A Systematic Review of the Clinical Diagnosis of Transient Hypogammaglobulinemia of Infancy
Abstract
:1. Introduction
1.1. Research Question
1.2. Research Aims and Objectives
- To systematically review the diagnostic criteria for THI.
- To identify gaps in the existing literature related to the diagnostic criteria for THI.
2. Methodology
2.1. Eligibility Criteria
2.2. Exclusion Criteria
- Infants diagnosed after 36 months (three years);
- Studies that did not use a screening tool/criterion to diagnose;
- Studies that were abstracts only (i.e., did not include the full text).
2.3. Information Sources
2.4. Search Strategy
- Screening tool OR diagnosis AND transient hypogammaglobulinemia AND infants;
- Transient hypogammaglobulinemia of infancy AND diagnosis.
2.5. Selection Process
2.6. Data Collection Process
2.7. Study Risk of Bias Assessment
2.8. Ethical Considerations
3. Results
3.1. Study Characteristics
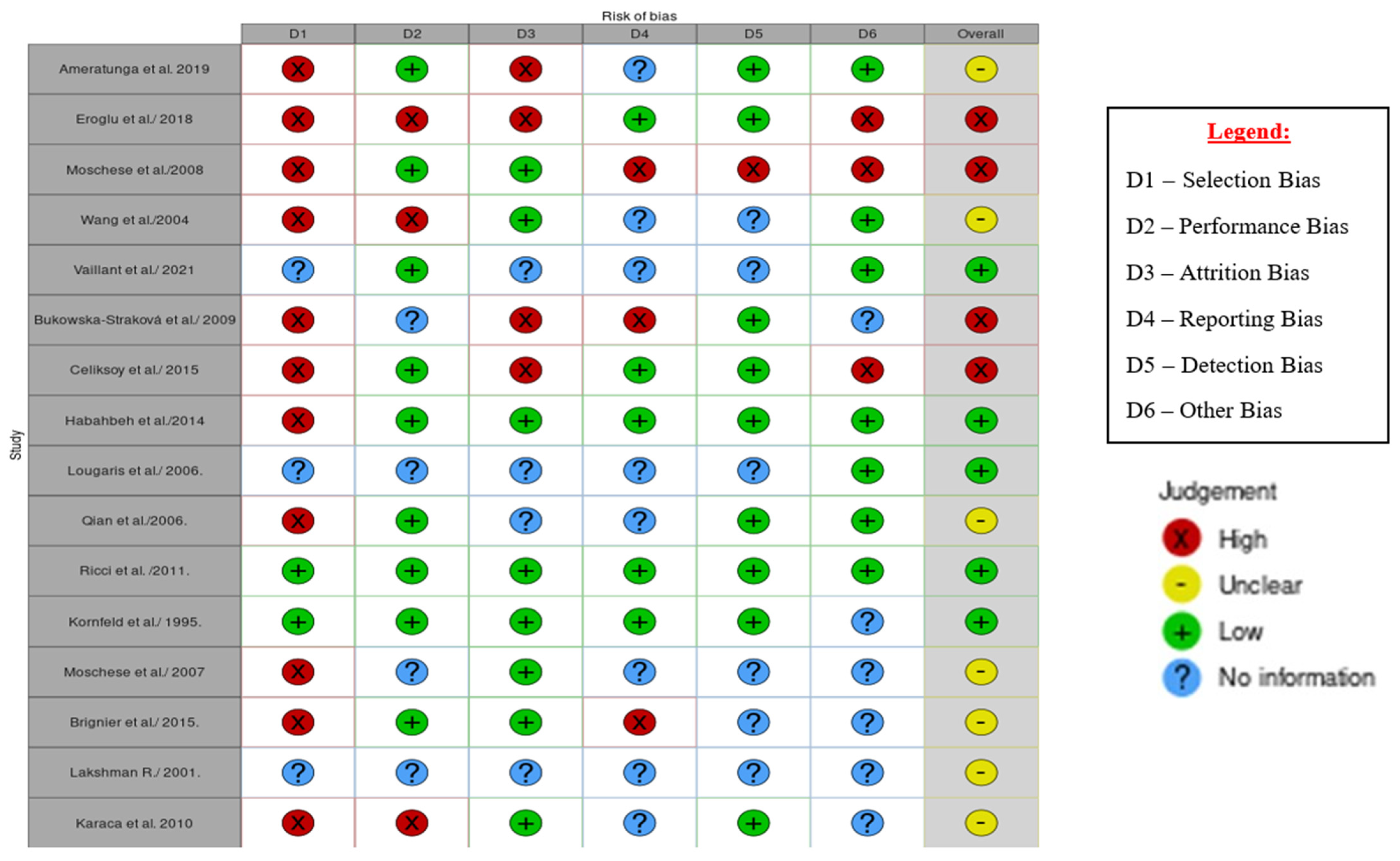
3.2. Risk of Bias in Studies
4. Discussion
- Onset of immunodeficiency at greater than 2 years of age
- Absent isohaemagglutinins and/or poor response to vaccines
- Defined causes of hypogammaglobulinemia were excluded according to a list of differential diagnosis” [26].
- Prematurity (very low IgG levels at birth);
- Inclusion of hypogammaglobulinemic children beyond 2 years of age;
- Selection of neonates or infants with a family history of immunodeficiency;
- Inconsistencies in the immunoglobulin evaluation;
- Inconsistencies in the selection of cases and their differential diagnosis.
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Vaillant, A.A.J.; Wilson, A.M. Transient Hypogammaglobulinemia of Infancy. StatPearls Internet. 2021. Available online: https://www.ncbi.nlm.nih.gov/books/NBK544356/ (accessed on 29 September 2021).
