Neonatal Resuscitation Skill-Training Using a New Neonatal Simulator, Facilitated by Local Motivators: Two-Year Prospective Observational Study of 9000 Trainings
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Setting
2.2. NeoNatalie Live—Newborn Resuscitation Simulator
2.3. Implementation of NeoNatalie Live and HBB Second Edition
2.4. Study Participants
2.5. Data Collection
2.6. Statistics
3. Results
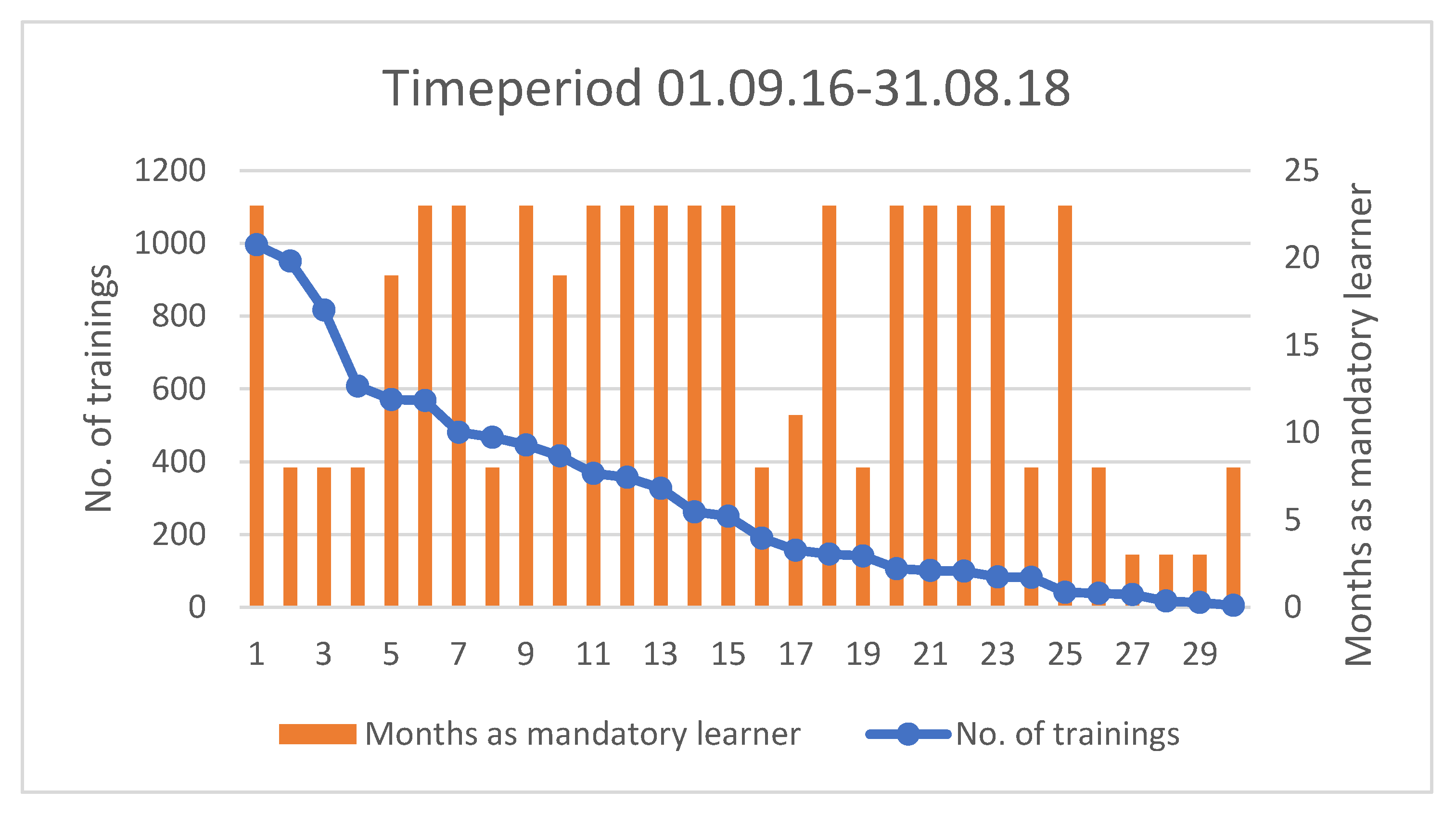
3.1. Participation and Frequency of Trainings Per Midwife
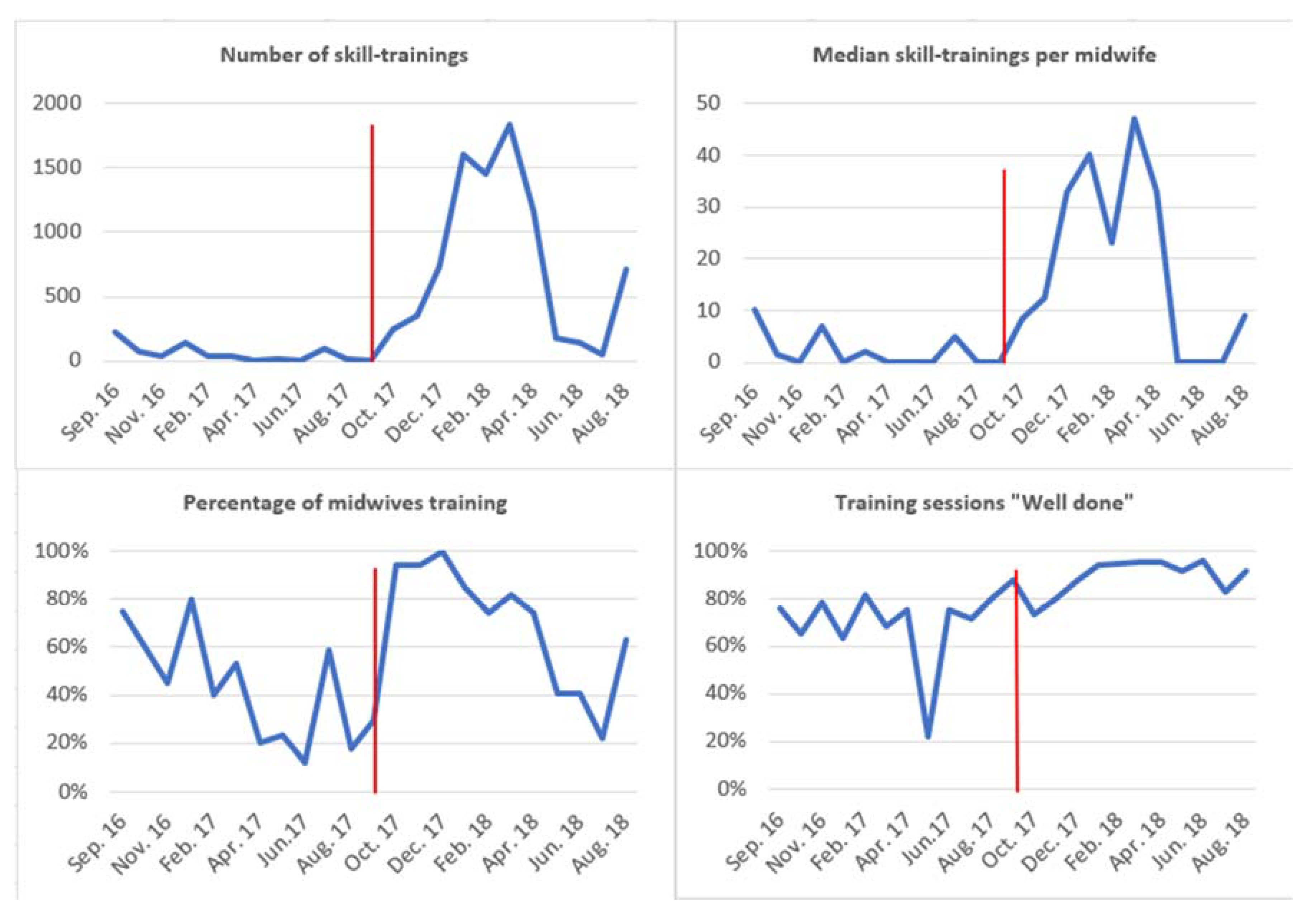
3.2. Training-Frequency, Participation and Ventilation Quality
4. Discussion
4.1. Local Motivators and Training Frequency
4.2. Features of the Simulator, NeoNatalie Live
4.3. Optimal Level of Training Frequency
4.4. Strengths and Limitations
4.5. Future Studies
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Liu, L.; Oza, S.; Hogan, D.; Chu, Y.; Perin, J.; Zhu, J.; Lawn, J.E.; Cousens, S.; Mathers, C.; Black, R.E. Global, regional, and national causes of under-5 mortality in 2000–15: An updated systematic analysis with implications for the Sustainable Development Goals. Lancet 2016, 388, 3027–3035. [Google Scholar] [CrossRef] [Green Version]
- Lehtonen, L.; Gimeno, A.; Llorca, A.P.; Vento, M. Early neonatal death: A challenge worldwide. Semin. Fetal Neonatal Med. 2017, 22, 153–160. [Google Scholar] [CrossRef]
- Ersdal, H.L.; Eilevstjønn, J.; Linde, J.E.; Yeconia, A.; Mduma, E.R.; Kidanto, H.; Perlman, J. Fresh stillborn and severely asphyxiated neonates share a common hypoxic–ischemic pathway. Int. J. Gynecol. Obstet. 2018, 141, 171–180. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Liddell, C.A.; Coates, M.M.; Mooney, M.D.; Levitz, C.E.; Schumacher, A.E.; Apfel, H.; Iannarone, M.; Phillips, B.; Lofgren, K.T.; et al. Global, regional, and national levels of neonatal, infant, and under-5 mortality during 1990–2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet 2014, 384, 957–979. [Google Scholar] [CrossRef] [Green Version]
