The Association between NICU Admission and Mental Health Diagnoses among Commercially Insured Postpartum Women in the US, 2010–2018
Abstract
:1. Introduction
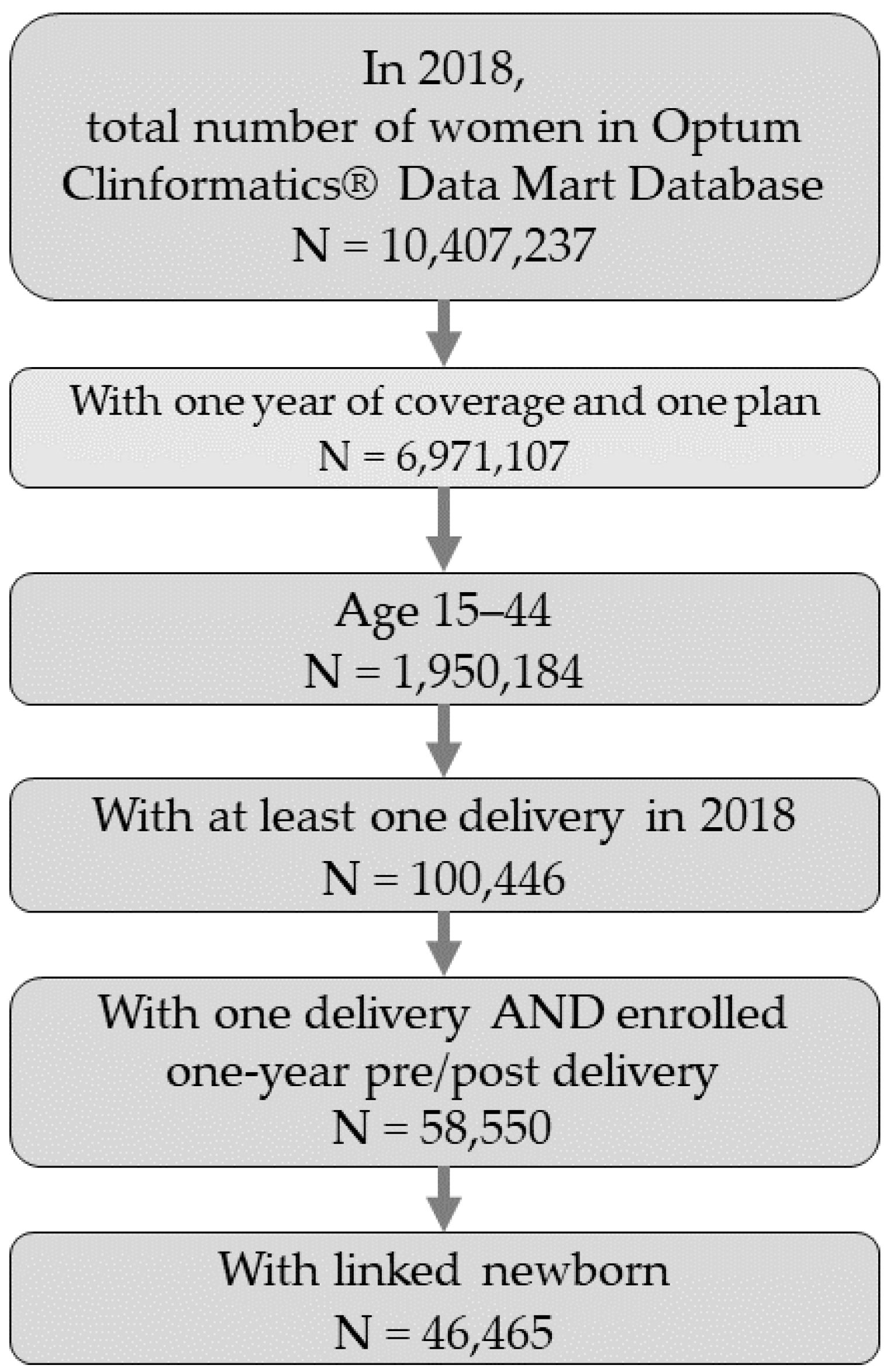
2. Materials and Methods
Statistical Analysis
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A. ICD-9 and ICD-10 Codes Used to Identify Maternal MH Disorders
| Group | ICD Diagnosis Code |
| Anxiety | 300.xx, 308.xx, 313.xx, 293.xx, F06.xx, F40.xx, F41.xx, F42.xx, F43.xx, F48.xx, R45.xx |
| Depression | 311.xx, 296.xx, 300.xx, F32.xx, F33.xx |
Appendix B. ICD-9 and ICD-10 Codes Used to Identify Other MH Disorders
| Group | ICD Diagnosis Code |
| Other MH Disorders | 312.xx, 314.xx, 313.xx, F90.xx, F91.xx, R46.xx, R46.xx, R46.xx, R46.xx, 309.xx, 309.xx, F43.xx |
Appendix C. ICD and CPT/HCPCS Codes Used to Identify Substance Use Disorder
| Group | ICD Diagnosis Code |
| ICD Diagnoses | 291.xx, 357.xx, 425.xx, 535.xx, 571.xx, 980.xx, 303.xx, 305.xx, 760.xx, F10.xx, G62.xx, I42.xx, K29.xx, K70.xx, O99.xx, 304.xx, F12.xx, F14.xx, 292.xx, 779.xx, 648.xx, 655.xx, 965.xx, F55.xx, O35.xx, F16.xx, F18.xxP04.xx, P96.xx, Q86.xx, F11.xx, F15.xx, F19.xx, F13.xx, T36.xx, T37.xx, T38.xx, T39.xx, T40.xx, T41.xx, T42.xx, T43.xx, T44.xx, T45.xx, T46.xx, T47.xx, T48.xx, T49.xx, T50.xx, T51.xx, T52.xx, T53.xx, T54xx, T55.xx, T56.xx, T57.xx, T58.xx, T59.xx, T60.xx, T61.xx, T62.xx, T63.xx, T64.xx, T65.xx, T71.xx, V65.xx, F17.xx |
| CPT/HCPCS | G0397, G0396, H0048, H2034, H0014, H0027, H0029, H0007, H0016, H0026, H0028, H0003, H0009, H0005, H0015, H001, H0012, H0011, H0013, H0020, H0008, T1006, H0050, H0022, H0006, H0021, H0047, H2036, H2035, H0001, H0049, T102, T1007, T1011, S9475, G0442, H0039, H0040, H0004, H2012, H0030, H0023, H0025, H0017, H0024, H0002, H0019, H018, G0443, T1009, H2015, H2016, H2011, T1008, T1010, H2025, H2026, H0033, H2001, H0038, H2014, H2019, H2020, H2ZZZZ, HZ63ZZZ, HZ33ZZZ, GZ3ZZZZ, HZ82ZZZ, HZ83ZZZ, HZ87ZZZ, HZ86ZZZ, HZ81ZZZ, HZ85ZZZ, HZ84ZZZ, HZ80ZZZ, HZ89ZZZ, HZ88ZZZ, HZ93ZZZ, HZ97ZZZ, HZ96ZZZ, HZ92ZZZ, HZ95ZZZ, HZ94ZZZ, HZ98ZZZ, HZ91ZZZ, HZ90ZZZ, HZ99ZZ |
| ICD Procedures | 9462, 9461, 9463, 946, 9446, 9469, 9468, 9467, 9465, 9464, 9466 |
