Three-Dimensional-Printed Customized Orthodontic and Pedodontic Appliances: A Critical Review of a New Era for Treatment
Abstract
:1. Introduction
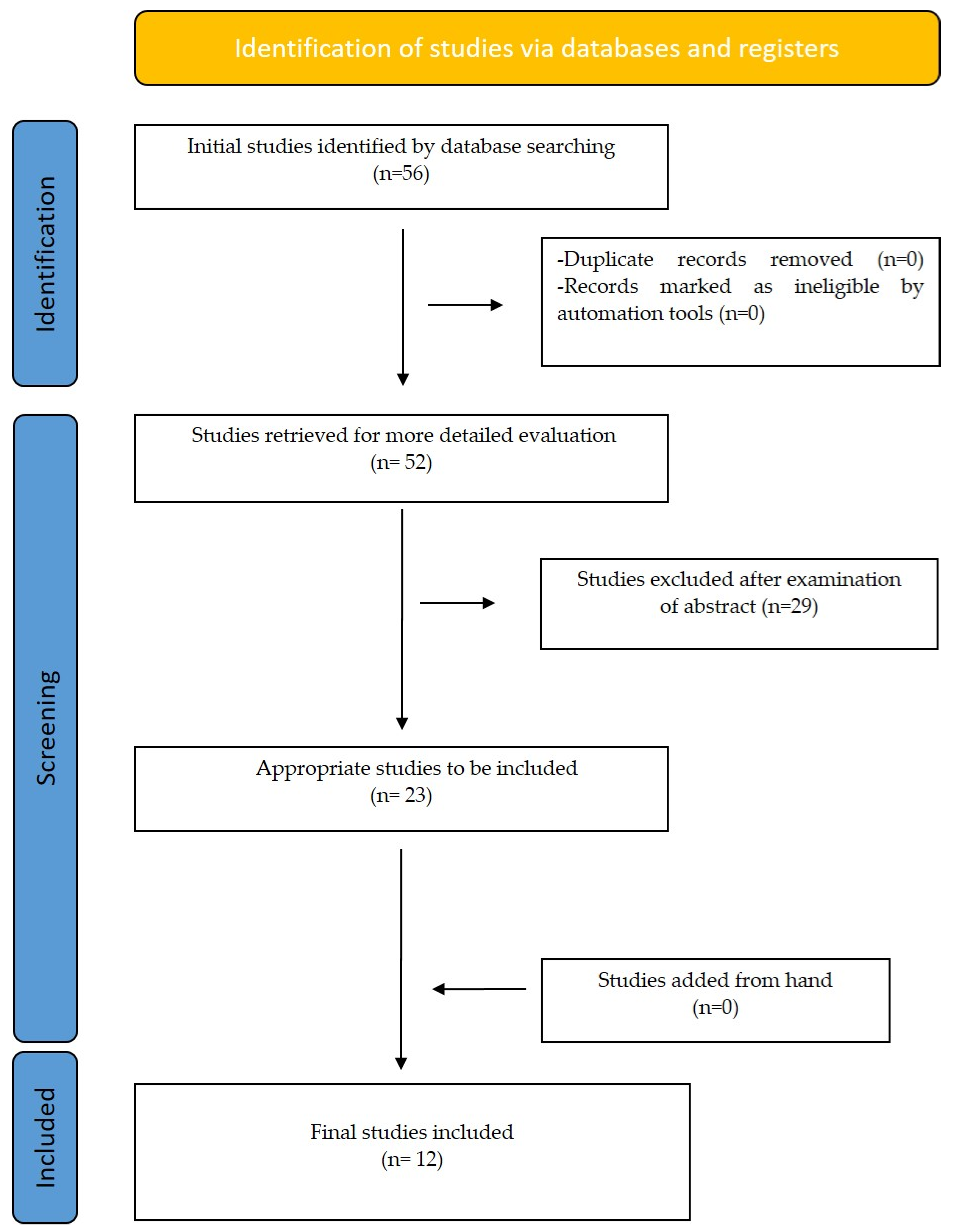
2. Materials and Methods
3. Results
4. Additive Manufacturing (3D Printing)
5. CAD Software
6. Designing and Printing Workflow
7. Band Design
8. Space Maintainer Appliances
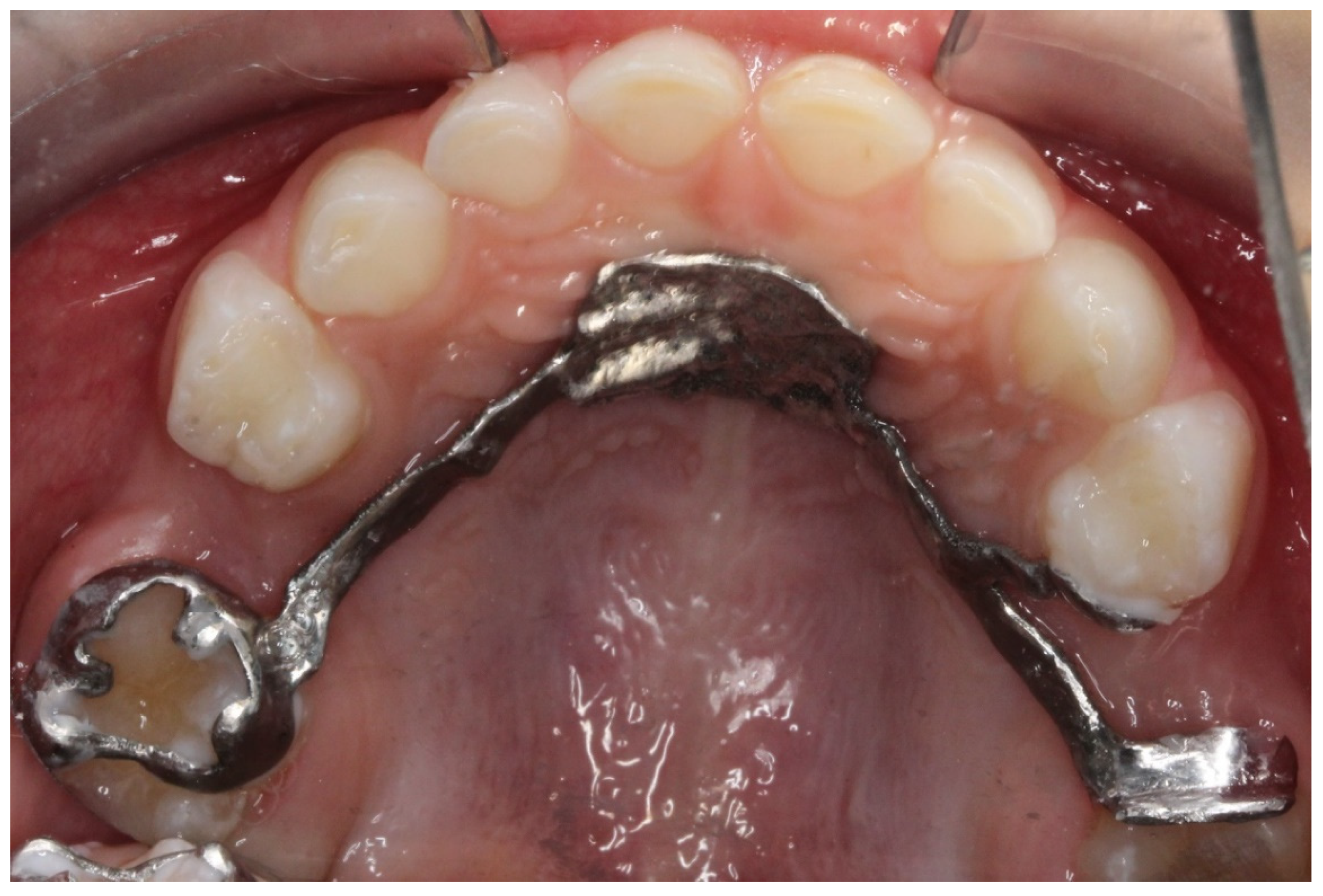
8.1. Lingual Arch Design
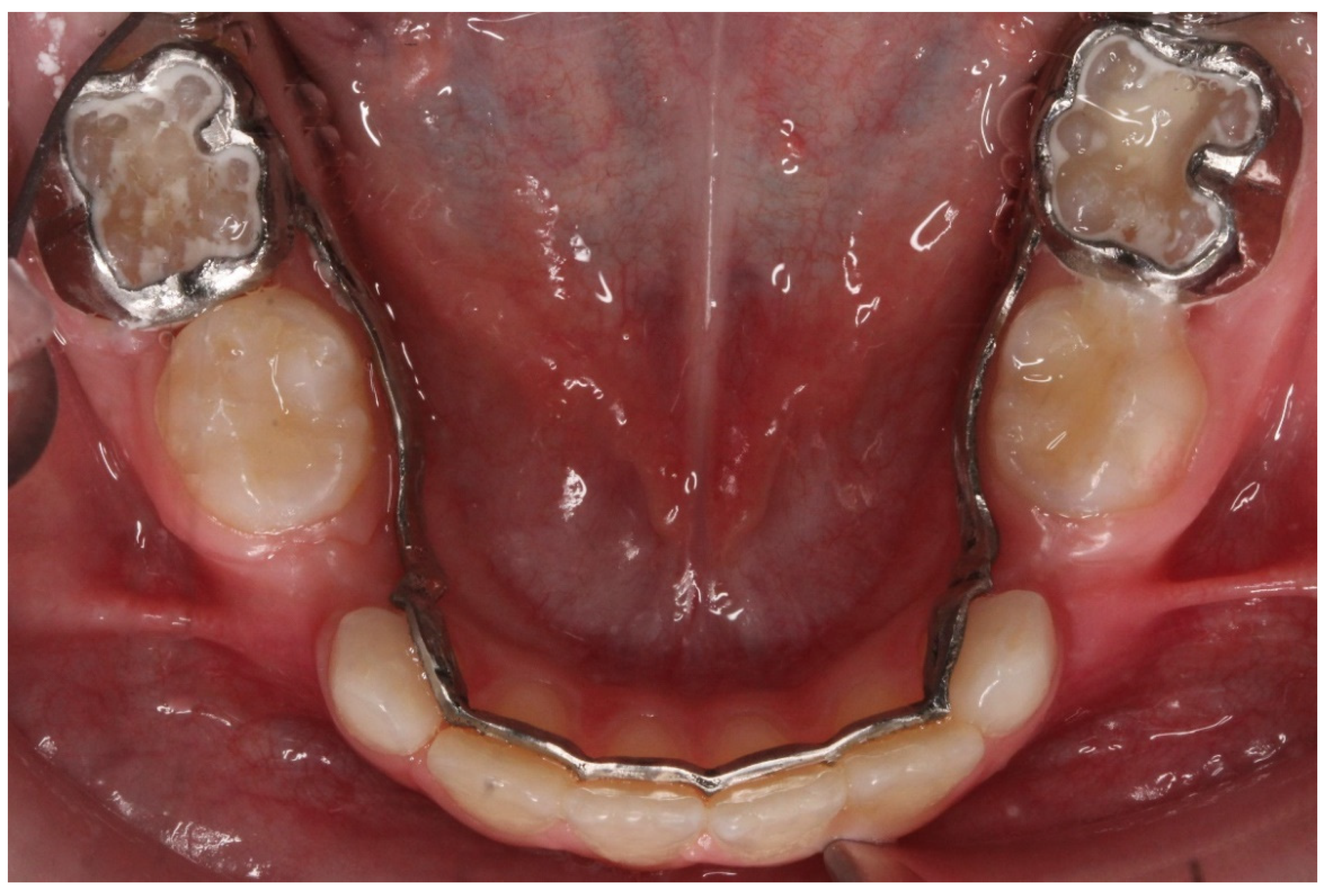
8.2. Band and Loop Appliance
8.3. Unerupted Molar Tooth Guiding Appliance
9. Rapid Palatal Expander (RPE)
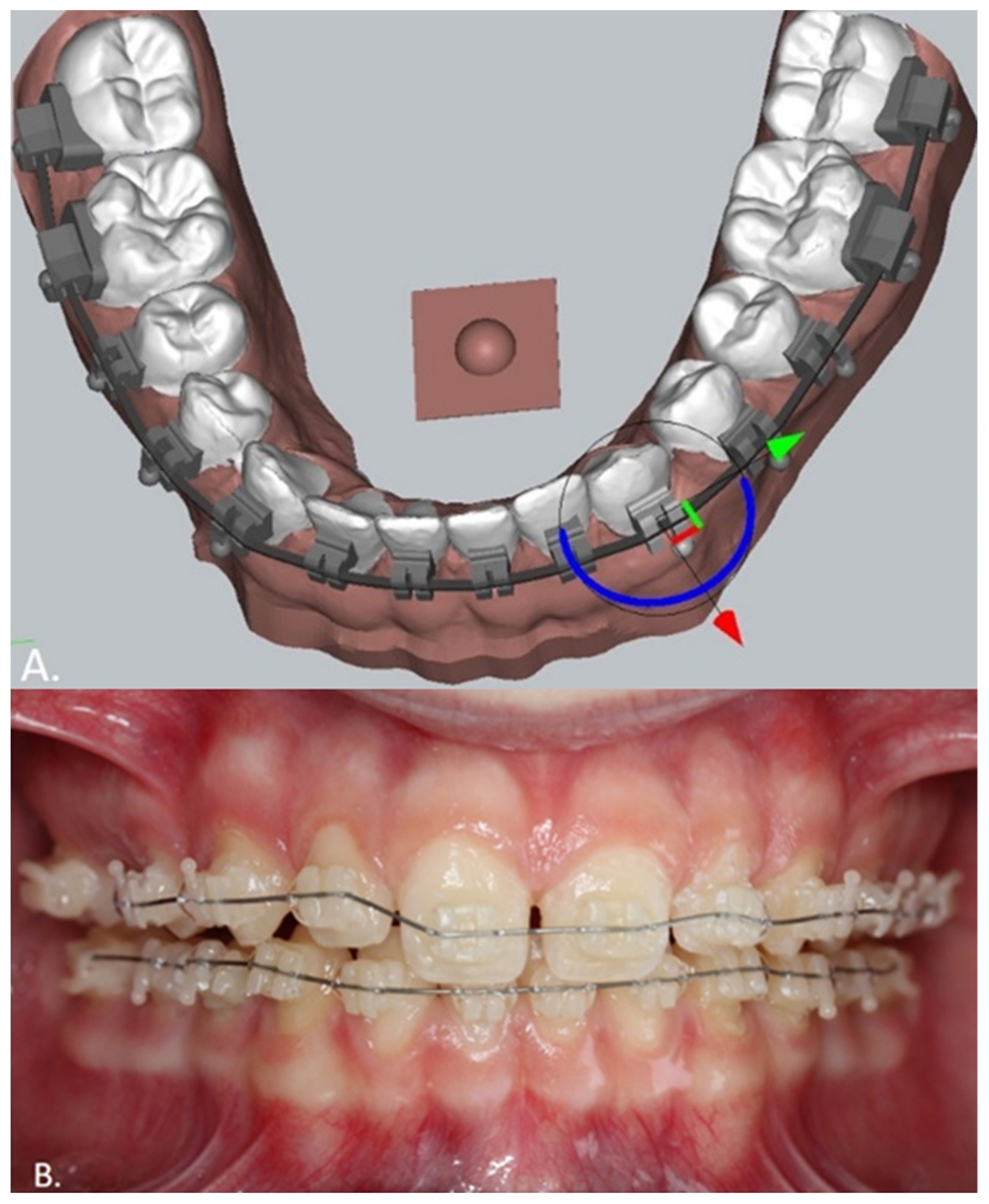
10. Customized Brackets
11. Clear Aligners
12. Discussion
13. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Panayi, N.C. DIY Orthodontics: Design it Yourself; Quintessence Publishing: Chicago, IL, USA, 2021. [Google Scholar]
- Jean-Marc, R.; Mohamed-Nur, A. 3D Diagnosis and Treatment Planning in Orthodontics: An Atlas for the Clinician; Springer: Berlin/Heidelberg, Germany, 2021. [Google Scholar]
- Shahrubudin, N.; Lee, T.; Ramlan, R. An Overview on 3D Printing Technology: Technological, Materials, and Applications. Procedia Manuf. 2019, 35, 1286–1296. [Google Scholar] [CrossRef]
- Kessler, A.; Hickel, R.; Reymus, M. 3D Printing in Dentistry-State of the Art. Oper. Dent. 2020, 45, 30–40. [Google Scholar] [CrossRef] [PubMed]
