infrared region by using gold nanorods. J. Am. Chem. Soc. 2006, 128, 2115–2120. [Google Scholar] [CrossRef]
- Dickerson, E.B.; Dreaden, E.C.; Huang, X.; El-Sayed, I.H.; Chu, H.; Pushpanketh, S.; McDonald, J.F.; El-Sayed, M.A. Gold nanorod assisted near-infrared plasmonic photothermal therapy (PPTT) of squamous cell carcinoma in mice. Cancer Lett. 2008, 269, 57–66. [Google Scholar] [CrossRef]
- Hainfeld, J.F.; Slatkin, D.N.; Smilowitz, H.M. The use of gold nanoparticles to enhance radiotherapy in mice. Phys. Med. Biol. 2004, 49, N309–N315. [Google Scholar] [CrossRef]
- Pinto, A.; Pocard, M. Photodynamic therapy and photothermal therapy for the treatment of peritoneal metastasis: A systematic review. Pleura Peritoneum 2018, 3, 20180124. [Google Scholar] [CrossRef] [PubMed]
- Gibot, L.; Demazeau, M.; Pimienta, V.; Mingotaud, A.F.; Vicendo, P.; Collin, F.; Martins-Froment, N.; Dejean, S.; Nottelet, B.; Roux, C.; et al. Role of Polymer Micelles in the Delivery of Photodynamic Therapy Agent to Liposomes and Cells. Cancers 2020, 12, 384. [Google Scholar] [CrossRef] [PubMed]
- Van Nostrum, C.F. Polymeric micelles to deliver photosensitizers for photodynamic therapy. Adv. Drug Deliv. Rev. 2004, 56, 9–16. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Scrivano, L.; Peterson, J.D.; Fens, M.; Hernandez, I.B.; Mesquita, B.; Torano, J.S.; Hennink, W.E.; van Nostrum, C.F.; Oliveira, S. EGFR-Targeted Nanobody Functionalized Polymeric Micelles Loaded with mTHPC for Selective Photodynamic Therapy. Mol. Pharm. 2020, 17, 1276–1292. [Google Scholar] [CrossRef] [PubMed]
- Park, J.H.; Lee, S.; Kim, J.-H.; Park, K.; Kim, K.; Kwon, I.C. Polymeric nanomedicine for cancer therapy. Prog. Polym. Sci. 2008, 33, 113–137. [Google Scholar] [CrossRef]
- Yeroslavsky, G.; Umezawa, M.; Okubo, K.; Nigoghossian, K.; Thi Kim Dung, D.; Miyata, K.; Kamimura, M.; Soga, K. Stabilization of indocyanine green dye in polymeric micelles for NIR-II fluorescence imaging and cancer treatment. Biomater. Sci. 2020, 8, 2245–2254. [Google Scholar] [CrossRef] [PubMed]
- Setaro, F.; Wennink, J.W.H.; Makinen, P.I.; Holappa, L.; Trohopoulos, P.N.; Yla-Herttuala, S.; van Nostrum, C.F.; de la Escosura, A.; Torres, T. Amphiphilic phthalocyanines in polymeric micelles: A supramolecular approach toward efficient third-generation photosensitizers. J. Mater. Chem. B 2020, 8, 282–289. [Google Scholar] [CrossRef]
- Yang, L.; Zhang, C.; Liu, J.; Huang, F.; Zhang, Y.; Liang, X.J.; Liu, J. ICG-Conjugated and (125) I-Labeled Polymeric Micelles with High Biosafety for Multimodality Imaging-Guided Photothermal Therapy of Tumors. Adv. Healthc. Mater. 2020, 9, e1901616. [Google Scholar] [CrossRef]
- Akbarzadeh, A.; Rezaei-Sadabady, R.; Davaran, S.; Joo, S.W.; Zarghami, N.; Hanifehpour, Y.; Samiei, M.; Kouhi, M.; Nejati-Koshki, K. Liposome: Classification, preparation, and applications. Nanoscale Res. Lett. 2013, 8, 102. [Google Scholar] [CrossRef]
- Johnston, M.J.; Semple, S.C.; Klimuk, S.K.; Ansell, S.; Maurer, N.; Cullis, P.R. Characterization of the drug retention and pharmacokinetic properties of liposomal nanoparticles containing dihydrosphingomyelin. Biochim. Biophys. Acta 2007, 1768, 1121–1127. [Google Scholar] [CrossRef]
- Ambreen, G.; Duse, L.; Tariq, I.; Ali, U.; Ali, S.; Pinnapireddy, S.R.; Bette, M.; Bakowsky, U.; Mandic, R. Sensitivity of Papilloma Virus-Associated Cell Lines to Photodynamic Therapy with Curcumin-Loaded Liposomes. Cancers 2020, 12, 3278. [Google Scholar] [CrossRef] [PubMed]
- De Oliveira, D.C.S.; de Freitas, C.F.; Calori, I.R.; Goncalves, R.S.; Cardinali, C.; Malacarne, L.C.; Ravanelli, M.I.; de Oliveira, H.P.M.; Tedesco, A.C.; Caetano, W.; et al. Theranostic verteporfin- loaded lipid-polymer liposome for photodynamic applications. J. Photochem. Photobiol. B 2020, 212, 112039. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Tian, J.; Fu, Y.; Yang, Y.; Chen, M.; Zhang, Q. Near-infrared light-triggered nanobomb for in situ on-demand maximization of photothermal/photodynamic efficacy for cancer therapy. Biomater. Sci. 2020. [Google Scholar] [CrossRef]
- Zheng, K.; Liu, H.; Liu, X.; Jiang, L.; Li, L.; Wu, X.; Guo, N.; Ding, C.; Huang, M. Photo-triggered release of doxorubicin from liposomes formulated by amphiphilic phthalocyanines for combination therapy to enhance antitumor efficacy. J. Mater. Chem. B 2020, 8, 8022–8036. [Google Scholar] [CrossRef] [PubMed]
- Deng, S.; Gigliobianco, M.R.; Censi, R.; Di Martino, P. Polymeric Nanocapsules as Nanotechnological Alternative for Drug Delivery System: Current Status, Challenges and Opportunities. Nanomaterials 2020, 10, 847. [Google Scholar] [CrossRef]
- Raffin Pohlmann, A.; Weiss, V.; Mertins, O.; Pesce da Silveira, N.; Staniscuaski Guterres, S. Spray-dried indomethacin-loaded polyester nanocapsules and nanospheres: Development, stability evaluation and nanostructure models. Eur. J. Pharm. Sci. 2002, 16, 305–312. [Google Scholar] [CrossRef]
- Barras, A.; Skandrani, N.; Gonzalez Pisfil, M.; Paryzhak, S.; Dumych, T.; Haustrate, A.; Heliot, L.; Gharbi, T.; Boulahdour, H.; Lehen’kyi, V.; et al. Improved photodynamic effect through encapsulation of two photosensitizers in lipid nanocapsules. J. Mater. Chem. B 2018, 6, 5949–5963. [Google Scholar] [CrossRef]
- Zhao, J.; Yang, H.; Li, J.; Wang, Y.; Wang, X. Fabrication of pH-responsive PLGA(UCNPs/DOX) nanocapsules with upconversion luminescence for drug delivery. Sci. Rep. 2017, 7, 18014. [Google Scholar] [CrossRef]