References
- Building US Capacity to Review and Prevent Maternal Deaths. Report from Nine Maternal Mortality Review Committees. 2018. Available online: http://reviewtoaction.org/national-resource/report-nine-mmrcs (accessed on 6 June 2022).
- Trost, S.L.; Beauregard, J.L.; Smoots, A.N.; Ko, J.Y.; Haight, S.C.; Simas, T.A.M.; Byatt, N.; Madni, S.A.; Goodman, D. Preventing Pregnancy-Related Mental Health Deaths: Insights From 14 US Maternal Mortality Review Committees, 2008–2017. Health Aff. 2021, 40, 1551–1559. [Google Scholar] [CrossRef] [PubMed]
- Gavin, N.I.; Gaynes, B.N.; Lohr, K.N.; Meltzer-Brody, S.; Gartlehner, G.; Swinson, T. Perinatal depression: A systematic review of prevalence and incidence. Obstet. Gynecol. 2005, 106, 1071–1083. [Google Scholar] [CrossRef]
- Fawcett, E.J.; Fairbrother, N.; Cox, M.L.; White, I.R.; Fawcett, J.M. The prevalence of anxiety disorders during pregnancy and the postpartum period: A multivariate Bayesian meta-analysis. J. Clin. Psychiatry 2019, 80, 18r12527. [Google Scholar] [CrossRef] [PubMed]
- Mangla, K.; Hoffman, M.C.; Trumpff, C.; O’Grady, S.; Monk, C. Maternal self-harm deaths: An unrecognized and preventable outcome. Am. J. Obstet. Gynecol. 2019, 221, 295–303. [Google Scholar] [CrossRef]
- Admon, L.K.; Dalton, V.K.; Kolenic, G.E.; Ettner, S.L.; Tilea, A.; Haffajee, R.L.; Brownlee, R.M.; Zochowski, M.K.; Tabb, K.M.; Muzik, M.; et al. Trends in Suicidality 1 Year Before and After Birth Among Commercially Insured Childbearing Individuals in the United States, 2006–2017. JAMA Psychiatry 2021, 78, 171–176. [Google Scholar] [CrossRef] [PubMed]
- Mukherjee, S.; Coxe, S.; Fennie, K.; Madhivanan, P.; Trepka, M.J. Antenatal Stressful Life Events and Postpartum Depressive Symptoms in the United States: The Role of Women’s Socioeconomic Status Indices at the State Level. J. Women’s Health 2017, 26, 276–285. [Google Scholar] [CrossRef]
- ACOG Committee Opinion 757. Screening for Perinatal Depression. 2018. Available online: https://www.acog.org/clinical/clinical-guidance/committee-opinion/articles/2018/11/screening-for-perinatal-depression (accessed on 6 June 2022).