- Dempsey, E.; Pammi, M.; Ryan, A.C.; Barrington, K.J. Standardised formal resuscitation training programmes for reducing mortality and morbidity in newborn infants. Cochrane Database Syst. Rev. 2015. Available online: https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD009106.pub2/full (accessed on 1 November 2021). [CrossRef] [PubMed]
- Mundell, W.C.; Kennedy, C.C.; Szostek, J.H.; Cook, D.E. Simulation technology for resuscitation training: A systematic review and meta-analysis—ScienceDirect. Resuscitation 2012, 84, 1174–1183. [Google Scholar] [CrossRef]
- Issenberg, S.B.; McGaghie, W.C.; Petrusa, E.R.; Lee Gordon, D.; Scalese, R.J. Features and uses of high-fidelity medical simulations that lead to effective learning: A BEME systematic review. Med. Teach. 2005, 27, 10–28. [Google Scholar] [CrossRef]
- Morris, S.M.; Fratt, E.M.; Rodriguez, J.; Ruman, A.; Wibecan, L.; Nelson, B.D. Implementation of the Helping Babies Breathe Training Program: A Systematic Review. Pediatrics 2020, 146, e20193938. Available online: https://pediatrics.aappublications.org/content/146/3/e20193938 (accessed on 1 November 2021). [CrossRef]
- NeoNatalie [Internet]. Laerdal Medical. Available online: https://laerdal.com/no/products/simulation-training/obstetrics-paediatrics/neonatalie/ (accessed on 1 November 2021).
- Helping Babies Breathe [Internet]. AAP.org. Available online: http://www.aap.org/en-us/advocacy-and-policy/aap-health-initiatives/helping-babies-survive/Pages/Helping-Babies-Breathe.aspx (accessed on 1 November 2021).