- Tian, Y.; Chen, C.; Xu, X.; Wang, J.; Hou, X.; Li, K.; Lu, X.; Shi, H.; Lee, E.S.; Jiang, H.B. A Review of 3D Printing in Dentistry: Technologies, Affecting Factors, and Applications. Scanning 2021, 2021, 9950131. [Google Scholar] [CrossRef] [PubMed]
- Khorsandi, D.; Fahimipour, A.; Abasian, P.; Saber, S.S.; Seyedi, M.; Ghanavati, S.; Ahmad, A.; De Stephanis, A.A.; Taghavinezhaddilami, F.; Leonova, A.; et al. 3D and 4D printing in dentistry and maxillofacial surgery: Printing techniques, materials, and applications. Acta Biomater. 2021, 122, 26–49. [Google Scholar] [CrossRef]
- Francisco, I.; Ribeiro, M.P.; Marques, F.; Travassos, R.; Nunes, C.; Pereira, F.; Caramelo, F.; Paula, A.B.; Vale, F. Application of Three-Dimensional Digital Technology in Orthodontics: The State of the Art. Biomimetics 2022, 7, 23. [Google Scholar] [CrossRef]
- Kravitz, N.D.; Groth, C.; Shannon, T. CAD/CAM software for three-dimensional printing. J. Clin. Orthod. 2018, 52, 22–27. [Google Scholar] [PubMed]
- Cozzani, M.; Antonini, S.; Lupini, D.; Decesari, D.; Anelli, F.; Doldo, T. A New Proposal: A Digital Flow for the Construction of a Haas-Inspired Rapid Maxillary Expander (HIRME). Materials 2020, 13, 2898. [Google Scholar] [CrossRef]
- Graf, S.; Cornelis, M.A.; Hauber Gameiro, G.; Cattaneo, P.M. Computer-aided design and manufacture of hyrax devices: Can we really go digital? Am. J. Orthod. Dentofac. Orthop. 2017, 152, 870–874. [Google Scholar] [CrossRef] [Green Version]
