Subtalar Arthroereisis for Flexible Flatfoot in Children—Clinical, Radiographic and Pedobarographic Outcome Comparing Three Different Methods
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patients and Indications
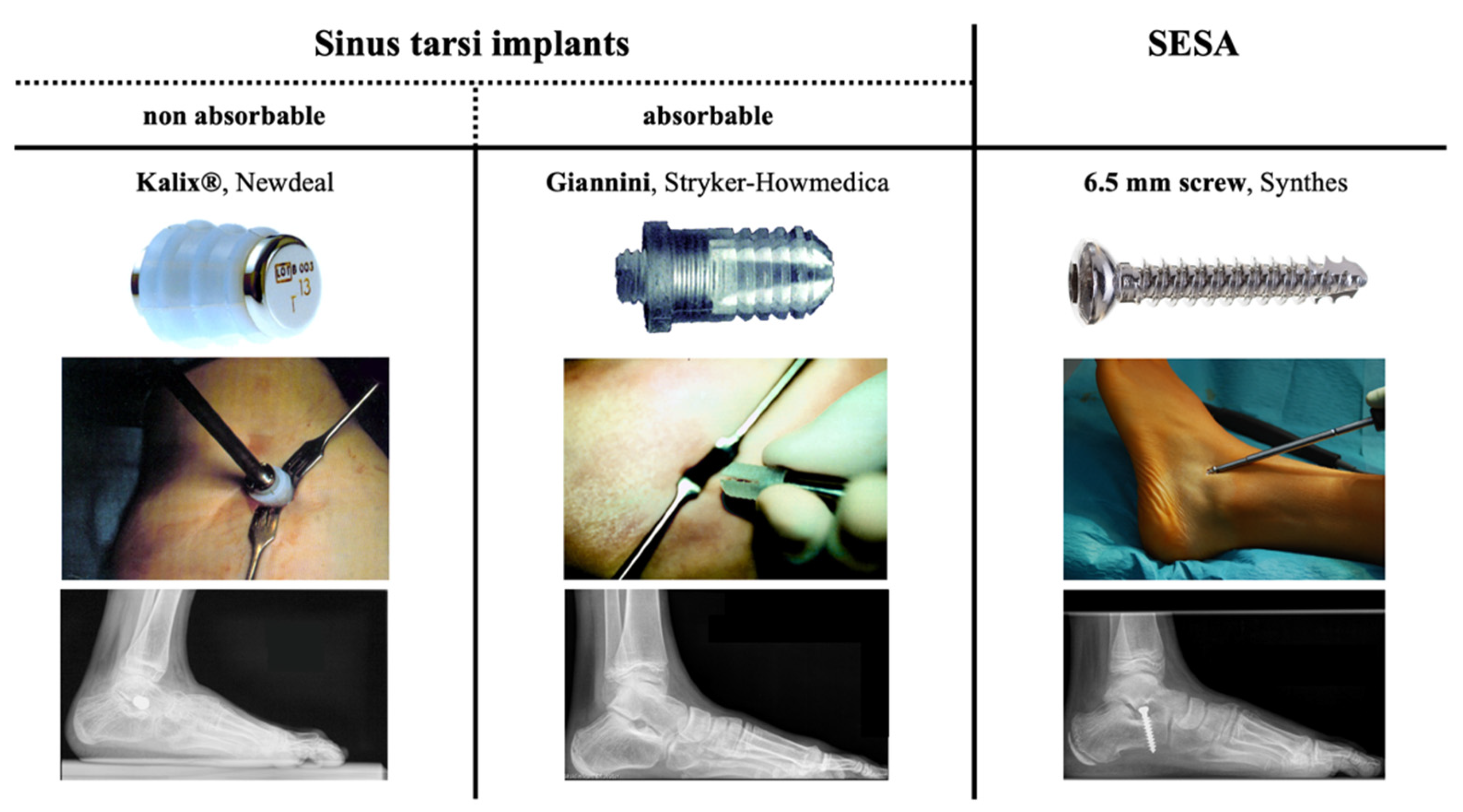
2.2. Implants
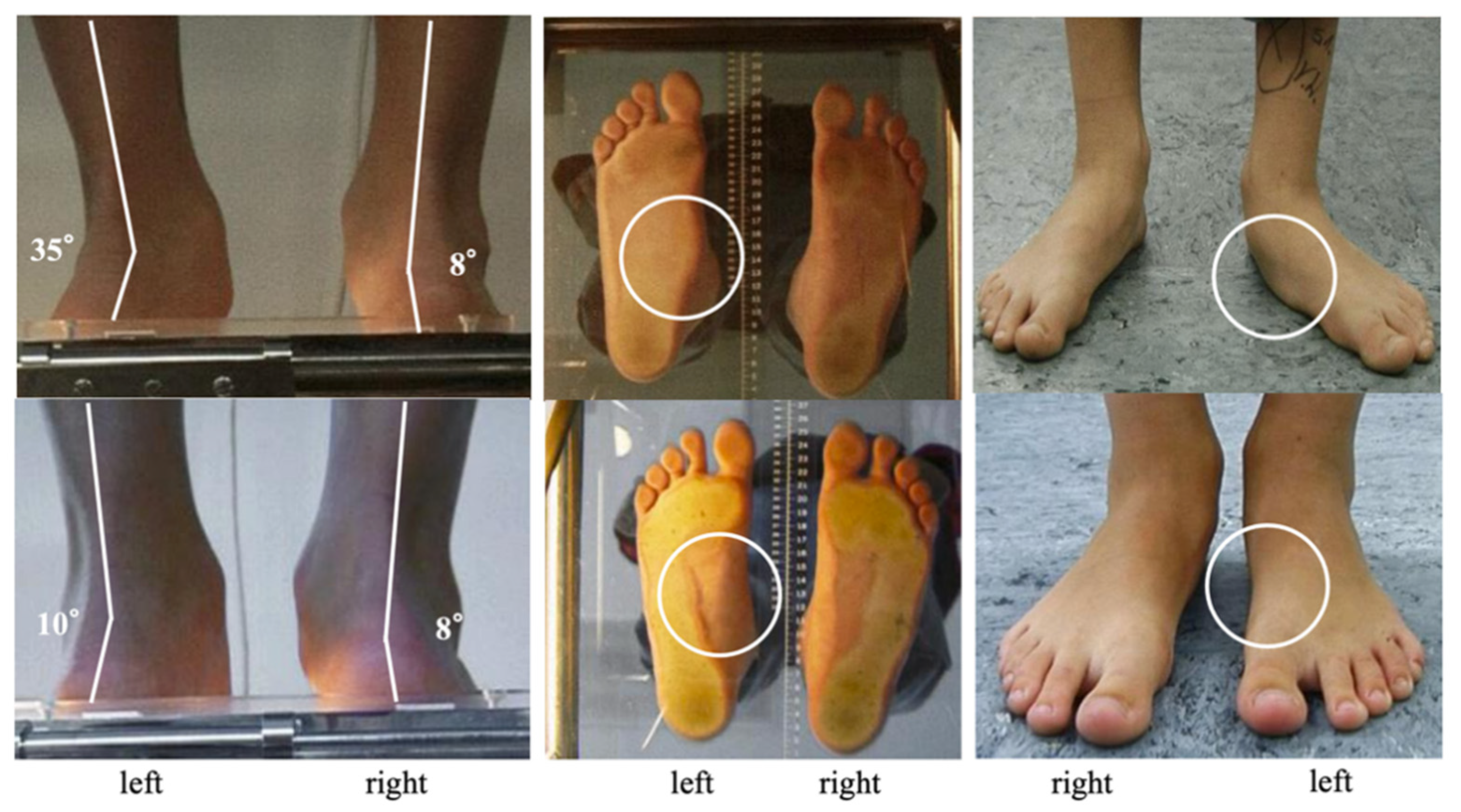
2.3. Pre- and Postoperative Assessment
2.4. Surgical Technique, Perioperative Management and Follow-Up
2.5. Statistical Report
3. Results
3.1. Clinical Outcome
3.2. Radiographic Outcome
3.3. Pedobarographic Outcome
3.4. Complications
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Metcalfe, S.A.; Bowling, F.L.; Reeves, N.D. Subtalar joint arthroereisis in the management of pediatric flexible flatfoot: A critical review of the literature. Foot Ankle Int. 2011, 32, 1127–1139. [Google Scholar] [CrossRef]
- Bernasconi, A.; Lintz, F.; Sadile, F. The role of arthroereisis of the subtalar joint for flatfoot in children and adults. EFORT Open Rev. 2017, 2, 438–446. [Google Scholar] [CrossRef]
- Hösl, M.; Böhm, H.; Oestreich, C.; Dussa, C.U.; Schäfer, C.; Döderlein, L.; Nader, S.; Fenner, V. Self-perceived foot function and pain in children and adolescents with flexible flatfeet—Relationship between dynamic pedobarography and the foot function index. Gait Posture 2020, 77, 225–230. [Google Scholar] [CrossRef]
- Hagen, L.; Pape, J.P.; Kostakev, M.; Peterlein, C.D. Pedobarographic changes during first month after subtalar extra-articular screw arthroereisis (sesa) operation of juvenile flexible flatfoot. Arch. Orthop. Trauma Surg. 2020, 140, 313–320. [Google Scholar] [CrossRef]
- Franz, A.; Herz, D.; Raabe, J.; Seeberger, U.; Bollmann, C. Pedobarographic outcome after subtalar screw arthroereisis in flexible juvenile flatfoot. Foot Ankle Surg. 2020. [Google Scholar] [CrossRef]
- De Pellegrin, M.; Moharamzadeh, D.; Strobl, W.M.; Biedermann, R.; Tschauner, C.; Wirth, T. Subtalar extra-articular screw arthroereisis (sesa) for the treatment of flexible flatfoot in children. J. Child Orthop. 2014, 8, 479–487. [Google Scholar] [CrossRef] [Green Version]