- Amantino, C.F.; de Baptista-Neto, A.; Badino, A.C.; Siqueira-Moura, M.P.; Tedesco, A.C.; Primo, F.L. Anthraquinone encapsulation into polymeric nanocapsules as a new drug from biotechnological origin designed for photodynamic therapy. Photodiagnosis Photodyn. Ther. 2020, 31, 101815. [Google Scholar] [CrossRef]
- Bazylinska, U.; Wawrzynczyk, D.; Szewczyk, A.; Kulbacka, J. Engineering and biological assessment of double core nanoplatform for co-delivery of hybrid fluorophores to human melanoma. J. Inorg. Biochem. 2020, 208, 111088. [Google Scholar] [CrossRef]
- Bazylinska, U.; Kulbacka, J.; Chodaczek, G. Nanoemulsion Structural Design in Co-Encapsulation of Hybrid Multifunctional Agents: Influence of the Smart PLGA Polymers on the Nanosystem-Enhanced Delivery and Electro-Photodynamic Treatment. Pharmaceutics 2019, 11, 405. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Li, R.; Yang, B. Carbon Dots: A New Type of Carbon-Based Nanomaterial with Wide Applications. ACS Cent. Sci. 2020, 6, 2179–2195. [Google Scholar] [CrossRef] [PubMed]
- Battigelli, A.; Menard-Moyon, C.; Bianco, A. Carbon nanomaterials as new tools for immunotherapeutic applications. J. Mater. Chem. B 2014, 2, 6144–6156. [Google Scholar] [CrossRef] [PubMed]
- Lu, D.; Tao, R.; Wang, Z. Carbon-based materials for photodynamic therapy: A mini-review. Front. Chem. Sci. Eng. 2019, 13, 310–323. [Google Scholar] [CrossRef]
- Sun, D.; Zhang, Z.; Chen, M.; Zhang, Y.; Amagat, J.; Kang, S.; Zheng, Y.; Hu, B.; Chen, M. Co-Immobilization of Ce6 Sono/Photosensitizer and Protonated Graphitic Carbon Nitride on PCL/Gelation Fibrous Scaffolds for Combined Sono-Photodynamic Cancer Therapy. ACS Appl. Mater. Interfaces 2020, 12, 40728–40739. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Vinothini, K.; Ramesh, T.; Rajan, M.; Ramu, A. Combined photodynamic-chemotherapy investigation of cancer cells using carbon quantum dot-based drug carrier system. Drug Deliv. 2020, 27, 791–804. [Google Scholar] [CrossRef] [PubMed]
- Sahu, A.; Min, K.; Jeon, J.; Yang, H.S.; Tae, G. Catalytic nanographene oxide with hemin for enhanced photodynamic therapy. J. Control. Release 2020, 326, 442–454. [Google Scholar] [CrossRef] [PubMed]
- Monteiro, A.R.; Neves, M.G.P.M.S.; Trindade, T. Functionalization of Graphene Oxide with Porphyrins: Synthetic Routes and Biological Applications. Chempluschem 2020, 85, 1857–1880. [Google Scholar] [CrossRef]
- Thakur, N.S.; Bhaumik, J.; Kirar, S.; Banerjee, U.C. Development of Gold-Based Phototheranostic Nanoagents through a Bioinspired Route and Their Applications in Photodynamic Therapy. ACS Sustain. Chem. Eng. 2017, 5, 7950–7960. [Google Scholar] [CrossRef]
- Kong, F.Y.; Zhang, J.W.; Li, R.F.; Wang, Z.X.; Wang, W.J.; Wang, W. Unique Roles of Gold Nanoparticles in Drug Delivery, Targeting and Imaging Applications. Molecules 2017, 22, 1445. [Google Scholar] [CrossRef]
- Tabero, A.; Planas, O.; Gallavardin, T.; Nieves, I.; Nonell, S.; Villanueva, A. Smart Dual-Functionalized Gold Nanoclusters for Spatio-Temporally Controlled Delivery of Combined Chemo- and Photodynamic Therapy. Nanomaterials 2020, 10, 2474. [Google Scholar] [CrossRef] [PubMed]
- Chuang, C.C.; Chen, Y.N.; Wang, Y.Y.; Huang, Y.C.; Lin, S.Y.; Huang, R.Y.; Jang, Y.Y.; Yang, C.C.; Huang, Y.F.; Chang, C.W. Stem Cell-Based Delivery of Gold/Chlorin e6 Nanocomplexes for Combined Photothermal and Photodynamic Therapy. ACS Appl. Mater. Interfaces 2020, 12, 30021–30030. [Google Scholar] [CrossRef] [PubMed]
- Demir Duman, F.; Sebek, M.; Thanh, N.T.K.; Loizidou, M.; Shakib, K.; MacRobert, A.J. Enhanced photodynamic therapy and fluorescence imaging using gold nanorods for porphyrin delivery in a novel in vitro squamous cell carcinoma 3D model. J. Mater. Chem. B 2020, 8, 5131–5142. [Google Scholar] [CrossRef] [PubMed]
- Seabra, A.B. Iron Oxide Magnetic Nanoparticles in Photodynamic Therapy: A Promising Approach Against Tumor Cells; Springer: Berlin/Heidelberg, Germany, 2017. [Google Scholar]
- Kuo, S.H.; Wu, P.T.; Huang, J.Y.; Chiu, C.P.; Yu, J.; Liao, M.Y. Fabrication of Anisotropic Cu Ferrite-Polymer Core-Shell Nanoparticles for Photodynamic Ablation of Cervical Cancer Cells. Nanomaterials 2020, 10, 2429. [Google Scholar] [CrossRef] [PubMed]
- Wang, G.; Zhang, X.; Skallberg, A.; Liu, Y.; Hu, Z.; Mei, X.; Uvdal, K. One-step synthesis of water-dispersible ultra-small Fe3O4 nanoparticles as contrast agents for T1 and T2 magnetic resonance imaging. Nanoscale 2014, 6, 2953–2963. [Google Scholar] [CrossRef]
- Xu, Y.; Li, W.; Chen, S.; Huang, B.; Pei, W.; Niu, C. Near-Infrared Responsive Phase-Shifted Nanoparticles for Magnetically Targeted MR/US Imaging and Photothermal Therapy of Cancer. Front. Bioeng. Biotechnol. 2020, 8, 599107. [Google Scholar] [CrossRef]
- Wang, M.; Abbineni, G.; Clevenger, A.; Mao, C.; Xu, S. Upconversion nanoparticles: Synthesis, surface modification and biological applications. Nanomedicine 2011, 7, 710–729. [Google Scholar] [CrossRef]
- Auzel, F. Upconversion and anti-Stokes processes with f and d ions in solids. Chem. Rev. 2004, 104, 139–173. [Google Scholar] [CrossRef]
- Dong, H.; Du, S.R.; Zheng, X.Y.; Lyu, G.M.; Sun, L.D.; Li, L.D.; Zhang, P.Z.; Zhang, C.; Yan, C.H. Lanthanide Nanoparticles: From Design toward Bioimaging and Therapy. Chem. Rev. 2015, 115, 10725–10815. [Google Scholar] [CrossRef]
- Zhao, L.; Choi, J.; Lu, Y.; Kim, S.Y. NIR Photoregulated Theranostic System Based on Hexagonal-Phase Upconverting Nanoparticles for Tumor-Targeted Photodynamic Therapy and Fluorescence Imaging. Nanomaterials 2020, 10, 2332. [Google Scholar] [CrossRef]
- Lee, S.Y.; Lee, R.; Kim, E.; Lee, S.; Park, Y.I. Near-Infrared Light-Triggered Photodynamic Therapy and Apoptosis Using Upconversion Nanoparticles With Dual Photosensitizers. Front. Bioeng. Biotechnol. 2020, 8, 275. [Google Scholar] [CrossRef] [PubMed]
