Industrial Development of Standardized Fetal Progenitor Cell Therapy for Tendon Regenerative Medicine: Preliminary Safety in Xenogeneic Transplantation
Abstract
:1. Introduction
2. Materials and Methods
2.1. Primary hFPT Isolation, Cell Banking, and Characterization
2.1.1. Fetal Tendon Tissue Donation and Primary hFPT Enzymatic Isolation
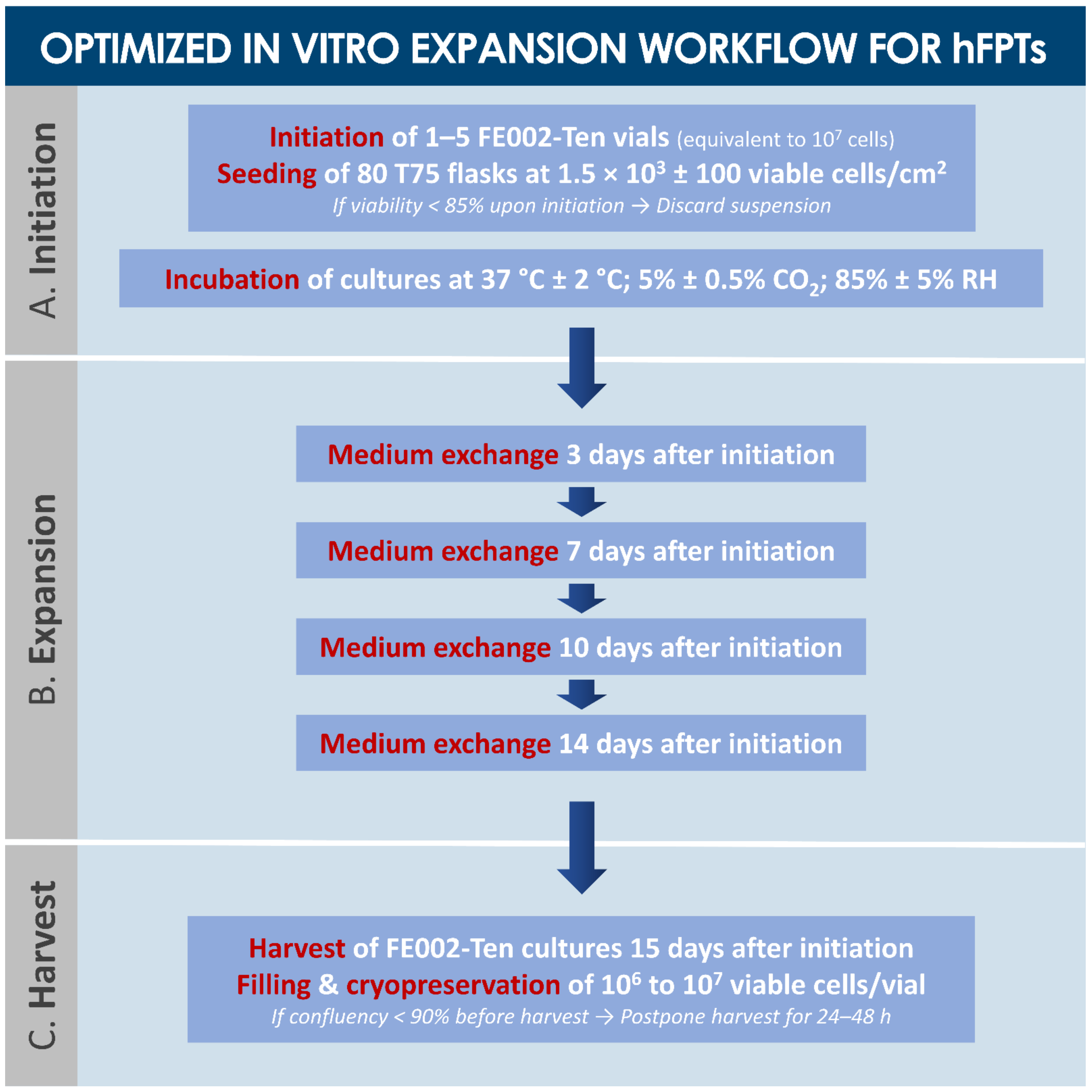
2.1.2. Pilot hFPT Expansion for Technical Specification Optimization
2.1.3. Optimized Multi-Tiered hFPT Biobanking Workflow Elaboration
2.2. In Vitro Tumorigenicity Study of hFPTs in Soft Agar Colony Formation Assays
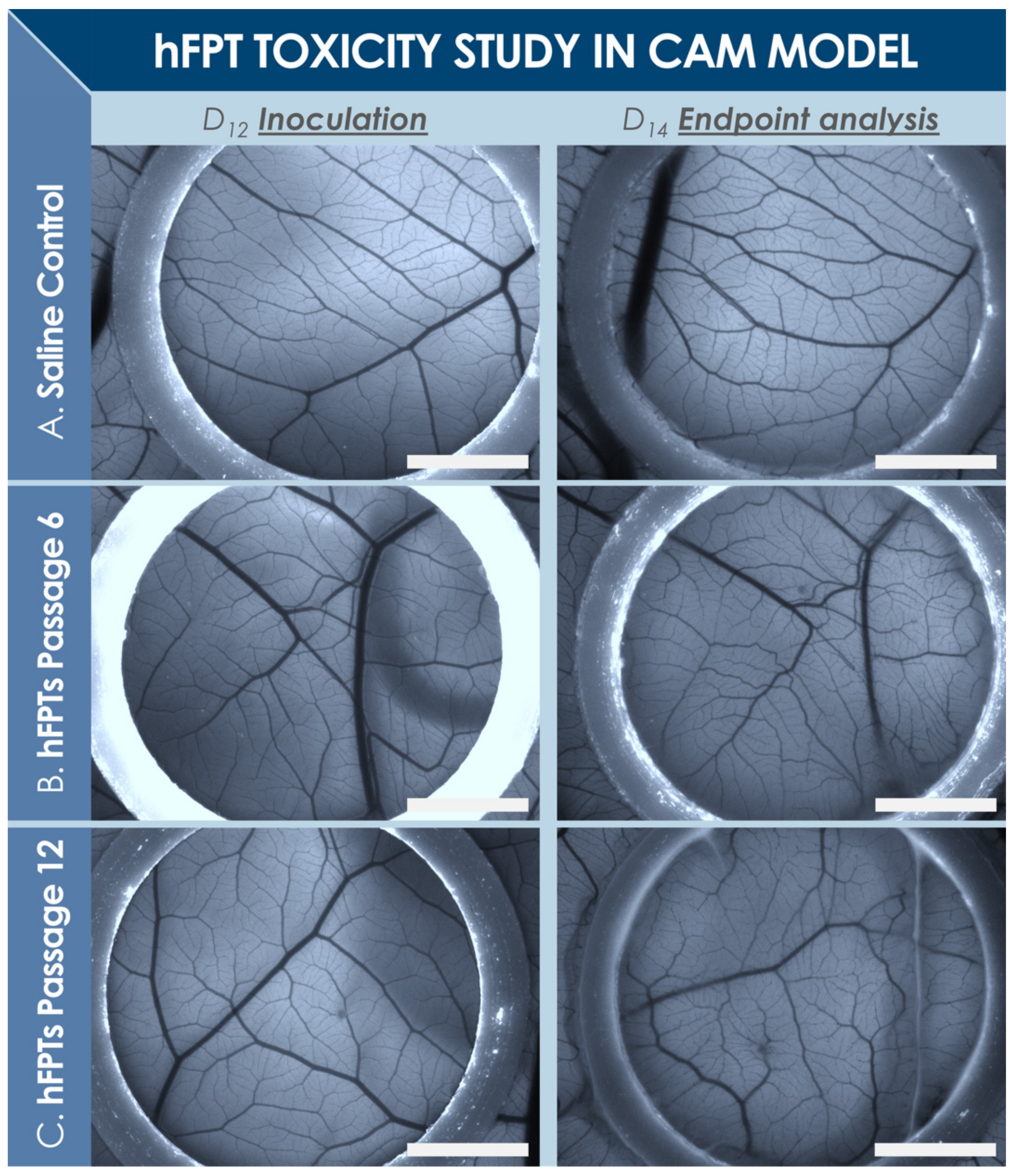
2.3. Preclinical Toxicity Study of hFPTs in a Standardized CAM Model
2.4. Preclinical Safety Study of hFPTs in a Rabbit Model of Patellar Tendon Defect
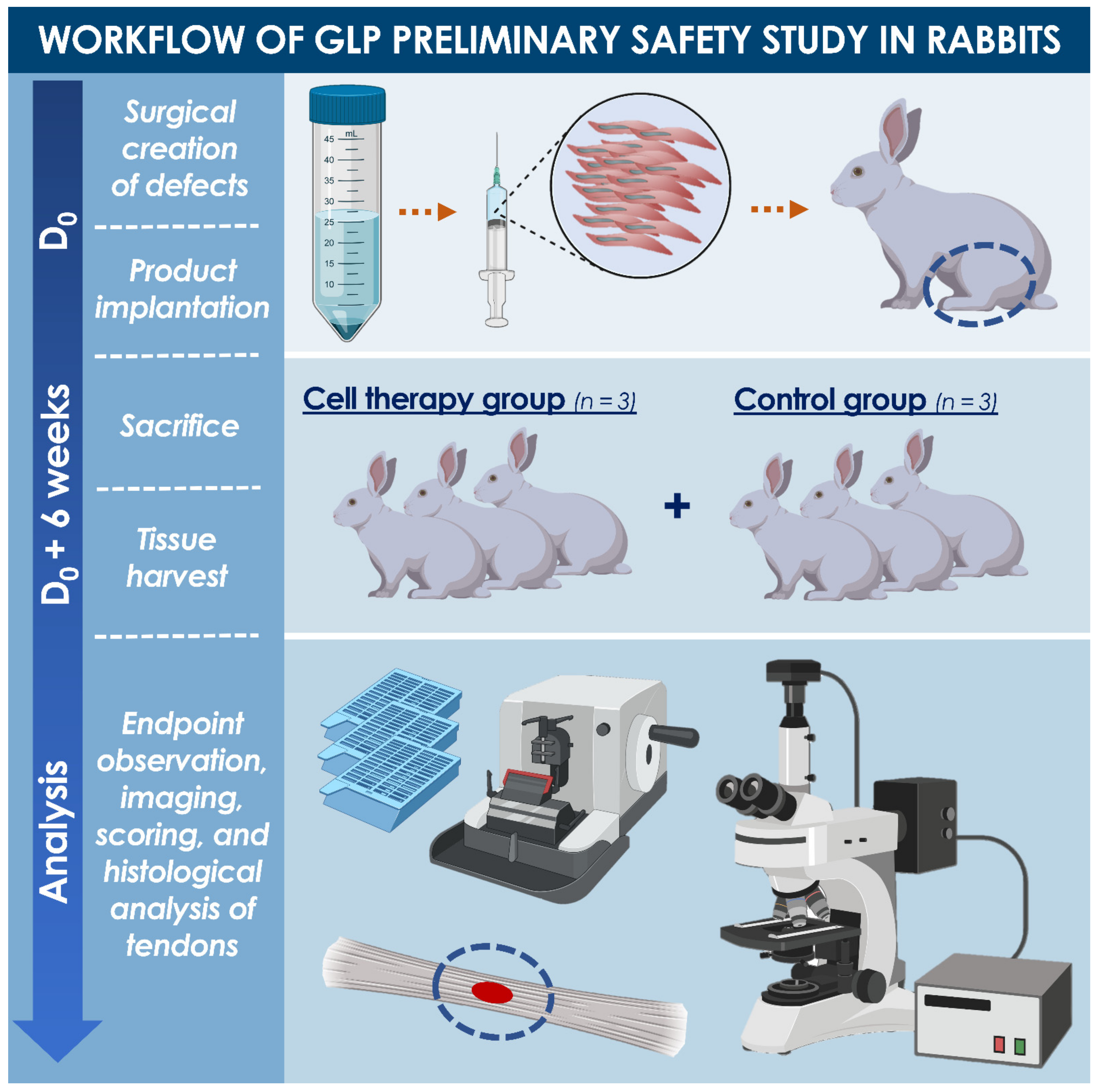
2.4.1. GLP Pilot Safety Study Design
2.4.2. GLP Pilot Safety Study Workflow
2.4.3. Processing of Harvested Tendons
2.4.4. Statistical Analysis
3. Results
3.1. Optimized Technical Specifications for Multi-Tiered hFPT Cell Banking
3.2. In Vitro Soft Agar Colony Formation Assays for hFPTs
3.3. In Ovo Standardized Toxicity Study of hFPTs
3.4. In Vivo Preliminary Safety of hFPTs in a Pilot GLP Study of Rabbit Tendon Defect
3.4.1. Treatment Administration and General Animal Observations
3.4.2. Study of Animal Blood Compositions
3.4.3. Macroscopic Evaluation of Harvested Tendon Tissues
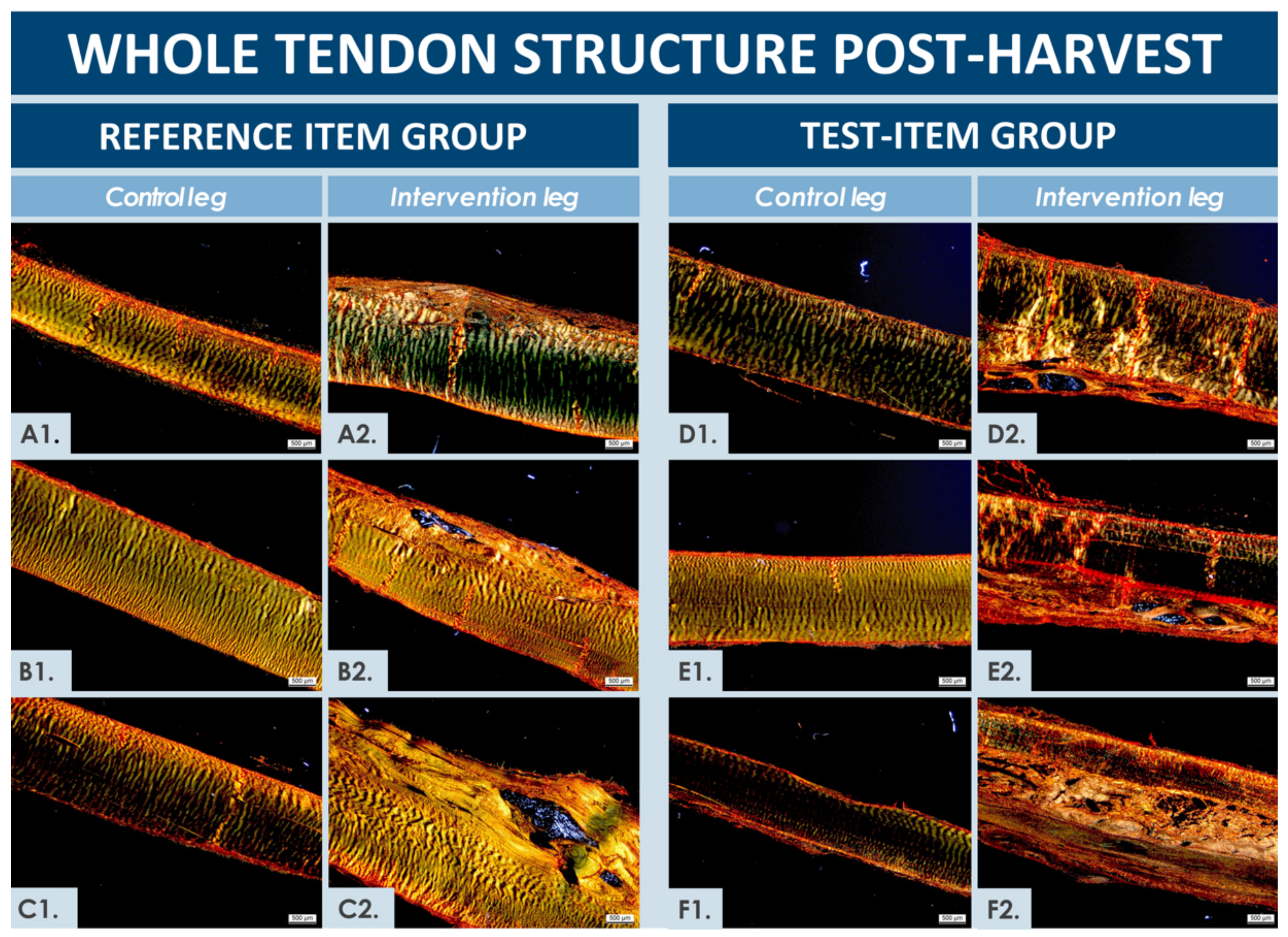
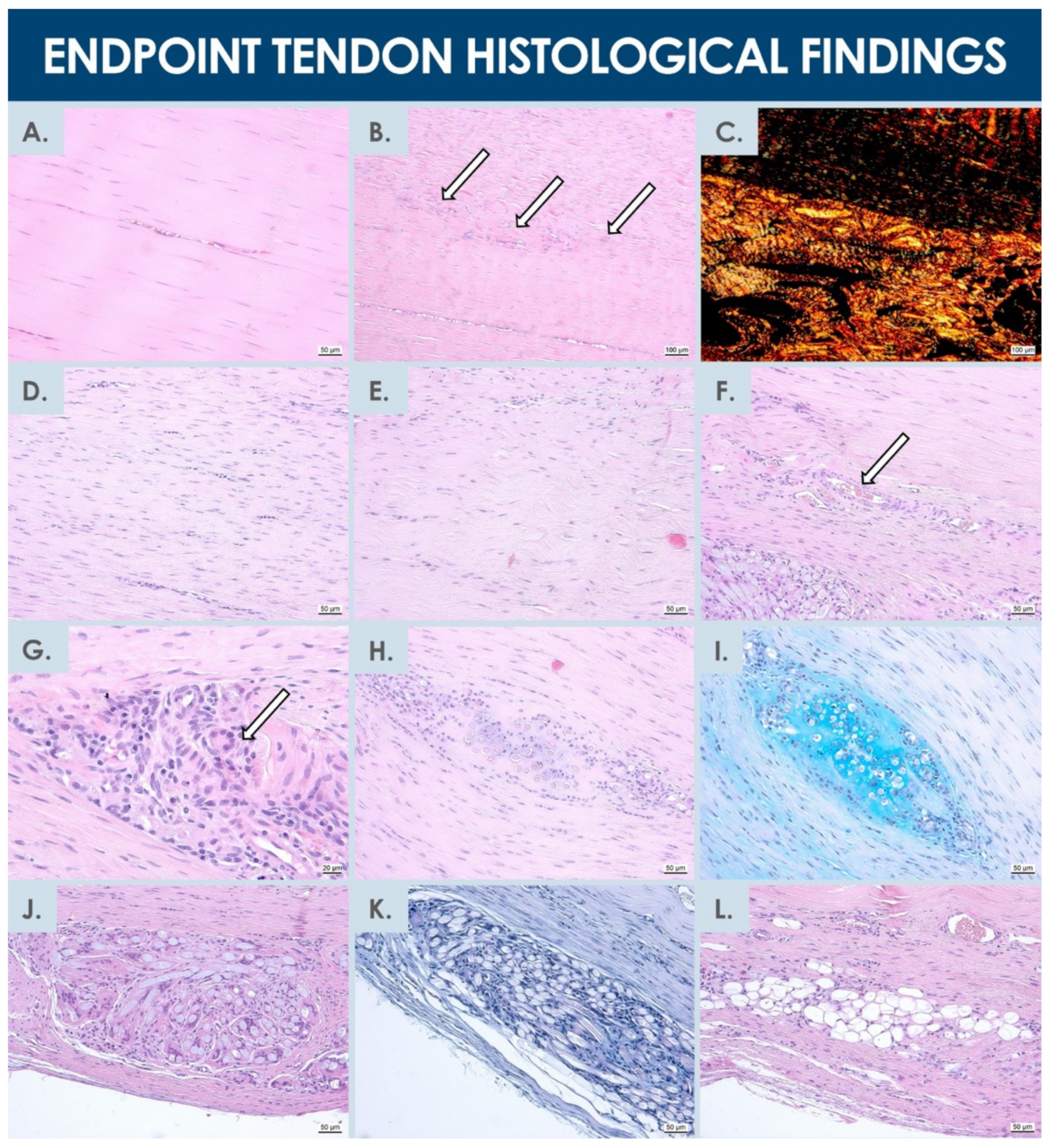
3.4.4. Microscopic and Histological Evaluation of Harvested Tendon Tissues
4. Discussion
4.1. Optimized Multi-Tiered hFPT Banking for Safe and Sustainable Tendon Cell Therapies
4.2. hFPTs for Formulation of Standardized Transplants in Tendon Tissue Engineering
4.3. High Clinical Need for Effective and Efficient Biological Products for Tendon Repair
4.4. Limited Available Cell Therapy Options for Tendon Regeneration
4.5. FE002-Ten hFPTs as Safe Cell Sources for Tendon Tissue Engineering
4.6. Study Limitations and Future Directions
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AB | Alcian blue |
| API | active pharmaceutical ingredient |
| BPyV | bovine polyomavirus |
| CAM | chorioallantoic membrane |
| CD | cluster of differentiation |
| CHUV | Centre hospitalier universitaire Vaudois |
| DMEM | Dulbecco’s modified Eagle medium |
| DMSO | dimethyl sulfoxide |
| EBV | Epstein-Barr virus |
| ECACC | European Collection of Authenticated Cell Cultures |
| ECM | extracellular matrix |
| EDTA | ethylenediaminetetraacetic acid |
| EOPCB | end of production cell bank |
| ESC | embryonic stem cell |
| ESWT | extracorporeal shock wave therapy |
| FBS | fetal bovine serum |
| FIRDI | Food Industry Research and Development Institute |
| FPC | fetal progenitor cells |
| GLP | good laboratory practices |
| GMP | good manufacturing practices |
| HA | hyaluronic acid |
| HAV | hepatitis A virus |
| HBV | hepatitis B virus |
| HBoV | human bocavirus |
| hCMV | human cytomegalovirus |
| HCV | hepatitis C virus |
| HE | hematoxylin-eosin |
| hFPT | human fetal progenitor tenocytes |
| HHV | human herpes virus |
| HIV | human immunodeficiency virus |
| HPV | human papilloma virus |
| HTLV | human T-cell lymphotropic virus |
| ISO | International Organization for Standardization |
| KIPyV | KI polyomavirus |
| MCB | master cell bank |
| MoA | mechanism of action |
| MRI | magnetic resonance imaging |
| MSC | mesenchymal stem cell |
| NO | nitric oxide |
| NSAID | non-steroidal anti-inflammatory drug |
| OECD | Organization for Economic Cooperation and Development |
| PBS | phosphate-buffered saline |
| PCB | parental cell bank |
| PDT | population doubling time |
| PDV | population doubling value |
| PEMF | pulsed electromagnetic field therapy |
| PRP | platelet-rich plasma |
| PTFE | polytetrafluoroethylene |
| RH | relative humidity |
| SAID | steroidal anti-inflammatory drug |
| SD | standard deviation |
| SR | Picrosirius red |
| SV40 | simian virus 40 |
| TEM | transmission electron microscopy |
| UK | United Kingdom |
| USA | United States of America |
| WCB | working cell bank |
| WUPyV | WU polyomavirus |
Appendix A
| Animal ID | Treatment Group | Operated Hindlimb |
|---|---|---|
| 1 | Test-item | Left |
| 2 | Test-item | Right |
| 3 | Test-item | Left |