- Jay, R.M.; Din, N. Correcting pediatric flatfoot with subtalar arthroereisis and gastrocnemius recession: A retrospective study. Foot Ankle Spec. 2013, 6, 101–107. [Google Scholar] [CrossRef]
- Gutierrez, P.R.; Lara, M.H. Giannini prosthesis for flatfoot. Foot Ankle Int. 2005, 26, 918–926. [Google Scholar] [CrossRef]
- Green, W.T.; Grice, D.S. The management of calcaneus deformity. Instr. Course Lect. 1956, 13, 135–149. [Google Scholar]
- Ettinger, S.; Mattinger, T.; Stukenborg-Colsman, C.; Yao, D.; Claassen, L. Outcomes of evans versus hintermann calcaneal lengthening osteotomy for flexible flatfoot. Foot Ankle Int. 2019, 40, 661–671. [Google Scholar] [CrossRef]
- Evans, D. Calcaneo-valgus deformity. J. Bone Joint Surg. Br. 1975, 57, 270–278. [Google Scholar] [CrossRef]
- De Pellegrin, M. Subtalar screw-arthroereisis for correction of flat foot in children. Orthopade 2005, 34, 941–953. [Google Scholar] [CrossRef]
- Scialpi, L.; Mori, C.; Mori, F.; Sperti, M.; Solarino, G. Arthroerisis with giannini’s endo-orthotic implant and pisani’s talocalcaneal arthroerisis. A comparison of surgical methods. Chir. Organi Mov. 2008, 92, 61–65. [Google Scholar] [CrossRef] [PubMed]
- Faldini, C.; Mazzotti, A.; Panciera, A.; Perna, F.; Stefanini, N.; Giannini, S. Bioabsorbable implants for subtalar arthroereisis in pediatric flatfoot. Musculoskelet Surg. 2018, 102, 11–19. [Google Scholar] [CrossRef]
- Giannini, B.S.; Ceccarelli, F.; Benedetti, M.G.; Catani, F.; Faldini, C. Surgical treatment of flexible flatfoot in children a four-year follow-up study. J. Bone Joint Surg. Am. 2001, 83 (Suppl. 2), 73–79. [Google Scholar] [CrossRef] [PubMed]
- Viladot, R.; Pons, M.; Alvarez, F.; Omana, J. Subtalar arthroereisis for posterior tibial tendon dysfunction: A preliminary report. Foot Ankle Int. 2003, 24, 600–606. [Google Scholar] [CrossRef] [PubMed]