- Sakamoto, F.H.; Lopes, J.D.; Anderson, R.R. Photodynamic therapy for acne vulgaris: A critical review from basics to clinical practice: Part I. Acne vulgaris: When and why consider photodynamic therapy? J. Am. Acad. Dermatol. 2010, 63, 183–193. [Google Scholar] [CrossRef] [PubMed]
- Guy, R.; Green, M.R.; Kealey, T. Modeling acne in vitro. J. Investig. Dermatol. 1996, 106, 176–182. [Google Scholar] [CrossRef] [PubMed]
- Downing, D.T.; Stewart, M.E.; Wertz, P.W.; Strauss, J.S. Essential fatty acids and acne. J. Am. Acad. Dermatol. 1986, 14, 221–225. [Google Scholar] [CrossRef]
- Kligman, A.M.; Wheatley, V.R.; Mills, O.H. Comedogenicity of human sebum. Arch. Dermatol. 1970, 102, 267–275. [Google Scholar] [CrossRef]
- Calzavara-Pinton, P.G.; Rossi, M.T.; Aronson, E.; Sala, R.; Italian Group for Photodynamic Therapy. A retrospective analysis of real-life practice of off-label photodynamic therapy using methyl aminolevulinate (MAL-PDT) in 20 Italian dermatology departments. Part 1: Inflammatory and aesthetic indications. Photochem. Photobiol. Sci. 2013, 12, 148–157. [Google Scholar] [CrossRef]
- Yang, G.L.; Zhao, M.; Wang, J.M.; He, C.F.; Luo, Y.; Liu, H.Y.; Gao, J.; Long, C.Q.; Bai, J.R. Short-term clinical effects of photodynamic therapy with topical 5-aminolevulinic acid for facial acne conglobata: An open, prospective, parallel-arm trial. Photodermatol. Photoimmunol. Photomed. 2013, 29, 233–238. [Google Scholar] [CrossRef]
- Morton, C.A.; Szeimies, R.M.; Basset-Seguin, N.; Calzavara-Pinton, P.G.; Gilaberte, Y.; Haedersdal, M.; Hofbauer, G.F.L.; Hunger, R.E.; Karrer, S.; Piaserico, S.; et al. European Dermatology Forum guidelines on topical photodynamic therapy 2019 Part 2: Emerging indications—field cancerization, photorejuvenation and inflammatory/infective dermatoses. J. Eur. Acad. Dermatol. Venereol. 2020, 34, 17–29. [Google Scholar] [CrossRef]
- Bourke, J.F.; Berth-Jones, J.; Hutchinson, P.E. Cryotherapy of common viral warts at intervals of 1, 2 and 3 weeks. Br. J. Dermatol. 1995, 132, 433–436. [Google Scholar] [CrossRef]
- Stender, I.M.; Na, R.; Fogh, H.; Gluud, C.; Wulf, H.C. Photodynamic therapy with 5-aminolaevulinic acid or placebo for recalcitrant foot and hand warts: Randomised double-blind trial. Lancet 2000, 355, 963–966. [Google Scholar] [CrossRef]
- Liang, J.; Lu, X.N.; Tang, H.; Zhang, Z.; Fan, J.; Xu, J.H. Evaluation of photodynamic therapy using topical aminolevulinic acid hydrochloride in the treatment of condylomata acuminata: A comparative, randomized clinical trial. PhotoDermatol. Photoimmunol. Photomed. 2009, 25, 293–297. [Google Scholar] [CrossRef] [PubMed]
- Kohl, E.; Torezan, L.A.; Landthaler, M.; Szeimies, R.M. Aesthetic effects of topical photodynamic therapy. J. Eur. Acad. Dermatol. Venereol. 2010, 24, 1261–1269. [Google Scholar] [CrossRef] [PubMed]
- Goldberg, D.J. Photodynamic therapy in skin rejuvenation. Clin. Dermatol. 2008, 26, 608–613. [Google Scholar] [CrossRef] [PubMed]
- Shin, H.T.; Kim, J.H.; Shim, J.; Lee, J.H.; Lee, D.Y.; Lee, J.H.; Yang, J.M. Photodynamic therapy using a new formulation of 5-aminolevulinic acid for wrinkles in Asian skin: A randomized controlled split face study. J. Dermatol. Treat. 2015, 26, 246–251. [Google Scholar] [CrossRef]
- Smits, T.; Kleinpenning, M.M.; van Erp, P.E.; van de Kerkhof, P.C.; Gerritsen, M.J. A placebo-controlled randomized study on the clinical effectiveness, immunohistochemical changes and protoporphyrin IX accumulation in fractionated 5-aminolaevulinic acid-photodynamic therapy in patients with psoriasis. Br. J. Dermatol. 2006, 155, 429–436. [Google Scholar] [CrossRef]
- Choi, Y.M.; Adelzadeh, L.; Wu, J.J. Photodynamic therapy for psoriasis. J. Dermatol. Treat. 2015, 26, 202–207. [Google Scholar] [CrossRef]
- Almutawa, F.; Thalib, L.; Hekman, D.; Sun, Q.; Hamzavi, I.; Lim, H.W. Efficacy of localized phototherapy and photodynamic therapy for psoriasis: A systematic review and meta-analysis. Photodermatol. Photoimmunol. Photomed. 2015, 31, 5–14. [Google Scholar] [CrossRef]
- Elmets, C.A.; Lim, H.W.; Stoff, B.; Connor, C.; Cordoro, K.M.; Lebwohl, M.; Armstrong, A.W.; Davis, D.M.R.; Elewski, B.E.; Gelfand, J.M.; et al. Joint American Academy of Dermatology-National Psoriasis Foundation guidelines of care for the management and treatment of psoriasis with phototherapy. J. Am. Acad. Dermatol. 2019, 81, 775–804. [Google Scholar] [CrossRef]
- Orenstein, A.; Nelson, J.S.; Liaw, L.H.; Kaplan, R.; Kimel, S.; Berns, M.W. Photochemotherapy of hypervascular dermal lesions: A possible alternative to photothermal therapy? Lasers Surg. Med. 1990, 10, 334–343. [Google Scholar] [CrossRef]
- Zhao, Y.; Tu, P.; Zhou, G.; Zhou, Z.; Lin, X.; Yang, H.; Lu, Z.; Gao, T.; Tu, Y.; Xie, H.; et al. Hemoporfin Photodynamic Therapy for Port-Wine Stain: A Randomized Controlled Trial. PLoS ONE 2016, 11, e0156219. [Google Scholar] [CrossRef]
- Jerjes, W.; Upile, T.; Hamdoon, Z.; Mosse, C.A.; Akram, S.; Morley, S.; Hopper, C. Interstitial PDT for vascular anomalies. Lasers Surg. Med. 2011, 43, 357–365. [Google Scholar] [CrossRef] [PubMed]
- Maxfield, L.; Crane, J.S. Leishmaniasis. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2020. [Google Scholar]
- Enk, C.D.; Fritsch, C.; Jonas, F.; Nasereddin, A.; Ingber, A.; Jaffe, C.L.; Ruzicka, T. Treatment of cutaneous leishmaniasis with photodynamic therapy. Arch. Dermatol. 2003, 139, 432–434. [Google Scholar] [CrossRef] [PubMed]
