Development and Evaluation of a Virtual Model for Fetal Alcohol Spectrum Disorder (FASD) Assessment and Diagnosis in Children: A Pilot Study
Abstract
:1. Introduction
2. Methods
3. Results
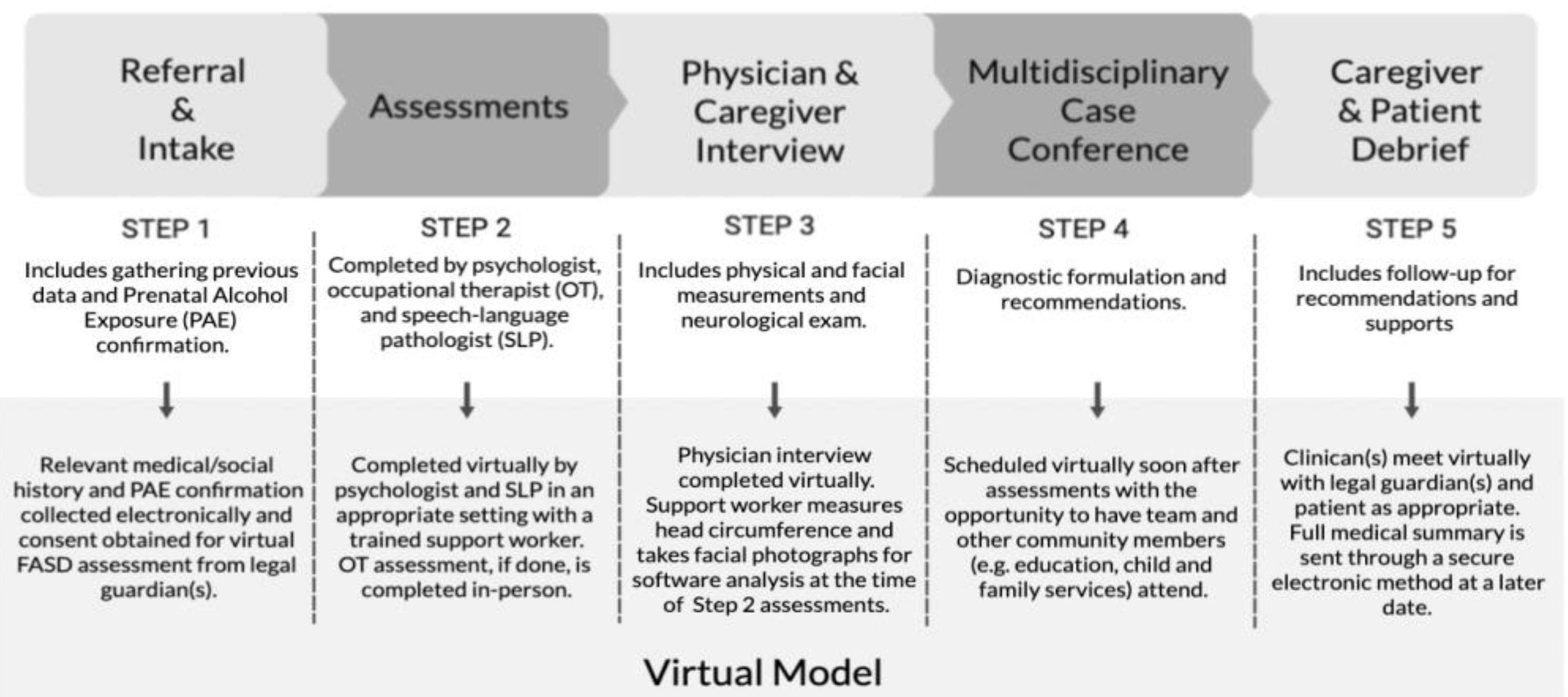
3.1. Development of a Virtual Model
3.1.1. In-Person FASD Diagnosis and Assessment Model
3.1.2. Virtual Assessments
3.1.3. Other Considerations of Using the Virtual Model
3.1.4. Moving from an In-Person to Virtual Diagnostic Process
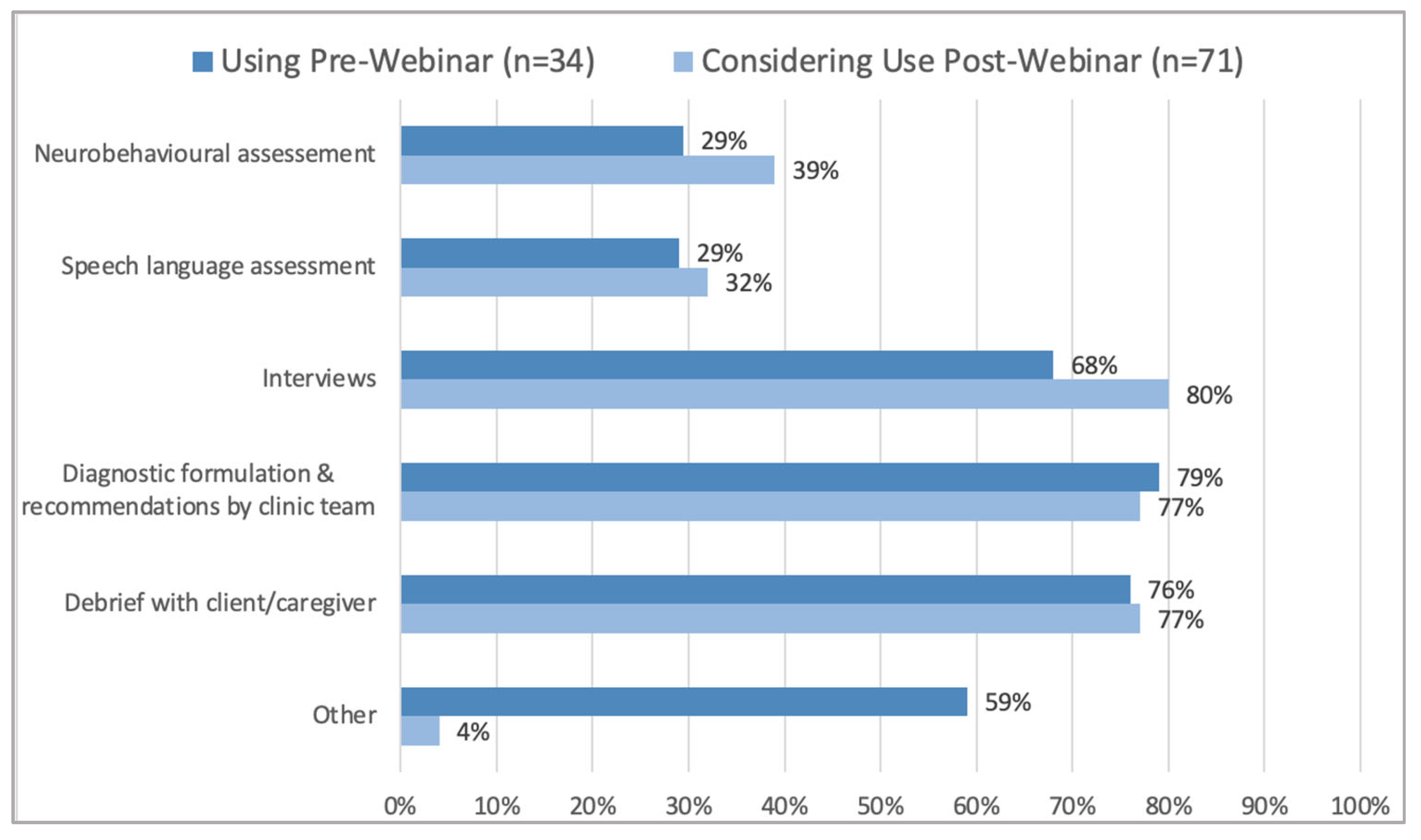
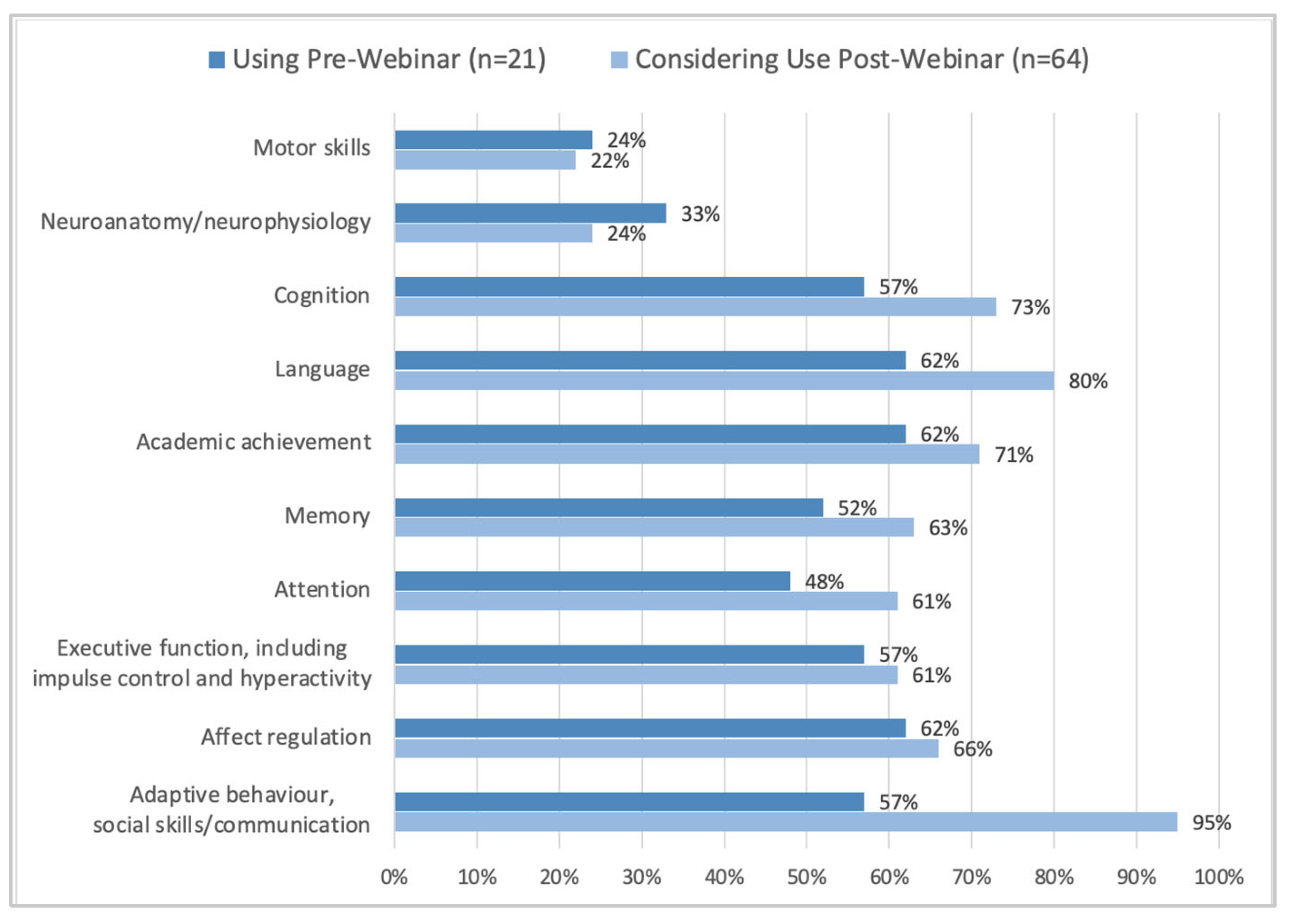
3.2. Evaluation of the Model
FASD Assessment and Diagnostic Teams
3.3. Caregiver Experiences
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
Speech Language Tests
Appendix B
Psychologist Tools
References
