Cardiovascular Magnetic Resonance from Fetal to Adult Life—Indications and Challenges: A State-of-the-Art Review
Abstract
:1. Introduction
2. Role of Cardiovascular Magnetic Resonance during Fetal Life
2.1. Background
2.2. Overview of the Principal Sequences Used during Fetal CMR Scans
2.3. Fetal CMR Applications in the Clinical Scenario
2.4. Current Limitations
3. Role of Cardiovascular Magnetic Resonance during Childhood
3.1. Introduction
3.2. Imaging Modalities in Childhood
3.3. Indications
3.4. Sequences Used in Paediatric CMR
- a.
- Spin-echo or “black-blood” sequences (BB SE): blood appears dark whereas tissues are in shades of grey. These sequences are less susceptible to turbulent flow or metallic artefacts. Respiratory motion is controlled by breath-holding and multiple averages. Recommended for: anatomy definition, stents, complex CHDs [48,49].
- b.
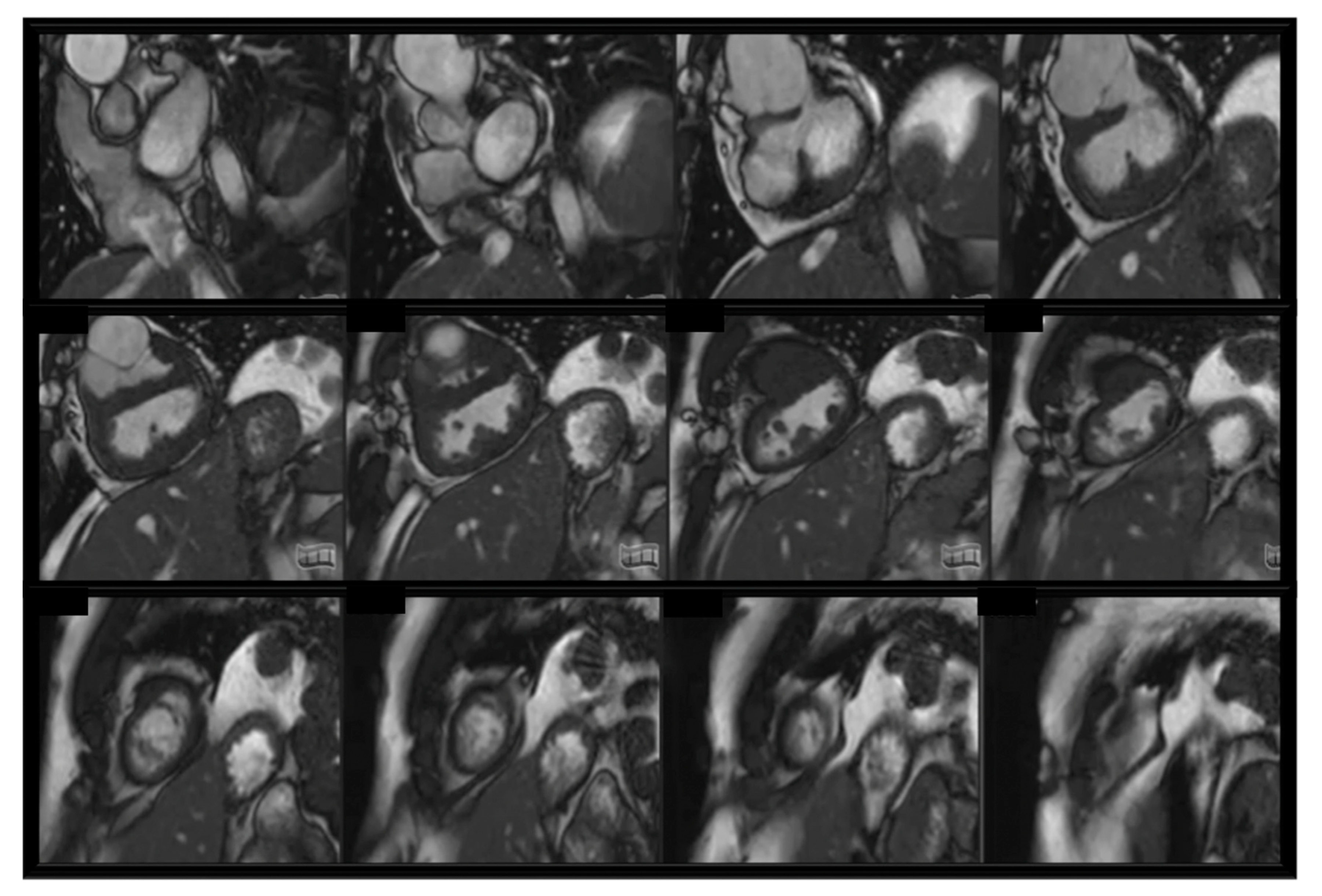
- Steady-state free precession sequences (SSFP): blood appears bright. Two-dimensional (2D) SSFP is the most frequent sequence to assess anatomy, function, and valve motion in CHDs. SSFP cine slices stuck are usually used to assess ventricular volumes and ejection fraction. Cardiac motion controlled by retrospective ECG-gating. Recommended for: baseline heart assessment and CHDs including single ventricles [48]; see Figure 1.
- c.
- Contrast-enhanced magnetic resonance angiography (CE-MRA): gadolinium-based contrast administration increases the contrast between blood pool and surrounding tissue. Breath-holding and high spatial resolution sequences. No ECG-trigger, images reconstruction on average cardiac cycle. Recommended for: vessel anatomy assessment (aortic arch, pulmonary arteries and veins, collateral vessels) [50].
- d.
- Three-dimensional (3D) SSFP sequences: both ECG and respiratory gating (through diaphragmatic navigator) compensates respiratory motion. Contrast medium can be administered. High resolution 3D dataset of whole heart and intrathoracic vasculature. Recommended for: complex CHDs, proximal coronaries anatomy, visualisation of vessels anatomy. Limitation in case of low-pressure flow and stent [51,52,53].
- e.
- Velocity-encoded phase-contrast (PC) cine sequences: blood flow measurement across a vessel. Blood flows comparison is also fundamental to assess complex CHDs physiopathology. Recommended for: shunt assessment, collaterals, assessment of regurgitation or stenosis.
- f.
- Late gadolinium enhancement (LGE) sequences: abnormal deposition of contrast agent within the myocardium late after contrast medium injection. To detect myocardial fibrosis/scar (bright) in the contest of healthy myocardium (dark). Recommended for: cardiomyopathies, ischemic heart disease, myocarditis, CHDs (post- and pre-surgical scars) [48,54,55].
3.5. Clinical Applications of CMR in Childhood
- a.
- Aortic arch anomalies: anatomical assessment for vascular rings, interrupted aortic arch, truncus arteriosus, aortic coarctation, connective tissue disorders (Marfan, Loeys-Dietz, Turner syndrome) [56]. Three-dimensional CE-MRA and SSFP sequences allow decision making for surgery or catheter-guided treatment [45]. Blood flow measurements with PC sequences provide information about vascular narrowing or presence of collaterals;
- b.
