Abstract
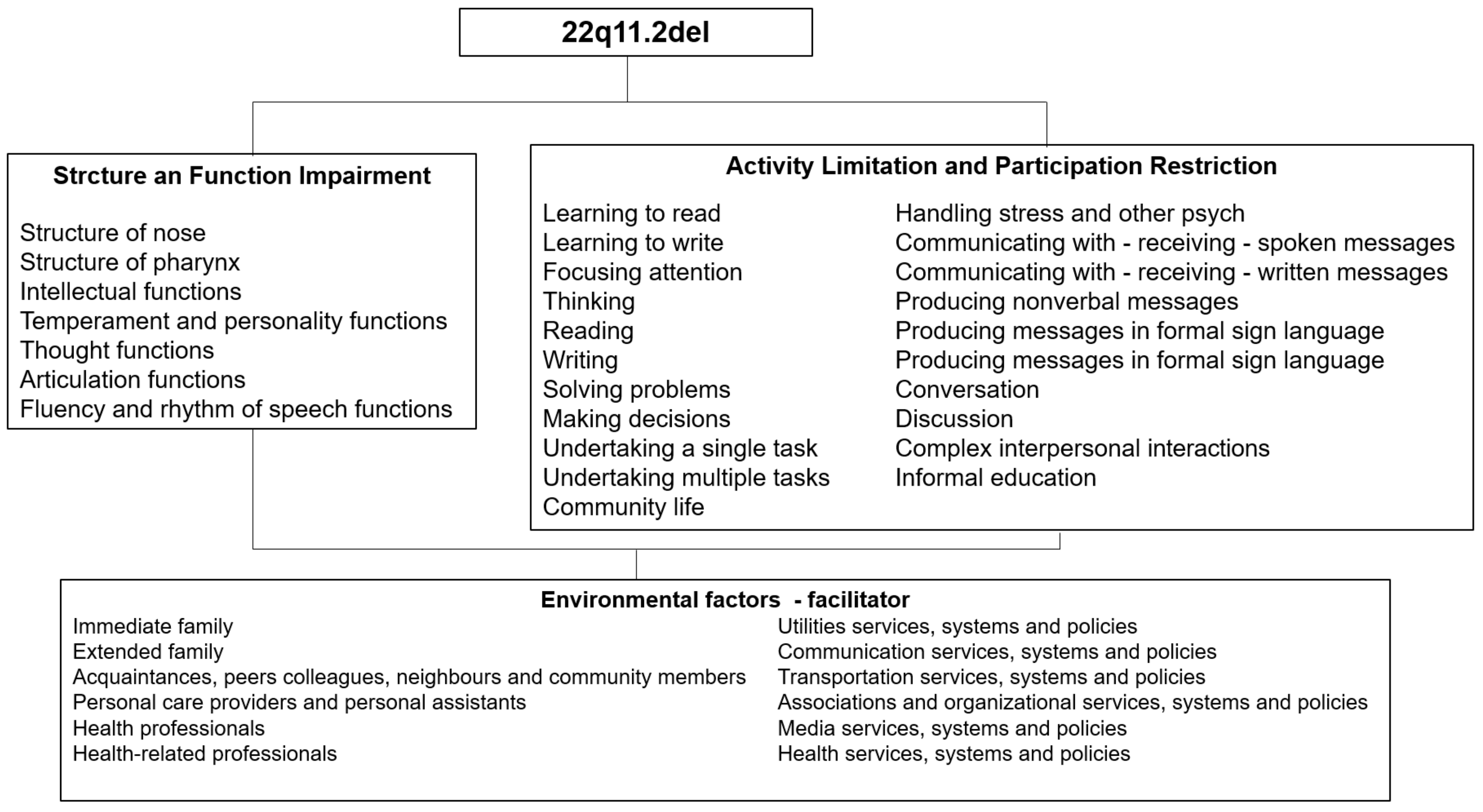
The 22q11.2 deletion syndrome (DS) can have a significant impact on functionality. The purpose was to describe 22q11.2DS children with functioning from a biopsychosocial perspective, focusing on the impact of children’s health condition from domains of the International Classification of Functioning, Disability, and Health (ICF). Methods: A descriptive, cross-sectional case series study with seven 22q11.2DS children. A questionnaire with an ICF checklist for 22q11.2DS was completed using a structured interview. The Wechsler Abbreviated Scale of Intelligence (WASI) was used to determine the Intelligence Quotient (IQ). Results: Seven participants from 7 to 12 years old, presented some level of IQ impairment. It was observed that 22q11.2DS children experience significant intellectual, cognitive, and speech impairments across ICF Body Function domains. Impairments related to nose and pharynx were found in only one patient. The most relevant categories considered limitations in the Activity and Participation components pertained to producing nonverbal messages, communication, handling stress, and social interaction. Family, health professionals, and acquaintances were perceived as facilitators in the component Environmental Factors. Conclusion: The sample has its functioning affected by aspects that go beyond impairments in body structure and function. The organization of information from the perspective of the ICF is a different approach that helps clinical reasoning.
