Marine Algae: A Potential Resource of Anti-HSV Molecules
Abstract
:1. Introduction
2. Diseases, Symptoms, and Their Mode of Infection
3. Pathogenesis of HSV
4. Establishment of Primary Infection
5. Involvement of Virion Host Shutoff Protein in Causing Infection
6. Immune Evading Strategies of HSV
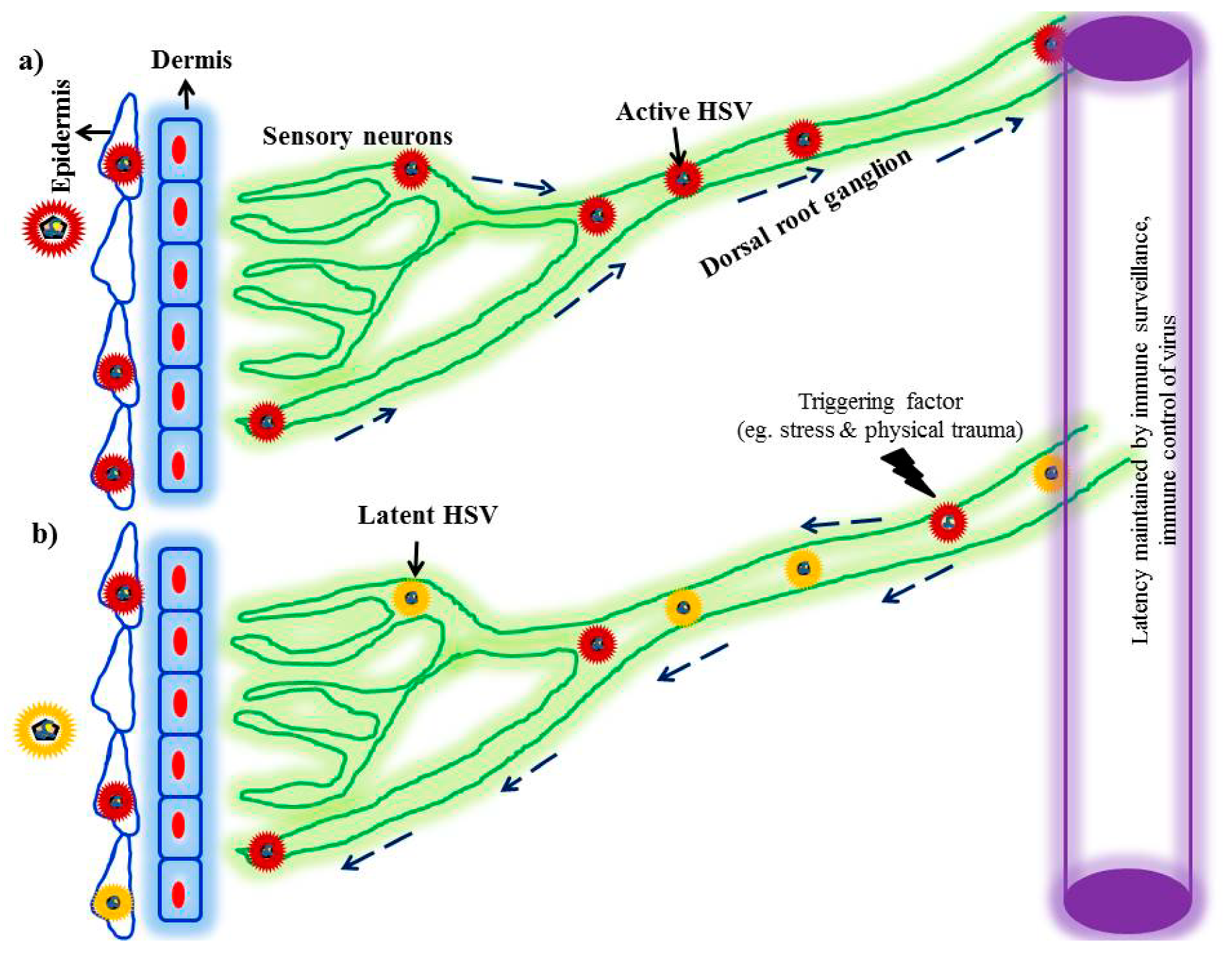
7. State of Viral Latency and Reactivation
8. Role of Keratin in Primary Recurrent Lesions
9. Anti-HSV Molecules from Marine Algae
9.1. Green Algae
9.2. Red Algae
9.3. Brown Algae
10. Concluding Remarks and Future Prospects
Author Contributions
Funding
Conflicts of Interest
References
- Kitazato, K.; Wang, Y.; Kobayashi, N. Viral infectious disease and natural products with antiviral activity. Drug Discov. Ther. 2007, 1, 14–22. [Google Scholar]
- Roback, J.D.; Su, L.; Zimring, J.C.; Hillyer, C.D. Transfusion-transmitted cytomegalovirus: Lessons from a murine model. Transfus. Med. Rev. 2007, 21, 26–36. [Google Scholar] [CrossRef]
- Luecke, S.; Paludan, S.R. Innate recognition of alphaherpesvirus DNA. Adv. Virus Res. 2015, 92, 63–100. [Google Scholar] [CrossRef]
- Sehrawat, S.; Kumar, D.; Rouse, B.T. Herpesviruses: Harmonious Pathogens but Relevant Cofactors in Other Diseases? Front. Cell Infect. Microbiol. 2018, 8, 177. [Google Scholar] [CrossRef]
- Vadlapudi, A.; Vadlapatla, R.; Mitra, A. Update on emerging antivirals for the management of herpes simplex virus infections: A patenting perspective. Recent Pat. Anti-Infect. Drug Discov. 2013, 8, 55–67. [Google Scholar]
- Whitley, R.J.; Roizman, B. Herpes simplex virus infections. Lancet 2001, 357, 1513–1518. [Google Scholar] [CrossRef]
- Esmann, J. The many challenges of facial herpes simplex virus infection. J. Antimicrob. Chemother. 2001, 47, 17–27. [Google Scholar] [CrossRef]
- WHO. Herpes Simplex Virus. Available online: https://www.who.int/news-room/fact-sheets/detail/herpes-simplex-virus (accessed on 24 June 2019).