- Pulmonary arteries: CMR can provide detailed visualisation of spatial alignment of pulmonary artery bifurcation and side branches, as well as anatomical combined with functional information of aorto-pulmonary collaterals. Through-plane flow measurements can quantify flow distribution in between the lungs [57];
- c.
- Pulmonary veins: CMR is a fundamental tool to assess anomalous connection and stenosis of pulmonary veins. It can combine luminal anatomy (CE-MRA, 3D SSFP), accurate quantification of blood flow patterns (PC sequences) occurring in the presence of pulmonary venous obstruction and aorto-pulmonary collaterals [58];
- d.
- Shunt lesions: CMR is considered the gold standard for flow assessment. CMR can provide non-invasive anatomical detection of intracardiac and extracardiac shunts, flow direction and shunt quantification. Velocity-encoded PC sequences can accurately calculate Qp/Qs [59];
- e.
- Tetralogy of fallot: CMR enables assessment of right ventricular outflow tract (RVOT) and pulmonary arteries, as well as quantification of right ventricle volume and function and pulmonary valve regurgitation. Assessment of pulmonary flow distribution. Scar quantification. Key-imaging for surgical and/or percutaneous treatment decision making and follow up [60];
- f.
- g.
- Single ventricles: CMR provides detailed anatomical, functional and flow assessment throughout palliative stages in single ventricle setting as well as during follow up after completion of the Fontan circulation (Fontan pathway obstruction, baffle leaks, lung flow distribution, thrombus formation and collateral flow) [63]; see Figure 2;
- h.
- Cardiac tumours: CMR represents a non-invasive instrument for tumour size and location, tissue characterisation, relationship and/or infiltration of surrounding structures, vascularisation and haemodynamic relevance [64];
- i.
- Cardiomyopathies: CMR provides non-invasive myocardial tissue characterisation (oedema, scar, replacement, and distribution of fibrosis) as well as global and wall motion abnormalities in idiopathic cardiomyopathy or secondary to neuromuscular disorders. Gold standard for follow up to measure response to treatments as well as family screening [65];
- j.
- Myocarditis: in the acute phase of myocarditis, CMR study is used to assess global ventricular function and regional wall motion abnormalities, early myocardial inflammatory changes (T2-weighted sequences), as well as myocardial necrosis/fibrosis (LGE sequences). In chronic myocarditis, CMR can be used to monitor biventricular function and to demonstrate inflammatory and fibrosis evolution. The LGE sequences typically visualise a patchy with a subepicardial and mid-wall contrast distribution most commonly detected in the lateral and inferior walls of the left ventricle. The presence of pericardial effusion provides supportive evidence for myocarditis [66].
3.6. Limitations
4. Role of Cardiovascular Magnetic Resonance in the Adult Population
4.1. Congenital Heart Disease
4.2. Coronary Artery Disease (CAD)
4.3. Cardiomyopathies
4.4. Pericardial Disease
4.5. Cardiac Masses
4.6. Valvular Heart Disease and Great Vessels Assessment
4.7. CMR during Pregnancy and Breastfeeding
5. Conclusions
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| Arteriovenous | AV |
| Azygous vein | AZY |
| Balanced steady-state free precession “bright blood” sequences | bSSFP |
| Black blood spin-echo | BB SE |
| Cardiovascular | CV |
| Cardiovascular magnetic resonance | CMR |
| Congenital heart disease | CHD |
| Contrast-enhanced magnetic resonance angiography | CE-MRA |
| Coronary artery disease | CAD |
| Coronary computed tomography | CTCA |
| Computerized tomography | CT |
| Contrast-enhanced | CE |
| Dilated cardiomyopathy | DCM |
| Doppler ultrasound | DUS |
| Early gadolinium enhancement | EGE |
| Echo time | TE |
| Electrocardiographic | ECG |
| Extracellular volumes | EV |
| Gadolinium-based contrast agent | GBCA |
| Hepatic Veins | HV |
| Hypertrophic cardiomyopathy | HCM |
| Ischemia and unobstructed coronary arteries | INOCA |
| Inversion time | TI |
| Late gadolinium enhancement | LGE |
| Left pulmonary artery | LPA |
| Left ventricular outflow tract | LVOT |
| Myocardial blood flow | MBF |
| Myocardial infarction | MI |
| Myocardial infarction and non-obstructive coronary arteries | MINOCA |
| Myocardial perfusion reserve | MPR |
| Magnetic resonance angiography | MRA |
| Microvascular obstruction | MVO |
| Optimised gating | MOG |
| Phase-contrast | PC |
| Magnetic resonance imaging | MRI |
| Right Pulmonary Artery | RPA |
| Right ventricular outflow tract | RVOT |
| Single photon emission computed tomography | SPECT |
| Tetralogy of fallot | TOF |
| Total cavopulmonary connection | TCPC |
References
- Leiner, T.; Bogaert, J.; Friedrich, M.G.; Mohiaddin, R.; Muthurangu, V.; Myerson, S.; Powell, A.J.; Raman, S.V.; Pennell, D.J. SCMR Position Paper (2020) on clinical indications for cardiovascular magnetic resonance. J. Cardiovasc. Magn. Reson. 2020, 22, 76. [Google Scholar] [CrossRef]
- Buechel, E.V.; Grosse-Wortmann, L.; Fratz, S.; Eichhorn, J.; Sarikouch, S.; Greil, G.; Beerbaum, P.; Bucciarelli-Ducci, C.; Bonello, B.; Sieverding, L.; et al. Indications for cardiovascular magnetic resonance in children with congenital and acquired heart disease: An expert consensus paper of the Imaging Working Group of the AEPC and the Cardiovascular Magnetic Resonance Section of the EACVI. Eur. Heart J. Cardiovasc. Imaging 2015, 16, 281–297. [Google Scholar] [CrossRef]
