Daily Behaviors, Worries and Emotions in Children and Adolescents with ADHD and Learning Difficulties during the COVID-19 Pandemic
Abstract
:1. Introduction
2. Materials and Methods
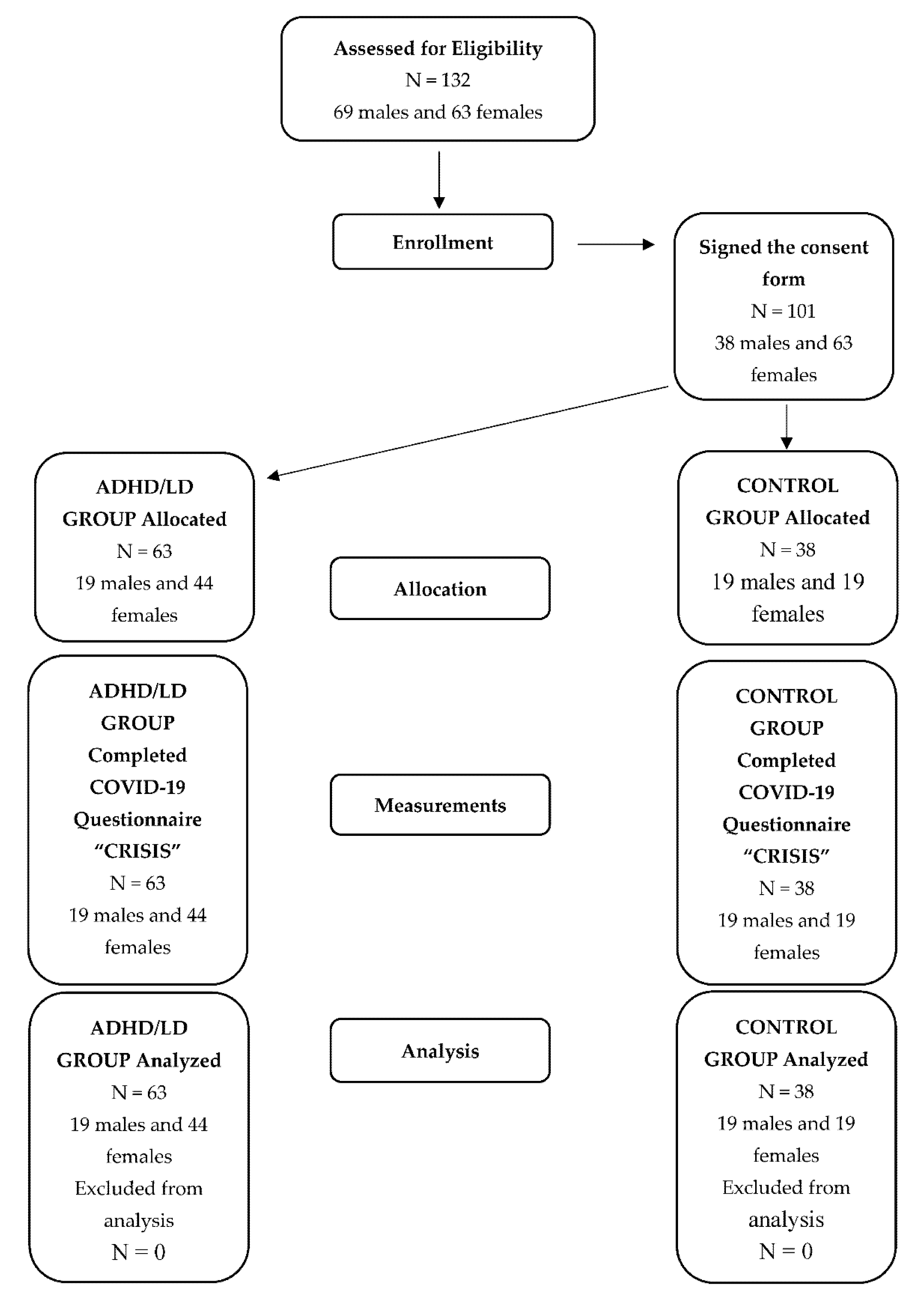
2.1. Procedure
2.2. Participants and Clinical Measures
2.3. Learning Difficulties Screening Procedure
2.3.1. Software for Screening Learning Skills and Difficulties (LAMDA)
2.3.2. Screening of Learning Difficulties for Pupils (SLD)
2.3.3. Reading Test—Alpha Test
2.4. ADHD Screening Procedure
2.4.1. The Child Behavior Checklist (CBCL)–Teacher Report Form (TRF)
2.4.2. ADHD Rating Scale IV (ADHD–RS–IV)
2.4.3. Kiddie–Schedule for Affective Disorders and Schizophrenia–Present and Lifetime Version (K–SADS–PL)
2.5. The Coronavirus Health Impact Survey (CRISIS)
Variables Extrapolated from the CRISIS Questionnaire
3. Results
3.1. Statistical Analysis
3.2. Outcome and Types of Analyses
3.3. Descriptive Statistics
3.4. Exploratory Analyses
3.5. SEM for EW-d
3.6. Changes in Items in the Domains “Daily Behaviours” and “Use of Digital Media”
4. Discussion
4.1. Emotional and Psychological Effects
4.2. Behavioural Effects
4.3. Strengths and Limitations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- AAP. Clinical practice guideline: Diagnosis and evaluation of the child with attention-deficit/hyperactivity disorder. American Academy of Pediatrics. Pediatrics 2000, 105, 1158–1170. [Google Scholar] [CrossRef]
- Lecendreux, M.; Konofal, E.; Faraone, S.V. Prevalence of attention deficit hyperactivity disorder and associated features among children in France. J. Atten. Disord. 2011, 15, 516–524. [Google Scholar] [CrossRef] [PubMed]
- DuPaul, G.J.; Volpe, R.J. ADHD and learning disabilities: Research findings and clinical implications. Curr. Atten. Disord. Rep. 2009, 1, 152–155. [Google Scholar] [CrossRef]
- Fletcher, J.M.; Shaywitz, S.E.; Shaywitz, B.A. Comorbidity of learning and attention disorders. Separate but equal. Pediatr. Clin. N. Am. 1999, 46, 885–897. [Google Scholar] [CrossRef]
- DuPaul, G.J.; Gormley, M.J.; Laracy, S.D. Comorbidity of LD and ADHD: Implications of DSM-5 for Assessment and Treatment. J. Learn. Disabil. 2013, 46, 43–51. [Google Scholar] [CrossRef] [PubMed]
- Sahoo, M.K.; Biswas, H.; Padhy, S.K. Psychological Co-morbidity in Children with Specific Learning Disorders. J. Fam. Med. Prim. Care 2015, 4, 21–25. [Google Scholar] [CrossRef]
- DuPaul, G.J.; Pinho, T.D.; Pollack, B.L.; Gormley, M.J.; Laracy, S.D. First-Year College Students with ADHD and/or LD: Differences in Engagement, Positive Core Self-Evaluation, School Preparation, and College Expectations. J. Learn. Disabil. 2017, 50, 238–251. [Google Scholar] [CrossRef] [PubMed]