- Gardlo, K.; Horska, Z.; Enk, C.D.; Rauch, L.; Megahed, M.; Ruzicka, T.; Fritsch, C. Treatment of cutaneous leishmaniasis by photodynamic therapy. J. Am. Acad. Dermatol. 2003, 48, 893–896. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Asilian, A.; Davami, M. Comparison between the efficacy of photodynamic therapy and topical paromomycin in the treatment of Old World cutaneous leishmaniasis: A placebo-controlled, randomized clinical trial. Clin. Exp. Dermatol. 2006, 31, 634–637. [Google Scholar] [CrossRef] [PubMed]
- Grover, C.; Khurana, A. An update on treatment of onychomycosis. Mycoses 2012, 55, 541–551. [Google Scholar] [CrossRef]
- Westerberg, D.P.; Voyack, M.J. Onychomycosis: Current trends in diagnosis and treatment. Am. Fam. Physician 2013, 88, 762–770. [Google Scholar]
- Sotiriou, E.; Koussidou-Eremonti, T.; Chaidemenos, G.; Apalla, Z.; Ioannides, D. Photodynamic therapy for distal and lateral subungual toenail onychomycosis caused by Trichophyton rubrum: Preliminary results of a single-centre open trial. Acta Derm. Venereol. 2010, 90, 216–217. [Google Scholar] [CrossRef]
- Gilaberte, Y.; Robres, M.P.; Frias, M.P.; Garcia-Doval, I.; Rezusta, A.; Aspiroz, C. Methyl aminolevulinate photodynamic therapy for onychomycosis: A multicentre, randomized, controlled clinical trial. J. Eur. Acad. Dermatol. Venereol. 2017, 31, 347–354. [Google Scholar] [CrossRef] [PubMed]
- Liu, K.; Motan, T.; Claman, P. No. 350-Hirsutism: Evaluation and Treatment. J. Obstet. Gynaecol. Can. 2017, 39, 1054–1068. [Google Scholar] [CrossRef] [PubMed]
- Calzavara-Pinton, P.G.; Venturini, M.; Sala, R. Photodynamic therapy: Update 2006. Part 2: Clinical results. J. Eur. Acad. Dermatol. Venereol. 2007, 21, 439–451. [Google Scholar] [CrossRef] [PubMed]
- Comacchi, C.; Bencini, P.L.; Galimberti, M.G.; Cappugi, P.; Torchia, D. Topical photodynamic therapy for idiopathic hirsutism and hypertrichosis. Plast. Reconstr. Surg. 2012, 129, 1012e–1014e. [Google Scholar] [CrossRef] [PubMed]
- Murray, J.C. Keloids and hypertrophic scars. Clin. Dermatol. 1994, 12, 27–37. [Google Scholar] [CrossRef]
- Tosa, M.; Ogawa, R. Photodynamic therapy for keloids and hypertrophic scars: A review. Scars Burn. Health 2020, 6, 2059513120932059. [Google Scholar] [CrossRef] [PubMed]
- Brown, J.J.; Bayat, A. Genetic susceptibility to raised dermal scarring. Br. J. Dermatol. 2009, 161, 8–18. [Google Scholar] [CrossRef]
- Mustoe, T.A.; Cooter, R.D.; Gold, M.H.; Hobbs, F.D.; Ramelet, A.A.; Shakespeare, P.G.; Stella, M.; Teot, L.; Wood, F.M.; Ziegler, U.E.; et al. International clinical recommendations on scar management. Plast. Reconstr. Surg. 2002, 110, 560–571. [Google Scholar] [CrossRef]
- Campbell, S.M.; Tyrrell, J.; Marshall, R.; Curnow, A. Effect of MAL-photodynamic therapy on hypertrophic scarring. Photodiagnosis Photodyn. Ther. 2010, 7, 183–188. [Google Scholar] [CrossRef]
- Bruscino, N.; Lotti, T.; Rossi, R. Photodynamic therapy for a hypertrophic scarring: A promising choice. PhotoDermatol. Photoimmunol. Photomed. 2011, 27, 334–335. [Google Scholar] [CrossRef]
- Hordinsky, M.; Donati, A. Alopecia areata: An evidence-based treatment update. Am. J. Clin. Dermatol. 2014, 15, 231–246. [Google Scholar] [CrossRef]
- Linares-Gonzalez, L.; Rodenas-Herranz, T.; Saenz-Guirado, S.; Ruiz-Villaverde, R. Successful response to photodynamic therapy with 5-aminolevulinic acid nanoemulsified gel in a patient with universal alopecia areata refractory to conventional treatment. Dermatol. Ther. 2020, 33, e13416. [Google Scholar] [CrossRef]
- Bissonnette, R.; Shapiro, J.; Zeng, H.; McLean, D.I.; Lui, H. Topical photodynamic therapy with 5-aminolaevulinic acid does not induce hair regrowth in patients with extensive alopecia areata. Br. J. Dermatol. 2000, 143, 1032–1035. [Google Scholar] [CrossRef]
- Giorgio, C.M.; Babino, G.; Caccavale, S.; Russo, T.; De Rosa, A.B.; Alfano, R.; Fulgione, E.; Argenziano, G. Combination of photodynamic therapy with 5-aminolaevulinic acid and microneedling in the treatment of alopecia areata resistant to conventional therapies: Our experience with 41 patients. Clin. Exp. Dermatol. 2020, 45, 323–326. [Google Scholar] [CrossRef] [PubMed]
- Daruich, A.; Matet, A.; Dirani, A.; Bousquet, E.; Zhao, M.; Farman, N.; Jaisser, F.; Behar-Cohen, F. Central serous chorioretinopathy: Recent findings and new physiopathology hypothesis. Prog. Retin. Eye Res. 2015, 48, 82–118. [Google Scholar] [CrossRef] [PubMed]
- Siaudvytyte, L.; Diliene, V.; Miniauskiene, G.; Balciuniene, V.J. Photodynamic therapy and central serous chorioretinopathy. Med. Hypothesis Discov. Innov. Ophthalmol. 2012, 1, 67–71. [Google Scholar] [PubMed]
- Van Dijk, E.H.C.; Fauser, S.; Breukink, M.B.; Blanco-Garavito, R.; Groenewoud, J.M.M.; Keunen, J.E.E.; Peters, P.J.H.; Dijkman, G.; Souied, E.H.; MacLaren, R.E.; et al. Half-Dose Photodynamic Therapy versus High-Density Subthreshold Micropulse Laser Treatment in Patients with Chronic Central Serous Chorioretinopathy: The PLACE Trial. Ophthalmology 2018, 125, 1547–1555. [Google Scholar] [CrossRef]
- Tan, W.; Zou, J.; Yoshida, S.; Jiang, B.; Zhou, Y. The Role of Inflammation in Age-Related Macular Degeneration. Int. J. Biol. Sci. 2020, 16, 2989–3001. [Google Scholar] [CrossRef]
- Gao, Y.; Yu, T.; Zhang, Y.; Dang, G. Anti-VEGF Monotherapy Versus Photodynamic Therapy and Anti-VEGF Combination Treatment for Neovascular Age-Related Macular Degeneration: A Meta-Analysis. Invest. Ophthalmol. Vis. Sci. 2018, 59, 4307–4317. [Google Scholar] [CrossRef]