- Chattopadhyay, D.; Mukhopadhyay, A.; Ojha, D.; Sadhukhan, P.; Dutta, S. Immuno-metabolic changes in herpes virus infection. Cytokine 2018, 112, 52–62. [Google Scholar] [CrossRef] [PubMed]
- Cardozo, F.; Larsen, I.; Carballo, E.; Jose, G.; Stern, R.; Brummel, R.; Camelini, C.; Rossi, M.; Simões, C.; Brandt, C. In vivo anti-HSV activity of a sulfated derivative of Agaricus brasiliensis mycelial polysaccharide. Antimicrob. Agents Chemother. 2013, 57, 2541–2549. [Google Scholar] [CrossRef] [PubMed]
- Wilhelmus, K.R. Antiviral treatment and other therapeutic interventions for herpes simplex virus epithelial keratitis. Cochrane Database Syst. Rev. 2015, 1, CD002898. [Google Scholar] [CrossRef] [PubMed]
- Gupta, R.; Warren, T.; Wald, A. Genital herpes. Lancet 2007, 370, 2127–2137. [Google Scholar] [CrossRef]
- Mettenleiter, T.C.; Klupp, B.G.; Granzow, H. Herpesvirus assembly: A tale of two membranes. Curr. Opin. Microbiol. 2006, 9, 423–429. [Google Scholar] [CrossRef] [PubMed]
- Ren, X.; Xue, C.; Kong, Q.; Zhang, C.; Bi, Y.; Cao, Y. Proteomic analysis of purified Newcastle disease virus particles. Proteome Sci. 2012, 10, 32. [Google Scholar] [CrossRef] [PubMed]
- Whitley, R.; Kimberlin, D.W.; Cg, P. Pathogenesis and Disease. In Human Herpesviruses: Biology, Therapy, and Immunoprophylaxis; Arvin, A.C.-F.G., Mocarski, E., Eds.; Cambridge University Press: Cambridge, UK, 2007. [Google Scholar]
- Koelle, D.M.; Corey, L. Herpes simplex: Insights on pathogenesis and possible vaccines. Annu. Rev. Med. 2008, 59, 381–395. [Google Scholar] [CrossRef] [PubMed]
- Kumar, S.P.; Chandy, M.L.; Shanavas, M.; Khan, S.; Suresh, K.V. Pathogenesis and life cycle of herpes simplex virus infection-stages of primary, latency and recurrence. J. Oral Maxillofac. Surg. Med. Pathol. 2016, 28, 350–353. [Google Scholar] [CrossRef]
- George, A.K.; Anil, S. Acute herpetic gingivostomatitis associated with herpes simplex virus 2: Report of a case. J. Int. Oral Health: Jioh 2014, 6, 99. [Google Scholar]
- Rosain, J.; Froissart, A.; Estrangin, E.; Rozenberg, F. Severe acute pharyngotonsillitis due to herpes simplex virus type 2 in a young woman. J. Clin. Virol. 2015, 63, 63–65. [Google Scholar] [CrossRef]
- Spruance, S.L.; Overall, J.C., Jr.; Kern, E.R.; Krueger, G.G.; Pliam, V.; Miller, W. The natural history of recurrent herpes simplex labialis: Implications for antiviral therapy. N. Engl. J. Med. 1977, 297, 69–75. [Google Scholar] [CrossRef]
- Kopriva, F. Recurrent herpetic whitlow in an immune competent girl without vesicular lesions. Eur. J. Pediatrics 2002, 161, 120–121. [Google Scholar] [CrossRef]
- Wei, E.Y.; Coghlin, D.T. Beyond Folliculitis: Recognizing rerpes gladiatorum in adolescent athletes. J. Pediatrics 2017, 190, 283. [Google Scholar] [CrossRef]
- Harindra, V.; Paffett, M.C. Recurrent eczema herpeticum: An underrecognised condition. Sex. Transm. Infect. 2001, 77, 76. [Google Scholar] [CrossRef]
- Friedman, H.M. Keratin, a dual role in herpes simplex virus pathogenesis. J. Clin. Virol. 2006, 35, 103–105. [Google Scholar] [CrossRef] [PubMed]
- Raborn, G.W.; Grace, M.G. Recurrent herpes simplex labialis: Selected therapeutic options. J. Can. Dent. Assoc. 2003, 69, 498–504. [Google Scholar] [PubMed]
- Cabrera, J.R.; Borbolla, A. Herpes simplex virus and neurotrophic factors. J. Hum. Virol. Retrovirol. 2015, 2, 00027. [Google Scholar]
- Freeman, E.E.; Weiss, H.A.; Glynn, J.R.; Cross, P.L.; Whitworth, J.A.; Hayes, R.J. Herpes simplex virus 2 infection increases HIV acquisition in men and women: Systematic review and meta-analysis of longitudinal studies. AIDS 2006, 20, 73–83. [Google Scholar] [CrossRef]
- James, S.; Whitley, R. Treatment of herpes simplex virus infections in pediatric patients: Current status and future needs. Clin. Pharm. Ther. 2010, 88, 720–724. [Google Scholar] [CrossRef]
- Moraru, M.; Cisneros, E.; Gómez-Lozano, N.; de Pablo, R.; Portero, F.; Cañizares, M.; Vaquero, M.; Roustán, G.; Millán, I.; López-Botet, M. Host genetic factors in susceptibility to herpes simplex type 1 virus infection: Contribution of polymorphic genes at the interface of innate and adaptive immunity. J. Immunol. 2012, 188, 1103434. [Google Scholar] [CrossRef]
- Gallina, G.; Cumbo, V.; Messina, P.; Modica, M.; Caruso, C. MHC-linked genetic factors (HLA-B35) influencing recurrent circumoral herpetic lesions. Dis. Markers 1987, 5, 191–197. [Google Scholar]
- Pasieka, T.J.; Lu, B.; Crosby, S.D.; Wylie, K.M.; Morrison, L.A.; Alexander, D.E.; Menachery, V.D.; Leib, D.A. Herpes simplex virus virion host shutoff attenuates establishment of the antiviral state. J. Virol. 2008, 82, 5527–5535. [Google Scholar] [CrossRef]
