Hepatitis A Immunity and Paediatric Liver Transplantation—A Single-Centre Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients and Data Acquisition
2.2. Chemiluminescence Microparticle Immunoassay for the Determination of Hepatitis A Immunity
2.3. Statistical Analysis
3. Results
3.1. Study Population
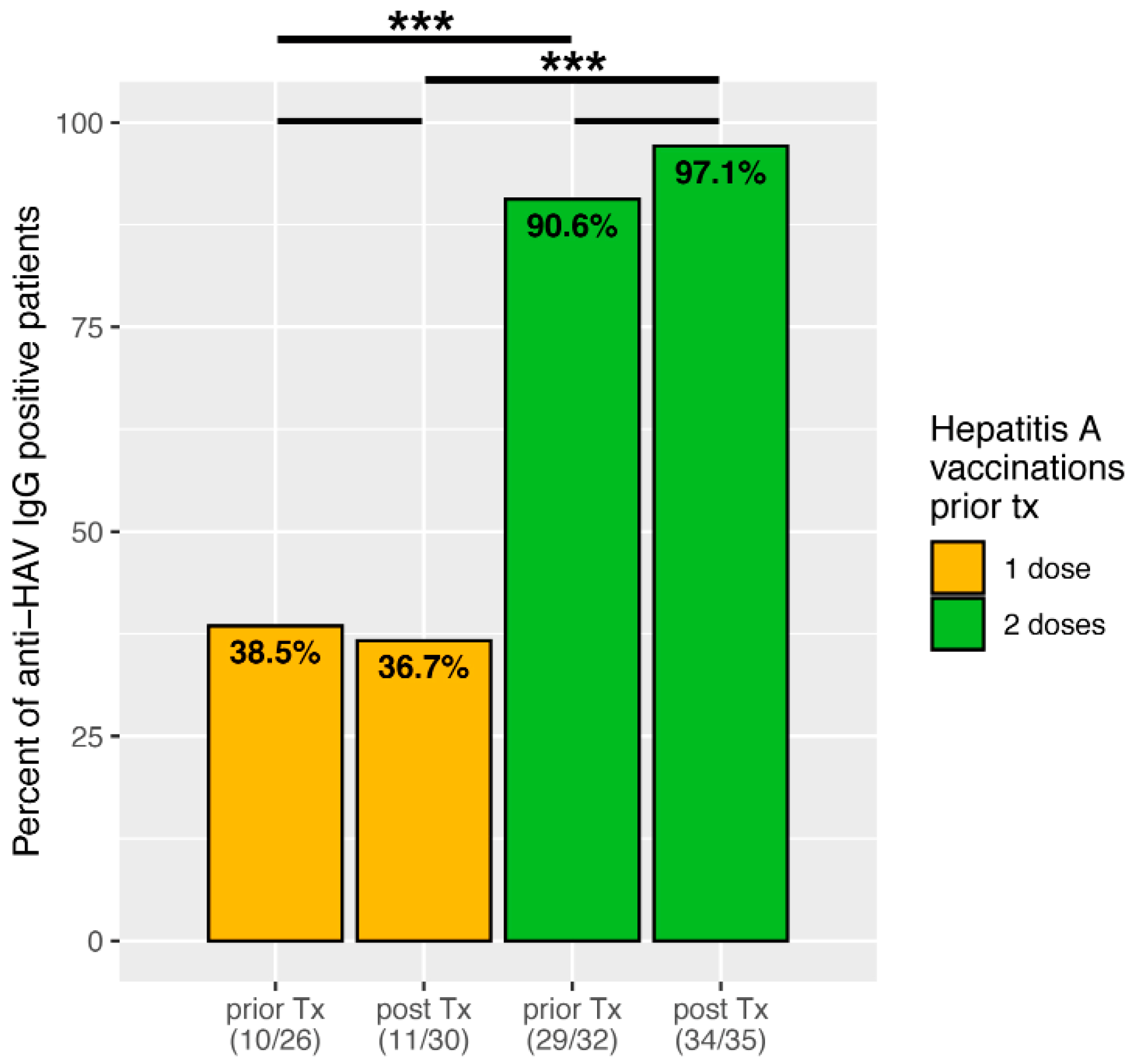
3.2. Hepatitis A Seroconversion Depending on Vaccination Doses Received before Liver Transplantation
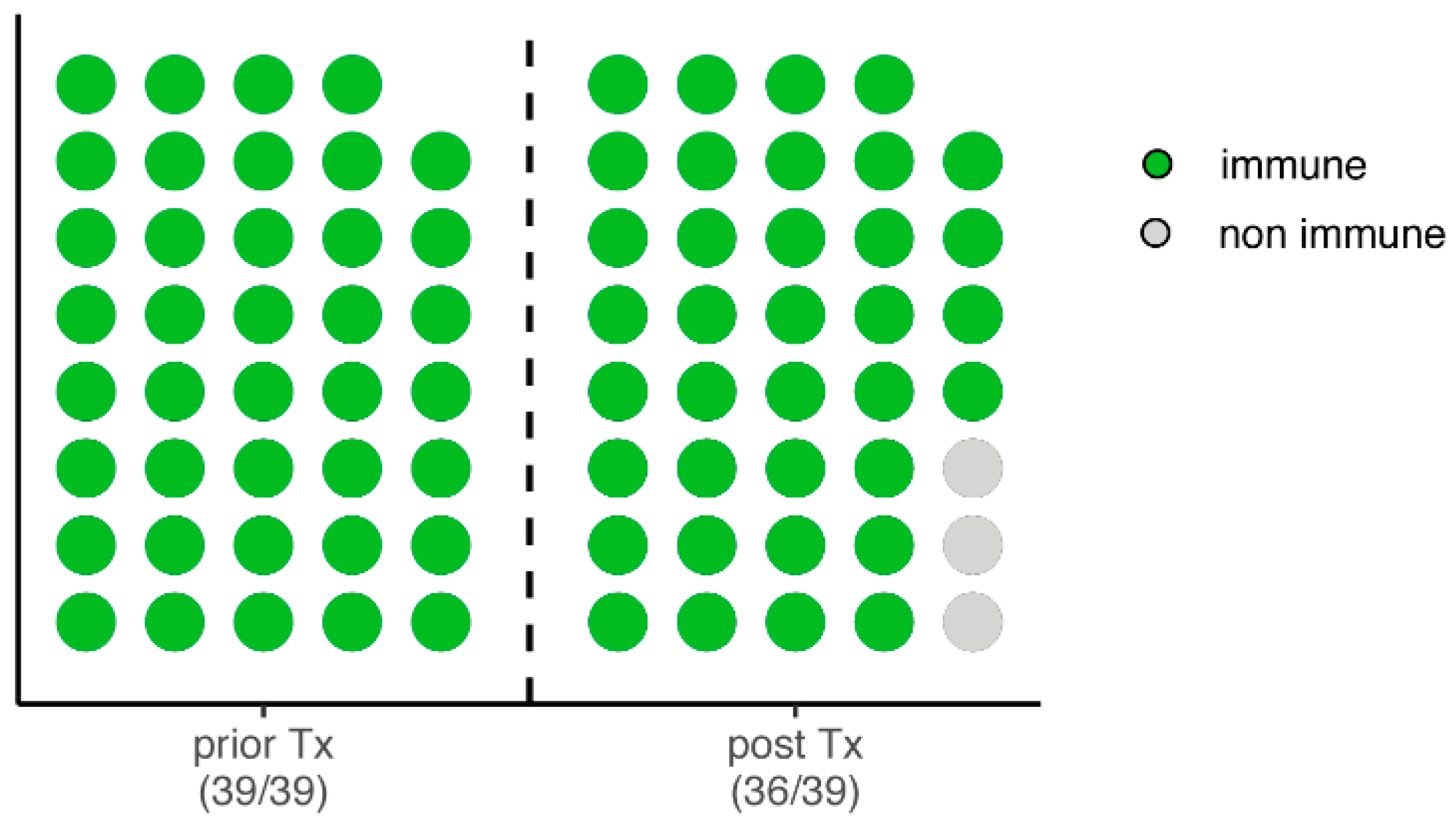
3.3. Intraindividual Change in Hepatitis A Immunity from Prior to Post Liver Transplantation
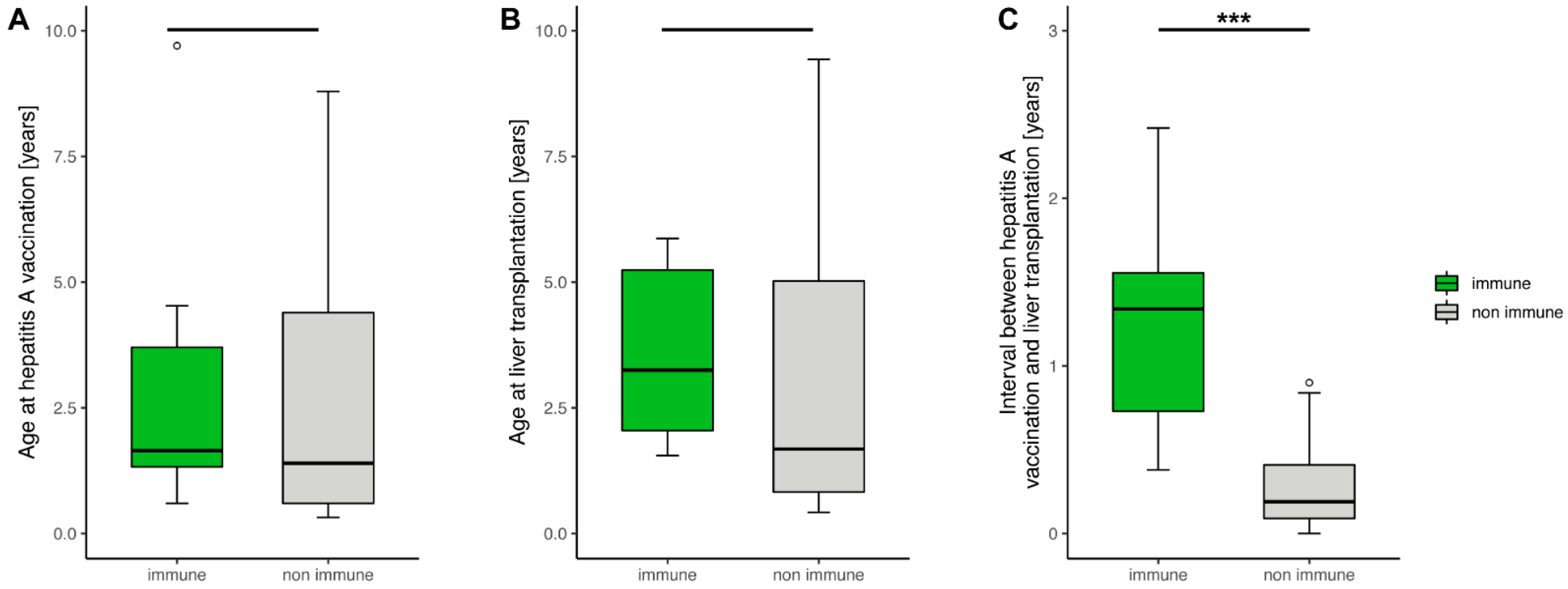
3.4. Factors Influencing Hepatitis A Immunity in Liver Transplanted Children
3.5. Factors Influencing Immunity after a Single Hepatitis A Dose
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Matheny, S.C.; Kingery, J.E. Hepatitis A. Am. Fam. Physician 2012, 86, 1027–1034. [Google Scholar] [PubMed]
- Tavoschi, L.; Severi, E.; Carrillo Santisteve, P.; Lopalco, P. Hepatitis A in the EU/EEA: The case for scaling up prevention. Vaccine 2018, 36, 2501–2503. [Google Scholar] [CrossRef] [PubMed]
- Debray, D.; Cullufi, P.; Devictor, D.; Fabre, M.; Bernard, O. Liver failure in children with hepatitis A. Hepatology 1997, 26, 1018–1022. [Google Scholar] [CrossRef]
- Zhang, L. Hepatitis A vaccination. Hum. Vaccin. Immunother 2020, 16, 1565–1573. [Google Scholar] [CrossRef] [PubMed]
- Juliao, P.; Abadia, I.; Welby, S.; Wery, S.; Wong, D.; De Leon, T.; DeAntonio, R.; Naranjo, L.; Guignard, A.; Marano, C. Hepatitis A antibody persistence 8 and 10 years after 1-dose and 2-dose vaccination in children from Panama. Vaccine 2021, 39, 26–34. [Google Scholar] [CrossRef] [PubMed]
- Van Herck, K.; Van Damme, P. Prevention of hepatitis A by Havrix: A review. Expert Rev. Vaccines 2005, 4, 459–471. [Google Scholar] [CrossRef] [PubMed]
