2. General Characteristics of Diseases in the Human Stomatognathic System and Its Prosthetic Treatment
This paper deals with the design and production of prosthetic restorations under the Dentistry 4.0 approach, the adaptation of the augmented holistic Industry 4.0 model in the conditions of a micro-enterprise cooperating with a network of dental clinics, usually private. Therefore, an analysis of the condition in the human stomatognathic system, leading to partial or complete loss of natural dentition and the possibility of prosthetic treatment, has been made.
The stomatognathic system includes soft and hard tissues of the mouth and surrounding areas. Prosthetics of the system involves the introduction of artificial devices and substances to replace the mentioned tissues with dental prosthetic restorations. It ensures that the system will continue to function, while not only improving the patient’s appearance but also his comfort and health. The scope of dental prosthetics includes not only the restoration of the proper functioning of the stomatognathic system but also prophylaxis [
4].
Prosthetic treatment may be necessary for several reasons. It is most often associated with damage or loss of teeth. It may be a consequence of the tooth tissue abrasion as a result of bruxism, the need to strengthen the crown on previously treated root canal teeth in which degrading lesions, periodontal diseases, as well as caries and changes caused by it, require the implementation of restoration a prosthetic tooth crown, both in the form of a prosthetic crown and partial restorations, such as onlay, inlay, or veneer, and ultimately also single or multiple missing teeth or completely toothless. Dental deficiencies can be congenital, including due to a lack of tooth buds. However, the causes of missing teeth are most often acquired. The first case is extractions of teeth, which are directly caused by diseases in the oral cavity, such as periodontal disease. However, the leading cause of dental extractions is caries. The results of epidemiological studies illustrating examples of the extent of the disease and the causes of dental extractions caused by it are collated in publications [
1,
3] and are presented in
Table 2,
Table 3,
Table 4 and
Table 5.
Caries is a bacterial infectious disease of the hard tissues of a tooth. Bacteria that cause the development of dentin disease include anaerobes, Gram-negative bacteria, and streptococci [
99]. As a result of tooth tissue degradation and reaching the pulp, it causes an inflammatory process and, finally, necrosis. Low oxidoreductive potential and low oxygen levels promote colonization by subsequent anaerobic bacteria [
100], intensifying the severity of the disease. Those bacteria produce acids in the plaque, which is the result of intra- and extracorporeal metabolism of sugars. It is a reason for the demineralization of inorganic substances and the subsequent proteolysis of organic substances. The course of such a pathological process affects the successive decalcification and breakdown of the hard tissues of the tooth, which results in inflammatory changes and irreversible destruction of the periodontal tissue, leading to loss of dentition [
97,
101,
102]. At present, caries is a human disease in many countries around the entire globe [
13,
95,
96,
97,
98,
99,
100,
101,
102,
103,
104,
105,
106,
107,
108,
109,
110,
111]. In addition to local lesions in the stomatognathic system, caries also causes numerous systemic complications in many distant organs. Caries affects most adults and 60–90% of schoolchildren [
110,
112] in most countries. For example, in Poland, with a high share of tooth decay [
102,
113], only 0.1% of adults aged 35–44 and only 19.3% of 12-year-old children are free from caries [
111,
112] (
Table 3).
The level of caries severity intensifies when the diet of a given society has an excess of purified sugars [
97,
102,
109,
110,
111]. It is considered the most common and expensive chronic disease. Caries is a human disease, and the scale of its prevalence depends, among others, on the economic situation and the general level of culture in society and may also be the result of many years of systemic neglect in the organization of health care in a given country [
97,
109,
111,
114,
115]. Minimizing the impact of caries bacteria on teeth requires strict observance of the principles of oral hygiene and proper prevention, as well as early detection of tooth decay initiation and periodontal disease [
97,
114,
116]. Teeth with irreversible pulpitis and pulp necrosis are now effectively left in the mouth for many years after modern endodontic treatment using liquid gutta-percha [
117,
118]. Peri-apical lesions, such as granulomas or cysts, may develop in treated endodontic teeth [
119]; however, according to statistical studies, it only applies to 3% of cases 8 years after treatment [
120,
121,
122,
123] (
Table 4).
Table 5, on the other hand, indicates epidemiological data on the number of teeth treated endodontically with periapical lesions revealed in pantomographic images [
119,
120,
121,
122,
123,
124,
125,
126,
127,
128,
129,
130,
131,
132,
133]. Of the 3% of failures, most were revealed within the first three years of discontinuation of treatment and resulted from improperly developed and inaccurately filled root canals [
119,
120,
121,
122,
123,
124,
125,
126], which concerns 91% of teeth treated endodontically with revealed periapical lesions [
119].
Numerous tooth extractions are very often a necessity in the treatment of tooth decay [
13,
95,
96,
98,
103,
104], in particular, if the patient is negligent in prevention, in the case of cancer or as a result of injuries during an accident [
134] or if there are errors in treatment, tooth fractures after endodontic treatment. Other reasons for the failure of endodontic treatment include iatrogenic causes, such as root or crown fractures [
120]. The endodontic treatment of teeth is statistically more often performed in women, and the least biting teeth of the jaw are subjected to it, while most often premolars and molars of the jaw [
104] and molars of the mandible [
126].
Figure 1 illustrates the extent and diversity of the most common dental defects of a patient. It presents as an example of the classical classification of upper and lower jaw dental defects, as well as left and right arches.
The tooth as a result of conservative or endodontic treatment often requires prosthetic reconstruction due to the significant loss of hard tissues and the limitations of composite materials for direct reconstruction in the oral cavity. Teeth with living pulp are also subjected to prosthetic treatment in case of tooth wear and the need to increase the occlusion height, desire to improve the cosmetic effects, or the need to reproduce the missing tooth or teeth when creating a structure in the form of a prosthetic bridge. Tooth deficiencies from single to complete toothlessness are still prevalent and inevitable. Extractions of teeth temporarily solve problems but, at the same time, affect the formation of other issues related to the violation of the structure and balance of the stomatognathic system. It can function properly only if it ensures an even distribution of chewing forces on the teeth in all sections of the dental arches. Improving the health condition, and mainly food chewing conditions and treatment of associated digestive system diseases, elimination of frequent headaches caused by masticatory dysfunctions, as well as the desire to improve the appearance of patients’ faces, requires the use of modern dental prosthetics and the use of appropriate biomaterials and appropriate technologies [
3,
4,
5,
6,
7,
8,
9,
10,
11,
12,
79,
135].
Prosthetic restorations are each time individually designed and manufactured in a way dedicated to each patient. Both alive and dead teeth after endodontic treatment are subjected to prosthetic treatment. The need for prosthetic reconstruction is often a consequence of endodontic or conservative treatment associated with significant loss of hard tissues and the limitations of tooth reconstruction using composite materials. The possibility of making a prosthetic bridge reproducing missing teeth is closely related to the presence of prosthetic pillars characterized by the required quality and correct placement. Those restorations can be based on the patient’s own teeth or implants [
136], but they should not be simultaneously attached to implants and their own teeth. Devices permanently attached indelibly in the mouth to stop the dysfunction of the system are generally classified as dental prostheses [
6].
Out of the four groups (
Table 6), they include permanent prosthetic restorations not removable from the oral cavity by the patient and forming a kind of unity with the living organism, including bridges, onlays, crown-root inlays, and crowns, as well as crowns and bridges based on implants screwed directly or indirectly through implant platforms or cemented to implantology abutments embedded in implants. The second group is mobile prosthetic restorations that can be removed by the patient from the mouth. Those include skeletal, acetal, acrylate, and nylon dentures based not only on own teeth and mucosa or exclusively on the mucosa but also on dentures based on implants on telescopes integrated with the implant connector or mounted on a beam screwed to the implants. The use of removable dentures based on teeth and mucosa or only on the mucosa is still necessary in some cases. However, it involves limited retention of those elements in the planned place during use and significant degradation of tissues affected by such a prosthesis. The financial aspect still determines its use. They are also performed for medical reasons in patients with a tooth system that is not indicated for the introduction of bridges based on their own teeth, and bone base reconstruction using a bone substitute or autograft or both of these materials is not possible at the same time, or it does not give satisfactory results. Also, during such treatment, long-term, temporary prostheses are used. The third case is combined with prosthetic restorations. Then, removable dentures and permanent restorations, which is the case with precision dentures, are connected. The connecting elements are bolts and latches.
The last case is implantology hybrid solutions, combining the advantages of withdrawn prosthetic restorations with the perfect mounting of permanent prosthetic restorations. Such a type of prosthetic restoration includes prosthetic implant bridges based on telescopic crowns. The prosthetic restoration can be removed by the patient for hygienic procedures once a week or even once a month. Such a solution prevents bone base degradation, which can occur in the case of permanent prosthetic restorations and, in particular, in patients with periodontal disease. An example of such a prosthetic restoration is the design of the authors’ titanium hygienic bridge, which combines the advantages of a titanium prosthetic restoration core with the option of its withdrawal.
The extent of the patient’s dental defects determines the scope of prosthetic treatment and the choice of the type of prosthetic restoration (compare
Figure 1). It indicates a large number of possibilities and diversity of the manufactured prosthetic restorations [
1].
Implants of the stomatognathic system are used to supplement teeth defects and replace, improve, or increase any hard tissue of the jaw, mandible, or temporomandibular joint in the mouth [
135]. For years, the most convenient shape of dental implants has been worked on, and their general classification is presented in
Table 7.
A correctly designed dental restoration meets biological, strength, and technological expectations. The materials used and the design features of the implant introduced to the body must, first and foremost, guarantee compliance with the bio tolerance requirements. An implant cannot initiate inflammation, nor can it promote chronic and acute immune responses and toxicological reactions, nor can it irritate adjacent tissues [
13]. In such cases, various substances differing from medicines, or a mixture of various natural and synthetic substances, are classified as biomaterials, often also referred to as biomedical materials, which can replace or supplement living tissues in performing all or some of their functions [
14]. Besides, depending on the intended use of implants or other dental restorations, dental biomaterials must meet different requirements [
1].
Table 8 presents guidelines regarding the desired properties of implants and related requirements for the biomaterials used for them. However, in the case of a dental crown, the high compressive strength and high tribological properties are expected. Still, other expectations are concerning biomaterials used for orthopedic implants.