- Fakioglu, E.; Wilson, S.S.; Mesquita, P.M.; Hazrati, E.; Cheshenko, N.; Blaho, J.A.; Herold, B.C. Herpes simplex virus downregulates secretory leukocyte protease inhibitor: A novel immune evasion mechanism. J. Virol. 2008, 82, 9337–9344. [Google Scholar] [CrossRef]
- Oroskar, A.A.; Read, G.S. Control of mRNA stability by the virion host shutoff function of herpes simplex virus. J. Virol. 1989, 63, 1897–1906. [Google Scholar]
- Kwong, A.D.; Frenkel, N. Herpes simplex virus-infected cells contain a function (s) that destabilizes both host and viral mRNAs. Proc. Natl. Acad. Sci. USA 1987, 84, 1926–1930. [Google Scholar] [CrossRef] [PubMed]
- Kalamvoki, M.; Qu, J.; Roizman, B. Translocation and colocalization of ICP4 and ICP0 in cells infected with herpes simplex virus 1 mutants lacking glycoprotein E, glycoprotein I, or the virion host shutoff product of the UL41 gene. J. Virol. 2008, 82, 1701–1713. [Google Scholar] [CrossRef] [PubMed]
- Duerst, R.J.; Morrison, L.A. Herpes simplex virus 2 virion host shutoff protein interferes with type I interferon production and responsiveness. Virology 2004, 322, 158–167. [Google Scholar] [CrossRef]
- Suzutani, T.; Nagamine, M.; Shibaki, T.; Ogasawara, M.; Yoshida, I.; Daikoku, T.; Nishiyama, Y.; Azuma, M. The role of the UL41 gene of herpes simplex virus type 1 in evasion of non-specific host defence mechanisms during primary infection. J. Gen. Virol. 2000, 81, 1763–1771. [Google Scholar] [CrossRef] [PubMed]
- Murphy, J.A.; Duerst, R.J.; Smith, T.J.; Morrison, L.A. Herpes simplex virus type 2 virion host shutoff protein regulates alpha/beta interferon but not adaptive immune responses during primary infection in vivo. J. Virol. 2003, 77, 9337–9345. [Google Scholar] [CrossRef] [PubMed]
- Rolinski, J.; Hus, I. Immunological aspects of acute and recurrent herpes simplex keratitis. J. Immunol. Res. 2014, 2014, 513560. [Google Scholar] [CrossRef]
- Hook, L.M.; Lubinski, J.M.; Jiang, M.; Pangburn, M.K.; Friedman, H.M. Herpes simplex virus type 1 and 2 glycoprotein C prevents complement-mediated neutralization induced by natural immunoglobulin M antibody. J. Virol. 2006, 80, 4038–4046. [Google Scholar] [CrossRef] [Green Version]
- Morrison, L.A.; Knipe, D.M. Immunization with replication-defective mutants of herpes simplex virus type 1: Sites of immune intervention in pathogenesis of challenge virus infection. J. Virol. 1994, 68, 689–696. [Google Scholar]
- Riley, L.E. Herpes Simplex Virus. Semin. Perinatol. 1998, 22, 284–292. [Google Scholar]
- Leib, D. Counteraction of Interferon-Induced Antiviral Responses by Herpes Simplex Viruses. In Viral Proteins Counteracting Host Defenses; Springer: Berlin, Germany, 2002; pp. 171–185. [Google Scholar]
- Arduino, P.G.; Porter, S.R. Herpes Simplex Virus Type 1 infection: Overview on relevant clinico-pathological features. J. Oral Pathol. Med. 2008, 37, 107–121. [Google Scholar] [CrossRef]
- Grinde, B. Herpesviruses: Latency and reactivation–viral strategies and host response. J. Oral Microbiol. 2013, 5, 22766. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thellman, N.M.; Triezenberg, S.J. Herpes simplex virus establishment, maintenance, and reactivation: In vitro modeling of latency. Pathogens 2017, 6, 28. [Google Scholar] [CrossRef] [PubMed]
- Blyth, W.; Hill, T. Establishment, maintenance, and control of herpes simplex virus (HSV) latency. In Immunobiology of Herpes Simplex Virus Infection; CRC Press: Boca Raton, FL, USA, 1984; pp. 9–32. [Google Scholar]
- Nicola, A.V.; Hou, J.; Major, E.O.; Straus, S.E. Herpes simplex virus type 1 enters human epidermal keratinocytes, but not neurons, via a pH-dependent endocytic pathway. J. Virol. 2005, 79, 7609–7616. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rajendran, R. Shafer’s Textbook of Oral Pathology; Elsevier: Amsterdam, The Netherlands, 2009. [Google Scholar]
- Nikkels, A.F.; Pièrard, G.E. Treatment of mucocutaneous presentations of herpes simplex virus infections. Am. J. Clin. Dermatol. 2002, 3, 475–487. [Google Scholar] [CrossRef] [PubMed]
- Spruance, S. Pathogenesis of herpes simplex labialis: Excretion of virus in the oral cavity. J. Clin. Microbiol. 1984, 19, 675–679. [Google Scholar]
- El Gamal, A.A. Biological importance of marine algae. Saudi Pharm. J. 2010, 18, 1–25. [Google Scholar] [CrossRef] [Green Version]
- Lordan, S.; Ross, R.P.; Stanton, C. Marine bioactives as functional food ingredients: Potential to reduce the incidence of chronic diseases. Mar. Drugs 2011, 9, 1056–1100. [Google Scholar] [CrossRef] [Green Version]