- Kamath-Rayne, B.D.; Thukral, A.; Visick, M.K.; Schoen, E.; Amick, E.; Deorari, A.; Cain, C.J.; Keenan, W.J.; Singhal, N.; Little, G.A.; et al. Helping Babies Breathe, Second Edition: A Model for Strengthening Educational Programs to Increase Global Newborn Survival. Glob. Health Sci. Pract. 2018, 6, 538–551. [Google Scholar] [CrossRef] [Green Version]
- Bang, A.; Patel, A.; Bellad, R.; Gisore, P.; Goudar, S.S.; Esamai, F.; Liechty, E.A.; Meleth, S.; Goco, N.; Niermeyer, S.; et al. Helping Babies Breathe (HBB) training: What happens to knowledge and skills over time? BMC Pregnancy Childbirth 2016, 16, 364. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5120476/ (accessed on 1 November 2021). [CrossRef] [PubMed] [Green Version]
- Versantvoort, J.M.D.; Kleinhout, M.Y.; Ockhuijsen, H.D.L.; Bloemenkamp, K.; Hoogen, A.V.D. Helping Babies Breathe and its effects on intrapartum-related stillbirths and neonatal mortality in low-resource settings: A systematic review. Arch. Dis. Child. 2020, 105, 127–133. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dol, J.; Campbell-Yeo, M.; Murphy, G.T.; Aston, M.; McMillan, D.; Richardson, B. The impact of the Helping Babies Survive program on neonatal outcomes and health provider skills: A systematic review. JBI Database Syst. Rev. Implement Rep. 2018, 16, 701–737. [Google Scholar] [CrossRef] [PubMed]
- Moshiro, R.; Ersdal, H.; Mdoe, P.; Kidanto, H.; Mbekenga, C. Factors affecting effective ventilation during newborn resuscitation: A qualitative study among midwives in rural Tanzania. Glob. Health Action 2018, 11, 1423862. [Google Scholar] [CrossRef]
- NeoNatalie Live–Safer Births [Internet]. 2021. Available online: http://www.saferbirths.com/portfolio_page/newborn-ventilation-trainer/ (accessed on 1 November 2021).