- National Institute of Mental Health. Perinatal depression. NIH Publication No. 20-MH-8116. Available online: https://www.nimh.nih.gov/health/publications/perinatal-depression (accessed on 6 June 2022).
- Vigod, S.N.; Villegas, L.; Dennis, C.-L.; E Ross, L. Prevalence and risk factors for postpartum depression among women with preterm and low-birth-weight infants: A systematic review. BJOG Int. J. Obstet. Gynaecol. 2010, 117, 540–550. [Google Scholar] [CrossRef] [PubMed]
- Lefkowitz, D.S.; Baxt, C.; Evans, J.R. Prevalence and Correlates of Posttraumatic Stress and Postpartum Depression in Parents of Infants in the Neonatal Intensive Care Unit (NICU). J. Clin. Psychol. Med Settings 2010, 17, 230–237. [Google Scholar] [CrossRef] [PubMed]
- Segre, L.S.; McCabe, J.E.; Chuffo-Siewert, R.; O’Hara, M.W. Depression and Anxiety Symptoms in Mothers of Newborns Hospitalized on the Neonatal Intensive Care Unit. Nurs. Res. 2014, 63, 320–332. [Google Scholar] [CrossRef] [Green Version]
- Stasik-O’Brien, S.M.; McCabe-Beane, J.E.; Segre, L.S. Using the EPDS to Identify Anxiety in Mothers of Infants on the Neonatal Intensive Care Unit. Clin. Nurs. Res. 2017, 28, 473–487. [Google Scholar] [CrossRef]
- Davila, R.C.; Segre, L.S. A Nurse-Based Model of Psychosocial Support for Emotionally Distressed Mothers of Infants in the NICU. J. Obstet. Gynecol. Neonatal Nurs. 2018, 47, 114–121. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vance, A.J.; Malin, K.J.; Miller, J.; Shuman, C.J.; Moore, T.A.; Benjamin, A. Parents’ pandemic NICU experience in the United States: A qualitative study. BMC Pediatr. 2021, 21, 558. [Google Scholar] [CrossRef]
- Schecter, R.; Pham, T.; Hua, A.; Spinazzola, R.; Sonnenklar, J.; Li, D.; Papaioannou, H.; Milanaik, R. Prevalence and Longevity of PTSD Symptoms Among Parents of NICU Infants Analyzed Across Gestational Age Categories. Clin. Pediatr. 2019, 59, 163–169. [Google Scholar] [CrossRef]
- Malouf, R.; Harrison, S.; Burton, H.A.; Gale, C.; Stein, A.; Franck, L.S.; Alderdice, F. Prevalence of anxiety and post-traumatic stress (PTS) among the parents of babies admitted to neonatal units: A systematic review and meta-analysis. eClinicalMedicine 2021, 43, 101233. [Google Scholar] [CrossRef]
- Loewenstein, K. Parent psychological distress in the neonatal intensive care unit within the context of the social eco-logical model: A scoping review. J. Am. Psychiatr. Nurses Assoc. 2018, 24, 495–509. [Google Scholar] [CrossRef]
- Miles, M.S.; Holditch-Davis, D.; Schwartz, T.A.; Scher, M. Depressive Symptoms in Mothers of Prematurely Born Infants. J. Dev. Behav. Pediatr. 2007, 28, 36–44. [Google Scholar] [CrossRef] [PubMed]
- Liu, L.; Oza, S.; Hogan, D.; Chu, Y.; Perin, J.; Zhu, J.; Lawn, J.E.; Cousens, S.; Mathers, C.; Black, R.E. Global, regional, and national causes of under-5 mortality in 2000–15: An updated systematic analysis with implications for the Sustainable Development Goals. Lancet 2016, 388, 3027–3035. [Google Scholar] [CrossRef] [Green Version]
- Harrison, W.; Wasserman, J.R.; Goodman, D.C. Regional Variation in Neonatal Intensive Care Admissions and the Relationship to Bed Supply. J. Pediatr. 2018, 192, 73–79.e4. [Google Scholar] [CrossRef]
- Haidari, E.S.; Lee, H.C.; Illuzzi, J.L.; Phibbs, C.S.; Lin, H.; Xu, X. Hospital variation in admissions to neonatal intensive care units by diagnosis severity and category. J. Perinatol. 2020, 41, 468–477. [Google Scholar] [CrossRef]
- Ms, V.A.G.; Geller, P.A.; Bonacquisti, A.; Patterson, C.A. NICU infant health severity and family outcomes: A systematic review of assessments and findings in psychosocial research. J. Perinatol. 2018, 39, 156–172. [Google Scholar] [CrossRef]
