An Investigation into the Prevalence of Enamel Hypoplasia in an Urban Area Based on the Types and Affected Teeth
Abstract
1. Introduction
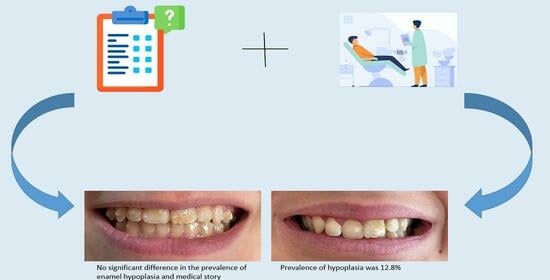
2. Materials and Methods
- The child’s details such as age, gender, date and place of birth, and current place of residence;
- Information about the parents including their education level and occupation.
- Details regarding the child’s mother’s health during pregnancy, including any diseases and medications taken.
- Information about the type of birth (natural or via operation), whether it was within the normal range or premature, and whether there were any complications during birth. Additionally, the birth weight of the child was recorded.
- Details about the child’s feeding after birth, including whether or not they were breastfed, the duration of breastfeeding, and if they were fed with milk formula.
- The child’s health status during the first 5 years of life, any medications taken during this period, and any current diseases or medical conditions.
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Seow, W.K. Developmental defects of enamel and dentine: Challenges for basic science research and clinical management. Aust. Dent. J. 2014, 59 (Suppl. S1), 143–154. [Google Scholar] [CrossRef] [PubMed]
- Guatelli-Steinberg, D. Micro-to Macroscopic. In A Companion to Dental Anthropology, 450; Irish, J.D., Scott, G.R., Eds.; Wiley-Blackwell: Hoboken, NJ, USA, 2015. [Google Scholar]
- Hillson, S. Tooth Development in Human Evolution and Bioarchaeology; Cambridge University Press: Cambridge, UK, 2014. [Google Scholar]
- Jälevik, B.; Klingberg, G.A. Dental treatment, dental fear and behaviour management problems in children with severe enamel hypomineralization of their permanent first molars. Int. J. Paediatr. Dent. 2002, 12, 24–32. [Google Scholar] [CrossRef]
- Seow, W.K.; Ford, D.; Kazoullis, S.; Newman, B.; Holcombe, T. Comparison of Enamel Defects in the Primary and Permanent Dentitions of Children from a Low-fluoride District in Australia. Pediatr. Dent. 2011, 33, 207–212. [Google Scholar] [PubMed]
- Arrow, P. Risk factors in the occurrence of enamel defects of the first permanent molars among schoolchildren in Western Australia. Community Dent. Oral Epidemiol. 2009, 37, 405–415. [Google Scholar] [CrossRef] [PubMed]
- Børsting, T.; Schuller, A.; van Dommelen, P.; Stafne, S.N.; Skeie, M.S.; Skaare, A.B.; Mørkved, S.; Salvesen, K.Å.; Stunes, A.K.; Mosti, M.P.; et al. Maternal vitamin D status in pregnancy and molar incisor hypomineralisation and hypomineralised second primary molars in the offspring at 7–9 years of age: A longitudinal study. Eur. Arch. Paediatr. Dent. 2022, 23, 557–566. [Google Scholar] [CrossRef] [PubMed]
- Fagrell, T.; Ludvigsson, J.; Ullbro, C.; Lundin, S.-Å.; Koch, G. Aetiology of severe demarcated enamel opacities—An evaluation based on prospective medical and social data from 17,000 children. Swed. Dent. J. 2011, 35, 57–67. [Google Scholar] [PubMed]
- Ford, D.; Seow, W.K.; Kazoullis, S.; Holcombe, T.; Newman, B. A controlled study of risk factors for enamel hypoplasia in the permanent teeth. Pediatr. Dent. 2009, 31, 382–388. [Google Scholar]