Implants must ensure a combination of natural body tissues, including in the mouth with artificially manufactured implants and prosthetic restorations. In addition to the requirements for the structure and mechanical properties and fulfillment of operational requirements, an essential criterion for the selection of biomaterials for individual implants and prosthetic restorations, including dental, is the diversity of technological and economic conditions, as well as the availability of clinical methods of varying levels, and crucial considerations, in this case, aesthetic. Practice indicates that the most frequently mentioned criteria in dental engineering fill foundry cobalt alloys, titanium and its alloys, and ceramics based on zirconia [
83,
137,
138,
139,
140,
141,
142,
143,
144,
145,
146,
147], and there are serious reasons to expand the canon with magnesium alloys.
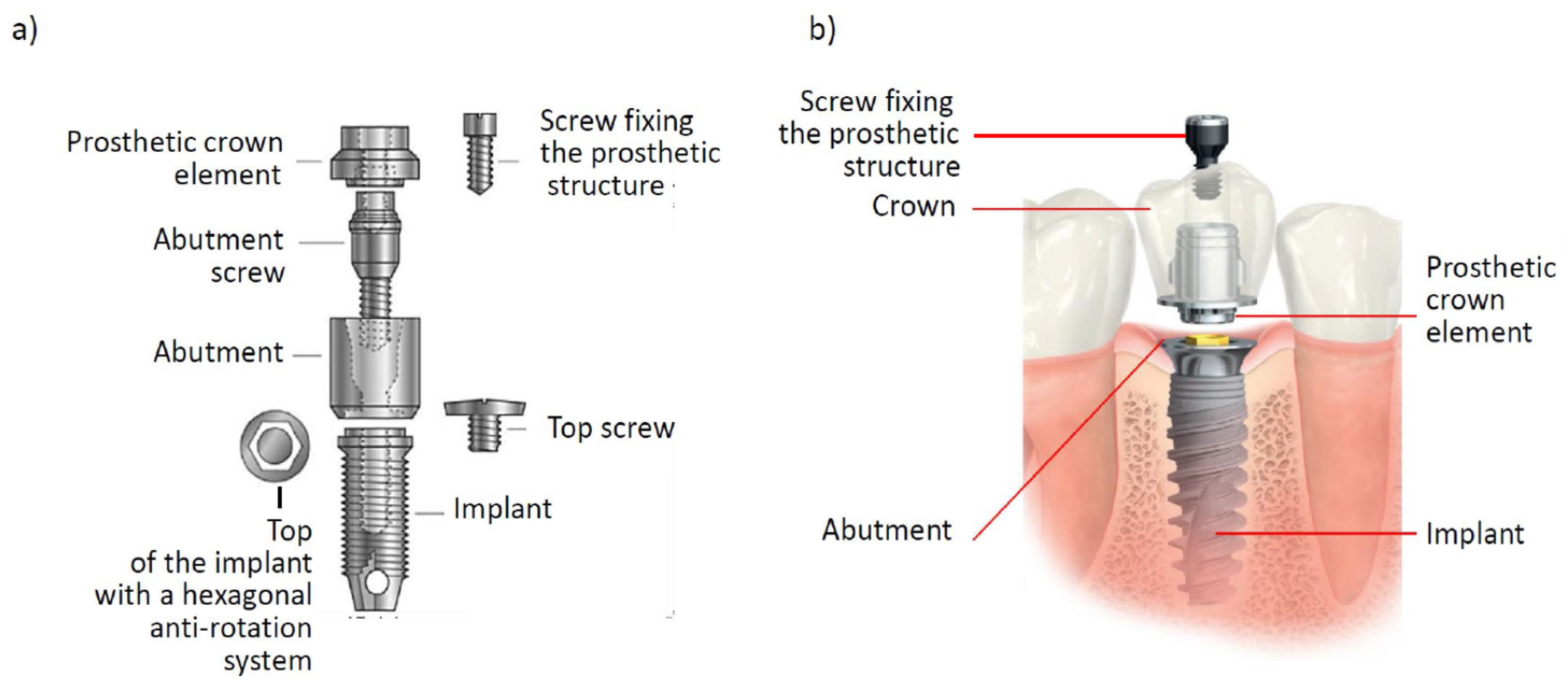
Dental implants have gained a cylindrical shape since the 1960s and are screwed into the bone, according to the concept of P.I. Braenemark [
5,
7,
8,
9,
10,
11,
12]. It was found out that it is the most advantageous of the possible connections. In 1965, titanium was used for dental implants, and the phenomenon of osseointegration confirmed at that time became a breakthrough and practically initiated the development of modern implantology. Osteointegration involves the fusion of implant surfaces with trabecular bone structures [
5,
7,
8,
9,
10,
11,
12,
148,
149,
150,
151,
152,
153,
154,
155,
156]. Starting from the 1980s, studies have shown that titanium oxide formed as a layer on the surface of titanium enables bone tissue regeneration by stimulating its growth and formation of epithelial attachment, which is a bone defensive reaction, guaranteeing implant fixation and stabilization [
157,
158,
159]. The dental implantation procedure includes, in the first stage, examination, diagnostics, and preparation for implantation, in the second stage, implant placement, and the third stage consists of prosthetic loading of the implant. As part of the primary stabilization, a hole is made in the bone into which the implant is screwed, causing its immobilization with the assumed force. Ultimately, secondary stabilization by osseointegration takes place (
Figure 2).
In the first stage of the dental implantation procedure, inflammation occurs as a consequence of bone trauma as a result of surgical intervention. The second stage involves bone healing, starting from supplying blood through small blood vessels damaged during surgery to local osteonecrosis compacted to a depth of 1 mm along the entire length of the implant. The body is stimulated to differentiate stem cells into osteoblasts that stimulate bone healing and osteoid or bone matrix formation in newly created connective tissue. After about 2–3 days of the process, bone mineralization takes place over the next week, thanks to osteoblasts, so that after 4–6 weeks, there may be a repair bone, though with poor mineralization, but already connected to the patient’s bone. The prosthetic restoration can take place after at least three months after the implant’s placement. A temporary immediate reconstruction should be performed. It is also currently accepted that patients who meet stringent requirements can have direct implantation involving the removal of a tooth that does not have large periapical lesions and must be removed (e.g., as a result of root fracture, which often occurs after root canal treatment) and its replacement with an implant. A temporary reconstruction will be placed in the remaining alveolus, which, due to the risk of non-acceptance of the implant, must remain excluded from the occlusion.
Regardless of the widespread use of cylindrical implants with a helical surface, currently, several works are being carried out, including the own work of the authors of this article [
81,
91,
92,
160]. They deal with implants for whose manufacturing, it is necessary to use the cone-beam computed tomography (CBCT) method, to assess the state of deficiencies to patients’ teeth and individual design of adequate individual prosthetic restorations. The widespread use of CBCT tomography allows planning prosthetic implant treatment and individual design of appropriate prosthetic restoration [
91,
92]. The technology of producing prosthetic restorations and engineering materials used for the purpose is systematically progressing. Regardless of the development of the digitization of dental diagnostics through the use of CBCT tomography, in the last decade, the role of computer-aided design/manufacturing CAD/CAM in dental engineering has been increasing [
91,
92,
161,
162,
163,
164,
165,
166,
167,
168].
Metal foundations made of cobalt–chromium alloys, titanium alloys, zirconium oxides, and aluminum oxides, as well as poly (methyl methacrylate) (PMMA), can be manufactured by milling in numerically controlled machining centers (CNC). Frameworks made of metal alloys are increasingly manufactured by additive methods. The digital prosthetic model is individually designed with the use of computer-aided design (CAD) and scan results of an intraoral scanner, under the supervision of the attending dentist. Such an approach allows planning the placement of the implants, ensuring entirely aesthetic reconstruction, with optimal use of the patient’s bone base. Implantology abutments should not fit in the interdental spaces but the lumen of the prosthetic crown. It is necessary to use the surgical guide, developed by authors [
92]. It allows the dentist to place the implants in places strictly designated for such a purpose. The authors’ procedure was developed as a result of cooperation between a dentist and a dental engineer. According to the procedure, the implantation area requires a combination of a three-dimensional bone base model made with the use of a CBCT tomogram with a three-dimensional scan directly from the oral cavity or an impression scan used for a three-dimensional model of the dentition and soft tissues in the oral cavity. On this basis, the prosthetic restoration design is made, and the placement of the implants is planned. It involves planning technological holes to guide the pilot drill in such a way that holes are made in the bone in the right direction, which is achieved by creating a surgical guide using the stereolithographic (SLA) method. The guide is made of PMMA, and the pilot tunnels are filled with a titanium sleeve, produced by the selective laser sintering (SLS) method. It is a radical turnaround in the CAD/CAM design of the implant device system and in clinical procedures. On the other hand, the finite element method (FEM) is commonly used as a computational simulation tool for prosthetic restorations and enables the prediction of their behavior in application conditions [
169,
170,
171,
172,
173,
174,
175,
176,
177,
178,
179,
180,
181,
182,
183,
184,
185,
186,
187,
188,
189,
190,
191,
192].
Completion of the design of the prosthetic restoration by choosing the shape and material design by choosing, e.g., cobalt or titanium alloys, the numerical CNC milling machine performs machining of the appropriately selected material disc, when, in the case of choosing ceramic materials, e.g., ZrO
2, coloring paints and sintering are also applied using resistance or microwave ovens, followed by surface application and firing of facing ceramics, regardless of the material [
91,
92].
Computer-aided technologies for both design and manufacturing (CAD/CAM) are widely used in the field of additive manufacturing (AM) technologies. Among the full range of known additive technologies, mainly selective laser sintering (SLS) and stereolithography (SLA) are used in dental prosthetics [
2,
3,
80,
160,
162,
166,
193,
194,
195,
196,
197,
198,
199,
200,
201,
202,
203,
204,
205,
206,
207,
208,
209,
210,
211,
212,
213,
214,
215,
216,
217,
218,
219,
220,
221,
222,
223]. The use of additive manufacturing technologies is unrivaled for the design and manufacturing of prosthetic restorations from solid and microporous materials compared to casting technologies, powder metallurgy, and the production of metallic foams. Selective laser sintering (SLS) is the only one that allows for a full mapping of the designed shape, which positively affects both the shape of the framework and then the entire prosthetic restoration, as well as its mass, which is crucial for the patient, especially in the case of extensive prosthetic restorations. Additionally, only by means of selective laser sintering, the porous skeletal structures of implants can be produced, e.g., teeth, but also bones from metal alloys with the required biocompatible properties can be produced [
208].
