1. Introduction
Cephalosporins, which belong to the group of semi-synthetic β-lactam antibiotics, have their origins as early as in the middle of the 20th century. The first research work on their use in the therapeutics was carried out at the turn of the 19th and 20th century. The discoverer of cephalosporins is considered to be the Italian scientist Giuseppe Brotzu (1895–1976), professor and microbiologist of the Medical Faculty in Cagliari (Sardinia). In 1945 the scientist became interested in people who swam in rivers polluted with faeces or consumed shellfish fished from them. These people did not get sick, while in other parts of Italy, there was a typhoid pandemic—at the time known as abdominal typhus. On this basis, Brotzu hypothesised that these sewage systems probably contain microorganisms that inhibit the growth of pathogenic intestinal bacteria—
Salmonella typhi—that can prevent the spread of typhus [
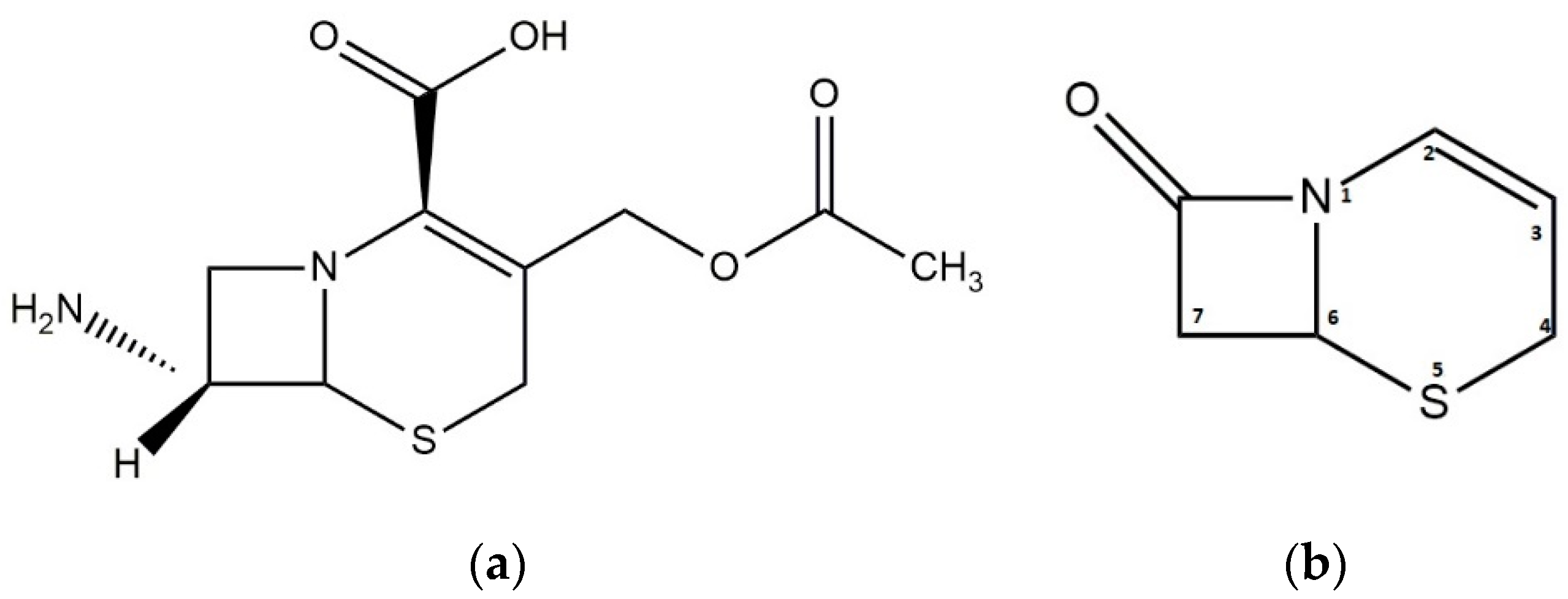
1]. In 1948, together with Howard Florey, they discovered that a strain of the fungus can produce seven antibiotics—five varieties of cephalosporin P, N and C. The latter is considered to be the most important, as it is on its basis that all the cephalosporin antibiotics used today are created. Despite its considerable advantages, such as high resistance to staphylococcal penicillinase enzyme and hydrolysis in an acidic environment, like the rest of the natural penicillin, it has unfortunately not been used in the therapeutic field due to its low activity. For this reason, we are currently using its semi-synthetic derivatives obtained from 7-aminocephalosporic acid, which was formed as a product of the hydrolytic decomposition of cephalosporin C. The basis for the structure of cephalosporins is the aforementioned 7-aminocephalosporic acid, which contains the characteristic Δ2-cephem system (
Figure 1) [
2].