- Miyamoto, N.; Mandai, M.; Oishi, A.; Nakai, S.; Honda, S.; Hirashima, T.; Oh, H.; Matsumoto, Y.; Uenishi, M.; Kurimoto, Y. Long-term results of photodynamic therapy or ranibizumab for polypoidal choroidal vasculopathy in LAPTOP study. Br. J. Ophthalmol. 2019, 103, 844–848. [Google Scholar] [CrossRef]
- Koh, A.; Lai, T.Y.Y.; Takahashi, K.; Wong, T.Y.; Chen, L.J.; Ruamviboonsuk, P.; Tan, C.S.; Feller, C.; Margaron, P.; Lim, T.H.; et al. Efficacy and Safety of Ranibizumab With or Without Verteporfin Photodynamic Therapy for Polypoidal Choroidal Vasculopathy: A Randomized Clinical Trial. JAMA Ophthalmol. 2017, 135, 1206–1213. [Google Scholar] [CrossRef]
- Barry, Z.; Park, B.; Corson, T.W. Pharmacological Potential of Small Molecules for Treating Corneal Neovascularization. Molecules 2020, 25, 3468. [Google Scholar] [CrossRef]
- Chang, J.H.; Gabison, E.E.; Kato, T.; Azar, D.T. Corneal neovascularization. Curr. Opin. Ophthalmol. 2001, 12, 242–249. [Google Scholar] [CrossRef]
- Diaz-Davalos, C.D.; Carrasco-Quiroz, A.; Rivera-Diez, D. Neovascularization corneal regression in patients treated with photodynamic therapy with verteporfin. Rev. Med. Inst. Mex. Seguro Soc. 2016, 54, 164–169. [Google Scholar] [PubMed]
- Hamdan, J.; Boulze, M.; Aziz, A.; Alessi, G.; Hoffart, L. Corneal neovascularisation treatments compared: Subconjunctival bevacizumab injections and/or photodynamic therapy. J. Fr. Ophtalmol. 2015, 38, 924–933. [Google Scholar] [CrossRef] [PubMed]
- Dougherty, T.J.; Cooper, M.T.; Mang, T.S. Cutaneous phototoxic occurrences in patients receiving Photofrin. Lasers Surg. Med. 1990, 10, 485–488. [Google Scholar] [CrossRef]
- Tawakol, A.; Castano, A.P.; Anatelli, F.; Bashian, G.; Stern, J.; Zahra, T.; Gad, F.; Chirico, S.; Ahmadi, A.; Fischman, A.J.; et al. Photosensitizer delivery to vulnerable atherosclerotic plaque: Comparison of macrophage-targeted conjugate versus free chlorin(e6). J. Biomed. Opt. 2006, 11, 021008. [Google Scholar] [CrossRef] [PubMed]
- Jenkins, M.P.; Buonaccorsi, G.A.; Raphael, M.; Nyamekye, I.; McEwan, J.R.; Bown, S.G.; Bishop, C.C. Clinical study of adjuvant photodynamic therapy to reduce restenosis following femoral angioplasty. Br. J. Surg. 1999, 86, 1258–1263. [Google Scholar] [CrossRef]
- Rockson, S.G.; Kramer, P.; Razavi, M.; Szuba, A.; Filardo, S.; Fitzgerald, P.; Cooke, J.P.; Yousuf, S.; DeVault, A.R.; Renschler, M.F.; et al. Photoangioplasty for human peripheral atherosclerosis: Results of a phase I trial of photodynamic therapy with motexafin lutetium (Antrin). Circulation 2000, 102, 2322–2324. [Google Scholar] [CrossRef]
- Houthoofd, S.; Vuylsteke, M.; Mordon, S.; Fourneau, I. Photodynamic therapy for atherosclerosis. The potential of indocyanine green. Photodiagnosis Photodyn. Ther. 2020, 29, 101568. [Google Scholar] [CrossRef]
- Patel, B.; Han, E.; Swan, K. Richard Schatzki: A familiar ring. AJR Am. J. Roentgenol. 2013, 201, W678–W682. [Google Scholar] [CrossRef]
- Qiu, H.; Mao, Y.; Gu, Y.; Wang, Y.; Zhu, J.; Zeng, J. Vascular targeted photodynamic therapy for bleeding gastrointestinal mucosal vascular lesions: A preliminary study. Photodiagn. Photodyn. Ther. 2012, 9, 109–117. [Google Scholar] [CrossRef]
- Li, C.Z.; Cheng, L.F.; Wang, Z.Q.; Gu, Y. Attempt of photodynamic therapy on esophageal varices. Lasers Med. Sci. 2009, 24, 167–171. [Google Scholar] [CrossRef]
- Botelho, J.; Machado, V.; Hussain, S.B.; Zehra, S.A.; Proenca, L.; Orlandi, M.; Mendes, J.J.; D’Aiuto, F. Periodontitis and circulating blood cell profiles: A systematic review and meta-analysis. Exp. Hematol. 2020. [Google Scholar] [CrossRef] [PubMed]
- Diogo, P.; Faustino, M.A.F.; Neves, M.G.P.M.S.; Palma, P.J.; Baptista, I.P.; Gonçalves, T.; Santos, J.M. An Insight into Advanced Approaches for Photosensitizer Optimization in Endodontics—A Critical Review. J. Funct. Biomater. 2019, 10, 44. [Google Scholar] [CrossRef] [PubMed]
- De Oliveira, R.R.; Schwartz-Filho, H.O.; Novaes, A.B., Jr.; Taba, M., Jr. Antimicrobial photodynamic therapy in the non-surgical treatment of aggressive periodontitis: A preliminary randomized controlled clinical study. J. Periodontol. 2007, 78, 965–973. [Google Scholar] [CrossRef] [PubMed]
- Chambrone, L.; Wang, H.L.; Romanos, G.E. Antimicrobial photodynamic therapy for the treatment of periodontitis and peri-implantitis: An American Academy of Periodontology best evidence review. J. Periodontol. 2018, 89, 783–803. [Google Scholar] [CrossRef] [PubMed]
- Joshi, K.; Baiju, C.S.; Khashu, H.; Bansal, S. Clinical effectiveness of indocyanine green mediated antimicrobial photodynamic therapy as an adjunct to scaling root planing in treatment of chronic periodontitis—A randomized controlled clinical trial. Photodiagn. Photodyn. Ther. 2020, 29, 101591. [Google Scholar] [CrossRef]
- Lavanya, N.; Jayanthi, P.; Rao, U.K.; Ranganathan, K. Oral lichen planus: An update on pathogenesis and treatment. J. Oral Maxillofac. Pathol. 2011, 15, 127–132. [Google Scholar] [CrossRef]
- Aghahosseini, F.; Arbabi-Kalati, F.; Fashtami, L.A.; Fateh, M.; Djavid, G.E. Treatment of oral lichen planus with photodynamic therapy mediated methylene blue: A case report. Med. Oral Patol. Oral Cir. Bucal 2006, 11, E126–E129. [Google Scholar]
- Cosgarea, R.; Pollmann, R.; Sharif, J.; Schmidt, T.; Stein, R.; Bodea, A.; Auschill, T.; Sculean, A.; Eming, R.; Greene, B.; et al. Photodynamic therapy in oral lichen planus: A prospective case-controlled pilot study. Sci. Rep. 2020, 10, 1667. [Google Scholar] [CrossRef]
- Murphy, R.M. Peptide aggregation in neurodegenerative disease. Annu. Rev. Biomed. Eng. 2002, 4, 155–174. [Google Scholar] [CrossRef]
