Pediatric Lichen Myxedematosus: A Diagnostic and Management Challenge
Abstract
:1. Introduction
2. Case Descriptions
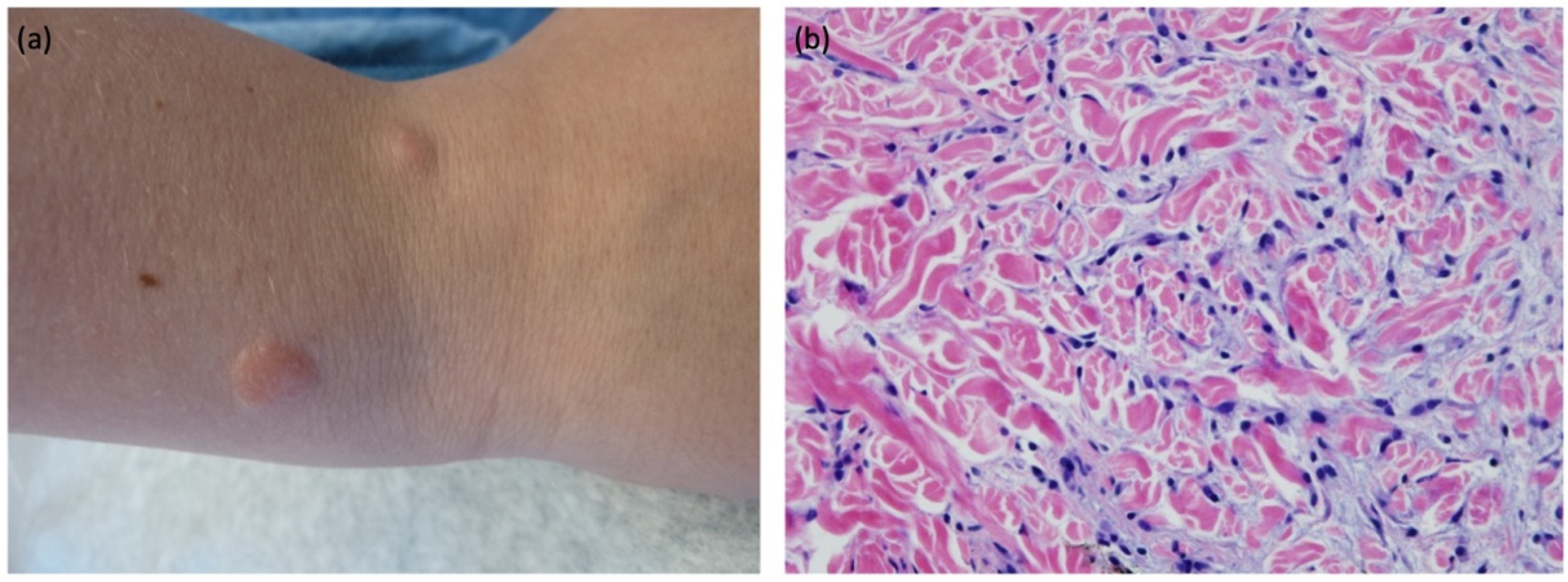
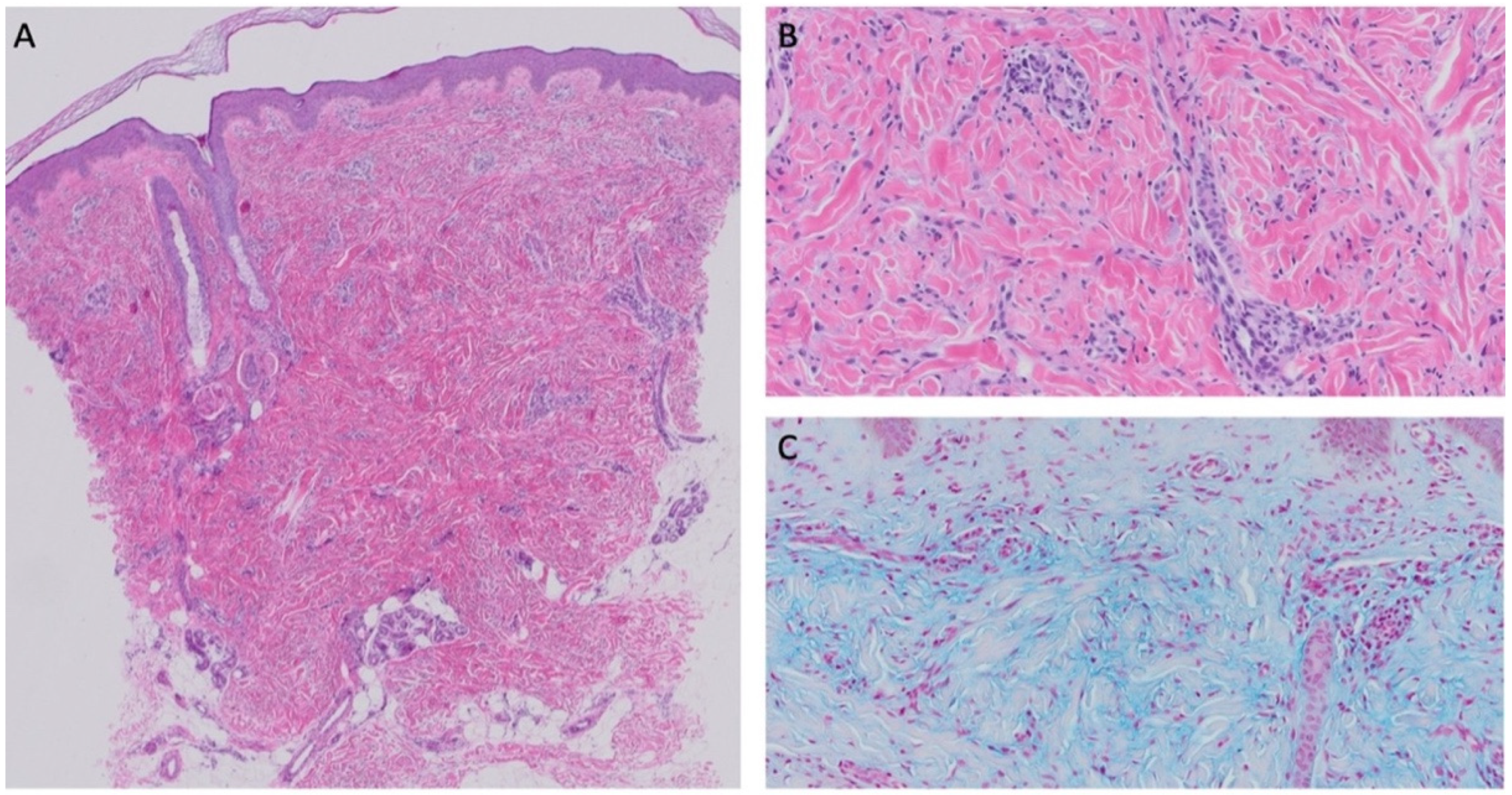
2.1. Case 1
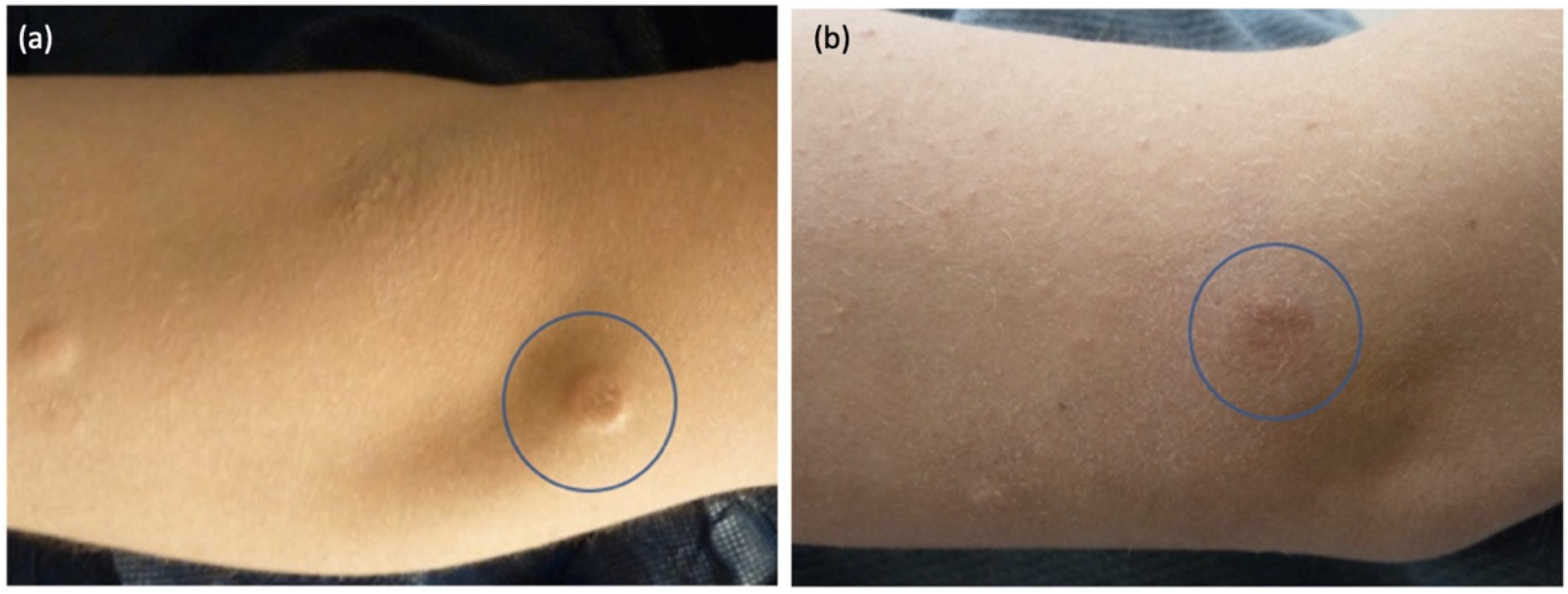
2.2. Case 2
3. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Rongioletti, F.; Rebora, A. Updated classification of papular mucinosis, lichen myxedematosus, and scleromyxedema. J. Am. Acad. Dermatol. 2001, 44, 273–281. [Google Scholar] [CrossRef] [PubMed]
- Nofal, A.; Amer, H.; Alakad, R.; Nofal, E.; El Desouky, F.; Yosef, A.; Albalat, W.; Gharib, K.; Mostafa, I.; Fathy, S.; et al. Lichen myxedematosus: Diagnostic criteria, classification, and severity grading. Int. J. Dermatol. 2017, 56, 284–290. [Google Scholar] [CrossRef] [PubMed]
- Zeng, R.; Li, M.; Jiang, Y.; Liu, W. Nodular lichen myxedematosus during childhood: A case report. Pediatr. Dermatol. 2014, 31, e160–e163. [Google Scholar] [CrossRef] [PubMed]
- Ogita, A.; Higashi, N.; Hosone, M.; Kawana, S. Nodular-type lichen myxedematosus: A case report. Case Rep. Dermatol. 2010, 2, 195–200. [Google Scholar] [CrossRef] [PubMed]
- Fang, X.; Yang, B.; Zhou, G.; Zhang, F. Localized lichen myxedematosus in childhood: What is the accurate diagnosis? Int. J. Dermatol. 2017, 56, 333–336. [Google Scholar] [CrossRef] [PubMed]