- Theeten, H.; Van Herck, K.; Van Der Meeren, O.; Crasta, P.; Van Damme, P.; Hens, N. Long-term antibody persistence after vaccination with a 2-dose Havrix (inactivated hepatitis A vaccine): 20 years of observed data, and long-term model-based predictions. Vaccine 2015, 33, 5723–5727. [Google Scholar] [CrossRef]
- Langan, R.C.; Goodbred, A.J. Hepatitis A. Am. Fam. Physician 2021, 104, 368–374. [Google Scholar]
- Samandari, T.; Bell, B.P.; Armstrong, G.L. Quantifying the impact of hepatitis A immunization in the United States, 1995–2001. Vaccine 2004, 22, 4342–4350. [Google Scholar] [CrossRef]
- Cervio, G.; Trentadue, J.; D’Agostino, D.; Luque, C.; Giorgi, M.; Armoni, J.; Debbag, R. Decline in HAV-associated fulminant hepatic failure and liver transplant in children in Argentina after the introduction of a universal hepatitis A vaccination program. Hepat Med. 2011, 3, 99–106. [Google Scholar] [CrossRef]
- Laue, T.; Demir, Z.; Debray, D.; Cananzi, M.; Gaio, P.; Casotti, V.; D’Antiga, L.; Urbonas, V.; Baumann, U. Under-Vaccination in Pediatric Liver Transplant Candidates with Acute and Chronic Liver Disease-A Retrospective Observational Study of the European Reference Network Transplant Child. Children 2021, 8, 675. [Google Scholar] [CrossRef] [PubMed]
- Feldman, A.G.; Sundaram, S.S.; Beaty, B.L.; Torres, R.; Curtis, D.J.; Kempe, A. Immunization Status at the Time of Liver Transplant in Children and Adolescents. JAMA 2019, 322, 1822–1824. [Google Scholar] [CrossRef]
- Ferreira, C.T.; da Silveira, T.R.; Vieira, S.M.; Taniguchi, A.; Pereira-Lima, J. Immunogenicity and safety of hepatitis A vaccine in children with chronic liver disease. J. Pediatr. Gastroenterol Nutr. 2003, 37, 258–261. [Google Scholar] [CrossRef] [PubMed]