- DaDeppo, L.M.W. Integration Factors Related to the Academic Success and Intent to Persist of College Students with Learning Disabilities. Learn. Disabil. Res. Pract. 2009, 24, 122–131. [Google Scholar] [CrossRef]
- Kok, F.M.; Groen, Y.; Fuermaier, A.B.M.; Tucha, O. Problematic Peer Functioning in Girls with ADHD: A Systematic Literature Review. PLoS ONE 2016, 11, e0165119. [Google Scholar] [CrossRef]
- Mannuzza, S.; Klein, R.G. Long-term prognosis in attention-deficit/hyperactivity disorder. Child Adolesc. Psychiatr. Clin. N. Am. 2000, 9, 711–726. [Google Scholar] [CrossRef]
- Leitch, S.; Sciberras, E.; Post, B.; Gerner, B.; Rinehart, N.; Nicholson, J.M.; Evans, S. Experience of stress in parents of children with ADHD: A qualitative study. Int. J. Qual. Stud. Health Well-Being 2019, 14, 1690091. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Korpa, T.; Alexander, A.; Katsounas, M. Parenting stress and psychopathology in mothers of children with ADHD. Educ. Res. 2018, 8, 47–56. [Google Scholar]
- Edwards, G.; Barkley, R.A.; Laneri, M.; Fletcher, K.; Metevia, L. Parent-adolescent conflict in teenagers with ADHD and ODD. J. Abnorm. Child Psychol. 2001, 29, 557–572. [Google Scholar] [CrossRef]
- Lifford, K.J.; Harold, G.T.; Thapar, A. Parent–Child Relationships and ADHD Symptoms: A Longitudinal Analysis. J. Abnorm. Child Psychol. 2008, 36, 285–296. [Google Scholar] [CrossRef]
- Burt, S.A.; Krueger, R.F.; McGue, M.; Iacono, W. Parent-child conflict and the comorbidity among childhood externalizing disorders. Arch. Gen. Psychiatry 2003, 60, 505–513. [Google Scholar] [CrossRef] [Green Version]
- Viner, R.M.; Russell, S.J.; Croker, H.; Packer, J.; Ward, J.; Stansfield, C.; Mytton, O.; Bonell, C.; Booy, R. School closure and management practices during coronavirus outbreaks including COVID-19: A rapid systematic review. Lancet Child Adolesc. Health 2020, 4, 397–404. [Google Scholar] [CrossRef]
- Allen, K.; Kern, M.L.; Vella-Brodrick, D.; Hattie, J.; Waters, L. What Schools Need to Know About Fostering School Belonging: A Meta-analysis. Educ. Psychol. Rev. 2018, 30, 1–34. [Google Scholar] [CrossRef]
- Jose, P.E.; Ryan, N.; Pryor, J. Does Social Connectedness Promote a Greater Sense of Well-Being in Adolescence Over Time? J. Res. Adolesc. 2012, 22, 235–251. [Google Scholar] [CrossRef]
- Brooks, S.K.; Smith, L.E.; Webster, R.K.; Weston, D.; Woodland, L.; Hall, I.; Rubin, G.J. The impact of unplanned school closure on children’s social contact: Rapid evidence review. Eurosurveillance 2020, 25, 2000188. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Loades, M.E.; Chatburn, E.; Higson-Sweeney, N.; Reynolds, S.; Shafran, R.; Brigden, A.; Linney, C.; McManus, M.N.; Borwick, C.; Crawley, E. Rapid Systematic Review: The Impact of Social Isolation Adolescents in the Context of COVID-19. J. Am. Acad. Child Adolesc. Psychiatry 2020, 59, 1218–1239. [Google Scholar] [CrossRef] [PubMed]
