Post-Event Application of Neurotropin Protects against Ischemic Insult toward Better Outcomes in a Murine Model of Subarachnoid Hemorrhage
Abstract
:1. Introduction
2. Materials and Methods
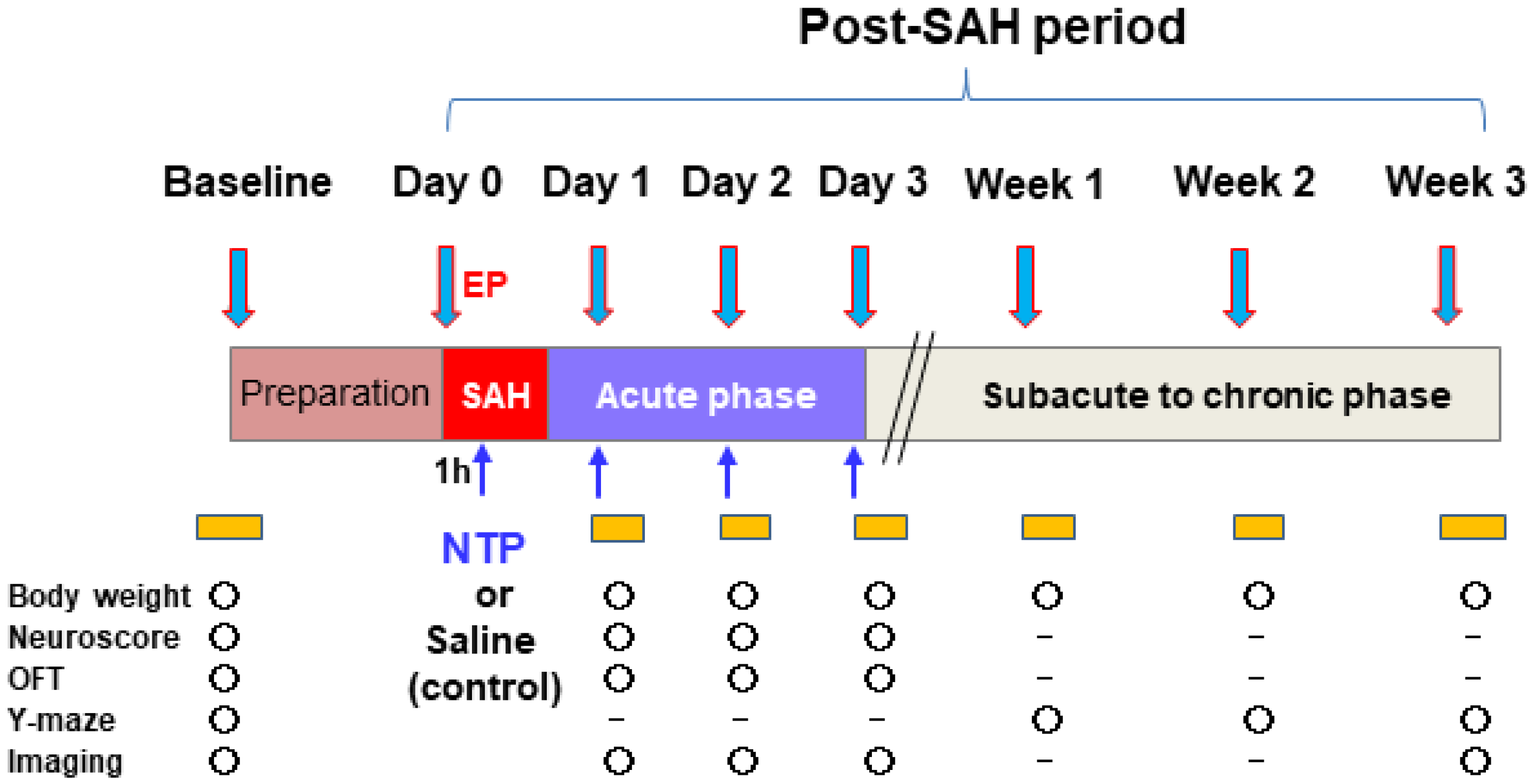
2.1. Study Design and Animals
2.2. Experimental SAH Model
2.3. MRI Data Acquisition
2.4. Hemodynamic Measurements
2.5. Neurological and Locomotive Function Tests
2.6. Experimental Protocols
2.7. Statistical Analysis
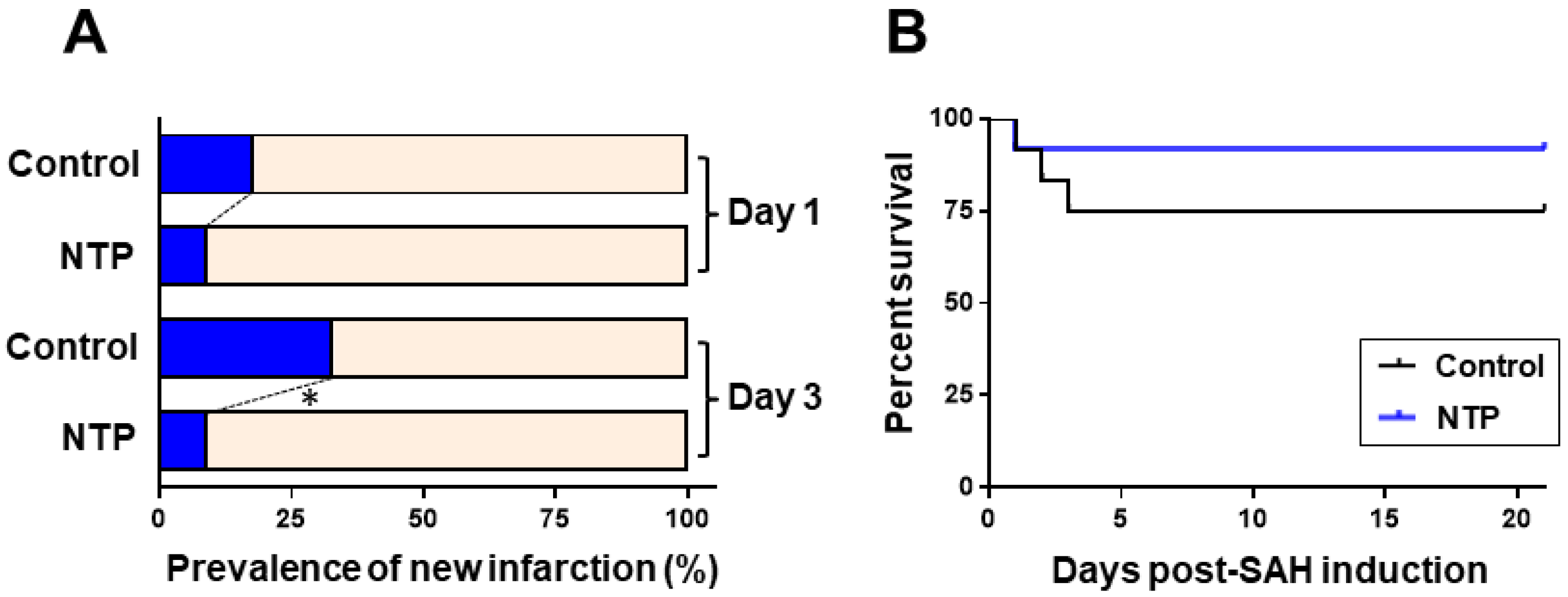
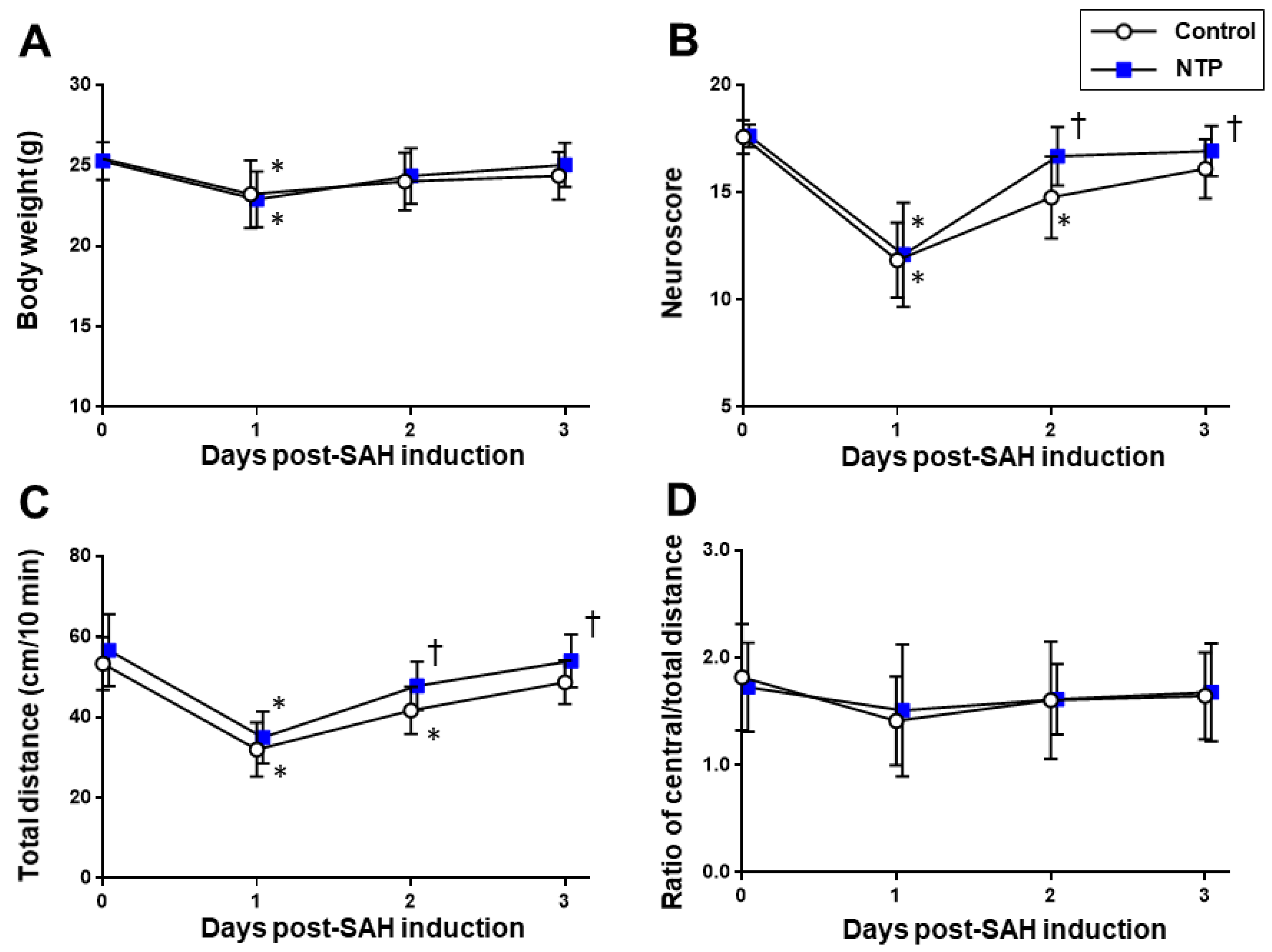
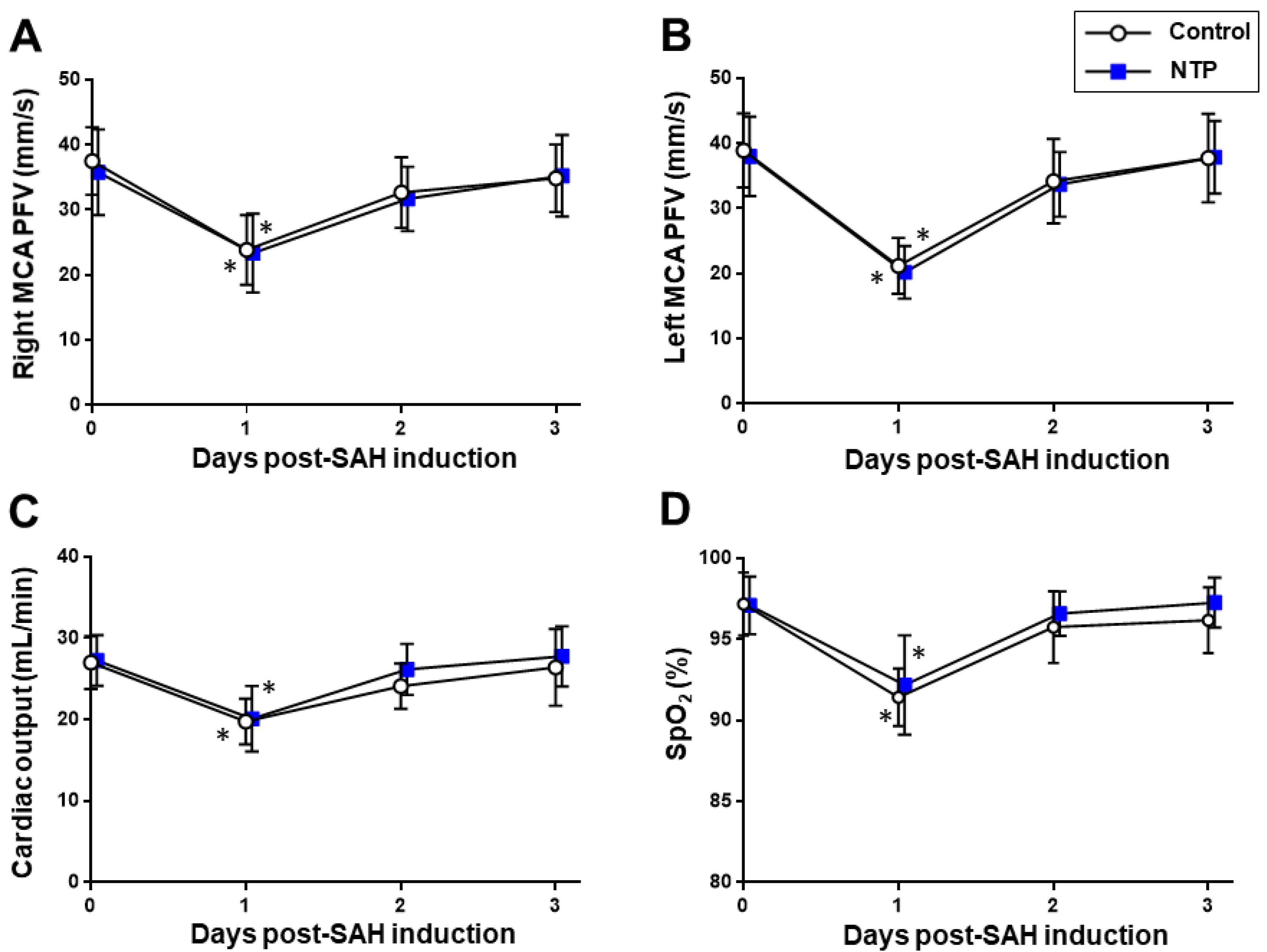
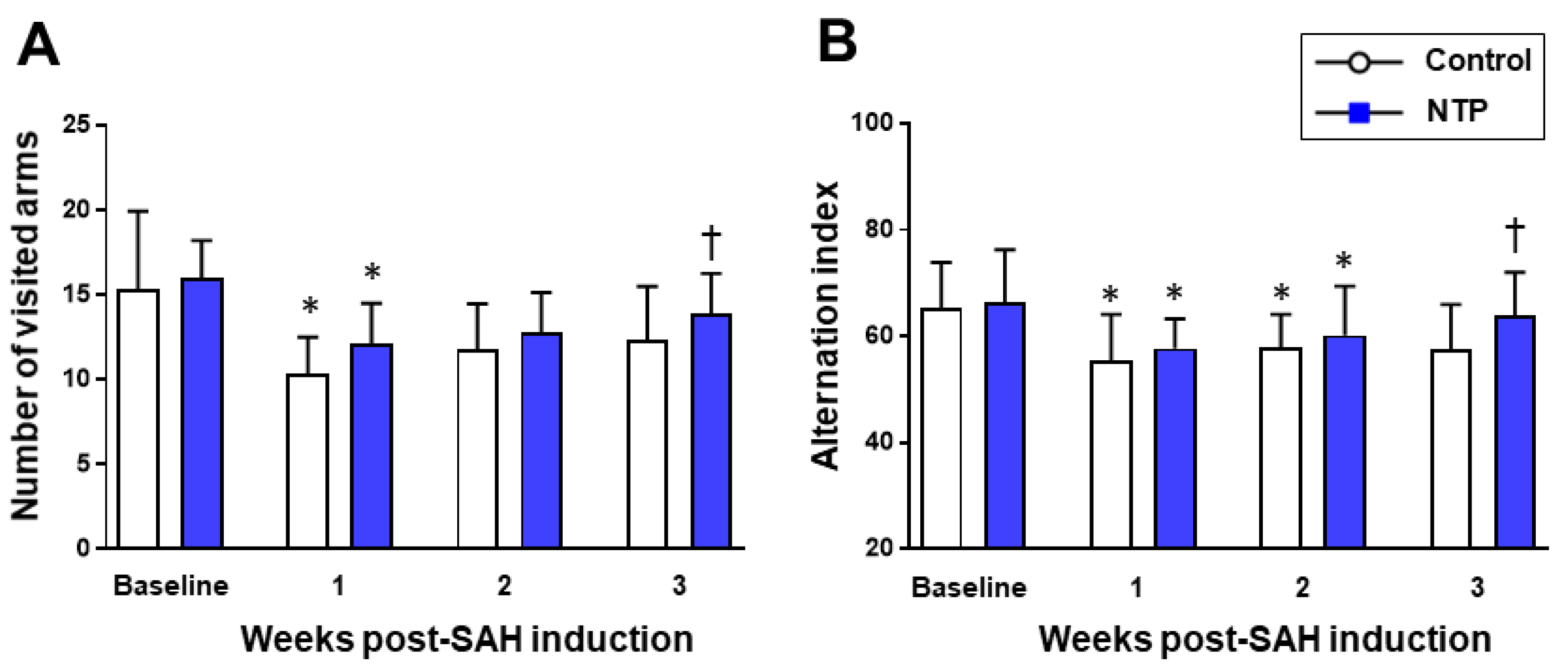
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Suarez, J.I.; Tarr, R.W.; Selman, W.R. Aneurysmal Subarachnoid Hemorrhage. N. Engl. J. Med. 2006, 354, 387–396. [Google Scholar] [CrossRef]
- Zhang, J.H. Vascular neural network in subarachnoid hemorrhage. Transl. Stroke Res. 2014, 5, 423–428. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Plesnila, N. Pathophysiological Role of Global Cerebral Ischemia following Subarachnoid Hemorrhage: The Current Experimental Evidence. Stroke Res. Treat. 2013, 2013, 1–7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Macdonald, R.L. Delayed neurological deterioration after subarachnoid haemorrhage. Nat. Rev. Neurol. 2014, 10, 44–58. [Google Scholar] [CrossRef] [PubMed]
- Aonuma, S.; Kohama, Y.; Yashiki, S.; Chen, I.-J.; Egawa, H.; Ohnishi, N. Studies on biologically Active Substances from Rabbit Skin Tissues infected with Vaccinia virus.-Isolation and Properties of Inhibitor to Gastric Acid Secretion. Yakugaku Zasshi 1976, 96, 1247–1254. [Google Scholar] [CrossRef] [Green Version]