- Knapp, J.; de Sousa, M.T.; Schönnagel, B.P. Fetal Cardiovascular MRI—A Systemic Review of the Literature: Challenges, New Technical Developments, and Perspectives. Rofo 2022, 194, 841–851. [Google Scholar] [CrossRef]
- Patenaude, Y.; Pugash, D.; Lim, K.; Morin, L.; Bly, S.; Butt, K.; Cargill, Y.; Davies, G.; Denis, N.; Hazlitt, G.; et al. RETIRED: The Use of Magnetic Resonance Imaging in the Obstetric Patient. J. Obstet. Gynaecol. Can. 2014, 36, 349–355. [Google Scholar] [CrossRef] [PubMed]
- Taylor, A.M. Cardiac imaging: MR or CT? Which to use when. Pediatr. Radiol. 2008, 38, 433–438. [Google Scholar] [CrossRef]
- Wu, K.C.; Zerhouni, E.A.; Judd, R.M.; Lugo-Olivieri, C.H.; Barouch, L.A.; Schulman, S.P.; Blumenthal, R.S.; Lima, J.A.C. Prognostic Significance of Microvascular Obstruction by Magnetic Resonance Imaging in Patients With Acute Myocardial Infarction. Circulation 1998, 97, 765–772. [Google Scholar] [CrossRef]
- Kellman, P.; Hansen, M.S.; Nielles-Vallespin, S.; Nickander, J.; Themudo, R.; Ugander, M.; Xue, H. Myocardial perfusion cardiovascular magnetic resonance: Optimized dual sequence and reconstruction for quantification. J. Cardiovasc. Magn. Reson. 2017, 19, 43. [Google Scholar] [CrossRef] [PubMed]
- Peyvandi, S.; De Santiago, V.; Chakkarapani, E.; Chau, V.; Campbell, A.; Poskitt, K.J.; Xu, D.; Barkovich, A.J.; Miller, S.; McQuillen, P. Association of Prenatal Diagnosis of Critical Congenital Heart Disease With Postnatal Brain Development and the Risk of Brain Injury. JAMA Pediatr. 2016, 170, e154450. [Google Scholar] [CrossRef]
- Holland, B.J.; Myers, J.A.; Woods, C.R. Prenatal diagnosis of critical congenital heart disease reduces risk of death from cardiovascular compromise prior to planned neonatal cardiac surgery: A meta-analysis. Ultrasound Obstet. Gynecol. 2015, 45, 631–638. [Google Scholar] [CrossRef] [PubMed]
- Kovacevic, A.; Simmelbauer, A.; Starystach, S.; Elsässer, M.; Müller, A.; Bär, S.; Gorenflo, M. Counseling for Prenatal Congenital Heart Disease—Recommendations Based on Empirical Assessment of Counseling Success. Front. Pediatr. 2020, 8, 26. [Google Scholar] [CrossRef]
- McElhinney, D.B.; Tworetzky, W.; Lock, J.E. Current Status of Fetal Cardiac Intervention. Circulation 2010, 121, 1256–1263. [Google Scholar] [CrossRef]
- Gholipour, A.; Estroff, J.A.; Barnewolt, C.E.; Robertson, R.L.; Grant, P.E.; Gagoski, B.; Warfield, S.K.; Afacan, O.; Connolly, S.A.; Neil, J.J.; et al. Fetal MRI: A technical update with educational aspirations. Concepts Magn. Reson. Part A 2014, 43, 237–266. [Google Scholar] [CrossRef]
- Roy, C.W.; van Amerom, J.; Marini, D.; Seed, M.; Macgowan, C. Fetal Cardiac MRI: A Review of Technical Advancements. Top Magn Reson Imaging. Top. Magn. Reson. Imaging 2019, 28, 235–244. [Google Scholar] [CrossRef]
- Nacif, M.S.; Zavodni, A.; Kawel, N.; Choi, E.-Y.; Lima, J.A.C.; Bluemke, D.A. Cardiac magnetic resonance imaging and its electrocardiographs (ECG): Tips and tricks. Int. J. Cardiovasc. Imaging 2011, 28, 1465–1475. [Google Scholar] [CrossRef] [PubMed]
- Jansz, M.S.; Seed, M.; van Amerom, J.F.P.; Wong, D.; Grosse-Wortmann, L.; Yoo, S.-J.; Macgowan, C.K. Metric optimized gating for fetal cardiac MRI. Magn. Reson. Med. 2010, 64, 1304–1314. [Google Scholar] [CrossRef]
- Haris, K.; Hedström, E.; Bidhult, S.; Testud, F.; Maglaveras, N.; Heiberg, E.; Hansson, S.R.; Arheden, H.; Aletras, A.H. Self-gated fetal cardiac MRI with tiny golden angle iGRASP: A feasibility study. J. Magn. Reson. Imaging 2017, 46, 207–217. [Google Scholar] [CrossRef]
- Kording, F.; Yamamura, J.; De Sousa, M.T.; Ruprecht, C.; Hedström, E.; Aletras, A.H.; Grant, P.E.; Powell, A.J.; Fehrs, K.; Adam, G.; et al. Dynamic fetal cardiovascular magnetic resonance imaging using Doppler ultrasound gating. J. Cardiovasc. Magn. Reson. 2018, 20, 17. [Google Scholar] [CrossRef]
- Haris, K.; Hedström, E.; Kording, F.; Bidhult, S.; Steding-Ehrenborg, K.; Ruprecht, C.; Heiberg, E.; Arheden, H.; Aletras, A.H. Free-breathing fetal cardiac MRI with doppler ultrasound gating, compressed sensing, and motion compensation. J. Magn. Reson. Imaging 2019, 51, 260–272. [Google Scholar] [CrossRef] [PubMed]
- Roy, C.W.; Seed, M.; Kingdom, J.C.; Macgowan, C.K. Motion compensated cine CMR of the fetal heart using radial undersampling and compressed sensing. J. Cardiovasc. Magn. Reson. 2017, 19, 29. [Google Scholar] [CrossRef] [PubMed]
- Seed, M.; Van Amerom, J.F.P.; Yoo, S.-J.; Al Nafisi, B.; Grosse-Wortmann, L.; Jaeggi, E.; Jansz, M.S.; MacGowan, C.K. Feasibility of quantification of the distribution of blood flow in the normal human fetal circulation using CMR: A cross-sectional study. J. Cardiovasc. Magn. Reson. 2012, 14, 79. [Google Scholar] [CrossRef]
- Ryd, D.; Sun, L.; Steding-Ehrenborg, K.; Bidhult, S.; Kording, F.; Ruprecht, C.; Macgowan, C.K.; Seed, M.; Aletras, A.H.; Arheden, H.; et al. Quantification of blood flow in the fetus with cardiovascular magnetic resonance imaging using Doppler ultrasound gating: Validation against metric optimized gating. J. Cardiovasc. Magn. Reson. 2019, 21, 74. [Google Scholar] [CrossRef]