- Wolf, M.; Schumacher, P.; Jäger, F.; Wego, J.; Fritz, U.; Korbmacher-Steiner, H.; Jäger, A.; Schauseil, M. Novel Lingual Retainer Created Using CAD/CAM Technology: Evaluation of Its Positioning Accuracy. J. Orofac. Orthop. 2015, 76, 164–174. [Google Scholar] [CrossRef]
- Panayi, N.; Tsolakis, A. In-house computer-aided design and 3-dimensional printing of customized orthodontic brackets using hybrid ceramic resin: Is it the time for the orthodontist to take over? Am. J. Orthod. Dentofac. Orthop. 2021, 1, 187–193. [Google Scholar] [CrossRef]
- Jindal, P.; Juneja, M.; Siena, F.L.; Bajaj, D.; Breedon, P. Mechanical and geometric properties of thermoformed and 3D printed clear dental aligners. Am. J. Orthod. Dentofac. Orthop. 2019, 156, 694–701. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Koenig, N.; Choi, J.Y.; McCray, J.; Hayes, A.; Schneider, P.; Kim, K.B. Comparison of dimensional accuracy between direct-printed and thermoformed aligners. Korean J. Orthod. 2022, in press. [CrossRef]
- Lee, S.Y.; Kim, H.; Kim, H.J.; Chung, C.J.; Choi, Y.J.; Kim, S.J.; Cha, J.Y. Thermo-mechanical properties of 3D printed photocurable shape memory resin for clear aligners. Sci. Rep. 2022, 12, 6246. [Google Scholar] [CrossRef] [PubMed]
- Kodama, H. A scheme for three-dimensional display by automatic fabrication of three-dimensional model. IEICE Trans. Electron. 1981, 237–241. [Google Scholar]