- Jiao, W.Y.; Na Wang, L.; Liu, J.; Fang, S.F.; Jiao, F.Y.; Pettoello-Mantovani, M.; Somekh, E. Behavioral and Emotional Disorders in Children during the COVID-19 Epidemic. J. Pediatr. 2020, 221, 264–266.e1. [Google Scholar] [CrossRef] [PubMed]
- Pizarro-Ruiz, J.P.; Ordóñez-Camblor, N. Effects of COVID-19 confinement on the mental health of children and adolescents in Spain. Sci. Rep. 2021, 11, 11713. [Google Scholar] [CrossRef]
- Cui, Y.; Li, Y.; Zheng, Y. Mental health services for children in China during the COVID-19 pandemic: Results of an expert-based national survey among child and adolescent psychiatric hospitals. Eur. Child Adolesc. Psychiatry 2020, 29, 743–748. [Google Scholar] [CrossRef]
- Breaux, R.; Dvorsky, M.R.; Marsh, N.P.; Green, C.D.; Cash, A.R.; Shroff, D.M.; Buchen, N.; Langberg, J.M.; Becker, S.P. Prospective impact of COVID-19 on mental health functioning in adolescents with and without ADHD: Protective role of emotion regulation abilities. J. Child Psychol. Psychiatry 2021, 62, 1132–1139. [Google Scholar] [CrossRef]
- Ravens-Sieberer, U.; Kaman, A.; Erhart, M.; Devine, J.; Schlack, R.; Otto, C. Impact of the COVID-19 pandemic on quality of life and mental health in children and adolescents in Germany. Eur. Child Adolesc. Psychiatry 2021, 1–11. [Google Scholar] [CrossRef]
- Ellis, W.E.; Dumas, T.M.; Forbes, L.M. Physically isolated but socially connected: Psychological adjustment and stress among adolescents during the initial COVID-19 crisis. Can. J. Behav. Sci. Rev. Can. Sci. Comport. 2020, 52, 177–187. [Google Scholar] [CrossRef]
- Xie, X.; Xue, Q.; Zhou, Y.; Zhu, K.; Liu, Q.; Zhang, J.; Song, R. Mental Health Status among Children in Home Confinement during the Coronavirus Disease 2019 Outbreak in Hubei Province, China. JAMA Pediatr. 2020, 174, 898–900. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Summers, J.; Baribeau, D.; Mockford, M.; Goldhopf, L.; Ambrozewicz, P.; Szatmari, P.; Vorstman, J. Supporting Children with Neurodevelopmental Disorders during the COVID-19 Pandemic. J. Am. Acad. Child Adolesc. Psychiatry 2021, 60, 2–6. [Google Scholar] [CrossRef]
- Protopappas, A.; Skaloumbakas, C. Software for screening learning skills and difficulties (LAMDA). Greek Minist. Educ. Res. Relig. Aff. EPEAEK II Action 2008, 1. [Google Scholar]
- Panteliadou, S.; Antoniou, F. Screening of Learning Difficulties for pupils. In Assessing Second Language Students with Learning and Other Disabilities; Tsagari, D., Spanoudis, G., Eds.; Cambridge Scholars Publishing: Newcastle, UK, 2007. [Google Scholar]