1. Introduction
The 22q11.2 deletion syndrome (22q11.2DS; 22q11.2del) is the most common microdeletion syndrome in humans. Recent research shows 22q11DS has an estimated prevalence of 1 per 2148 live births [1]. Clinical manifestations of 22q11.2DS are highly heterogeneous and can range from mild to severe, and typically include a congenital heart defect (CHD), velopharyngeal insufficiency with or without cleft palate, mild-to-moderate immune impairment, characteristic facial features, learning disabilities, and language difficulties [2]. Impaired cognitive and behavioral problems are frequent, and mean Intelligence Quotient (IQ) scores have been found to be reduced in approximately 50% of patients [3]. In addition, subjects with a 22q11.2DS deletion show a higher risk for the development of psychiatric problems during adolescence and early adulthood [3,4].
Furthermore, speech and language difficulties comprise one of the most distressing aspects for parents of children with 22q11.2DS [2,5]. Studies have highlighted that the difficulties in the production of spoken language presented in 22q11.2DS seem to exceed the anatomofunctional alterations of the phono-articulatory organs [5,6,7,8,9,10], with difficulties being found in more complex tasks such as in the production of oral narrative, in the task of verbal fluency [11], and other communication skills [12]. This can have a significant impact on functionality.
Despite the prevalence of the syndrome, it frequently goes undiagnosed because of mild or variable phenotypic expression. Diagnosis can be confirmed by fluorescence in situ hybridization (FISH), a cytogenetic test that is not available in many cases due to their high cost. 22q11DS is also often diagnosed using quantitative chromosomal microarray (CMA) or targeted deletion analysis. Hence, it is important to identify the common symptoms as well as the functional domains that may be affected in 22q112DS children to diagnose, and plan comprehensive evaluations, rehabilitation therapies, and long-term follow-up [13,14].
In this context, the World Health Organization created the International Classification of Functioning, Disability, and Health (ICF), which serves as a companion to the International Classification of Diseases to characterize how health-related conditions affect people’s lives. The ICF focuses on how context affects functioning and the level of disability [15]. In this case, “functioning” does not refer to the quantification of ability or symptoms, but rather to how those symptoms affect an individual’s age-appropriate ability to respond to the demands of daily life. Although the most common symptoms and domains that may be affected in people with 22q11.2DS are known, the biopsychosocial framework for comprehensively describing functioning and disability that is provided by the ICF may enhance our understanding of the broader impact of 22q11.2DS on the functioning of individual children.
Recent research studies have begun to use the ICF to assess children’s functioning status in the context of their health condition [16,17,18]. Havstam et al. [16] were the first researchers on children with cleft lip and palate (CLP) to utilize the ICF to provide an integrated and comprehensive understanding of CLP and how a communication disability may emerge. Additionally, studies have applied the framework of the ICF to consider children’s communication [18]. However, to our knowledge, applications of the ICF related to children with 22q11.2DS specifically are lacking.
Can a biopsychosocial approach, based on the ICF, change the care of children and adolescents with 22q11.2DS? The ICF framework can provide health professionals not only with the opportunity to value the positive aspects of functioning, as well as the disability aspects. This may provide a more comprehensive approach to this population. Thus, the purpose of this study was to describe children with 22q11.2DS functioning from a biopsychosocial perspective, focusing on the impact of children’s health conditions from four major domains of functioning: Body Functions, Body Structures, Activities and Participation, and Environmental Factors.
2. Materials and Methods
2.1. Study Design, Study Patients, and Data Collection
We performed a descriptive, quantitative, cross-sectional case series study with seven 22q11.2 deletion syndrome children. Patients were recruited from a high-complexity hospital and two other genetics centers in Rio de Janeiro, Brazil, between 1 February 2019 and 31 February 2020, and they were either inpatients or outpatients. This is a public hospital that offers multi-professional advice, support, and treatment to children and youth with physical, cognitive, and/or psychiatric disabilities. The research protocol followed the normative guidelines of Resolution No. 466/12 of the National Health Council of the Brazilian Ministry of Health. Local ethics committee approval was obtained prior to the start (n.2.970.203) and patient data were kept anonymous. Consent from all participants was obtained in writing and documented on a specific form signed by the local Ethics Committee.
Participants for this study were children and inclusion criteria for the study were a positive genetic test, FISH microarray for the 22Q11.2 chromosomal deletion, and age between 6 and 12 years old. All children from the various genetics centers in the city of Rio de Janeiro with a positive FISH test were included. The families of all eligible children were contacted directly for participation in the clinic by phone or by mail. The study participants were invited consecutively to the clinic at the times when the investigator was present. Only one guardian refused to participate in the study. Parents’ informed consent was obtained and signed in person by them and the researcher before the assessments. Children between 6 and 12 years old also signed in person, together with the researchers and their parents, a free and informed consent form.