- Knutsen, A. Transient Hypogammaglobulinemia of Infancy: Background, Pathophysiology, Epidemiology. Transient Hypogammaglobulinemia of Infancy. 2019. Available online: https://emedicine.medscape.com/article/888706-overview#a4 (accessed on 20 March 2022).
- Ameratunga, R.; Ahn, Y.; Steele, R.; Woon, S.-T. Transient hypogammaglobulinaemia of infancy: Many patients recover in adolescence and adulthood. Clin. Exp. Immunol. 2019, 198, 224–232. [Google Scholar] [CrossRef]
- Moschese, V.; Graziani, S.; Avanzini, M.A.; Carsetti, R.; Marconi, M.; La Rocca, M.; Chini, L.; Pignata, C.; Soresina, A.R.; Consolini, R.; et al. A Prospective Study on Children with Initial Diagnosis of Transient Hypogammaglobulinemia of Infancy: Results from the Italian Primary Immunodeficiency Network. Available online: https://pubmed.ncbi.nlm.nih.gov/18547478/ (accessed on 21 September 2021).
- Immune Deficiency Foundation. Available online: https://primaryimmune.org/ (accessed on 21 September 2021).
- Duse, M.; Lacobini, M.; Leonardi, L.; Smacchia, P.; Antonetti, L.; Giancane, G. Transient Hypogammaglobulinemia of Infancy: Intravenous Immunoglobulin as First Line Therapy. Available online: https://pubmed.ncbi.nlm.nih.gov/20378022/ (accessed on 29 September 2021).
- Wang, L.J.; Yang, Y.H.; Lin, Y.T.; Chiang, B.L. Immunological and Clinical Features of Pediatric Patients with Primary Hypogammaglobulinemia in Taiwan. Available online: https://pubmed.ncbi.nlm.nih.gov/15366655/ (accessed on 29 March 2022).
- Data Collection form for Intervention Reviews for RCTs & Non-RCTs-Template. Cochrane Developmental, Psychosocial & Learning Problem. Available online: https://dplp.cochrane.org/data-extraction-forms (accessed on 17 April 2022).