Specifically, the relevant material properties include the absence of allergic and cytotoxic reactions in contact with living tissues, osteoconductivity, and osteoinductivity when the pore diameter is 50–500 µm, ensuring bone ingrowth, mechanical stabilization, the possibility of sterilization and sterility as elements of biological safety, resorptive and tissue substitution capacity with bone reconstruction, and the ability to fill the defect space [
3,
224,
225].
The results of procedural benchmarking [
85,
226,
227,
228,
229] and analysis of technology value using the weighted scoring method and dendrological matrix using a 10-stage universal unipolar positive scale without zero relative states create the conditions for the comparative assessment of individual technologies in the process of manufacturing porous materials [
85,
226,
227,
228,
229]. The analysis perfectly objectifies the made estimations. Detailed attribution of weights to individual criteria of technology assessment in terms of their potential as a measure of the objective value and attractiveness indicated by customers and [
230] has enabled to accurately compare those technologies in the interesting area of prosthetic restorations. The potential and attractiveness of technologies of additive manufacturing (TAM) with successively given coordinates of potential and attractiveness (8.6; 6.6) are much higher than other analyzed technologies. The determined coordinates ensure the location of the technology in the quarter-spreading oak of the said dendrological matrix, which means very favorable development prospects for those technologies. Other obtained technologies lower coordinates, that is why their development prospects in the analyzed area of application are not as desirable as technologies of powder metallurgy (TPM) (3.5; 5.0), technologies of casting (TC) (4.9; 4.4), and the technology of metallic foams (TMF) manufacturing (6.5; 4.3). The results of foresight studies [
231,
232] also confirm the very high development prospects of selective laser sintering (SLS) of metal and ceramic powders, which still belongs to embryonic, experimental, or prototype technologies [
209,
232,
233,
234] with very high potential and attractiveness. It justifies the excellent research interest in this issue concerning dental prosthetics.
It should be noted that, as in any case of sintering, among others, in powder metallurgy, sintering occurs in the liquid phase in 90% of the commercial value of sintered products [
163] because mass transport in the liquid phase is hundreds of times faster than in the case of sintering in solids [
163,
235,
236,
237,
238,
239,
240]. The liquid phase is formed under those conditions, and the liquid phase wets the particles of the remaining undissolved powders [
209,
223], inducing capillary forces [
220,
228], which affects the thickening and, as a result, the melting of a solid with high surface energy, even in relatively distant areas, and then their solidification [
127]. Liquid phase sintering (LPS) includes coexisting liquid and solid during part or all of the sintering process [
127]. The structure of sintered materials with a liquid phase consists of evenly distributed solid phase particles in the matrix of solidified liquid, including during SLS (
Figure 3).
Very modern technologies used in the manufacturing of implants and other prosthetic restorations include surface engineering technologies [
211,
241,
242,
243], e.g., atomic layers deposition ALD (
Figure 4), and less preferably physical vapor deposition (PVD). The particular benefits of the use of those technologies in dental prosthetics include barrier prevention by applied surface layers of unfavorable greying of cover ceramics as a result of revival diffusion of titanium atoms and other metals to ceramic surfaces of crowns and bridges, and even cracking of the porcelain facing layer. In turn, inside the pores of the skeletal porous structure selectively sintered by laser, e.g., from Co–Cr alloys, titanium, or its alloys powders, thin layers, e.g., TiO
2, ZrO
2, or Al
2O
3, can be applied inside the pores (
Figure 4), ensuring the proliferation and growth of living osteoblast cells. Studies using human cells from the hFOB 1.19 osteoblast culture line (Human ATCC-CRL-11372) American Type Culture Collection ATCC (USA) have been performed. In the example of the Ti6Al4V alloy, it has been indicated that coverage with ALD layers promotes the growth of viable cells, and their viability increases by up to more than 12% [
244,
245]. The stereolithographic (SLA) method is applicable to the implant template model.
A new class of implantable devices that, by all means, are desirable to use, among others, in dental implantology are implant-scaffolds. Those are new applications for which, due to the inability to depart from medical indications to classical prosthesis/implantation, it is necessary for natural cells to grow into the implanted elements and not just to generate living cells on their surface [
2,
3,
80,
244,
245]. The wholly innovative and patent-protected implant-scaffolds, developed by the authors of this paper, contain a solid zone, like all implants used so far, and a hybrid porous zone is connected to it, fulfilling the function of scaffolds. The zone contains 100–600 µm micropores of various shapes.
Personalized implant-scaffolds (
Figure 5) are made from powders of biomaterials, e.g., titanium and its alloys or Co–Cr alloys, through selective laser sintering (SLS). Inside the pores of implant-scaffolds, layers are applied using the atomic layers deposition (ALD) method, providing favorable conditions for the growth and proliferation of live cells after implantation. Implant-scaffolds can also be dedicated to dental implantology. The idea is developed by the author’s concept of hybrid multilayer biological-engineering composites [
244,
245]. The structure of those hybrid multilayer composites is the artificial part, produced in the form of a porous skeleton by the SLS method with optional ALD layers inside the pores, and the biological part, consisting of living cells filling the micropores of skeletal engineering materials [
244,
245]. Such hybrid multilayer biological-engineering composites after completing in-vitro and in-vivo tests will find their use in dentistry and regenerative medicine, in general, to replace damaged and removed parts of the body, including teeth.
Implantology treatment is teamwork characterized by the cooperation of a dentist, often a surgeon, prosthetist, often an orthodontist, and dental engineer, using tissue engineering methods. In each case, prosthetic restorations are individually designed and manufactured for a specific patient. The activities and operations of planning, designing, and manufacturing them constitute a complex clinical and manufacturing process. The synergy of advanced interdisciplinary knowledge in the field of imaging medicine and dentistry, tissue engineering, dental engineering, material engineering, and computer-aided design currently allows the dentist to implement complex treatment plans. The detailed design and management plan prepared in the dental engineering laboratory, resulting from the treatment plan, are the conditions for the effectiveness of clinical management. It applies, especially to the design and manufacturing of individual prosthetic components and surgical guides. Those works must be carried out in such a way that the chance factor is minimized as much as possible during the implant surgery. At the same time, it is necessary to ensure the full repeatability of medical procedures and ensure the least invasive procedure. It requires a mutual understanding by the dentist and dental engineer of the specifics and limitations of both technological and mid-surgical, creating a framework of trust and cooperation.
It should be taken into account that, as in any technical or industrial operation, it is now necessary to use the principles of the augmented holistic Industry 4.0 model in modern dental engineering. It applies to various spheres of activity, equally on both engineering design of different types of prosthetic restorations and their production. It also indicates a significant increase in the role and importance of the dental engineer, his knowledge, and experience in modern prosthetic treatment in dentistry. Thanks to this, it is not only possible to individually design prosthetic restorations, taking into account the patient’s anatomical features, but the process of manufacturing these restorations is subject to all the rigors of modern industry, using the most modern technologies. In this respect, the production of prosthetic restorations does not differ in principle from the manufacturing of the most advanced products available on the market, e.g., car, aircraft, or robot components.
3. The Dentistry 4.0 Concept as a Consequence of the Current State of Civilization and Technology Development
This paper analyzes the possibilities of adapting the extended holistic Industry 4.0 model to the design and production of prosthetic restorations based on extensive literature studies. The implementation of the Industry 4.0 stage of the industrial revolution is progressing dynamically in individual industrial sectors. The process primarily involves creating so-called smart factories and, in fact, transforming existing manufacturing plants in such a way that, among others, digital technologies, data analysis, cloud computing, and additive technologies gain the practical significance. Undoubtedly, it also includes dental clinics and the processes of transformation of dental prosthesis restoration manufacturing centers into smart factories. The whole complex process is taking place in many places around the world and is termed Dentistry 4.0 [
1,
94] with varying degrees of advancement.
Systematic progress includes an increasing number of dental clinics, mainly centers for the production of prosthetic restorations. The progress is inevitable, and besides the technical aspect, it has a deep moral and ethical sense for those entities, which, for various reasons, but always consciously shirk active participation in the process, actually act to the detriment of patients. Patients receive less well-designed and manufactured prosthetic restorations, and the clinical procedure can be more invasive and expose them to greater pain sensations and a higher risk of complications. Those changes are evolutionary, and digital dentistry is as if absorbed successively by conventional dentistry. Over the past two decades, these changes have become increasingly dynamic and widespread [
1,
93]. It is undoubtedly a breakthrough, although such development depends on many factors. Those factors include the development of dental materials, manufacturing processes, and the level of equipment in technological machines. It involves ever-increasing requirements for financial commitment. It is even more challenging to overcome the barriers associated with mastering and adapting to the needs of dental prosthetics’ very complex tools, machines, and cyber-IT systems being customized. It forces the cooperation of dentists with dental engineers, creating a specific supply chain. Those factors are typical attributes of the generalized Industry 4.0 holistic model. For this reason, considerations on such issues are presented later in this paper.
The value of society, as well as the increase in people’s productivity and efficiency, depend on innovation and technological processes. Various strategic programs, including sustainable development goals (SDG) established by the UN, have been created in various countries. The Society 5.0 program deals with the development of the information society and human well-being. It was implemented in 2016 by the Government of Japan [
22,
246,
247,
248,
249,
250,
251,
252]. The Industry 4.0 program introduced in Germany [
15,
16,
17,
18] concerns the technological development of industry and IT aiding for manufacturing. The approach has been widespread in the European Union [
19,
21] and in many other countries of the world [
20]. Currently, the most advanced developmental stage of the industrial revolution is developing, the detailed aspects of which have been extensively described in the literature [
22,
23,
24,
25,
26,
27,
28,
29,
30,
31,
32,
33,
34,
35,
36,
37,
38,
39,
40,
41,
42,
43,
44,
45,
46,
47,
48,
49,
50,
51,
52,
53,
54,
55,
56,
57,
58,
59,
60,
61,
62,
63,
64,
65,
66,
67,
68,
69,
70,
71,
72,
73,
74,
75,
76]. The first stage of Industry 1.0 is associated with the invention of steam machines at the end of the 18th century [
77]. Computer-aided design and production using electronic devices but also an electronic cloud, augmented reality, machine learning, and advanced robotization applies to the current stage of Industry 4.0. It is accompanied by care for the full implementation of the sustainable development principle and zeroes technology emissivity [
253]. It applies to the so-called green life cycle of products and services from design to the recycling of post-production and post-operational waste. The Economy 4.0 model, taking into account the development stage of Industry 4.0, models the relationship between economic growth, concern for the climate and the human environment, and ensuring the quality of human health and life [
254,
255].
