The International Classification of Functioning, Disability and Health: Accuracy in Aquatic Activities Reports among Children with Developmental Delay
Abstract
:1. Introduction
1.1. The ICF Framework
1.1.1. The ICF’s Main Terminology
- Well-being (or quality of life)—a general term encompassing the total universe of human life domains, including physical, mental and social aspects. Well-being is a subjective feeling, i.e., what people feel about their health condition and its consequences on their life;
- Health condition—an umbrella term for an illness, disorder, injury or trauma as well as other circumstances, such as pregnancy, aging, stress, a congenital anomaly or genetic predisposition. HCs are coded using the International Classification of Diseases, Tenth Revision (ICD-10) [17];
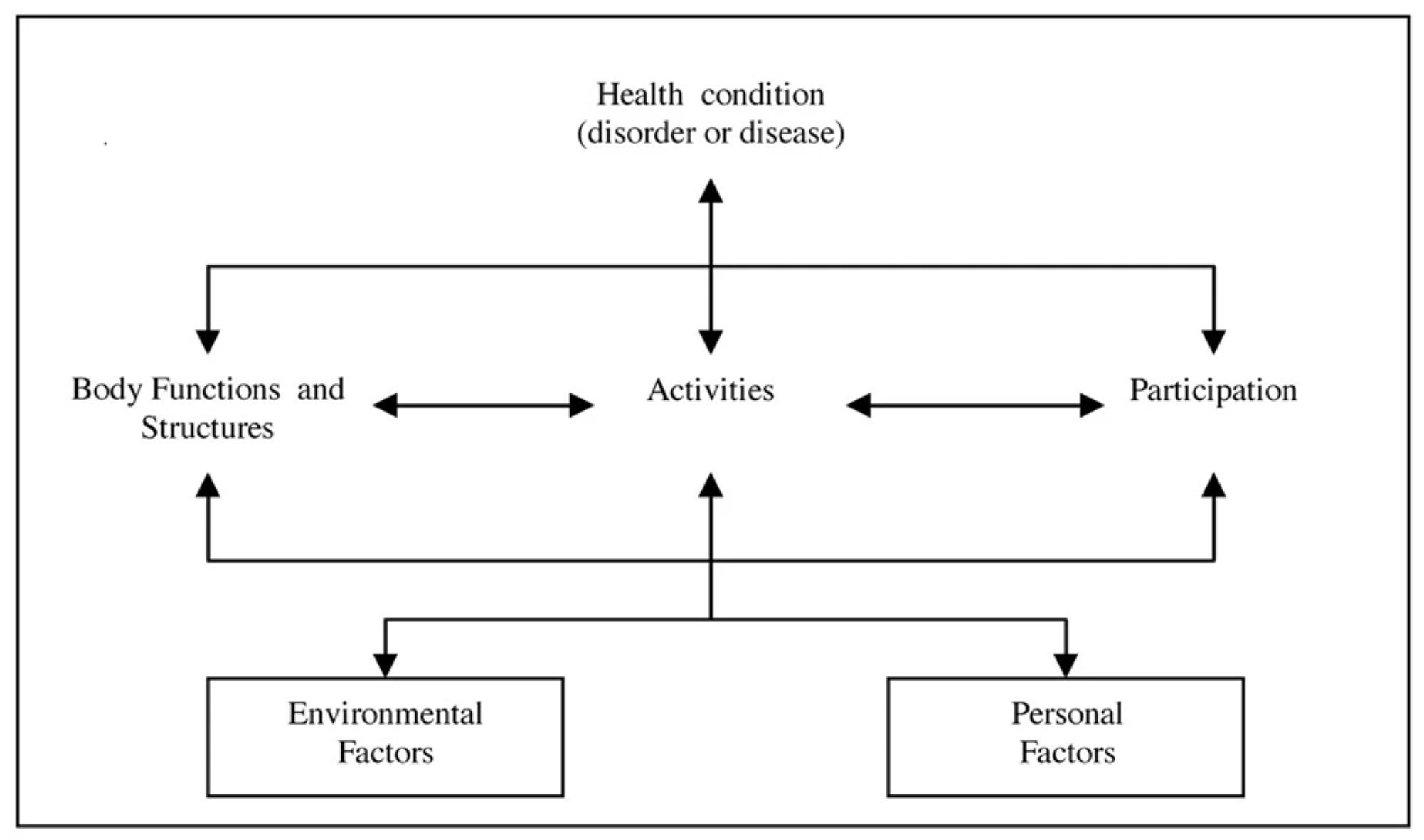
- “Functioning” and “Disability”—two umbrella terms which are associated with health conditions. These two classifications are complementary and should be used together. Both terms encompass all the aspects of the interaction between the individual’s body functions, activities and participation and its contextual factors. “Functioning” represents all the positive aspects, while “Disability” represents all the negative aspects, such as impairments, activity limitations and participation restrictions [11,12,13,18,19];
- Qualifiers—the ICF framework offers means to assess a person’s functioning using universal numeric codes with values from 0 = no problem to 4 = complete problem. Their role is to specify the extent or the magnitude of functioning or disability within the BF and BS components of functioning. The other two qualifiers are related to theindividual’s environment while he/she is performing an activity (related to A&P). These codes define the individual’s “Capacity” (the highest probable level of functioning in a uniform or standard environment) and the “Performance” (what individuals do in their current environment). The EF qualifiers refer to the effect of the environment on functioning, i.e., whether they help (facilitators) or interfere (barriers) [11,12,13,18].
1.1.2. The ICF Model—Interactions between the Components
1.1.3. The Use of the ICF in the Professional Literature
1.2. The Aim of this Scoping Review
- The level of use of the ICF framework in general, i.e., the extent to which it is actually used in studies between 2010 and 2020;
- The level of mastery of the authors of the articles in their use of the ICF terms and the level of understanding of the framework itself, i.e., whether the ICF framework is fully understood and communicated accurately.