- Hynan, M.T.; Steinberg, Z.; Baker, L.; Cicco, R.; A Geller, P.; Lassen, S.; A Milford, C.; O Mounts, K.; Patterson, C.; Saxton, S.; et al. Recommendations for mental health professionals in the NICU. J. Perinatol. 2015, 35, S14–S18. [Google Scholar] [CrossRef] [Green Version]
- Edwards, E.M.; Greenberg, L.T.; Profit, J.; Draper, D.; Helkey, D.; Horbar, J.D. Quality of Care in US NICUs by Race and Ethnicity. Pediatrics 2021, 148, e2020037622. [Google Scholar] [CrossRef]
- Karvonen, K.L.; Baer, R.J.; Rogers, E.E.; Steurer, M.A.; Ryckman, K.K.; Feuer, S.K.; Anderson, J.G.; Franck, L.S.; Gano, D.; Petersen, M.A.; et al. Racial and ethnic disparities in outcomes through 1 year of life in infants born prematurely: A population based study in California. J. Perinatol. 2021, 41, 220–231. [Google Scholar] [CrossRef]
- Profit, J.; Gould, J.B.; Bennett, M.; Goldstein, B.A.; Draper, D.; Phibbs, C.S.; Lee, H.C. Racial/Ethnic Disparity in NICU Quality of Care Delivery. Available online: https://publications.aap.org/pediatrics/article-abstract/140/3/e20170918/38311/Racial-Ethnic-Disparity-in-NICU-Quality-of-Care (accessed on 6 June 2022).
- Roque, A.T.F.; Lasiuk, G.C.; Radünz, V.; Hegadoren, K. Scoping Review of the Mental Health of Parents of Infants in the NICU. J. Obstet. Gynecol. Neonatal Nurs. 2017, 46, 576–587. [Google Scholar] [CrossRef] [Green Version]
- Jubinville, J.; Newburn-Cook, C.; Hegadoren, K.; Lacaze-Masmonteil, T. Symptoms of Acute Stress Disorder in Mothers of Premature Infants. Adv. Neonatal Care 2012, 12, 246–253. [Google Scholar] [CrossRef]
- Chan, A.L.; Guo, N.; Popat, R.; Robakis, T.; Blumenfeld, Y.Y.; Main, E.; Scott, K.A.; Butwick, A.J. Racial and Ethnic Disparities in Hospital-Based Care Associated with Postpartum Depression. J. Racial Ethn. Health Disparities 2020, 8, 220–229. [Google Scholar] [CrossRef]
- Farr, S.L.; Denk, C.E.; Dahms, E.W.; Dietz, P.M. Evaluating Universal Education and Screening for Postpartum Depression Using Population-Based Data. J. Women’s Health 2014, 23, 657–663. [Google Scholar] [CrossRef]
- Declercq, E.; Feinberg, E.; Belanoff, C. Racial inequities in the course of treating perinatal mental health challenges: Results from listening to mothers in California. Birth 2021, 49, 132–140. [Google Scholar] [CrossRef]
- Lucero, N.B.; Beckstrand, R.L.; Callister, L.C.; Birkhead, A.C.S. Prevalence of postpartum depression among Hispanic immigrant women. J. Am. Acad. Nurse Pract. 2012, 24, 726–734. [Google Scholar] [CrossRef]
- Kozhimannil, K.B.; Trinacty, C.M.; Busch, A.B.; Huskamp, H.A.; Adams, A.S. Racial and Ethnic Disparities in Postpartum Depression Care Among Low-Income Women. Psychiatr. Serv. 2011, 62, 619–625. [Google Scholar] [CrossRef]
- Iturralde, E.; Hsiao, C.A.; Nkemere, L.; Kubo, A.; Sterling, S.A.; Flanagan, T.; Avalos, L.A. Engagement in perinatal depression treatment: A qualitative study of barriers across and within racial/ethnic groups. BMC Pregnancy Child-Birth 2021, 21, 512. [Google Scholar] [CrossRef]
- Dagher, R.K.; Bruckheim, H.E.; Colpe, L.J.; Edwards, E.; White, D.B. Perinatal Depression: Challenges and Opportunities. J. Women’s Health 2021, 30, 154–159. [Google Scholar] [CrossRef]
- Givrad, S.; Hartzell, G.; Scala, M. Promoting infant mental health in the neonatal intensive care unit (NICU): A review of nurturing factors and interventions for NICU infant-parent relationships. Early Hum. Dev. 2020, 154, 105281. [Google Scholar] [CrossRef]
- The Trimester Project: New Mom Health: A Village for Mothers. Available online: https://newmomhealth.com/aboutus (accessed on 26 May 2022).