- Diana, A.; Posfay-Barbe, K.M.; Belli, D.C.; Siegrist, C.A. Vaccine-induced immunity in children after orthotopic liver transplantation: A 12-yr review of the Swiss national reference center. Pediatr. Transpl. 2007, 11, 31–37. [Google Scholar] [CrossRef] [PubMed]
- R Core Team. R: A Language and Environment for Statistical Computing; R Core Team: Vienna, Austria, 2021. [Google Scholar]
- Wickham, H. ggplot2: Elegant Graphics for Data Analysis; Springer: New York, NY, USA, 2016; pp. 189–201. [Google Scholar]
- Stalke, A.; Sgodda, M.; Cantz, T.; Skawran, B.; Lainka, E.; Hartleben, B.; Baumann, U.; Pfister, E.D. KIF12 Variants and Disturbed Hepatocyte Polarity in Children with a Phenotypic Spectrum of Cholestatic Liver Disease. J. Pediatr. 2022, 240, 284–291.e9. [Google Scholar] [CrossRef]
- L’Huillier, A.G.; Wildhaber, B.E.; Belli, D.C.; Diana, A.; Rodriguez, M.; Siegrist, C.A.; Posfay-Barbe, K.M. Successful serology-based intervention to increase protection against vaccine-preventable diseases in liver-transplanted children: A 19-yr review of the Swiss national reference center. Pediatr. Transpl. 2012, 16, 50–57. [Google Scholar] [CrossRef]
- Henry, B.; Baclic, O.; National Advisory Committee on, I. Summary of the National Advisory Committee on Immunization (NACI) Statement Update on the Recommended Use of Hepatitis A Vaccine. Can. Commun. Dis. Rep. 2016, 42, 193–194. [Google Scholar] [CrossRef]
- Rubin, L.G.; Levin, M.J.; Ljungman, P.; Davies, E.G.; Avery, R.; Tomblyn, M.; Bousvaros, A.; Dhanireddy, S.; Sung, L.; Keyserling, H.; et al. 2013 IDSA clinical practice guideline for vaccination of the immunocompromised host. Clin. Inf. Dis. 2014, 58, e44–e100. [Google Scholar] [CrossRef]