The most common impairments of 22q11.2DS children were explored using the ICF checklist developed in a previous study [19]. A questionnaire with this checklist for 22q11.2DS was completed using a structured interview with the children and parents by the investigator’s direct observations, and by information retrieved from medical records. All participants and their parents were interviewed by health professionals trained in the principles of the ICF. Before an interview started, each patient’s medical record sheet was checked and relevant information on socio-demographic variables and diagnoses was extracted. The participants were also instructed to bring updated medical reports and exam results to the interview for additional information. The data were collected by using a patient profile questionnaire containing demographic information, medical diagnoses, and information about other health-related issues, which were recorded using a patient profile questionnaire.
Impairments in 23 items from the Body Functions component and 9 from the Body Structure component were investigated by using the ICF checklist for 22q11.2DS. We also checked limitations in 44 items from the Activities and Participation component and assessed as barriers or facilitators 28 items from the Environmental Factors component [19].
The Test of Childhood Language ABFW was used only to fill in vocabulary, fluency, and language pragmatics questions in the ICF checklist [20]. We performed an adapted version of the Portuguese Wechsler Abbreviated Scale of Intelligence (WASI) [21] to determine the full-scale, verbal, and performance IQ of the children. WASI is a brief instrument used to assess people’s intellectual ability from 6 to 89 years old. It consists of four subtests, two of which are part of a verbal scale (Vocabulary and Similarities), and two of which are part of a performance scale (Block Design and Matrix Reasoning). The scale was performed by a trained psychologist at a previously scheduled time, and it took around forty minutes. Age-adjusted scores were derived and transformed into a score using norms available for each measure. These scores are already age-standardized, where higher scores indicate better performance.
2.2. Statistical Analysis
The answers from the study population were considered as frequencies of impairments/limitations for the ICF components Body Functions, Body Structures, and Activities and Participation. As for the Environmental Factors, absolute frequencies of categories were named to be a facilitator or barrier. The ICF categories considered not applicable by the participants were marked as “not relevant/not applicable”.
Data were collected manually initially, and then entered, organized, and analyzed using Epi Info software version 7.0. Following that, the data were exported and descriptive statistics (frequency, percentage, mean) were used to describe the studied variables.
3. Results
3.1. Demographic Characteristics
Our analyses revealed that five out of seven of them were boys; only one subject presented with a hearing loss diagnosis; and the population age was from 7 to 12 years old with a mean of 10.28 and a std. deviation of 2.05 (Table 1). The IQ was assessed using WASI by measuring verbal IQ (VIQ), performance IQ (PIQ), and general cognition full-scale (FSIQ). Table 1 shows the mean performance on WASI scores and a comparison of means between participants. Cognitive assessment was completed for six of the seven patients enrolled in the study. Due to scheduling on a different day from the ICF questionnaire application, cognitive assessments were not performed on one patient, who did not reply to phone calls, emails, or text messages; after a period of ten months without any contact, the participant was excluded from cognitive testing. We identified that all subjects presented with IQ impairment. In the verbal IQ, one child had an average IQ, one had a low-average intellectual disability, two had an IQ in the borderline range, and two had an extremely low verbal IQ. As for the performance IQ, two children had a low-average, three had a borderline range, and one had an extremely low performance IQ. Finally, in the full-scale IQ, two children had low-average IQ, one had an IQ in the borderline range, and three had an extremely low full-scale IQ. In sum, we found that children with 22q11.2DS had significant deficits across all cognitive measures: full-scale IQ, verbal IQ, and performance IQ scores.

Table 1.
Demographic characteristics of 22q11.2DS children.
3.2. Impairments of 22q11.2DS Children Using the ICF Checklist
At the level of Body Functions and Structures, we identified that impairments related to nose and pharynx were found in only one patient, and none of the children presented with external ear structure impairment. We observed that 22q11.2DS children experience significant intellectual, cognitive, and speech impairment across ICF Body Function domains (Table 2). This is especially identified in the items related to fluency and rhythm of speech and intellectual functions, where we had the highest number for confirmed impairment (n = 5). Further, areas related to personality were also shown to affect four out of seven children.

Table 2.
Body Structures and Functions in children with 22q11.2DS.
We also observed that all participants presented with a major limitation/restriction related to Activity and Participation in producing nonverbal messages (Table 3). Other restrictions for the children were related to communication and social interaction, where most of them (four or more children) showed participation limitations. Items such as community life, complex interpersonal interactions, abilities to discuss, having a conversation, communicating with written and spoken messages, as well as in writing, reading, and thinking were also found to be limitations for the study population (Table 3).

Table 3.
Activity and Participation of children with 22q11.2Ds.