- Firefly: Lighting the Path for Moms in Recovery and Their Babies. Available online: https://fireflytn.org/ (accessed on 26 May 2022).
- Cox, E.Q.; Sowa, N.A.; Meltzer-Brody, S.; Gaynes, B.N. The Perinatal Depression Treatment Cascade. J. Clin. Psychiatry 2016, 77, 1189–1200. [Google Scholar] [CrossRef]
- Hardeman, R.R.; Karbeah, J.; Kozhimannil, K.B. Applying a critical race lens to relationship-centered care in pregnancy and childbirth: An antidote to structural racism. Birth 2019, 47, 3–7. [Google Scholar] [CrossRef]


| (a) | ||||||||
| Demographic | Overall | Overall % | No NICU | No NICU % 95% CI | <14 days NICU | <14 days NICU % 95% CI | ≥14 days NICU | ≥14 days NICU % |
| 95% CI | 95% CI | |||||||
| 55,500 | 50,614 | 3671 | 1215 | |||||
| Age | ||||||||
| ≤18 | 220 | 0.40% | 210 | 95.45% [92.64, 98.27] | (<11) | 3.18% | (<11) | 1.36% |
| [−0.43, 1.23] | [−9.82, 16.18] | [−11.8, 14.49] | ||||||
| 19–26 | 6689 | 12.05% [11.27, 12.83] | 6131 | 91.66% [90.97, 92.35] | 436 | 6.52% [4.20, 8.84] | 122 | 1.82% |
| [−0.55, 4.20] | ||||||||
| 27–34 | 32,663 | 58.85% [58.32, 59.39] | 29,944 | 91.68% [91.36, 91.99] | 2047 | 6.27% [5.22, 7.32] | 672 | 2.06% |
| [0.98, 3.13] | ||||||||
| 35–39 | 12,388 | 22.32% [21.59, 23.05] | 11,211 | 90.50% [89.96, 91.04] | 876 | 7.07% [5.37, 8.77] | 301 | 2.43% |
| [0.69, 4.17] | ||||||||
| ≥40 | 3540 | 6.38% [5.57, 7.18] | 3118 | 88.08% [86.94, 89.22] | 305 | 8.62% [5.47, 11.76] | 117 | 3.31% |
| [0.07, 6.54] | ||||||||
| Race/Ethnicity | ||||||||
| Asian | 4236 | 7.63% [6.83, 8.43] | 3869 | 91.34% [90.45, 92.22] | 277 | 6.54% [3.63, 9.45] | 90 | 2.12% |
| [−0.85, 5.10] | ||||||||
| Black | 4692 | 8.45% [7.66, 9.25] | 4213 | 89.79% [88.88, 90.71] | 335 | 7.14% [4.38, 9.90] | 144 | 3.07% |
| [0.25, 5.89] | ||||||||
| Hispanic | 6353 | 11.45% [10.66, 12.23] | 5780 | 90.98% [90.24, 91.72] | 438 | 6.89% [4.52, 9.27] | 135 | 2.12% |
| [−0.31, 4.56] | ||||||||
| Unknown race | 4149 | 7.48% [6.68, 8.28] | (<11) | (<11) | (<11) | |||
| White | 36,070 | 64.99% [64.50, 65.48] | 32,954 | 91.36% [91.06, 91.66] | 2346 | 6.50% [5.51, 7.50] | 770 | 2.13% |
| [1.11, 3.16] | ||||||||
| Region | ||||||||
| Midwest | 12,990 | 23.41% [22.68, 24.13] | 11,913 | 91.71% [91.21, 92.20] | 811 | 6.24% [4.58, 7.91] | 266 | 2.05% |
| [0.35, 3.75] | ||||||||
| West | 11,059 | 19.93% [19.18, 20.67] | 10,185 | 92.10% [91.57, 92.62] | 663 | 6.00% [4.19, 7.80] | 211 | 1.91% |
| [0.06, 3.75] | ||||||||
| Northeast | 6067 | 10.93% [10.15, 11.72] | 5466 | 90.09% [89.30, 90.89] | 479 | 7.90% [5.48, 10.31] | 122 | 2.01% |
| [−0.48, 4.50] | ||||||||
| South | 25,350 | 45.68% [45.06, 46.29] | 23,017 | 90.80% [90.42, 91.17] | 1717 | 6.77% [5.58, 7.96] | 616 | 2.43% |