- Panteliadou, S.; Antoniou, F. Reading Test-Alpha Test. In Assessing Second Language Students with Learning and Other Disabilities; Tsagari, D., Spanoudis, G., Eds.; Cambridge Scholars Publishing: Newcastle, UK, 2007. [Google Scholar]
- Achenbach, M.; Rescorla, A. Manual for the ASEBA School-Age Forms & Profiles; ASEBA: Burlington, NJ, USA, 2001. [Google Scholar]
- DuPaul, G.J.; Power, T.J.; McGoey, K.E.; Ikeda, M.J.; Anastopoulos, A.D. Reliability and Validity of Parent and Teacher Ratings of Attention-Deficit/Hyperactivity Disorder Symptoms. J. Psychoeduc. Assess. 1998, 16, 55–68. [Google Scholar] [CrossRef] [Green Version]
- Kolaitis, G.; Korpa, T.; Kolvin, I.; Tsiantis, J. Schedule for affective disorders and schizophrenia for school-age children-present episode (K-SADS-P): A pilot inter-rater reliability study for Greek children and adolescents. Eur. Psychiatry 2003, 18, 374–375. [Google Scholar] [CrossRef]
- Nikolaidis, A.; Paksarian, D.; Alexander, L.; Derosa, J.; Dunn, J.; Nielson, D.M.; Droney, I.; Kang, M.; Douka, I.; Bromet, E.; et al. The Coronavirus Health and Impact Survey (CRISIS) reveals reproducible correlates of pandemic-related mood states across the Atlantic. Sci. Rep. 2021, 11, 8139. [Google Scholar] [CrossRef]
- Guryan, J.; Hurst, E.; Kearney, M. Parental education and parental time with children. J. Econ. Perspect. 2008, 22, 23–46. [Google Scholar] [CrossRef] [Green Version]
- Torvik, F.A.; Eilertsen, E.M.; McAdams, T.A.; Gustavson, K.; Zachrisson, H.D.; Brandlistuen, R.; Gjerde, L.C.; Havdahl, A.; Stoltenberg, C.; Ask, H.; et al. Mechanisms linking parental educational attainment with child ADHD, depression, and academic problems: A study of extended families in The Norwegian Mother, Father and Child Cohort Study. J. Child Psychol. Psychiatry 2020, 61, 1009–1018. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shiels, K.; Hawk, L.W. Self-regulation in ADHD: The role of error processing. Clin. Psychol. Rev. 2010, 30, 951–961. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Solanto, M.V.; Pope-Boyd, S.A.; Tryon, W.W.; Stepak, B. Social functioning in predominantly inattentive and combined subtypes of children with ADHD. J. Atten. Disord. 2009, 13, 27–35. [Google Scholar] [CrossRef] [Green Version]
- Graziano, P.A.; McNamara, J.P.; Geffken, G.R.; Reid, A.M. Differentiating co-occurring behavior problems in children with ADHD: Patterns of emotional reactivity and executive functioning. J. Atten. Disord. 2013, 17, 249–260. [Google Scholar] [CrossRef] [PubMed]
- Gerdes, A.C.; Hoza, B.; Arnold, L.E.; Hinshaw, S.P.; Wells, K.C.; Hechtman, L.; Greenhill, L.L.; Swanson, J.M.; Pelham, J.W.E.; Wigal, T. Child and parent predictors of perceptions of parent-child relationship quality. J. Atten. Disord. 2007, 11, 37–48. [Google Scholar] [CrossRef]