2. Materials and Methods
2.1. Study Design
2.2. Search Strategy
- Article selection: studies published in the time period from 1 January 2010 until 31 January 2020, which investigated the effect of AAs on children with developmental disability at elementary school age (6–12 years), were collected;
- The search was limited to studies that were published in English, full articles and open to the public on the Internet or in the medical libraries of Alcala University, Ben Gurion University in the Negev, Tel Aviv University and Sheba Medical Center;
- Electronic databases: Relevant articles were identified by searching among the international healthcare databases PubMed, PubMed Central® (PMC), Google Scholar, Physiotherapy Evidence Database, Cochrane Library, ResearchGate, Scientific Research and Scielo. The search also reviewed the bibliographic references of the collected papers for the purpose of locating additional studies not found in the basic databases;
- Keyword combinations used for the search were the term “A child/children” with all terms related to aquatic activities and accompanying the following concepts: “hydro”, “aquatic”, “pool”, “swimming” and “water” (Table 1);
- The selection process of the articles contained two stages: at the first stage, the researchers looked for the criteria word or combination (Table 1) in the title and the abstract. If it was found to be matching, the next stage of evaluating the full text was performed. After these stages, both reviewers (MHF and IRC—both physical therapists and aquatic therapists for many years) debated about disparities, which were cleared up after re-examination of the full text and discussions about them. No rerun work was carried out prior to the final analysis.
2.3. Inclusion and Exclusion Criteria
- Studies characteristics: All articles should have been published within the defined time period. The articles should contain all the details of the research, including the full results. The articles types were: descriptive research, a systematic scoping review, a literature review, an intervention review, an experts’ opinion article, a consensus process to report, narrative review and quasi-experiment or an integrative review;
- Population: The main population of the studies should be children with developmental delays aged 6–12. Studies that included different age groups were also included as long as this age group was included in the study. For example, in the review by Gorter and Currie, 2011 [25] of 6 previous articles, out of the 40 children participating in the various studies, 30 matched the age group defined in the current review;
- Aquatic methods used in the interventions: The focus is on studies that examined the effect of AAs without aids, such as floats, special seats and more. The types of intervention included different aquatic activities, such as swimming, aquatic therapy or any other physical activity in the aquatic environment, individually or in groups. The techniques used by the instructors, the means of instruction and the nature of accessibility to the children, as well as the environment in which the intervention took place, were different and diverse. In the world, AAs are widely used by many professionals, each referring to the activity under a different category, hence the need to expand the number of categories in order to include in the review as many types of AAs as possible;
- Relation to the ICF: the article should refer to the ICF, whether in the form of an explanation, a link to the research topics or in the results, as described in Daugaard et al.’s [22] guidelines on ICF reporting criteria;
- Quality assessment: The evaluation of the articles was carried out by a review reading, including a data collection and analysis process in which all the criteria defined in the guidelines of Daugaard et al. [22] were scanned and summarized for each and every article. A discussion was held between the ICF expert (HTN) and the lead author (MHF), and the final conclusions were reached after a procedure of agreement between the two researchers.
3. Results
3.1. Electronic Search Results
3.2. Articles Included
3.3. Quality Analysis—The ICF Reporting Criteria
3.4. An Expansion on the Results of the ICF Critical Reading Presented in Table 3
- A.
- The ICF’s language (criteria 2, 4 and 5)—term definitions and interactions: All nine articles were published ten years or more after the advent of the ICF model in the world. In most of the articles, the introduction of the model, its terms, domains and categories is very short or missing (except for the articles of Gorter and Currie [25], Cross et al. [10] and Declerck [20]). The vast majority of authors seem to presuppose that the model’s structure and principles are clearly understood by the readers and tend to skip explanations of the terms and their role as tools for evaluating functioning and disability.Another point is that there is an inconsistency in the language of the model. Some authors replace the definition of “components” with the word “levels” (Blohm [26]) or “categories” (Gorter and Currie [25]), and the term “domain” is also replaced by the term “category” (Cross et al. [10]; Declerck [20]) and “area” (Khalaji et al. [28]). Another misapplication is of the word “Disability” as a term that describes a health status, e.g., “Cerebral Palsy is the most common motor disability” [20] (p. 1) and “children with disabilities” [10] (p. 6);
- B.
- Addressing the various components of the ICF (criteria 1 and 9): In this area, there is a noticeable omission to the unique important factor added in the ICF model—the contextual components and especially the PF. Only two articles addressed the contextual components specifically while explaining the model (Gorter and Currie [25] and Declerck [20]). These two articles are also the only articles that refer to the PF as an important component in the children’s lives for future studies [25] and as an important factor to look for in the studies’ outcomes [20]. In all other articles, the PF is mentioned incidentally or not mentioned at all;
- C.
- D.
- Awareness of the literature predating the study and relevant reference to the ICF literature (criterion 3): As expected, all nine articles addressed previous research and publications. Eight out of nine also linked them to various components of the ICF. Only one (Khalaji et al. [28]) did not refer to the ICF literature at all. One surprising fact is that Khalaji et al. [28] did not refer to ICF literature at all even though the study was looking for researches on hydrotherapy and its application for the improvement of the ICF in spastic diplegia cerebral palsy patients;
- E.
- The ICF linking to another tool and ICF-based instruments, including previous articles (criteria 3, 6 and 10): Only one group of authors - Güeita-Rodríguez et al. [4,29,30]—provided a full description of the recommended methodology (e.g., linking research outcomes to the ICF components). Some authors gave an example of links between the results of the studies reviewed and the ICF components but did not explain the methodology used [10,25,26,27]. Most authors did not mention the linkage process at all [25,29].Regarding the relationship between the ICF and the tools that were described in the articles, there is little more information on this subject. In five of the articles, the researchers explain the linkage made between the ICF components and the ICF-based tools that were developed in order to allow researchers to provide measures of functioning (Cross et al. [10]) or quality of life (Declerck [20]) and therapeutic intervention tools, questionnaires and APT-CSs (Güeita-Rodríguez et al. [4,29,30]).
- F.
- Knowledge translation between different settings (criterion 11): The analysis of the studies found that six of the articles refer to the ICF model as a language that creates a connection between the various assessment tools and enables the construction of a common base of knowledge between the various professions [4,10,20,27,29,30]. It can also serve as a framework that addresses the aquatic environment and group activities as two EFs that constitute unique factors that affect the child’s quality of life, functioning and motivation (Sutthibuta [27]). Güeita-Rodríguez et al. [4,29,30] developed preliminary APT-CSs for children and youth with neurological disorders. All data collection and consent work were based on a combination between the ICF-CY model, the WHO methodology for the ICF’s core sets (ICF-CSs) [31,32], the principles of the Rehab-Cycle model [33] and the Delphi technique [34].
4. Discussion
- A.