- Kühnisch, J.; Thiering, E.; Kratzsch, J.; Heinrich-Weltzien, R.; Hickel, R.; Heinrich, J. Elevated serum 25(OH)-vitamin D levels are negatively correlated with molar-incisor hypomineralization. J. Dent. Res. 2015, 94, 381–387. [Google Scholar] [CrossRef]
- Lygidakis, N.A.; Garot, E.; Somani, C.; Taylor, G.D.; Rouas, P.; Wong, F.S.L. Best clinical practice guidance for clinicians dealing with children presenting with molar-incisor-hypomineralisation (MIH): An updated European Academy of Paediatric Dentistry policy document. Eur. Arch. Paediatr. Dent. 2022, 23, 3–21. [Google Scholar] [CrossRef]
- Tapias-Ledesma, M.A.; Jiménez, R.; Lamas, F.; González, A.; Carrasco, P.; De Miguel, A.G. Factors associated with first molar dental enamel defects: A multivariate epidemiological approach. J. Dent. Child. 2003, 70, 215–220. [Google Scholar]
- Franco, K.M.D.; Peres, S.R.; Moura-Ribeiro, M.V.L. Prenatal and neonatal variables associated with enamel hypoplasia in deciduous teeth in low birth weight preterm infants. J. Appl. Oral. Sci. 2007, 15, 518–523. [Google Scholar] [CrossRef] [PubMed]
- Fagrell, T.G.; Lingström, P.; Olsson, S.; Steiniger, F.; Norén, J.G. Bacterial invasion of dentinal tubules beneath apparently intact but hypomineralized enamel in molar teeth with molar incisor hypomineralization. Int. J. Paediatr. Dent. 2008, 18, 333–340. [Google Scholar] [CrossRef] [PubMed]
- Americano, G.C.; Jacobsen, P.E.; Soviero, V.M.; Haubek, D. A systematic review on the association between molar incisor hypomineralization and dental caries. Int. J. Paediatr. Dent. 2017, 27, 11–21. [Google Scholar] [CrossRef] [PubMed]
- Cruvinel, V.R.; Gravina, D.B.; Azevedo, T.D.; Bezerra, A.C.; Toledo, A.O. Prevalence of dental caries and caries-related risk factors in premature and term children. Braz. Oral Res. 2010, 24, 329–335. [Google Scholar] [CrossRef][Green Version]
- Martínez Gómez, T.P.; Guinot Jimeno, F.; Bellet Dalmau, L.J.; Giner Tarrida, L. Prevalence of molar-incisor hypomineralisation observed using transillumination in a group of children from Barcelona (Spain). Int. J. Paediatr. Dent. 2012, 22, 100–109. [Google Scholar] [CrossRef] [PubMed]
- Giuca, M.R.; Cappè, M.; Carli, E.; Lardani, L.; Pasini, M. Investigation of Clinical Characteristics and Etiological Factors in Children with Molar Incisor Hypomineralization. Int. J. Dent. 2018, 2018, 7584736. [Google Scholar] [CrossRef]
- Lopes, L.B.; Machado, V.; Mascarenhas, P.; Mendes, J.J.; Botelho, J. The prevalence of molar-incisor hypomineralization: A systematic review and meta-analysis. Sci. Rep. 2021, 17, 22405. [Google Scholar] [CrossRef]
- Fatturi, A.L.; Wambier, L.M.; Chibinski, A.C.; Assunção, L.R.D.S.; Brancher, J.A.; Reis, A.; Souza, J.F. A systematic review and meta-analysis of systemic exposure associated with molar incisor hypomineralization. Community Dent. Oral. Epidemiol. 2019, 47, 407–415. [Google Scholar] [CrossRef] [PubMed]
- Schwendicke, F.; Elhennawy, K.; Reda, S.; Bekes, K.; Manton, D.J.; Krois, J. Global burden of molar incisor hypomineralization. J. Dent. 2018, 68, 10–18. [Google Scholar] [CrossRef]