Cephalosporins belong to the well-tolerated group of antibiotics, which is extremely diverse and can be grouped into five classes in terms of their activity. The classification into a particular generation is based on the differences in action: bactericidal effect on Gram-negative bacteria (including
Bacteroides and Gram-positive anaerobics),
Proteus,
Pseudomonas, reaching the cerebrospinal fluid and sensitivity to β-lactamases. It can be assumed that a lower generation has greater activity against Gram-positive bacteria, and a higher generation has greater activity against Gram-negative bacteria. There are some exceptions, such as cefepime, which is included in the fourth generation, and its activity against Gram-positive bacteria is comparable to that of the first generation, and against Gram-negative bacteria is equal to the third generation [
3]. Currently, in a hospital and out-of-hospital treatment, there are infections caused by resistant strains of bacteria that are insensitive to methicillin. These are mainly
Staphylococcus aureus,
Streptococcus pneumoniae,
Enterococcus spp. The use of similar chemotherapy regimens varies according to the type of hospital or out-of-hospital infection, as using the same regimens is not equally effective. Therefore, the need to look for new antibacterial compounds that will be able to overcome the existing resistance mechanisms is growing [
4]. The new group of cephalosporin antibiotics includes the fifth generation. Unlike the fourth generation, these compounds have a broad spectrum of effect on Gram-positive bacteria and an extended spectrum of resistance to methicillin, i.e., MRSA and other resistant enterococci, mainly VRSA (
S. aureus resistant to vancomycin) [
5].
An example of generation V cephalosporin is ceftaroline. It exhibits a wide spectrum of activity against Gram-positive and Gram-negative pathogens and most importantly it shows activity against VISA (
S. aureus strain moderately resistant to vancomycin), hVISA (precursor of VISA), MRSA and VRSA. It has been proven effective against bacterial pathogens of the respiratory system, e.g.,
S. pneumoniae [
6]. Ceftaroline is made from the prodrug ceftaroline fosamil. The indications for the use of this antibiotic are the complications caused by skin and soft tissues infections and community-acquired pneumonia [
7]. The difference between ceftaroline and ceftobiprole is demonstrated in terms of their resistance to drug degrading enzymes, including β-lactamases. Ceftobiprole possesses high resistance, while ceftaroline has limited activity on Gram-negative bacteria, while the activity of ceftobiprole can be compared to fourth-generation antibiotics [
8]. Besides ceftobiprole and ceftaroline, it is worth mentioning the latest fifth-generation semi-synthetic cephalosporin, ceftolozane. This drug was approved in 2014 by the FDA in combination with tazobactam, and is used in abdominal and urinary tract infections. In 2019, the combination of these drugs was authorised for hospital treatment of bacterial pneumonia, and is effective against the organisms causing these infections, such as
Pseudomonas aeruginosa [
9].
Ceftobiprole was first registered and authorised for marketing and hospital treatment in Canada in 2008 under the name Zevtera. The next countries to use this medicine were Switzerland and Ukraine. It is a pyrrolidine cephalosporin (
Figure 2a), which was developed in cooperation between Johnson&Johnson and Basilea Pharmaceutica. This compound is obtained by dissolving its prodrug in water, medocaryl ceftobiprole sodium salt (
Figure 2b). Obtaining a derivative in the form of salt is necessary because ceftobiprole itself is insoluble in water. The given salt is obtained during a process consisting of three stages of synthesis. The metabolism of medocaryl ceftobiprole is dynamic. Salt is converted to active ceftobiprole, CO
2 and diacetyl using enzymes called plasma esterases. A very small part of the prodrug is converted to an open ring form. This fact can be confirmed by a urine test, as it is mainly this way that the active drug is eliminated (up to 83%) [
4].