| [1.21, 3.65] | ||||||||
| Insurance | ||||||||
| POS | 38,661 | 69.66% [69.20, 70.12] | 35,218 | 91.09% [90.80, 91.39] | 2583 | 6.68% [5.72, 7.64] | 860 | 2.22% |
| [1.24, 3.21] | ||||||||
| EPO/HMO | 15,656 | 28.21% [27.50, 28.91] | 14,304 | 91.36% | 1011 | 6.46% [4.94, 7.97] | 341 | 2.18% |
| [90.90, 91.82] | [0.63, 3.73] | |||||||
| PPO | 983 | 1.77% [0.95, 2.60] | 905 | 92.07% | 65 | 6.61% [0.57, 12.65] | 13 | 1.32% |
| [90.30, 93.83] | [−4.89, 7.53] | |||||||
| Other | 200 | 187 | 93.50% | 12 | 6.00% | (<11) | 0.50% | |
| [89.97, 97.03] | [−7.44, 19.44] | [−13.3, 14.32] | ||||||
| Other MH Conditions (excluding anxiety and depression) | ||||||||
| No other MH | 52,450 | 94.50% [94.31, 94.70] | 47,892 | 91.31% [91.06, 91.56] | 3420 | 6.52% [5.69, 7.35] | 1138 | 2.17% |
| [1.32, 3.02] | ||||||||
| Pre-other MH | 2983 | 5.37% [4.57, 6.18] | 2657 | 89.07% [87.89, 90.26] | 249 | 8.35% [4.91, 11.78] | 77 | 2.58% |
| [−0.96, 6.12] | ||||||||
| Substance | ||||||||
| Use Disorder | ||||||||
| No SUD | 54,751 | 98.65% [98.55, 98.75] | 49,973 | 91.27% [91.03, 91.52] | 3596 | 6.57% [5.76, 7.38] | 1182 | 2.16% |
| [1.33, 2.99] | ||||||||
| Pre-SUD | 749 | 1.35% [0.52, 2.18] | 641 | 85.58% [82.86, 88.30] | 75 | 10.01% [3.22, 16.81] | 33 | 4.41% |
| [−2.60, 11.41] | ||||||||
| (b) | ||||||||
| Demographic | Overall | Overall % | No NICU | No NICU % 95% CI | <14 days NICU | <14 days NICU % 95% CI | ≥14 days NICU | ≥14 days NICU % |
| 95% CI | 95% CI | |||||||
| 49,431 | 44,301 | 3986 | 1144 | |||||
| Age | ||||||||
| ≤18 | 57 | 50 | 87.72% [78.62, 96.82] | (<11) | 10.53% | (<11) | 1.75% | |
| [−14.0, 35.08] | [−24.0, 27.49] | |||||||
| 19–26 | 3722 | 7.53% [6.68, 8.38] | 3388 | 91.03% [90.06,91.99] | 274 | 7.36% [4.27,10.45] | 60 | 1.61% |
| [−1.57, 4.80] | ||||||||
| 27–34 | 29,059 | 58.79% [58.22, 59.35] | 26,212 | 90.20% [89.84, 90.56] | 2224 | 7.65% [6.55, 8.76] | 623 | 2.14% |
| [1.01,3.28] | ||||||||
| 35–39 | 13,455 | 27.22% [26.47, 27.97] | 11,985 | 89.07% [88.52, 89.63] | 1147 | 8.52% [6.91, 10.14] | 323 | 2.40% |
| [0.73, 4.07] | ||||||||
| ≥40 | 3138 | 6.35% [5.50, 7.20] | 2666 | 84.96% [83.60, 86.32] | 335 | 10.68% [7.37, 13.98] | 137 | 4.37% |
| [0.94, 7.79] | ||||||||
| Race/Ethnicity | ||||||||
| Asian | 4635 | 9.38% [8.54, 10.22] | 4130 | 89.10% [88.15, 90.05] | 394 | 8.50% [5.75, 11.25] | 111 | 2.39% |
| [−0.45, 5.24] | ||||||||
| Black | 3834 | 7.76% [6.91, 8.60] | 3369 | 87.87% [86.77, 88.97] | 349 | 9.10% [6.08, 12.12] | 116 | 3.03% |
| [−0.09, 6.14] | ||||||||
| Hispanic | 6458 | 13.06% [12.24, 13.89] | 5772 | 89.38% [88.58, 90.17] | 533 | 8.25% [5.92, 10.59] | 153 | 2.37% |