- Hata, T.; Kita, T.; Itoh, E.; Oyama, R.; Kawabata, A. Mechanism of the Analgesic Effect of Neurotropin. Jpn. J. Pharmacol. 1988, 48, 165–173. [Google Scholar] [CrossRef] [Green Version]
- Yamazaki, Y.; Kobatake, K. Successful treatment of nummular headache with Neurotropin®. J. Headache Pain 2011, 12, 661–662. [Google Scholar] [CrossRef] [Green Version]
- Ukai, K.; Sakakura, Y.; Baba, S.; Usami, A.; Takimoto, I.; Nishimura, T. Effect of specific desensitization therapy in combination with an immunopotentiator, Neurotropin, on perennial nasal allergy--with special reference to mite specific IgG and IgG4 antibody levels. Arerugi 1990, 39, 1437–1447. [Google Scholar]
- De Reuck, J.; Decoo, D.; Boon, P.; Van Der Linden, C. Neurotropin Treatment of Brain Edema Accompanying Acute Middle Cerebral Artery Infarction. Brain Edema IX 1994, 60, 332–334. [Google Scholar]
- De Reuck, J.; Decoo, D.; Vanderdonckt, P.; Dallenga, A.; Ceusters, W.; Kalala, J.P.; De Meulemeester, K.; Abdullah, J.; Santens, P.; Huybrechts, J.; et al. A double-blind study of neurotropin in patients with acute ischemic stroke. Acta Neurol. Scand. 2009, 89, 329–335. [Google Scholar] [CrossRef]
- Nakajo, Y.; Yang, D.; Takahashi, J.C.; Zhao, Q.; Kataoka, H.; Yanamoto, H. ERV enhances spatial learning and prevents the development of infarcts, accompanied by upregulated BDNF in the cortex. Brain Res. 2015, 1610, 110–123. [Google Scholar] [CrossRef]