- Nelson, N.P.; Weng, M.K.; Hofmeister, M.G.; Moore, K.L.; Doshani, M.; Kamili, S.; Koneru, A.; Haber, P.; Hagan, L.; Romero, J.R.; et al. Prevention of Hepatitis A Virus Infection in the United States: Recommendations of the Advisory Committee on Immunization Practices, 2020. MMWR Recomm. Rep. 2020, 69, 1–38. [Google Scholar] [CrossRef]
- Feldman, A.G.; Kempe, A.; Beaty, B.L.; Sundaram, S.S.; Studies of Pediatric Liver Transplantation Research Group. Immunization practices among pediatric transplant hepatologists. Pediatr. Transpl. 2016, 20, 1038–1044. [Google Scholar] [CrossRef]
- Elisofon, S.A.; Magee, J.C.; Ng, V.L.; Horslen, S.P.; Fioravanti, V.; Economides, J.; Erinjeri, J.; Anand, R.; Mazariegos, G.V.; Studies of Pediatric Liver Transplantation Research Group. Society of pediatric liver transplantation: Current registry status 2011–2018. Pediatr. Transpl. 2020, 24, e13605. [Google Scholar] [CrossRef] [PubMed]
- Leiskau, C.; Junge, N.; Pfister, E.D.; Goldschmidt, I.; Mutschler, F.; Laue, T.; Ohlendorf, J.; Nasser, H.; Beneke, J.; Richter, N.; et al. Recipient-Specific Risk Factors Impairing Patient and Graft Outcome after Pediatric Liver Transplantation-Analysis of 858 Transplantations in 38 Years. Children 2021, 8, 641. [Google Scholar] [CrossRef]
- Tessitore, M.; Sorrentino, E.; Schiano Di Cola, G.; Colucci, A.; Vajro, P.; Mandato, C. Malnutrition in Pediatric Chronic Cholestatic Disease: An Up-to-Date Overview. Nutrients 2021, 13, 2785. [Google Scholar] [CrossRef] [PubMed]
- Rytter, M.J.; Kolte, L.; Briend, A.; Friis, H.; Christensen, V.B. The immune system in children with malnutrition—A systematic review. PLoS ONE 2014, 9, e105017. [Google Scholar] [CrossRef] [PubMed]
- Ashur, Y.; Adler, R.; Rowe, M.; Shouval, D. Comparison of immunogenicity of two hepatitis A vaccines—VAQTA and HAVRIX—In young adults. Vaccine 1999, 17, 2290–2296. [Google Scholar] [CrossRef] [PubMed]
- Davis, J.P. Experience with hepatitis A and B vaccines. Am. J. Med. 2005, 118, 7S–15S. [Google Scholar] [CrossRef]