- Rongioletti, F.; Ferreli, C.; Atzori, L. Acral persistent papular mucinosis. Clin. Dermatol. 2021, 39, 211–214. [Google Scholar] [CrossRef] [PubMed]
- Lee, M.Y.; Byun, J.Y.; Choi, H.Y.; Choi, Y.W. Mucinous nevus. Ann. Dermatol. 2018, 30, 465–467. [Google Scholar] [CrossRef] [PubMed]
- Cobos, G.; Braunstein, I.; Abuabara, K.; Chu, E.Y.; James, W. Mucinous nevus: Report of a case and review of the literature. JAMA Dermatol. 2013, 150, 1018–1019. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Luchsinger, I.; Coulombe, J.; Rongioletti, F.; Haspeslagh, M.; Dompmartin, A.; Melki, I.; Dagher, R.; Bader-Meunier, B.; Fraitag, S.; Bodemer, C. Self-healing juvenile cutaneous mucinosis: Clinical and histopathologic findings of 9 patients: The relevance of long-term follow-up. J. Am. Acad. Dermatol. 2018, 78, 1164–1170. [Google Scholar] [CrossRef] [PubMed]
- Wadee, S.; Roode, H.; Schulz, E.J. Self-healing juvenile cutaneous mucinosis in a patient with nephroblastoma. Clin. Exp. Dermatol. 1994, 19, 90–93. [Google Scholar] [CrossRef] [PubMed]
- Barreau, M.; Dompmartin-Blanchère, A.; Jamous, R.; Chababi, M.; Soutou, B.; Reynier-Rezzi, J.; Laplaud, A.-L.; Acher, A.; Rod, J.; Jeanne-Pasquier, C.; et al. Nodular lesions of self-healing juvenile cutaneous mucinosis: A pitfall! Am. J. Dermatopathol. 2012, 34, 699–705. [Google Scholar] [CrossRef] [PubMed]