- Shaw, J.; Jamieson, T.; Agarwal, P.; Griffin, B.; Wong, I.; Bhatia, R.S. Virtual care policy recommendations for patient-centred primary care: Findings of a consensus policy dialogue using a nominal group technique. J. Telemed. Telecare 2017, 24, 608–615. [Google Scholar] [CrossRef] [PubMed]
- Tenforde, A.S.; Hefner, J.E.; Kodish-Wachs, J.E.; Iaccarino, M.A.; Paganoni, S. Telehealth in Physical Medicine and Rehabilitation: A Narrative Review. PM&R 2017, 9 (Suppl. S5), S51–S58. [Google Scholar] [CrossRef]
- Drago, A.; Winding, T.; Antypa, N. Videoconferencing in psychiatry, a meta-analysis of assessment and treatment. Eur. Psychiatry 2016, 36, 29–37. [Google Scholar] [CrossRef] [PubMed]
- Juárez, A.P.; Weitlauf, A.S.; Nicholson, A.; Pasternak, A.; Broderick, N.; Hine, J.; Stainbrook, J.A.; Warren, Z. Early Identification of ASD Through Telemedicine: Potential Value for Underserved Populations. J. Autism Dev. Disord. 2018, 48, 2601–2610. [Google Scholar] [CrossRef] [PubMed]
- Stainbrook, J.A.; Weitlauf, A.S.; Juárez, A.P.; Taylor, J.L.; Hine, J.; Broderick, N.; Nicholson, A.; Warren, Z. Measuring the service system impact of a novel telediagnostic service program for young children with autism spectrum disorder. Autism 2018, 23, 1051–1056. [Google Scholar] [CrossRef]
- Badawy, S.M.; Radovic, A. Digital Approaches to Remote Pediatric Health Care Delivery During the COVID-19 Pandemic: Existing Evidence and a Call for Further Research. JMIR Pediatr. Parent. 2020, 3, e20049. [Google Scholar] [CrossRef]
- Census of Canada. 2016 Census of Canada Population and Dwelling Release. 2017. Available online: https://open.alberta.ca/dataset/7d02c106-a55a-4f88-8253-4b4c81168e9f/resource/e435dd59-2dbd-4bf2-b5b6-3173d9bd6c39/download/2016-census-population-and-dwelling-counts.pdf (accessed on 2 May 2022).
- Marcin, J.; Shaikh, U.; Steinhorn, R.H. Addressing health disparities in rural communities using telehealth. Pediatr. Res. 2015, 79, 169–176. [Google Scholar] [CrossRef]
- Chudley, A.E.; Conry, J.; Cook, J.L.; Loock, C.; Rosales, T.; LeBlanc, N. Fetal alcohol spectrum disorder: Canadian guidelines for diagnosis. CMAJ. 2005, 172 (suppl. S5), S1–S21. [Google Scholar] [CrossRef] [Green Version]
- FASD Alberta. FASD Alberta Networks. Available online: https://fasdalberta.ca/ (accessed on 14 April 2022).