- Chaulagain, D.R.; Malqvist, M.; Brunell, O.; Wrammert, J.; Basnet, O.; Ashish, K.C. Performance of health workers on neonatal resuscitation care following scaled-up quality improvement interventions in public hospitals of Nepal—A prospective observational study. BMC Health Serv. Res. 2021, 21, 362. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8054430/ (accessed on 1 November 2021). [CrossRef]
- Mduma, E.; Ersdal, H.; Svensen, E.; Kidanto, H.; Auestad, B.; Perlman, J. Frequent brief on-site simulation training and reduction in 24-h neonatal mortality--an educational intervention study. Resuscitation 2015, 93, 1–7. [Google Scholar] [CrossRef]
- Mduma, E.; Kvaløy, J.T.; Soreide, E.; Svensen, E.; Mdoe, P.; Perlman, J.; Johnson, C.; Kidanto, H.L.; Ersdal, H.L. Frequent refresher training on newborn resuscitation and potential impact on perinatal outcome over time in a rural Tanzanian hospital: An observational study. BMJ Open 2019, 9, e030572. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6773328/ (accessed on 1 November 2021). [CrossRef] [Green Version]
- Størdal, K.; Eilevstjønn, J.; Mduma, E.; Holte, K.; Thallinger, M.; Linde, J.; Mdoe, P.; Kidanto, H.; Ersdal, H.L. Increased perinatal survival and improved ventilation skills over a five-year period: An observational study. PLoS ONE 2020, 15, e0240520. [Google Scholar] [CrossRef]
- Haynes, J.; Bjorland, P.; Gomo, Ø.; Ushakova, A.; Rettedal, S.; Perlman, J.; Ersdal, H. Novel Neonatal Simulator Provides High-Fidelity Ventilation Training Comparable to Real-Life Newborn Ventilation. Children 2021, 8, 940. [Google Scholar] [CrossRef]
- Al-Ghareeb, A.Z.; Cooper, S.J. Barriers and enablers to the use of high-fidelity patient simulation manikins in nurse education: An integrative review. Nurse Educ. Today 2016, 36, 281–286. [Google Scholar] [CrossRef]
- Bergh, A.-M.; Baloyi, S.; Pattinson, R.C. What is the impact of multi-professional emergency obstetric and neonatal care training? Best Pract. Res. Clin. Obstet. Gynaecol. 2015, 29, 1028–1043. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McGaghie, W.C.; Issenberg, S.B.; Petrusa, E.R.; Scalese, R.J. A critical review of simulation-based medical education research: 2003–2009. Med. Educ. 2010, 44, 50–63. [Google Scholar] [CrossRef] [PubMed]
- Hatala, R.; Cook, D.A.; Zendejas, B.; Hamstra, S.J.; Brydges, R. Feedback for simulation-based procedural skills training: A meta-analysis and critical narrative synthesis. Adv. Health Sci. Educ. 2014, 19, 251–272. [Google Scholar] [CrossRef]
- Wilson, C.; Furness, E.; Proctor, L.; Sweetman, G.; Hird, K. A randomised trial of the effectiveness of instructor versus automated manikin feedback for training junior doctors in life support skills. Perspect. Med. Educ. 2021, 10, 95–100. [Google Scholar] [CrossRef]
- Handeland, J.A.; Prinz, A.; Ekra, E.M.R.; Fossum, M. The role of manikins in nursing students’ learning: A systematic review and thematic metasynthesis. Nurse Educ. Today 2021, 98, 104661. [Google Scholar] [CrossRef]