- McGuinness, L.A.; Higgins, J.P.T. Risk-of-bias VISualization (robvis): An R package and Shiny web app for visualizing risk-of-bias assessments. Res. Synth. Methods 2021, 12, 55–61. [Google Scholar] [CrossRef]
- Cipe, F.E.; Doğu, F.; Güloğlu, D.; Aytekin, C.; Polat, M.; Biyikli, Z.; Ikincioğullari, A. B-cell subsets in patients with transient hypogammaglobulinemia of infancy, partial IgA deficiency, and selective IgM deficiency. J. Investig. Allergol. Clin. Immunol. 2013, 23, 94–100. [Google Scholar]
- Eroglu, F.K.; Kaya, F.A.; Cagdas, D.; Özgür, T.T.; Yılmaz, T.; Tezcan, İ.; Sanal, Ö. B lymphocyte subsets and outcomes in patients with an initial diagnosis of transient hypogammaglobulinemia of infancy. Scand. J. Immunol. 2018, 88, e12709. [Google Scholar] [CrossRef]
- Celiksoy, M.H.; Yildiran, A. A Comparison of B Cell Subsets in Primary Immune Deficiencies that Progress with Antibody Deficiency and Age-Matched Healthy Children. Available online: https://www.elsevier.es/en-revista-allergologia-et-immunopathologia-105-pdf-S0301054616000094 (accessed on 29 April 2022).
- Karaca, N.E.; Aksu, G.; Gulez, N.; Yildiz, B.; Azarsiz, E.; Kutukculer, N. New Laboratory Findings in Turkish Patients with Transient Hypogammaglobulinemia of Infancy. Iran. J. Allergy Asthma Immunol. 2010, 9, 237–243. [Google Scholar]
- Moschese, V.; Carsetti, R.; Graziani, S.; Chini, L.; Soresina, A.R.; La Rocca, M.; Bossi, G.; Di Cesare, S.; Plebani, A. Memory B-cell subsets as a predictive marker of outcome in hypogammaglobulinemia during infancy. J. Allergy Clin. Immunol. 2007, 120, 474–476. [Google Scholar] [CrossRef]
- Lougaris, V.; Soresina, A.; Meini, A.; Vettore, E.; Cattaneo, G.; Plebani, A. Diagnostic Criteria of Hypogammaglobulinemia in infancy. In Proceedings of the VTH International Neonatal Hematology and Immunology Meeting, Boston, MA, USA, 2006; Volume 2, pp. 16–17. Available online: https://www.pagepress.org/journals/index.php/hmr/article/view/446 (accessed on 13 April 2022).
- Ricci, G.; Piccinno, V.; Giannetti, A.; Miniaci, A.; Specchia, F.; Masi, M. Evolution of Hypogammaglobulinemia in Premature and Full-Term Infants. Int. J. Immunopathol. Pharmacol. 2011, 24, 721–726. [Google Scholar] [CrossRef]
- Bukowska-Straková, K.; Kowalczyk, D.; Baran, J.; Siedlar, M.; Kobylarz, K.; Zembala, M. The B-cell Compartment in the Peripheral Blood of Children With Different Types of Primary Humoral Immunodeficiency. Pediatr. Res. 2009, 66, 28–34. [Google Scholar] [CrossRef] [Green Version]
- Habahbeh, Z.M.; Abu-Shukair, M.E.; Almutereen, M.A.; Alzyoud, R.M.; Wahadneh, A.M. Primary Antibody Deficiencies at Queen Rania Children Hospital in Jordan: Single Center Experience. Iran. J. Immunol. 2014, 11, 49–58. [Google Scholar]
- Qian, J.H.; Chen, T.X.; Zhu, J.X.; Zhu, X.D. Clinical Features and Follow-up of Chinese Patients with Symptomatic Hypogammaglobulinemia in Infancy. Chin. Med. J. 2009, 122, 1877–1887. Available online: https://journals.lww.com/cmj/Fulltext/2009/08020/Clinical_features_and_follow_up_of_Chinese.8.aspx (accessed on 25 March 2022).