- de Bot, R.; Stevens, J.; Hermus, J.P.S.; Staal, H.M.; van Rhijn, L.W.; Witlox, A.M. Clinical and radiological outcomes of subtalar kalix ii arthroereisis for a symptomatic pediatric flexible flatfoot. Foot Ankle Spec. 2019, 14, 9–18. [Google Scholar] [CrossRef] [Green Version]
- Kuhn, H.; Zuther, W.; Heine, A.; Kuester, H.-H. Die subtalare arthrorise mittels kalix® implantat beim flexiblen knick-senkfuß. Fuß Sprunggelenk 2010, 8, 48–54. [Google Scholar] [CrossRef]
- Schroeder, S.; Ihme, N.; Kochs, A.; Niedhart, C. Subtalare arthrorise mittels kalix-schraube bei knick-senkfuß. Eine retrospektive studie. FussSprungg 2006, 4, 214–220. [Google Scholar] [CrossRef]
- Jerosch, J.; Schunck, J.; Abdel-Aziz, H. The stop screw technique—A simple and reliable method in treating flexible flatfoot in children. Foot Ankle Surg. 2009, 15, 174–178. [Google Scholar] [CrossRef]
- Palisano, R.; Rosenbaum, P.; Walter, S.; Russell, D.; Wood, E.; Galuppi, B. Development and reliability of a system to classify gross motor function in children with cerebral palsy. Dev. Med. Child Neurol. 1997, 39, 214–223. [Google Scholar] [CrossRef]
- Budiman-Mak, E.; Conrad, K.J.; Roach, K.E. The foot function index: A measure of foot pain and disability. J. Clin. Epidemiol. 1991, 44, 561–570. [Google Scholar] [CrossRef]
- Cavanagh, P.R.; Rodgers, M.M. The arch index: A useful measure from footprints. J. Biomech. 1987, 20, 547–551. [Google Scholar] [CrossRef]
- Singh, D. Nils silfverskiöld (1888–1957) and gastrocnemius contracture. Foot Ankle Surg. 2013, 19, 135–138. [Google Scholar] [CrossRef] [PubMed]
- Strayer, L.M., Jr. Recession of the gastrocnemius; an operation to relieve spastic contracture of the calf muscles. J. Bone Jt. Surg. Am. 1950, 32, 671–676. [Google Scholar] [CrossRef]
- Hoke, M. An operation for the correction of extremely relaxed flat feet. JBJS 1931, 13, 773–783. [Google Scholar]
- LeLièvre, J. Current concepts and correction in the valgus foot. Clin. Orthop. Relat. Res. 1970, 70, 43–55. [Google Scholar] [PubMed]