- The ICF’s language (criteria 2, 4 and 5)—Term definitions and interactions: The complexity of the model requires a different perception than the traditional medical model, which views disability as a problem of the person caused by his/her health condition and to be managed by medical care. It also differs from the social model, which views disability as a complex collection of conditions, mostly created by the social environment where the management of the problem requires social action. The ICF is more than an integration of these two opposing models. It provides a “biopsychosocial” approach regarding the person’s functioning or disability [11,12,13]. The model is a globally agreed-on conceptual framework and common language for health purposes [35]. The change in terms and the addition of contextual factors requires more in-depth consideration and the provision of more details to create a sufficient level of knowledge among readers and professionals at a level that will allow a uniform, international, interprofessional language. According to the principles of the ICF framework, the various health components do not stand on their own. Each of the different components has multiple interactions with the other components and can affect and be affected by them. For this reason, in any reference to the model, it is necessary to give place to the interactions and effects, explain them and look for the interactions between the various components.As for the inconsistency in the language of the model, the ICF framework is a new professional language that uses a mix of known and new concepts and terms in a special way that is explained in the model. Each ICF component (except for personal factors) consists of various domains (chapters), and within each domain, there are categories, which are the wording units of classification that enable the assessors to select the appropriate health and health-related states of an individual. The ICF terminology is important in the creation of an international uniform language [11,12,13,15,20].As for the misapplication of the word “Disability” as a term that describes a health status, previously, when the classification model was based on a medical diagnosis, the word “disability” was defined as a problem of the person caused by his/her health condition and required medical care aimed at cure or helping the patient to adjust. Within the ICF model, disability, similarly (but opposite) to functioning, is an umbrella term for impairments, activity limitations and participation restrictions and results from the interaction between the person’s health condition and his/her contextual factors. By defining disability as an umbrella term, the ICF model acknowledges that every human-being can experience a decrement in health and thereby experience some disability. It shifts the focus from the health condition to the context, such as personality, past experience and the situation (PFs and EFs), which can be factors that promote functioning and, to the same extent, may cause disability in a particular situation [11,12,13,15].Only three articles [10,20,26] explicitly addressed the interaction between the ICF components indicates a deficiency in the overall broader reference to the model. Among the articles referring to the interactions, Sutthibuta [27] refers to interactions only within the social aspect. This reference is also incorrect, as the ICF model does not separate the various factors that affect the functioning and disability of the individual. By definition, all factors, including the social factors, have an influence on the child’s functioning and should be taken into consideration [11,12,13].One important interaction that professionals should recognize and note is the aquatic environment. The AE provides new opportunities for various limiting physical, social and emotional conditions, so professionals should be aware of its benefits when looking at the overall changes in the child’s functioning;
- B.
- Addressing the various components of the ICF (criteria 1 and 9): The fact that the two contextual factors are the components that have been left out in most of the studies is very thought-provoking, as these two components constitute one of the essential changes that the ICF model represent, and in fact, these are the newly added components in the classification [11,18]. According to the ICF framework, “Contextual Factors represent the complete background of an individual’s life and living” [13] (p. 15). EFs are extrinsic to the individual; PFs, on the other hand, are intrinsic (and not classified in the current version of the ICF). These factors have always been part of every person’s life and somehow were ignored until the ICF was published [16]. However, without the personal and environmental background of each person, it is not possible to really understand his/her functioning and the connections between the various components of the ICF in the context of that person. It is also important to notice that the concept of “quality of life” is often associated with the ICF as one of the PF domains, as estimating quality of life is primarily a subjective issue [19,36,37].Evaluation and classification according to the ICF framework without information about the PFs and EFs of the person are deficient and do not faithfully reflect the person’s functioning [19,38]. This fact is of particular importance when investigating children’s abilities and behavior in the AE. The aquatic atmosphere is a unique environment that changes motor control ability and reduces the control of gravity over the body [10,20,23]; therefore, children require a special emotional and physical adjustment (PF) for them to act in it and cooperate;
- C.
- The ICF qualifiers (criteria 7 and 8): The qualifiers of the ICF model are very important. Their role is to enable an assessment of the range or size of functioning or the disability and the changes within the various categories of functioning and the environment. Without the qualifiers, the ICF classes have no meaning. The qualifiers make it possible to compare between the current situation and improvement or deterioration in the future. This is why when we do any assessment, the codes should be accompanied by qualifiers. [11,12,13,14,21,38]. Future articles and studies should address these issues in the same way as addressing all components and domains of the ICF, especially when linking intervention outcomes to ICF components;
- D.
- The ICF linking to another tool and ICF-based instruments, including previous articles (criteria 3, 6 and 10): The linking process provides researchers with the ability to analyze research results in terms of description, comparison, quantitative data collection and more [39,40]. The process by which it is recommended to make the link between research results and the components of the ICF is described by Cieza et al. [40,41] and discussed in Fayed et al. [42]. To achieve the desired global change and to make the ICF the key factor in clinical use for rehabilitation purposes and studies, the ICF should be part of all studies, and researchers should use linking rules for the purposes of understanding the measures and to relate them to the ICF. To do so, researchers have to agree on linkages and develop versions of currently used instruments based-on the ICF (such as the work of Güeita-Rodríguez et al. [29]), which examine all the ICF categories and domains of the individual [32,43,44,45,46,47];
- E.
- SummaryFrom the analysis of the articles, one can see that most of the authors focused mainly on the importance of the ICF framework as a common language. Unfortunately, there is a very small focus on the other area of the ICF model as a tool for evaluating functioning and disability and for monitoring progress in aquatic rehabilitation procedures (as defined in the model objectives [11,12,13]);
- F.
- Recommendations for future research arising from this review:
- 1.
- It is important to use the model as a whole, using the appropriate terminology and without omitting various components, which is disruptive to the holistic approach of the framework;
- 2.
- Researchers should be aware of the possibilities that exist in the ICF model as an evaluation tool for research interventions. Previous studies [48,49] have demonstrated the use of this model for the purposes of evaluating children as an important factor for a holistic view of the child, as a tool that enables systematic data collection and broad information and as an interprofessional language;
- 3.
- It is very important in future studies to use uniform and selective tools whenever linking the results of the various studies to the ICF fields;
- 4.