| 4 | Reference item | Right |
| 5 | Reference item | Left |
| 6 | Reference item | Right |
| Parameter | Grading Scale with Corresponding Descriptions |
|---|---|
| Inflammation | 0 (None); 1 (Mild); 2 (Severe) |
| Tissue adhesion | 0 (Normal); 1 (Mild); 2 (Severe) |
| Fibrosis | 0 (None); 1 (Mild); 2 (Severe) |
| Defect filling extent and quality | 0 (Healthy tendon tissue with aligned fibers); 1 (Disorganized tendon tissue); 2 (Scar tissue, partial filling, or no filling) |
| Evaluation | Grading Scale with Corresponding Descriptions | ||
|---|---|---|---|
| Hypercellularity 1 [A – C] | A (None); B (Mild); C (High) | ||
| Vascularity 2 [A – D] | Hypervascularity | Predominant Size | Transverse Vessels |
| A (No); B (Yes) | A (Small); B (Large) | A (None, Rare); B (Some, Many) | |
| Inflammatory reaction [A – D] | A (None); B (Mild, some macrophages); C (Moderate, more macrophages, some foreign body cells); D (Severe, many foreign body cells, granulocytes) | ||
| Foreign material [A – C] | A (None); B (Some, scattered); C (More, clustered) | ||
| New matrix quality [A – C] | A (Tendon-like matrix); B (Pre-differentiated, immature matrix); C (Scar tissue, fibrosis) | ||
| New matrix directionality [A – C] | A (Aligned fibers); B (Mildly disorganized fibers); C (No discernable directionality) | ||
References
- Vacanti, J.P.; Langer, R. Tissue engineering: The design and fabrication of living replacement devices for surgical reconstruction and transplantation. Lancet 1999, 354, 32–34. [Google Scholar] [CrossRef]
- Marks, P.; Gottlieb, S. Balancing safety and innovation for cell-based regenerative medicine. N. Engl. J. Med. 2018, 378, 954–959. [Google Scholar] [CrossRef] [PubMed]
- De Jong, J.P.; Nguyen, J.T.; Sonnema, A.J.; Nguyen, E.C.; Amadio, P.C.; Moran, S.L. The incidence of acute traumatic tendon injuries in the hand and wrist: A 10-year population-based study. Clin. Orthop. Surg. 2014, 6, 196–202. [Google Scholar] [CrossRef] [PubMed]
- Clayton, R.A.; Court-Brown, C.M. The epidemiology of musculoskeletal tendinous and ligamentous injuries. Injury 2008, 39, 1338–1344. [Google Scholar] [CrossRef]
- Costa-Almeida, R.; Calejo, I.; Gomes, M.E. Mesenchymal stem cells empowering tendon regenerative therapies. Int. J. Mol. Sci. 2019, 20, 3002. [Google Scholar] [CrossRef] [Green Version]
- Romero, A.; Barrachina, L.; Ranera, B.; Remacha, A.R.; Moreno, B.; de Blas, I.; Sanz, A.; Vasquez, F.J.; Vitoria, A.; Junquera, C.; et al. Comparison of autologous bone marrow and adipose tissue derived mesenchymal stem cells, and platelet-rich plasma, for treating surgically induced lesions of the equine superficial digital flexor tendon. Vet. J. 2017, 224, 76–84. [Google Scholar] [CrossRef]
- Ribitsch, I.; Baptista, P.M.; Lange-Consiglio, A.; Melotti, L.; Patruno, M.; Jenner, F.; Schnabl-Feichter, E.; Dutton, L.C.; Connolly, D.J.; van Steenbeeck, F.G.; et al. Large animal models in regenerative medicine and tissue engineering: To Do or not to do. Front. Bioeng. Biotechnol. 2020, 8, 972. [Google Scholar] [CrossRef]
- Grognuz, A.; Aeberhard, P.A.; Michetti, M.; Hirt-Burri, N.; Scaletta, C.; de Buys Roessingh, A.S.; Raffoul, W.; Applegate, L.A. Cell therapies for tendon: Treatments and regenerative medicine. In Regenerative Medicine and Plastic Surgery; Duscher, D., Shiffman, M., Eds.; Springer Nature Switzerland AG: Cham, Switzerland, 2019; pp. 385–408. [Google Scholar] [CrossRef]
- Kane, S.F.; Olewinski, L.H.; Tamminga, K.S. Management of chronic tendon injuries. Am. Fam. Physician 2019, 100, 147–157. [Google Scholar]
- Van der Vlist, A.C.; Winters, M.; Weir, A.; Ardern, C.L.; Welton, N.J.; Caldwell, D.M.; Verhaar, J.A.; de Vos, R.J. Which treatment is most effective for patients with Achilles tendinopathy? A living systematic review with network meta-analysis of 29 randomised controlled trials. Br. J. Sports Med. 2021, 55, 249–256. [Google Scholar] [CrossRef]
- Jiang, N.; Wang, B.; Chen, A.; Dong, F.; Bin, Y. Operative versus nonoperative treatment for acute Achilles tendon rupture: A meta-analysis based on current evidence. Int. Orthop. 2012, 36, 765–773. [Google Scholar] [CrossRef] [Green Version]
- Sayel, F.A.; Pitakveerakul, A.; Alshalawi, S.; Wiewiorski, M.; Valderrabano, V. Neglected iatrogenic flexor hallucis longus tendon rupture after Haglund’s endoscopic surgery: A case report. J. Foot Ankle Surg. 2020, 59, 169–172. [Google Scholar] [CrossRef]