The mechanism of ceftobiprole’s action is based on combining it with the penicillin-binding proteins (PBP), thus disturbing the synthesis of the cell wall (peptidoglycan). This leads to inhibition of cell growth and ultimately to the death of bacteria as a result of the osmotic activity or autolytic enzyme activity. It is related to specific proteins such as PBP2a in methicillin-resistant
staphylococci, and PBP2b and PBP2x in β-lactam-resistant
pneumococci [
10,
11,
12]. The structures of cephalosporins of generations I–IV were not able to form a suitable bond with PBP2a. It was only the presence of a hydrophobic chain located at C3 carbon in the ceftobiprole that facilitated the binding and conformational changes in PBP2a, thanks to which it was possible to create an acyl-enzyme complex. The resistance of
S. aureus and other
staphylococci results from the acquisition and expression of mecA or mecC. These genes encode PBP2a, which is the protein that binds the penicillin. It shows a low level of affinity to β-lactams, thus preventing inhibition of cell wall synthesis [
13].
Unlike ceftriaxone, ceftobiprole has a strong effect on penicillin-resistant
S. pneumoniae (PRSP) via PBP2x protein. Thanks to interaction with PBP-type proteins, ceftobiprole also has high activity against other PBPS
staphylococci (PBP1, PBP3, PBP4). An example of affinity for PBP2 and PBP3 is the binding of ceftobiprole in
Escherichia coli [
14,
15].
The indication for ceftobiprole application is adult pneumonia (CAP—Community Acquired Pneumonia) and hospital-acquired pneumonia (HAP—Hospital Acquired Pneumonia), but excluding ventilator treatment [
16,
17]. Ceftobiprole is a broad-spectrum antibiotic which can be used against several bacteria in monotherapy. In 2015, the FDA authorised it to treat diseases such as lung and skin infections. Its efficacy has been demonstrated in two-stage, third phase clinical trials with pneumonia patients. It was recommended to administer the drug every 8 h in a 2 h infusion in a dose of 500 mg [
18]. The microbiological diagnosis of bacterial pneumonia is usually difficult to establish, so action must be taken empirically. In general,
S. pneumoniae is cited as the main cause of the disease in adults. To a lesser extent, infections are caused by
P. aeruginosa and
S. aureus (MRSA), which should definitely not be overlooked due to their resistance to antibiotic therapy. In hospital pneumonia, however, the most common cause of infection is
Enterobacteriaceae bacteria, such as
Klebsiella,
Enterobacter,
Serratia and only later
Pseudomonas and
Staphylococcus. Furthermore, these strains are resistant to many drugs, which underlines the seriousness of the situation in the case of the disease [
19,
20].
Ceftobiprole can also be administered to patients during the treatment of complicated skin and soft tissue infections. Based on information contained in the pharmacovigilance study databases in Europe,
