Developing a Novel Pediatric Eye Chart Assessing Visual Acuity by Minimum Separable Threshold
Abstract
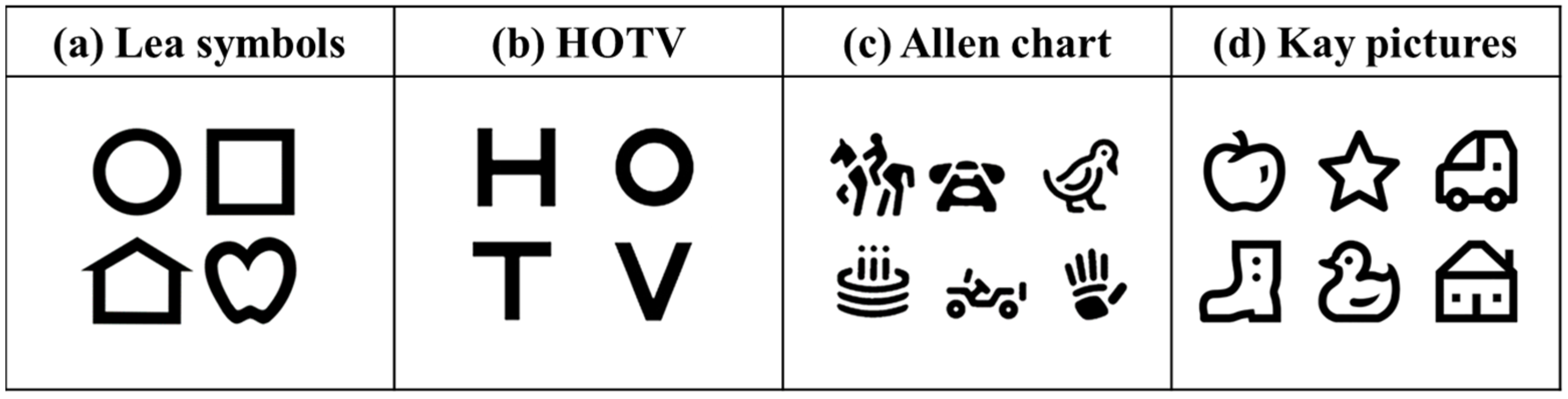
1. Introduction
2. Methods
2.1. Participants and Methods
2.2. Ethical Consideration
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Levi, D.M.; Knill, D.C.; Bavelier, D. Stereopsis and amblyopia: A mini-review. Vision Res. 2015, 114, 17–30. [Google Scholar] [CrossRef] [PubMed]
- Sprunger, D.T.; Lambert, S.R.; Hercinovic, A.; Morse, C.L.; Repka, M.X.; Hutchinson, A.; Cruz, O.A.; Wallace, D.K. Pediatric Ophthalmology/Strabismus Panel, Hoskins Center for Quality Eye Care. Amblyopia PPP. 2022. Available online: https://www.aao.org/education/preferred-practice-pattern/amblyopia-ppp-2022 (accessed on 24 March 2024).