- Hishiyama, S.; Kotoda, M.; Ishiyama, T.; Mitsui, K.; Matsukawa, T. Neuroprotective effects of neurotropin in a mouse model of hypoxic–ischemic brain injury. J. Anesth. 2019, 33, 495–500. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, T.; Li, Y.H.; Mashimo, T. The Antiallodynic and Antihyperalgesic Effects of Neurotropin?? in Mice with Spinal Nerve Ligation. Anesth. Analg. 2005, 101, 793–799. [Google Scholar] [CrossRef] [PubMed]
- Kudo, T.; Kushikata, T.; Kudo, M.; Kudo, T.; Hirota, K. Antinociceptive effects of neurotropin in a rat model of central neuropathic pain: DSP-4 induced noradrenergic lesion. Neurosci. Lett. 2011, 503, 20–22. [Google Scholar] [CrossRef] [PubMed]
- Kawai, H.; Asaoka, N.; Miyake, T.; Nagayasu, K.; Nakagawa, T.; Shirakawa, H.; Kaneko, S. Neurotropin inhibits neuronal activity through potentiation of sustained Kv currents in primary cultured DRG neurons. J. Pharmacol. Sci. 2018, 137, 313–316. [Google Scholar] [CrossRef]
- Okazaki, R.; Namba, H.; Yoshida, H.; Okai, H.; Miura, T.; Kawamura, M. The Antiallodynic Effect of Neurotropin® Is Mediated via Activation of Descending Pain Inhibitory Systems in Rats with Spinal Nerve Ligation. Anesthesia Analg. 2008, 107, 1064–1069. [Google Scholar] [CrossRef]
- Fang, W.; Zhao, D.; Wang, F.; Li, M.; Fan, S.; Liao, W.; Zheng, Y.; Liao, S.-W.; Xiao, S.; Luan, P.; et al. Neurotropin® alleviates hippocampal neuron damage through a HIF-1α/MAPK pathway. CNS Neurosci. Ther. 2017, 23, 428–437. [Google Scholar] [CrossRef]