- Forg, P.; Feldman, K.; Flake, E.; Green, D.R. Flake-austin modification of the sta-peg arthroereisis: A retrospective study. J. Am. Podiatr. Med. Assoc. 2001, 91, 394–405. [Google Scholar] [CrossRef] [PubMed]
- Cicchinelli, L.D.; Pascual Huerta, J.; García Carmona, F.J.; Fernández Morato, D. Analysis of gastrocnemius recession and medial column procedures as adjuncts in arthroereisis for the correction of pediatric pes planovalgus: A radiographic retrospective study. J. Foot Ankle Surg. 2008, 47, 385–391. [Google Scholar] [CrossRef]
- Baker, J.R.; Klein, E.E.; Weil, L., Jr.; Weil, L.S., Sr.; Knight, J.M. Retrospective analysis of the survivability of absorbable versus nonabsorbable subtalar joint arthroereisis implants. Foot Ankle Spec. 2013, 6, 36–44. [Google Scholar] [CrossRef]
- Hamel, J. Radiologisch-dokumentierte korrektureffekte beim kindlichen pes planovalgus mit der calcaneostop-arthrorise und der calcaneus-verlängerungosteotomie. Fuß Sprunggelenk 2010, 8, 43–47. [Google Scholar] [CrossRef]
- Kim, H.; Weinstein, S. Flatfoot in children: Differential diagnosis and management. Curr. Orthop. 2000, 14, 441–447. [Google Scholar] [CrossRef]
- Ruozi, B.; Belletti, D.; Manfredini, G.; Tonelli, M.; Sena, P.; Vandelli, M.A.; Forni, F.; Tosi, G. Biodegradable device applied in flatfoot surgery: Comparative studies between clinical and technological aspects of removed screws. Mater. Sci. Eng. C Mater. Biol. Appl. 2013, 33, 1773–1782. [Google Scholar] [CrossRef] [PubMed]
- Hamel, J. Die calcaneostop-arthrorise—Eine retrospektive klinische studiemitkomplikations-analyse. Fuß Sprunggelenk 2010, 8, 35–41. [Google Scholar]
- Rein, S.; Hagert, E.; Hanisch, U.; Lwowski, S.; Fieguth, A.; Zwipp, H. Immunohistochemical analysis of sensory nerve endings in ankle ligaments: A cadaver study. Cells Tissues Organs 2013, 197, 64–76. [Google Scholar] [CrossRef]
- Rein, S.; Hanisch, U.; Zwipp, H.; Fieguth, A.; Lwowski, S.; Hagert, E. Comparative analysis of inter- and intraligamentous distribution of sensory nerve endings in ankle ligaments: A cadaver study. Foot Ankle Int. 2013, 34, 1017–1024. [Google Scholar] [CrossRef]