- Wang, Y.; Liang, Y.B.; Sun, L.P.; Duan, X.R.; Yuan, R.Z.; Wong, T.Y.; Yi, P.; Friedman, D.S.; Wang, N.L.; Wang, J.J. Prevalence and causes of amblyopia in a rural adult population of Chinese the Handan Eye Study. Ophthalmology 2011, 118, 279–283. [Google Scholar] [CrossRef] [PubMed]
- Hashemi, H.; Pakzad, R.; Yekta, A.; Bostamzad, P.; Aghamirsalim, M.; Sardari, S.; Valadkhan, M.; Pakbin, M.; Heydarian, S.; Khabazkhoob, M. Global and regional estimates of prevalence of amblyopia: A systematic review and meta-analysis. Strabismus 2018, 26, 168–183. [Google Scholar] [CrossRef] [PubMed]
- Fu, Z.; Hong, H.; Su, Z.; Lou, B.; Pan, C.W.; Liu, H. Global prevalence of amblyopia and disease burden projections through 2040: A systematic review and meta-analysis. Br. J. Ophthalmol. 2020, 104, 1164–1170. [Google Scholar] [CrossRef] [PubMed]
- Xiao, O.; Morgan, I.G.; Ellwein, L.B.; He, M.; Refractive Error Study in Children Study Group. Prevalence of amblyopia in school-aged children and variations by age, gender, and ethnicity in a multi-country refractive error study. Ophthalmology 2015, 122, 1924–1931. [Google Scholar] [CrossRef] [PubMed]
- Packwood, E.A.; Cruz, O.A.; Rychwalski, P.J.; Keech, R.V. The psychosocial effects of amblyopia study. J. AAPOS 1999, 3, 15–17. [Google Scholar] [CrossRef] [PubMed]
- Kumaran, S.E.; Khadka, J.; Baker, R.; Pesudovs, K. Functional limitations recognised by adults with amblyopia and strabismus in daily life: A qualitative exploration. Ophthalmic Physiol. Opt. 2019, 39, 131–140. [Google Scholar] [CrossRef] [PubMed]
- van Leeuwen, R.; Eijkemans, M.J.; Vingerling, J.R.; Hofman, A.; de Jong, P.T.; Simonsz, H.J. Risk of bilateral visual impairment in individuals with amblyopia: The Rotterdam study. Br. J. Ophthalmol. 2007, 91, 1450–1451. [Google Scholar] [CrossRef]
- Chen, P.L.; Chen, J.T.; Tai, M.C.; Fu, J.J.; Chang, C.C.; Lu, D.W. Anisometropic amblyopia treated with spectacle correction alone: Possible factors predicting success and time to start patching. Am. J. Ophthalmol. 2007, 143, 54–60. [Google Scholar] [CrossRef]
- Mohan, K.; Saroha, V.; Sharma, A. Successful occlusion therapy for amblyopia in 11- to 15-year-old children. J. Pediatr. Ophthalmol. Strabismus 2004, 41, 89–95. [Google Scholar] [CrossRef]
- Xiao, S.; Angjeli, E.; Wu, H.C.; Gaier, E.D.; Gomez, S.; Travers, D.A.; Binenbaum, G.; Langer, R.; Hunter, D.G.; Repka, M.X.; et al. Randomized controlled trial of a dichoptic digital therapeutic for amblyopia. Ophthalmology 2022, 129, 77–85. [Google Scholar] [CrossRef] [PubMed]
- Li, R.W.; Provost, A.; Levi, D.M. Extended perceptual learning results in substantial recovery of positional acuity and visual acuity in juvenile amblyopia. Investig. Ophthalmol. Vis. Sci. 2007, 48, 5046–5051. [Google Scholar] [CrossRef] [PubMed]
- Gambacorta, C.; Nahum, M.; Vedamurthy, I.; Bayliss, J.; Jordan, J.; Bavelier, D.; Levi, D.M. An action video game for the treatment of amblyopia in children: A feasibility study. Vision Res. 2018, 148, 1–14. [Google Scholar] [CrossRef]
- Holmes, J.M.; Lazar, E.L.; Melia, B.M.; Astle, W.F.; Dagi, L.R.; Donahue, S.P.; Frazier, M.G.; Hertle, R.W.; Repka, M.X.; Quinn, G.E.; et al. Effect of age on response to amblyopia treatment in children. Arch. Ophthalmol. 2011, 129, 1451–1457. [Google Scholar] [CrossRef] [PubMed]
- Stewart, C.E.; Stephens, D.A.; Fielder, A.R.; Moseley, M.J. Modeling dose-response in amblyopia: Toward a child-specific treatment plan. Investig. Ophthalmol. Vis. Sci. 2007, 48, 2589–2594. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Romo, E.; Perez-Rico, C.; Roldán-Díaz, I.; Arévalo-Serrano, J.; Blanco, R. Treating amblyopia in adults with prosthetic occluding contact lenses. Acta Ophthalmol. 2018, 96, e347–e354. [Google Scholar] [CrossRef] [PubMed]