- Belghit, I.; Rasinger, J.D.; Heesch, S.; Biancarosa, I.; Liland, N.; Torstensen, B.; Waagbø, R.; Lock, E.-J.; Bruckner, C.G. In-depth metabolic profiling of marine macroalgae confirms strong biochemical differences between brown, red and green algae. Algal Res. 2017, 26, 240–249. [Google Scholar] [CrossRef]
- Yasuhara-Bell, J.; Lu, Y. Marine compounds and their antiviral activities. Antivir. Res. 2010, 86, 231–240. [Google Scholar] [CrossRef]
- Ahmadi, A.; Zorofchian Moghadamtousi, S.; Abubakar, S.; Zandi, K. Antiviral Potential of Algae Polysaccharides Isolated from Marine Sources: A Review. Biomed. Res. Int. 2015, 2015, 825203. [Google Scholar] [CrossRef] [Green Version]
- Zhao, C.; Yang, C.; Liu, B.; Lin, L.; Sarker, S.D.; Nahar, L.; Yu, H.; Cao, H.; Xiao, J. Bioactive compounds from marine macroalgae and their hypoglycemic benefits. Trends Food Sci. Technol. 2018, 72, 1–12. [Google Scholar] [CrossRef]
- Gerber, P.; Dutcher, J.D.; Adams, E.V.; Sherman, J.H. Protective effect of seaweed extracts for chicken embryos infected with influenza B or mumps virus. Proc. Soc. Exp. Biol. Med. 1958, 99, 590–593. [Google Scholar] [CrossRef] [PubMed]
- Talarico, L.B.; Zibetti, R.G.; Faria, P.C.; Scolaro, L.A.; Duarte, M.E.; Noseda, M.D.; Pujol, C.A.; Damonte, E.B. Anti-herpes simplex virus activity of sulfated galactans from the red seaweeds Gymnogongrus griffithsiae and Cryptonemia crenulata. Int. J. Biol. Macromol. 2004, 34, 63–71. [Google Scholar] [CrossRef] [PubMed]
- Ghosh, T.; Chattopadhyay, K.; Marschall, M.; Karmakar, P.; Mandal, P.; Ray, B. Focus on antivirally active sulfated polysaccharides: From structure–activity analysis to clinical evaluation. Glycobiology 2008, 19, 2–15. [Google Scholar] [CrossRef] [PubMed]
- Vaheri, A. Heparin and related polyonic substances as virus inhibitors. Acta Pathol. Microbiol. Scand. 1964, 171, 1–98. [Google Scholar]
- Witvrouw, M.; De Clercq, E. Sulfated polysaccharides extracted from sea algae as potential antiviral drugs. Gen. Pharm. Vasc. Syst. 1997, 29, 497–511. [Google Scholar] [CrossRef]
- Cohen, J. Microbicide Fails to Protect against HIV; American Association for the Advancement of Science: Washington, DC, USA, 2008. [Google Scholar]
- Ehresmann, D.; Deig, E.; Hatch, M. Antiviral properties of algal polysaccharides and related compounds. Mar. Algae Pharm. Sci. 1979, 11, 293–302. [Google Scholar]
- Hatch, M.; Ehresmann, D.; Deig, E.; Vedros, N. Further-studies on chemical compoisition and an initial in vivo evaluation of antiviral material in extracts of macroscopic marine-algae. J. Phycol. 1977, 13, 28. [Google Scholar]
- Lee, J.-B.; Koizumi, S.; Hayashi, K.; Hayashi, T. Structure of rhamnan sulfate from the green alga Monostroma nitidum and its anti-herpetic effect. Carbohydr. Polym. 2010, 81, 572–577. [Google Scholar] [CrossRef]
- Hayashi, T.; Hayashi, K.; Maeda, M.; Kojima, I. Calcium spirulan, an inhibitor of enveloped virus replication, from a blue-green alga Spirulina platensis. J. Nat. Prod. 1996, 59, 83–87. [Google Scholar] [CrossRef]
- Lee, J.-B.; Hayashi, K.; Hayashi, T.; Sankawa, U.; Maeda, M. Antiviral activities against HSV-1, HCMV, and HIV-1 of rhamnan sulfate from Monostroma latissimum. Planta Med. 1999, 65, 439–441. [Google Scholar] [CrossRef] [PubMed]
- Leiro, J.M.; Castro, R.; Arranz, J.A.; Lamas, J. Immunomodulating activities of acidic sulphated polysaccharides obtained from the seaweed Ulva rigida C. Agardh. Int. Immunopharmacol. 2007, 7, 879–888. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, T.; Suzuki, H.; Wada, Y.; Kodama, T.; Doi, T. Fucoidan induces nitric oxide production via p38 mitogen-activated protein kinase and NF-κB-dependent signaling pathways through macrophage scavenger receptors. Biochem. Biophys. Res. Commun. 2006, 343, 286–294. [Google Scholar] [CrossRef] [PubMed]
- Mandal, P.; Pujol, C.A.; Carlucci, M.J.; Chattopadhyay, K.; Damonte, E.B.; Ray, B. Anti-herpetic activity of a sulfated xylomannan from Scinaia hatei. Phytochemistry 2008, 69, 2193–2199. [Google Scholar] [CrossRef]
- Ray, S.; Pujol, C.A.; Damonte, E.B.; Ray, B. Additionally sulfated xylomannan sulfates from Scinaia hatei and their antiviral activities. Carbohydr. Polym. 2015, 131, 315–321. [Google Scholar] [CrossRef]
- Lopes, N.; Ray, S.; Espada, S.F.; Bomfim, W.A.; Ray, B.; Faccin-Galhardi, L.C.; Linhares, R.E.C.; Nozawa, C. Green seaweed Enteromorpha compressa (Chlorophyta, Ulvaceae) derived sulphated polysaccharides inhibit herpes simplex virus. Int. J. Biol. Macromol. 2017, 102, 605–612. [Google Scholar] [CrossRef]