- Kodama, H. Automatic method for fabricating a three-dimensional plastic model with photo-hardening polymer. Rev. Sci. Instrum. 1981, 52, 1770–1773. [Google Scholar] [CrossRef]
- Hull, C. On Stereolithography. Virtual Phys. Prototyp. 2012, 7, 177. [Google Scholar] [CrossRef]
- Dawood, A.; Marti Marti, B.; Sauret-Jackson, V.; Darwood, A. 3D printing in dentistry. Br. Dent. J. 2015, 219, 521–529. [Google Scholar] [CrossRef]
- Abo Sharkh, H.; Makhoul, N. In-House Surgeon-Led Virtual Surgical Planning for Maxillofacial Reconstruction. J. Oral. Maxillofac. Surg. 2020, 78, 651–660. [Google Scholar] [CrossRef]
- Schmidt, R.; Ratto, M. Design-to-fabricate: Maker hardware requires maker software. IEEE Comput. Graph. Appl. 2013, 33, 26–34. [Google Scholar] [CrossRef]
- Nasef, A.A.; El-Beialy, A.R.; Mostafa, Y.A. Virtual techniques for designing and fabricating a retainer. Am. J. Orthod. Dentofac. Orthop. 2014, 146, 394–398. [Google Scholar] [CrossRef]
- Keim, R.G. In-house aligners. J. Clin. Orthod. 2021, 55, 449. [Google Scholar] [PubMed]
- Revilla-León, M.; Meyer, M.J.; Zandinejad, A.; Özcan, M. Additive manufacturing technologies for processing zirconia in dental applications. Int. J. Comput. Dent. 2020, 23, 27–37. [Google Scholar] [PubMed]
- Wiechmann, D. Modulus-driven lingual orthodontics. Clin. Impr. 2001, 10, 2–7. [Google Scholar]