- Knobloch, K. Drug-induced tendon disorders. Adv. Exp. Med. Biol. 2016, 920, 229–238. [Google Scholar] [CrossRef]
- Abate, M.; Silbernagel, K.G.; Siljeholm, C.; Di Iorio, A.; De Amicis, D.; Salini, V.; Werner, S.; Paganelli, R. Pathogenesis of tendinopathies: Inflammation or degeneration? Arthritis Res. 2009, 11, 235. [Google Scholar] [CrossRef] [Green Version]
- Mehrzad, R.; Mookerjee, V.; Schmidt, S.; Jehle, C.C.; Kiwanuka, E.; Liu, P.Y. The economic impact of flexor tendon lacerations of the hand in the United States. Ann. Plast. Surg. 2019, 83, 419–423. [Google Scholar] [CrossRef]
- Hopkins, C.; Fu, S.C.; Chua, E.; Hu, X.; Rolf, C.; Mattila, V.M.; Qin, L.; Yung, P.S.; Chan, K.M. Critical review on the socio-economic impact of tendinopathy. Asia Pac. J. Sports Med. Arthrosc. Rehabil. Technol. 2016, 4, 9–20. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Verdan, C.E. Half a century of flexor-tendon surgery. Current status and changing philosophies. J. Bone Jt. Surg. Am. 1972, 54, 472–491. [Google Scholar] [CrossRef]
- Kannus, P.; Józsa, L. Histopathological changes preceding spontaneous rupture of a tendon. A controlled study of 891 patients. J. Bone Jt. Surg. Am. 1991, 73, 1507–1525. [Google Scholar] [CrossRef]
- Maffulli, N.; Wong, J.; Almekinders, L.C. Types and epidemiology of tendinopathy. Clin. Sports Med. 2003, 22, 675–692. [Google Scholar] [CrossRef]
- Sharma, P.; Maffulli, N. Tendon injury and tendinopathy: Healing and repair. J. Bone Jt. Surg. Am. 2005, 87, 187–202. [Google Scholar] [CrossRef] [Green Version]
- Tuncali, D.; Yavuz, N.; Terzioglu, A.; Aslan, G. The rate of upper-extremity deep-structure injuries through small penetrating lacerations. Ann. Plast. Surg. 2005, 55, 146–148. [Google Scholar] [CrossRef]
- Reinking, M. Tendinopathy in athletes. Phys. Sport 2012, 13, 3–10. [Google Scholar] [CrossRef] [PubMed]
- James, R.; Kesturu, G.; Balian, G.; Chhabra, A.B. Tendon: Biology, biomechanics, repair, growth factors, and evolving treatment options. J. Hand Surg. Am. 2008, 33, 102–112. [Google Scholar] [CrossRef]
- Voleti, P.B.; Buckley, M.R.; Soslowsky, L.J. Tendon healing: Repair and regeneration. Annu. Rev. Biomed. Eng. 2012, 14, 47–71. [Google Scholar] [CrossRef] [PubMed]
- O’Brien, M. Structure and metabolism of tendons. Scand. J. Med. Sci. Sports 1997, 7, 55–61. [Google Scholar] [CrossRef] [PubMed]
- Kannus, P. Structure of the tendon connective tissue. Scand. J. Med. Sci. Sports 2000, 10, 312–320. [Google Scholar] [CrossRef]
- Conrad, S.; Weber, K.; Walliser, U.; Geburek, F.; Skutella, T. Stem cell therapy for tendon regeneration: Current status and future directions. Adv. Exp. Med. Biol. 2019, 1084, 61–93. [Google Scholar] [CrossRef]
- Ho, J.O.; Sawadkar, P.; Mudera, V. A review on the use of cell therapy in the treatment of tendon disease and injuries. J. Tissue Eng. 2014, 5. [Google Scholar] [CrossRef]
- Wehbé, M.A. Tendon graft donor sites. J. Hand Surg. Am. 1992, 17, 1130–1132. [Google Scholar] [CrossRef]
- Valentin, J.E.; Badylak, J.S.; McCabe, G.P.; Badylak, S.F. Extracellular matrix bioscaffolds for orthopaedic applications. A comparative histologic study. J. Bone Jt. Surg. Am. 2006, 88, 2673–2686. [Google Scholar] [CrossRef]
- Chong, A.K.; Riboh, J.; Smith, R.L.; Lindsey, D.P.; Pham, H.M.; Chang, J. Flexor tendon tissue engineering: Acellularized and reseeded tendon constructs. Plast. Reconstr. Surg. 2009, 123, 1759–1766. [Google Scholar] [CrossRef]
- Jakubietz, M.G.; Jakubietz, D.F.; Gruenert, J.G.; Zahn, R.; Meffert, R.H.; Jakubietz, R.G. Adequacy of palmaris longus and plantaris tendons for tendon grafting. J. Hand Surg. Am. 2011, 36, 695–698. [Google Scholar] [CrossRef]
- Pridgen, B.C.; Woon, C.Y.; Kim, M.; Thorfinn, J.; Lindsey, D.; Pham, H.; Chang, J. Flexor tendon tissue engineering: Acellularization of human flexor tendons with preservation of biomechanical properties and biocompatibility. Tissue Eng. Part C Methods 2011, 17, 819–828. [Google Scholar] [CrossRef]
- Burk, J.; Plenge, A.; Brehm, W.; Heller, S.; Pfeiffer, B.; Kasper, C. Induction of tenogenic differentiation mediated by extracellular tendon matrix and short-term cyclic stretching. Stem Cells Int. 2016, 2016, 7342379. [Google Scholar] [CrossRef] [Green Version]