- From the current analysis and the conclusions of Nguyen et al. [16] arises an inference regarding the importance of developing orderly models that will make it easier for professionals to use the ICF as a clinical tool for setting treatment goals and indices, i.e., a tool that will use the ICF framework’s qualifiers as an important part of the evaluation system. In Appendix A, our recommendations for promoting the accessibility and use of the ICF model in AAs and research are detailed.
5. Conclusions
- This systematic review, based on the ICF reporting criteria, showed that despite the rising awareness in the field of AAs, the ICF is applied inaccurately and most often not according to the model’s biopsychosocial principles. This inaccurate and incomplete application of the ICF hampers the comparability of research and further development of aquatic activities on an international level;
- Knowledge and understanding of the model are still lacking for some researchers, as expressed in the articles by confusion between the concepts or ignoring some of the model’s components. In order for the ICF to become a guiding tool in research for the purpose of evaluations and setting goals for AAs, it seems that there is a need for broader training programs for professionals in the field of AAs, as well as in-depth familiarity with the ICF model and its goals and applications in order to allow professionals to promote and perfect their abilities using the model.
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A. Recommendations for Promoting Awareness and Use of the ICF Model in AA Interventions and Studies with Children with Developmental Delay
- Perhaps it would be useful for the ICF research and development group to develop a model with guidelines for submitting and publishing an article based on the ICF model, e.g., a list of topics (similar to the CONSORT model [50]) that would include, among other things, instruction to consider previous articles in the context the ICF framework for the specific purposes of the current article and instruction to make sure that the authors give a full explanation of the model and include the ICF reporting criteria guidelines [22], the guidelines for the linking processes [40,41], a concise definition of the model (as in the ICF introduction [12]) and more;
- It is worthwhile to build a special core set for AAs, which is uniform and relates, on the one hand, to the characteristics of the different age groups and, on the other hand, to the characteristics of the intervention in the aquatic environment (for example, a model that would unify the recommendations found in Güeita-Rodríguez et al. 2019 [30] and the ICF code sets for the children and youth of de Camargo et al. [51] or the brief common ICF core set for children and youth with cerebral palsy [52]);
- It may be worthwhile to build a “bank” of relevant definitions in order to determine functioning goals for intervention in the water environment with children with developmental delay (like the recommendations of Tesio [53]);
- To develop and promote ICF-based assessment kits for children attending AAs, so the professionals will use a uniform language for intervention and research. These assessment kits should be electronic-based in order to facilitate use and make it accessible to everyone (like the recommendations of Rauch et al. [54]);
- To develop more ICF courses for professionals all over the world;
- To translate the ICF e-learning tool of the ICF research branch [55] into many languages.
References
- Moffatt, F. The individual physical health benefits of swimming: A literature review. In The Health and Wellbeing Benefits of Swimming; Cumming, I., Ed.; Swim England’s Swimming and Health Commission: Loughborough, UK, 2017; pp. 8–25. Available online: https://www.sportengland.org/media/11765/health-and-wellbeing-benefits-of-swimming-report.pdf (accessed on 30 January 2023).
- Reid Campion, M. Introduction to hydrotherapy. In Hydrotherapy: Principles and Practice; Reid Campion, M., Ed.; Butterworth-Heinemann: Boston, MA, USA, 1997; pp. 3–30. [Google Scholar]
- Fragala-Pinkham, M.; O’Neil, M.E.; Haley, S.M. Summative evaluation of a pilot aquatic exercise program for children with disabilities. Disabil. Health J. 2010, 3, 162–170. [Google Scholar] [CrossRef] [PubMed]
- Güeita-Rodríguez, J.; García-Muro, F.; Cano-Díez, B.; Rodríguez-Fernández, Á.L.; Lambeck, J.; Palacios-Ceña, D. Identification of intervention categories for aquatic physical therapy in pediatrics using the International Classification of Functioning, Disability and Health-Children and Youth: A global expert survey. Braz. J. Phys. Ther. 2017, 21, 287–295. [Google Scholar] [CrossRef] [PubMed]
- Hillier, S.; McIntyre, A.; Plummer, L. Aquatic physical therapy for children with developmental coordination disorder: A pilot randomized controlled trial. Phys. Occup. Ther. Pediatr. 2010, 30, 111–124. [Google Scholar] [CrossRef]
- Kārkliņa, B.; Declerck, M.; Daly, D.J. Quantification of aquatic interventions in children with disabilities: A systematic literature review. Int. J. Aquat. Res. Educ. 2013, 7, 344–379. [Google Scholar] [CrossRef]
- Pan, C.Y. Effects of water exercise swimming program on aquatic skills and social behaviors in children with autism spectrum disorders. Autism 2010, 14, 9–28. [Google Scholar] [CrossRef]
- Vaščáková, T.; Kudláček, M.; Barrett, U. Halliwick Concept of Swimming and its Influence on Motoric Competencies of Children with Severe Disabilities. Eur. J. Adapt. Phys. Act. 2015, 8, 44–49. [Google Scholar] [CrossRef]
- Geytenbeek, J. Evidence for Effective Hydrotherapy. Physiotherapy 2002, 88, 514–529. [Google Scholar] [CrossRef]
- Cross, A.; Rosenbaum, P.; Gorter, J.W. Exploring the aquatic environment for disabled children: How we can conceptualize and advance interventions with the ICF. Crit. Rev. Phys. Rehabil. Med. 2013, 25, 59–76. Available online: https://www.researchgate.net/publication/274816275 (accessed on 1 January 2013). [CrossRef]
- World Health Organization. The International Classification of Functioning, Disability and Health (ICF); World Health Organization: Geneva, Switzerland, 2001. Available online: http://apps.who.int/iris/bitstream/handle/10665/42407/9241545429.pdf;jsessionid=EFB5A18701A32C05186DECC5CD1CBEB2?sequence=1 (accessed on 30 January 2023).
- World Health Organization. Towards a Common Language for Functioning, Disability and Health ICF; World Health Organization: Geneva, Switzerland, 2002. Available online: https://cdn.who.int/media/docs/default-source/classification/icf/icfbeginnersguide.pdf (accessed on 30 January 2023).
- World Health Organization. International Classification of Functioning, Disability and Health: Children and Youth Version: ICF-CY; World Health Organization: Geneva, Switzerland, 2007. Available online: http://apps.who.int/iris/bitstream/10665/43737/1/9789241547321_eng.pdf (accessed on 30 January 2023).