- Hysi, D.; Kuscu, O.O.; Droboniku, E.; Toti, C.; Xhemnica, L.; Caglar, E. Prevalence and aetiology of Molar-Incisor Hypomineralisation among children aged 8-10 years in Tirana, Albania. Eur. J. Paediatr. Dent. 2016, 17, 75–79. [Google Scholar]
- Sujak, S.L.; Abdul Kadir, R.; Dom, T.N.M. Esthetic perception and psychosocial impact of developmental enamel defects among Malaysian adolescents. J. Oral Sci. 2004, 46, 221–226. [Google Scholar] [CrossRef] [PubMed]
- Vargas-Ferreira, F.; Ardenghi, T.M. Developmental enamel defects and their impact on child oral health-related quality of life. Braz. Oral Res. 2011, 25, 531–537. [Google Scholar] [CrossRef] [PubMed]
- Bendo, C.B.; Scarpelli, A.C.; Novaes, J.B., Jr.; Valle, M.P.P.; Paiva, S.M.; Pordeus, I.A. Enamel hypoplasia in permanent incisors: A six-month follow-up. Rev. Gauch. Odontol. 2007, 55, 107–112. [Google Scholar]
- Alsumait, A.; ElSalhy, M.; Behzadi, S.; Raine, K.D.; Gokiert, R.; Cor, K.; Almutawa, S.; Amin, M. Impact evaluation of a school-based oral health program: Kuwait National Program. BMC Oral Health 2019, 19, 202. [Google Scholar] [CrossRef] [PubMed]
- Nota, A.; Bosco, F.; Ehsani, S.; Giugliano, F.; Moreo, G.; Tecco, S. Oral Hygiene in a Sample of Children/Adolescents Living in Family-Homes from the Province of Milan (Italy): A Pilot Study. Dent. J. 2020, 8, 33. [Google Scholar] [CrossRef] [PubMed]
- Nota, A.; Palumbo, L.; Pantaleo, G.; Gherlone, E.F.; Tecco, S. Developmental Enamel Defects (DDE) and Their Association with Oral Health, Preventive Procedures, and Children’s Psychosocial Attitudes towards Home Oral Hygiene: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2020, 17, 4025. [Google Scholar] [CrossRef] [PubMed]
- Vargas-Ferreira, F.; Salas, M.M.; Nascimento, G.G.; Tarquinio, S.B.; Faggion, C.M.; Peres, M.A.; Thomson, W.M.; Demarco, F.F. Association between developmental defects of enamel and dental caries: A systematic review and meta-analysis. J. Dent. 2015, 43, 619–628. [Google Scholar] [CrossRef] [PubMed]
- Smadi, L.; Kharma, L.; Mfarej, E.B.; Abdalmohdi, A. Oral health status, attitudes and gender variations among governmental schoolchildren at Al-Mafraq governate—Jordan. Dentistry 3000 2021, 9, 152–160. [Google Scholar] [CrossRef]
- Jälevik, B.; Szigyarto-Matei, A.; Robertson, A. The prevalence of developmental defects of enamel, a prospective cohort study of adolescents in Western Sweden: A Barn I TAnadvarden (BITA, children in dental care) study. Eur. Arch. Paediatr. Dent. 2018, 19, 187–195. [Google Scholar] [CrossRef]
- Werheijm, K.L.; Duggal, M.; Mejare, P.L.; Papa-giannoulis, L. Judgement criteria for molar incisor hypomineralization (MIH) in epidemiologic studies: A summary of the European meeting on MIH held in Athens, 2003. Eur. J. Paediatr. Dent. 2003, 4, 110–113. [Google Scholar]
- Commission on Oral Health, Research & Epidemiology. A review of the developmental defects of enamel index (DDE index). Report of an FDI working group. Int. Dent. J. 1992, 42, 411–426. [Google Scholar]
- Fotedar, S.; Sogi, G.M.; Sharma, K.R. Enamel hypoplasia and its correlation with dental caries in 12 and 15 years old school children in Shimla, India. J. Indian Assoc. Public Health Dent. 2014, 12, 18–22. [Google Scholar] [CrossRef]