- Kornfeld, S.J.; Kratz, J.; Haire, R.N.; Litman, G.W.; Good, R.A. X-linked agammaglobulinemia presenting as transient hypogammaglobulinemia of infancy. J. Allergy Clin. Immunol. 1995, 95, 915–917. [Google Scholar] [CrossRef]
- Brignier, A.C.; Mahlaoui, N.; Reimann, C.; Picard, C.; Kracker, S.; de Vergnes, N.; Rieux-Laucatet, F.; Frange, P.; Suarez, F.; Neven, B.; et al. Early-onset hypogammaglobulinemia: A survey of 44 patients. J. Allergy Clin. Immunol. 2015, 136, 1097–1099. [Google Scholar] [CrossRef]
- Lakshman, R. Indian Pediatrics—Personal Practice. Available online: https://www.indianpediatrics.net/aug2001/aug-864-871.htm (accessed on 25 March 2022).
- ESID—European Society for Immunodeficiencies. Available online: https://esid.org/Education/Diagnostic-Criteria-PID (accessed on 17 May 2022).
- Conley, M.E.; Notarangelo, L.D.; Etzioni, A. Diagnostic Criteria for Primary Immunodeficiencies. Clin. Immunol. 1999, 93, 190–197. [Google Scholar] [CrossRef]
- Picard, C.; Bobby Gaspar, H.; Al-Herz, W.; Bousfiha, A.; Casanova, J.L.; Chatila, T.; Crow, Y.J.; Cunningham-Rundles, C.; Etzioni, A.; Franco, J.L.; et al. International Union of Immunological Societies: 2017 Primary Immunodeficiency Diseases Committee Report on Inborn Errors of Immunity. J. Clin. Immunol. 2018, 38, 96–128. [Google Scholar] [CrossRef] [Green Version]
- Bonilla, F.A.; Barlan, I.; Chapel, H.; Costa-Carvalho, B.T.; Cunningham-Rundles, C.; de la Morena, M.T.; Espinosa-Rosales, F.J.; Hammarström, L.; Nonoyama, S.; Quinti, I.; et al. International Consensus Document (ICON): Common Variable Immunodeficiency Disorders. J. Allergy Clin. Immunol. Pract. 2016, 4, 38–59. [Google Scholar] [CrossRef] [Green Version]
- Bundy, V.; Barbieri, K.; Keller, M. Primary Immunodeficiency: Overview of Management. UpTo-Date. 2021. Available online: https://www.uptodate.com/contents (accessed on 29 April 2022).