- Cook, J.L.; Green, C.R.; Lilley, C.M.; Anderson, S.M.; Baldwin, M.E.; Chudley, A.E.; Conry, J.L.; LeBlanc, N.; Loock, C.A.; Lutke, J.; et al. Fetal alcohol spectrum disorder: A guideline for diagnosis across the lifespan. CMAJ. 2015, 188, 191–197. [Google Scholar] [CrossRef] [Green Version]
- Whittingham, L.M.; Coons-Harding, K.D. Connecting People with People: Diagnosing Persons with Fetal Alcohol Spectrum Disorder Using Telehealth. J. Autism Dev. Disord. 2021, 51, 1067–1080. [Google Scholar] [CrossRef]
- Katzenellenbogen, R. HEADSS: The “Review of Systems” for Adolescents. The Virtual Mentor. 2005, 7, 231–233. [Google Scholar] [CrossRef]
- Astley, S.J.; Clarren, S.K. Measuring the facial phenotype of individuals with prenatal alcohol exposure: Correlations with brain dysfunction. Alcohol Alcohol. 2001, 36, 147–159. [Google Scholar] [CrossRef] [Green Version]
- Pradhan, T.; Six-Workman, E.A.; Law, K.-B. An Innovative Approach to Care: Integrating Mental Health Services Through Telemedicine in Rural School-Based Health Centers. Psychiatr. Serv. 2019, 70, 239–242. [Google Scholar] [CrossRef]
- Benoit, T.; Bowes, C.; Bowman, N.; Cantin, D.; Chudley, A.; Crolly, D.; Livingston, A.; Longstaffe, S.; Marles, S.; Miller, C.; et al. Telemedicine diagnosis for fetal alcohol syndrome—The Manitoba experience. Paediatr. Child Health 2002, 7, 147–151. [Google Scholar] [CrossRef] [Green Version]
- Ens, C.D.; Hanlon-Dearman, A.; Millar, M.C.; Longstaffe, S. Using Telehealth for Assessment of Fetal Alcohol Spectrum Disorder: The Experience of Two Canadian Rural and Remote Communities. Telemed. e-Health 2010, 16, 872–877. [Google Scholar] [CrossRef]
- Hanlon-Dearman, A.; Edwards, C.; Schwab, D.; Millar, M.C.; Longstaffe, S. “Giving Voice”: Evaluation of an Integrated Telehealth Community Care Model by Parents/Guardians of Children Diagnosed with Fetal Alcohol Spectrum Disorder in Manitoba. Telemed. e-Health 2014, 20, 478–484. [Google Scholar] [CrossRef]
- Sutherland, R.; Trembath, D.; Hodge, A.; Drevensek, S.; Lee, S.; Silove, N.; Roberts, J. Telehealth language assessments using consumer grade equipment in rural and urban settings: Feasible, reliable and well tolerated. J. Telemed. Telecare 2017, 23, 106–115. [Google Scholar] [CrossRef]
- Monique, C.W.; Deborah, G.T.; Trevor, G.R.; Louise, M.C. Internet-Based Telehealth Assessment of Language Using the CELF–4. Lang. Speech Hear. Serv. Sch. 2010, 41, 445–458. [Google Scholar] [CrossRef]
- Eriks-Brophy, A.; Quittenbaum, J.; Anderson, D.; Nelson, T. Part of the problem or part of the solution? Communication assessments of Aboriginal children residing in remote communities using videoconferencing. Clin. Linguist. Phon. 2008, 22, 589–609. [Google Scholar] [CrossRef]
- Lucas, B.R.; Doney, R.; Latimer, J.; Watkins, R.E.; Tsang, T.W.; Hawkes, G.; Fitzpatrick, J.P.; Oscar, J.; Carter, M.; Elliott, E.J. Impairment of motor skills in children with fetal alcohol spectrum disorders in remote Australia: The Lililwan Project. Drug Alcohol Rev. 2016, 35, 719–727. [Google Scholar] [CrossRef]
- Nal, G.; Güney, G.; Gün, F.; Huri, M. Telehealth in paediatric occupational therapy: A scoping review. Int. J. Ther. Rehabil. 2021, 28, 1–16. [Google Scholar] [CrossRef]
- Hen-Herbst, L.; Jirikowic, T.; Hsu, L.-Y.; McCoy, S.W. Motor performance and sensory processing behaviors among children with fetal alcohol spectrum disorders compared to children with developmental coordination disorders. Res. Dev. Disabil. 2020, 103, 103680. [Google Scholar] [CrossRef] [PubMed]