- Warwar, A.N.; Abdullah, M.I.; Sami, W.A. The incidence of enamel hypoplasia in children between 8 and 15 years in Anbar Governorate, Iraq. J. Int. Oral Health 2019, 11, 70–74. [Google Scholar] [CrossRef]
- Agrawal, A.; Saxena, A. Prevalence of enamel hypoplasia amongst children of Central India. Int. J. Dent. Res. 2023, 5, 40–42. [Google Scholar]
- Basha, S.; Mohamed, R.N.; Swamy, H.S. Prevalence and associated factors to developmental defects of enamel in primary and permanent dentition. Oral Health Dent. Manag. 2014, 13, 588–594. [Google Scholar] [PubMed]
- Robles, M.-J.; Ruiz, M.; Bravo-Perez, M.; González, E.; Peñalver, M.A. Prevalence of enamel defects in primary and permanent teeth in a group of schoolchildren from Granada (Spain). Med. Oral Pathol. Oral. Cir. Bucal. 2013, 18, 187–193. [Google Scholar] [CrossRef] [PubMed]
- Daneshkazemi, A.R.; Davari, A. Assessment of DMFT and enamel hypoplasia among junior high school children in Iran. J. Contemp. Dent. Pract. 2005, 6, 85–92. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Hanoon, S.A. Effect of protein energy malnutrition (PEM) on oral health status of children aged 6 years old in Sammawa city. J. Baghdad. Coll. Dent. 2012, 24, 150–155. [Google Scholar]
- Tomczyk, J.; Tomczyk-Gruca, M.; Zalewska, M. Frequency and chronological distribution of linear enamel hypoplasia (LEH) in the Late Neolithic and Early Bronze Age population from Żerniki Górne (Poland)—Preliminary report. Anthropol. Rev. 2012, 75, 61–73. [Google Scholar] [CrossRef][Green Version]
- Idiculla, J.J.; Brave, V.R.; Puranik, R.S.; Vanaki, S. Enamel hypoplasia and its correlation with dental caries in school children of Bagalkot, Karnataka. J. Oral Health Community Dent. 2011, 5, 31–36. [Google Scholar]
- Cruvinel, V.R.; Gravina, D.B.; Azevedo, T.D.; Rezende, C.S.; Bezerra, A.C.; Toledo, O.A. Prevalence of enamel defects and associated risk factors in both dentitions in preterm and full term born children. J. Appl. Oral Sci. 2012, 20, 310–317. [Google Scholar] [CrossRef] [PubMed]
- Garot, E.; Rouas, P.; Somani, C.; Taylor, G.D.; Wong, F.; Lygidakis, N.A. An update of the aetiological factors involved in molar incisor hypomineralisation (MIH): A systematic review and meta-analysis. Eur. Arch. Paediatr. Dent. 2022, 23, 23–38. [Google Scholar] [CrossRef] [PubMed]
- Haque Afzal, S.; Wigen, T.I.; Skaare, A.B.; Brusevold, I.J. Molar–incisor hypomineralisation in Norwegian children: Prevalence and associated factors. Eur. J. Oral Sci. 2023, 131, e12930. [Google Scholar] [CrossRef]
- Khazaei, Y.; Harris, C.P.; Heinrich, J.; Standl, M.; Kühnisch, J. Association study on nutrition in the first year of life and molar-incisor hypomineralization (MIH)-results from the GINIplus and LISA Birth Cohort Studies. Int. J. Environ. Res. Public Health 2021, 18, 11411. [Google Scholar] [CrossRef] [PubMed]
- Glick, M.; Williams, D.M.; Kleinman, D.V.; Vujicic, M.; Watt, R.G.; Weyant, R.J. A new definition for oral health developed by the FDI World Dental Federation opens the door to a universal definition of oral health. Br. Dent. J. 2016, 221, 792–793. [Google Scholar] [CrossRef]