- Nagaraj, L.V.; Fangman, W.; White, W.L.; Woosley, J.T.; Prose, N.; Selim, M.A.; Morrell, D.S. Self-healing juvenile cutaneous mucinosis: Cases highlighting subcutaneous/fascial involvement. J. Am. Acad. Dermatol. 2006, 55, 1036–1043. [Google Scholar] [CrossRef] [PubMed]
- Pucevich, M.V.; Latour, D.L.; Bale, G.F.; King, L.E., Jr. Self-healing juvenile cutaneous mucinosis. J. Am. Acad. Dermatol. 1984, 11, 327–332. [Google Scholar] [CrossRef]
- Suter, L.; Vakilzadeh, F.; Macher, E. Atypical tuberous myxedema Jadassohn-Dossekker. Report of a case. Dermatologica 1980, 161, 265–269. [Google Scholar] [CrossRef] [PubMed]
- Montero-Vilchez, T.; Martinez-Lopez, A.; Cuenca-Barrales, C.; Martin-Castro, A.; Molina-Leyva, A.; Arias-Santiago, S. Nodular lichen myxoedematous: A new adverse event associated with ustekinumab. Aust. J. Dermaol. 2020, 61, e344–e345. [Google Scholar] [CrossRef] [PubMed]

| Rongioletti and Rebora (2001) | Nofal et al. (2017) |
|---|---|
Scleromyxedema
| Constant Features (Scleromyxedema or Pure Cutaneous)
|
Localized LM
| Variable Associated Features (Scleromyxedema or Pure Cutaneous)
|
| Clinicopathologic Subtypes: self-healing (juvenile and adult variant) *, discrete papular, acral persistent, papular mucinosis of infancy, nodular | |