- Wang, H.; Li, Y.-L.; Shen, W.-Z.; Rui, W.; Ma, X.-J.; Cen, Y.-Z. Antiviral activity of a sulfoquinovosyldiacylglycerol (SQDG) compound isolated from the green alga Caulerpa racemosa. Bot. Mar. 2007, 50, 185–190. [Google Scholar] [CrossRef]
- Carlucci, M.J.; Pujol, C.A.; Ciancia, M.; Noseda, M.D.; Matulewicz, M.C.; Damonte, E.B.; Cerezo, A.S. Antiherpetic and anticoagulant properties of carrageenans from the red seaweed Gigartina skottsbergii and their cyclized derivatives: Correlation between structure and biological activity. Int. J. Biol. Macromol. 1997, 20, 97–105. [Google Scholar] [CrossRef]
- Rodríguez, M.C.; Merino, E.R.; Pujol, C.A.; Damonte, E.B.; Cerezo, A.S.; Matulewicz, M.C. Galactans from cystocarpic plants of the red seaweed Callophyllis variegata (Kallymeniaceae, Gigartinales). Carbohydr. Res. 2005, 340, 2742–2751. [Google Scholar] [CrossRef]
- Kulshreshtha, G.; Burlot, A.S.; Marty, C.; Critchley, A.; Hafting, J.; Bedoux, G.; Bourgougnon, N.; Prithiviraj, B. Enzyme-assisted extraction of bioactive material from Chondrus crispus and Codium fragile and its effect on herpes simplex virus (HSV-1). Mar. Drugs 2015, 13, 558–580. [Google Scholar] [CrossRef] [Green Version]
- Serkedjieva, J. Antiherpes virus effect of the red marine alga Polysiphonia denudata. Z. Nat. C 2000, 55, 830–835. [Google Scholar] [CrossRef] [PubMed]
- Zandi, K.; Salimi, M.; Sartavi, K. In vitro antiviral activity of the red marine alga from Persian gulf, Gracilaria salicornia against herpes simplex virus type 2. J. Biol. Sci. 2007, 7, 1274–1277. [Google Scholar]
- Rhimou, B.; Hassane, R.; Nathalie, B. Antiviral activity of the extracts of Rhodophyceae from Morocco. Afr. J. Biotechnol. 2010, 9, 7968–7975. [Google Scholar]
- Gonzalez, M.; Alarcón, B.; Carrasco, L. Polysaccharides as antiviral agents: Antiviral activity of carrageenan. Antimicrob. Agents Chemother. 1987, 31, 1388–1393. [Google Scholar] [CrossRef] [Green Version]
- Nakashima, H.; Kido, Y.; Kobayashi, N.; Motoki, Y.; Neushul, M.; Yamamoto, N. Purification and characterization of an avian myeloblastosis and human immunodeficiency virus reverse transcriptase inhibitor, sulfated polysaccharides extracted from sea algae. Antimicrob. Agents Chemother. 1987, 31, 1524–1528. [Google Scholar] [CrossRef] [Green Version]
- Neushul, M. Antiviral carbohydrates from marine red algae. In Thirteenth International Seaweed Symposium; Springer: Berlin, Germany, 1990; pp. 99–104. [Google Scholar]
- Witvrouw, M.; Desmyter, J.; De Clercq, E. Antiviral Portrait Series: 4. Polysuifates as inhibitors of HIV and other enveloped viruses. Antivir. Chem. Chemother. 1994, 5, 345–359. [Google Scholar] [CrossRef]
- Huheihel, M.; Ishanu, V.; Tal, J.; Arad, S.M. Activity of Porphyridium sp. polysaccharide against herpes simplex viruses in vitro and in vivo. J. Biochem. Biophys. Methods 2002, 50, 189–200. [Google Scholar] [CrossRef]
- Geresh, S.; Arad, S. The extracellular polysaccharides of the red microalgae: Chemistry and rheology. Bioresour. Technol. 1991, 38, 195–201. [Google Scholar] [CrossRef]
- Baba, M.; Schols, D.; De Clercq, E.; Pauwels, R.; Nagy, M.; Györgyi-Edelényi, J.; Löw, M.; Görög, S. Novel sulfated polymers as highly potent and selective inhibitors of human immunodeficiency virus replication and giant cell formation. Antimicrob. Agents Chemother. 1990, 34, 134–138. [Google Scholar] [CrossRef] [Green Version]
- De Clercq, E.; Herdewijn, P. Strategies in the design of antiviral drugs. Pharm. Sci. Encycl. Drug Discov. Dev. Manuf. 2010. [Google Scholar] [CrossRef]
- Mandal, P.; Pujol, C.A.; Damonte, E.B.; Ghosh, T.; Ray, B. Xylans from Scinaia hatei: Structural features, sulfation and anti-HSV activity. Int. J. Biol. Macromol. 2010, 46, 173–178. [Google Scholar] [CrossRef] [PubMed]
- Malagoli, B.G.; Cardozo, F.T.; Gomes, J.H.S.; Ferraz, V.P.; Simões, C.M.; Braga, F.C. Chemical characterization and antiherpes activity of sulfated polysaccharides from Lithothamnion muelleri. Int. J. Biol. Macromol. 2014, 66, 332–337. [Google Scholar] [CrossRef] [PubMed]
- de SF-Tischer, P.C.; Talarico, L.B.; Noseda, M.D.; Guimarães, S.M.P.B.; Damonte, E.B.; Duarte, M.E.R. Chemical structure and antiviral activity of carrageenans from Meristiella gelidium against herpes simplex and dengue virus. Carbohydr. Polym. 2006, 63, 459–465. [Google Scholar] [CrossRef]
- Boulho, R.; Marty, C.; Freile-Pelegrín, Y.; Robledo, D.; Bourgougnon, N.; Bedoux, G. Antiherpetic (HSV-1) activity of carrageenans from the red seaweed Solieria chordalis (Rhodophyta, Gigartinales) extracted by microwave-assisted extraction (MAE). J. Appl. Phycol. 2017, 29, 2219–2228. [Google Scholar] [CrossRef]