- Petersen, P.E.; Bourgeois, D.; Ogawa, H.; Estupinan-Day, S.; Ndiaye, C. The global burden of oral diseases and risks to oral health. Bull. World Health Organ. 2005, 83, 661–669. [Google Scholar]
- Kaewkamnerdpong, I.; Urwannachotima, N.; Prasertsom, P.; Charoenruk, N.; Krisdapong, S. Impact of oral diseases on 12- and 15-year-old children’s quality of life: Condition-specific oral health related quality of life analysis. BMC Oral Health 2023, 23, 722. [Google Scholar] [CrossRef]
- Mejia, G.C. Measuring the oral health of populations. Community Dent. Oral Epidemiol. 2012, 40 (Suppl. S2), 95–101. [Google Scholar] [CrossRef]
- Gift, H.C.; Atchison, K.A. Oral health, health, and health-related quality of life. Med. Care 1995, 33, NS57–NS77. [Google Scholar] [CrossRef]
| Forms of Enamel Hypoplasia | Clinical Features | Teeth (According to Their Symbol) |
|---|---|---|
| Mild | Pits (single/multiple, shallow/deep tiny areas of enamel loss. | |
| Moderate | Grooves or lines of enamel loss (<2 mm wide) | |
| Severe | Areas of partial or complete absence of enamel of a tooth crown. |
| Children | Total n = 243 (100.0) | Female n = 133 (54.7) | Male n = 110 (45.3) | p-Value * |
|---|---|---|---|---|
| With hypoplasia | 31 (12.8) | 15 (11.3) | 16 (14.5) | 0.231 |
| Without hypoplasia | 212 (87.2) | 118 (89.7) | 94 (85.5) |
| Teeth | Female (Number of Teeth Affected) | Male (Number of Teeth Affected) | Total |
|---|---|---|---|
| # 11 | 4 | 3 | 7 |
| # 12 | 1 | 1 | 2 |
| # 13 | 1 | 1 | 2 |
| # 14 | 1 | - | 1 |
| # 15 | - | 2 | 2 |
| # 16 | 4 | 10 | 14 |
| # 21 | 6 | 3 | 9 |
| # 22 | - | - | - |
| # 23 | 1 | - | 1 |
| # 24 | - | 1 | 1 |
| # 25 | - | - | - |
| # 26 | 3 | 9 | 12 |
| # 31 | 1 | 1 | 2 |
| # 32 | 1 | 1 | 2 |
| # 33 | 1 | - | 1 |
| # 34 | - | - | - |
| # 35 | - | 1 | 1 |
| # 36 | 3 | 8 | 11 |
| # 41 | 1 | 1 | 2 |
| # 42 | - | - | - |
| # 43 | - | - | - |
| # 44 | - | - | - |
| # 45 | - | - | - |
| # 46 | 6 | 11 | 17 |
| No Total | 34 | 53 | 87 |
| Types of Enamel Hypoplasia | Total n (%) | Female n (%) | Male n (%) | Value p * |
|---|---|---|---|---|
| Mild | 51 (58.6) | 22 (64.7) | 29 (54.7) | 0.063 |
| Moderate | 14 (16.1) | 3 (8.8) | 11 (20.8) | 0.001 |
| Severe | 5 (5.7) | 2 (5.9) | 3 (5.7) | 0.356 |
| Atypical restorations | 17 (19.5) | 7 (20.6) | 10 (18.9) | 0.117 |
| Total | 87 (100.0) | 34 (100.0) | 53 (100.0) | - |
| Education of Parents | Female (%) | Male (%) | ||
|---|---|---|---|---|
| Mother n = 133 | Father = 133 | Mother n = 110 | Father n = 110 | |
| Elementary education | - | - | 1 (0.9) | 1 (0.9) |
| Secondary education | 36 (27.0) | 51 (38.3) | 36 (32.7) | 46 (41.8) |
| Postsecondary education | 96 (72.2) | 81 (60.9) | 73 (66.4) | 62 (56.4) |
| No answer | 1 (0.8) | 1 (0.8) | - | 1 (0.9) |
| Education of Parents | Female (%) | Male (%) | ||
|---|---|---|---|---|
| Mother n = 15 | Father n = 15 | Mother n = 16 | Father n = 16 | |
| Elementary education | - | - | - | - |
| Secondary education | 4 (26.6) | 6 (40.0) | 4 (25.0) | 7 (43.7) |
| Postsecondary education | 10 (66.7) | 8 (53.3) | 12 (75.0) | 9 (56.3) |
| No answer | 1 (6.7) | 1 (6.7) | - | - |
| Total n = 243 (%) | Female n = 133 (%) | Male n = 110 (%) | p-Value * | |