| * Clinical criteria for juvenile variant include: (1) young age at presentation (2) acute eruption of papules on the face, neck, scalp, abdomen, thighs (3) variable development of nodules on face and periarticular regions (4) variable association with fevers, arthralgias, weakness (5) spontaneous resolution, typically within weeks to months | |
Atypical Subtypes of LM
| Distinguishing Features Systemic (Scleromyxedema):
|
Pure Cutaneous Subtype:
|
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Barry, K.K.; Reusch, D.B.; Schmidt, B.A.R.; Hawryluk, E.B. Pediatric Lichen Myxedematosus: A Diagnostic and Management Challenge. Children 2022, 9, 949. https://doi.org/10.3390/children9070949
Barry KK, Reusch DB, Schmidt BAR, Hawryluk EB. Pediatric Lichen Myxedematosus: A Diagnostic and Management Challenge. Children. 2022; 9(7):949. https://doi.org/10.3390/children9070949
Chicago/Turabian StyleBarry, Kelly K., Diana B. Reusch, Birgitta A. R. Schmidt, and Elena B. Hawryluk. 2022. "Pediatric Lichen Myxedematosus: A Diagnostic and Management Challenge" Children 9, no. 7: 949. https://doi.org/10.3390/children9070949
APA StyleBarry, K. K., Reusch, D. B., Schmidt, B. A. R., & Hawryluk, E. B. (2022). Pediatric Lichen Myxedematosus: A Diagnostic and Management Challenge. Children, 9(7), 949. https://doi.org/10.3390/children9070949