Due to the use of extensive information and sensory systems and technologies, with the necessary participation of people and the aiding of production automation along with the introduction of the Industry 4.0 stage of industrial development, the digital age in the industry was initiated [
15,
18,
19,
20,
21,
22,
25,
26,
27,
28,
29,
30,
31,
32,
33,
34,
35,
36,
37,
38,
39,
40,
41,
42,
43,
44,
45,
46,
47,
48,
49,
50,
51,
52,
53,
54,
55,
56,
57,
58,
59,
60,
61,
62,
63,
64,
65,
66,
67,
68,
69,
70,
71,
72,
73,
74,
75,
76]. The Internet of things (IoT), together with the Internet of people and services, integrate internal and inter-organizational networks [
22,
27,
29,
32,
39,
41,
43,
45,
47,
49,
66], enabling connecting participants in the value chain when previously, despite the use of various other technologies’ operations connecting different machines, the full visibility of processes at the factory was impossible. Currently, high computing power, metadata processing, and other cyberspace attributes, enabling the creation of social, business, biological, and cyber-physical systems (CPS), with a close connection with the technological activity, are used [
22,
28,
33,
44,
46,
57,
58,
60,
63]. Those systems perform various tasks using the Internet of things, as well as sensors, radiofrequency, and identification elements, triggering devices, and even cell phones [
22,
27,
29,
32,
39,
41,
43,
45,
47,
66].
The Industry 4.0 concept significantly improves the manufacturing process and reduces the costs of materials, storage, and management. Smart factory systems allow improving operational flexibility with various production configurations and supply chain efficiency. The system mentioned above of sensors cooperating with the Internet of things, the use of big data sets, and results-oriented orientation ensures improvement of supply chain efficiency and accuracy of predictions in this respect, guaranteeing a sustainable increase in productivity [
256]. Many elements related to the application of the Industry 4.0 concept also improve the competitiveness of not only companies but also regions. Beneficial acceleration of industrial growth, improvement of production economics, increase of productivity, and changes in the profile of labor force can be specified here [
42,
48].
Comparison of Industry 4.0 and Society 5.0 models indicates that the latter is much broader in terms of not only technical aspects but also includes a longer historical perspective. On the contrary to the name, the Industry 4.0 model does not even cover all cyber-physical systems. Still, in fact, it only concerns a fragment of the issue related to cyber-IT systems [
22,
34]. The model presented in the report [
17] did not take into account engineering materials that are necessary for the manufacturing of any product or manufacturing processes, except for additive technologies. Those technologies often turn out to be impossible to use, they are rarely unrivaled, and in many cases, only alternative or complementary. There are also no technological machines in the model. In fact, the model [
17] is an IT component of industrial development, but not the only one [
1]. Although it is popularized by many official documents, including in the European Industry Digitization Strategy [
19], through the development of so-called Digital Innovation Hubs [
21] and in four flagship projects of the European Institute of Innovation and Technology (EIT) [
257], the model contained in work [
17] is incomplete and requires supplementation and augmentation. It is not true that by paying attention to the development of cyber-IT systems [
18,
258], one can ignore the need for progress in the field of materials used to manufacture any product, as well as machines and production technologies. It is also advisable to take into account the anticipated development trend of living and bioengineering machines [
259]. Dynamic development of additive technologies [
1,
15,
16,
17,
18,
19,
20,
21,
25,
26,
27,
28,
29,
30,
31,
32,
33,
34,
35,
36,
37,
38,
39,
40,
41,
42,
43,
44,
45,
46,
47,
48,
50,
51,
53,
54,
55,
56,
57,
59,
60,
62,
64,
66,
202,
203,
209,
224,
225,
230,
232,
233,
234,
241,
246,
247,
248,
249,
250,
251,
252,
260,
261,
262,
263,
264,
265,
266,
267,
268,
269,
270,
271,
272,
273,
274,
275,
276,
277,
278,
279,
280,
281,
282,
283,
284,
285,
286,
287,
288,
289,
290,
291,
292,
293,
294,
295] justifies their inclusion in the industrial development model, but it is necessary to take into account other technologies that make it possible to manufacture many products and which also currently require very advanced computer support [
1,
22,
24,
25,
34]. Currently, various hybrid technologies are also used, combining conventional, although advanced technologies for the production of materials or products with incremental technologies of their production are commonly used. The model should also take such an aspect into account.
The authors’ views on the full augmented holistic Industry 4.0 model (
Figure 6) and the need to augment the current model has already been presented previously [
20,
37,
296]. The model in the form of an octahedron contains people playing a leading role, a technological platform with four complementary components, and products that are the target of the action. Unbalance of the advanced level of the contractual level of impact of each of the individual components in the technological platform of the extended holistic model of Industry 4.0 indicates the need to increase the intensity of development of the particular component, and not only cyber-IT systems, which is allowed in the current model or any other developed in an unsustainable way.
Such a point of view is indirectly confirmed in a recently published report because the idea of Industry 4.0 is based on a combination of modern manufacturing processes of various technology components, i.e., digital production technology, nanotechnology, biotechnology, and new materials [
82]. In practice, according to the holistic augmented Industry 4.0 model presented by the authors, all technologies, machines, and materials used in practice decide on real progress. However, each of them individually determines growth to varying degrees, and no progress is possible without any of them. New technologies bring about integration and sustainable industrial development (ISID) by bringing new goods to the market and improving production efficiency. The evolutionary introduction of advanced digital production (ADP) technology of the Industry 4.0 stage of the industrial revolution consists of a combination of hardware, software, and connectivity. The dissemination of advanced digital production technologies (ADP) involves the development and use of artificial intelligence, analysis of big data sets, cloud computing, Internet of things (IoT), and advanced robotics and successively combines physical and digital production systems. Currently, only ten countries in the world introduce ADP technologies, having 90% patents and exporting up to 70%; the idea should be expected to develop in the economies of other 40 countries over time and perhaps the next ones in the future [
82].
On the contrary to appearances, the augmented holistic Industry 4.0 model is used not only in large manufacturing organizations in the high technology industry, such as space, aviation, automotive, machine, defense, or electronics, but also in small and medium enterprises and smart factories created there. It is a guarantee of real progress as, e.g., as much as 99% of all enterprises in the European Union are micro and small and medium-sized enterprises (SMEs). For example, more than half of the total value added of EUR 3.9 billion in 2015 generated almost 23 million small and medium enterprises in the European Union [
297]. From this point of view, the issue is significant for centers for the production of prosthetic restorations, which usually belong to the group of entrepreneurs.
The basis of manufacturing being launched and performed in engineering designing is the basis for the production of all products. Engineering designing inseparably includes structural designing (including the development of the shape and geometric form of the product or its element), material (related to shaping the structure and properties of materials corresponding to the requirements in working conditions), and technological (related to the processing of engineering materials to manufacture a product) [
23,
83,
231,
298,
299].
All products require the use of engineering materials for their manufacturing, which, therefore, play a crucial role [
83]. The material is solid with properties that enable it to be used by man in the manufacturing of products and can be natural or engineered when the natural resources used to require complex manufacturing processes to adapt them to technical needs. The expected functional properties of the product are ensured as a result of designing the expected material, processed in the expected manufacturing process, ensuring the expected shape and geometric features of the product, the expected material structure, ensuring the expected mechanical, physical, and/or chemical properties of the material, which guarantees the expected operating functions of products [
83,
299] (
Figure 7). It is the 6xE principle of the six expectations, exposing the material science and material engineering paradigm.
