1. Introduction
Intussusception is one of the most common causes of intestinal obstruction in children [
1,
2]. The diagnosis is usually confirmed by ultrasound, which has 98–100% sensitivity and 88% specificity [
3]. Pneumatic reduction (PR) is the gold standard of treatment in children with intussusception and has been shown to be safe and effective, with reported success rates of over 80% [
4,
5,
6]. However, when multiple attempts at PR fails to reduce intussusception, it must be performed manually by surgical means. Known contraindications for PR are peritonitis and intestinal perforation [
7,
8,
9]. In addition, the presence of a pathological leading point (PLP) is a major factor associated with PR failure [
10]. However, in a considerable number of cases without an apparent PLP, PR is unsuccessful in reducing intussusception, and surgical reduction is required. Here, we evaluated the factors associated with PR failure in pediatric cases of ileocolic intussusception without PLPs.
2. Materials and Methods
Data were collected retrospectively from two tertiary hospitals. All children aged 0–14 years who were diagnosed with intussusception between January 2013 and December 2014 were evaluated. The diagnosis and classification of intussusception were confirmed by ultrasound. Only patients with ileocolic-type intussusception were included, and patients with other types of intussusception and those with pathologically confirmed PLPs were excluded. All PR procedures were performed under fluoroscopy, and when PR failed, the patient was transferred to the operative room for surgical reduction.
Data on patient characteristics (age, weight, and weight percentile) and clinical and laboratory data (body temperature, white blood cell count with differential, hemoglobin levels, C-reactive protein levels, and absolute neutrophil count) were collected, and their association with PR failure was analyzed using univariate and multivariate logistic regression analyses. A receiver operating characteristic (ROC) curve was constructed to determine the optimum cutoff values of the significant factors. Statistical analyses were conducted using SPSS software (version 8.0, SPSS Inc., Chicago, IL, USA).
This study was approved by the Institutional Review Board of Samsung Medical Center (IRB number 2018-10-075), and the requirement for informed consent was waived.
3. Results
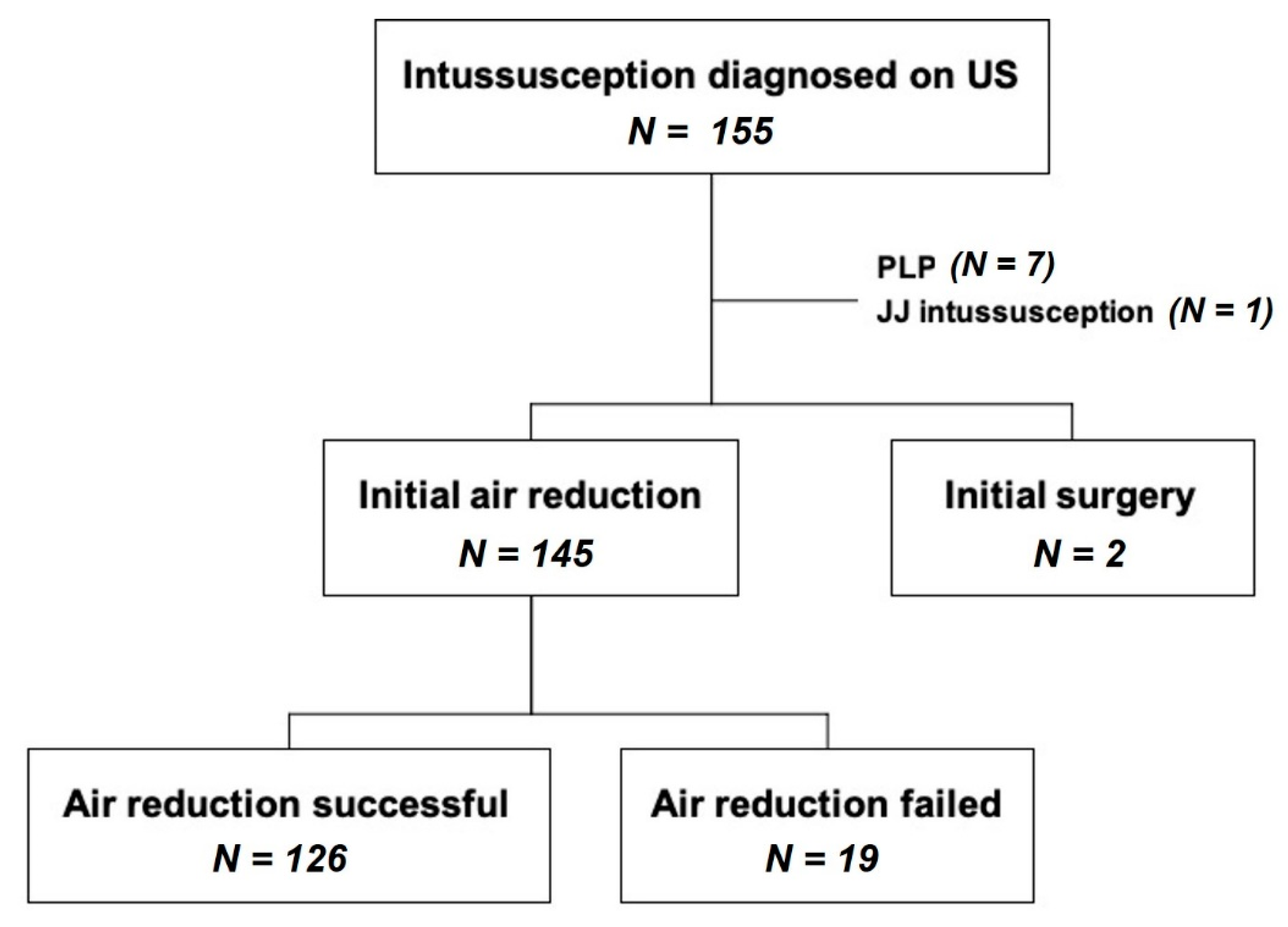
