Collagen-Based Matrices for Osteoconduction: A Preclinical In Vivo Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Biomaterials
2.2. Animals
2.3. Anesthetic Procedure
2.4. Surgical and Postoperative Procedures
2.5. Bone Labeling
2.6. Sacrifice
2.7. Micro-CT Analysis
2.8. Histological Processing and Histomorphometric Analysis
2.9. Statistical Analysis
3. Results
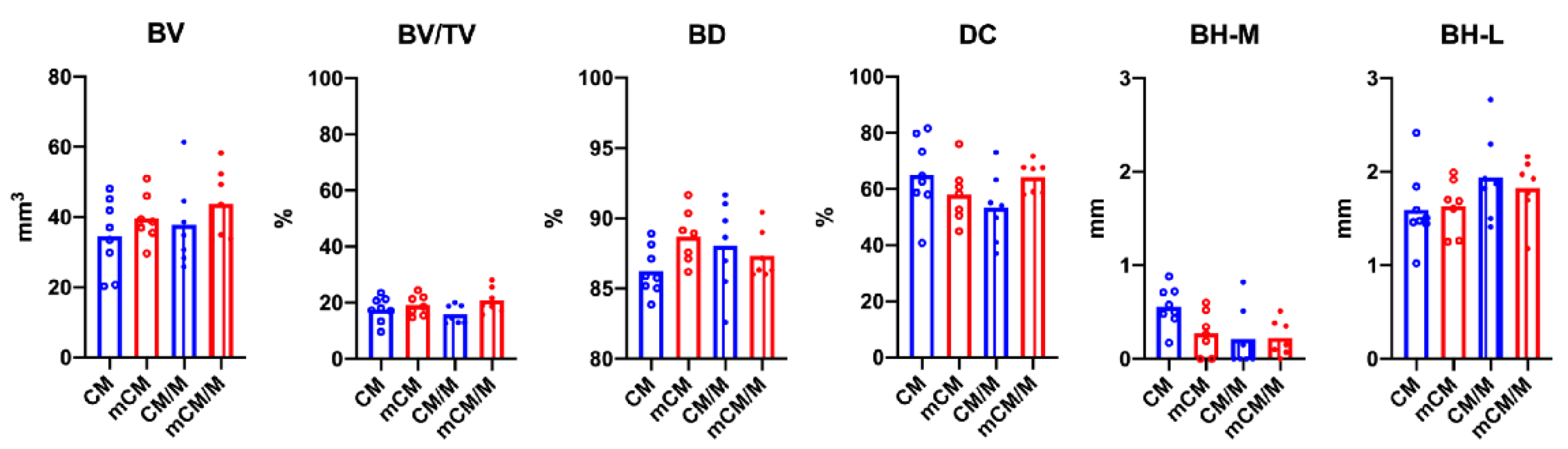
3.1. Micro-CT Analyses
3.2. Histological Analyses
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Gultekin, B.A.; Cansiz, E.; Borahan, M.O. Clinical and 3-Dimensional Radiographic Evaluation of Autogenous Iliac Block Bone Grafting and Guided Bone Regeneration in Patients with Atrophic Maxilla. J. Oral Maxillofac. Surg. 2017, 75, 709–722. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Milinkovic, I.; Cordaro, L. Are there specific indications for the different alveolar bone augmentation procedures for implant placement? A systematic review. Int. J. Oral Maxillofac. Surg. 2014, 43, 606–625. [Google Scholar] [CrossRef] [PubMed]
- Stopa, Z.; Siewert-Gutowska, M.; Abed, K.; Szubinska-Lelonkiewicz, D.; Kaminski, A.; Fiedor, P. Evaluation of the Safety and Clinical Efficacy of Allogeneic Bone Grafts in the Reconstruction of the Maxilla and Mandible. Transplant. Proc. 2018, 50, 2199–2201. [Google Scholar] [CrossRef] [PubMed]
- Artas, G.; Gul, M.; Acikan, I.; Kirtay, M.; Bozoglan, A.; Simsek, S.; Yaman, F.; Dundar, S. A comparison of different bone graft materials in peri-implant guided bone regeneration. Braz. Oral Res. 2018, 32, e59. [Google Scholar] [CrossRef]
- Kadouch, J.A. Calcium hydroxylapatite: A review on safety and complications. J. Cosmet. Dermatol. 2017, 16, 152–161. [Google Scholar] [CrossRef]
- Mate Sanchez de Val, J.E.; Calvo-Guirado, J.L.; Gomez-Moreno, G.; Perez-Albacete Martinez, C.; Mazon, P.; De Aza, P.N. Influence of hydroxyapatite granule size, porosity, and crystallinity on tissue reaction In Vivo. Part A: Synthesis, characterization of the materials, and SEM analysis. Clin. Oral Implants Res. 2016, 27, 1331–1338. [Google Scholar] [CrossRef]
- Ikumi, R.; Miyahara, T.; Akino, N.; Tachikawa, N.; Kasugai, S. Guided bone regeneration using a hydrophilic membrane made of unsintered hydroxyapatite and poly (L-lactic acid) in a rat bone-defect model. Dent. Mater. J. 2018, 37, 912–918. [Google Scholar] [CrossRef] [Green Version]
- Sbricoli, L.; Guazzo, R.; Annunziata, M.; Gobbato, L.; Bressan, E.; Nastri, L. Selection of Collagen Membranes for Bone Regeneration: A Literature Review. Materials 2020, 13, 786. [Google Scholar] [CrossRef] [Green Version]
- Ricard-Blum, S. The collagen family. Cold Spring Harb. Perspect. Biol. 2011, 3, a004978. [Google Scholar] [CrossRef] [Green Version]
- Bunyaratavej, P.; Wang, H.L. Collagen membranes: A review. J. Periodontol. 2001, 72, 215–229. [Google Scholar] [CrossRef] [Green Version]
- Caballé-Serrano, J.; Zhang, S.; Ferrantino, L.; Simion, M.; Chappuis, V.; Bosshardt, D.D. Tissue Response to a Porous Collagen Matrix Used for Soft Tissue Augmentation. Materials 2019, 12, 3721. [Google Scholar] [CrossRef] [Green Version]