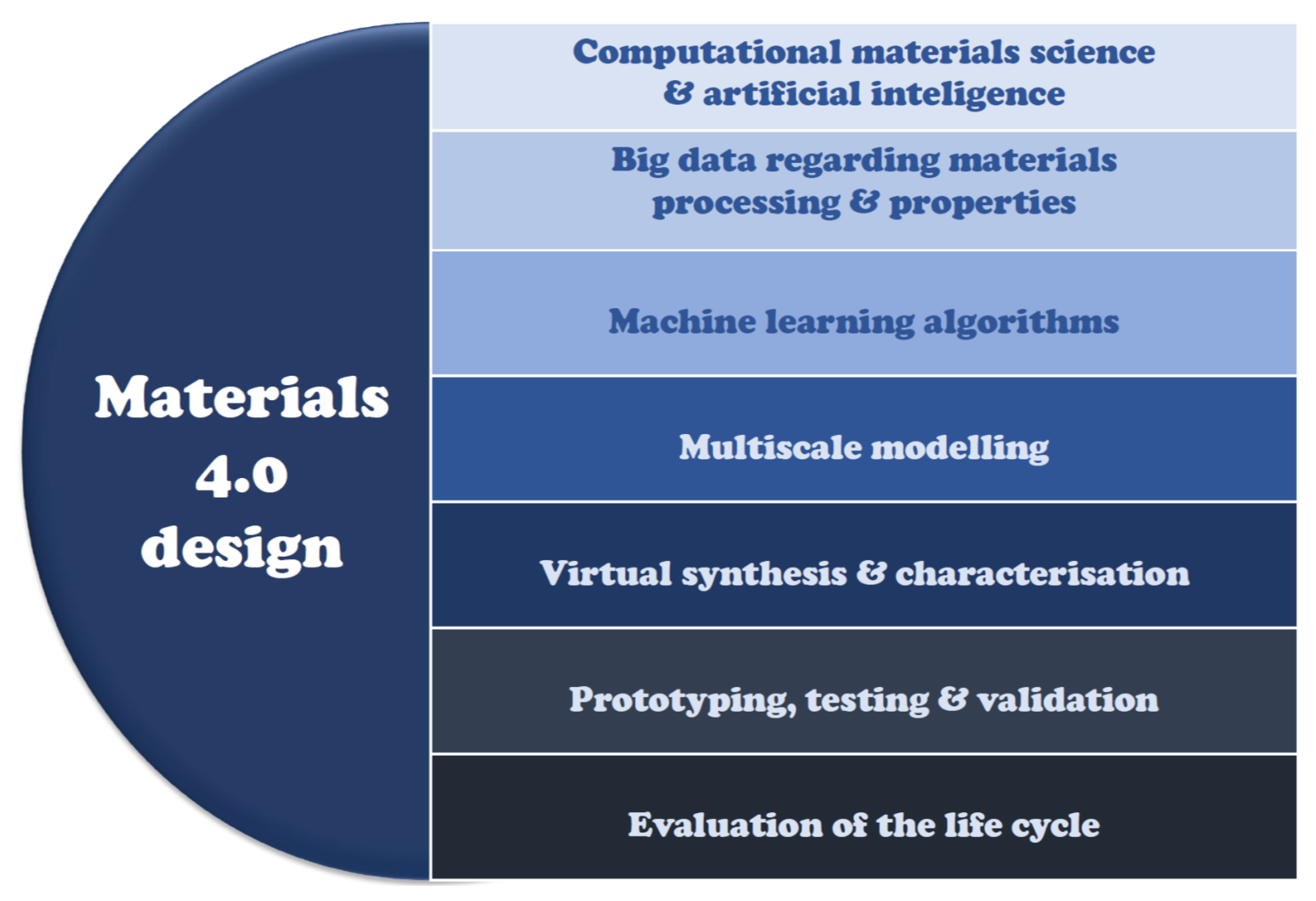
Multi-criteria optimization, inevitably computer-aided one, enables material design and selection of one or more alternative materials for a particular product or its element from among metals, ceramics, polymers, composites, and special materials, e.g., porous or foams. The criteria are taken into account relating to the chemical composition, manufacturing conditions, operating and maintenance conditions, as well as the method of removing material waste in the post-use phase. Economic aspects and price conditions regarding its acquisition, processing into a product, and its exploitation, as well as the costs of removing post-production and post-operational waste, are also important. The modeling of processes and material properties is also included. Today, over 100,000 engineering materials are used. Initially, throughout almost the entire history of human civilization until the early twentieth century, the materials were selected by trial and error. Over time, a material selection methodology was developed, followed by the material’s design in recent decades. The currently avant-garde Materials 4.0 method not only covers human systems but uses advanced cyber-physical systems containing material data, artificial intelligence tools, and intelligent machine learning algorithms (
Figure 8) [
24,
83,
84,
85,
86,
87,
88,
89].
Manufacturing products from raw materials requires the use of various processes, the use of many machines, and the organization of operations according to a well-prepared plan with properly used materials, energy, capital, and people. Manufacturing requires the involvement of people of different professions and to perform various tasks and the use of multiple machines, equipment, and tools. Currently, the degree of automation is usually high, and the use of computers to control the processes and products as well as computer networks and robots is significant [
83,
231,
299]. A general diagram of technological processes is shown in
Figure 9.
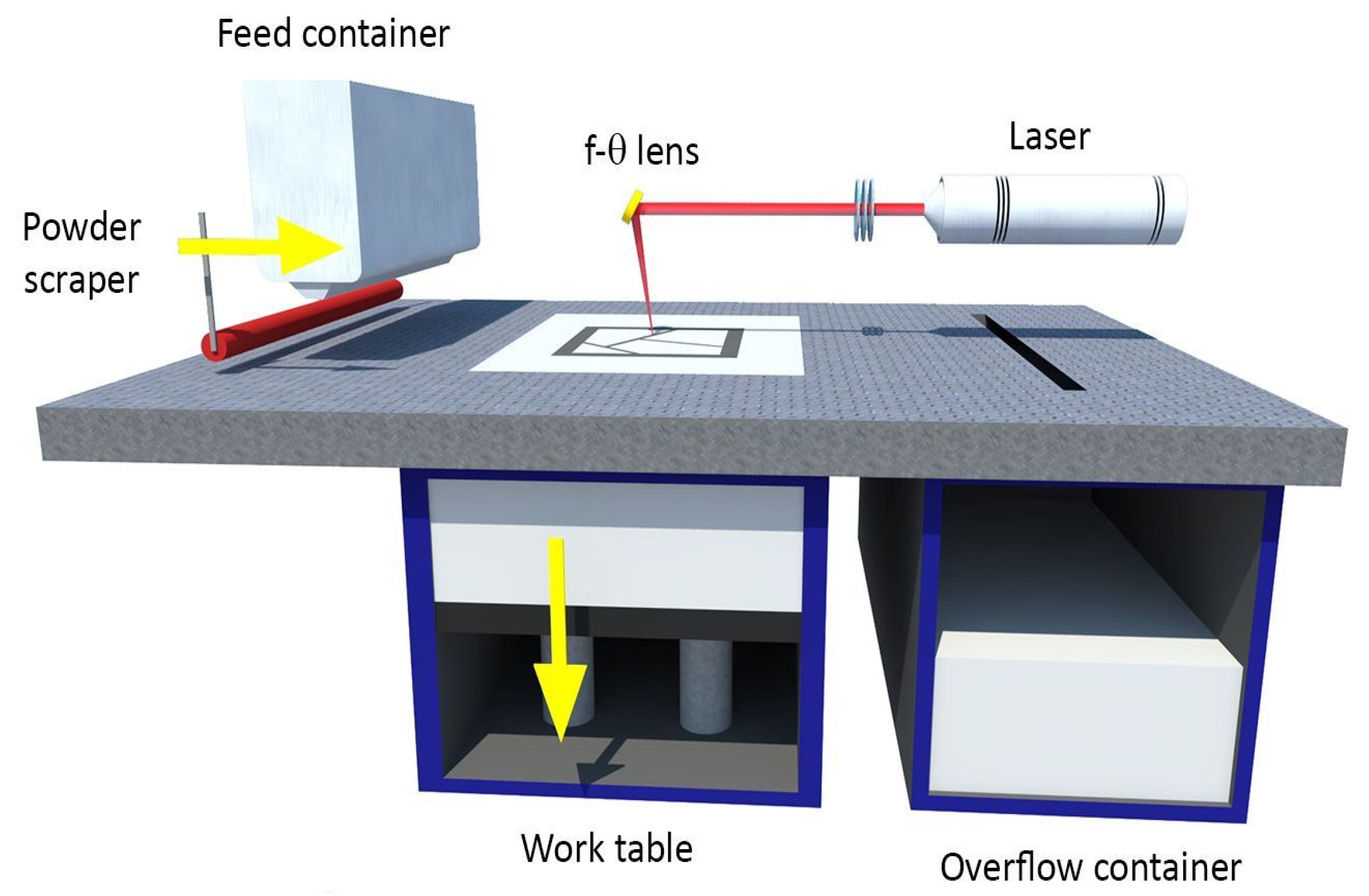
As it was previously indicated, additive technologies play an important role [
77,
136,
202,
300,
301,
302,
303,
304,
305,
306,
307,
308,
309,
310,
311,
312,
313,
314,
315,
316,
317,
318,
319,
320,
321,
322,
323,
324,
325,
326,
327,
328,
329,
330,
331,
332,
333]. They rely on joining together layer by layer of properly prepared powders or liquids, thin fibers, and sometimes in the form of a rolled role of metals and alloys, ceramics, and polymeric materials. Additive technologies are currently very popular in many applications in various industrial sectors [
135,
266,
271,
278,
279,
281,
283,
290,
312] in the photovoltaic industry [
285,
295]. Additive technologies also find numerous applications in medicine and medical industry, among others, for planning operations by producing models of anatomical organs, for epitheses, e.g., of the eye, nose, ear, taking into account the individual anatomical features of the patient [
232,
284,
286,
288,
289,
293]. Additive technologies are also used to produce scaffolds with a porous structure corresponding to the anatomical shape of a natural organ [
194,
197,
209,
233,
234,
241,
262,
265,
287,
292,
294,
316]. Stereolithography (SLA) [
135,
202,
334,
335,
336,
337] and selective laser sintering (SLS) [
2,
3,
80,
193,
194,
195,
196,
197,
198,
199,
200,
201,
202,
219,
224,
243,
244,
245,
260,
262,
263,
264,
265,
267,
270,
274,
277,
280,
282,
293,
338,
339,
340,
341,
342,
343,
344,
345,
346,
347] (
Figure 10) and selective laser melting (SLM) [
202,
225,
261,
264,
266,
268,
269,
272,
273,
275,
276,
291] are wrongly treated as a separate group, although it is only a variation of the previous one in the case of sintering with liquid phase used in engineering and dental prosthetics [
2,
3,
80,
193,
195,
196,
197,
198,
199,
200,
201,
287,
294]. Selective laser sintering (SLS) is used to manufacture metal prosthetic restorations. SLA is used for the manufacturing of models and rapid prototyping and some polymeric temporary and mobile restorations.
Additive technologies greatly simplify the technological process as no molds or matrices are required. The product manufacturing in other processes, e.g., casting, powder metallurgy, or plastic working or other tools in the case of machining, requires considerable financial outlays and time to prepare the production. It is particularly burdensome in unit manufacturing, and, as a result, determines that in such cases, additive technologies are extremely competitive [
202,
203]. However, it is necessary to make supports that attach the manufactured product to the work table. At the end of the process, the supports are cut off, and the product surface is processed by grinding or sanding.
In a large number of cases, additive technologies are complementary to other traditional technologies, so the latter still has a non-threatened position. Those technologies are considered as conventional, but now also require very advanced computer aiding and are usually highly automated and computerized. It should be noted that it is not currently and in the foreseeable future to eliminate those traditional technologies by replacing them with additive technologies. That fact must be taken into account in the current model of industrial development.