| All Children Included (n = 65) | |
|---|---|
| Gender, male (%)/female (%) | 23 (35.4%)/42 (64.6%) |
| Diagnosis | Biliary atresia: 30 (46.2%) Progressive familial intrahepatic cholestasis: 13 (20%) Cystic fibrosis: 5 (7.7%) Cryptogenic cirrhosis: 5 (7.7%) Alagille syndrome: 4 (6.2%) Metabolic conditions: 3 (4.6%) Hepatic malignancy: 1 (1.5%) Acute liver failure: 1 (1.5%) Primary sclerosing cholangitis: 1 (1.5%) KIF12 variant: 1 (1.5%) Alpha-1 antitrypsin deficiency: 1 (1.5%) |
| Number of hepatitis A doses prior to transplantation | 1 dose: 30 (46.1%) 2 doses: 35 (53.8%) |
| Age at 1st hepatitis A dose prior to transplantation in years, median (IQR) | 2.1 (1.2–4.1) |
| Age at 2nd hepatitis A dose prior to transplantation in years, median (IQR) | 3.1 (2.1–5.1) |
| Age at time of transplant in years, median (IQR) | 4.6 (2.0–7.8) |
| Immune (n = 36) | Non-Immune (n = 3) | p | |
|---|---|---|---|
| Gender, male (%)/female (%) | 13 (36.1%)/23 (63.9%) | 0 (0.0%)/3 (100.0%) | 0.5377 |
| Completed basic immunisation with 2 vaccine doses | 29 (80.6%) | 0 (0.0%) | <0.0131 |
| Occurrence of biopsy-proven acute rejection (%) | 14 (38.9%) | 3 (100.0%) | 0.0744 |
| Vaccination administered below 12 months of age (%) | 1 (2.8%) | 1 (33.3%) | 0.1498 |
| Immunosuppression | |||
| Tacrolimus (%) | 29 (80.6%) | 2 (66.7%) | 0.5082 |
| Ciclosporine (%) | 7 (19.4%) | 1 (33.3%) | 0.5082 |
| Intensified immunosuppression, calcineurin inhibitor + prednisolone or mycophenolate mofetil | 15 (41.7%) | 3 (100.0%) | 0.0893 |
| Immune (n = 45) | Non-Immune (n = 20) | p | |
|---|---|---|---|
| Gender, male (%)/female (%) | 16 (35.6%)/29 (64.4%) | 7 (35.0%)/13 (65.0%) | 0.966 |
| Completed basic immunisation with 2 vaccine doses | 34 (75.6%) | 1 (5.0%) | <0.00001 |