- Mayfield, L.; Nobreus, N.; Attstrom, R.; Linde, A. Guided bone regeneration in dental implant treatment using a bioabsorbable membrane. Clin. Oral Implants Res. 1997, 8, 10–17. [Google Scholar] [CrossRef] [PubMed]
- Kuchler, U.; Rybaczek, T.; Dobask, T.; Heimel, P.; Tangl, S.; Klehm, J.; Menzel, M.; Gruber, R. Bone-conditioned medium modulates the osteoconductive properties of collagen membranes in a rat calvaria defect model. Clin. Oral Implants Res. 2018, 29, 381–388. [Google Scholar] [CrossRef] [PubMed]
- Salamanca, E.; Hsu, C.C.; Huang, H.M.; Teng, N.C.; Lin, C.T.; Pan, Y.H.; Chang, W.J. Bone regeneration using a porcine bone substitute collagen composite in vitro and In Vivo. Sci. Rep. 2018, 8, 984. [Google Scholar] [CrossRef] [Green Version]
- Zuhr, O.; Bäumer, D.; Hürzeler, M. The addition of soft tissue replacement grafts in plastic periodontal and implant surgery: Critical elements in design and execution. J. Clin. Periodontol. 2014, 41 (Suppl. 15), S123–S142. [Google Scholar] [CrossRef]
- Thoma, D.S.; Jung, R.E.; Schneider, D.; Cochran, D.L.; Ender, A.; Jones, A.A.; Görlach, C.; Uebersax, L.; Graf-Hausner, U.; Hämmerle, C.H. Soft tissue volume augmentation by the use of collagen-based matrices: A volumetric analysis. J. Clin. Periodontol. 2010, 37, 659–666. [Google Scholar] [CrossRef] [Green Version]
- Jung, R.E.; Hürzeler, M.B.; Thoma, D.S.; Khraisat, A.; Hämmerle, C.H. Local tolerance and efficiency of two prototype collagen matrices to increase the width of keratinized tissue. J. Clin. Periodontol. 2011, 38, 173–179. [Google Scholar] [CrossRef]
- Thoma, D.S.; Villar, C.C.; Cochran, D.L.; Hämmerle, C.H.; Jung, R.E. Tissue integration of collagen-based matrices: An experimental study in mice. Clin. Oral Implants Res. 2012, 23, 1333–1339. [Google Scholar] [CrossRef]
- Thoma, D.S.; Zeltner, M.; Hilbe, M.; Hämmerle, C.H.; Hüsler, J.; Jung, R.E. Randomized controlled clinical study evaluating effectiveness and safety of a volume-stable collagen matrix compared to autogenous connective tissue grafts for soft tissue augmentation at implant sites. J. Clin. Periodontol. 2016, 43, 874–885. [Google Scholar] [CrossRef]
- Ferrantino, L.; Bosshardt, D.; Nevins, M.; Santoro, G.; Simion, M.; Kim, D. Tissue Integration of a Volume-Stable Collagen Matrix in an Experimental Soft Tissue Augmentation Model. Int. J. Periodont. Restor. Dent. 2016, 36, 807–815. [Google Scholar] [CrossRef]
- Zeltner, M.; Jung, R.E.; Hämmerle, C.H.; Hüsler, J.; Thoma, D.S. Randomized controlled clinical study comparing a volume-stable collagen matrix to autogenous connective tissue grafts for soft tissue augmentation at implant sites: Linear volumetric soft tissue changes up to 3 months. J. Clin. Periodontol. 2017, 44, 446–453. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mathes, S.H.; Wohlwend, L.; Uebersax, L.; von Mentlen, R.; Thoma, D.S.; Jung, R.E.; Görlach, C.; Graf-Hausner, U. A bioreactor test system to mimic the biological and mechanical environment of oral soft tissues and to evaluate substitutes for connective tissue grafts. Biotechnol. Bioeng. 2010, 107, 1029–1039. [Google Scholar] [CrossRef] [PubMed]