| [−0.04, 4.78] | ||||||||
| Unknown race | 2429 | 4.91% [4.05, 5.77] | (<11) | (<11) | (<11) | |||
| White | 32075 | 64.89% [64.37, 65.41] | 28843 | 89.92% [89.58, 90.27] | 2521 | 7.86% [6.81, 8.91] | 711 | 2.22% |
| [1.13, 3.30] | ||||||||
| Region | ||||||||
| Midwest | 13,224 | 26.75% [26.00, 27.51] | 11,858 | 89.67% [89.12, 90.22] | 1049 | 7.93% [6.30, 9.57] | 317 | 2.40% |
| [0.71, 4.08] | ||||||||
| West | 11,018 | 22.29% [21.51, 23.07] | 9923 | 90.06% [89.47, 90.65] | 838 | 7.61% [5.81, 9.40] | 257 | 2.33% |
| [0.49, 4.18] | ||||||||
| Northeast | 5275 | 10.67% [9.84, 11.50] | 4659 | 88.32% [87.40, 89.24] | 515 | 9.76% [7.20, 12.33] | 101 | 1.91% |
| [−0.76, 4.59] | ||||||||
| South | 19,738 | 39.93% [39.25, 40.61] | 17,700 | 89.67% [89.23, 90.12] | 1572 | 7.96% [6.63, 9.30] | 466 | 2.36% |
| [0.98, 3.74] | ||||||||
| Insurance | ||||||||
| POS | 37,235 | 75.33% [74.89, 75.77] | 33,386 | 89.66% [89.34, 89.99] | 2983 | 8.01% [7.04, 8.99] | 866 | 2.33% |
| [1.32, 3.33] | ||||||||
| EPO/HMO | 11,070 | 22.39% [21.62, 23.17] | 9893 | 89.37% [88.76, 89.98] | 918 | 8.29% [6.51, 10.08] | 259 | 2.34% |
| [0.50, 4.18] | ||||||||
| PPO | 630 | 1.27% [0.40, 2.15] | 576 | 91.43% [89.14, 93.71] | 45 | 7.14% | (<11) | 1.43% |
| [−0.38, 14.67] | [−6.32, 9.18] | |||||||
| Other | 496 | 1.00% [0.13, 1.88] | 446 | 89.92% [87.13, 92.71] | 40 | 8.06% | (<11) | 2.02% |
| [−0.37, 16.50] | [−6.70, 10.73] | |||||||
| Other MH Conditions (excluding anxiety and depression) | ||||||||
| No other MH | 42,773 | 86.53% [86.21, 86.85] | 38,499 | 90.01% [89.71, 90.31] | 3336 | 7.80% [6.89, 8.71] | 938 | 2.19% |
| [1.26, 3.13] | ||||||||
| Pre-other MH | 6518 | 13.19% [12.36, 14.01] | 5673 | 87.04% [86.16, 87.91] | 645 | 9.90% [7.59, 12.20] | 200 | 3.07% |
| [0.68, 5.46] | ||||||||
| Substance Use Disorder | ||||||||
| No SUD | 47,883 | 96.87% [96.71, 97.02] | 43,013 | 89.83% [89.54, 90.12] | 3783 | 7.90% [7.04, 8.76] | 1087 | 2.27% |
| [1.38, 3.16] | ||||||||
| Pre-SUD | 1548 | 3.13% [2.26, 4.00] | 1288 | 83.20% [81.16, 85.25] | 203 | 13.11% [8.47, 17.76] | 57 | 3.68% |
| [−1.21, 8.57] | ||||||||
| (a) | ||||
| Covariate | OR | 95%CI | p-Value | |
| Delivery Year | 1.057 | 1.053 | 1.062 | <0.0001 |
| NICU vs. no NICU | 1.234 | 1.192 | 1.278 | <0.0001 |
| Race/Ethnicity (ref: White) | ||||
| Asian | 0.357 | 0.340 | 0.375 | <0.0001 |
| Black | 0.769 | 0.741 | 0.799 | <0.0001 |
| Hispanic | 0.690 | 0.668 | 0.713 | <0.0001 |
| Age (ref: ≤18) | ||||
| 19–26 | 1.066 | 0.870 | 1.306 | 0.5369 |
| 27–34 | 1.018 | 0.833 | 1.245 | 0.8605 |
| 35–39 | 1.080 | 0.883 | 1.321 | 0.4548 |