- Portnoy, S.; Seed, M.; Sled, J.G.; Macgowan, C.K. Non-invasive evaluation of blood oxygen saturation and hematocrit from T1 and T2 relaxation times: In-vitro validation in fetal blood. Magn. Reson. Med. 2017, 78, 2352–2359. [Google Scholar] [CrossRef] [PubMed]
- Sun, L.; MacGowan, C.K.; Portnoy, S.; Sled, J.G.; Yoo, S.-J.; Grosse-Wortmann, L.; Jaeggi, E.; Kingdom, J.; Seed, M. New advances in fetal cardiovascular magnetic resonance imaging for quantifying the distribution of blood flow and oxygen transport: Potential applications in fetal cardiovascular disease diagnosis and therapy. Echocardiography 2017, 34, 1799–1803. [Google Scholar] [CrossRef]
- Chaptinel, J.; Yerly, J.; Mivelaz, Y.; Prsa, M.; Alamo, L.; Vial, Y.; Berchier, G.; Rohner, C.; Gudinchet, F.; Stuber, M. Fetal cardiac cine magnetic resonance imaging in utero. Sci. Rep. 2017, 7, 15540. [Google Scholar] [CrossRef] [PubMed]
- de Sousa, M.T.; Hecher, K.; Yamamura, J.; Kording, F.; Ruprecht, C.; Fehrs, K.; Behzadi, C.; Adam, G.; Schoennagel, B.P. Dynamic fetal cardiac magnetic resonance imaging in four-chamber view using Doppler ultrasound gating in normal fetal heart and in congenital heart disease: Comparison with fetal echocardiography. Ultrasound Obstet. Gynecol. 2018, 53, 669–675. [Google Scholar] [CrossRef] [PubMed]
- de Sousa, M.T.; Hecher, K.; Kording, F.; Yamamura, J.; Lenz, A.; Adam, G.; Bannas, P.; Schoennagel, B.P. Fetal dynamic magnetic resonance imaging using Doppler ultrasound gating for the assessment of the aortic isthmus: A feasibility study. Acta Obstet. et Gynecol. Scand. 2020, 100, 67–73. [Google Scholar] [CrossRef] [PubMed]
- Dong, S.-Z.; Zhu, M.; Li, F. Preliminary experience with cardiovascular magnetic resonance in evaluation of fetal cardiovascular anomalies. J. Cardiovasc. Magn. Reson. 2013, 15, 40. [Google Scholar] [CrossRef]
- Roy, C.W.; Marini, D.; Lloyd, D.F.A.; Mawad, W.; Yoo, S.-J.; Schrauben, E.M.; Jaeggi, E.; Seed, M.; Macgowan, C.K. Preliminary Experience Using Motion Compensated CINE Magnetic Resonance Imaging to Visualise Fetal Congenital Heart Disease. Circ. Cardiovasc. Imaging 2018, 11, e007745. [Google Scholar] [CrossRef]
- Li, X.; Li, X.; Hu, K.; Yin, C. The value of cardiovascular magnetic resonance in the diagnosis of fetal aortic arch anomalies. J. Matern. Neonatal Med. 2016, 30, 1366–1371. [Google Scholar] [CrossRef]
- Lloyd, D.F.A.; Pushparajah, K.; Simpson, J.; van Amerom, J.; van Poppel, M.P.; Schulz, A.; Kainz, B.; Deprez, M.; Lohezic, M.; Allsop, J.; et al. Three-dimensional visualisation of the fetal heart using prenatal MRI with motion-corrected slice-volume registration: A prospective, single-centre cohort study. Lancet 2019, 393, 1619–1627. [Google Scholar] [CrossRef]
- Al Nafisi, B.; van Amerom, J.F.; Forsey, J.; Jaeggi, E.; Grosse-Wortmann, L.; Yoo, S.-J.; Macgowan, C.K.; Seed, M. Fetal circulation in left-sided congenital heart disease measured by cardiovascular magnetic resonance: A case–control study. J. Cardiovasc. Magn. Reson. 2013, 15, 65. [Google Scholar] [CrossRef]
- Sun, L.; Macgowan, C.K.; Sled, J.G.; Yoo, S.-J.; Manlhiot, C.; Porayette, P.; Grosse-Wortmann, L.; Jaeggi, E.; McCrindle, B.W.; Kingdom, J.; et al. Reduced Fetal Cerebral Oxygen Consumption Is Associated With Smaller Brain Size in Fetuses With Congenital Heart Disease. Circulation 2015, 131, 1313–1323. [Google Scholar] [CrossRef]
- Maeno, Y.V.; Kamenir, S.A.; Sinclair, B.; van der Velde, M.E.; Smallhorn, J.F.; Hornberger, L.K. Prenatal Features of Ductus Arteriosus Constriction and Restrictive Foramen Ovale in d-Transposition of the Great Arteries. Circulation 1999, 99, 1209–1214. [Google Scholar] [CrossRef] [PubMed]
- Hoffman, J.I.; Kaplan, S. The incidence of congenital heart disease. J. Am. Coll. Cardiol. 2002, 39, 1890–1900. [Google Scholar] [CrossRef] [PubMed]
- Nieminen, H.P.; Jokinen, E.V.; Sairanen, H.I. Causes of Late Deaths After Pediatric Cardiac Surgery: A Population-Based Study. J. Am. Coll. Cardiol. 2007, 50, 1263–1271. [Google Scholar] [CrossRef] [PubMed]
- Ntsinjana, H.N.; Hughes, M.L.; Taylor, A.M. The Role of Cardiovascular Magnetic Resonance in Pediatric Congenital Heart Disease. J. Cardiovasc. Magn. Reson. 2011, 13, 51. [Google Scholar] [CrossRef]
- Lai, W.W.; Geva, T.; Shirali, G.S.; Frommelt, P.C.; Humes, R.A.; Brook, M.M.; Pignatelli, R.H.; Rychik, J. Guidelines and Standards for Performance of a Pediatric Echocardiogram: A Report from the Task Force of the Pediatric Council of the American Society of Echocardiography. J. Am. Soc. Echocardiogr. 2006, 19, 1413–1430. [Google Scholar] [CrossRef]
- Bennett, D.; Marcus, R.; Stokes, M. Incidents and complications during pediatric cardiac catheterization. Pediatr. Anesth. 2005, 15, 1083–1088. [Google Scholar] [CrossRef]
- Kleinerman, R.A. Cancer risks following diagnostic and therapeutic radiation exposure in children. Pediatr. Radiol. 2006, 36 (Suppl. S2), 121–125. [Google Scholar] [CrossRef]
- Lock, J.E.; Keane, J.F.; Perry, S.B. (Eds.) Diagnostic and Interventional Catheterisation in Congenital Heart Disease, 2nd ed.; Springer: Berlin/Heidelberg, Germany, 1999. [Google Scholar]
- Pennell, D.J.; Sechtem, U.P.; Higgins, C.B.; Manning, W.J.; Pohost, G.M.; Rademakers, F.E.; Van Rossum, A.C.; Shaw, L.J.; Yucel, E.K. Clinical indications for cardiovascular magnetic resonance (CMR): Consensus Panel report? Eur. Heart J. 2004, 25, 1940–1965. [Google Scholar] [CrossRef]