- Sherwood, R.J.; Francis, G. The effect of mannequin fidelity on the achievement of learning outcomes for nursing, midwifery and allied healthcare practitioners: Systematic review and meta-analysis. Nurse Educ. Today 2018, 69, 81–94. [Google Scholar] [CrossRef] [PubMed]
- Gurung, R.; Gurung, A.; Sunny, A.K.; Basnet, O.; Shrestha, S.K.; Gomo, Ø.H.; Myklebust, H.; Girnary, S.; Ashish, K.C. Effect of skill drills on neonatal ventilation performance in a simulated setting- observation study in Nepal. BMC Pediatr. 2019, 19, 387. [Google Scholar] [CrossRef] [PubMed]


| Before (1 September 2016–30 September 2017) | After (1 October 2017–31 August 2018) | p-Value | |
|---|---|---|---|
| Mandatory learners, n | 15–18 | 18–27 | |
| Median per month (quartiles) | 17.0 (15.0, 19.3) | 27.0 (18.0, 27.0) | <0.001 † |
| Skill-trainings, n | 688 | 8451 | <0.001 † |
| Median per month (quartiles) | 39.5 (8.3, 87.0) | 713 (173, 1455) | |
| Skill-trainings/midwife/month, n | |||
| Median (quartiles) | 2.3 (0.5, 5.0) | 26.4 (6.4, 53.9) | <0.001 † |
| Midwives training, % | |||
| Median (quartiles) | 43 (21, 60) | 74 (41, 94) | 0.016 † |
| Training performance Trainings “well done”, % | |||
| Median (quartiles) | 75 (66, 80) | 92 (83, 95) | <0.001 † |
| Valid ventilations, % | |||
| Median (quartiles) | 98 (87, 100) | 100 (88, 100) | <0.001 † |
| Ventilation rate, n | |||
| Median (quartiles) | 51 (45, 56) | 51 (47, 54) | 0.754 † |
| Selected patient cases, n (%) | |||
| Patient case 1 | 194 (28.2) | 2154 (25.5) | 0.131 ‡ |
| Patient case 2 | 134 (19.5) | 1924 (22.8) | |
| Patient case 3 | 147 (21.4) | 1881 (22.3) | |
| Patient case 4 | 142 (20.7) | 1760 (20.8) | |
| Random patient case | 71 (10.3) | 732 (8.7) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vadla, M.S.; Mdoe, P.; Moshiro, R.; Haug, I.A.; Gomo, Ø.; Kvaløy, J.T.; Oftedal, B.; Ersdal, H. Neonatal Resuscitation Skill-Training Using a New Neonatal Simulator, Facilitated by Local Motivators: Two-Year Prospective Observational Study of 9000 Trainings. Children 2022, 9, 134. https://doi.org/10.3390/children9020134
Vadla MS, Mdoe P, Moshiro R, Haug IA, Gomo Ø, Kvaløy JT, Oftedal B, Ersdal H. Neonatal Resuscitation Skill-Training Using a New Neonatal Simulator, Facilitated by Local Motivators: Two-Year Prospective Observational Study of 9000 Trainings. Children. 2022; 9(2):134. https://doi.org/10.3390/children9020134
Chicago/Turabian StyleVadla, May Sissel, Paschal Mdoe, Robert Moshiro, Ingunn Anda Haug, Øystein Gomo, Jan Terje Kvaløy, Bjørg Oftedal, and Hege Ersdal. 2022. "Neonatal Resuscitation Skill-Training Using a New Neonatal Simulator, Facilitated by Local Motivators: Two-Year Prospective Observational Study of 9000 Trainings" Children 9, no. 2: 134. https://doi.org/10.3390/children9020134
APA StyleVadla, M. S., Mdoe, P., Moshiro, R., Haug, I. A., Gomo, Ø., Kvaløy, J. T., Oftedal, B., & Ersdal, H. (2022). Neonatal Resuscitation Skill-Training Using a New Neonatal Simulator, Facilitated by Local Motivators: Two-Year Prospective Observational Study of 9000 Trainings. Children, 9(2), 134. https://doi.org/10.3390/children9020134