- Bobo, E.; Lin, L.; Acquaviva, E.; Caci, H.; Franc, N.; Gamon, L.; Picot, M.-C.; Pupier, F.; Speranza, M.; Falissard, B.; et al. How do children and adolescents with Attention Deficit Hyperactivity Disorder (ADHD) experience lockdown during the COVID-19 outbreak? Encephale 2020, 46, S85–S92. [Google Scholar] [CrossRef]
- Tang, S.; Xiang, M.; Cheung, T.; Xiang, Y.-T. Mental health and its correlates among children and adolescents during COVID-19 school closure: The importance of parent-child discussion. J. Affect. Disord. 2021, 279, 353–360. [Google Scholar] [CrossRef] [PubMed]
- Sciberras, E.; Patel, P.; Stokes, M.A.; Coghill, D.; Middeldorp, C.M.; Bellgrove, M.A.; Becker, S.P.; Efron, D.; Stringaris, A.; Faraone, S.V.; et al. Physical Health, Media Use, and Mental Health in Children and Adolescents with ADHD during the COVID-19 Pandemic in Australia. J. Atten. Disord. 2020, 12, 1087054720978549. [Google Scholar] [CrossRef]
- Qin, Z.; Shi, L.; Xue, Y.; Lin, H.; Zhang, J.; Liang, P.; Lu, Z.; Wu, M.; Chen, Y.; Zheng, X.; et al. Prevalence and Risk Factors Associated with Self-Reported Psychological Distress among Children and Adolescents during the COVID-19 Pandemic in China. JAMA Netw. Open 2021, 4, e2035487. [Google Scholar] [CrossRef]
- Magson, N.R.; Freeman, J.Y.A.; Rapee, R.M.; Richardson, C.E.; Oar, E.L.; Fardouly, J. Risk and Protective Factors for Prospective Changes in Adolescent Mental Health during the COVID-19 Pandemic. J. Youth Adolesc. 2021, 50, 44–57. [Google Scholar] [CrossRef]
- Lee, S.A.; Jobe, M.C.; Mathis, A.A. Mental health characteristics associated with dysfunctional coronavirus anxiety. Psychol. Med. 2021, 51, 1403–1404. [Google Scholar] [CrossRef] [Green Version]
- Abdelfattah, F.; Rababah, A.; Alqaryouti, I.; Alsartawi, Z.; Khlaifat, D.; Awamleh, A. Exploring feelings of worry and sources of stress during COVID-19 pandemic among parents of children with disability: A sample from Arab countries. Educ. Sci. 2021, 11, 216. [Google Scholar] [CrossRef]
- Vogel, M.; Meigen, C.; Sobek, C.; Ober, P.; Igel, U.; Körner, A.; Kiess, W.; Poulain, T. Well-being and COVID-19-related worries of German children and adolescents: A longitudinal study from pre-COVID to the end of lockdown in Spring 2020. JCPP Adv. 2021, 1, e12004. [Google Scholar] [CrossRef] [PubMed]
- Romero-Blanco, C.; Rodríguez-Almagro, J.; Onieva-Zafra, M.D.; Parra-Fernández, M.L.; Prado-Laguna, M.D.C.; Hernández-Martínez, A. Physical Activity and Sedentary Lifestyle in University Students: Changes during Confinement Due to the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2020, 17, 6567. [Google Scholar] [CrossRef]
- Belfort, E.L.; Miller, L. Relationship Between Adolescent Suicidality, Self-Injury, and Media Habits. Child Adolesc. Psychiatr. Clin. N. Am. 2018, 27, 159–169. [Google Scholar] [CrossRef]