S. aureus (37.5%) was the main agent of skin and soft tissue infections, of which MRSA was 22.8%.
P. aeruginosa,
E. coli and
Enterococcus spp. were the lesser causes of the disease, so a broad-spectrum antibiotic becomes an obvious choice of empirical treatment [
21]. The use of ceftobiprole is considered when the infections are severe and extensive, life-threatening, with a high content of methicillin-resistant
staphylococci; patients hospitalized are elderly with coexisting diseases, mainly cirrhosis B and C and haemodialysis; the patient is undergoing immunosuppressive therapy; there are pre-treated chronic ulcers with symptoms of infection; there are traumatic infections or surgical wounds [
22]. The efficacy of ceftobiprole has also been analysed in the pharmacotherapy of diabetic foot infection. It was used in the moderate to the severe stage without bone involvement. The most common cause of this disease was, as above, in skin infections,
S. aureus, while Gram-negative sticks such as
P. aeruginosa were less frequent [
23]. The in vitro ceftobiprole activity against anaerobic and aerobic isolates was investigated and compared with other antibiotics. It has been shown to have a wide range of effects on Gram-positive and Gram-negative aerobic and anaerobic bacteria. It is also more effective against Gram-positive aerobic bacteria than, e.g., cefepime, vancomycin, levofloxacin, ceftazidime or cefotaxime [
24]. Moreover, in comparison to vancomycin (vancomycin with ceftazidime), it was found that the average treatment time was shorter —8.7 vs. 9.5 days. During the study, a faster response to treatment was obtained when ceftobiprole was applied to the patient [
25]. Another indication for ceftobiprole application is infection from vascular catheters. Although treatment with ceftobiprole is beneficial, in the case of monotherapy, consideration should be given to whether it would not be better for the patient to use a combination of active glycopeptide against
P. aeruginosa. This is since, in recent years, we have observed a significant increase in the number of cases caused by Gram-negative bacteria, mainly the previously mentioned
P. aeruginosa and
E. coli. The cause of this condition may be a solid organ transplant, previous use of β-lactams, long hospital stays or endured surgery [
26,
27]. The last indication for pharmacotherapy is fever in patients hospitalised without septic shock or severe immunosuppression. Once the fever has occurred and before treatment begins, it is necessary to collect bacterial culture samples because the main cause of the fever may be venous catheters, followed by infections depending on co-occurring diseases or local epidemiology [
28].
Although ceftobiprole has no biological activity after oral administration, it shows similar pharmacokinetic properties on intravenous administration compared to other cephalosporins. The administered prodrug, ceftobiprole medocaril, is hydrolysed in the blood to active cephalosporin through esterases. As the drug is excreted only in the urine, the administered dose should be adjusted in persons with renal impairment or creatinine clearance [
29,
30]. It is easy to achieve optimal pharmacokinetic/pharmacodynamic (PK/PD) parameters in a 2-h infusion as the half-life period is more than 3 h [
31,
32]. The recommended dose infusion is 500 mg every 8 h, but linear pharmacokinetics are observed for a dose range of 125–1000 mg, which is not dependent on the time of administration. The balance is obtained already on the first day. In patients with healthy kidneys, there is no drug accumulation when supplied every 8 h. During the study, systemic exposure, the area under the curve (AUC) and maximum plasma concentration (C
max) on day one and day five were similar (AUC 90 ± 12.4 mg h/L and 102 ± 11.9; and C
max was 29.2 ± 5.52 mg/L and 33 ± 4.83). The systemic and renal clearance was also very similar. The half-life period t
1/2 on the first and fifth day was 3.3 ± 0.3 h and 3.1 ± 0.3 h, respectively. These results are consistent with data characteristic for β-lactam antibiotics, especially cephalosporins [
33]. The binding to plasma proteins is only 16%, so penetration through tissues is facilitated. For example, during a single infusion of 500 mg, the penetration into striated muscles was 69% and into adipose tissue was 49% [
34]. PK/PD profile was determined using the collected data, thus confirming that the possibility of reaching T > MIC (the time when the drug concentration is higher than Minimum Inhibitory Concentration (MIC)) about 30–40% is more than 90% when MIC is equal to 2 mg/L in soft, adipose and bone tissues are taken into account [
35]. For the safety of the antibiotic, an efficacy study was conducted with respect to the pharmacokinetic-dynamic index, in which serious side effects were excluded, and the most common side effect was a reversible change in taste [
36,
37].