- Evans, B.J.; Yu, C.S.; Massa, E.; Mathews, J.E. Randomised controlled trial of intermittent photic stimulation for treating amblyopia in older children and adults. Ophthalmic Physiol. Opt. 2011, 31, 56–68. [Google Scholar] [CrossRef]
- Epelbaum, M.; Milleret, C.; Buisseret, P.; Dufier, J.L. The sensitive period for strabismic amblyopia in humans. Ophthalmology 1993, 100, 323–327. [Google Scholar] [CrossRef]
- Fronius, M.; Cirina, L.; Ackermann, H.; Kohnen, T.; Diehl, C.M. Efficiency of electronically monitored amblyopia treatment between 5 and 16 years of age: New insight into declining susceptibility of the visual system. Vision Res. 2014, 103, 11–19. [Google Scholar] [CrossRef]
- Pediatric Eye Disease Investigator Group (PEDIG) Writing Committee; Wallace, D.K.; Kraker, R.T.; Beck, R.W.; Cotter, S.A.; Davis, P.L.; Holmes, J.M.; Repka, M.X.; Suh, D.W. Randomized trial to evaluate combined patching and atropine for residual amblyopia. Arch. Ophthalmol. 2011, 129, 960–962. [Google Scholar] [CrossRef]
- Kawase, Y. Vision testing in health-check program for three-year-old children: Criteria, methods and results of the visual acuity test. Jpn. Orthopt. J. 2010, 39, 61–65. [Google Scholar] [CrossRef]
- US Preventive Services Task Force; Grossman, D.C.; Curry, S.J.; Owens, D.K.; Barry, M.J.; Davidson, K.W.; Doubeni, C.A.; Epling, J.W., Jr.; Kemper, A.R.; Krist, A.H.; et al. Vision screening in children aged 6 months to 5 years: US Preventive Services Task Force Recommendation Statement. JAMA 2017, 318, 836–844. [Google Scholar] [CrossRef] [PubMed]
- Mema, S.C.; McIntyre, L.; Musto, R. Childhood vision screening in Canada: Public health evidence and practice. Can. J. Public. Health 2012, 103, 40–45. [Google Scholar] [CrossRef] [PubMed]
- Gu, Y.T.; Shi, B.; Li, D.L.; Zhang, T.T.; Wang, P.; Jiang, J.; Pan, C.W. Cost-effectiveness of screening for amblyopia among kindergarten children in China. Prev. Med. Rep. 2024, 39, 102662. [Google Scholar] [CrossRef] [PubMed]
- Speeg-Schatz, C.; Lobstein, Y.; Burget, M.; Berra, O.; Riehl, C.; Hoffmann, C. A review of preschool vision screening for strabismus and amblyopia in France: 23 years experience in the Alsace region. Binocul. Vis. Strabismus Q. 2004, 19, 151–158. [Google Scholar] [PubMed]
- Kanda, T.; Kawase, Y. Visual acuity testing of three-year-old children using landolt ring and picture targets. Jpn. J. Public Health 1993, 40, 893–900. [Google Scholar]
- Becker, R.; Hübsch, S.; Gräf, M.H.; Kaufmann, H. Examination of young children with Lea symbols. Br. J. Ophthalmol. 2002, 86, 513–516. [Google Scholar] [CrossRef] [PubMed]
- Mochizuki, H.; Otani, S.; Omori, S.; Yoshida, M.; Watanabe, F.; Fujiyama, Y.; Niida, T. Investigation of the health checkup results for 3-year-old children with strabisumus or amblyopia. Jpn. Orthopt. J. 2019, 47, 73–79. [Google Scholar] [CrossRef]
- Zhang, X.; Wang, J.; Li, Y.; Jiang, B. Diagnostic test accuracy of Spot and Plusoptix photoscreeners in detecting amblyogenic risk factors in children: A systemic review and meta-analysis. Ophthalmic Physiol. Opt. 2019, 39, 260–271. [Google Scholar] [CrossRef]
- Klimek, D.L.; Cruz, O.A.; Scott, W.E.; Davitt, B.V. Isoametropic amblyopia due to high hyperopia in children. J. AAPOS 2004, 8, 310–313. [Google Scholar] [CrossRef]
- Ziylan, S.; Yabas, O.; Zorlutuna, N.; Serin, D. Isoametropic amblyopia in highly hyperopic children. Acta Ophthalmol. Scand. 2007, 85, 111–113. [Google Scholar] [CrossRef] [PubMed]
- ISO 8597:1994; Optics and Optical Instruments—Visual Acuity Testing—Method of Correlating Optotypes. ISO: Geneva, Switzerland, 1994.