The classification of technological machines corresponds to the classification of technological processes to enable their implementation (
Figure 11). Cyber-physical systems (CPS) ensure that those machines communicate with other smart components, as well as with products via the Internet of things (IoT) [
22,
53], and create digital twins as a virtual copy of the physical world. The existing Industry 4.0 model includes nine technologies [
15,
18,
19,
20,
21,
25,
26,
27,
28,
29,
30,
31,
32,
33,
34,
35,
36,
37,
38,
39,
40,
41,
42,
43,
44,
45,
46,
47,
48,
49,
50,
51,
52,
53,
54,
55,
56,
57,
58,
59,
60,
61,
62,
63,
64,
65,
66,
67,
68,
69,
70,
71,
72,
73,
74,
75,
76,
348]. The industrial Internet of things [
22,
27,
29,
32,
39,
41,
43,
45,
47,
66], big data sets [
55,
57,
59], cloud computing for data processing [
35,
36,
62] simulations, self-learning processes, and artificial intelligence [
26,
62] are used. The existing Industry 4.0 model also includes autonomous robots, horizontal and vertical systems integration, cybersecurity, additive production, and augmented reality [
348]. However, the model should be supplemented, as previously mentioned, with engineering materials, living and bioengineering machines, and other technology groups, in addition to additive technologies (
Figure 12).
The Industry 4.0 system is based on smart factories [
51,
55] developing smart production. Smart factories use the embedded cyber-physical system and smart exchange data through smart networks connecting value creation modules with smart factories. Comprehensive engineering includes connections of stakeholders (clients, employees, or suppliers), products, and production machines, which are connected through the exchange of data from a virtual network with the participation of cloud computing [
35,
36,
62]. Identification systems, including radiofrequency identification (RFID) chips and quick reference codes (QR), provide wireless identification and location of materials, intermediates, and products in the value chain. The actuator system using the collected data in real-time enables products, people, or product changes.
A similar situation applies to medicine and dentistry, in particular, to technical aiding centers for medicine and centers for the production of prosthetic restorations. Well-known and used tools in the area include digital documentation, online prescriptions, digital X-ray tomograms and photos, online media marketing, patient registration and treatment progress software, and the use of cloud storage [
93]. The Dentistry 4.0 includes, among others, electronic medical records, digital patient records, diagnostic information, including 3D imaging using cone-beam computed tomography CBCT and intraoral and optical scanning, electronic development of treatment plans, software improved workflow tools, and increasingly available CNC milling and additive technologies, such as stereolithography and SLS. With regard to the development of Dentistry 4.0, all elements of the technological platform of the holistic augmented Industry 4.0 model regarding prosthetic and implantology dental engineering restorations are relevant, both in clinical practice and the production phase. Therefore, Dentistry 4.0 model includes digitization and computerizations of the design and manufacturing processes of prosthetic restorations for the use of cloud computing. The system contains biomaterials, as well as engineering design of prosthetic restorations and technologies for their production, including additive technologies, as well as machines and devices and supported cyber-IT systems. The issue of Dentistry 4.0 has been presented in the next subchapters of this paper.
4. General Characteristics of the Dentistry 4.0 Stage of Design and Manufacture of Prosthetic Restorations
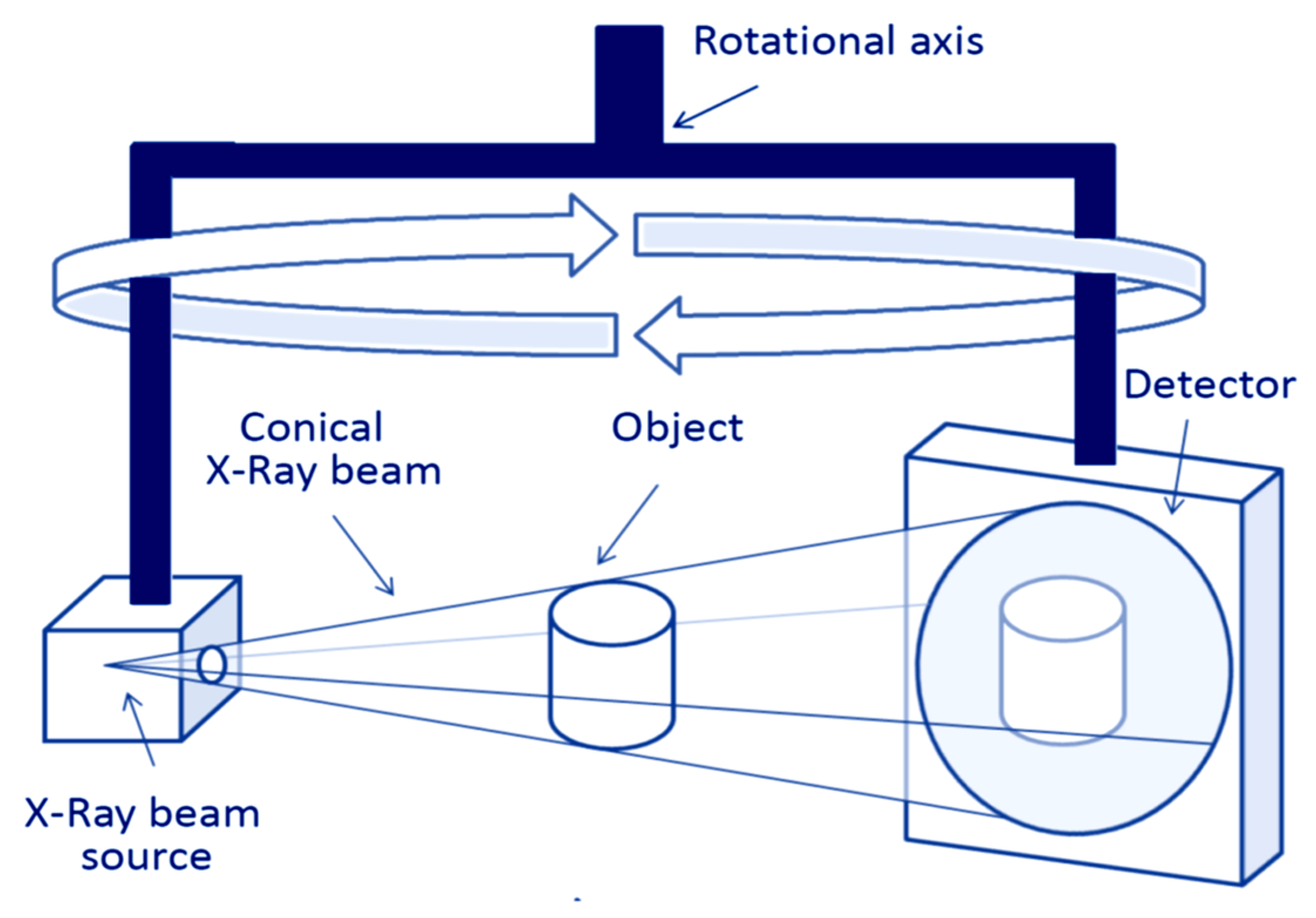
Dentistry 4.0 is the imperative of the moment in modern dentistry and, at the same time, a unique opportunity for its development. A significant determinant of the development is the increased awareness of dentists regarding the need to use the model and the formation of a new generation of dental engineers. In addition to knowledge of the latest manufacturing technologies using appropriate machines, their competence also includes perfect IT preparation. It is not only about the ability to program and use advanced IT tools but also the use of cloud computing, the Internet of things, augmented reality, and medical imaging techniques, including cone-beam computed tomography (CBCT). It also requires knowledge of the appropriate software to connect computer networks of dental clinics and prosthetic restoration manufacturing centers. CBCT tomography (
Figure 13) uses divergent cone-shaped X-rays for medical imaging. The scanner rotates around the patient’s head, and, at that time, about 600 different images are recorded, each of which contains a set of volumetric data after a single rotation by another 200 degrees. Scanning software creates a digital volume composed of three-dimensional voxels of anatomical data, which are collected, reconstructed, and visualized by specialized software. The importance of this CBCT method is increasing.
Currently, the traditional relationship between a dentist and a laboratory or a center for the production of prosthetic restorations is changing. To date, the dentist has planned treatment and, according to his/her plan, commissioned the manufacturing of prosthetic restorations. The qualitative change is currently taking place. A dentist still supervises the treatment and is making the diagnosis of the patient’s teeth state and registration of the situation of the teeth with the use of CBCT tomography. However, the planning, designing, and manufacturing of the prosthetic restoration are in the competence of the dental engineer cooperating with the dentist. It ensures that the highest possible quality standards and narrow dimensional tolerances are achieved. In many cases, it requires the design of a surgical guide, which, due to the diagnosis of the actual state of the bony processes of the maxilla and the mandible, allows the correct execution of holes in which implants and/or implant-scaffolds should be fixed. The idea of a digital twin gives a chance to do virtual experiments during the design and digital verification of the prosthetic restoration. On this basis, a real stereolithographic (SLA) model of rapid prototyping can be made in order to determine the correctness of short-circuit height in the articulator. In this way, the roles change because the competence of the dental engineer cooperating with the dentist undergoes the full scope of design and manufacturing of prosthetic restorations. The dentist invariably supervises the entire treatment from the medical side and assembles the manufactured prosthetic restoration in the patient’s mouth.
The relations according to the Dentistry 4.0 concept between the medical tasks of the dental clinic and the design and manufacturing capabilities of the manufacturing center for the design and manufacturing of dental prosthetic restorations concerning the patient’s expectations are schematically shown in
Figure 14. Significant progress has now been made compared to the previous historical Dentistry 3.0 stage, when, in addition to the evident improvement in conservative dentistry, X-ray evolution occurred in the diagnosis of patients’ dentition [
349]. In contrast, the improved level of oral care with a significant reduction in the cost of implant-prosthetic treatment and, in particular, the production of prosthetic restorations is associated with 3D imaging manifested in the use of CBCT, data processing using cloud computing, and personalization of additive technologies. The 3D printing, mainly SLS, constitutes the essence of the current very advanced stage of Dentistry 4.0. The approach appropriate for the Dentistry 4.0 stage ensures business efficiency. Digital technology affects the minimization of the cost of manufacturing personalized prosthetic restorations in some cases by more than 70% compared with conventional methods [
349].