- Yamamoto, S.; Mutoh, T.; Sasaki, K.; Mutoh, T.; Tatewaki, Y.; Taki, Y. Non-invasive three-dimensional power Doppler imaging for the assessment of acute cerebral blood flow alteration in a mouse model of subarachnoid haemorrhage. Clin. Exp. Pharmacol. Physiol. 2019, 46, 99–102. [Google Scholar] [CrossRef] [Green Version]
- Yamamoto, S.; Mutoh, T.; Sasaki, K.; Mutoh, T.; Taki, Y. Central action of rapamycin on early ischemic injury and related cardiac depression following experimental subarachnoid hemorrhage. Brain Res. Bull. 2019, 144, 85–91. [Google Scholar] [CrossRef]
- Mutoh, T.; Mutoh, T.; Sasaki, K.; Nakamura, K.; Taki, Y.; Ishikawa, T. Value of Three-Dimensional Maximum Intensity Projection Display to Assist in Magnetic Resonance Imaging (MRI)-Based Grading in a Mouse Model of Subarachnoid Hemorrhage. Med. Sci. Monit. 2016, 22, 2050–2055. [Google Scholar] [CrossRef] [Green Version]
- Sasaki, K.; Yamamoto, S.; Mutoh, T.; Tsuru, Y.; Taki, Y.; Kawashima, R. Rapamycin protects against early brain injury independent of cerebral blood flow changes in a mouse model of subarachnoid haemorrhage. Clin. Exp. Pharmacol. Physiol. 2018, 45, 859–862. [Google Scholar] [CrossRef]
- Mutoh, T.; Sasaki, K.; Tatewaki, Y.; Kunitoki, K.; Takano, Y.; Taki, Y. Preceding functional tooth loss delays recovery from acute cerebral hypoxia and locomotor hypoactivity after murine subarachnoid haemorrhage. Clin. Exp. Pharmacol. Physiol. 2018, 45, 344–348. [Google Scholar] [CrossRef]
- Mutoh, T.; Mutoh, T.; Sasaki, K.; Nakamura, K.; Tatewaki, Y.; Ishikawa, T.; Taki, Y. Neurocardiac protection with milrinone for restoring acute cerebral hypoperfusion and delayed ischemic injury after experimental subarachnoid hemorrhage. Neurosci. Lett. 2017, 640, 70–75. [Google Scholar] [CrossRef] [PubMed]