- Dobson, V.; Clifford-Donaldson, C.E.; Miller, J.M.; Garvey, K.A.; Harvey, E.M. A comparison of Lea Symbol vs. ETDRS letter distance visual acuity in a population of young children with a high prevalence of astigmatism. J. AAPOS 2009, 13, 253–257. [Google Scholar] [CrossRef] [PubMed]
- Gräf, M.H.; Becker, R.; Kaufmann, H. Lea symbols: Visual acuity assessment and detection of amblyopia. Graefe’s Arch. Clin. Exp. Ophthalmol. 2000, 238, 53–58. [Google Scholar] [CrossRef] [PubMed]
- Gräf, M.H.; Becker, R. Determining visual acuity with LH symbols and Landolt rings. Klin. Monatsbl. Augenheilkd. 1999, 215, 86–90. [Google Scholar] [CrossRef]
- Candy, T.R.; Mishoulam, S.R.; Nosofsky, R.M.; Dobson, V. Adult discrimination performance for pediatric acuity test optotypes. Investig. Ophthalmol. Vis. Sci. 2011, 52, 4307–4313. [Google Scholar] [CrossRef] [PubMed]
- Birch, E.E.; Strauber, S.F.; Beck, R.W.; Holmes, J.M.; Pediatric Eye Disease Investigator Group. Comparison of the Amblyopia Treatment Study HOTV and Electronic-Early Treatment of Diabetic Retinopathy Study Visual Acuity Protocols in Amblyopic Children Aged 5 to 11 Years. J. AAPOS 2009, 13, 75–78. [Google Scholar] [CrossRef] [PubMed]
- Cyert, L.; Schmidt, P.; Maguire, M.; Moore, B.; Dobson, V.; Quinn, G.; Vision in Preschoolers (VIP) Study Group. Threshold visual acuity testing of preschool children using the crowded HOTV and Lea Symbols acuity tests. J. AAPOS 2003, 7, 396–399. [Google Scholar] [CrossRef] [PubMed]
- Anstice, N.S.; Jacobs, R.J.; Simkin, S.K.; Thomson, M.; Thompson, B.; Collins, A.V. Do picture-based charts overestimate visual acuity? Comparison of Kay Pictures, Lea Symbols, HOTV and Keeler logMAR charts with Sloan letters in adults and children. PLoS ONE 2017, 12, e0170839. [Google Scholar] [CrossRef]
- Levin, L.A.; Nilsson, F.E.; Hoeve, J.V.; Wu, S.; Kaufman, P.L.; Alm, A. Adler’s Physiology of the Eye, 11th ed.; Elsevier: New York, NY, USA, 2011. [Google Scholar]
- Lai, Y.H.; Wu, H.J.; Chang, S.J. A reassessment and comparison of the Landolt C and tumbling E charts in managing amblyopia. Sci. Rep. 2021, 11, 18277. [Google Scholar] [CrossRef]
- Lai, Y.H.; Wang, H.Z.; Hsu, H.T. Development of visual acuity in preschool children as measured with Landolt C and Tumbling E charts. J. AAPOS 2011, 15, 251–255. [Google Scholar] [CrossRef]
- Treacy, M.P.; Hurst, T.P.; Conway, M.; Duignan, E.S.; Dimitrov, B.D.; Brennan, N.; Cassidy, L. The early treatment in diabetic retinopathy study chart compared with the tumbling-E and Landolt-C. Ophthalmology 2015, 122, 1062–1063. [Google Scholar] [CrossRef] [PubMed]