- Madden, R.H.; Bundy, A. The ICF has made a difference to functioning and disability measurement and statistics. Disabil. Rehabil. 2019, 41, 1450–1462. [Google Scholar] [CrossRef]
- McDougall, J.; Wright, V.; Rosenbaum, P. The ICF model of functioning and disability: Incorporating quality of life and human development. Dev. Neurorehabil. 2010, 13, 204–211. [Google Scholar] [CrossRef]
- Nguyen, T.; Stewart, D.; Rosenbaum, P.; Baptiste, S.; De Camargo, O.K.; Gorter, J.W. Using the ICF in transition research and practice? Lessons from a scoping review. Res. Dev. Disabil. 2018, 72, 225–239. [Google Scholar] [CrossRef] [PubMed]
- Moriyama, I.M.; Loy, R.M.; Robb-Smith, A.H.T. Chapter 7: Related health classifications. In History of the Statistical Classification of Diseases and Causes of Death; Rosenberg, H.M., Hoyert, D.L., Eds.; National Center for Health Statistics: Hyattsville, MD, USA, 2011; pp. 9–22. Available online: https://stacks.cdc.gov/view/cdc/5928 (accessed on 30 January 2023).
- De Camargo, O.K. The ICF and the biopsychosocial model of health: From ‘disease’ to ‘health condition’ (Section A1). In ICF a Hands-On Approach for Clinicians and Families; Simon, L., Ronen, G.M., Rosenbaum, P.L., Eds.; Mac Keith Press: London, UK, 2019; pp. 8–18. [Google Scholar]
- Leonardi, M.; Sykes, C.R.; Madden, R.C.; Ten Napel, H.; Hollenweger, J.; Snyman, S.; Madden, R.H.; De Camargo, O.K.; Raggi, A.; Van Gool, C.H.; et al. Do we really need to open a classification box on personal factors in ICF? Letter to the editor, On behalf of the Functioning and Disability Reference Group of the WHO-FIC. Disabil. Rehabil. 2016, 38, 1327–1328. [Google Scholar] [CrossRef]
- Declerck, M. Swimming and the Physical, Social and Emotional Well-Being of Youth with Cerebral Palsy. Ph.D. Thesis, University of Edinburgh, Edinburgh, Scotland, 4 July 2014. Available online: http://hdl.handle.net/1842/9459 (accessed on 26 September 2014).
- World Health Organization. How to Use the ICF: A Practical Manual for Using the International Classification of Functioning, Disability and Health (ICF); Exposure Draft for Comment; World Health Organization: Geneva, Switzerland, 2013. Available online: https://www.who.int/publications/m/item/how-to-use-the-icf---a-practical-manual-for-using-the-international-classification-of-functioning-disability-and-health (accessed on 1 October 2013).
- Daugaard, R.; Sykes, C.; Van Gool, C.H.; Saleeby, P.W.; Maribo, T. ICF Reporting Criteria: Guidelines for quality reporting on use of ICF. In Proceedings of the WHO-FIC Network Annual Meeting, Seoul, Republic of Korea, 22–27 October 2018; Available online: https://www.reteclassificazioni.it/download_doc.php?uuid=facb3e21-ea8b-41eb-b9ce-5f1b468035eb (accessed on 30 January 2023).
- Saleeby, P.; Sykes, C.; Martinuzzi, A.; Hough, J.; Lee, H.; Leonardi, M.; Leplege, A.; Maribo, T.; Ten Napel, H.; Paltarnaa, J.; et al. Developing Criteria to Evaluate ICF Literature. In Proceedings of the WHO-FIC Network Annual Meeting, Barcelona, Spain, 11–17 October 2014; Available online: https://www.researchgate.net/publication/271385535_Development_of_Criteria_to_Review_ICF_Literature (accessed on 1 October 2014).
- Prodinger, B.; Tennant, A.; Stucki, G. Standardized reporting of functioning information on ICF-based common metrics. Eur. J. Phys. Rehabil. Med. 2018, 54, 110–117. [Google Scholar] [CrossRef] [PubMed]
- Gorter, J.W.; Currie, S.J. Aquatic exercise programs for children and adolescents with cerebral palsy: What do we know and where do we go? Int. J. Pediatr. 2011, 2011, 712165. [Google Scholar] [CrossRef]
- Blohm, D. Effectiveness of aquatic interventions for children with cerebral palsy: Systematic review of current literature. J. Aquatic Phys. Ther. 2011, 19, 19–29. [Google Scholar]
- Sutthibuta, U. Systematic review of aquatic exercise programming for children and adolescents with cerebral palsy. Int. J. Child Dev. Ment. Health 2014, 2, 49–66. Available online: https://he01.tci-thaijo.org/index.php/cdmh/article/view/66618 (accessed on 30 January 2014).