- Thoma, D.S.; Naenni, N.; Benic, G.I.; Hämmerle, C.H.; Jung, R.E. Soft tissue volume augmentation at dental implant sites using a volume stable three-dimensional collagen matrix—Histological outcomes of a preclinical study. J. Clin. Periodontol. 2017, 44, 185–194. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thoma, D.S.; Hämmerle, C.H.; Cochran, D.L.; Jones, A.A.; Görlach, C.; Uebersax, L.; Mathes, S.; Graf-Hausner, U.; Jung, R.E. Soft tissue volume augmentation by the use of collagen-based matrices in the dog mandible—A histological analysis. J. Clin. Periodontol. 2011, 38, 1063–1070. [Google Scholar] [CrossRef] [PubMed]
- Caballé-Serrano, J.; Zhang, S.; Sculean, A.; Staehli, A.; Bosshardt, D.D. Tissue Integration and Degradation of a Porous Collagen-Based Scaffold Used for Soft Tissue Augmentation. Materials 2020, 13, 2420. [Google Scholar] [CrossRef]
- Spiller, K.L.; Anfang, R.R.; Spiller, K.J.; Ng, J.; Nakazawa, K.R.; Daulton, J.W.; Vunjak-Novakovic, G. The role of macrophage phenotype in vascularization of tissue engineering scaffolds. Biomaterials 2014, 35, 4477–4488. [Google Scholar] [CrossRef] [Green Version]
- Alibardi, L. Immunocalization of telomerase in cells of lizard tail after amputation suggests cell activation for tail regeneration. Tissue Cell 2016, 48, 63–71. [Google Scholar] [CrossRef]
- De Oliveira, E.S.M.; Pelegrine, A.A.; Alves Pinheiro da Silva, A.; Manhaes Junior, L.R.; de Mello, E.O.R.; Gaiba Franca, S.; Aloise, A.C.; Ferreira, L.M. Xenograft enriched with autologous bone marrow in inlay reconstructions: A tomographic and histomorphometric study in rabbit calvaria. Int. J. Biomater. 2012, 2012, 170520. [Google Scholar] [CrossRef]
- Tamimi, F.; Torres, J.; Kathan, C.; Baca, R.; Clemente, C.; Blanco, L.; Lopez Cabarcos, E. Bone regeneration in rabbit calvaria with novel monetite granules. J. Biomed. Mater. Res. A 2008, 87, 980–985. [Google Scholar] [CrossRef]
- Delgado-Ruiz, R.A.; Calvo-Guirado, J.L.; Romanos, G.E. Critical size defects for bone regeneration experiments in rabbit calvariae: Systematic review and quality evaluation using ARRIVE guidelines. Clin. Oral Implants Res. 2015, 26, 915–930. [Google Scholar] [CrossRef]
- Yip, I.; Ma, L.; Mattheos, N.; Dard, M.; Lang, N.P. Defect healing with various bone substitutes. Clin. Oral Implants Res. 2015, 26, 606–614. [Google Scholar] [CrossRef] [PubMed]
- Yang, C.; Unursaikhan, O.; Lee, J.S.; Jung, U.W.; Kim, C.S.; Choi, S.H. Osteoconductivity and biodegradation of synthetic bone substitutes with different tricalcium phosphate contents in rabbits. J. Biomed. Mater. Res. B Appl. Biomater. 2014, 102, 80–88. [Google Scholar] [CrossRef] [PubMed]
- Fujioka-Kobayashi, M.; Kobayashi, E.; Schaller, B.; Mottini, M.; Miron, R.J.; Saulacic, N. Effect of recombinant human bone morphogenic protein 9 (rhBMP9) loaded onto bone grafts versus barrier membranes on new bone formation in a rabbit calvarial defect model. J. Biomed. Mater. Res. A 2017, 105, 2655–2661. [Google Scholar] [CrossRef] [PubMed]
- Data on Geistlich. Geistlich Pharma AG, Wolhusen, Switzerland. Available online: https://www.geistlich-pharma.com/en/ (accessed on 1 February 2020).