- Lusvarghi, S.; Bewley, C.A. Griffithsin: An antiviral lectin with outstanding therapeutic potential. Viruses 2016, 8, 296. [Google Scholar] [CrossRef]
- Levendosky, K.; Mizenina, O.; Martinelli, E.; Jean-Pierre, N.; Kizima, L.; Rodriguez, A.; Kleinbeck, K.; Bonnaire, T.; Robbiani, M.; Zydowsky, T.M. Griffithsin and carrageenan combination to target HSV-2 and HPV. Antimicrob. Agents Chemother. 2015. [Google Scholar] [CrossRef] [Green Version]
- Nixon, B.; Stefanidou, M.; Mesquita, P.M.; Fakioglu, E.; Segarra, T.; Rohan, L.; Halford, W.; Palmer, K.E.; Herold, B.C. Griffithsin protects mice from genital herpes by preventing cell-to-cell spread. J. Virol. 2013, 87, 6257–6269. [Google Scholar] [CrossRef] [Green Version]
- Siamopoulou, P.; Bimplakis, A.; Iliopoulou, D.; Vagias, C.; Cos, P.; Berghe, D.V.; Roussis, V. Diterpenes from the brown algae Dictyota dichotoma and Dictyota linearis. Phytochemistry 2004, 65, 2025–2030. [Google Scholar] [CrossRef]
- Vallim, M.A.; Barbosa, J.E.; Negratilde, D.; De-Paula, J.C.; Galvatilde, V.A.G.; Teixeira, V.L.; de Palmer Paixatilde, I.C.N. In vitro antiviral activity of diterpenes isolated from the Brazilian brown alga Canistrocarpus cervicornis. J. Med. Plants Res. 2010, 4, 2379–2382. [Google Scholar]
- de Araujo, J.M.; Tappin, M.R.R.; da Rocha Fortes, R.; Lopes-Filho, E.A.P.; Salgueiro, F.; De Paula, J.C. Chemodiversity of the brown algae Canistrocarpus cervicornis (Dictyotaceae, Phaeophyceae) in tropical and subtropical populations along the southwestern Atlantic coast of Brazil. J. Appl. Phycol. 2018, 30, 611–618. [Google Scholar] [CrossRef]
- Mashjoor, S.; Yousefzadi, M.; Esmaeili, M.A.; Rafiee, R. Cytotoxicity and antimicrobial activity of marine macro algae (Dictyotaceae and Ulvaceae) from the Persian Gulf. Cytotechnology 2016, 68, 1717–1726. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pardo-Vargas, A.; de Barcelos Oliveira, I.; Stephens, P.R.S.; Cirne-Santos, C.C.; de Palmer Paixão, I.C.N.; Ramos, F.A.; Jiménez, C.; Rodríguez, J.; Resende, J.A.L.C.; Teixeira, V.L. Dolabelladienols A–C, new diterpenes isolated from Brazilian brown alga Dictyota pfaffii. Mar. Drugs 2014, 12, 4247–4259. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Garrido, V.; Barros, C.; Melchiades, V.A.; Fonseca, R.R.; Pinheiro, S.; Ocampo, P.; Teixeira, V.L.; Cavalcanti, D.N.; Giongo, V.; Ratcliffe, N.A. Subchronic toxicity and anti-HSV-1 activity in experimental animal of dolabelladienetriol from the seaweed, Dictyota pfaffii. Regul. Toxicol. Pharm. 2017, 86, 193–198. [Google Scholar] [CrossRef] [PubMed]
- Berteau, O.; Mulloy, B. Sulfated fucans, fresh perspectives: Structures, functions, and biological properties of sulfated fucans and an overview of enzymes active toward this class of polysaccharide. Glycobiology 2003, 13, 29–40. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hayashi, K.; Nakano, T.; Hashimoto, M.; Kanekiyo, K.; Hayashi, T. Defensive effects of a fucoidan from brown alga Undaria pinnatifida against herpes simplex virus infection. Int. Immunopharmacol. 2008, 8, 109–116. [Google Scholar] [CrossRef]
- Hoshino, T.; Hayashi, T.; Hayashi, K.; Hamada, J.; Lee, J.-B.; Sankawa, U. An antivirally active sulfated polysaccharide from Sargassum horneri (TURNER) C. AGARDH. Biol. Pharm. Bull. 1998, 21, 730–734. [Google Scholar] [CrossRef] [Green Version]
- Cuong, H.D.; Thuy, T.T.T.; Huong, T.T.; Ly, B.M.; Van, T.T.T. Structure and hypolipidaemic activity of fucoidan extracted from brown seaweed Sargassum henslowianum. Nat. Prod. Res. 2015, 29, 411–415. [Google Scholar] [CrossRef]
- Ponce, N.M.; Pujol, C.A.; Damonte, E.B.; Flores, M.A.L.; Stortz, C.A. Fucoidans from the brown seaweed Adenocystis utricularis: Extraction methods, antiviral activity and structural studies. Carbohydr. Res. 2003, 338, 153–165. [Google Scholar] [CrossRef]
- Preeprame, S.; Hayashi, K.; Lee, J.-B.; Sankawa, U.; Hayashi, T. A novel antivirally active fucan sulfate derived from an edible brown alga, Sargassum horneri. Chem. Pharm. Bull. 2001, 49, 484–485. [Google Scholar] [CrossRef] [Green Version]
- Mandal, P.; Mateu, C.G.; Chattopadhyay, K.; Pujol, C.A.; Damonte, E.B.; Ray, B. Structural features and antiviral activity of sulphated fucans from the brown seaweed Cystoseira indica. Antivir. Chem. Chemother. 2007, 18, 153–162. [Google Scholar] [CrossRef] [Green Version]
- Adhikari, U.; Mateu, C.G.; Chattopadhyay, K.; Pujol, C.A.; Damonte, E.B.; Ray, B. Structure and antiviral activity of sulfated fucans from Stoechospermum marginatum. Phytochemistry 2006, 67, 2474–2482. [Google Scholar] [CrossRef] [PubMed]