| Age at 1st hepatitis A dose, median (IQR) | 2.14 (1.35–4.09) | 1.48 (0.60–4.40) | 0.215 |
| Age at liver transplantation, median (IQR) | 5.54 (3.13–8.19) | 1.84 (0.81–5.05) | 0.0008 |
| Interval between last hepatitis A dose and liver transplantation, median (IQR) | 1.41 (0.56–2.65) | 0.18 (0.07–0.41) | <0.00001 |
| Occurrence of biopsy-proven acute rejection (%) | 15 (50.0%) | 8 (40.0%) | 0.648 |
| Vaccination administered below 12 months of age (%) | 1 (2.2%) | 6 (30.0%) | 0.000855 |
| Immunosuppression | |||
| Tacrolimus (%) | 33 (73.3%) | 12 (60.0%) | 0.282 |
| Tacrolimus trough level, median (IQR) [µg/L] | 5.0 (3.9–6.5) | 4.4 (3.8–4.7) | 0.150 |
| Ciclosporine (%) | 12 (26.7%) | 8 (40.0%) | 0.282 |
| Ciclosporine trough level, median (IQR) [µg/L] | 131 (110–171) | 118 (113–163) | 0.881 |
| Intensified immunosuppression, calcineurin inhibitor + prednisolone or mycophenolate mofetil | 19 (42.2%) | 12 (60.0%) | 0.185 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Laue, T.; Ohlendorf, J.; Leiskau, C.; Baumann, U. Hepatitis A Immunity and Paediatric Liver Transplantation—A Single-Centre Analysis. Children 2022, 9, 1953. https://doi.org/10.3390/children9121953
Laue T, Ohlendorf J, Leiskau C, Baumann U. Hepatitis A Immunity and Paediatric Liver Transplantation—A Single-Centre Analysis. Children. 2022; 9(12):1953. https://doi.org/10.3390/children9121953
Chicago/Turabian StyleLaue, Tobias, Johanna Ohlendorf, Christoph Leiskau, and Ulrich Baumann. 2022. "Hepatitis A Immunity and Paediatric Liver Transplantation—A Single-Centre Analysis" Children 9, no. 12: 1953. https://doi.org/10.3390/children9121953
APA StyleLaue, T., Ohlendorf, J., Leiskau, C., & Baumann, U. (2022). Hepatitis A Immunity and Paediatric Liver Transplantation—A Single-Centre Analysis. Children, 9(12), 1953. https://doi.org/10.3390/children9121953