Furthermore, we investigated which Environmental Factors related to the physical, social, and attitudinal environment in which people live and conduct their lives might be facilitators or barriers to children’s functioning. Within the ICF checklist related to children with 22q11.2DS, we found that the Environmental Factors that were considered facilitators for all participants were their immediate family (e310), transportation services, systems, and policies (e540); utility services, systems, and policies (e530); and media services, systems, and policies (e560) (Table 4). Most of the participants (five out of seven) also considered facilitators their extended family (e315); acquaintances, peers’ colleagues, neighbors, and community members (e325); as well as personal care providers and personal assistants (e340); health professionals (e355); individual attitudes of immediate family members (e410); and communication services, systems, and policies (e535) (Table 4).

Table 4.
Environmental Factors related to children with 22q11. DS.
We also identified Environmental Factors related to the use of products, none of the participants made use of products and technology for personal use in daily living (e115), only one participant reported the use of products and technology for culture and recreation (e140), two reported the use of products for communication (e125), and five children use products and technology for education (e130) (Table 4).
The main findings (over 45%) related to the functionality of children and adolescents with 22q11.2DS are described in Figure 1.
Figure 1.
Main findings related to the functionality of children and adolescents with 22q11.2DS.
4. Discussion
Our findings point out that all four components of the ICF (Body Functions, Body Structures, Activities and Participation, and Environmental Factors) are relevant for children with 22q11.2DS, confirming the hypothesis that these children have their functioning affected by aspects that go beyond the impairments in body structure and function. According to the ICF, impairments are defined as problems in body function or structure. All the variables in this study relating voice and speech to articulation functions, alternative vocalization functions, and fluency and rhythm functions are, by definition, impairments of Body Functions. In agreement, it has been described that speech and language disorders in the school-aged years, such as hypernasality and voice disorders, as well as language impairments, are related to difficulties with narrative and descriptive language [13,22], which goes along with the findings in our study where fluency and rhythm functions were considered impaired for five out of the seven children interviewed. This impairs communication and can affect the social participation of these children. The Boerma et al. [5] study indicates an important language problem in children with 22q11.2DS and that expressive language exceeds that seen in developmental language disorder (DLD), possibly due to the intellectual impairment in the 22q11del and DLD groups.
Moreover, we found that mental functions were also significantly affected in the children with 22q11.2DS; items related to intellectual functions, thought functions, perceptual functions, higher-level cognitive functions, temperament, and personality functions were the most frequently impaired. General mental functions constitute the way the individual reacts in a particular way to situations, including the set of mental characteristics that make the individual distinct from others [15]. During the interview, four children demonstrated variations in emotional reactivity; such behavior was also emphasized by the parents as being frequent in the child’s daily routine as they answered the checklist. Our findings are of great importance because impairments in mental functions can signal risk factors for developing psychiatric disorders. A previous study found similar results when they described 22q11.2DS children’s temperaments as being moderately difficult [23]. In line with this, other studies described children with 22q11.2DS at increased risk for psychiatric disorders throughout development, especially attention-deficit/hyperactivity disorder (ADHD), anxiety and affective disorders, psychosis, and schizophrenia spectrum disorders [24]. In accordance with our findings, perceptual function impairments were also found in another study where they reported that 22q11.2DS children were significantly slower to recognize happiness, sadness, and anger (but not fear) on a dynamic emotion task, compared to other children [25]. Such behaviors should be considered since psychiatric disorders are among the most common manifestations of 22q11DS, and diagnoses characteristically prevalent in childhood include ADHD (30–40%), anxiety (30–40%), and mood (20–30%) disorders, which increase in prevalence during adolescence [25].
Body Structure impairments were found only in two participants, both related to structures involved in voice and speech. This could be related to the specific speech and language disorders that continue into the school-aged years [6,13]. However, the data of the patients in our study are not in line with previous qualitative research when it comes to impairments in Body Structures. In the latter, patients experienced more problems than in this present research. This could be due to a lack of clinical reports on patient’s records, and long waiting lists did not make needed and/or new evaluations possible; therefore, in our research, health professionals rated the patients in the Body Structures category according to the medical and professional reports available at that time, as recommended by the ICF manual [15]; consequently, complementary exams to fully assess the items from the Body Structures from the ICF checklist for 22q11.2DS was not possible and could have impacted the Body Structures impairments assessment. Thus, we cannot confirm the instrument reliability for Body Structures, because the small number of patients having some classifiable impairment in those components prevents a meaningful analysis. Furthermore, we must consider the absence of information in the medical record as proof of the absence of impairment, and thus these items could not be completed reliably due to insufficient information.