- Lovati, A.B.; Bottagisio, M.; Moretti, M. Decellularized and engineered tendons as biological substitutes: A critical review. Stem Cells Int. 2016, 2016, 7276150. [Google Scholar] [CrossRef] [Green Version]
- Aeberhard, P.A.; Grognuz, A.; Peneveyre, C.; McCallin, S.; Hirt-Burri, N.; Antons, J.; Pioletti, D.P.; Raffoul, W.; Applegate, L.A. Efficient decellularization of equine tendon with preserved biomechanical properties and cytocompatibility for human tendon surgery indications. Artif. Organs 2019, 44, E161–E171. [Google Scholar] [CrossRef]
- Petrou, I.G.; Grognuz, A.; Hirt-Burri, N.; Raffoul, W.; Applegate, L.A. Cell therapies for tendons: Old cell choice for modern innovation. Swiss Med. Wkly. 2014, 144, w13989. [Google Scholar] [CrossRef]
- Adzick, N.S.; Longaker, M.T. Scarless fetal healing. Therapeutic implications. Ann. Surg. 1992, 215, 3–7. [Google Scholar] [CrossRef]
- Awad, H.A.; Boivin, G.P.; Dressler, M.R.; Smith, F.N.; Young, R.G.; Butler, D.L. Repair of patellar tendon injuries using a cell-collagen composite. J. Orthop. Res. 2003, 21, 420–431. [Google Scholar] [CrossRef]
- Chen, X.; Song, X.H.; Yin, Z.; Zou, X.H.; Wang, L.L.; Hu, H.; Cao, T.; Zheng, M.; Ouyang, H.W. Stepwise differentiation of human embryonic stem cells promotes tendon regeneration by secreting fetal tendon matrix and differentiation factors. Stem Cells 2009, 27, 1276–1287. [Google Scholar] [CrossRef]
- Akhundov, K.; Pietramaggiori, G.; Waselle, L.; Darwiche, S.; Guerid, S.; Scaletta, C.; Hirt-Burri, N.; Applegate, L.A.; Raffoul, W. Development of a cost-effective method for platelet-rich plasma (PRP) preparation for topical wound healing. Ann. Burn. Fire Disasters 2012, 25, 207–213. [Google Scholar]
- Xu, W.; Wang, Y.; Liu, E.; Sun, Y.; Luo, Z.; Xu, Z.; Liu, W.; Zhong, L.; Lv, Y.; Wang, A.; et al. Human iPSC-derived neural crest stem cells promote tendon repair in a rat patellar tendon window defect model. Tissue Eng. Part A 2013, 19, 2439–2451. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chong, A.K.; Ang, A.D.; Goh, J.C.; Hui, J.H.; Lim, A.Y.; Lee, E.H.; Lim, B.H. Bone marrow-derived mesenchymal stem cells influence early tendon-healing in a rabbit Achilles tendon model. J. Bone Jt. Surg. Am. 2007, 89, 74–81. [Google Scholar] [CrossRef]
- Connell, D.; Datir, A.; Alyas, F.; Curtis, M. Treatment of lateral epicondylitis using skin-derived tenocyte-like cells. Br. J. Sports Med. 2009, 43, 293–298. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Docheva, D.; Muller, S.A.; Majewski, M.; Evans, C.H. Biologics for tendon repair. Adv. Drug Deliv. Rev. 2015, 84, 222–239. [Google Scholar] [CrossRef] [Green Version]
- Van den Boom, N.A.C.; Winters, M.; Haisma, H.J.; Moen, M.H. Efficacy of stem cell therapy for tendon disorders: A systematic review. Orthop. J. Sports Med. 2020, 8, 2325967120915857. [Google Scholar] [CrossRef]
- Chen, J.; Yu, Q.; Wu, B.; Lin, Z.; Pavlos, N.J.; Xu, J.; Ouyang, H.; Wang, A.; Zheng, M.H. Autologous tenocyte therapy for experimental Achilles tendinopathy in a rabbit model. Tissue Eng. Part A 2011, 17, 2037–2048. [Google Scholar] [CrossRef]
- Grognuz, A.; Scaletta, C.; Farron, A.; Pioletti, D.P.; Raffoul, W.; Applegate, L.A. Stability enhancement using hyaluronic acid gels for delivery of human fetal progenitor tenocytes. Cell Med. 2016, 8, 87–97. [Google Scholar] [CrossRef] [Green Version]
- Grognuz, A.; Scaletta, C.; Farron, A.; Raffoul, W.; Applegate, L.A. Human fetal progenitor tenocytes for regenerative medicine. Cell Transpl. 2016, 25, 463–479. [Google Scholar] [CrossRef] [Green Version]
- Hulmes, D.J. Building collagen molecules, fibrils, and suprafibrillar structures. J. Struct. Biol. 2002, 137, 2–10. [Google Scholar] [CrossRef]
- Le Blanc, K.; Tammik, C.; Rosendahl, K.; Zetterberg, E.; Ringden, O. HLA expression and immunologic properties of differentiated and undifferentiated mesenchymal stem cells. Exp. Hematol. 2003, 31, 890–896. [Google Scholar] [CrossRef]
- Docheva, D.; Hunziker, E.B.; Fässler, R.; Brandau, O. Tenomodulin is necessary for tenocyte proliferation and tendon maturation. Mol. Cell Biol. 2005, 25, 699–705. [Google Scholar] [CrossRef] [Green Version]