- Powell, A.J.; Geva, T. Blood Flow Measurement by Magnetic Resonance Imaging in Congenital Heart Disease. Pediatr. Cardiol. 2000, 21, 47–58. [Google Scholar] [CrossRef]
- Anderson, R.H.; Razavi, R.; Taylor, A.M. Cardiac anatomy revisited. J. Anat. 2004, 205, 159–177. [Google Scholar] [CrossRef]
- Hughes, M.L.; Stockton, E.; Taylor, A.; McEwan, A. A prospective audit of paediatric cardiac MRI under general anaesthesia; practise and problems. J. Cardiovasc. Magn. Reson. 2009, 11, P249. [Google Scholar] [CrossRef]
- Kaiser, T.; Kellenberger, C.J.; Albisetti, M.; Bergsträsser, E.; Buechel, E.R.V. Normal values for aortic diameters in children and adolescents—Assessment in vivo by contrast-enhanced CMR-angiography. J. Cardiovasc. Magn. Reson. 2008, 10, 56. [Google Scholar] [CrossRef] [PubMed]
- Tsai-Goodman, B.; Geva, T.; Odegard, K.C.; Sena, L.M.; Powell, A.J. Clinical role, accuracy, and technical aspects of cardiovascular magnetic resonance imaging in infants. Am. J. Cardiol. 2004, 94, 69–74. [Google Scholar] [CrossRef]
- Fratz, S.; Hess, J.; Schuhbaeck, A.; Buchner, C.; Hendrich, E.; Martinoff, S.; Stern, H. Routine clinical cardiovascular magnetic resonance in paediatric and adult congenital heart disease: Patients, protocols, questions asked and contributions made. J. Cardiovasc. Magn. Reson. 2008, 10, 46. [Google Scholar] [CrossRef] [PubMed]
- Finn, J.P.; Nael, K.; Deshpande, V.; Ratib, O.; Laub, G. Cardiac MR Imaging: State of the Technology. Radiology 2006, 241, 338–354. [Google Scholar] [CrossRef] [PubMed]
- Garg, R.; Powell, A.J.; Sena, L.; Marshall, A.C.; Geva, T. Effects of metallic implants on magnetic resonance imaging evaluation of Fontan palliation. Am. J. Cardiol. 2005, 95, 688–691. [Google Scholar] [CrossRef]
- Macgowan, C.K.; Al-Kwifi, O.S.; Varodayan, F.; Yoo, S.-J.; Wright, G.A.; Kellenberger, C.J. Optimization of 3D contrast-enhanced pulmonary magnetic resonance angiography in pediatric patients with congenital heart disease. Magn. Reson. Med. 2005, 54, 207–212. [Google Scholar] [CrossRef]
- Piccini, D.; Monney, P.; Sierro, C.; Coppo, S.; Bonanno, G.; van Heeswijk, R.B.; Chaptinel, J.; Vincenti, G.; De Blois, J.; Koestner, S.C.; et al. Respiratory Self-navigated Postcontrast Whole-Heart Coronary MR Angiography: Initial Experience in Patients. Radiology 2014, 270, 378–386. [Google Scholar] [CrossRef]
- Tangcharoen, T.; Bell, A.; Hegde, S.; Hussain, T.; Beerbaum, P.; Schaeffter, T.; Razavi, R.; Botnar, R.M.; Greil, G.F. Detection of Coronary Artery Anomalies in Infants and Young Children with Congenital Heart Disease by Using MR Imaging. Radiology 2011, 259, 240–247. [Google Scholar] [CrossRef]
- Buechel, E.R.V.; Balmer, C.; Bauersfeld, U.; Kellenberger, C.J.; Schwitter, J. Feasibility of perfusion cardiovascular magnetic resonance in paediatric patients. J. Cardiovasc. Magn. Reson. 2009, 11, 51. [Google Scholar] [CrossRef] [PubMed]
- Moscatelli, S.; Bianco, F.; Cimini, A.; Panebianco, M.; Leo, I.; Bucciarelli-Ducci, C.; Perrone, M.A. The Use of Stress Cardiovascular Imaging in Pediatric Population. Children 2023, 10, 218. [Google Scholar] [CrossRef] [PubMed]
- Stagnaro, N.; Moscatelli, S.; Cheli, M.; Bondanza, S.; Marasini, M.; Trocchio, G. Dobutamine Stress Cardiac MRI in Pediatric Patients with Suspected Coronary Artery Disease. Pediatr. Cardiol. 2022, 44, 451–462. [Google Scholar] [CrossRef] [PubMed]
- Eichhorn, J.; Fink, C.; Delorme, S.; Ulmer, H. Rings, slings and other vascular abnormalities. Ultrafast computed tomography and magnetic resonance angiography in pediatric cardiology. Z. Kardiol. 2004, 93, 201–208. [Google Scholar] [CrossRef]
- Knobel, Z.; Kellenberger, C.J.; Kaiser, T.; Albisetti, M.; Bergsträsser, E.; Buechel, E.R.V. Geometry and dimensions of the pulmonary artery bifurcation in children and adolescents: Assessment in vivo by contrast-enhanced MR-angiography. Int. J. Cardiovasc. Imaging 2010, 27, 385–396. [Google Scholar] [CrossRef]
- Grosse-Wortmann, L.; Al-Otay, A.; Goo, H.W.; Macgowan, C.K.; Coles, J.G.; Benson, L.N.; Redington, A.N.; Yoo, S.-J. Anatomical and Functional Evaluation of Pulmonary Veins in Children by Magnetic Resonance Imaging. J. Am. Coll. Cardiol. 2007, 49, 993–1002. [Google Scholar] [CrossRef]
- Beerbaum, P.; Körperich, H.; Barth, P.; Esdorn, H.; Gieseke, J.; Meyer, H. Noninvasive Quantification of Left-to-Right Shunt in Pediatric Patients. Circulation 2001, 103, 2476–2482. [Google Scholar] [CrossRef]
- Wald, R.M.; Redington, A.N.; Pereira, A.; Provost, Y.L.; Paul, N.S.; Oechslin, E.N.; Silversides, C.K. Refining the assessment of pulmonary regurgitation in adults after tetralogy of Fallot repair: Should we be measuring regurgitant fraction or regurgitant volume? Eur. Heart J. 2008, 30, 356–361. [Google Scholar] [CrossRef] [PubMed]
- Prakash, A.; Torres, A.J.; Printz, B.F.; Prince, M.R.; Nielsen, J.C. Usefulness of Magnetic Resonance Angiography in the Evaluation of Complex Congenital Heart Disease in Newborns and Infants. Am. J. Cardiol. 2007, 100, 715–721. [Google Scholar] [CrossRef]
- Gewillig, M. The Fontan circulation. Heart 2005, 91, 839–846. [Google Scholar] [CrossRef]
- Moscatelli, S.; Borrelli, N.; Sabatino, J.; Leo, I.; Avesani, M.; Montanaro, C.; Di Salvo, G. Role of Cardiovascular Imaging in the Follow-Up of Patients with Fontan Circulation. Children 2022, 9, 1875. [Google Scholar] [CrossRef] [PubMed]