- Sinha, S.; Astani, A.; Ghosh, T.; Schnitzler, P.; Ray, B. Polysaccharides from Sargassum tenerrimum: Structural features, chemical modification and anti-viral activity. Phytochemistry 2010, 71, 235–242. [Google Scholar] [CrossRef] [PubMed]
- Chattopadhyay, K.; Mateu, C.G.; Mandal, P.; Pujol, C.A.; Damonte, E.B.; Ray, B. Galactan sulfate of Grateloupia indica: Isolation, structural features and antiviral activity. Phytochemistry 2007, 68, 1428–1435. [Google Scholar] [CrossRef] [PubMed]
- Peng, Y.; Xie, E.; Zheng, K.; Fredimoses, M.; Yang, X.; Zhou, X.; Wang, Y.; Yang, B.; Lin, X.; Liu, J.; et al. Nutritional and chemical composition and antiviral activity of cultivated seaweed Sargassum naozhouense Tseng et Lu. Mar. Drugs 2013, 11, 20–32. [Google Scholar] [CrossRef] [Green Version]
- Bandyopadhyay, S.S.; Navid, M.H.; Ghosh, T.; Schnitzler, P.; Ray, B. Structural features and in vitro antiviral activities of sulfated polysaccharides from Sphacelaria indica. Phytochemistry 2011, 72, 276–283. [Google Scholar] [CrossRef]
- Saha, S.; Navid, M.H.; Bandyopadhyay, S.S.; Schnitzler, P.; Ray, B. Sulfated polysaccharides from I: Structural features and in vitro antiviral activities. Carbohydr. Polym. 2012, 87, 123–130. [Google Scholar] [CrossRef]
- Rabanal, M.; Ponce, N.M.; Navarro, D.A.; Gómez, R.M.; Stortz, C.A. The system of fucoidans from the brown seaweed Dictyota dichotoma: Chemical analysis and antiviral activity. Carbohydr. Polym. 2014, 101, 804–811. [Google Scholar] [CrossRef]
- Lee, J.-B.; Hayashi, K.; Maeda, M.; Hayashi, T. Antiherpetic activities of sulfated polysaccharides from green algae. Planta Med. 2004, 70, 813–817. [Google Scholar] [CrossRef]
- Ghosh, P.; Adhikari, U.; Ghosal, P.K.; Pujol, C.A.; Carlucci, M.a.J.; Damonte, E.B.; Ray, B. In vitro anti-herpetic activity of sulfated polysaccharide fractions from Caulerpa racemosa. Phytochemistry 2004, 65, 3151–3157. [Google Scholar] [CrossRef]
- Gomaa, H.H.; Elshoubaky, G.A. Antiviral activity of sulfated polysaccharides carrageenan from some marine seaweeds. Int. J. Curr. Pharm. Rev. Res. 2016, 7, 34–42. [Google Scholar]
- Duarte, M.; Noseda, D.; Noseda, M.; Tulio, S.; Pujol, C.; Damonte, E. Inhibitory effect of sulfated galactans from the marine alga Bostrychia montagnei on herpes simplex virus replication in vitro. Phytomedicine 2001, 8, 53–58. [Google Scholar] [CrossRef] [PubMed]
- Carlucci, M.J.; Scolaro, L.A.; Errea, M.I.; Matulewicz, M.C.; Damonte, E.B. Antiviral activity of natural sulphated galactans on herpes virus multiplication in cell culture. Planta Med. 1997, 63, 429–432. [Google Scholar] [CrossRef] [PubMed]
- Chattopadhyay, K.; Ghosh, T.; Pujol, C.A.; Carlucci, M.J.; Damonte, E.B.; Ray, B. Polysaccharides from Gracilaria corticata: Sulfation, chemical characterization and anti-HSV activities. Int. J. Biol. Macromol. 2008, 43, 346–351. [Google Scholar] [CrossRef] [PubMed]
- Pujol, C.; Estevez, J.; Carlucci, M.; Ciancia, M.; Cerezo, A.; Damonte, E. Novel DL-galactan hybrids from the red seaweed Gymnogongrus torulosus are potent inhibitors of herpes simplex virus and dengue virus. Antivir. Chem. Chemother. 2002, 13, 83–89. [Google Scholar] [CrossRef] [Green Version]
- Matsuhiro, B.; Conte, A.F.; Damonte, E.B.; Kolender, A.A.; Matulewicz, M.C.; Mejías, E.G.; Pujol, C.A.; Zúñiga, E.A. Structural analysis and antiviral activity of a sulfated galactan from the red seaweed Schizymenia binderi (Gigartinales, Rhodophyta). Carbohydr. Res. 2005, 340, 2392–2402. [Google Scholar] [CrossRef]
- Thompson, K.D.; Dragar, C. Antiviral activity of Undaria pinnatifida against herpes simplex virus. Phytother. Res. 2004, 18, 551–555. [Google Scholar] [CrossRef]





| Disease | Virus | Symptoms | Mode of Infection | Age Group | Course of Infection | Incubation Period | Ref. |
|---|---|---|---|---|---|---|---|
| Acute herpetic gingivostomatitis | HSV-1 | High body temperature (102–104 °F), lethargy, swollen erythematous, anorexia, friable gums, vesicular lesions (on the oral mucosa, tongue, lips and later rupture and coalesce, leaving ulcerated plaques) and regional lymphadenopathy. | Through infected saliva. | >0.6 to >5 years and in adult. | 5–7 days | 3–6 days | [18] |
| Acute herpetic pharyngotonsillitis | HSV-2 | Headache, fever, malaise, sore throat, ulcerative lesions on tonsils and pharynx showing grayish exudates. | Through infected saliva and mucous. | >0.6 to >5 years and in adult. | 5–7 days | 3–6 days | [19] |