- Ferris, F.L., III; Kassoff, A.; Bresnick, G.H.; Bailey, I. New visual acuity charts for clinical research. Am. J. Ophthalmol. 1982, 94, 91–96. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, R.A.; Davies, L.N.; Dunne, M.C.; Gilmartin, B. Statistical guidelines for clinical studies of human vision. Ophthalmic Physiol. Opt. 2011, 31, 123–136. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, R.A. When to use the Bonferroni correction. Ophthalmic Physiol. Opt. 2014, 34, 502–508. [Google Scholar] [CrossRef] [PubMed]
- Cesana, B.M.; Antonelli, P. Bland and Altman agreement method: To plot differences against means or differences against standard? An endless tale? Clin. Chem. Lab. Med. 2023, 62, 262–269. [Google Scholar] [CrossRef] [PubMed]
- Royston, P. Approximating the Shapiro-Wilk W-test for non-normality. Stat. Comp. 1992, 2, 117–119. [Google Scholar] [CrossRef]
- Rigal, R. Right-left orientation: Development of correct use of right and left terms. Percept. Mot. Skills 1994, 79, 1259–1278. [Google Scholar] [CrossRef]
- Murphy, C.M. Pointing in the context of a shared activity. Child Dev. 1978, 49, 371–380. [Google Scholar] [CrossRef]
- Kolomiyets, V.A.; Kachan, O.V. Effect of optical-reflection method of accommodative facility training on meridional acuity in astigmats with amblyopia. J. Ophthalmol. 2021, 5, 47–55. [Google Scholar] [CrossRef]
- Hered, R.W.; Murphy, S.; Clancy, M. Comparison of the HOTV and Lea Symbols charts for preschool vision screening. J. Pediatr. Ophthalmol. Strabismus 1997, 34, 24–28. [Google Scholar] [CrossRef]
- Bonneh, Y.S.; Sagi, D.; Polat, U. Spatial and temporal crowding in amblyopia. Vision Res. 2007, 47, 1950–1962. [Google Scholar] [CrossRef]
- Suchman, R.G.; Trabasso, T. Color and form preference in young children. J. Exp. Child Psychol. 1966, 3, 177–187. [Google Scholar] [CrossRef]
- Han, L. Study on the Characteristics of color preference in the paintings of children aged 4 to 6. Educ. Teach. Res. 2014, 28, 123–125. [Google Scholar] [CrossRef]








| p-Value | |
|---|---|
| Landolt ring vs. Circle | 0.92 |
| Landolt ring vs. Square | 0.31 |
| Circle vs. Square | 0.40 |
| Q1 | Q2 | Q3 | Interquartile Range | |
|---|---|---|---|---|
| Landolt ring | 0.34 | 0.64 | 0.72 | 0.38 |
| Circle | 0.34 | 0.62 | 0.78 | 0.44 |
| Square | 0.30 | 0.60 | 0.76 | 0.46 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Iwata, Y. Developing a Novel Pediatric Eye Chart Assessing Visual Acuity by Minimum Separable Threshold. Children 2024, 11, 397. https://doi.org/10.3390/children11040397
Iwata Y. Developing a Novel Pediatric Eye Chart Assessing Visual Acuity by Minimum Separable Threshold. Children. 2024; 11(4):397. https://doi.org/10.3390/children11040397
Chicago/Turabian StyleIwata, Yo. 2024. "Developing a Novel Pediatric Eye Chart Assessing Visual Acuity by Minimum Separable Threshold" Children 11, no. 4: 397. https://doi.org/10.3390/children11040397
APA StyleIwata, Y. (2024). Developing a Novel Pediatric Eye Chart Assessing Visual Acuity by Minimum Separable Threshold. Children, 11(4), 397. https://doi.org/10.3390/children11040397