- Siegel, R.L.; Issekutz, T.; Schwaber, J.; Rosen, F.S.; Geha, R.S. Deficiency of T helper cells in transient hypogammaglobulinemia of infancy. N. Engl. J. Med. 1981, 305, 1307–1313. [Google Scholar] [CrossRef]
- Sütçü, M.; Aktürk, H.; Salman, N.; Özçeker, D.; Gülümser-Şişko, S.; Acar, M.; Somer, A. Transient hypogammaglobulinemia of infancy: Predictive factors for late recovery. Turk. J. Pediatr. 2015, 57, 592–598. [Google Scholar]
- Walker, A.M.; Kemp, A.S.; Hill, D.J.; Shelton, M.J. Features of transient hypogammaglobulinaemia in infants screened for immunological abnormalities. Arch. Dis. Child. 1994, 70, 183–186. [Google Scholar] [CrossRef] [Green Version]
- Tiller, T.L., Jr.; Buckley, R.H. Transient hypogammaglobulinemia of infancy: Review of the literature, clinical and immunologic features of 11 new cases, and long-term follow-up. J. Pediatr. 1978, 92, 347–353. [Google Scholar] [CrossRef]
- Singh, S.; Bansal, A. Transient Hypogammaglobulinemia of Infancy: Twelve years’ experience from Northern India. Pedriatic Asthma Allergy Immunol. 2005, 18, 77–81. [Google Scholar] [CrossRef]
- McGeady, S.J. Transient Hypogammaglobulinemia of Infancy. In Stiehm’s Immune Deficiencies; Kathleen, E., Sullivan, E., Richard, S., Eds.; Academic Press: Cambridge, MA, USA, 2014; pp. 417–426. ISBN 9780124055469. [Google Scholar]
- Speletas, M.; Mamara, A.; Papadopoulou-Alataki, E.; Iordanakis, G.; Liadaki, K.; Bardaka, F.; Kanariou, M.; Germenis, A.E. TNFRSF13B/TACI alterations in Greek patients with antibody deficiencies. J. Clin. Immunol. 2011, 31, 550–559. [Google Scholar] [CrossRef]
- Ameratunga, R.; Woon, S.T.; Gillis, D.; Koopmans, W.; Steele, R. New diagnostic criteria for common variable immune deficiency (CVID), which may assist with decisions to treat with intravenous or subcutaneous immunoglobulin. Clin. Exp. Immunol. 2013, 174, 203–211. [Google Scholar] [CrossRef]
- Picard, C.; Al-Herz, W.; Bousfiha, A.; Casanova, J.L.; Chatila, T.; Conley, M.E.; Cunningham-Rundles, C.; Etzioni, A.; Holland, S.M.; Klein, C.; et al. Primary Immunodeficiency Diseases: An Update on the Classification from the International Union of Immunological Societies Expert Committee for Primary Immunodeficiency 2015. J. Clin. Immunol. 2015, 35, 696–726. [Google Scholar] [CrossRef] [Green Version]
- Cavaliere, F.M.; Milito, C.; Martini, H.; Schlesier, M.; Dräger, R.; Schütz, K.; Brunetti, G.; Pesce, A.M.; Thon, V.; Warnatz, K.; et al. Quantification of IgM and IgA anti-pneumococcal capsular polysaccharides by a new ELISA assay: A valuable diagnostic and prognostic tool for common variable immunodeficiency. J. Clin. Immunol. 2013, 33, 838–846. [Google Scholar] [CrossRef]
- Pulvirenti, F.; Milito, C.; Cavaliere, F.M.; Mezzaroma, I.; Cinetto, F.; Quinti, I. IGA Antibody Induced by Immunization with Pneumococcal Polysaccharides Is a Prognostic Tool in Common Variable Immune Deficiencies. Front. Immunol. 2020, 11, 1283. [Google Scholar] [CrossRef]
- Janssen, L.M.A.; Heron, M.; Murk, J.L.; Leenders, A.C.A.P.; Rijkers, G.T.; de Vries, E. Focusing on Good Responders to Pneumococcal Polysaccharide Vaccination in General Hospital Patients Suspected for Immunodeficiency. A Decision Tree Based on the 23-Valent Pneumococcal IgG Assay. Front. Immunol. 2019, 10, 2496. [Google Scholar] [CrossRef]
- Siegel, R.L. Clinical disorders associated with T cell subset abnormalities. Adv. Pediatr. 1984, 31, 447–480. [Google Scholar]
- Kutukculer, N.; Azarsiz, E.; Karaca, N.E.; Aksu, G.; Berdeli, A. Fcγ receptor polymorphisms in patients with transient hypogammaglobulinemia of infancy presenting with mild and severe infections. Asian Pac. J. Allergy Immunol. 2015, 33, 312–319. [Google Scholar]