In the two hospitals, 155 patients were diagnosed with intussusception during the study period. Ten patients were excluded from the study for the following reasons: two patients presented with signs of peritonitis and underwent surgery without PR, seven patients demonstrated PLPs on postoperative pathologic evaluation, and one patient had jejunojejunal intussusception. The remaining 145 children with ileocolic intussusception were analyzed (
Figure 1).
The patient characteristics are shown in
Table 1. The mean age at diagnosis was 24.6 months, and there were 95 boys and 50 girls. The body weight percentiles of approximately 56% of the patients were in the range of 25–75%.
Univariate analysis showed that a high segmented neutrophil count (
p = 0.017, odds ratio [OR] 1.046, 95% confidence interval [CI] 1.008~1.086), low hemoglobin level (
p = 0.01, OR 0.545, 95% CI 0.334~0.863), high body temperature (
p = 0.049, OR 2.203, 95% CI 1.004~4.837), and high weight percentile (
p = 0.015, OR 1.567, 95% CI 1.093~2.247) were significant factors associated with the failure of PR. Multivariate analysis was performed with the variables that were significant in univariate analysis and showed that a high segmented neutrophil count (
p = 0.014, OR 1.052, 95% CI 1.010~1.095), low hemoglobin level (
p = 0.018, OR 0.522, 95% CI 0.304~0.896), and higher weight percentile (
p = 0.01, OR 1.668, 95% CI 1.032~2.457) were independent risk factors for PR failure (
Table 2).
ROC curves were used to determine significant cutoff values associated with a negative impact on PR success. A segmental neutrophil level >67.3% (95% CI 1.735–15.609), hemoglobin level <12.2 g/dL (95% CI 2.247–22.86), and weight percentile >75% (95% CI 1.275–12.28) significantly affected the efficacy of PR.
4. Discussion
Intussusception is a common cause of acute abdomen in children requiring surgery. Fortunately, most patients can be treated with non-surgical treatments such as air enema reduction. PR is the first-line treatment for intussusception and is both safe and effective, with a reported success rate of more than 80% [
4,
11,
12]. Surgical treatment is required for patients in whom PR fails after multiple attempts. In this study, PR failed in 12.9% of patients who subsequently underwent surgical reduction. Additionally, we identified three independent risk factors associated with pneumatic reduction failure in the absence of a PLP: low hemoglobin level, high segmental neutrophil level, and higher weight percentiles.