- Wiechmann, D.; Rummel, V.; Thalheim, A.; Simon, J.; Wiechmann, L. Customized brackets and archwires for lingual orthodontic treatment. Am. J. Orthod. Dentofac. Orthop. 2003, 124, 593–599. [Google Scholar] [CrossRef] [PubMed]
- Joffe, L. Invisalign: Early experiences. J. Orthod. 2003, 30, 348–352. [Google Scholar] [CrossRef]
- McKenna, S. Invisalign: Technology or mythology? J. Mass. Dent. Soc. 2001, 50, 8–9. [Google Scholar]
- Barbin, T.; Velôso, D.V.; Del Rio Silva, L.; Borges, G.A.; Presotto, A.G.C.; Barão, V.A.R.; Mesquita, M.F. 3D metal printing in dentistry: An in vitro biomechanical comparative study of two additive manufacturing technologies for full-arch implant-supported prostheses. J. Mech. Behav. Biomed. Mater. 2020, 108, 103821. [Google Scholar] [CrossRef]
- Alghazzawi, T.F. Advancements in CAD/CAM technology: Options for practical implementation. J. Prosthodont. Res. 2016, 60, 72–84. [Google Scholar] [CrossRef]
- Domagała, I.; Przystupa, K.; Firlej, M.; Pieniak, D.; Gil, L.; Borucka, A.; Naworol, I.; Biedziak, B.; Levkiv, M. Analysis of the Statistical Comparability of the Hardness and Wear of Polymeric Materials for Orthodontic Applications. Materials 2021, 14, 2925. [Google Scholar] [CrossRef]
- Brożek, R.; Pałka, K.; Koczorowski, R.; Dorocka-Bobkowska, B. Effect of artificial saliva on the mechanical properties of a polymer material reinforced with fiber, used in esthetic tooth restorations. Dent. Med. Probl. 2020, 57, 261–267. [Google Scholar] [CrossRef]