| ≥40 | 1.141 | 0.930 | 1.399 | 0.2051 |
| Insurance (ref: HMO/EPO) | ||||
| POS | 1.004 | 0.980 | 1.028 | 0.7485 |
| PPO | 1.129 | 1.038 | 1.227 | 0.0045 |
| Other | 1.059 | 0.944 | 1.188 | 0.3265 |
| Region (ref: West) | ||||
| Midwest | 1.142 | 1.109 | 1.175 | <0.0001 |
| Northeast | 1.018 | 0.981 | 1.056 | 0.3414 |
| South | 1.010 | 0.983 | 1.038 | 0.4511 |
| No SUD vs. Yes SUD | 0.572 | 0.540 | 0.605 | <0.0001 |
| No Other MH vs. Yes Other MH | 0.535 | 0.518 | 0.552 | <0.0001 |
| No pre-MH diagnoses of anxiety and/or depression vs. yes pre-MH diagnoses of anxiety and/or depression | 0.145 | 0.141 | 0.149 | <0.0001 |
| (b) | ||||
| Covariate | OR | 95%CI | p-Value | |
| Delivery Year | 1.057 | 1.053 | 1.062 | <0.0001 |
| NICU status (ref: No NICU) | ||||
| NICU <14 days | 1.194 | 1.149 | 1.241 | <0.0001 |
| NICU ≥14 days | 1.375 | 1.285 | 1.472 | <0.0001 |
| Race/Ethnicity (ref: White) | ||||
| Asian | 0.324 | 0.306 | 0.343 | <0.0001 |
| Black | 0.768 | 0.735 | 0.803 | <0.0001 |
| Hispanic | 0.697 | 0.672 | 0.724 | <0.0001 |
| Age (ref: ≤18) | ||||
| 19–26 | 0.947 | 0.760 | 1.181 | 0.6305 |
| 27–34 | 0.867 | 0.697 | 1.079 | 0.2015 |
| 35–39 | 0.901 | 0.723 | 1.121 | 0.3497 |
| ≥40 | 0.934 | 0.747 | 1.166 | 0.5451 |
| Insurance (ref: HMO/EPO) | ||||
| POS | 0.993 | 0.966 | 1.021 | 0.6274 |
| PPO | 1.083 | 0.979 | 1.197 | 0.1214 |
| Other | 1.005 | 0.873 | 1.156 | 0.9499 |
| Region (ref: West) | ||||
| Midwest | 1.102 | 1.067 | 1.140 | <0.0001 |
| Northeast | 0.935 | 0.895 | 0.977 | 0.0027 |
| South | 0.990 | 0.960 | 1.021 | 0.5355 |
| No SUD vs. Yes SUD | 0.545 | 0.507 | 0.585 | <0.0001 |
| No Other MH vs. Yes Other MH | 0.454 | 0.437 | 0.472 | <0.0001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Beck, D.C.; Tabb, K.M.; Tilea, A.; Hall, S.V.; Vance, A.; Patrick, S.W.; Schroeder, A.; Zivin, K. The Association between NICU Admission and Mental Health Diagnoses among Commercially Insured Postpartum Women in the US, 2010–2018. Children 2022, 9, 1550. https://doi.org/10.3390/children9101550
Beck DC, Tabb KM, Tilea A, Hall SV, Vance A, Patrick SW, Schroeder A, Zivin K. The Association between NICU Admission and Mental Health Diagnoses among Commercially Insured Postpartum Women in the US, 2010–2018. Children. 2022; 9(10):1550. https://doi.org/10.3390/children9101550
Chicago/Turabian StyleBeck, Dana C., Karen M. Tabb, Anca Tilea, Stephanie V. Hall, Ashlee Vance, Stephen W. Patrick, Amy Schroeder, and Kara Zivin. 2022. "The Association between NICU Admission and Mental Health Diagnoses among Commercially Insured Postpartum Women in the US, 2010–2018" Children 9, no. 10: 1550. https://doi.org/10.3390/children9101550