- Khalaji, M.; Kalantari, M.; Shafiee, Z.; Hosseini, M.A. The effect of hydrotherapy on health of cerebral palsy patients: An integrative review. Iran. Rehabil. J. 2017, 15, 173–180. [Google Scholar] [CrossRef]
- Güeita-Rodríguez, J.; García-Muro, F.; Rodríguez-Fernández, Á.L.; Lambeck, J.; Fernández-De-Las-Peñas, C.; Palacios-Ceña, D. What areas of functioning are influenced by aquatic physiotherapy? Experiences of parents of children with cerebral palsy. Dev. Neurorehabil. 2018, 21, 506–514. [Google Scholar] [CrossRef]
- Güeita-Rodríguez, J.; García-Muro, F.; Rodríguez-Fernández, Á.L.; Cano-Díez, B.; Chávez-Santacruz, D.; Palacios-Ceña, D. Preliminary aquatic physical therapy core sets for children and youth with neurological disorders: A consensus process. Pediatr. Phys. Ther. 2019, 31, 272–278. [Google Scholar] [CrossRef]
- Schiariti, V.; Selb, M.; Cieza, A.; O’Donnell, M. International Classification of Functioning, Disability and Health Core Sets for children and youth with cerebral palsy: A consensus meeting. Dev. Med. Child Neurol. 2015, 57, 149–158. [Google Scholar] [CrossRef]
- Selb, M.; Escorpizo, R.; Kostanjsek, N.; Stucki, G.; Üstün, B.; Cieza, A. A guide on how to develop an International Classification of Functioning, Disability and Health Core Set. Eur. J. Phys. Rehabil. Med. 2015, 51, 105–117. [Google Scholar] [PubMed]
- Stucki, G.; Sangha, O. Principles of rehabilitation. In Rheumatology, 2nd ed.; Klippel, J.H., Dieppe, P.A., Eds.; Mosby Elsevier: London, UK, 1998; pp. 1–11. [Google Scholar]
- Duffield, C. The Delphi technique: A comparison of results obtained using two expert panels. Int. J. Nurs. Stud. 1993, 30, 227–237. [Google Scholar] [CrossRef]
- Kostanjsek, N. Use of The International Classification of Functioning, Disability and Health (ICF) as a conceptual framework and common language for disability statistics and health information systems. BMC Public Health 2011, 11 (Suppl. S4), 1–6. [Google Scholar] [CrossRef] [PubMed]
- De Camargo, O.K. Personal factors in clinical practice and public health. (Section A3). In ICF a Hands-On Approach for Clinicians and Families; De Camargo, O.K., Simon, L., Ronen, G.M., Rosenbaum, P.L., Eds.; Mac Keith Press: London, UK, 2019; pp. 25–36. [Google Scholar]
- Patel, K.; Straudi, S.; Yee Sien, N.; Fayed, N.; Melvin, J.L.; Sivan, M. Applying the WHO ICF framework to the outcome measures used in the evaluation of long-term clinical outcomes in coronavirus outbreaks. Int. J. Environ. Res. Public Health 2020, 17, 6476. [Google Scholar] [CrossRef] [PubMed]
- Kohler, F.; Connolly, C.; Sakaria, A.; Stendara, K.; Buhagiar, M.; Mojaddidi, M. Can the ICF be used as a rehabilitation outcome measure? A study looking at the inter- and intra-rater reliability of ICF categories derived from an ADL assessment tool. J. Rehabil. Med. 2013, 45, 881–887. [Google Scholar] [CrossRef] [PubMed]
- Lustenberger, N.A.; Prodinger, B.; Dorjbal, D.; Rubinelli, S.; Schmitt, K.; Scheel-Sailer, A. Compiling standardized information from clinical practice: Using content analysis and ICF linking rules in a goal-oriented youth rehabilitation program. Disabil. Rehabil. 2019, 41, 613–621. [Google Scholar] [CrossRef]
- Cieza, A.; Fayed, N.; Bickenbach, J.; Prodinger, B. Refinements of the ICF Linking Rules to strengthen their potential for establishing comparability of health information. Disabil. Rehabil. 2019, 41, 574–583. [Google Scholar] [CrossRef]
- Cieza, A.; Geyh, S.; Chatterji, S.; Kostanjsek, N.; Ustun, B.; Stucki, G. ICF Linking Rules: An update based on lessons learned. J. Rehabil. Med. 2005, 37, 212–218. [Google Scholar] [CrossRef]
- Fayed, N.; Cieza, A.; Edmond Bickenbach, J. Linking health and health-related information to the ICF: A systematic review of the literature from 2001 to 2008. Disabil. Rehabil. 2011, 33, 1941–1951. [Google Scholar] [CrossRef]
- Foley, K.R.; Dyke, P.; Girdler, S.; Bourke, J.; Leonard, H. Young adults with intellectual disability transitioning from school to post-school: A literature review framed within the ICF. Disabil. Rehabil. 2012, 34, 1747–1764. [Google Scholar] [CrossRef]
- Stucki, G.; Ewert, T.; Cieza, A. Value and application of the ICF in rehabilitation medicine. Disabil. Rehabil. 2003, 25, 628–634. [Google Scholar] [CrossRef] [PubMed]
- Stucki, G.; Cieza, A.; Ewert, T.; Kostanjsek, N.; Chatterji, S.; Ustun, T.B. Application of the International Classification of Functioning, Disability and Health (ICF) in clinical practice. Disabil. Rehabil. 2002, 24, 281–282. [Google Scholar] [CrossRef]
- Lexell, J.; Brogårdh, C. The use of ICF in the neurorehabilitation process. NeuroRehabilitation 2015, 36, 5–9. [Google Scholar] [CrossRef]
- Ballert, C.S.; Hopfe, M.; Kus, S.; Mader, L.; Prodinger, B. Using the refined ICF Linking Rules to compare the content of existing instruments and assessments: A systematic review and exemplary analysis of instruments measuring participation. Disabil. Rehabil. 2019, 41, 584–600. [Google Scholar] [CrossRef] [PubMed]
- Jelsma, J.; Scott, D. Impact of using the ICF framework as an assessment tool for students in paediatric physiotherapy: A preliminary study. Physiotherapy 2011, 97, 47–54. [Google Scholar] [CrossRef] [PubMed]
- Schiariti, V.; Klassen, A.F.; Cieza, A.; Sauve, K.; O’Donnell, M.; Armstrong, R.; Mâsse, L.C. Comparing contents of outcome measures in cerebral palsy using the International Classification of Functioning (ICF-CY): A systematic review. Eur. J. Paediatr. Neurol. 2014, 18, 1–12. [Google Scholar] [CrossRef]
- Falci, S.G.; Marques, L.S. CONSORT: When and how to use it. Dent. Press J. Orthod. 2015, 20, 13–15. [Google Scholar] [CrossRef]
- ICF code sets for children and youth (Appendix 6). ICF: A Hands-On Approach for Clinicians and Families; de Camargo, O.K., Simon, L., Ronen, G.M., Rosenbaum, P.L., Eds.; Mac Keith Press: London, UK, 2019; pp. 1–11. ISBN 9781911612049. [Google Scholar]
- Schiariti, V.; Longo, E.; Shoshmin, A.; Kozhushko, L.; Besstrashnova, Y.; Król, M.; Neri Correia Campos, T.; Náryma Confessor Ferreira, H.; Verissimo, C.; Shaba, D.; et al. Implementation of the International Classification of Functioning, Disability, and Health (ICF) Core Sets for Children and Youth with Cerebral Palsy: Global Initiatives Promoting Optimal Functioning. Int. J. Environ. Res. Public Health 2018, 15, 1899. [Google Scholar] [CrossRef]
- Tesio, L. From codes to language: Is the ICF a classification system or a dictionary? BMC Public Health 2011, 11 (Suppl. S4), 1–4. [Google Scholar] [CrossRef]
- Rauch, A.; Cieza, A.; Stucki, G. How to apply the International Classification of Functioning, Disability and Health (ICF) for rehabilitation management in clinical practice. Eur. J. Phys. Rehabil. Med. 2008, 44, 329–342. Available online: https://www.researchgate.net/publication/23229007 (accessed on 1 October 2008).