The application of the Dentistry 4.0 idea also reduces the time spent on the design and manufacturing of the prosthetic restoration. It is also associated with a reduction in the amount of time spent by the dentist and medical staff, and what is extremely important, the patient’s time, logistics, and the time and expenditure required to match prosthetic restorations during necessary tests with the participation of the patient. At the same time, it is one of the reasons for reducing the total costs of the procedure, enabling the production and implementation of non-standard restorations during one visit to the dentist [
349]. However, prior to the use of CBCT tomography, it requires the visualization of the state of teeth [
349]. The attributes given correspond to the standards of the dental version of the smart factory. A prerequisite for the success of this modern approach and, at the same time, its opportunity is to use networks and other computer tools to significantly extend the reach and integration of the network of suppliers, cooperating dental clinics, and patients. Undoubtedly, the determinants of the possibility of implementing the Dentistry 4.0 idea are the investment limitations of the technological machines and computer software used and very high costs, incomparably greater than in the case of using conventional technologies, when the costs are even several dozen times lower. Both the horizontal and vertical technological line integration system in intelligent centers for the production of dental prosthetic restorations and the cyber-physical system ensures the creation of a value chain. Sensors in technological machines make the identification and location of the factors, creating value, things, and people, and the system for monitoring the processes of generating and collecting smart data in real-time takes into account changes in technological processes, people, and products and activates executive devices.
The concept of “digital twins” of the physical world reduces the risk of design and technological errors. Data collection enables the use of artificial intelligence tools for virtual experiments and simulations. Network production integration systems in various areas are related to intelligent implant connections and prosthetic restorations as products with machines and people. In essence, those centers are connected to many dental clinics with cooperation bonds, and cloud computing can be used more and more commonly to send electronic patient data, including CBCT images. The information obtained and collected in this way creates the conditions for the design of prosthetic restorations, models, and surgical guides by means of computer-aided design (CAD) and production planning using numerically controlled CNC machines, machines for SLS additive manufacturing, and coating of internal surfaces with ALD methods.
Table 9 lists materials used in dental prosthetics as an example of the authors’ own experience.
The Dentistry 4.0 approach requires the dental engineer to start treatment planning with the dentist, who diagnoses the condition of the teeth based on the CBCT tomogram. The assessment of the patient’s teeth condition by a dentist allows the teeth to be qualified for removal. The dental engineer and the dentist who is responsible for treatment are planning the type of prosthetic restoration and how to mount it on existing teeth or planned dental implants. In the case of restorations based on the patient’s own teeth, the dental engineer can prepare wax-up or mock-up restorations in order to agree with the patient’s assumed aesthetic effect. Performing those works with PMMA allows imitation of restorations faced with composite or porcelain and allows the dentist to make corrections. Preparation of the pillar teeth with the degree enables verification of the position of prosthetic restoration in the oral cavity and thus ensuring the correct occlusion position. In the case of restoration mounted on implants, the dental engineer prepares surgical guides, determining the placement of the implants in cooperation with the dentist and then, using the CAD program, determines their final positions in the mouth. In the case of individual implants, the teeth are qualified for extraction, a project of a copy of the tooth is made by reverse engineering methods using CAD software, and then the implant is made using the SLS method. An implant insertion surgical guide and customized instruments are also manufactured. In all those activities, the dental engineer works closely with the dentist. The associated clinical activity places high demands on dental engineering in all related areas from the selection of engineering materials to manufacture. It is necessary to ensure repeatability and adequacy of prosthetic restorations, including implants, to the patient’s individual anatomical features. The use of conventional technologies is currently unacceptable, including related to the production of gypsum models and subsequent casting. Fully digitized technologies are highly desirable and require virtual intraoral scans. Own tests have shown that the inaccuracy of impressions is about 0.3%, dimensions differing by about ± 0.05–0.1 mm. The tested masses include polyether and polyvinyl siloxane masses—the additive silicones used for impressions reflecting the patient’s teeth. The accuracy of the working model can be achieved by increasing the volume of gypsum during setting by about 0.08%. The change in the volume of mapped teeth on the working model is –0.2% to 0.4%.
Ensuring the required accuracy needs eliminating factors that increase the inaccuracy of the working model. It is possible to scan an impression directly from the impression tray using a prosthetic scanner or based on the results of scanning with an intraoral scanner. The accuracy of 3D models made with an intraoral scanner varies in the range of 50–70 μm and is close to the maximum accuracy of CNC numerically controlled milling machines. However, the technology still does not allow performing repetitive scans of the entire arch. In the case of casting methods, accuracy is included in a wide range and depends on many factors. As a result, the inaccuracy of the procedure of duplicating the teeth to the working model reduces the accuracy of the prosthetic restoration significantly.
To eliminate the lack of dimensional inaccuracy of manufactured prosthetic restorations, computer-aided design/computer-aided manufacturing CAD/CAM and full digitization of the manufacturing technologies [
91,
171,
176,
178,
185,
187,
192,
349,
350,
351,
352,
353,
354,
355,
356,
357,
358,
359,
360,
361,
362,
363,
364,
365] are used. The manufacturing of metal foundations is increasingly used by machining with milling Co–Cr alloys, titanium alloys, as well as prefabricated ceramics, including oxides zirconia and alumina, and reinforced with lithium disilicate, as well as poly (methyl methacrylate) (PMMA) and wax. Additive manufacturing technologies, including selective laser sintering, have a wide area of use, including dental engineering of computer-aided design/manufacturing technology [
27,
29,
178,
180,
201,
224,
244,
245,
260,
262,
264,
265,
267,
269,
277,
280,
293,
366,
367,
368,
369,
370,
371].
An essential goal of using CAD technology in dental prosthetics is to increase the accuracy of the production process [
349,
350,
351,
352,
353,
354,
355,
356,
357,
358,
359,
360,
361,
362,
363,
364,
365,
370,
372,
373,
374,
375,
376,
377]. One of the essential criteria for the long-term success of prosthetic restorations [
378,
379,
380,
381,
382] is the highest possible compatibility of prosthetic restorations with the patient’s anatomical features. Digitization of the prosthetic restoration is carried out in one of two ways using extraoral or intraoral scanners [
383,
384,
385,
386,
387,
388,
389,
390,
391,
392,
393,
394,
395,
396,
397,
398,
399,
400,
401,
402,
403,
404,
405,
406,
407]. The first one consists of the extraoral scanning [
361,
364] of a traditional classical impression. Extraoral scanners use three main methods, including using laser radiation, structured light, and direct contact. Optical scanners using laser radiation and structural light do not require physical contact, do not affect the density and quality of the surface of the scanned object [
361], and usually provide a shorter scanning process than contact scanners [
355]. Those scanners do not fully eliminate the impact of surface gloss, brightness, and other optical properties of the scanned object [
363]. The second way to digitize a prosthetic restoration is to make a digital prosthetic model by scanning dental arches using an intraoral scanner [
387,
389,
401]. Both types of scanners using CAD software, in turn, allow for the production of a physical model using CAM technologies using milling or additive 3D printing technologies and appropriate engineering materials, including ceramics, polymers, or metals [
388,
390,
392,
393,
394,
405].
A radical turnaround in clinical procedures and in the way of technical preparation of implantation using CAD/CAM methods is worked. They include the authors’ own methods [
3,
206,
207,
208,
210,
212,
223,
244,
245] regarding data acquisition by means of cone-beam computed tomography (CBCT) in planning and performing implant prosthetic treatment and also in endodontics and orthodontics [
408,
409,
410,
411,
412,
413,
414,
415,
416,
417,
418,
419,
420,
421,
422,
423,
424,
425,
426,
427].
Using CAM software, it is possible to manufacture precisely the prosthesis with an accuracy of up to 0.05 mm [
136]. CAD/CAM techniques can also be used to prepare temporary restorations made of acrylic materials for intraoral placement. The widespread use of CAD/CAM methods and the full digitization of manufacturing technology create broad premises for the successive introduction of the assumptions of the augmented holistic Industry 4.0 model among manufacturing centers and other dental prosthetics manufacturers.
5. Examples of Digitization of the Design and Manufacture of Prosthetic Restorations and Dental Implants under the Dentistry 4.0 Model
This subchapter presents, for example, the authors’ own projects regarding the application of the augmented holistic Industry 4.0 concept at the dental prosthetic restoration center according to idea Dentistry 4.0.
Table 10 summarizes how the requirements of the technological platform of this model are met in the case of producing fully personalized prosthetic restorations and made on-demand.
The first of these examples concerns digitization under the Dentistry 4.0 model related to the manufacturing of dental bridges using CAD/CAM design technology and manufacturing using 3D printing in SLS technology. When designing a bridge or crown on a Co–Cr alloy or titanium framework, attention should be paid to the arrangement of the abutment teeth and ensuring adequate distribution of occlusal forces on the alveolar ridge while providing an even load on the abutment teeth. In particular, in the case of long bridges, including circular bridges, it is crucial to ensure the right mass of the manufactured element while ensuring high accuracy that will preserve the expected strength of these elements. The most crucial step in the procedure for producing a prosthetic restoration is to provide the highest possible efficiency in the reproduction of the oral situation. According to the authors’ research, the best results are still achieved when performing a traditional impression using silicone impression masses and performing a 3D scan directly from the impression spoon [
160].
The procedure ensures that the prosthetic elements are kept to the highest position with the minimum distance for the introduction of cement connecting tooth tissues with prosthetic restoration while maintaining the most upper marginal tightness for works in which the preparation is performed with the degree. It is crucial to ensure the highest strength of the designed element, in particular, so that the cross-sections of the connectors maintain the appropriate assumed surface area. Currently, SLS laser sintering of titanium and Co–Cr alloy powders is increasingly used in the manufacturing of prosthetic restorations. The technology is gaining recognition because it allows reducing the time necessary to manufacture the foundation by three times and, at the same time, allows to increase the accuracy of the manufactured element relative to the design, which reduces weight and post-production time (
Figure 15).
The dentist conducting the treatment performs the preparation of the teeth with the formation of a degree and maintaining the parallelism of all pillar teeth (a). Dental engineer using a scanner that allows making a scan of the impression spoon makes a virtual model of teeth along with models of posts (b), which will be needed to make appropriate faced porcelain. The designer must then consider pillars. Then, a prosthetic restoration project is created using libraries, which are then verified and corrected by the designer (d). The finished model (e) is transferred to the computer-aided manufacturing (CAM) software and placed on the platform where then the supports (f) are designed. After manufacturing the foundation on the SLS device, the ceramist technician performs the characterization of the foundation by forming teeth (g). The ready effect of these efforts is visible in the picture (h).