- Keles, S.; Artac, H.; Kara, R.; Gokturk, B.; Ozen, A.; Reisli, I. Transient hypogammaglobulinemia and unclassified hypogammaglobulinemia: ‘similarities and differences’. Pediatr. Allergy Immunol. 2010, 21, 843–851. [Google Scholar] [CrossRef]

| Population | Intervention | Comparison | Outcome | Study Type |
|---|---|---|---|---|
| Infants (human children aged 4–36 months) | Screening tool or diagnostic criteria used to make a diagnosis | N/A | Clinical diagnosis (the criteria or clinical assessment used to diagnose THI) | All study types |
| Author/Year | Aim | Type of Study/Design | Participants | Diagnostic Criteria Used/Referenced |
|---|---|---|---|---|
| Ameratunga et al., 2019 [3] | To determine the clinical features and recovery for patients with THI | Retrospective case series | 47 patients < 4 years (at the time of diagnosis) | History, examination, immunological studies, vaccine response, and isohaemagglutinin production |
| Eroglu et al., 2018 [11] | To analyse the B-cell subsets of patients with a THI diagnosis and compare with healthy age-matched Turkish children | Retrospective cohort study | 20 patients with comparison between THI and healthy aged- matched children | Low levels of IgG (<2 SD) with/without decreases in IgA or IgM. Lymphocyte subsets, isohaemagglutinins, and vaccine responses. The exclusion of the defined causes of secondary hypogammaglobulinemia |
| Moschese et al., 2008 [4] | To characterise the clinical and immunological features of children with THI and to assess the predictive parameters of clinical evolution | Prospective cohort study | 77 THI children at initial diagnosis and 57 patients at follow-up | Exclusion of other causes of hypogammaglobulinemia. Diagnosis conducted with the normalisation of IgG levels. Memory B-cell subsets and in vitro immunoglobulin production was evaluated |
| Wang et al., 2004 [7] | To review clinical features and the outcome of children with primary hypogammaglobulinemia | Retrospective, case–control study | 33 patients | Quantifications of serum immunoglobulins (IgA/IgM/IgG) and lymphocyte subsets were performed |
| Vaillant and Wilson et al., 2021 [1] | To review the clinical presentation, epidemiology, pathophysiology, and treatment of THI | Literature review | Clinical book chapter about all aspects of THI | Low serum IgG as well as the detection of isohaemagglutinins (IgM) and IgG antibodies (post-exposure) |
| Bukowska-Straková et al., 2009 [17] | To evaluate the B-cell compartment in the peripheral blood of children with different types of hypogammaglobulinemia | Retrospective, longitudinal, observational study | 600 children with immunodeficiencies. Additionally included 28 adults with CVID and 12 healthy controls | Used the criteria of the International Union of Immunological Societies in addition to patients whose level of Ig were normalised before age 4 for THI |
| Celiksoy et al., 2015 [12] | To analyse the memory of the B-cell subsets of patients with antibody deficiencies | Retrospective study | 67 patients (20 patients with THI aged 1–3). A total of 28 healthy children of matching ages were also included | Low serum IgG levels; low IgA and/or IgM levels upon admission; normalisation of low Ig levels during follow-up; the normal production of an antibody specific to isohaemagglutinins; and an intact cellular immunity |
| Lougaris et al., 2006 [15] | Not stated | Report | Reviewed the comparison of the Ig value with age- matched controls | Lab analysis of the serum IgG, IgM, and IgA. Differential diagnosis between these two conditions (THI and CVID) could not be made with certainty before 2–3 years of age |
| Qian et al., 2006 [19] | To determine the clinical signs, immunological changes, and the outcomes with hypogammaglobulinemia | Prospective | 91 patients < 2 years with warning signs of PID | Serum immunoglobulin and lymphocyte subsets were analysed. The normalisation of Ig levels in follow-up visits was noted in order to confirm the diagnosis |