According to the studies about using ceftobiprole in monotherapy, we can say that it is as effective as another antibiotic administered in the same indication. Furthermore, when compared to other cephalosporins, ceftobiprole shows a low risk of infection due to
Clostridium difficile, and when compared to ceftaroline, there are no neutropenia-related adverse effects [
38,
39]. The efficacy of ceftobiprole against ceftazidime in the treatment of nosocomial pneumonia was also analyzed. Obtained results showed a slight percentage difference in the incidence of serious side effects, to the detriment of ceftobiprole, 3.9% vs. 3.1% [
40]. During clinical trials, the effectiveness of ceftobiprole to vancomycin in the treatment of skin and soft tissue infections caused by Gram-positive microorganisms was compared, however no differences in tolerance were found [
41]. Another study compared ceftobiprol with a combination of vancomycin and ceftazidime in the treatment of infections such as purulent diabetic foot and wounds (postoperative, traumatic and burn), finding no difference in treatment effectiveness and similar drug tolerance [
42]. Despite good results and favourable safety and efficacy profiles, in 2010, the FDA and the EMA did not approve the use of ceftobiprole in tissue infection due to the absence or insufficient controls in about one-third of patients during clinical trials. The studies were found to be unreliable and were not conducted per good clinical practice [
43]. For this reason, Basilea Pharmaceutica has launched Phase 3 studies to determine the effectiveness of treatment and the safety of ceftobiprole in relation to vancomycin with aztreonam.
Ceftobiprole, like other antibiotics, should be monitored for drug levels in the blood (Therapeutic Drug Monitoring Test (TDM)) to reduce hospitalization time and improve safety. Appropriate procedures for the determination methods should therefore be established. In the hospital use, one of this methods is high-performance liquid chromatography (HPLC) with spectrophotometric detection (DAD). The process involves the quantitative determination of the substance using calibration solutions. Chromatographic separation was carried out in mobile phase with a composition of acetonitrile-phosphate buffer, on biphenyl column in linear gradient mode. Ceftobiprole was monitored at wavelength 320 nm. The method was validated and described by the guidelines of the European Medicines Agency demonstrating appropriate accuracy and precision. The other method for the determination of ceftobiprole is HPLC combined with tandem mass spectroscopy (MS/MS). Compared to the results obtained with the DAD detector, higher specificity and sensitivity are obtained. Future-oriented ceftobiprole studies are necessary to determine the exact therapeutic range with the required efficacy and safety [
44].
The main subject of the presented investigations was to develop and optimize the conditions for the determination of ceftobiprole using thin-layer chromatography with densitometric detection. TLC with densitometric detection is a rapid and not complicated analytical technique for the separation, identification and quantification of medicinal substances. Its simplicity, low cost and the need for minimal cleaning of the sample allows for conducting various types of analyzes in different areas of science. Furthermore, TLC technique allows to perform several analyses simultaneously. The developed and validated chromatographic-densitometric method for the determination of ceftobiprole can be an alternative to the used HPLC method and can also be used in kinetic studies. To our knowledge, this is the first report in the scientific literature to carry out such studies.
3. Results and Discussion
Nowadays, antibiotics are one of the more dynamically developing groups of medicines. Currently, research is being conducted which focuses on the search for new antibiotics with a broad spectrum of effects. One of the representatives of the latest fifth generation cephalosporins is ceftobiprole, which shows good activity against both, Gram-positive and Gram-negative bacteria, and an additionally extended spectrum with the mentioned methicillin-resistant strains MRSA. Ceftobiprole was first registered and approved for marketing and hospital treatment in Canada in 2008 under the name Zevtera. Other countries using this medicine were Switzerland and Ukraine. The indication for administration of this antibiotic is complex infections of the skin and soft tissues and community-acquired pneumonia. The uniqueness of ceftobiprole is based on its broad spectrum of action, thanks to which it can be administered during treatment against one or more microorganisms in monotherapy.
The main objective of this study was to establish a method for the qualitative and quantitative analysis of ceftobiprole by thin-layer chromatography with densitometric detection. For this purpose, firstly, a number of parameters were optimized such as a kind of stationary and mobile phase, method of stationary phase activation, the development path, the rate of solution application on the plates, the time of saturation of the chromatographic chamber, the time from the application of solution on the plate to its placement into the chamber. To optimise the conditions different types of chromatographic plates were tested, such as TLC Silica gel 60 F254, HPTLC Silica gel 60 F254 and HPTLC Cellulose. During analyses carried out on TLC Silica gel 60 F254 and HPTLC Silicagel 60 F254 plates in mobile phases with variable solvent compositions, characterised by different eluotropic strengths, no spots that could originate from ceftobiprole were observed. Probably, this could be due to the active substance remaining at the start point or moving with the eluent front, i.e., too high an affinity of the tested substance to the mobile or stationary phase. While, on HPTLC Cellulose plates, a compact peak originating from ceftobiprole without additional background interferences was recorded by both visual and densitometric detection.