The ICF focuses on how context affects function. “Functioning” does not refer to the quantification of symptoms, but rather to how those symptoms affect an individual’s ability to respond to the demands of daily life [15]. These domains are related, but are independent, and the presence of below-average cognitive abilities does not necessarily confer low function; therefore, the IQ assessed using the Wechsler Abbreviated Scale of Intelligence (WASI) from which full-scale IQ (FSIQ), verbal IQ (VIQ), and performance IQ (PIQ) were obtained was of great worth for understanding 22q11.2del children’s functioning. The level of intelligence in children and adolescents with 22q11.2 deletion syndrome is highly variable [26]. In our study, we found that the FSIQ of all children had a significant deficit, and four out of the six children assessed presented with an FSIQ below 70. While divergent cognitive trajectories across age have been reported [27], others suggest some cognitive decline for most 22q11.2DS individuals as they grow into adulthood [28]. This is in accordance with previous findings where approximately 50% of individuals with 22q11.2DS had an intellectual disability (ID), defined by an IQ score of less than 70 [29].
Although the intelligence profile is highly variable in 22q11.2DS children, examination of sub-scale scores on the WASI revealed that four out of the six children had lower VIQ scores compared to PIQ scores. Although the magnitude of the difference on average is variable (from 1 to 19 IQ points), it may be worth investigating in future studies if some individuals perhaps speak less or if some aspect of verbal communication is diminished by transmission. These results were also described where a subgroup of children with 22q11.2DS during early primary school age showed a discrepancy between verbal abilities and perceptual reasoning abilities, favoring the verbal domain [30].
The most relevant categories considered limitations in the Activity and Participation component pertained to producing nonverbal messages, communication, handling stress, and social interaction. Because verbal communication is a major contributor to the foundation of a person’s identity and their social validation, disruptions in one’s speech may result in decreased self-concept. Decrements in self-esteem, in turn, may contribute to feelings of uneasiness during verbal exchanges in social settings [31]. These results indicate a correlation with our findings in Body Structures and Functions, where speech difficulties of children with 22q11.2DS were also relevant categories and can potentially be associated with psychological or emotional problems including difficulties with self-esteem, depression, and anxiety [32].
In addition, categories related to the learning process, such as reading, writing, thinking, and focusing attention, were also recorded as a limitation for most of the children. These findings are also described in the literature, where learning disabilities and academic achievement difficulties, as well as deficits in attention and concentration, are reported in children with 22q11.2DS [11]. In sum, we see that disruption to the Body Functions and Structures of children with 22q11.2DS is but one component of functioning as described by the ICF. The interrelated nature of the ICF components suggest that the functioning and disability of an individual emerge from the interaction of one’s Body Functions and Structures with other components of the ICF such as Activity and Participation [15], and this examination of all interactions is necessary for a complete description of functioning in children with 22q11.2DS.
Family, health professionals, and acquaintances were perceived as facilitators for the 22q11.2DS children in the component Environmental Factors. For more than half of the participants health services, systems, and policies were also important facilitators. This emphasizes the importance of children’s social networks and the influence of a good relationship with health professionals. Although there is a reasonable body of literature describing IQ, achievement, neurocognitive, and behavioral abnormalities in children with 22q11DS [3,29], there is a lack of published studies that have assessed the role of the environment in functioning in these domains.
The reported use of products was not relevant for this study population: one participant reported using products and technology for culture and recreation, two reported using products for communication, and five children used products and technology for education; this category contains items like a calculator, which was the item cited by all five participants. The role of other products and their use remains unclear since studies that correlate specific environmental factors from the ICF and the 22q11.2DS children were not found in the literature.
Studies in general only highlight the deficiencies of structure and function, according to a biomedical approach that is now outdated. The current focus of healthcare, whether clinical or rehabilitation, should be directed toward activity and participation from a biopsychosocial perspective. Dorsman [33] finds that the lack of information regarding contextual level factors may be limiting the understanding of the neurocognitive and neuropsychiatric trajectories of people with 22q11.2DS. The use of the ICF can lead to this direction as it considers the subject in its fullest and beyond the health condition itself. The functioning of 22q11.2DS children is an important factor that affects their activity, participation, and quality of life. Although this is a case-series study, thus limiting its generalizability to larger populations of patients, this study can also provide information that allows hypotheses to develop, leading to further advanced studies. An ICF-based checklist approach, such as the one used in this research, can be used to identify common profiles of functioning, activities, participation, and environment of the 22q11.2DS child population. The value of using the ICF in the assessment of children with 22q11.2DS is that it enables health professionals to focus on what should be the goal of intervention: improvement in the child’s functioning.
The findings from our experience on the applicability of an ICF checklist for 22q11.2DS show that ways of operationalizing the ICF can contribute to overcoming the biomedical perspective, creating possibilities to incorporate a biopsychosocial approach into the healthcare routine. However, one limitation of our study was that some questions used in the ICF questionnaire for 22q11.2DS were not completely clear to the parents, and a previous explanation was needed for better understanding. This should be taken into consideration for improvement in future studies. One limiting factor for this study is also the sample size of seven. In order to draw stronger conclusions, a larger sample size is required. We justify the sample size of the study with the relatively rare nature of 22q11.2DS and the difficulty in recruiting active participants.