- Mutoh, T.; Mutoh, T.; Nakamura, K.; Yamamoto, Y.; Tsuru, Y.; Tsubone, H.; Ishikawa, T.; Taki, Y. Acute cardiac support with intravenous milrinone promotes recovery from early brain injury in a murine model of severe subarachnoid haemorrhage. Clin. Exp. Pharmacol. Physiol. 2017, 44, 463–469. [Google Scholar] [CrossRef] [PubMed]
- Mutoh, T.; Mutoh, T.; Sasaki, K.; Yamamoto, Y.; Tsuru, Y.; Tsubone, H.; Ishikawa, T.; Taki, Y. Isoflurane postconditioning with cardiac support promotes recovery from early brain injury in mice after severe subarachnoid hemorrhage. Life Sci. 2016, 153, 35–40. [Google Scholar] [CrossRef]
- Altay, O.; Suzuki, H.; Hasegawa, Y.; Caner, B.; Krafft, P.R.; Fujii, M.; Tang, J.; Zhang, J.H. Isoflurane Attenuates Blood–Brain Barrier Disruption in Ipsilateral Hemisphere After Subarachnoid Hemorrhage in Mice. Stroke 2012, 43, 2513–2516. [Google Scholar] [CrossRef] [Green Version]
- Szentes, N.; Tékus, V.; Mohos, V.; Borbély, É.; Helyes, Z. Exploratory and locomotor activity, learning and memory functions in somatostatin receptor subtype 4 gene-deficient mice in relation to aging and sex. GeroScience 2019, 41, 631–641. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nishiyama, T.; Matsukawa, T.; Yamashita, K. Comparison between neurotropin and mepivacaine for stellate ganglion injection. J. Anesth. 2006, 20, 240–242. [Google Scholar] [CrossRef]