- Benilova, I.; Karran, E.; De Strooper, B. The toxic Abeta oligomer and Alzheimer’s disease: An emperor in need of clothes. Nat. NeuroSci. 2012, 15, 349–357. [Google Scholar] [CrossRef]
- Lee, J.S.; Lee, B.I.; Park, C.B. Photo-induced inhibition of Alzheimer’s beta-amyloid aggregation in vitro by rose bengal. Biomaterials 2015, 38, 43–49. [Google Scholar] [CrossRef] [PubMed]
- Lee, B.I.; Suh, Y.S.; Chung, Y.J.; Yu, K.; Park, C.B. Shedding Light on Alzheimer’s beta-Amyloidosis: Photosensitized Methylene Blue Inhibits Self-Assembly of beta-Amyloid Peptides and Disintegrates Their Aggregates. Sci. Rep. 2017, 7, 7523. [Google Scholar] [CrossRef] [PubMed]
- Lee, B.I.; Lee, S.; Suh, Y.S.; Lee, J.S.; Kim, A.K.; Kwon, O.Y.; Yu, K.; Park, C.B. Photoexcited Porphyrins as a Strong Suppressor of beta-Amyloid Aggregation and Synaptic Toxicity. Angew. Chem. Int. Ed. Engl. 2015, 54, 11472–11476. [Google Scholar] [CrossRef] [PubMed]
- White, M.D.; Mallucci, G.R. Therapy for prion diseases: Insights from the use of RNA interference. Prion 2009, 3, 121–128. [Google Scholar] [CrossRef] [PubMed]
- Cobb, N.J.; Surewicz, W.K. Prion diseases and their biochemical mechanisms. Biochemistry 2009, 48, 2574–2585. [Google Scholar] [CrossRef]
- Kostelanska, M.; Freisleben, J.; Backovska Hanusova, Z.; Mosko, T.; Vik, R.; Moravcova, D.; Hamacek, A.; Mosinger, J.; Holada, K. Optimization of the photodynamic inactivation of prions by a phthalocyanine photosensitizer: The crucial involvement of singlet oxygen. J. Biophotonics 2019, 12, e201800340. [Google Scholar] [CrossRef]
- Deane, K.D.; Holers, V.M. The Natural History of Rheumatoid Arthritis. Clin. Ther. 2019, 41, 1256–1269. [Google Scholar] [CrossRef]
- Gallardo-Villagran, M.; Leger, D.Y.; Liagre, B.; Therrien, B. Photosensitizers Used in the Photodynamic Therapy of Rheumatoid Arthritis. Int. J. Mol. Sci. 2019, 20, 3339. [Google Scholar] [CrossRef]
- Hendrich, C.; Siebert, W.E. Photodynamic therapy for rheumatoid arthritis? Lasers Surg. Med. 1997, 21, 359–364. [Google Scholar] [CrossRef]
- Kirdaite, G.; Lange, N.; Busso, N.; Van Den Bergh, H.; Kucera, P.; So, A. Protoporphyrin IX photodynamic therapy for synovitis. Arthritis Rheum. 2002, 46, 1371–1378. [Google Scholar] [CrossRef]
- Dietze, A.; Berg, K. ALA-induced porphyrin formation and fluorescence in synovitis tissue In-vitro and in vivo studies. Photodiagn. Photodyn. Ther. 2005, 2, 299–307. [Google Scholar] [CrossRef]
- Baumgart, D.C.; Sandborn, W.J. Crohn’s disease. Lancet 2012, 380, 1590–1605. [Google Scholar] [CrossRef]
- Favre, L.; Borle, F.; Velin, D.; Bachmann, D.; Bouzourene, H.; Wagnieres, G.; van den Bergh, H.; Ballabeni, P.; Gabrecht, T.; Michetti, P.; et al. Low dose endoluminal photodynamic therapy improves murine T cell-mediated colitis. Endoscopy 2011, 43, 604–616. [Google Scholar] [CrossRef] [PubMed]
- Baccani, I.; Faraoni, P.; Marini, M.; Gnerucci, A.; Orsini, B.; Pecile, P.; Romano, G.; Fusi, F.; Rossolini, G.M.; Antonelli, A. Synergistic effect of photodynamic therapy at 400 nm and doxycycline against Helicobacter pylori. Future Microbiol. 2019, 14, 1199–1205. [Google Scholar] [CrossRef]
- Cassidy, C.M.; Tunney, M.M.; Caldwell, D.L.; Andrews, G.P.; Donnelly, R.F. Development of novel oral formulations prepared via hot melt extrusion for targeted delivery of photosensitizer to the colon. Photochem. Photobiol. 2011, 87, 867–876. [Google Scholar] [CrossRef]
- Koerner, R.J. Contribution of endotracheal tubes to the pathogenesis of ventilator-associated pneumonia. J. Hosp. Infect. 1997, 35, 83–89. [Google Scholar] [CrossRef]
- Biel, M.A.; Sievert, C.; Usacheva, M.; Teichert, M.; Wedell, E.; Loebel, N.; Rose, A.; Zimmermann, R. Reduction of Endotracheal Tube Biofilms Using Antimicrobial Photodynamic Therapy. Lasers Surg. Med. 2011, 43, 586–590. [Google Scholar] [CrossRef]
- Zangirolami, A.C.; Dias, L.D.; Blanco, K.C.; Vinagreiro, C.S.; Inada, N.M.; Arnaut, L.G.; Pereira, M.M.; Bagnato, V.S. Avoiding ventilator-associated pneumonia: Curcumin-functionalized endotracheal tube and photodynamic action. Proc. Natl. Acad. Sci. USA 2020, 117, 22967–22973. [Google Scholar] [CrossRef]
- Almeida, A.; Faustino, M.A.F.; Neves, M.G.P.M.S. Antimicrobial Photodynamic Therapy in the Control of COVID-19. Antibiotics 2020, 9, 320. [Google Scholar] [CrossRef]
- Moghissi, K.; Dixon, K.; Gibbins, S. Does PDT have potential in the treatment of COVID 19 patients? Photodiagn. Photodyn. Ther. 2020, 31, 101889. [Google Scholar] [CrossRef]
- Dias, L.D.; Blanco, K.C.; Bagnato, V.S. COVID-19: Beyond the virus. The use of photodynamic therapy for the treatment of infections in the respiratory tract. Photodiagn. Photodyn. Ther. 2020, 31, 101804. [Google Scholar] [CrossRef] [PubMed]
- Gendrot, M.; Andreani, J.; Duflot, I.; Boxberger, M.; Le Bideau, M.; Mosnier, J.; Jardot, P.; Fonta, I.; Rolland, C.; Bogreau, H.; et al. Methylene blue inhibits replication of SARS-CoV-2 in vitro. Int. J. Antimicrob. Agents 2020, 56, 106202. [Google Scholar] [CrossRef] [PubMed]
- Onuma, Y.; Muramatsu, T.; Kharlamov, A.; Serruys, P.W. Freeing the vessel from metallic cage: What can we achieve with bioresorbable vascular scaffolds? Cardiovasc. Interv. Ther. 2012, 27, 141–154. [Google Scholar] [CrossRef]
- Kharlamov, A.N.; Tyurnina, A.E.; Veselova, V.S.; Kovtun, O.P.; Shur, V.Y.; Gabinsky, J.L. Silica-gold nanoparticles for atheroprotective management of plaques: Results of the NANOM-FIM trial. Nanoscale 2015, 7, 8003–8015. [Google Scholar] [CrossRef]
- Pang, Y.; Wei, C.; Li, R.; Wu, Y.; Liu, W.; Wang, F.; Zhang, X.; Wang, X. Photothermal conversion hydrogel based mini-eye patch for relieving dry eye with long-term use of the light-emitting screen. Int. J. Nanomed. 2019, 14, 5125–5133. [Google Scholar] [CrossRef]