Early identification of patients who are likely to show PR failure is important for avoiding excessive PR. Intestinal perforation may occur if PR is performed with excessive air pressure in patients with a high probability of failure. Second, if pediatric surgeons receive an early notification regarding patients with a high probability of failure of air enema reduction, it is possible for them to be prepared to proceed with rapid surgical treatment after PR failure. Therefore, it is important to investigate objective indicators that can identify patients with a high probability of PR failure.
A symptom duration of >24 h, rectal bleeding, extremes of age, rectal prolapse, severe dehydration, and radiological signs of obstruction have been reported to negatively impact pneumatic reduction [
5,
12,
13,
14]. However, these factors are not considered absolute contraindications for PR. In this study, three factors negatively affected the effectiveness of PR: a low hemoglobin level (g/dL), high segmental neutrophil level (%), and high body weight percentile (%). A low hemoglobin level, which could be explained by rectal bleeding, has been reported to be significantly associated with PR failure [
15], and a low hemoglobin level was significant when the level was <12.2 g/dL in the current study. Segmental neutrophils are also associated with PR failure [
12], and in the current study, this parameter was significant if the level was >67.3%. However, the body weight percentile has not been addressed in previous reports, but it was associated with PR failure when the percentile was >75% in our series. Despite the presence of factors that affect its efficacy, PR remains the first-line treatment for pediatric intussusception in the absence of peritonitis and reduces the frequency of unnecessary laparotomy [
12,
16]. Our findings regarding the factors that negatively affect successful PR can be used to alert physicians to initiate an early surgical consultation.
This study had several limitations. First, this was a retrospective study, which is associated with risk of various bias in data collection and interpretation. Second, duration of symptoms, which is a well-known risk factor for failure of PR, was not included in the analysis [
4,
12,
14]. Although exclusion of this variable was intended to minimize the possibility of recall bias, excluding symptom duration from the risk factor analysis may have impacted the results. Symptom duration is related to the variables found to be significant risk factors in this study. Longer duration of symptoms would lead to inflammation and venous bleeding from the bowel segment and subsequently elevated segmented neutrophil levels and decreased hemoglobin. Third, it is not possible to definitely confirm the absence of PLPs unless surgery is performed in these patients. Thus, a small proportion of patients among those who underwent successful pneumatic reduction actually had underlying PLPs. However, a patient with a PLP would be more likely to have recurrence of intussusception. Non-recurrence after pneumatic reduction in these patients supports the likelihood that they have been without PLPs at the time of successful pneumatic reduction.
In conclusion, although PR is highly effective in reducing intussusception in children, a low hemoglobin level, a high segmental neutrophil level, and higher weight percentiles were associated with pneumatic reduction failure in the absence of a PLP.
Author Contributions
Conceptualization, S.L. and S.-M.J.; methodology, J.-I.L.; formal analysis, S.L. and A.Y.; investigation, S.-M.J. and A.Y.; resources, J.-M.S.; data curation, J.-I.L., S.-M.J. and J.-M.S.; writing—original draft preparation, A.Y. and S.L.; writing—review and editing, S.L. and S.-M.J.; supervision, J.-M.S.; project administration, S.-M.J. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Institutional Review Board of Samsung Medical Center (IRB number 2018-10-075).