- Wade, M.; Prime, H.; Browne, D.T. Why we need longitudinal mental health research with children and youth during (and after) the COVID-19 pandemic. Psychiatry Res. 2020, 290, 113143. [Google Scholar] [CrossRef] [PubMed]
- Öster, C.; Ramklint, M.; Meyer, J.; Isaksson, J. How do adolescents with ADHD perceive and experience stress? An interview study. Nord. J. Psychiatry 2020, 74, 123–130. [Google Scholar] [CrossRef] [PubMed] [Green Version]

| ADHD | Controls | p-Value | |
|---|---|---|---|
| Caregiver age, years | 44.8 ± 5.4 (40 to 48) | 43.4 ± 6.2 (38 to 49) | 0.25 |
| Caregiver relation to child | 0.10 | ||
| Mother | 46 (73.0) | 21 (55.3) | |
| Father | 16 (25.4) | 17 (44.7) | |
| Grandparent | 1 (1.6) | 0 (0.0) | |
| Greek origin | 62 (98.4) | 35 (92.1) | 0.15 |
| Living area | 0.022 | ||
| Large city | 54 (85.7) | 30 (79.0) | |
| Small city | 4 (6.4) | 8 (21.0) | |
| Village | 5 (7.9) | 0 (0.0) | |
| Single-parent family | 77 (11.1) | 6 (15.8) | 0.55 |
| Presence of elderly people at home | 5 (7.9) | 2 (5.3) | 0.71 |
| Presence of other children at home | 37 (58.7) | 27 (71.1) | 0.28 |
| Number of other persons at home | 2.9 ± 0.7 3 (3, 3) | 2.8 ± 0.9, 3 (2, 3) | 0.71 |
| Working during quarantine | 3 (7.9) | 35 (92.1) | <0.001 |
| Working but living in home | 29 (46.0) | 35 (100.0) | <0.001 |
| Healthcare worker | 6 (9.5) | 0 (0.0) | 0.09 |
| Number of rooms at home | 4.4 ± 1.6, 4 (3, 5) | 5.4 ± 1.0, 5 (5, 6) | 0.001 |
| Insurance | 61 (96.8) | 38 (100.0) | 0.52 |
| Subsidy | 14 (22.2) | 2 (5.3) | 0.026 |
| Child’s physical health status according to caregiver n (%) | 0.075 | ||
| Excellent | 39 (61.9) | 32 (84.2) | |
| Very good | 18 (28.6) | 6 (15.8) | |
| Good | 4 (6.3) | 0 (0.0) | |
| Fair | 2 (3.2) | 0 (0.0) | |
| Poor | 0 (0.0) | 0 (0.0) | |
| Child’s mental health status according to caregiver n (%) | <0.001 | ||
| Excellent | 23 (36.5) | 34 (89.5) | |
| Very good | 26 (41.3) | 4 (10.5) | |
| Good | 12 (19.0) | 0 (0.0) | |
| Fair | 2 (3.2) | 0 (0.0) | |
| Poor | 0 (0.0) | 0 (0.0) |
| logEW-b *** | β-Coefficient | 95% CI | p-Value |
|---|---|---|---|
| Interaction ADHD–Parental perception of child’s mental health (worsening) | 0.140 | 0.091, 0.189 | <0.001 |
| Increasing parental educational level | −0.030 | −0.047, −0.013 | <0.001 |
| Interaction ADHD–provision of activities support | 0.126 | 0.032, 0.220 | 0.009 |
| Educational support, yes vs. no | 0.121 | 0.041, 0.201 | 0.003 |
| Interaction ADHD-number of persons at home | 0.044 | 0.003, 0.085 | 0.035 |
| logEW-d | |||
| logEW-b | 0.563 | 0.414, 0.713 | <0.001 |
| logCOVID-worries | 0.137 | 0.035, 0.238 | 0.008 |
| Parental perception of child’s mental health (worsening) | 0.065 | 0.015, 0.115 | 0.010 |