- Sasaki, K.; Mutoh, T.; Nakamura, K.; Kojima, I.; Taki, Y.; Suarez, J.I.; Ishikawa, T. MRI-based in vivo assessment of early cerebral infarction in a mouse filament perforation model of subarachnoid hemorrhage. Neurosci. Lett. 2017, 653, 173–176. [Google Scholar] [CrossRef]
- Frontera, J.A.; Claassen, J.; Schmidt, J.M.; Wartenberg, K.E.; Temes, R.; Connolly, E.S.; Macdonald, R.L.; Mayer, S.A. Prediction of Symptomatic Vasospasmafter Subarachnoid Hemorrhage: The Modified Fisher Scale. Neurosurgery 2006, 59, 21–27. [Google Scholar] [CrossRef] [Green Version]
- Fukuda, Y.; Berry, T.L.; Nelson, M.; Hunter, C.L.; Fukuhara, K.; Imai, H.; Ito, S.; Granholm-Bentley, A.-C.; Kaplan, A.P.; Mutoh, T. Stimulated neuronal expression of brain-derived neurotrophic factor by Neurotropin. Mol. Cell. Neurosci. 2010, 45, 226–233. [Google Scholar] [CrossRef]
- Rhein, M.; Schwarzer, A.; Yang, M.; Kaever, V.; Brugman, M.; Meyer, J.; Ganser, A.; Baum, C.; Li, Z. Leukemias induced by altered TRK-signaling are sensitive to mTOR inhibitors in preclinical models. Ann. Hematol. 2010, 90, 283–292. [Google Scholar] [CrossRef]
- Yao, X.; Sun, C.; Fan, B.; Zhao, C.; Zhang, Y.; Duan, H.; Pang, Y.; Shen, W.; Li, B.; Wang, X.; et al. Neurotropin exerts neuroprotective effects after spinal cord injury by inhibiting apoptosis and modulating cytokines. J. Orthop. Transl. 2021, 26, 74–83. [Google Scholar] [CrossRef]
- Fukuda, Y.; Nakajima, K.; Mutoh, T. Neuroprotection by Neurotropin through Crosstalk of Neurotrophic and Innate Immune Receptors in PC12 Cells. Int. J. Mol. Sci. 2020, 21, 6456. [Google Scholar] [CrossRef] [PubMed]