- Murchison, N.D.; Price, B.A.; Conner, D.A.; Keene, D.R.; Olson, E.N.; Tabin, C.J.; Schweizer, R. Regulation of tendon differentiation by scleraxis distinguishes force-transmitting tendons from muscle-anchoring tendons. Development 2007, 134, 2697–2708. [Google Scholar] [CrossRef] [Green Version]
- Banos, C.C.; Thomas, A.H.; Kuo, C.K. Collagen fibrillogenesis in tendon development: Current models and regulation of fibril assembly. Birth Defects Res. C. Embryo Today 2008, 84, 228–244. [Google Scholar] [CrossRef]
- Taylor, S.E.; Vaughan-Thomas, A.; Clements, D.N.; Pinchbeck, G.; Macrory, L.C.; Smith, R.K.; Clegg, P.D. Gene expression markers of tendon fibroblasts in normal and diseased tissue compared to monolayer and three-dimensional culture systems. BMC Musculoskelet. Disord. 2009, 10, 27. [Google Scholar] [CrossRef] [Green Version]
- Andres, B.M.; Murrell, G.A. Treatment of tendinopathy: What works, what does not, and what is on the horizon. Clin. Orthop. Relat. Res. 2008, 466, 1539–1554. [Google Scholar] [CrossRef] [Green Version]
- Childress, M.A.; Beutler, A. Management of chronic tendon injuries. Am. Fam. Physician 2013, 87, 486–490. [Google Scholar]
- Andriolo, L.; Altamura, S.A.; Reale, D.; Candrian, C.; Zaffagnini, S.; Filardo, G. Nonsurgical treatments of patellar tendinopathy: Multiple injections of platelet-rich plasma are a suitable option: A systematic review and meta-analysis. Am. J. Sports Med. 2019, 47, 1001–1018. [Google Scholar] [CrossRef]
- Loiacono, C.; Palermi, S.; Massa, B.; Belviso, I.; Romano, V.; Di Gregorio, A.; Sirico, F.; Sacco, A.M. Tendinopathy: Pathophysiology, therapeutic options, and role of nutraceutics. A narrative literature review. Medicina 2019, 55, 447. [Google Scholar] [CrossRef] [Green Version]
- Applegate, L.A.; Scaletta, C.; Hirt-Burri, N.; Raffoul, W.; Pioletti, D.P. Whole-cell bioprocessing of human fetal cells for tissue engineering of skin. Ski. Pharm. Physiol. 2009, 22, 63–73. [Google Scholar] [CrossRef] [Green Version]
- Laurent, A.; Lin, P.; Scaletta, C.; Hirt-Burri, N.; Michetti, M.; de Buys Roessingh, A.S.; Raffoul, W.; She, B.R.; Applegate, L.A. Bringing safe and standardized cell therapies to industrialized processing for burns and wounds. Front. Bioeng. Biotechnol. 2020, 8, 581. [Google Scholar] [CrossRef]
- Applegate, L.A.; Weber, D.; Simon, J.P.; Scaletta, C.; Hirt-Burri, N.; de Buys Roessingh, A.S.; Raffoul, W. Organ donation and whole-cell bioprocessing in the Swiss fetal progenitor celltransplantation platform. In Organ Donation and Organ Donors; Saidi, R.F., Ed.; Nova Science Publishers: New York, NY, USA, 2013; pp. 125–147. [Google Scholar]
- Laurent, A.; Scaletta, C.; Hirt-Burri, N.; Raffoul, W.; de Buys Roessingh, A.S.; Applegate, L.A. Swiss Fetal Transplantation Program and nonenzymatically isolated primary progenitor cell types for regenerative medicine. In Stem Cells and Good Manufacturing Practices: Methods and Protocols; Kursad, T., Ed.; Springer Science+Business Media: New York, NY, USA, 2020. [Google Scholar] [CrossRef]
- Applegate, L.A.; Hirt-Burri, N.; Scaletta, C.; Bauen, J.F.; Pioletti, D.P. Bioengineering of human fetal tissues for clinical use. In Bioengineering: Principles, Methodologies and Applications; Saidi, R.F., Ed.; Nova Sciences Publishers: New York, NY, USA, 2009; pp. 1–19. [Google Scholar]
- Laurent, A.; Hirt-Burri, N.; Scaletta, C.; Michetti, M.; de Buys Roessingh, A.S.; Raffoul, W.; Applegate, L.A. Holistic approach of Swiss fetal progenitor cell banking: Optimizing safe and sustainable substrates for regenerative medicine and biotechnology. Front. Bioeng. Biotechnol. 2020, 8, 557758. [Google Scholar] [CrossRef]
- Laurent, A.; Scaletta, C.; Michetti, M.; Hirt-Burri, N.; de Buys Roessingh, A.S.; Raffoul, W.; Applegate, L.A. GMP tiered cell banking of non-enzymatically isolated dermal progenitor fibroblasts for allogenic regenerative medicine. In Stem Cells and Good Manufacturing Practices: Methods and Protocols; Kursad, T., Ed.; Springer Science+Business Media: New York, NY, USA, 2020. [Google Scholar] [CrossRef]
- Schöffl, V.; Heid, A.; Küpper, T. Tendon injuries of the hand. World J. Orthop. 2012, 3, 62–69. [Google Scholar] [CrossRef] [PubMed]
- Dahlgren, L.A.; Mohammed, H.O.; Nixon, A.J. Temporal expression of growth factors and matrix molecules in healing tendon lesions. J. Orthop. Res. 2005, 23, 84–92. [Google Scholar] [CrossRef]