- Shah, N.S.; Needleman, R.L.; Bokhari, O.; Buzas, D. 2013 subtalar arthroereisis survey: The current practice patterns of members of the aofas. Foot Ankle Spec. 2015, 8, 180–185. [Google Scholar] [CrossRef]
- Pavone, V.; Testa, G.; Vescio, A.; Wirth, T.; Andreacchio, A.; Accadbled, F.; Canavese, F. Diagnosis and treatment of flexible flatfoot: Results of 2019 flexible flatfoot survey from the european paediatric orthopedic society. J. Pediatr. Orthop. B 2020. [Google Scholar] [CrossRef]
- Pavone, V.; Vescio, A.; Canavese, F.; Costa, D.; Sessa, G.; Testa, G. Effects of body weight on the clinical and radiological outcomes of children with flexible flatfeet managed with the ‘calcaneo-stop’ procedure. J. Pediatr. Orthop. B 2019, 28, 228–234. [Google Scholar] [CrossRef] [PubMed]
- Hsieh, C.H.; Lee, C.C.; Tseng, T.H.; Wu, K.W.; Chang, J.F.; Wang, T.M. Body weight effects on extra-osseous subtalar arthroereisis. J. Clin. Med. 2019, 8, 1273. [Google Scholar] [CrossRef] [Green Version]







| Total | Kalix® | Giannini | SESA | |
|---|---|---|---|---|
| Number (patients/feet) | 73/113 | 11/21 | 37/56 | 25/36 |
| Age at operation in years (range) | 10.8 (5–16) | 10.2 (6–14) | 10.3 (5–16) | 12.0 (8–16) |
| Gender (male/female) | 45/28 | 6/5 | 24/13 | 15/10 |
| Etiology (idiopathic/ neuromuscular) | 48/25 | 3/8 | 26/11 | 19/6 |
| Side (right/left) (bilateral) | 52/61 (40) | 10/11 (10) | 27/29 (19) | 15/21 (11) |
| Body mass index in kg/m2 (range) | 20.5 (15.4–25.0) | 20.5 (16.3–25.0) | 20.9 (18.5–24.2) | 19.9 (15.4–24.8) |
| Lengthening of gastrocnemius muscle or Achilles tendon (yes/no) | 51/62 | 14/7 | 22/34 | 15/21 |
| Follow up in months (range) | 29.0 (1–111) | 29.6 (1–86) | 30.1 (1–79) | 27.0 (2–111) |
| Total | Kalix® | Giannini | SESA | p Value | |
|---|---|---|---|---|---|
| Excellent | 14/73 (19.2%) | 2/11 (18.2%) | 7/37 (18.9%) | 5/25 (20.0%) | 0.990 |
| Good | 39/73 (53.4%) | 6/11 (54.5%) | 20/37 (54.1%) | 13/25 (52.0%) | 0.984 |