- Chen, C.; Song, Z.; Zheng, X.; He, Z.; Liu, B.; Huang, X.; Kong, D.; Ding, D.; Tang, B.Z. AIEgen-based theranostic system: Targeted imaging of cancer cells and adjuvant amplification of antitumor efficacy of paclitaxel. Chem. Sci. 2017, 8, 2191–2198. [Google Scholar] [CrossRef]
- Liu, Y.; Liu, Y.; Bu, W.; Cheng, C.; Zuo, C.; Xiao, Q.; Sun, Y.; Ni, D.; Zhang, C.; Liu, J.; et al. Hypoxia Induced by Upconversion-Based Photodynamic Therapy: Towards Highly Effective Synergistic Bioreductive Therapy in Tumors. Angew. Chem. Int. Ed. Engl. 2015, 54, 8105–8109. [Google Scholar] [CrossRef]
- Chitgupi, U.; Lovell, J.F. Naphthalocyanines as contrast agents for photoacoustic and multimodal imaging. Biomed. Eng. Lett. 2018, 8, 215–221. [Google Scholar] [CrossRef]
- Cheng, Q.; Li, Z.-H.; Sun, Y.-X.; Zhang, X.-Z. Controlled synthesis of a core-shell nanohybrid for effective multimodal image-guided combined photothermal/photodynamic therapy of tumors. NPG Asia Mater. 2019, 11, 63. [Google Scholar] [CrossRef]
- Wang, Q.; Dai, Y.; Xu, J.; Cai, J.; Niu, X.; Zhang, L.; Chen, R.; Shen, Q.; Huang, W.; Fan, Q. All-in-one phototheranostics: Single laser triggers NIR-II fluorescence/photoacoustic imaging guided photothermal/photodynamic/chemo combination therapy. Adv. Funct. Mater. 2019, 29, 1901480. [Google Scholar] [CrossRef]
- Hu, K.; Xie, L.; Zhang, Y.; Hanyu, M.; Yang, Z.; Nagatsu, K.; Suzuki, H.; Ouyang, J.; Ji, X.; Wei, J.; et al. Marriage of black phosphorus and Cu(2+) as effective photothermal agents for PET-guided combination cancer therapy. Nat. Commun. 2020, 11, 2778. [Google Scholar] [CrossRef]
- Rautio, J.; Kumpulainen, H.; Heimbach, T.; Oliyai, R.; Oh, D.; Jarvinen, T.; Savolainen, J. Prodrugs: Design and clinical applications. Nat. Rev. Drug Discov. 2008, 7, 255–270. [Google Scholar] [CrossRef]
- Zhao, L.; Peng, J.; Huang, Q.; Li, C.; Chen, M.; Sun, Y.; Lin, Q.; Zhu, L.; Li, F. Near-Infrared Photoregulated Drug Release in Living Tumor Tissue via Yolk-Shell Upconversion Nanocages. Adv. Funct. Mater. 2013, 24, 363–371. [Google Scholar] [CrossRef]
- Zhang, Y.; Xu, C.; Yang, X.; Pu, K. Photoactivatable Protherapeutic Nanomedicine for Cancer. Adv. Mater. 2020, 32, e2002661. [Google Scholar] [CrossRef]
- Xiong, Q.; Lim, Y.; Li, D.; Pu, K.; Liang, L.; Duan, H. Photoactive Nanocarriers for Controlled Delivery. Adv. Funct. Mater. 2020, 30, 1903896. [Google Scholar] [CrossRef]
- Jiang, Y.; Pu, K. Multimodal Biophotonics of Semiconducting Polymer Nanoparticles. Acc. Chem. Res. 2018, 51, 1840–1849. [Google Scholar] [CrossRef]
- Palombo, F.; Focaccetti, C.; Barnaba, V. Therapeutic implications of immunogenic cell death in human cancer. Front. Immunol. 2014, 4, 503. [Google Scholar] [CrossRef]
- Garg, A.D.; Agostinis, P. ER stress, autophagy and immunogenic cell death in photodynamic therapy-induced anti-cancer immune responses. Photochem. Photobiol. Sci. 2014, 13, 474–487. [Google Scholar] [CrossRef]
- Hou, X.; Tao, Y.; Pang, Y.; Li, X.; Jiang, G.; Liu, Y. Nanoparticle-based photothermal and photodynamic immunotherapy for tumor treatment. Int. J. Cancer 2018, 143, 3050–3060. [Google Scholar] [CrossRef]
- Cheng, Y.; Cheng, H.; Jiang, C.; Qiu, X.; Wang, K.; Huan, W.; Yuan, A.; Wu, J.; Hu, Y. Perfluorocarbon nanoparticles enhance reactive oxygen levels and tumour growth inhibition in photodynamic therapy. Nat. Commun. 2015, 6, 8785. [Google Scholar] [CrossRef]
- Dang, J.; He, H.; Chen, D.; Yin, L. Manipulating tumor hypoxia toward enhanced photodynamic therapy (PDT). Biomater. Sci. 2017, 5, 1500–1511. [Google Scholar] [CrossRef]
- Li, W.; Yang, J.; Luo, L.; Jiang, M.; Qin, B.; Yin, H.; Zhu, C.; Yuan, X.; Zhang, J.; Luo, Z.; et al. Targeting photodynamic and photothermal therapy to the endoplasmic reticulum enhances immunogenic cancer cell death. Nat. Commun. 2019, 10, 3349. [Google Scholar] [CrossRef]
- Jiang, X.-D.; Xi, D.; Sun, C.-L.; Guan, J.; He, M.; Xiao, L.-J. Synthesis of a pyrene-fused aza-BODIPY as a near-infrared dye having the absorption maximum at 746 nm. Tetrahedron Lett. 2015, 56, 4868–4870. [Google Scholar] [CrossRef]
- Chen, D.; Zhong, Z.; Ma, Q.; Shao, J.; Huang, W.; Dong, X. Aza-BODIPY-Based Nanomedicines in Cancer Phototheranostics. ACS Appl. Mater. Interfaces 2020, 12, 26914–26925. [Google Scholar] [CrossRef]
- Wilson, B.C.; Patterson, M.S. The physics, biophysics and technology of photodynamic therapy. Phys. Med. Biol. 2008, 53, R61–R109. [Google Scholar] [CrossRef]
- Benov, L. Photodynamic therapy: Current status and future directions. Med. Princ. Pract. 2015, 24 (Suppl. S1), 14–28. [Google Scholar] [CrossRef]
- Junttila, M.R.; de Sauvage, F.J. Influence of tumour micro-environment heterogeneity on therapeutic response. Nature 2013, 501, 346–354. [Google Scholar] [CrossRef]
- Lee, S.H.; Park, O.K.; Kim, J.; Shin, K.; Pack, C.G.; Kim, K.; Ko, G.; Lee, N.; Kwon, S.H.; Hyeon, T. Deep Tumor Penetration of Drug-Loaded Nanoparticles by Click Reaction-Assisted Immune Cell Targeting Strategy. J. Am. Chem. Soc. 2019, 141, 13829–13840. [Google Scholar] [CrossRef]
- Ding, X.; Liow, C.H.; Zhang, M.; Huang, R.; Li, C.; Shen, H.; Liu, M.; Zou, Y.; Gao, N.; Zhang, Z.; et al. Surface plasmon resonance enhanced light absorption and photothermal therapy in the second near-infrared window. J. Am. Chem. Soc. 2014, 136, 15684–15693. [Google Scholar] [CrossRef]
- Bashkatov, A.; Genina, E.; Kochubey, V.; Tuchin, V. Optical properties of human skin, subcutaneous and mucous tissues in the wavelength range from 400 to 2000 nm. J. Phys. D Appl. Phys. 2005, 38, 2543. [Google Scholar] [CrossRef]