- Mangano, F.; Gandolfi, A.; Luongo, G.; Logozzo, S. Intraoral scanners in dentistry: A review of the current literature. BMC Oral. Health 2017, 17, 149. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aretxabaleta, M.; Unkovskiy, A.; Koos, B.; Spintzyk, S.; Xepapadeas, A.B. Accuracy Evaluation of Additively and Subtractively Fabricated Palatal Plate Orthodontic Appliances for Newborns and Infants-An In Vitro Study. Materials 2021, 14, 4103. [Google Scholar] [CrossRef] [PubMed]




| Materials | Characteristics | Use |
|---|---|---|
| Dental model resin | rigid, hard, high fracture toughness, temperature resistant | thermoforming procedure |
| Occlusal splint resin | transparent, medium fracture toughness | occlusal splints |
| IDB tray resin | transparent, soft | IDB tray |
| CoCr alloy | rigid, non-flexible, printed in SLS printers | metallic orthodontic appliances |
| Ti alloy | rigid, non-flexible, printed in SLS printers | metallic orthodontic appliances |
| Stainless steel alloy | rigid, non-flexible, printed in SLS printers | metallic orthodontic appliances |
| Permanent crown resin | low hardness, high fracture toughness | crowns, brackets (tested) |
| Zirconia slurry | high hardness, low fracture toughness, printed in zirconia printers | crowns, bridges, brackets, bands |