- Henderson, S.E.; Sugden, D.; Barnett, A.L. Movement Assessment Battery for Children-2. Res. Dev. Disabil. 1992. [Google Scholar] [CrossRef]
- Johnston, D.; Branton, E.; Rasmuson, L.; Schell, S.; Gross, D.P.; Pritchard-Wiart, L. Accuracy of motor assessment in the diagnosis of fetal alcohol spectrum disorder. BMC Pediatr. 2019, 19, 171. [Google Scholar] [CrossRef] [PubMed]
- Temple, V.; Drummond, C.; Valiquette, S.; Jozsvai, E. A comparison of intellectual assessments over video conferencing and in-person for individuals with ID: Preliminary data. J. Intellect. Disabil. Res. 2010, 54, 573–577. [Google Scholar] [CrossRef] [PubMed]
- Hodge, M.A.; Sutherland, R.; Jeng, K.; Bale, G.; Batta, P.; Cambridge, A.; Detheridge, J.; Drevensek, S.; Edwards, L.; Everett, M.; et al. Agreement between telehealth and face-to-face assessment of intellectual ability in children with specific learning disorder. J. Telemed. Telecare 2018, 25, 431–437. [Google Scholar] [CrossRef]
- Munro Cullum, C.; Hynan, L.S.; Grosch, M.; Parikh, M.; Weiner, M.F. Teleneuropsychology: Evidence for video teleconference-based neuropsychological assessment. J. Int. Neuropsychol. Soc. 2014, 20, 1028–1033. [Google Scholar] [CrossRef]
- Fitzpatrick, J.P.; Latimer, J.; Olson, H.C.; Carter, M.; Oscar, J.; Lucas, B.R.; Doney, R.; Salter, C.; Try, J.; Hawkes, G.; et al. Prevalence and profile of Neurodevelopment and Fetal Alcohol Spectrum Disorder (FASD) amongst Australian Aboriginal children living in remote communities. Res. Dev. Disabil. 2017, 65, 114–126. [Google Scholar] [CrossRef]
- Canada Health Infoway. Telehealth Benefits and Adoption: Connecting People and Providers. 2011. Available online: https://www.infoway-inforoute.ca/en/component/edocman/resources/reports/333-telehealth-benefits-and-adoption-connecting-people-and-providers-full (accessed on 15 January 2023).
- Kruse, C.S.; Krowski, N.; Rodriguez, B.; Tran, L.; Vela, J.; Brooks, M. Telehealth and patient satisfaction: A systematic review and narrative analysis. BMJ Open 2017, 7, e016242. [Google Scholar] [CrossRef]
- Orlando, J.F.; Beard, M.; Kumar, S. Systematic review of patient and caregivers’ satisfaction with telehealth videoconferencing as a mode of service delivery in managing patients’ health. PLoS ONE 2019, 14, e0221848. [Google Scholar] [CrossRef]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
King, S.; Burns, C.; Symes, B.; Jessiman, S.; Bell, A.; Rajani, H. Development and Evaluation of a Virtual Model for Fetal Alcohol Spectrum Disorder (FASD) Assessment and Diagnosis in Children: A Pilot Study. Children 2023, 10, 196. https://doi.org/10.3390/children10020196
King S, Burns C, Symes B, Jessiman S, Bell A, Rajani H. Development and Evaluation of a Virtual Model for Fetal Alcohol Spectrum Disorder (FASD) Assessment and Diagnosis in Children: A Pilot Study. Children. 2023; 10(2):196. https://doi.org/10.3390/children10020196
Chicago/Turabian StyleKing, Seema, Colleen Burns, Brent Symes, ShawnaLee Jessiman, Amber Bell, and Hasu Rajani. 2023. "Development and Evaluation of a Virtual Model for Fetal Alcohol Spectrum Disorder (FASD) Assessment and Diagnosis in Children: A Pilot Study" Children 10, no. 2: 196. https://doi.org/10.3390/children10020196
APA StyleKing, S., Burns, C., Symes, B., Jessiman, S., Bell, A., & Rajani, H. (2023). Development and Evaluation of a Virtual Model for Fetal Alcohol Spectrum Disorder (FASD) Assessment and Diagnosis in Children: A Pilot Study. Children, 10(2), 196. https://doi.org/10.3390/children10020196