- Fanizzi, C.; Sauerbeck, A.D.; Gangolli, M.; Zipfel, G.J.; Brody, D.L.; Kummer, T.T. Minimal Long-Term Neurobehavioral Impairments after Endovascular Perforation Subarachnoid Hemorrhage in Mice. Sci. Rep. 2017, 7, 1–13. [Google Scholar] [CrossRef] [Green Version]
- Ishikawa, T.; Yasuda, S.; Minoda, S.; Ibuki, T.; Fukuhara, K.; Iwanaga, Y.; Ariyoshi, T.; Sasaki, H. Neurotropin® Ameliorates Chronic Pain via Induction of Brain-Derived Neurotrophic Factor. Cell. Mol. Neurobiol. 2015, 35, 231–241. [Google Scholar] [CrossRef] [PubMed]
- Giacobbo, B.L.; Doorduin, J.; Klein, H.C.; Dierckx, R.A.J.O.; Bromberg, E.; de Vries, E.F.J. Brain-Derived Neurotrophic Factor in Brain Disorders: Focus on Neuroinflammation. Mol. Neurobiol. 2018, 56, 3295–3312. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fang, W.; Liao, W.; Zheng, Y.; Huang, X.; Weng, X.; Fan, S.; Chen, X.; Zhang, X.; Chen, J.; Xiao, S.; et al. Neurotropin reduces memory impairment and neuroinflammation via BDNF/NF-κB in a transgenic mouse model of Alzheimer’s disease. Am. J. Transl. Res. 2019, 11, 1541–1554. [Google Scholar] [PubMed]
- Zheng, Y.; Fang, W.; Fan, S.; Liao, W.; Xiong, Y.; Liao, S.; Li, Y.; Xiao, S.; Liu, J. Neurotropin inhibits neuroinflammation via suppressing NF-κB and MAPKs signaling pathways in lipopolysaccharide-stimulated BV2 cells. J. Pharmacol. Sci. 2018, 136, 242–248. [Google Scholar] [CrossRef]
- Odagiri, Y.; Uchida, H.; Hosokawa, M.; Takemoto, K.; Morley, A.A.; Takeda, T. Accelerated accumulation of somatic mutations in the senescence-accelerated mouse. Nat. Genet. 1998, 19, 116–117. [Google Scholar] [CrossRef]