- The ICF e-Learning Tool. 2022. Available online: https://www.icf-elearning.com/ (accessed on 30 January 2023).

| and | A child/children with developmental delays Aged 6–12 | and | ICF |
| First Named Author and Year | Type and Aim | Study Population | Interventions | Measures | Results |
|---|---|---|---|---|---|
| Blohm, 2011 [26] | A literature review of 8 articles aimed to review the available evidence regarding the effectiveness of aquatic interventions for children with CP. | 113 children or adolescents (ages 3–20) with CP. | Vary from AE sessions 2× weekly to AE combined with swimming sessions. | The ICF-CY framework was used in order to check the outcome measures and results. ICF-CY components examined: BF, A&P. | Ambulatory children and adolescents with CP clearly benefited from aquatic intervention programs in terms of ICF levels—BF, Act. and/or Par. The improvements were sustained several weeks after completion of a program, while others regressed to baseline values. No adverse effects of APT were presented. |
| Gorter and Currie, 2011 [25] | A literature review of 6 articles aimed to review published literature since 2005, with a focus on AE for children with CP. | 45 children and adolescents with spastic CP and other developmental disabilities. Ages 2–21. | Aerobic exercises, strength exercises and other activities that do not fall under any of the above categories. | The ICF-CY framework was used in order to classify the impact of health conditions according to the effect of the ICF-CY components BF, BS, A&P. | Researchers found evidence on effectiveness of AE in children and adolescents with CP are limited. There is a strong potential for aquatic physical activity to benefit children and adolescents with CP. |
| Cross et al., 2013 [10] | A scoping review of 23 articles aimed to (1) summarize and disseminate the research findings on aquatic interventions for children with disabilities; (2) identify the recurring issues within the pediatric aquatic literature; and (3) investigate the potential utility of ICF as part of the promotion processes of aquatic interventions for children with disabilities. | 382 children with disabilities aged 2–12. | Vary from AE, therapy or structured swimming sessions. | The ICF-CY framework was used in order to check the outcome measures and results. ICF components examined: BF, A&P. | The ICF provides a common framework that can enhance communication among aquatic researchers, practitioners, families and policy- and decision-makers, in turn leading to the development of evidence-based aquatic interventions. |
| Declerck, 2014 [20] | An RCT–cross-over design article that aimed to investigate the effect of swimming on the multiple aspects of functioning at different levels of the ICF framework among ambulant youth with CP. | 14 youth with CP, ages 7–17. | A 10-week swimming program in the community. Two sessions per week (30 to 60 min.). All sessions consisted of a 5-to-10 min warm-up, 20 to 40 min of learning new tasks and 5 to 10 min of free play, races and other games. | VAS; Faces Pain Scale—Revised; 10-meter walk test; 1 min fast walk test; PedsQLTM multidimensional fatigue scale; Bruininks–Oseretsky test of motor proficiency; PEDI-NL; Self-Perception Profile for youth with CP; PedsQL™ CP module version 3.0; WOTA 2; 5-point Likert scale; CAPE. | All youth had a high adherence towards the program; they participated in the intervention with high levels of enjoyment, and most youth continued to participate in swimming after completing the program. The intervention had a positive influence on their BF and A&P. One year after the start of the study, they participated in activities of the formal domain and in skill-based activities more with friends and others than with family or alone. |
| Sutthibuta, 2014 [27] | A systematic review of 3 articles aimed to review the literature according to ICF-CY for clinical applications, further research and practice. | 57 children and adolescents with CP aged 6–21. | Different AEs. | Cardiorespiratory endurance; muscle strength; gait analysis; Floor to Stand; PEDI; GMFM; WOTA. | It was shown that the previous studies were not enough to verify the effectiveness of hydrotherapy. |
| Güeita-Rodríguez et al., 2017 [4] | An experts’ opinion article aimed to identify intervention categories encountered by PTs working in aquatic therapy with disabled children using the ICF-CY. | 69 experts (APTs) with experience in AAs for children with disabilities. | The study relied on established linking rules in order to link participants’ responses to the ICF-CY. The ICF-CY language was used to provide a summary of the participants’ answers to questionnaires, and calibration linking was performed by two different health professionals who were trained in ICF-CY linking. | A Delphi consensus process. Response rates were analyzed using descriptive statistics. | A total of 99 ICF-CY categories were identified, which were divided into 4 ICF-CY components as follows: 41 BF, 8 BS, 36 A&P and 14 EF. Regarding the influence of aquatic therapy upon EFs, there was a notable consensus regarding the support, relationships and attitudes of family members. |
| Khalaji et al., 2017 [28] | An integrative review aimed to review the extant literature in the field of hydrotherapy and its applications for the improvement of ICF in spastic diplegia CP patients. | Children with spastic diplegia CP, aged 4–21. | Different types of hydrotherapy. | The ICF-CY framework was used in order to check the outcome measures and results. ICF components examined: BF, A&P. | Hydrotherapy, when administered with conventional methods for rehabilitation of children and adolescents with spastic diplegia CP, has positive effects on all areas of ICF. The exercises and their duration and intensity should be decided on the basis of the physical and cognitive conditions of the patients. |
| Güeita-Rodríguez et al., 2018 [29] | An integrative review aimed to explore the experiences regarding aquatic physiotherapy among parents of children with CP and to identify a list of relevant intervention categories for aquatic physiotherapy treatments. | 18 parents of children with CP. | Semistructured interviews and focus groups based on the components of the ICF as a frame of reference to explore and code experiences regarding aquatic physiotherapy. | A questionnaire for parents with a topic guide was developed based on the five ICF components. The identified findings of this questionnaire were organized by ICF-CY component and linked to the ICF-CY categories according to established linking rules. | A total of 107 ICF-CY linkages were performed: 42 categories of BF, 12 BS, 42 AP and 11 EF. Parents stressed the importance of AE for their children’s muscle functions and balance as well as for family and social relations and that the current services, systems and health policies represent a barrier for the practice of APT with their children. These results could be included in goal-setting and may enable APTs to develop treatment-based classification systems. |