- Eriksen, H.A.; Pajala, A.; Leppilahti, J.; Risteli, J. Increased content of type III collagen at the rupture site of human Achilles tendon. J. Orthop. Res. 2002, 20, 1352–1357. [Google Scholar] [CrossRef]
- Sharma, P.; Maffulli, N. Biology of tendon injury: Healing, modeling and remodeling. J. Musculoskelet. Neuronal Interact. 2006, 6, 181–190. [Google Scholar] [PubMed]
- Liu, C.F.; Aschbacher-Smith, L.; Barthelery, N.J.; Dyment, N.; Butler, D.; Wylie, C. What we should know before using tissue engineering techniques to repair injured tendons: A developmental biology perspective. Tissue Eng. Part B Rev. 2011, 17, 165–176. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hasslund, S.; Jacobson, J.A.; Dadali, T.; Basile, P.; Ulrich-Vinter, M.; Soballe, K.; Schwarz, E.M.; O’Keefe, R.J.; Mitten, D.J.; Awad, H.A. Adhesions in a murine flexor tendon graft model: Autograft versus allograft reconstruction. J. Orthop. Res. 2008, 26, 824–833. [Google Scholar] [CrossRef] [Green Version]
- Kaviani, A.; Perry, T.E.; Barnes, C.M.; Oh, J.T.; Ziegler, M.M.; Fishman, S.J.; Fauza, D.O. The placenta as a cell source in fetal tissue engineering. J. Pediatr. Surg. 2002, 37, 995–999. [Google Scholar] [CrossRef]
- Kryger, G.S.; Chong, A.K.; Costa, M.; Pham, H.; Bates, S.J.; Chang, J. A comparison of tenocytes and mesenchymal stem cells for use in flexor tendon tissue engineering. J. Hand Surg. Am. 2007, 32, 597–605. [Google Scholar] [CrossRef]
- Gulotta, L.V.; Kovacevic, D.; Packer, J.D.; Deng, X.H.; Rodeo, S.A. Bone marrow-derived mesenchymal stem cells transduced with scleraxis improve rotator cuff healing in a rat model. Am. J. Sports Med. 2011, 39, 1282–1289. [Google Scholar] [CrossRef]
- Butler, D.L.; Juncosa-Melvin, N.; Boivin, G.P.; Galloway, M.T.; Shearn, J.T.; Gooch, C.; Awad, H. Functional tissue engineering for tendon repair: A multidisciplinary strategy using mesenchymal stem cells, bioscaffolds, and mechanical stimulation. J. Orthop. Res. 2008, 26, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Ouyang, H.W.; Goh, J.C.; Thambyah, A.; Teoh, S.H.; Lee, E.H. Knitted poly-lactide-co-glycolide scaffold loaded with bone marrow stromal cells in repair and regeneration of rabbit Achilles tendon. Tissue Eng. 2003, 9, 431–439. [Google Scholar] [CrossRef]
- Watts, A.E.; Yeager, A.E.; Kopyov, O.V.; Nixon, A.J. Fetal derived embryonic-like stem cells improve healing in a large animal flexor tendonitis model. Stem Cell Res. 2011, 2, 4. [Google Scholar] [CrossRef] [Green Version]
- Ellera Gomes, J.L.; da Silva, R.C.; Silla, L.M.; Abreu, M.R.; Pellanda, R. Conventional rotator cuff repair complemented by the aid of mononuclear autologous stem cells. Knee Surg. Sports Traumatol. Arthrosc. 2012, 20, 373–377. [Google Scholar] [CrossRef] [Green Version]
- Woon, C.Y.; Farnebo, S.; Schmitt, T.; Kraus, A.; Megerle, K.; Pham, H.; Yan, X.; Gambhir, S.S.; Chang, J. Human flexor tendon tissue engineering: Revitalization of biostatic allograft scaffolds. Tissue Eng. Part A 2012, 18, 2406–2417. [Google Scholar] [CrossRef]
- Beck, J.; Evans, D.; Tonino, P.M.; Yong, S.; Callaci, J.J. The biomechanical and histologic effects of platelet-rich plasma on rat rotator cuff repairs. Am. J. Sports Med. 2012, 40, 2037–2044. [Google Scholar] [CrossRef]
- Hernández-Martínez, J.C.; Vásquez, C.R.; Ceja, C.B.; Fuentes, C.C.; Sesma, J.F.; Benitez, A.G. Comparative study on animal model of acute Achilles tendon rupture with surgical treatment using platelet-rich plasma. Acta Ortop. Mex. 2012, 26, 170–173. [Google Scholar]
- Sato, D.; Takahara, M.; Narita, A.; Yamakawa, J.; Hashimoto, J.; Ishikawa, H.; Ogino, T. Effect of platelet-rich plasma with fibrin matrix on healing of intrasynovial flexor tendons. J. Hand Surg. Am. 2012, 37, 1356–1363. [Google Scholar] [CrossRef]
- Randelli, P.S.; Arrigoni, P.; Cabitza, P.; Volpi, P.; Maffulli, N. Autologous platelet-rich plasma for arthroscopic rotator cuff repair. A pilot study. Disabil. Rehabil. 2008, 30, 1584–1589. [Google Scholar] [CrossRef]
- Maniscalco, P.; Gambera, D.; Lunati, A.; Vox, G.; Fossombroni, V.; Beretta, R.; Crainz, E. The “Cascade” membrane: A new PRP device for tendon ruptures. Description and case report on rotator cuff tendon. Acta Biomed. 2008, 79, 223–226. [Google Scholar]