| Aligner resin | high elastic index, transparent, stable mechanical properties | printed aligners |
| Inclusion Criteria | Exclusion Criteria |
|---|---|
| Studies that refer to 3D-printed customized orthodontic and pedodontic appliances. | Studies that are Reviews or authors′ opinion |
| In vitro studies prospective or retrospective. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tsolakis, I.A.; Gizani, S.; Tsolakis, A.I.; Panayi, N. Three-Dimensional-Printed Customized Orthodontic and Pedodontic Appliances: A Critical Review of a New Era for Treatment. Children 2022, 9, 1107. https://doi.org/10.3390/children9081107
Tsolakis IA, Gizani S, Tsolakis AI, Panayi N. Three-Dimensional-Printed Customized Orthodontic and Pedodontic Appliances: A Critical Review of a New Era for Treatment. Children. 2022; 9(8):1107. https://doi.org/10.3390/children9081107
Chicago/Turabian StyleTsolakis, Ioannis A., Sotiria Gizani, Apostolos I. Tsolakis, and Nearchos Panayi. 2022. "Three-Dimensional-Printed Customized Orthodontic and Pedodontic Appliances: A Critical Review of a New Era for Treatment" Children 9, no. 8: 1107. https://doi.org/10.3390/children9081107
APA StyleTsolakis, I. A., Gizani, S., Tsolakis, A. I., & Panayi, N. (2022). Three-Dimensional-Printed Customized Orthodontic and Pedodontic Appliances: A Critical Review of a New Era for Treatment. Children, 9(8), 1107. https://doi.org/10.3390/children9081107