- Shoji, H.; Miyakawa, T. Age-related behavioral changes from young to old age in male mice of a C57 BL /6J strain maintained under a genetic stability program. Neuropsychopharmacol. Rep. 2019, 39, 100–118. [Google Scholar] [CrossRef] [PubMed]
- Ackert-Bicknell, C.L.; Anderson, L.C.; Sheehan, S.; Hill, W.; Chang, B.; Churchill, G.A.; Chesler, E.J.; Korstanje, R.; Peters, L.L. Aging Research Using Mouse Models. Curr. Protoc. Mouse Biol. 2015, 5, 95–133. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mutoh, T.; Kazumata, K.; Terasaka, S.; Taki, Y.; Suzuki, A.; Ishikawa, T. Early Intensive Versus Minimally Invasive Approach to Postoperative Hemodynamic Management After Subarachnoid Hemorrhage. Stroke 2014, 45, 1280–1284. [Google Scholar] [CrossRef] [PubMed] [Green Version]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mutoh, T.; Yamamoto, S.; Moriya, T. Post-Event Application of Neurotropin Protects against Ischemic Insult toward Better Outcomes in a Murine Model of Subarachnoid Hemorrhage. Biomedicines 2021, 9, 664. https://doi.org/10.3390/biomedicines9060664
Mutoh T, Yamamoto S, Moriya T. Post-Event Application of Neurotropin Protects against Ischemic Insult toward Better Outcomes in a Murine Model of Subarachnoid Hemorrhage. Biomedicines. 2021; 9(6):664. https://doi.org/10.3390/biomedicines9060664
Chicago/Turabian StyleMutoh, Tatsushi, Shuzo Yamamoto, and Takahiro Moriya. 2021. "Post-Event Application of Neurotropin Protects against Ischemic Insult toward Better Outcomes in a Murine Model of Subarachnoid Hemorrhage" Biomedicines 9, no. 6: 664. https://doi.org/10.3390/biomedicines9060664