| Fair | 13/73 (17.8%) | 2/11 (18.2%) | 7/37 (18.9%) | 4/25 (16.0%) | 0.981 |
| Poor | 7/73 (9.6%) | 1/11 (9.1%) | 3/37 (8.1%) | 3/25 (12.0%) | 0.979 |
| Total | Kalix® | Giannini | SESA | |
|---|---|---|---|---|
| Implant-related complications | 17/113 (15.0%) | 6/21 (28.6%) | 10/56 (17.9%) | 1/36 (2.8%) |
| - Primary mal-position | 1/113 (0.9%) | 0/21 (0%) | 0/56 (0%) | 1/36 (2.8%) |
| - Secondary dislocation or breakage | 16/113 (14.1%) | 6/21 (28.6%) | 10/56 (17.9%) | 0/36 (0%) |
| Treatment-related pain based on | 12/113 (10.6%) | 4/21 (19.0%) | 4/56 (7.1%) | 4/36 (11.1%) |
| - Implant-related complications | 8/113 (7.1%) | 4/21 (19.0%) | 4/56 (7.1%) | 0/36 (0%) |
| - Peroneal muscle contractures | 4/113 (3.5%) | 0/21 (0%) | 0/56 (0%) | 4/36 (11.1%) |
| Premature removal | 14/113 (12.4%) | 6/21 (28.6%) | 4/56 (7.1%) | 4/36 (11.1%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vogt, B.; Toporowski, G.; Gosheger, G.; Rölfing, J.D.; Rosenbaum, D.; Schiedel, F.; Laufer, A.; Kleine-Koenig, M.-T.; Theil, C.; Roedl, R.; et al. Subtalar Arthroereisis for Flexible Flatfoot in Children—Clinical, Radiographic and Pedobarographic Outcome Comparing Three Different Methods. Children 2021, 8, 359. https://doi.org/10.3390/children8050359
Vogt B, Toporowski G, Gosheger G, Rölfing JD, Rosenbaum D, Schiedel F, Laufer A, Kleine-Koenig M-T, Theil C, Roedl R, et al. Subtalar Arthroereisis for Flexible Flatfoot in Children—Clinical, Radiographic and Pedobarographic Outcome Comparing Three Different Methods. Children. 2021; 8(5):359. https://doi.org/10.3390/children8050359
Chicago/Turabian StyleVogt, Bjoern, Gregor Toporowski, Georg Gosheger, Jan Duedal Rölfing, Dieter Rosenbaum, Frank Schiedel, Andrea Laufer, Marie-Theres Kleine-Koenig, Christoph Theil, Robert Roedl, and et al. 2021. "Subtalar Arthroereisis for Flexible Flatfoot in Children—Clinical, Radiographic and Pedobarographic Outcome Comparing Three Different Methods" Children 8, no. 5: 359. https://doi.org/10.3390/children8050359