- Sinha, M.; Gollavelli, G.; Ling, Y.-C. Exploring the photothermal hot spots of graphene in the first and second biological window to inactivate cancer cells and pathogens. RSC Adv. 2016, 6, 63859–63866. [Google Scholar] [CrossRef]
- Cao, Y.; Dou, J.-H.; Zhao, N.-J.; Zhang, S.; Zheng, Y.-Q.; Zhang, J.-P.; Wang, J.-Y.; Pei, J.; Wang, Y. Highly efficient NIR-II photothermal conversion based on an organic conjugated polymer. Chem. Mater. 2017, 29, 718–725. [Google Scholar] [CrossRef]
- Maestro, L.M.; Haro-Gonzalez, P.; del Rosal, B.; Ramiro, J.; Caamano, A.J.; Carrasco, E.; Juarranz, A.; Sanz-Rodriguez, F.; Sole, J.G.; Jaque, D. Heating efficiency of multi-walled carbon nanotubes in the first and second biological windows. Nanoscale 2013, 5, 7882–7889. [Google Scholar] [CrossRef] [PubMed]
- Wan, X.; Liu, M.; Ma, M.; Chen, D.; Wu, N.; Li, L.; Li, Z.; Lin, G.; Wang, X.; Xu, G. The Ultrasmall Biocompatible CuS@BSA Nanoparticle and Its Photothermal Effects. Front. Pharmacol. 2019, 10, 141. [Google Scholar] [CrossRef]
- Cai, X.; Xie, Z.; Ding, B.; Shao, S.; Liang, S.; Pang, M.; Lin, J. Monodispersed Copper(I)-Based Nano Metal-Organic Framework as a Biodegradable Drug Carrier with Enhanced Photodynamic Therapy Efficacy. Adv. Sci. 2019, 6, 1900848. [Google Scholar] [CrossRef]
- Zhu, L.; Gao, D.; Xie, L.; Dai, Y.; Zhao, Q. NIR II-Excited and pH-Responsive Ultrasmall Nanoplatform for Deep Optical Tissue and Drug Delivery Penetration and Effective Cancer Chemophototherapy. Mol. Pharm. 2020, 17, 3720–3729. [Google Scholar] [CrossRef] [PubMed]



| Types of Nanocarriers | Therapeutic Modalities | PDT Agents | PTT Agents | Imaging Modalities | Year | Ref. |
|---|---|---|---|---|---|---|
| Polymeric micelles | PDT | mTHPC | FL | 2020 | [57] | |
| Polymeric micelles | PDT + PTT | IGG | IGG | FL | 2020 | [59] |
| Polymeric micelles | PDT | Silicon phthalocyanine | 2020 | [60] | ||
| Polymeric micelles | PDT + PTT | ICG | ICG | FL, SPECT, PA, thermal | 2020 | [61] |
| Liposomes | PDT | curcumin | 2020 | [64] | ||
| Liposomes | PDT | verteporfin | FL | 2020 | [65] | |
| Liposomes | PDT + PTT | Ce6 | Cypate | FL | 2020 | [66] |
| Liposomes | PTT + Chemo | ZnPc(PEG)4 | FL | 2020 | [67] | |
| Polymeric nanocapsules | PDT | PpIX, hypericin | FL | 2018 | [70] | |
| Polymeric nanocapsules | PDT | anthraquinone | 2020 | [72] | ||
| Polymeric nanocapsules | PDT | Rose Bengal | FL | 2020 | [73] | |
| Polymeric nanocapsules | PDT + Chemo | verteporfin | FL | 2019 | [74] | |
| Carbon nanosheet | PDT + SDT | Ce6 | FL | 2020 | [78] | |
| Carbon dot | PDT + Chemo | Ce6 | FL | 2020 | [79] | |
| Graphene oxide nanosheet | PDT | Ce6 | FL | 2020 | [80] | |
| Gold nanocluster | PDT + Chemo | PpIX | 2020 | [84] | ||
| Gold nanorod | PDT + PTT | Ce6 | FL | 2020 | [85] | |
| Gold nanorod | PDT | TMPy | FL | 2020 | [86] | |
| Magnetic NP | PDT | MB | FL | 2020 | [88] | |
| Magnetic NP | PTT | ICG | MR/US/FL | 2020 | [90] | |
| Upconversion NP | PDT | pheophorbide | FL | 2020 | [94] | |
| Upconversion NP | PDT | Ce6/Rose Bengal | FL | 2020 | [95] |
| Disease | Photo-Sensitizer | Light Source | Wave-Length (nm) | Power Density (mW/cm2) | Energy Density (J/cm2) | Treatment Protocol | Outcome of PDT Group | Enrolled Patients | Ref. |
|---|---|---|---|---|---|---|---|---|---|
| Acne | 5-ALA | LED | 633 | 100 | 50 | 20 min | significantly improved acne lesion and reduced scar formation | 75 | [101] |
| Warts | 5-ALA | Halogen lamp | 590–700 | 50 | 70 | 23 min 20 s | reduced area and number of warts than placebo group | 45 | [104] |
| Photoaging | 5-ALA | Xenon lamp | 400–720 | 3500 | 10.5 | 3 s 3 times | better wrinkle reduction than ND:YAG laser therapy group | 13 | [108] |
| Cutaneous leishmaniasis | 5-ALA | LED | 633 | 100 | Once a week for 4 weeks | better treatment outcome than control group | 57 | [119] | |
| Onychomycosis | MAL | LED | 635 | 37 | Once a week for 3 weeks | better clinical response than placebo group, but failed statistical significance | 40 | [123] | |
| Central serous chorioretinopathy | Verteporfin | Laser | 689 | 50 | 83 s | better clinical response than high-density subthreshold micropulse laser treatment group | 179 | [139] | |
| Age-related macular degeneration | Verteporfin | Laser | 689 | 600 | 50 | 83 s | additional therapeutic effect with anti-VEGF therapy | 322 | [143] |
| Corneal neo-vascularization | Verteporfin | Laser | 689 | 600 | 50 | 83 s | combination with anti-VEGF therapy showed best therapeutic response | 7 | [147] |
| Esophageal varix | HMME | Laser | 150 | 40 min | less newly visible vessel than control group | 14 | [155] | ||
| Periodontitis | ICG | laser | 810 | 200 | 30 s | additional therapeutic effect with scaling and root planing | 29 | [160] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yoo, S.W.; Oh, G.; Ahn, J.C.; Chung, E. Non-Oncologic Applications of Nanomedicine-Based Phototherapy. Biomedicines 2021, 9, 113. https://doi.org/10.3390/biomedicines9020113
Yoo SW, Oh G, Ahn JC, Chung E. Non-Oncologic Applications of Nanomedicine-Based Phototherapy. Biomedicines. 2021; 9(2):113. https://doi.org/10.3390/biomedicines9020113
Chicago/Turabian StyleYoo, Su Woong, Gyungseok Oh, Jin Chul Ahn, and Euiheon Chung. 2021. "Non-Oncologic Applications of Nanomedicine-Based Phototherapy" Biomedicines 9, no. 2: 113. https://doi.org/10.3390/biomedicines9020113
APA StyleYoo, S. W., Oh, G., Ahn, J. C., & Chung, E. (2021). Non-Oncologic Applications of Nanomedicine-Based Phototherapy. Biomedicines, 9(2), 113. https://doi.org/10.3390/biomedicines9020113