- Sánchez, M.; Anitua, E.; Azofra, J.; Andia, I.; Padilla, S.; Mujika, I. Comparison of surgically repaired Achilles tendon tears using platelet-rich fibrin matrices. Am. J. Sports Med. 2007, 35, 245–251. [Google Scholar] [CrossRef] [PubMed]
- Schepull, T.; Kvist, J.; Norrman, H.; Trinks, M.; Berlin, G.; Aspenberg, P. Autologous platelets have no effect on the healing of human Achilles tendon ruptures: A randomized single-blind study. Am. J. Sports Med. 2011, 39, 38–47. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Martinello, T.; Bronzini, I.; Perazzi, A.; Testoni, S.; De Benedictis, G.M.; Negro, A.; Caporale, G.; Mascarello, F.; Iacopetti, I.; Patruno, M. Effects of in vivo applications of peripheral blood-derived mesenchymal stromal cells (PB-MSCs) and platlet-rich plasma (PRP) on experimentally injured deep digital flexor tendons of sheep. J. Orthop. Res. 2013, 31, 306–314. [Google Scholar] [CrossRef] [PubMed]
- Thanasas, C.; Papadimitriou, G.; Charalambidis, C.; Paraskevopoulos, I.; Papanikolaou, A. Platelet-rich plasma versus autologous whole blood for the treatment of chronic lateral elbow epicondylitis: A randomized controlled clinical trial. Am. J. Sports Med. 2011, 39, 2130–2134. [Google Scholar] [CrossRef]
- Gosens, T.; Peerbooms, J.C.; van Laar, W.; den Oudsten, B.L. Ongoing positive effect of platelet-rich plasma versus corticosteroid injection in lateral epicondylitis: A double-blind randomized controlled trial with 2-year follow-up. Am. J. Sports Med. 2011, 39, 1200–1208. [Google Scholar] [CrossRef]
- Ribatti, D. The chick embryo chorioallantoic membrane (CAM). A multifaceted experimental model. Mech. Dev. 2016, 141, 70–77. [Google Scholar] [CrossRef]
- Kunz, P.; Schenker, A.; Sähr, H.; Lehner, B.; Fellenberg, J. Optimization of the chicken chorioallantoic membrane assay as reliable in vivo model for the analysis of osteosarcoma. PLoS ONE 2019, 14, e0215312. [Google Scholar] [CrossRef]
- Derwin, K.A.; Baker, A.R.; Iannotti, J.P.; McCarron, J.A. Preclinical models for translating regenerative medicine therapies for rotator cuff repair. Tissue Eng. Part B Rev. 2010, 16, 21–30. [Google Scholar] [CrossRef] [Green Version]
- Lemme, N.J.; Li, N.Y.; DeFroda, S.F.; Kleiner, J.; Owens, B.D. Epidemiology of Achilles tendon ruptures in the United States: Athletic and nonathletic injuries from 2012 to 2016. Orthop. J. Sports Med. 2018, 6, 2325967118808238. [Google Scholar] [CrossRef] [Green Version]
- Beredjiklian, P.K.; Favata, M.; Cartmell, J.S.; Flanagan, C.L.; Crombleholme, T.M.; Soslowsky, J.L. Regenerative versus reparative healing in tendon: A study of biomechanical and histological properties in fetal sheep. Ann. Biomed. Eng. 2003, 31, 1143–1152. [Google Scholar] [CrossRef]
- Sørensen, A.K.; Bak, K.; Krarup, A.L.; Thune, C.H.; Nygaard, M.; Jorgensen, U.; Sloth, C.; Torp-Pedersen, S. Acute rotator cuff tear: Do we miss the early diagnosis? A prospective study showing a high incidence of rotator cuff tears after shoulder trauma. J. Shoulder Elb. Surg. 2007, 16, 174–180. [Google Scholar] [CrossRef]
- De Buys Roessingh, A.S.; Hohlfeld, J.; Scaletta, C.; Hirt-Burri, N.; Gerber, S.; Hohlfeld, P.; Gebbers, J.O.; Applegate, L.A. Development, characterization, and use of a fetal skin cell bank for tissue engineering in wound healing. Cell Transpl. 2006, 15, 823–834. [Google Scholar] [CrossRef] [Green Version]
- Hohlfeld, J.; de Buys Roessingh, A.S.; Hirt-Burri, N.; Chaubert, P.; Gerber, S.; Scaletta, C.; Hohlfeld, P.; Applegate, L.A. Tissue engineered fetal skin constructs for paediatric burns. Lancet 2005, 366, 840–842. [Google Scholar] [CrossRef]
- Quintin, A.; Hirt-Burri, N.; Scaletta, C.; Schizas, C.; Pioletti, D.P.; Applegate, L.A. Consistency and safety of cell banks for research and clinical use: Preliminary analysis of fetal skin banks. Cell Transpl. 2007, 16, 675–684. [Google Scholar] [CrossRef] [Green Version]
- Ramelet, A.A.; Hirt-Burri, N.; Raffoul, W.; Scaletta, C.; Pioletti, D.P.; Offord, E.; Mansourian, R.; Applegate, L.A. Chronic wound healing by fetal cell therapy may be explained by differential gene profiling observed in fetal versus old skin cells. Exp. Gerontol. 2009, 44, 208–218. [Google Scholar] [CrossRef] [Green Version]
- De Buys Roessingh, A.S.; Hirt-Burri, N.; Raffoul, W.; Scaletta, C.; Applegate, L.A. A Decade after foetal skin progenitor cell therapy in pediatric burn treatment. J. Regen. Med. 2015, 4, 1. [Google Scholar] [CrossRef]