Informed Consent Statement
Patient consent was waived by the Institutional Review Board of Samsung Medical Center.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
Abbreviations
| PR | pneumatic reduction |
| PLP | pathological leading point |
References
- Parashar, U.D.; Holman, R.C.; Cummings, K.C.; Staggs, N.W.; Curns, A.T.; Zimmerman, C.M.; Kaufman, S.F.; Lewis, J.E.; Vugia, D.J.; Powell, K.E.; et al. Trends in intussusception-associated hospitalizations and deaths among US infants. Pediatrics 2000, 106, 1413–1421. [Google Scholar] [CrossRef] [PubMed]
- Yoshimaru, K.; Kinoshita, Y.; Matsuura, T.; Esumi, G.; Wada, M.; Takahashi, Y.; Yanagi, Y.; Hayashida, M.; Ieiri, S.; Taguchi, T. Bowel obstruction without history of laparotomy: Clinical analysis of 70 patients. Pediatr. Int. 2016, 58, 1205–1210. [Google Scholar] [CrossRef] [PubMed]
- Verschelden, P.; Filiatrault, D.; Garel, L.; Grignon, A.; Perreault, G.; Boisvert, J.; Dubois, J. Intussusception in children: Reliability of US in diagnosis--a prospective study. Radiology 1992, 184, 741–744. [Google Scholar] [CrossRef] [PubMed]
- Beres, A.L.; Baird, R. An institutional analysis and systematic review with meta-analysis of pneumatic versus hydrostatic reduction for pediatric intussusception. Surgery 2013, 154, 328–334. [Google Scholar] [CrossRef] [PubMed]
- Stein, M.; Alton, D.J.; Daneman, A. Pneumatic reduction of intussusception: 5-year experience. Radiology 1992, 183, 681–684. [Google Scholar] [CrossRef] [PubMed]
- Sorantin, E.; Lindbichler, F. Management of intussusception. Eur. Radiol. 2004, 14 (Suppl. 4), L146–L154. [Google Scholar] [PubMed]
- Applegate, K.E. Clinically suspected intussusception in children: Evidence-based review and self-assessment module. AJR Am. J. Roentgenol. 2005, 185, S175–S183. [Google Scholar] [CrossRef] [PubMed]
- Zheng, J.Y.; Frush, D.P.; Guo, J.Z. Review of pneumatic reduction of intussusception: Evolution not revolution. J. Pediatr. Surg. 1994, 29, 93–97. [Google Scholar] [CrossRef]
- Beasley, S.W.; Glover, J. Intussusception: Prediction of outcome of gas enema. J. Pediatr. Surg. 1992, 27, 474–475. [Google Scholar] [CrossRef]
- Columbani, P.; Scholz, S. Intussusception. In Pediatric Surgery, 7th ed.; Elsevier Saunders: Philadelphia, PA, USA, 2012; pp. 1095–1099. [Google Scholar]
- Estevao-Costa, J.; Correia-Pinto, J.; Campos, M.; Mariz, C.; Carvalho, J.L. [Intestinal invagination in children. Reduction with pneumo-enema]. Acta Med. Port. 2001, 14, 381–384. [Google Scholar] [PubMed]
- Fragoso, A.C.; Campos, M.; Tavares, C.; Costa-Pereira, A.; Estevao-Costa, J. Pneumatic reduction of childhood intussusception. Is prediction of failure important? J. Pediatr. Surg. 2007, 42, 1504–1508. [Google Scholar] [CrossRef] [PubMed]
- Ramachandran, P.; Gupta, A.; Vincent, P.; Sridharan, S. Air enema for intussusception: Is predicting the outcome important? Pediatr. Surg. Int. 2008, 24, 311–313. [Google Scholar] [CrossRef] [PubMed]
- Fallon, S.C.; Lopez, M.E.; Zhang, W.; Brandt, M.L.; Wesson, D.E.; Lee, T.C.; Rodriguez, J.R. Risk factors for surgery in pediatric intussusception in the era of pneumatic reduction. J. Pediatr. Surg. 2013, 48, 1032–1036. [Google Scholar] [CrossRef] [PubMed]
- Guo, J.Z.; Ma, X.Y.; Zhou, Q.H. Results of air pressure enema reduction of intussusception: 6396 cases in 13 years. J. Pediatr. Surg. 1986, 21, 1201–1203. [Google Scholar] [CrossRef]
- Den Hollander, D.; Burge, D.M. Exclusion criteria and outcome in pressure reduction of intussusception. Arch. Dis. Child. 1993, 68, 79–81. [Google Scholar] [CrossRef] [PubMed][Green Version]
| Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).