- Beroukhim, R.S.; Prakash, A.; Buechel, E.R.V.; Cava, J.R.; Dorfman, A.L.; Festa, P.; Hlavacek, A.M.; Johnson, T.R.; Keller, M.S.; Krishnamurthy, R.; et al. Characterization of Cardiac Tumors in Children by Cardiovascular Magnetic Resonance Imaging. J. Am. Coll. Cardiol. 2011, 58, 1044–1054. [Google Scholar] [CrossRef] [PubMed]
- Karamitsos, T.D.; Francis, J.M.; Myerson, S.; Selvanayagam, J.B.; Neubauer, S. The Role of Cardiovascular Magnetic Resonance Imaging in Heart Failure. J. Am. Coll. Cardiol. 2009, 54, 1407–1424. [Google Scholar] [CrossRef] [PubMed]
- Vashist, S.; Singh, G.K. Acute myocarditis in children: Current concepts and management. Curr. Treat. Options Cardiovasc. Med. 2009, 11, 383–391. [Google Scholar] [CrossRef]
- Pezel, T.; Garot, P.; Hovasse, T.; Unterseeh, T.; Champagne, S.; Kinnel, M.; Toupin, S.; Louvard, Y.; Morice, M.C.; Sanguineti, F.; et al. Vasodilatation stress cardiovascular magnetic resonance imaging: Feasibility, workflow and safety in a large prospective registry of more than 35,000 patients. Arch. Cardiovasc. Dis. 2021, 114, 490–503. [Google Scholar] [CrossRef] [PubMed]
- Rappaport, B.; Mellon, R.D.; Simone, A.; Woodcock, J. Defining Safe Use of Anesthesia in Children. N. Engl. J. Med. 2011, 364, 1387–1390. [Google Scholar] [CrossRef]
- Shellock, F.G.; Woods, T.O.; Crues, J.V. MR Labeling Information for Implants and Devices: Explanation of Terminology. Radiology 2009, 253, 26–30. [Google Scholar] [CrossRef]
- Nazarian, S.; Hansford, R.; Roguin, A.; Goldsher, D.; Zviman, M.M.; Lardo, A.C.; Caffo, B.S.; Frick, K.D.; Kraut, M.A.; Kamel, I.R.; et al. A Prospective Evaluation of a Protocol for Magnetic Resonance Imaging of Patients With Implanted Cardiac Devices. Ann. Intern. Med. 2011, 155, 415–424. [Google Scholar] [CrossRef]
- Nazarian, S.; Beinart, R.; Halperin, H.R. Magnetic Resonance Imaging and Implantable Devices. Circ. Arrhythmia Electrophysiol. 2013, 6, 419–428. [Google Scholar] [CrossRef]
- Bucciarelli-Ducci, C.; Vardas, P. Reconsidering safety and reducing barriers to MRI in patients with cardiac implantable electronic devices. Eur. Heart J. 2021, 43, 2479–2481. [Google Scholar] [CrossRef] [PubMed]
- Bhuva, A.N.; Moralee, R.; Brunker, T.; Lascelles, K.; Cash, L.; Patel, K.P.; Lowe, M.; Sekhri, N.; Alpendurada, F.; Pennell, D.J.; et al. Evidence to support magnetic resonance conditional labelling of all pacemaker and defibrillator leads in patients with cardiac implantable electronic devices. Eur. Heart J. 2021, 43, 2469–2478. [Google Scholar] [CrossRef] [PubMed]
- Do, C.; DeAguero, J.; Brearley, A.; Trejo, X.; Howard, T.; Escobar, G.P.; Wagner, B. Gadolinium-Based Contrast Agent Use, Their Safety, and Practice Evolution. Kidney360 2020, 1, 561–568. [Google Scholar] [CrossRef] [PubMed]
- Baumgartner, H.; De Backer, J.; Babu-Narayan, S.V.; Budts, W.; Chessa, M.; Diller, G.-P.; Lung, B.; Kluin, J.; Lang, I.M.; Meijboom, F.; et al. 2020 ESC Guidelines for the management of adult congenital heart disease. Eur. Heart J. 2020, 42, 563–645. [Google Scholar] [CrossRef]
- Dyverfeldt, P.; Bissell, M.; Barker, A.J.; Bolger, A.F.; Carlhäll, C.-J.; Ebbers, T.; Francios, C.J.; Frydrychowicz, A.; Geiger, J.; Giese, D.; et al. 4D flow cardiovascular magnetic resonance consensus statement. J. Cardiovasc. Magn. Reson. 2015, 17, 72. [Google Scholar] [CrossRef]
- Demirkiran, A.; van Ooij, P.; Westenberg, J.J.M.; Hofman, M.B.M.; van Assen, H.C.; Schoonmade, L.J.; Asim, U.; Blanken, C.P.S.; Nederveen, A.J.; van Rossum, A.C.; et al. Clinical intra-cardiac 4D flow CMR: Acquisition, analysis, and clinical applications. Eur. Heart J. Cardiovasc. Imaging 2021, 23, 154–165. [Google Scholar] [CrossRef]
- Bulluck, H.; Dharmakumar, R.; Arai, A.E.; Berry, C.; Hausenloy, D.J. Cardiovascular Magnetic Resonance in Acute ST-Segment–Elevation Myocardial Infarction. Circulation 2018, 137, 1949–1964. [Google Scholar] [CrossRef]
- Raman, S.V.; Simonetti, O.P.; Winner, M.W.; Dickerson, J.A.; He, X.; Mazzaferri, E.L.; Ambrosio, G. Cardiac Magnetic Resonance With Edema Imaging Identifies Myocardium at Risk and Predicts Worse Outcome in Patients With Non–ST-Segment Elevation Acute Coronary Syndrome. J. Am. Coll. Cardiol. 2010, 55, 2480–2488. [Google Scholar] [CrossRef]
- Symons, R.; Pontone, G.; Schwitter, J.; Francone, M.; Iglesias, J.F.; Barison, A.; Zalewski, J.; de Luca, L.; Degrauwe, S.; Claus, P.; et al. Long-Term Incremental Prognostic Value of Cardiovascular Magnetic Resonance After ST-Segment Elevation Myocardial Infarction. JACC Cardiovasc. Imaging 2018, 11, 813–825. [Google Scholar] [CrossRef]
- Leo, I.; Araujo, L.T.; Bucciarelli-Ducci, C. Contemporary Non-Invasive Imaging in Chronic Coronary Syndrome: What Stress Cardiovascular Magnetic Resonance has to Offer. ABC Imagem Cardiovasc. 2023, 36, e20230004. [Google Scholar] [CrossRef]
- Eitel, I.; Desch, S.; De Waha, S.; Fuernau, G.; Gutberlet, M.; Schuler, G.; Thiele, H. Long-term prognostic value of myocardial salvage assessed by cardiovascular magnetic resonance in acute reperfused myocardial infarction. Heart 2011, 97, 2038–2045. [Google Scholar] [CrossRef]
- Eitel, I.; Kubusch, K.; Strohm, O.; Desch, S.; Mikami, Y.; de Waha, S.; Gutberlet, M.; Schuler, G.; Friedrich, M.G.; Thiele, H. Prognostic Value and Determinants of a Hypointense Infarct Core in T2-Weighted Cardiac Magnetic Resonance in Acute Reperfused ST-Elevation–Myocardial Infarction. Circ. Cardiovasc. Imaging 2011, 4, 354–362. [Google Scholar] [CrossRef]