- Williams, R.J.; Gamradt, S.C. Articular cartilage repair using a resorbable matrix scaffold. Instr. Course Lect. 2008, 57, 563–571. [Google Scholar] [PubMed]
- Bornstein, M.M.; Bosshardt, D.; Buser, D. Effect of two different bioabsorbable collagen membranes on guided bone regeneration: A comparative histomorphometric study in the dog mandible. J. Periodontol. 2007, 78, 1943–1953. [Google Scholar] [CrossRef]
- Thoma, D.S.; Nänni, N.; Benic, G.I.; Weber, F.E.; Hämmerle, C.H.; Jung, R.E. Effect of platelet-derived growth factor-BB on tissue integration of cross-linked and non-cross-linked collagen matrices in a rat ectopic model. Clin. Oral Implants Res. 2015, 26, 263–270. [Google Scholar] [CrossRef]
- Pihlman, H.; Keränen, P.; Paakinaho, K.; Linden, J.; Hannula, M.; Manninen, I.K.; Hyttinen, J.; Manninen, M.; Laitinen-Vapaavuori, O. Novel osteoconductive β-tricalcium phosphate/poly(L-lactide-co-e-caprolactone) scaffold for bone regeneration: A study in a rabbit calvarial defect. J. Mater. Sci. Mater. Med. 2018, 29, 156. [Google Scholar] [CrossRef] [Green Version]
- Schaller, B.; Fujioka-Kobayashi, M.; Zihlmann, C.; Schuler, V.C.; Katagiri, H.; Lang, N.P.; Saulacic, N. Effects of additional collagen in biphasic calcium phosphates: A study in a rabbit calvaria. Clin. Oral Investig. 2020, 24, 3093–3103. [Google Scholar] [CrossRef]






Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Katagiri, H.; El Tawil, Y.; Lang, N.P.; Imber, J.-C.; Sculean, A.; Fujioka-Kobayashi, M.; Saulacic, N. Collagen-Based Matrices for Osteoconduction: A Preclinical In Vivo Study. Biomedicines 2021, 9, 143. https://doi.org/10.3390/biomedicines9020143
Katagiri H, El Tawil Y, Lang NP, Imber J-C, Sculean A, Fujioka-Kobayashi M, Saulacic N. Collagen-Based Matrices for Osteoconduction: A Preclinical In Vivo Study. Biomedicines. 2021; 9(2):143. https://doi.org/10.3390/biomedicines9020143
Chicago/Turabian StyleKatagiri, Hiroki, Yacine El Tawil, Niklaus P. Lang, Jean-Claude Imber, Anton Sculean, Masako Fujioka-Kobayashi, and Nikola Saulacic. 2021. "Collagen-Based Matrices for Osteoconduction: A Preclinical In Vivo Study" Biomedicines 9, no. 2: 143. https://doi.org/10.3390/biomedicines9020143
APA StyleKatagiri, H., El Tawil, Y., Lang, N. P., Imber, J.-C., Sculean, A., Fujioka-Kobayashi, M., & Saulacic, N. (2021). Collagen-Based Matrices for Osteoconduction: A Preclinical In Vivo Study. Biomedicines, 9(2), 143. https://doi.org/10.3390/biomedicines9020143