Another limitation of the present study is that the clinical records were not enough to evaluate Body Structure and Function, and further evaluation was not always possible. This means that the prevalence of impairments in Body Function and Structure might have been underestimated. Rehabilitation based on the ICF approach focuses on humanized healthcare, where planning interventions are centered on the interaction between an individual’s health conditions, environmental factors, and individual factors, designed to remove barriers in several contexts. Therefore, further studies on Body Structure and Function related to Activity and Participation according to the ICF will clarify the impact and impairments of 22q11.2DS in children’s functioning.
5. Conclusions
Despite the small sample, but adding to the knowledge in the literature, our findings show that children have their functioning affected by aspects that go beyond the Body Functions and Structures described in their medical diagnosis. Relevant categories related to Activity and Participation limitations were observed, especially in the production of nonverbal messages, communication, stress management, and social interaction. Incorporating a biopsychosocial approach is important to expand the assessment of children with 22q11.2DS. It is necessary to leave the traditional action-centered medical model and instead evaluate the child from a biopsychosocial perspective to understand their future perception of functionality.
This is the first study to use ICF for the functional profile of 22q11.2DS children and adolescents; therefore, this study represents the first stage in the development of an ICF Core Set in 22q11.2DS, hoping that it can be a practical tool to give insight into the wider determinants of the 22q11.2DS population and be used in public health and social policy to help address inequalities within the child population. Our experience represents a strong stimulus for extending our sample and verifying the results obtained in this preliminary experience to obtain a full profile of 22q11.2DS functioning based on the ICF. Moreover, our results show that the ICF checklist for children with 22q11.2DS fulfills the requirement of a useful, reliable, and valid multidimensional framework for defining domains and describing functioning in children aged 7–12 years.
Author Contributions
Conceptualization and methodology: A.P.C.C., L.C. and C.T.M.R.; formal analysis, A.P.C.C. and L.C.; investigation, A.P.C.C., L.N.S., A.O.d.C. and C.M.D.W.; writing—original draft preparation, A.P.C.C. and C.T.M.R.; writing—review and editing, D.D.G.H. and L.S.; supervision, C.T.M.R., L.C. and D.D.G.H.; funding acquisition, C.T.M.R. and A.P.C.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by IFF/Fiocruz (PIBIC 09412); Deutscher Akademischer Austauschdienst—DAAD (57440919).
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved Ethics Committee of the National Institute of Women’s, Children’s, and Adolescents’ Health Fernandes Figueiras (IFF/Fiocruz) (protocol code 2.970.203. approval date 18 October 2018).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author due to restrictions for privacy and ethical considerations and subject confidentiality.
Acknowledgments
The authors would like to acknowledge the generous support of the Oswaldo Cruz Foundation, Deutscher Akademischer Austauschdienst (DAAD), and the Medical School Hamburg.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Blagojevic, C.; Heung, T.; Theriault, M.; Tomita-Mitchell, A.; Chakraborty, P.; Kernohan, K.; Bulman, D.E.; Bassett, A.S. Estimate of the contemporary live-birth prevalence of recurrent 22q11.2 deletions: A cross-sectional analysis from population-based newborn screening. Can. Med. Assoc. Open Access J. 2021, 9, E802–E809. [Google Scholar] [CrossRef] [PubMed]
- McDonald-McGinn, D.M.; Sullivan, K.E.; Marino, B.; Philip, N.; Swillen, A.; Vorstman, J.A.S.; Zackai, E.H.; Emanuel, B.S.; Vermeesch, J.R.; Morrow, B.E.; et al. 22q11.2 deletion syndrome. Nat. Rev. Dis. Primer. 2015, 1, 15071. [Google Scholar] [CrossRef] [PubMed]
- Óskarsdóttir, S.; Belfrage, M.; Sandstedt, E.; Viggedal, G.; Uvebrant, P. Disabilities and cognition in children and adolescents with 22q11 deletion syndrome. Dev. Med. Child Neurol. 2005, 47, 177–184. [Google Scholar] [CrossRef] [PubMed]
- Shprintzen, R.J. Velo-Cardio-Facial Syndrome: A Distinctive Behavioral Phenotype. MRDD Research Reviews. 2000. Available online: https://onlinelibrary.wiley.com/doi/10.1002/1098-2779(2000)6:2%3C142::AID-MRDD9%3E3.0.CO;2-H (accessed on 4 January 2022).