The second example concerns the digitization under the Dentistry 4.0 model related to the planning, design, and manufacturing of prosthetic elements and the surgical guide in the case of immediate implantation in place of the planned tooth extraction [
81] (
Figure 16). The entire design process is performed on the basis of a 3D tomogram of the patient obtained in the CBCT tomography (a) available in many implantology clinics. A digital twin of the patient’s entire dentition is created. After the tomogram is converted to a 3D digital model, the bone base models and intraoral scans (b) are assembled, and the tooth (c,d) is separated, which will be removed. It is then removed from the model, and the remaining model after this operation is a virtual model of the situation after the really successful and safe removal of the tooth by the dentist (e). Then, in consultation with the attending dentist, the dental engineer plans the optimal location of the implant in the alveolus (f). After accepting the place, the implant guide (g) is designed. Then, a working model with the implant analog implemented is created. Using a typical CAD prosthetic design software, one can design an individual abutment (h), filling the extraction socket. The design of the connector is transferred to the CAM software, and then the individual abutment is made by milling using a CNC milling center. Further, it is necessary to design, also in a typical way, the design of the PMMA temporary crown (i). The crown is made in CNC technology using a milling machine.
The presented procedure is an avant-garde, authors’ own method of performing the entire immediate implantation procedure, which is designed solely on the basis of data obtained in digital form. The dentist proceeds to medical procedures already having all the prosthetic elements necessary to perform the treatment (surgical guide, individual abutment, temporary crown). Thanks to the procedure, after its completion, the patient comes out with the tooth replaced with a fully useful prosthetic restoration. In addition, such a procedure may be 60% shorter compared to the same procedure performed in the traditional way using impression materials.
The third example concerns the preparation of a surgical guide for implantation of four implants, which will be the basis for the restoration of the entire arch using a permanent hybrid construction, which can be pulled out by the patient for hygiene (
Figure 17). The surgical guide is made for implantation of all implants planned for placement. It is prepared for introducing first of all pilot drill, although it is also possible to replace guide sleeves with sleeves for subsequent drills. The exact surgical guide for implant must be prepared based on detailed data on the volume of bone base obtained from the 3D tomogram, which is performed before planning the procedure. A dental engineer using CAD software creates a bone base model. Throughout the entire design process, it is possible to verify the accuracy of the model, as shown in the picture (a1–a4). Then, the bone base and intraoral situation models are assembled. The correct connection of the intraoral scan with the bone base model is significant for the success of the whole procedure.
Next, the bone base and intraoral situation models are assembled. The correct connection of the intraoral scan with the bone base model is significant for the success of the whole procedure. It is necessary to make a scanning plate that is visible on the 3D tomogram pattern (reflects X rays) (b). The CBCT pattern should be performed with this plate. Using the CAD software using the 3-point folding method, the position of soft tissues relative to the bone base can be mapped. A dental engineer, in consultation and under the supervision of a dentist, plans the placement of implants (c). The thickness and distribution of the cortical layer and spongy bone base are verified, and the optimal placement of the implants is planned to take into account the anatomy of the appendix and their optimal location, taking into account the position relative to the mandibular nerve canal. Next, the surgical guide is made using 3D SLA printing technology. Using advanced 3D printing technology allows ensuring tight adherence of the surgical guide to soft tissues. It is essential because the surgical guide during the procedure is fixed only on soft tissues. The dentist only makes a small incision of soft tissue only around the holes through which the implant will be inserted. Those holes can be made in soft tissues using a dedicated drill with a diameter close to the width of the implant being inserted. Thanks to that, recovery after the procedure is mild. The assembly model of the intraoral model and bone base model is shown in the photo (d).
The quick surgical guide printed in SLA technology with individually designed guide sleeves is shown in
Figure 17e. After drilling the holes using the surgical guide, a CBCT control test with control pins (f1–f4) is carried out, confirming the correct placement of the holes in accordance with the plan presented in the project.
6. Summary
Based on the extensive literature review and selected results from the authors’ own professional dental engineering practice, the scope of the modern idea of Dentistry 4.0 regarding technical aiding for dental prosthetics is indicated as part of the overall concept of the currently highest stage of Industry 4.0 of the industrial revolution. The progress of civilization depends on many factors associated with numerous inventions of humanity by inventing the steam machine recognized as the Industry 1.0 stage to the present stage of very advanced computerization, robotization, and automation. Since the progress is continuously being made, the UN has set 17 sustainable development goals (SDG), and several strategic programs have been developed, including the Society 5.0 program in Japan and Industry 4.0 in Germany, adopted in the European Union and widespread in many countries. While the Japanese program includes an extensive concern for the well-being of people, the German program mainly focuses on the development of industry, and both are based on very advanced computer-aiding using cyber-physical systems. The existing Industry 4.0 model is only an IT element of industrial development and, therefore, had to be augmented and supplemented. The authors of this paper have developed a full holistic model of technological development at the Industry 4.0 stage. The technology platform of the model includes four aspects, including materials, manufacturing processes, and technological machines, as well as their progress, and as the fourth element regarding cyber-information systems and the extensive use of information technology. Those issues have been generally discussed in this paper. It has been noted that this holistic augmented model has universal significance and can be used both in large manufacturing organizations in various industries, e.g., automotive, space, aviation, electronics, household appliances, and also in micro, small, and medium enterprises. Therefore, the possibility of adapting all assumptions of this universal model to the issues of designing and manufacturing prosthetic restorations as well as the cooperation of centers and laboratories for the manufacturing of those restorations with a network of generally private dental clinics has been considered in detail. An analysis of interrelationships between entities participating in the prosthetic treatment process has been made, paying attention to the relationship between patient expectations, design, and manufacturing capabilities of dental prosthesis restoration centers and the medical tasks of dental clinics. The basis of the considerations is a detailed literature analysis of diseases of the human stomatognathic system. The prevalence of caries and methods of its treatment have been pointed out, including endodontic, which allows the patient to leave his/her cured teeth for a long time in the mouth. Caries is the leading cause of dental extraction, and, in addition to periodontal disease and congenital disabilities, it mainly determines the need for prosthetic treatment. The classification of dental deficiencies has been made, and the possibilities of prosthetic treatment have been indicated along with the designation of prosthetic restorations in the event of partial or complete loss of natural dentition. Advanced prosthetic supplements offered by modern dentistry allow rebuilding all types of missing teeth. In the case of complete toothlessness, implants, permanent, and removable restorations are used for such a purpose. In the case of partial deficiencies, in particular, bridges based on their own teeth or implants are installed. It is also possible to manufacture bridges covering the full arch. In each case, dental prostheses are individually designed and manufactured for a specific patient and can be mounted alternatively on healthy or endodontically treated their own teeth or dental implants. In modern dentistry, cylindrical implants with a spiral surface are widely used. In several centers, independent work is also carried out, including own work carried out by the authors of this paper, on the introduction of individual implants produced using information obtained using cone-beam computed tomography (CBCT). Authors’ own research indicates a change in the traditional relationship between a dentist and a dental engineer, which requires engineering knowledge in the field of biomaterials used, manufacturing technology, extensive knowledge in the field of IT support in design and manufacturing, as well as networks enabling internal integration and with numerous external stakeholders and with cloud computing.
The methodology in those cases is based on close cooperation between the implant dentist responsible for diagnosis and treatment and the dental engineer. His/her tasks include determining implantation areas, creating a three-dimensional model of the bone base based on a CBCT tomogram registered by the dentist and its connection with the three-dimensional model of the dentition and soft tissues in the oral cavity, prepared based on impression material, and most preferably a three-dimensional scan directly from the oral cavity. Those activities enable the design of prosthetic reconstruction and implant placement of one or several implants by planning technological holes for guiding the pilot drill to the bone based on a specific implant system and finally implementing the final design. This is necessary to design and create the surgical guide. Therefore, the dentist diagnoses the patient’s condition, records the state of dental health using CBCT, and all prosthetic reconstruction is planned, designed, and manufactured by a dental engineer in consultation with the dentist while maintaining the highest possible quality standards and very narrow dimensional tolerances. Finally, the dentist assembles the manufactured prosthetic restoration in the patient’s mouth in full accordance with the precise plan designed by the dental engineer using the prosthetic restorations he/she made and surgical guides. The procedure also enables virtual experiments at the design stage and digital verification of the designed prosthetic restoration, in line with the idea of a digital twin. Besides, it is possible to simultaneously make a model using rapid prototyping by stereolithographic (SLA) method and check the correctness of maintaining the correct fault height using an articulator. The presented approach is a radical turnaround in both clinical procedures and engineering techniques of implant preparation using computer-aided design and CAD/CAM manufacturing methods and AM additive manufacturing technology, including mainly selective laser sintering and stereolithography. Selective laser sintering technology also allows for the production of entirely innovative implant-scaffolds developed by the authors. They are built of a solid zone, typical of previously used implants, and a porous zone that acts as a scaffold, as hybrid connected into a uniform whole. The pores of implant-scaffolds are internally covered with bioactive thin atomic layers deposition (ALD), e.g., TiO2 or Al2O3, providing favorable conditions for the proliferation and growth of living cells inside the pores of the device after implantation. The concept of hybrid multilayer engineering-biological composites developed by the authors, which is at the stage of in vitro and in vivo research, is a much more technologically advanced version of the concept. Surgical guides for the controlled making of holes in the bones are produced by methods of additive manufacturing (AM) or subtractive manufacturing by machining on a computerized numerical control (CNC) milling machine. For technological reasons, the surgical guide can be made of PMMA, in which pilot sleeves are filled with steel or titanium tubes dedicated to the selected implantation system. The authors’ own designs illustrate the practical application of the augmented holistic concept of Industry 4.0 for the prosthetic restoration center, called Dentistry 4.0. The first example is the manufacturing of dental bridges using solid metal discs milling technology. Alternatively, their manufacturing is made with selective laser sintering (SLS) using metal powders hybridized with mechanical treatment using a center numerically controlled (CNC). The additive manufacturing by stereolithography (SLA) technology has been used for manufacturing the surgical guide for implantation of four implants for the assembly of a full arch bridge. Thanks to digital technology, it is possible to reduce the cost of manufacturing some prosthetic restorations compared to conventional methods. The overall conclusion of the research and analyses carried out indicates that on the one hand, unavoidable, and on the other hand, extremely beneficial, mainly due to maintaining very high-quality standards and strict dimensional tolerances, is the implementation of the idea of Dentistry 4.0 in accordance with the assumptions of the authors’ own holistic Industry 4.0 model.