|---|---|---|---|---|
| Natural birth/operation | 137/106 (56.4/43.6) | 71/62 (53.4/46.6) | 66/44 (60.0/40.0) | 0.135 |
| Normal range/premature birth | 224/19 (92.2/7.8) | 126/7 (94.7/5.3) | 98/12 (89.1/10.9) | 0.001 |
| Healthy birth/complication during birth | 225/18 (92.6/7.4) | 126/7 (94.7/5.3) | 99/11 (90.0/10.0) | 0.001 |
| Average birth weight (in kg) | 3.36 + 0.47 [1.8–4.8] Me = 3.40, IR = 0.50 | 3.32 + 0.44 [1.8–4.8] Me = 3.30, IR = 0.50 | 3.41 + 0.51 [1.8–4.8] Me = 3.45, IR = 0.70 | 0.116 ɫ |
| Breastfeeding | 229 (94.2) | 128 (96.2) | 101 (91.8) | 0.136 |
| Average period of breastfeeding (in months) | 10.27 + 8.70 [0.5–60] Me = 6.0, IR = 6.5 | 10.47 + 9.23 [0.5–60.0] Me = 6.0, IR = 6.0 | 10.0 + 8.01 [1.0–48.0] Me = 6.5, IR = 9.0 | 0.684 ɫ |
| Feeding with milk formula | 14 (5.8) | 5 (3.8) | 9 (8.2) | 0.062 |
| Current diseases | 6 (2.5) | 1 (0.8) | 5 (4.5) | 0.117 |
| Diseases in early childhood | 15 (6.2) | 10 (7.5) | 5 (4.5) | 0.235 |
| Diseases during lactation | 9 (3.7) | 2 (1.5) | 7 (6.4) | 0.435 |
| Medications during lactation | 13 (5.3) | 7 (5.3) | 6 (5.5) | 0.688 |
| Total n = 31 (%) | Female n = 15 (%) | Male n = 16 (%) | p-Value * | |
|---|---|---|---|---|
| Natural birth | 18 (58.1) | 10(66.7) | 8 (50.0) | 0.78 |
| Birth operation | 12 (38.7) | 4 (26.7) | 8 (50.0) | 0.113 |
| No answer | 1 (3.2) | 1 (6.6) | 0 (0.0) | |
| Average birth weight (in kg) | 3.42 + 0.35 [3–4.6] Me = 3.3, IR = 0.4 | 3.33 + 0.22 [3.0–3.7] Me = 3.30, IR = 0.30 | 3.51 + 0.45 [3.0–4.6] Me = 3.45, IR = 0.62 | 0.567 ɫ |
| Breastfeeding | 26 (83.8) | 12 (80.0) | 14 (87.5) | 0.325 |
| Average period of breastfeeding (in months) | 12.1 + 10.1 [1.6–48], Me = 7.00, IR = 12.5 | 12.53 + 8.05 [3.0–24.0] Me = 12.00, IR = 14.00 | 12.11 + 12.39 [1.6–48.0] Me = 6.5, IR = 110.25 | 0.567 ɫ |
| Feeding with milk formula | 2 (6.5) | 0 (0.0) | 2 (12.5) | |
| Current diseases | 6 (19.4) | 1 (6.6) | 5 (31.3) | 0.001 |
| Diseases in early childhood | 15 (48.4) | 10 (66.7) | 5 (31.3) | 0.03 |
| Diseases during lactation | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| Medications during lactation | 0 (0.0) | 0 (0.0) | 0 (0.0) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Disha, V.; Zaimi, M.; Petrela, E.; Aliaj, F. An Investigation into the Prevalence of Enamel Hypoplasia in an Urban Area Based on the Types and Affected Teeth. Children 2024, 11, 474. https://doi.org/10.3390/children11040474
Disha V, Zaimi M, Petrela E, Aliaj F. An Investigation into the Prevalence of Enamel Hypoplasia in an Urban Area Based on the Types and Affected Teeth. Children. 2024; 11(4):474. https://doi.org/10.3390/children11040474
Chicago/Turabian StyleDisha, Valbona, Marin Zaimi, Elizana Petrela, and Fatbardha Aliaj. 2024. "An Investigation into the Prevalence of Enamel Hypoplasia in an Urban Area Based on the Types and Affected Teeth" Children 11, no. 4: 474. https://doi.org/10.3390/children11040474
APA StyleDisha, V., Zaimi, M., Petrela, E., & Aliaj, F. (2024). An Investigation into the Prevalence of Enamel Hypoplasia in an Urban Area Based on the Types and Affected Teeth. Children, 11(4), 474. https://doi.org/10.3390/children11040474