- Schwitter, J.; Arai, A. Assessment of cardiac ischaemia and viability: Role of cardiovascular magnetic resonance. Eur. Heart J. 2011, 32, 799–809. [Google Scholar] [CrossRef] [PubMed]
- Kramer, C.M.; Barkhausen, J.; Bucciarelli-Ducci, C.; Flamm, S.D.; Kim, R.J.; Nagel, E. Standardized cardiovascular magnetic resonance imaging (CMR) protocols: 2020 update. J. Cardiovasc. Magn. Reson. 2020, 22, 17. [Google Scholar] [CrossRef] [PubMed]
- Knuuti, J.; Wijns, W.; Saraste, A.; Capodanno, D.; Barbato, E.; Funck-Brentano, C.; Prescott, E.; Storey, R.F.; Deaton, C.; Cuisset, T.; et al. 2019 ESC Guidelines for the diagnosis and management of chronic coronary syndromes. Eur. Heart J. 2020, 41, 407–477. [Google Scholar] [CrossRef] [PubMed]
- Gulati, M.; Levy, P.D.; Mukherjee, D.; Amsterdam, E.; Bhatt, D.L.; Birtcher, K.K.; Blankstein, R.; Boyd, J.; Bullock-Palmer, R.P.; Conejo, T.; et al. 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR Guideline for the Evaluation and Diagnosis of Chest Pain. J. Am. Coll. Cardiol. 2021, 78, e187–e285. [Google Scholar] [CrossRef]
- Hussain, S.T.; Paul, M.; Plein, S.; McCann, G.P.; Shah, A.M.; Marber, M.S.; Chiribiri, A.; Morton, G.; Redwood, S.; MacCarthy, P.; et al. Design and rationale of the MR-INFORM study: Stress perfusion cardiovascular magnetic resonance imaging to guide the management of patients with stable coronary artery disease. J. Cardiovasc. Magn. Reson. 2012, 14, 65. [Google Scholar] [CrossRef]
- Greenwood, J.P.; Maredia, N.; Younger, J.; Brown, J.M.; Nixon, J.; Everett, C.C.; Bijsterveld, P.; Ridgway, J.P.; Radjenovic, A.; Dickinson, C.J.; et al. Cardiovascular magnetic resonance and single-photon emission computed tomography for diagnosis of coronary heart disease (CE-MARC): A prospective trial. Lancet 2012, 379, 453–460. [Google Scholar] [CrossRef]
- Murthy, V.; Naya, M.; Taqueti, V.R.; Foster, C.R.; Gaber, M.; Hainer, J.; Dorbala, S.; Blankstein, R.; Rimoldi, O.; Camici, P.G.; et al. Effects of Sex on Coronary Microvascular Dysfunction and Cardiac Outcomes. Circulation 2014, 129, 2518–2527. [Google Scholar] [CrossRef]
- Kotecha, T.; Martinez-Naharro, A.; Boldrini, M.; Knight, D.; Hawkins, P.; Kalra, S.; Patel, D.; Coghlan, G.; Moon, J.; Plein, S.; et al. Automated Pixel-Wise Quantitative Myocardial Perfusion Mapping by CMR to Detect Obstructive Coronary Artery Disease and Coronary Microvascular Dysfunction. JACC: Cardiovasc. Imaging 2019, 12, 1958–1969. [Google Scholar] [CrossRef]
- Leo, I.; Nakou, E.; Artico, J.; Androulakis, E.; Wong, J.; Moon, J.C.; Indolfi, C.; Bucciarelli-Ducci, C. Strengths and weaknesses of alternative noninvasive imaging approaches for microvascular ischemia. J. Nucl. Cardiol. 2022, 30, 227–238. [Google Scholar] [CrossRef]
- Agewall, S.; Beltrame, J.F.; Reynolds, H.R.; Niessner, A.; Rosano, G.; Caforio, A.L.P.; De Caterina, R.; Zimarino, M.; Roffi, M.; Kjeldsen, K.; et al. ESC working group position paper on myocardial infarction with non-obstructive coronary arteries. Eur. Heart J. 2016, 38, ehw149–ehw153. [Google Scholar] [CrossRef]
- Ibanez, B.; James, S.; Agewall, S.; Antunes, M.J.; Bucciarelli-Ducci, C.; Bueno, H.; Caforio, A.L.P.; Crea, F.; Goudevenos, J.A.; Halvorsen, S.; et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur. Heart J. 2018, 39, 119–177. [Google Scholar] [CrossRef]
- Tamis-Holland, J.E.; Jneid, H.; Reynolds, H.R.; Agewall, S.; Brilakis, E.S.; Brown, T.M.; Lerman, A.; Cushman, M.; Kumbhani, D.J.; Arslanian-Engoren, C.; et al. Contemporary Diagnosis and Management of Patients With Myocardial Infarction in the Absence of Obstructive Coronary Artery Disease: A Scientific Statement From the American Heart Association. Circulation 2019, 139, e891–e908. [Google Scholar] [CrossRef] [PubMed]
- Dastidar, A.G.; Baritussio, A.; De Garate, E.; Drobni, Z.D.; Biglino, G.; Singhal, P.; Milano, E.G.; Angelini, G.D.; Dorman, S.; Strange, J.; et al. Prognostic Role of CMR and Conventional Risk Factors in Myocardial Infarction With Nonobstructed Coronary Arteries. JACC Cardiovasc. Imaging 2019, 12, 1973–1982. [Google Scholar] [CrossRef]
- Williams, M.G.; Liang, K.; De Garate, E.; Spagnoli, L.; Fiori, E.; Dastidar, A.; Benedetto, U.; Biglino, G.; Johnson, T.W.; Luscher, T.; et al. Peak Troponin and CMR to Guide Management in Suspected ACS and Nonobstructive Coronary Arteries. JACC Cardiovasc. Imaging 2022, 15, 1578–1587. [Google Scholar] [CrossRef]
- Assomull, R.G.; Prasad, S.K.; Lyne, J.; Smith, G.; Burman, E.D.; Khan, M.; Sheppard, M.N.; Poole-Wilson, P.A.; Pennell, D.J. Cardiovascular Magnetic Resonance, Fibrosis, and Prognosis in Dilated Cardiomyopathy. J. Am. Coll. Cardiol. 2006, 48, 1977–1985. [Google Scholar] [CrossRef] [PubMed]
- Moon, J.C.C.; Reed, E.; Sheppard, M.N.; Elkington, A.G.; Ho, S.Y.; Burke, M.; Petrou, M.; Pennell, D.J. The histologic basis of late gadolinium enhancement cardiovascular magnetic resonance in hypertrophic cardiomyopathy. J. Am. Coll. Cardiol. 2004, 43, 2260–2264. [Google Scholar] [CrossRef] [PubMed]
- O’Hanlon, R.; Grasso, A.; Roughton, M.; Moon, J.C.; Clark, S.; Wage, R.; Webb, J.; Kulkarni, M.; Dawson, D.; Sulaibeekh, L.; et al. Prognostic Significance of Myocardial Fibrosis in Hypertrophic Cardiomyopathy. J. Am. Coll. Cardiol. 2010, 56, 867–874. [Google Scholar] [CrossRef]