- Boerma, T.; Everaert, E.; Vlieger, D.; Steggink, M.; Selten, I.; Houben, M.; Vorstman, J.; Gerrits, E.; Wijnen, F. Grammatical skills of Dutch children with 22q11.2 Deletion Syndrome in comparison with children with Developmental Language Disorder: Evidence from spontaneous language and standardized assessment. Front. Commun. 2023, 8, 1111584. [Google Scholar] [CrossRef]
- Glaser, B.; Mumme, D.L.; Blasey, C.; Morris, M.A.; Dahoun, S.P.; Antonarakis, S.E.; Reiss, A.L.; Eliez, S. Language skills in children with velocardiofacial syndrome (deletion 22q11.2). J. Pediatr. 2002, 140, 753–758. [Google Scholar] [CrossRef] [PubMed]
- Solot, C.B.; Sell, D.; Mayne, A.; Baylis, A.L.; Persson, C.; Jackson, O.; McDonald-McGinn, D.M. Speech-Language Disorders in 22q11.2 Deletion Syndrome: Best Practices for Diagnosis and Management. Am. J. Speech-Lang. Pathol. 2019, 28, 984–999. [Google Scholar] [CrossRef] [PubMed]
- Jacobson, C.; Shearer, J.; Habel, A.; Kane, F.; Tsakanikos, E.; Kravariti, E. Core neuropsychological characteristics of children and adolescents with 22q11.2 deletion: Cognitive deficits in 22q11.2 deletion syndrome. J. Intellect. Disabil. Res. 2010, 54, 701–713. [Google Scholar]
- Moss, E.M.; Batshaw, M.L.; Solot, C.B.; Gerdes, M.; McDonald-McGinn, D.M.; Driscoll, D.A.; Emanuel, B.S.; Zackai, E.H.; Wang, P.P. Psychoeducational profile of the 22q11.2 microdeletion: A complex pattern. J. Pediatr. 1999, 134, 193–198. [Google Scholar] [CrossRef] [PubMed]
- Scherer, N.J.; D’Antonio, L.L.; Kalbfleisch, J.H. Early speech and language development in children with velocardiofacial syndrome. Am. J. Med. Genet. 1999, 15, 714–723. [Google Scholar] [CrossRef]
- Persson, C.; Niklasson, L.; Óskarsdóttir, S.; Johansson, S.; Jönsson, R.; Söderpalm, E. Language skills in 5–8-year-old children with 22q11 deletion syndrome. Int. J. Lang. Commun. Disord. 2006, 41, 313–333. [Google Scholar] [CrossRef] [PubMed]
- Freire, T.; Gonçalves T dos, S.; Moretti, C.N.; Tabaquim M de, L.M.; Crenitte, P.A.P. Desempenho nas habilidades subjacentes a aprendizagem em um caso de Sindrome Velocardiofacial. Distúrbios Comun. 2015, 27, 237–247. [Google Scholar]
- Cancrini, C.; Puliafito, P.; Digilio, M.C.; Soresina, A.; Martino, S.; Rondelli, R.; Consolini, R.; Ruga, E.M.; Cardinale, F.; Finocchi, A.; et al. Clinical Features and Follow-Up in Patients with 22q11.2 Deletion Syndrome. J. Pediatr. 2014, 164, 1475–1480.e2. [Google Scholar] [CrossRef] [PubMed]
- McDonald-McGinn, D.M.; Hain, H.S.; Emanuel, B.S.; Zackai, E.H. 22q11.2 Deletion Syndrome. In GeneReviews®; Adam, M.P., Feldman, J., Mirzaa, G.M., Pagon, R.A., Wallace, S.E., Bean, L.J.H., Gripp, K.W., Amemiya, A., Eds.; University of Washington: Seattle, WA, USA, 1999; pp. 1993–2024. [Google Scholar]
- World Health Organization. International Classification of Functioning, Disability and Health: ICF; World Health Organization: Geneva, Switzerland, 2001; 299p. [Google Scholar]
- Havstam, C.; Sandberg, A.D.; Lohmander, A. Communication attitude and speech in 10-year-old children with cleft (lip and) palate: An ICF perspective. Int. J. Speech Lang. Pathol. 2011, 13, 156–164. [Google Scholar] [CrossRef] [PubMed]
- Deckers, S.R.; Van Zaalen, Y.; Stoep, J.; Van Balkom, H.; Verhoeven, L. Communication performance of children with Down Syndrome: An ICF-CY based multiple case study. Child Lang. Teach. Ther. 2016, 32, 293–311. [Google Scholar] [CrossRef]
- Westby, C. Application of the ICF in Children with Language Impairments. Semin. Speech Lang. 2007, 28, 265–272. [Google Scholar] [CrossRef]
- Corrêa, A.P.C.; Ribeiro, C.T.M.; Horovitz, D.D.G.; Ribeiro, L.C. Identification of relevant International Classification of Functioning Disability and Health (ICF) categories in patients with 22q11.2 Deletion Syndrome: A Delphi exercise. CoDAS 2020, 32, e20190158. [Google Scholar] [CrossRef] [PubMed]
- Béfi-Lopes, D.M.; de Andrade, C.R.F. ABFW: Teste de Linguagem Infantil nas Áreas de Fonologia, Vocabulário, Fluência e Pragmática; Pró-Fono: Barueri, Brazil, 2004. [Google Scholar]
- Trentini, C.M.; Yates, D.B.; Heck, V.S. Escala de Inteligência Wechsler Abreviada (WASI): Manual Profissional; Casa do Psicólogo: São Paulo, Brazil, 2014; 488p, Available online: https://sapiens-psi.com.br/wasi-escala-wechsler-abreviada-de-inteligencia-manuall (accessed on 4 January 2022).