| Stress due to restrictions | 0.059 | 0.022, 0.095 | 0.002 |
| Relations with friends (improved) | −0.080 | −0.141, −0.019 | 0.009 |
| Change in contacts (more contacts outside home) | −0.060 | −0.093, −0.026 | <0.001 |
| Interaction ADHD–reporting of physical health problems | 0.102 | −0.0004, 0.204 | 0.051 |
| Interaction ADHD–child’s age | −0.015 | −0.025, −0.005 | 0.003 |
| Interaction ADHD–parental educational level | 0.016 | 0.003, 0.028 | 0.013 |
| Measure of Goodness-of-Fit | Results |
|---|---|
| Chi-square test a | 13.914 (13), 0.380 |
| RMSEA b | 0.027 (<0.001, 0.104), 0.605 |
| SRMR c | 0.021 |
| CDet d | 0.807 |
| Item (Probability of Worsening) | ADHD Patients (N = 63) | Controls (N = 38) | p-Value |
|---|---|---|---|
| Bedtime weekdays (later) | 25 (39.7%) | 33 (86.8%) | <0.001 |
| Bedtime weekend (later) | 16 (25.4%) | 26 (68.4%) | <0.001 |
| Sleeping hours weekdays (more) | 17 (27.0%) | 21 (55.3%) | 0.006 |
| Sleeping hours weekend (more) | 5 (7.9%) | 12 (31.6%) | 0.005 |
| Physical exercise (less) | 32 (50.8%) | 20 (52.6%) | 0.99 |
| Time spent outdoors (less) | 24 (38.1%) | 32 (84.2%) | <0.001 |
| TV (more) | 22 (34.9%) | 37 (97.4%) | <0.001 |
| Social media (more) | 18 (28.6%) | 20 (52.6%) | 0.020 |
| Videogames (more) | 16 (25.4%) | 17 (44.7%) | 0.05 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Korpa, T.; Pappa, T.; Chouliaras, G.; Sfinari, A.; Eleftheriades, A.; Katsounas, M.; Kanaka-Gantenbein, C.; Pervanidou, P. Daily Behaviors, Worries and Emotions in Children and Adolescents with ADHD and Learning Difficulties during the COVID-19 Pandemic. Children 2021, 8, 995. https://doi.org/10.3390/children8110995
Korpa T, Pappa T, Chouliaras G, Sfinari A, Eleftheriades A, Katsounas M, Kanaka-Gantenbein C, Pervanidou P. Daily Behaviors, Worries and Emotions in Children and Adolescents with ADHD and Learning Difficulties during the COVID-19 Pandemic. Children. 2021; 8(11):995. https://doi.org/10.3390/children8110995
Chicago/Turabian StyleKorpa, Terpsichori, Theodora Pappa, Giorgos Chouliaras, Anastasia Sfinari, Anna Eleftheriades, Matthaios Katsounas, Christina Kanaka-Gantenbein, and Panagiota Pervanidou. 2021. "Daily Behaviors, Worries and Emotions in Children and Adolescents with ADHD and Learning Difficulties during the COVID-19 Pandemic" Children 8, no. 11: 995. https://doi.org/10.3390/children8110995
APA StyleKorpa, T., Pappa, T., Chouliaras, G., Sfinari, A., Eleftheriades, A., Katsounas, M., Kanaka-Gantenbein, C., & Pervanidou, P. (2021). Daily Behaviors, Worries and Emotions in Children and Adolescents with ADHD and Learning Difficulties during the COVID-19 Pandemic. Children, 8(11), 995. https://doi.org/10.3390/children8110995