| Ricci et al., 2011 [16] | To assess the clinical and immunological evolution of premature and full-term infants with hypogammaglobulinemia | Prospective, cross-sectional study | 24 children (11 premature and 13 full-term infants) | Reduction in IgG with/without a reduction in IgA and IgM |
| Kornfeld et al., 1995 [20] | To compare and diagnose a patient with XLA that presented with an initial diagnosis of THI and CVID | Retrospective case report | 1 patient | Low Ig levels, the vaccine response (to both diphtheria and tetanus), and the circulating B cells were evaluated |
| Moschese et al., 2007 [14] | To determine if memory B-cell subsets can be used as a predictive marker for the THI outcome | Retrospective cohort study | 36 patients with comparison of THI and healthy patients | Serum IgG levels < 2 SDs, circulating B cells > 2%, and an exclusion of known causes of secondary hypogammaglobulinemia |
| Brignier et al., 2015 [21] | To define hypogammaglobulinemia | Retrospective cohort study | 44 patients with early onset (i.e., <6 yrs.) | Serum immunoglobulin levels and T-cell defects were characterized. Exclusion of other PADs |
| Lakshman R. 2001 [22] | To discuss the clinical presentation, laboratory diagnosis, and management of hypogammaglobulinemia | Cross-sectional study | Management of hypogammaglobulinemia | A full blood count and peripheral smear examination, as well as quantitative estimations of serum Ig (IgG, IgA, IgM, and IgE), IgG subclass estimation, lymphocyte subset estimation, and the responses to vaccines (both diphtheria and tetanus) |
| Karaca et al., 2010 [13] | To evaluate the clinical and immunological data and outcomes | Retrospective, cross-sectional study | 101 patients | Measurement of the serum immunoglobulins (IgG, IgA, and IgM) as well as recording of vaccine responses and lymphocyte subpopulations |
| Habahbeh et al., 2014 [18] | To describe the clinical spectrum of primary antibody deficiency in order to increase awareness for early referral | Retrospective study using medical records | Medical records of 53 paediatric patients, 19% of which possessed THI | Pan-American Group for Immunodeficiency (PAGID) and the European Society for Immunodeficiency (ESID) diagnostic criteria. Molecular diagnosis not available at the hospital used in this study |
| Incidence of THI/Country | References |
|---|---|
| 23 per 106 births/Australia | [30] |
| 0.061–1.1 per 1000 live births/Japan | [2] |
| 11 per 104 births/USA | [31] |
| Prevalence of THI/Country | |
| 9.8%/Northern India | [32] |
| 10% of all cases of hypogammaglobulinemia/Taiwan | [33] |
| 18.5% of all cases of PID (the most prevalent/Japan | [33] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Justiz-Vaillant, A.A.; Hoyte, T.; Davis, N.; Deonarinesingh, C.; De Silva, A.; Dhanpaul, D.; Dookhoo, C.; Doorpat, J.; Dopson, A.; Durgapersad, J.; et al. A Systematic Review of the Clinical Diagnosis of Transient Hypogammaglobulinemia of Infancy. Children 2023, 10, 1358. https://doi.org/10.3390/children10081358
Justiz-Vaillant AA, Hoyte T, Davis N, Deonarinesingh C, De Silva A, Dhanpaul D, Dookhoo C, Doorpat J, Dopson A, Durgapersad J, et al. A Systematic Review of the Clinical Diagnosis of Transient Hypogammaglobulinemia of Infancy. Children. 2023; 10(8):1358. https://doi.org/10.3390/children10081358
Chicago/Turabian StyleJustiz-Vaillant, Angel A., Trudee Hoyte, Nikao Davis, Candice Deonarinesingh, Amir De Silva, Dylan Dhanpaul, Chloe Dookhoo, Justin Doorpat, Alexei Dopson, Joash Durgapersad, and et al. 2023. "A Systematic Review of the Clinical Diagnosis of Transient Hypogammaglobulinemia of Infancy" Children 10, no. 8: 1358. https://doi.org/10.3390/children10081358