Also, it was assessed whether the activation of Cellulose HPTLC plates (incubation in a drying apparatus at 60 °C for 24 h) affects improving the results of the analysis (compact spots with an appropriate RF values). No difference was observed in the obtained chromatographic image (peak shape and background level); the RF values obtained in 3 samples on each plate (activated and non-activated) was 0.32. The development time (about 40 min) also did not change.
In the study, mobile phases of the following composition were tested: chloroform: ethyl acetate: glacial acetic acid: water (4:4:4:1, v/v/v/v) and ethanol: 2-propanol: glacial acetic acid: water (4:4:1:3, v/v/v/v). It was found that a more favourable distribution (compact peak coming from the antibiotic, no blurring effect, an appropriate retardation factor value) was obtained using the second phase. The selected eluent was previously successfully used, for the quantification of cephalosporins 4th generation (cefepime). Both the type of stationary phase and the developing path (9.5 and 15 cm) were tested. It was observed that the extension of the path did not affect the quality of the obtained chromatogram, the retardation factors for each of the tested paths were similar, 0.32 and 0.33, respectively. The next step to optimise the assay was the speed of application of the ceftobiprole solution using the Linomat V. Two speeds were tested: 600 and 200 µL/s, and finally the second one was chosen due to the width of the obtained spots. A too-fast application speed, especially for aqueous solutions, resulted in the formation of large fuzzy spots.
The influence of the time from the moment of applying the solution on the plate to the moment of putting the plate in the chromatographic chamber, on the quality of the obtained chromatogram was also checked. The following time intervals were tested: 0, 5, 10, 15, 20 min. The results clearly demonstrated that the optimum time is 15 min; an increase in the time does not affect the quality of the chromatogram. The time of the chromatographic chamber saturation with the eluent vapour was also optimised, and finally fixed at 15 min.
After developing and drying at room temperature, chromatograms were detected under a UV lamp at wavelengths 254 nm and densitometrically. For the peaks recorded on the densitograms, absorption spectra in the range of 200–400 nm were recorded (
Figure 3). Further analyses were carried out at a wavelength of 232 nm, corresponding to the maximum absorption for ceftobiprole (
Figure 4).
The next stage of the study was to carry out a validation process for the method of ceftobiprole determination according to ICH guidelines. Determination of linearity range was conducted by applying spots of 0.001% standard solution to HPTLC Cellulose chromatography plates in volumes ranging from 2 to 50 µL. For the recorded surface areas, a dependence curve was plotted, and regression parameters were calculated. Three repetitions were made for each determination, taking the mean value for the calculation. The value of the correlation coefficient (r) of 0.9978 indicates a very good correlation between the concentration and peak area in the investigated linearity range from 0.02 to 0.35 µg/spot (
Figure 5a). The regression parameters were designated as follows: y = 12371.80x + 124.00, S
b = 96.41, S
a = 444.89, S
e = 125.93. The calculated LOD (0.0257 µg/spot) and LOQ (0.0779 µg/spot) values demonstrate the high sensitivity of the developed method.
Plotting the residuals enables to recognize problems with meagre or incorrect curve matching. Residuals analysis allows to check any regression assumptions and ensures that the obtained equation is correct. Thanks to this analysis we can easily and quickly detect outliers, which can distort the regression model. With this analysis, we can easily and quickly detect outliers that may distort the regression model. We can also detect inconsistencies between observed and predicted values. When the residuals are distributed randomly near zero, there is a good correlation between the obtained data and the regression model. The performed residual analysis confirmed the correctness of the obtained correlations, and
Figure 5b shows the residual scatter plot for the concentration values.