- Solot, C.B.; Knightly, C.; Handler, S.D.; Gerdes, M.; McDonald-McGinn, D.M.; Moss, E.; Wang, P.; Cohen, M.; Randall, P.; Larossa, D.; et al. Communication disorders in the 22Q11.2 microdeletion syndrome. J. Commun. Disord. 2000, 33, 187–203, quiz 203–204. [Google Scholar] [CrossRef] [PubMed]
- Antshel, K.M.; Stallone, K.; AbdulSabur, N.; Shprintzen, R.; Roizen, N.; Higgins, A.M.; Kates, W.R. Temperament in velocardiofacial syndrome. J. Intellect. Disabil. Res. 2007, 51, 218–227. [Google Scholar] [CrossRef] [PubMed]
- Tang, K.L.; Antshel, K.M.; Fremont, W.P.; Kates, W.R. Behavioral and Psychiatric Phenotypes in 22q11.2 Deletion Syndrome. J. Dev. Behav. Pediatr. 2015, 36, 639–650. [Google Scholar] [CrossRef] [PubMed]
- Franchini, M.; Schaer, M.; Glaser, B.; Kott-Radecka, M.; Debanné, M.; Schneider, M.; Menghetti, S.; Sander, D.; Eliez, S. Visual processing of emotional dynamic faces in 22q11.2 deletion syndrome: Visual processing of emotional dynamic faces in 22q11DS. J. Intellect. Disabil. Res. 2016, 60, 308–321. [Google Scholar] [CrossRef] [PubMed]
- Niarchou, M.; Zammit, S.; van Goozen, S.H.M.; Thapar, A.; Tierling, H.M.; Owen, M.J.; Bree, M.B.M.V.D. Psychopathology and cognition in children with 22q11.2 deletion syndrome. Br. J. Psychiatry 2014, 204, 46–54. [Google Scholar] [CrossRef] [PubMed]
- Duijff, S.N.; Klaassen, P.W.J.; Swanenburg de Veye, H.F.N.; Beemer, F.A.; Sinnema, G.; Vorstman, J.A.S. Cognitive and behavioral trajectories in 22q11DS from childhood into adolescence: A prospective 6-year follow-up study. Res. Dev. Disabil. 2013, 34, 2937–2945. [Google Scholar] [CrossRef] [PubMed]
- Green, T.; Gothelf, D.; Glaser, B.; Debbane, M.; Frisch, A.; Kotler, M.; Weizman, A.; Eliez, S. Psychiatric disorders and intellectual functioning throughout development in velocardiofacial (22q11.2 deletion) syndrome. J. Am. Acad. Child Adolesc. Psychiatry 2009, 48, 1060–1068. [Google Scholar] [CrossRef] [PubMed]
- Swillen, A.; McDonald-McGinn, D. Developmental trajectories in 22q11.2 deletion syndrome. Am. J. Med. Genet. C Semin. Med. Genet. 2015, 169, 172–181. [Google Scholar] [CrossRef] [PubMed]
- Amelsvoort, T. Cognitive deficits associated with schizophrenia in velo-cardio-facial syndrome. Schizophr. Res. 2004, 70, 223–232. [Google Scholar] [CrossRef] [PubMed]
- McCroskey, J.C.; Richmond, V.P.; Daly, J.A.; Falcione, R.L. Studies of the relationship between communication apprehension and self-esteem. Hum. Commun. Res. 1977, 3, 269–277. [Google Scholar] [CrossRef]
- Beitchman, J.H.; Wilson, B.; Johnson, C.J.; Atkinson, L.; Young, A.; Adlaf, E.; Escobar, M.; Douglas, L. Fourteen-Year Follow-up of Speech/Language-Impaired and Control Children: Psychiatric Outcome. J. Am. Acad. Child Adolesc. Psychiatry 2001, 40, 75–82. [Google Scholar] [CrossRef]
- Dorsman, K.A.; Neumann, J.; Hershberger, M.; Triplett, K.N.; Messiah, S.E.; Edgar, V.B. 22 Adaptive Functioning in 22q11.2 Deletion Syndrome Across the Lifespan: Where are the Social Determinants of Health? J. Int. Neuropsychol. Soc. 2023, 29, 630–631. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).