| Güeita-Rodríguez et al., 2019 [30] | A consensus process to report on the preliminary APT CS for children and youth with neurological disorders using the ICF-CY version. | 15 experts (APTs) who had over 5 years of experience working in water with children and youth with neurological disorders. | A Delphi consensus process that was undertaken in two languages (English and Spanish). The process was completed when a consensus was reached between the experts. | A consensus agreement among the experts was set in a Delphi consensus process. | 1. A comprehensive APT CS for children and youth with neurological disorders that included 64 different ICF-CY categories. These 64 categories represent 3.79% of all categories included in the ICF-CY classification; 2. Four brief APT CSs: APT CS aged 9 to 18 years; APT CS for the ages of 0 to less than 6 years; APT CS aged 6 to less than 14 years; APT CS aged 14 to 18 years. |
| ICF Reporting Criteria | Blohm [25] | Gorter and Currie [26] | Cross et al. [10] | Declerck [20] | Sutthibuta [27] | Güeita-Rodríguez et al. [4] | Khalaji et al. [28] | Güeita-Rodríguez et al. [29] | Güeita-Rodríguez et al. [30] | |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Are all components of the ICF framework considered? | No | Yes | Partially. All components are mentioned; only 5 of them are referred to. | Yes | Partially. All components are mentioned; only 4 of them are referred to. | No | No | No | No |
| 1.1 | Which components are NOT considered? | BS, PF, EF | PF | PF, EF | PF | Par. (may be included in Act.), PF. | PF | PF | ||
| 1.2 | Reasons for excluding components are explained? | No | No | No | PF categories are not classified to date. | No | PF categories are not classified to date. | PF categories are not classified to date. | ||
| 2 | The interactions in ICF are considered? 2.1 ICF interactions are discussed? | No | No | Yes | Yes | Partially. The model was explained, but the focus is only on the social part. | No | No | No | No |
| 3 | Demonstrated awareness of the literature predating the study and relevant reference to ICF literature is provided? | Yes | Yes | Yes | Yes | Yes | Yes | Partially. There is no literature reference regarding ICF. | Yes | Yes |
| 4 | Explicit references to ICF definitions and categories are included? | No | Yes | Yes | Yes | No | Yes | No | Yes | Yes |
| 5 | Consistent use of ICF language is demonstrated? | No. Mixing concepts between ICF components and “Levels”. | No. Mixing concepts between ICF components and “categories”. | Partially. Mixing concepts between ICF domains and “categories”. “Disability” is used incorrectly—”Children with disabilities”. | Partially. Mixing concepts between ICF “domains” and “categories”. “Disability” is used as a word that describes a health status. | Yes | Yes | Partially. Mixing concepts between ICF “domains” and “areas”. | Yes | Yes |
| 6 | Where ICF is linked/mapped to another tool, description of the methodology is given? | No | Partially. There are examples of results linked to ICF’s components, but no explanation of the methodology. | Partially. A short description of the matching of outcomes to the ICF components. No explanation of the methodology. | No | No | Yes | Partially. There are examples of results linked to ICF’s components, but no explanation of the methodology. | Yes | Yes |
| 7 | If there is linkage between ICF qualifiers and other measures, description of the methodology is given? | No linkage | Partially. Only the term “barriers”. No linkage methodology was given. | No linkage. | No linkage. | No linkage. | Partially. A brief reference on capacity and performance. | No linkage. | Partially. A reference to the term “Barriers”. No linkage methodology was given. | Partially. A brief explanation of the numerical marking method and of “capacity” and “performance”. |
| 8 | Description of the use of ICF qualifiers, e.g., five-point scale, three-point scale, present? | No | No | No | No | No | No | No | Partially. Mention the 5-point scale and the term “Barriers” with no description. | Partially. A brief description of the numerical marking method. |
| 8.1 | Description of the reason for selection of qualifier use is provided? | No | No | No | No | No | No | No | No | No |
| 9 | The person’s perspective is recognized in the reporting? | No | Yes | Not really. Just an incidental mention. | Yes | Not really. Just mention it. | No | No | Yes. With parents’ opinions of their children’s needs. | Maybe. Age-specific ATP-CS groups. For purposes of their use in studies. |
| 10 | The relationship between the ICF and an ICF-based instrument is described? | No | No | Yes. The ICF as a tool to classify the various outcome measures. | Yes. The multiple facets of functioning in addition to quality of life. | No | Yes. Using the Delphi consensus process with ICF-CS to identify relevant intervention categories for APT. | No | Yes. The interview guide for parents—abilities of the children’s functioning were linked to the ICF components. | Yes. The APT CSs—a standard of functioning for the use in AT for children and youth. |
| 11 | Knowledge translation between different settings is discussed? | No | No | Yes. ICF common language for researchers and interventions. | Yes. ICF linkage to children functioning; ICF as a tool for understanding the relationships between the components found in research. | Yes. The AT activities and QoL is consistent with the ICF framework. | Yes. The Delphi consensus process with standardized WHO methodology for ICF-CSs relevant to APT treatments. | No | Yes. The ICF-CY as a reference for parent interview guide. | Yes. ICF-CY APT- CSs development process that included gathering knowledge from previous studies and an experts’ consensus process based on the Delphi method. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hadar-Frumer, M.; Ten Napel, H.; Yuste-Sánchez, M.J.; Rodríguez-Costa, I. The International Classification of Functioning, Disability and Health: Accuracy in Aquatic Activities Reports among Children with Developmental Delay. Children 2023, 10, 908. https://doi.org/10.3390/children10050908
Hadar-Frumer M, Ten Napel H, Yuste-Sánchez MJ, Rodríguez-Costa I. The International Classification of Functioning, Disability and Health: Accuracy in Aquatic Activities Reports among Children with Developmental Delay. Children. 2023; 10(5):908. https://doi.org/10.3390/children10050908
Chicago/Turabian StyleHadar-Frumer, Merav, Huib Ten Napel, Maria José Yuste-Sánchez, and Isabel Rodríguez-Costa. 2023. "The International Classification of Functioning, Disability and Health: Accuracy in Aquatic Activities Reports among Children with Developmental Delay" Children 10, no. 5: 908. https://doi.org/10.3390/children10050908
APA StyleHadar-Frumer, M., Ten Napel, H., Yuste-Sánchez, M. J., & Rodríguez-Costa, I. (2023). The International Classification of Functioning, Disability and Health: Accuracy in Aquatic Activities Reports among Children with Developmental Delay. Children, 10(5), 908. https://doi.org/10.3390/children10050908