- Al-Dourobi, K.; Laurent, A.; Deghayli, L.; Flahaut, M.; Abdel-Sayed, P.; Scaletta, C.; Michetti, M.; Waselle, L.; Simon, J.P.; Ezzi, O.E.; et al. Retrospective evaluation of Progenitor Biological Bandage use: A complementary and safe therapeutic management option for prevention of hypertrophic scarring in pediatric burn care. Pharmaceuticals 2021, 14, 201. [Google Scholar] [CrossRef]

| Test-Parameter | Variables and Grading | ||||||
|---|---|---|---|---|---|---|---|
| Culture vessel brand and surface (cm2) 1 | Nunc™ EasYFlask™ | TPP® VENT Flasks | Corning® TC Treated Flasks | ||||
| ++ | ++ | ++ | |||||
| T75 | T225 | T75 | T150 | T75 | T175 | ||
| +++ | + | +++ | ++ | ++ | ++ | ||
| FBS source and lot | Sigma® lot A | Sigma® lot B | Sigma® lot C | Invitrogen® lot A | Invitrogen® lot B | HyClone™ lot A | |
| +++ | + | ++ | ++ | − | + | ||
| Cell seeding density (viable cells/cm2) | 1.0 × 103 | 1.5 × 103 | 3.0 × 103 | 6.0 × 103 | 1.0 × 104 | 2.0 × 104 | |
| + | +++ | +++ | ++ | + | + | ||
| Relative culture medium volume (mL/75 cm2) | 5.0 | 7.5 | 10.0 | 12.5 | 15.0 | 17.5 | |
| − | + | +++ | +++ | ++ | + | ||
| Culture period from seeding to harvest (days) | 10 | 12 | 14 | 16 | 18 | 20 | |
| − | + | +++ | +++ | + | − | ||
| Passage Number | Cell Bank Tier | Average Vial Quantities/Batch at Each Harvest | PDT (h) | Viability 1 (%) | Sterility (+ or −) | Mycoplasma (+ or −) | Morphology 2 (+ or −) |
|---|---|---|---|---|---|---|---|
| 1 | [PCB] | 80–100 | 82 ± 3 | 99 ± 1 | + | − | + |
| 2 | [MCB] | 80–100 | 82 ± 5 | 98 ± 2 | + | − | + |
| 3 | [WCBT1] 3 | 200–250 | 84 ± 4 | 98 ± 2 | + | − | + |
| 4 | [WCBT2] | 200–250 | 86 ± 6 | 99 ± 1 | + | − | + |
| 5 | [WCBT3] | 200–250 | 88 ± 5 | 97 ± 1 | + | − | + |
| 6 | [WCBT4] | 200–250 | 87 ± 6 | 98 ± 2 | + | − | + |
| 7 | [WCBT5] | 200–250 | 88 ± 7 | 99 ± 1 | + | − | + |
| 8 | / | 20–30 | 91 ± 4 | 97 ± 3 | + | − | + |
| 9 | / | 20–30 | 93 ± 9 | 98 ± 2 | + | − | + |
| 10 | / | 20–30 | 100 ± 7 | 97 ± 1 | + | − | + |
| 11 | / | 20–30 | 108 ± 12 | 97 ± 1 | + | − | + |
| 12 | [EOPCB] | 50–60 | 111 ± 11 | 98 ± 2 | + | − | + |
| Cellularity | Vasculature | Inflammation | Biomaterial Presence | Tissue Quality | Alignment | |
|---|---|---|---|---|---|---|
| Score ranges | [A–C] | [A–D] | [A–D] | [A–C] | [A–C] | [A–C] |
| Test-item group | 3 × C | 1 × A; 1 × C-D; 1 × D | 1 × B; 1 × B-C; 1 × C | 2 × A; 1 × B | 2 × A; 1 × B | 2 × B; 1 × C |
| Reference item group | 1 × B-C; 2 × C | 1 × B; 1 × B-C; 1 × C | 1 × A-B; 1 × B; 1 × C | 1 × A; 1 × A-B; 1 × B | 2 × A; 1 × B | 3 × B |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Laurent, A.; Abdel-Sayed, P.; Grognuz, A.; Scaletta, C.; Hirt-Burri, N.; Michetti, M.; de Buys Roessingh, A.S.; Raffoul, W.; Kronen, P.; Nuss, K.; et al. Industrial Development of Standardized Fetal Progenitor Cell Therapy for Tendon Regenerative Medicine: Preliminary Safety in Xenogeneic Transplantation. Biomedicines 2021, 9, 380. https://doi.org/10.3390/biomedicines9040380
Laurent A, Abdel-Sayed P, Grognuz A, Scaletta C, Hirt-Burri N, Michetti M, de Buys Roessingh AS, Raffoul W, Kronen P, Nuss K, et al. Industrial Development of Standardized Fetal Progenitor Cell Therapy for Tendon Regenerative Medicine: Preliminary Safety in Xenogeneic Transplantation. Biomedicines. 2021; 9(4):380. https://doi.org/10.3390/biomedicines9040380
Chicago/Turabian StyleLaurent, Alexis, Philippe Abdel-Sayed, Anthony Grognuz, Corinne Scaletta, Nathalie Hirt-Burri, Murielle Michetti, Anthony S. de Buys Roessingh, Wassim Raffoul, Peter Kronen, Katja Nuss, and et al. 2021. "Industrial Development of Standardized Fetal Progenitor Cell Therapy for Tendon Regenerative Medicine: Preliminary Safety in Xenogeneic Transplantation" Biomedicines 9, no. 4: 380. https://doi.org/10.3390/biomedicines9040380
APA StyleLaurent, A., Abdel-Sayed, P., Grognuz, A., Scaletta, C., Hirt-Burri, N., Michetti, M., de Buys Roessingh, A. S., Raffoul, W., Kronen, P., Nuss, K., von Rechenberg, B., Applegate, L. A., & Darwiche, S. E. (2021). Industrial Development of Standardized Fetal Progenitor Cell Therapy for Tendon Regenerative Medicine: Preliminary Safety in Xenogeneic Transplantation. Biomedicines, 9(4), 380. https://doi.org/10.3390/biomedicines9040380