Cook’s distance is a parameter related to the removed residuals. Its purpose is to assess the degree of change in the regression coefficients when a case is omitted from the coefficient calculations. For our data the average value of Cook’s distance was 0.3331. For the received data, we can infer that the residuals placed near zero, and are randomly scattered without any patterns. So, the hypothesis of linearity is correct, confirmed by there being no trend (in the relation of residuals with concentration), and for the examined points there are no significant deviations that could violate the obtained regression.
The precision of the method was assessed by analysing peak areas registered for ceftobiprole, within the same day for intra-day precision, and after a week for inter-day precision. Nine spots of 30 µL each were applied to the chromatographic plate, and the analysis was performed in three replicates. The calculated low values of %RSD (1.61 for intra-day and 1.65 for inter-day) indicated high precision of the described procedure for ceftobiprole solutions.
The robustness of the developed TLC method with densitometric detection was estimated on the basis of slight changes in the experimental conditions, e.g., sorbent nature, chromatographic chamber size, saturation chamber time, developing path, and volume of solvents in mobile phase. During the estimation, RF values and absorption spectra were registered, and not valid changes were observed in chromatographic conditions, which confirms that described method is robust.
Then, the usefulness of the developed chromatographic-densitometric method for the determination of ceftobiprole was verified by the analysis of drug stability under stress conditions. For all determinations, 10 µL of a 0.01% ceftobiprole solution was applied onto the chromatography plates. Stability studies were conducted in solutions of 0.1 M HCL, 0.001 M HCL, 0.1 M NaOH, 0.001 M NaOH, distilled water and buffer pH 9.21. Samples were taken at hourly intervals (up to 5 h, and after 24 h) at 40 and 60 °C.
In all recorded densitograms, an additional peak with R
F close to 0.64 appeared, next to the main peak of ceftobiprole. It probably comes from the degradation product of the active ingredient (
Figure 6). The peaks were well separated and did not interfere with each other, which confirms the applicability of the developed method for the determination of ceftobiprole in the presence of additional compounds.
The obtained results indicate high stability of ceftobiprole in acidic and neutral medium. The concentration of the antibiotic, after 24 h of incubation in 0.1 M HCl decreased by 7.6%, and in water by about 13% in comparison to the initial value. It was observed that recorded surface areas (concentration) significantly decreased with increasing pH. In basic solutions, no peaks originating from the antibiotic were recorded after 24 h, which indicates its complete degradation. In 0.001 M NaOH, drug concentration successively decreased with incubation time, finally reaching 14.40% after 5 h. The degradation process was found to be faster when the drug was incubated in basic medium compared to the buffer solution. A similar relationship was found when analysing changes in the concentration of the antibiotic at 60 °C. It was observed that after an hour of incubation in 0.1 M NaOH, the ceftobiprole concentration decreased by 62.87%, i.e., more than half of the initial concentration, while after 4 h the concentration was only 6.37%. In the case of 0.01 M NaOH solutions, the areas of the recorded peaks decrease more slowly compared to more basic solutions; after 2 h of the experiment the drug concentration was 39.60% of the initial value, reaching 4.12% after 5 h. The conducted experiments show that the stability of ceftobiprole decreases with increasing alkalinity of the solutions and temperature (
Table 1).
Based on the calculated dependence of natural logarithms from ceftobiprole concentrations over time, the plotted curves of the dependence lnc = f(t) showed a rectilinear relationship. Therefore, it was found that the degradation of ceftobiprole in the studied conditions was consistent with the first order rates of kinetics reactions. Then, the values of the reaction rate constant (k) and t
0.5 and t
0.1 times were calculated (
Table 2).
The calculated values of kinetic parameters confirm the dependence that the degradation reaction rate constant increasing with the increase of pH and temperature (
Table 3). The k values are higher in sodium hydroxide solutions and lower in acidic ones. The lowest values of the reaction rate constant were obtained for solutions prepared in 0.1 and 0.01 M HCl (9.212 h
−1 at 40 °C), and the highest for 0.1 M NaOH at 60 °C (0.6886 h
−1).