| Herpes labialis | HSV-1 | Lesions with pain, burning, and tingling at a face, around the lips, erythematous papules. | Through infected saliva and mucous. | All age groups. | 0–14 days | 3–6 days | [20] |
| Herpetic whitlow | HSV-1 and HSV-2 | Infections and lesions in fingers associated with swelling, tenderness, and reddening of the infected finger. Occasionally with fever and swollen lymph nodes. | Transmitted from primary orofacial and genital infected victims. May also be transmitted from self or other infected victims. Healthcare personnel’s, including dentists during oral examinations oral care with ungloved hands | Thumb-sucking children with primary HSV-1 oral infection Adults aged 20 to 30 following contact with HSV-2-infected genitals. | 10–14 days | 2–20 days | [21] |
| Herpes gladiatorum | HSV-1 | Infection of the face, arms, neck, and upper trunk. Fever. Swollen lymph glands. The affected area suffers a tingling feeling. A bunch of clear, fluid-filled blisters surrounded by redness lesions which may or may not provoke painfully. | Typically seen in wrestlers and participants in some contact sports such as rugby. Infection is promoted by trauma to the skin sustained during matches. | Males and females of all ages of athletes. | <8 days | 7–10 days | [22] |
| Eczema herpeticum | HSV-1 or HSV-2 | Clusters of itchy and/or painful blisters with uncontrolled atopic dermatitis, which may end up in increased morbidity, and mortality, if it prolongs further. | Through infected saliva and contact. | Males and females of all ages but is more common in infants and children with atopic dermatitis. | 5 to 12 days | 7 to 10 days | [23] |
| Family of Herpes Virus | Name of the Virus | Site of Latency | References |
|---|---|---|---|
| Gammaherpesvirinae | Epstein-Barr Virus (EBV) or human herpesvirus 4 (HHV-4) | Lymphocytes | [45] |
| Betaherpesvirinae | Murine cytomegalovirus | Salivary gland, spleen, and lymphocytes | [46] |
| Alphaherpesvirinae | Herpes simplex virus | Nervous site, especially trigeminal ganglion | [47] |
| Species | Extracts/Compounds | Activity (IC50 = μg/mL) | References | |
|---|---|---|---|---|
| HSV-1 | HSV-2 | |||
| Green Algae | ||||
| Caulerpa brachypus | SP-rhamnan type and galactan type | 1.9 (rhamnan type) & 0.65 (galactan type) | - | [115] |
| Caulerpa okamurai | SP-galactan type | 0.55 | - | [115] |
| Caulerpa racemosa | SP fractions | 4.2 | 3.0 | [116] |
| Caulerpa scapelliformis | SP-galactan type | 1.6 | - | |
| Chaetomorpha crassa | SP-arabinoxylogalactan type | 0.85 | - | [115] |
| Chaetomorpha spiralis | SP-arabinoxylogalactan type | 1.9 | - | [115] |
| Codium fragile | SP-arabinan type | 0.86 | - | [115] |
| Codium latum | SP-arabinan type | 0.38 | - | [115] |
| Enteromorpha compressa | sulphated heteroglycuronan | 28.2 | - | [73] |
| Monostroma nitidum | SP-rhamnan type | 0.4 | - | [115] |
| Red Algae | ||||
| Acanthophora specifira | Carrageenan | 80.5 | - | [117] |
| Bostrychia montagnei | Sulfated galactan | 13 | 11 | [118] |
| Callophyllis variegata | Sulfated galactan | 0.2 | 0,2 | [76] |
| Gigartina skottsbergii | Lambda-type carrageenan | 0.6 | 0.4 | [119] |
| Grateloupia indica | Sulfated galactan | 0.3 | 0.3 | [120] |
| Gymnogongrus torulosus | DL-hybrid sulfated galactan | 0.6 | [121] | |
| Meristiella gelidium | Mixture of iota/kappa/nu-carrageenans | 2–0.04 | [122] | |
| Scinaia hatei | Sulfated xylomannan | 0.5 | 0.5 | [71] |
| Brown Algae | ||||
| Adenocystis utricularis | Sulfated galactofucan | 0.3 | 0.5 | [106] |
| Cystoseira indica | Sulfated fucan | 2.8 | 1.3 | [108] |
| Hydroclathrus clathratus | Carrageenan | 100.5 | [117] | |
| Laminaria angustata | Xylogalactofucan | 0.2–25 | [123] | |
| Stoechospermum marginatum | Sulfated fucan | 3.6 | 0.5 | [109] |
| Undaria pinnatifida | Galactofucan sulfate | 32 | 0.5 | [103,114] |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mahomoodally, M.F.; Lobine, D.; Rengasamy, K.R.R.; Gowrishankar, S.; Tewari, D.; Zengin, G.; Kim, D.H.; Sivanesan, I. Marine Algae: A Potential Resource of Anti-HSV Molecules. Processes 2019, 7, 887. https://doi.org/10.3390/pr7120887
Mahomoodally MF, Lobine D, Rengasamy KRR, Gowrishankar S, Tewari D, Zengin G, Kim DH, Sivanesan I. Marine Algae: A Potential Resource of Anti-HSV Molecules. Processes. 2019; 7(12):887. https://doi.org/10.3390/pr7120887
Chicago/Turabian StyleMahomoodally, Mohamad Fawzi, Devina Lobine, Kannan R. R. Rengasamy, Shanmugaraj Gowrishankar, Devesh Tewari, Gokhan Zengin, Doo Hwan Kim, and Iyyakkannu Sivanesan. 2019. "Marine Algae: A Potential Resource of Anti-HSV Molecules" Processes 7, no. 12: 887. https://doi.org/10.3390/pr7120887