- Dorbala, S.; Cuddy, S.; Falk, R.H. How to Image Cardiac Amyloidosis. JACC Cardiovasc. Imaging 2019, 13, 1368–1383. [Google Scholar] [CrossRef]
- Maceira, A.M.; Joshi, J.; Prasad, S.K.; Moon, J.C.; Perugini, E.; Harding, I.; Sheppard, M.N.; Poole-Wilson, P.A.; Hawkins, P.N.; Pennell, D.J. Cardiovascular Magnetic Resonance in Cardiac Amyloidosis. Circulation 2005, 111, 186–193. [Google Scholar] [CrossRef] [PubMed]
- Perry, R.; Shah, R.; Saiedi, M.; Patil, S.; Ganesan, A.; Linhart, A.; Selvanayagam, J.B. The Role of Cardiac Imaging in the Diagnosis and Management of Anderson-Fabry Disease. JACC Cardiovasc. Imaging 2019, 12, 1230–1242. [Google Scholar] [CrossRef] [PubMed]
- Kirk, P.; Roughton, M.; Porter, J.; Walker, J.; Tanner, M.; Patel, J.; Wu, D.; Taylor, J.; Westwood, M.; Anderson, L.; et al. Cardiac T2* Magnetic Resonance for Prediction of Cardiac Complications in Thalassemia Major. Circulation 2009, 120, 1961–1968. [Google Scholar] [CrossRef] [PubMed]
- Hulten, E.; Aslam, S.; Osborne, M.; Abbasi, S.; Bittencourt, M.S.; Blankstein, R. Cardiac sarcoidosis—State of the art review. Cardiovasc. Diagn. Ther. 2016, 6, 50–63. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, V.M.; Schulz-Menger, J.; Holmvang, G.; Kramer, C.M.; Carbone, I.; Sechtem, U.; Kindermann, I.; Gutberlet, M.; Cooper, L.T.; Liu, P.; et al. Cardiovascular Magnetic Resonance in Nonischemic Myocardial Inflammation. J. Am. Coll. Cardiol. 2018, 72, 3158–3176. [Google Scholar] [CrossRef]
- Corrado, D.; Van Tintelen, P.J.; McKenna, W.J.; Hauer, R.N.W.; Anastastakis, A.; Asimaki, A.; Basso, C.; Bauce, B.; Brunckhorst, C.; Bucciarelli-Ducci, C.; et al. International Experts. Arrhythmogenic right ventricular cardiomyopathy: Evalu-ation of the current diagnostic criteria and differential diagnosis. Eur. Heart J. 2020, 41, 1414–1429. [Google Scholar] [CrossRef]
- Groenink, M.; Wilde, A.A. The “Accordion Sign,” a New Tune in Arrhythmogenic Right Ventricular Dysplasia/Cardiomyopathy Magnetic Resonance Imaging? J. Am. Coll. Cardiol. 2009, 53, 1300–1301. [Google Scholar] [CrossRef] [PubMed]
- Čelutkienė, J.; Pudil, R.; López-Fernández, T.; Grapsa, J.; Nihoyannopoulos, P.; Bergler-Klein, J.; Cohen-Solal, A.; Farmakis, D.; Tocchetti, C.G.; von Haehling, S.; et al. Role of cardiovascular imaging in cancer patients receiving cardiotoxic therapies: A position statement on behalf of the H eart F ailure A ssociation (HFA), the E uropean A ssociation of C ardiovascular I maging (EACVI) and the Cardio-Oncology Council of the European Society of Cardiology (ESC). Eur. J. Heart Fail. 2020, 22, 1504–1524. [Google Scholar] [CrossRef]
- Cury, R.C.; Abbara, S.; Sandoval, L.J.-D.; Houser, S.; Brady, T.J.; Palacios, I.F. Visualization of Endomyocardial Fibrosis by Delayed-Enhancement Magnetic Resonance Imaging. Circulation 2005, 111, e115–e117. [Google Scholar] [CrossRef]
- Francone, M.; Dymarkowski, S.; Kalantzi, M.; Bogaert, J. Real-time cine MRI of ventricular septal motion: A novel approach to assess ventricular coupling. J. Magn. Reson. Imaging 2005, 21, 305–309. [Google Scholar] [CrossRef]
- Leo, I. Imaging in Women with Heart Failure: Sex-Specific Characteristics and Current Challenges. 2022. Available online: https://www.cfrjournal.com/articles/imaging-women-heart-failure-sex-specific-characteristics-and-current-challenges (accessed on 4 December 2022).
- Ray, J.G.; Vermeulen, M.J.; Bharatha, A.; Montanera, W.J.; Park, A.L. Association Between MRI Exposure During Pregnancy and Fetal and Childhood Outcomes. JAMA 2016, 316, 952–961. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Bournissen, F.; Shrim, A.; Koren, G. Safety of gadolinium during pregnancy. Can. Fam. Physician 2006, 52, 309–310. [Google Scholar] [PubMed]
- Sachs, H.C.; Frattarelli, D.A.C.; Galinkin, J.L.; Green, T.P.; Johnson, T.; Neville, K.; Paul, I.M.; Anker, J.V.D. COMMITTEE ON DRUGS The Transfer of Drugs and Therapeutics Into Human Breast Milk: An Update on Selected Topics. Pediatrics 2013, 132, e796–e809. [Google Scholar] [CrossRef] [PubMed]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Moscatelli, S.; Leo, I.; Lisignoli, V.; Boyle, S.; Bucciarelli-Ducci, C.; Secinaro, A.; Montanaro, C. Cardiovascular Magnetic Resonance from Fetal to Adult Life—Indications and Challenges: A State-of-the-Art Review. Children 2023, 10, 763. https://doi.org/10.3390/children10050763
Moscatelli S, Leo I, Lisignoli V, Boyle S, Bucciarelli-Ducci C, Secinaro A, Montanaro C. Cardiovascular Magnetic Resonance from Fetal to Adult Life—Indications and Challenges: A State-of-the-Art Review. Children. 2023; 10(5):763. https://doi.org/10.3390/children10050763
Chicago/Turabian StyleMoscatelli, Sara, Isabella Leo, Veronica Lisignoli, Siobhan Boyle, Chiara Bucciarelli-Ducci, Aurelio Secinaro, and Claudia Montanaro. 2023. "Cardiovascular Magnetic Resonance from Fetal to Adult Life—Indications and Challenges: A State-of-the-Art Review" Children 10, no. 5: 763. https://doi.org/10.3390/children10050763
APA StyleMoscatelli, S., Leo, I., Lisignoli, V., Boyle, S., Bucciarelli-Ducci, C., Secinaro, A., & Montanaro, C. (2023). Cardiovascular Magnetic Resonance from Fetal to Adult Life—Indications and Challenges: A State-of-the-Art Review. Children, 10(5), 763. https://doi.org/10.3390/children10050763