The calculated values of t0.5 and t0.1, as well as the activation energy (Ea), confirm the higher stability of ceftobiprole in an acidic environment compared to alkaline one.
The stability of ceftobiprole was also tested by exposing solutions to radiation simulating sunlight (
Table 4). The tests were carried out on the Suntest CPS+ simulator equipped with a xenon lamp, which simulates natural sunlight in the wavelength range of 300–800 nm.
Analysing the obtained results, it can be concluded that the degradation process of ceftobiprole is also influenced by sunlight. By irradiating the aqueous solution of the antibiotic, it was found that after 3 h the concentration of ceftobiprole drops to 38.84%, while after 24 h drug is completely degraded. The degradation process follows the kinetics of the first-order reaction, which is confirmed by the determined dependencies of ln(c) as a function of time. Similarly, calculated kinetic parameters confirm that, under the solar irradiation, the degradation takes place at the rate of 0.5163 h−1 (t0.5 = 1.34 h).
We have observed that the degradation process of ceftobiprole takes place in solutions, and is strongly dependent on the environment (acidic, alkaline, radiation), temperature and incubation time. On the basis of the obtained results, it can be concluded that ceftobiprole is more susceptible to degradation in an alkaline environment than in an acidic one.
By conducting research on the behaviour of ceftobiprole in various conditions, new information about this substance was obtained. One of the most important features of a drug substance is lipophilicity. Therefore, it was decided to determine the logP values for the analysed antibiotic using the TLC technique and computational methods [
47]. In recent years, the RP-TLC technique was often used to assess the lipophilicity of many different substances, and then the relationship of this feature with biological activity was assessed [
48]. In the next stage of our research, lipophilicity was examined by RP-TLC method by determining appropriate R
F values. Then the R
M parameters were calculated, and analysed depending on the amount of organic modifier (methanol) in the used mobile phases. The obtained R
M values increased linearly with the decrease in the amount of methanol in eluent (regression coefficients r > 0.97;
Figure 7). Then, based on the linear relationship between the R
M values and the volume fraction of the organic modifier, the R
M0 values corresponding to 100% of water were obtained by extrapolation. As can be seen, the experimentally obtained R
M0 value for ceftobiprole (equivalent to the logP
exp value) is −1.4339.
Moreover, descriptors describing the lipophilicity of ceftobiprole were determined using the computational methods of the Virtual Computational Chemistry Laboratory, such as ALOGPs, AC_logP, ALOGP, MLOGP, XLOGP2, XLOGP3, ALOGPS and AClogS [
49]. All the results reflecting the lipophilic properties of ceftobiprole, both determined experimentally (as parameter R
M0 ≈ logP
exp) and by calculation methods are presented in
Figure 8.
When analyzing the received results, it can be noticed that logP values determined (as RM0 and calculated using different algorithms) for ceftobiprole ranged from −3.53 for ALOGPS to 0.07 MLOGP.
Based on the calculated data (
Figure 9) it can be concluded that the logP
exp lipophilicity parameter (R
M0) obtained in our study was the most similar to the computational data obtained by the ALOGP (based on electrotopological-state descriptors) and ALOGPs (based on the solubility descriptors) software, and both chromatographic and computational methods confirmed the hydrophilic character of ceftobiprole.
In summary, the presented study discusses the optimization and validation process of a new chromatographic-densitometric method for the determination of ceftobiprole, a fifth generation cephalosporin. The developed chromatographic method allows for both qualitative and quantitative determinations, and is characterized by the simplicity of determinations with the possibility of performing several analyses at the same time. Due to the above features, it is relatively quick to determine not only the content of a given compound, e.g., in a pharmaceutical product, but also its purity. The obtained validation parameters allow to conclude that the method guarantees reliable results of active substance determination in the low concentration range. In addition, it provides high sensitivity and precision at a relatively low research cost compared to other analytical methods. Additionally, it has been proven that the presented procedure can be used for the analysis of an active substance in free form, as well as in the presence of potential degradation products.